Abstract.
Significance
Hyperspectral near-infrared spectroscopy (hsNIRS) combined with diffuse correlation spectroscopy (DCS) provides a noninvasive approach for monitoring cerebral blood flow (CBF), the cerebral metabolic rate of oxygen () and the oxidation state of cytochrome-c-oxidase (oxCCO). is calculated by combining tissue oxygen saturation () with CBF, whereas oxCCO can be measured directly by hsNIRS. Although both reflect oxygen metabolism, a direct comparison has yet to be studied.
Aim
We aim to investigate the relationship between and oxCCO during periods of restricted oxygen delivery and lower metabolic demand.
Approach
A hybrid hsNIRS/DCS system was used to measure hemodynamic and metabolic responses in piglets exposed to cerebral ischemia and anesthetic-induced reductions in brain activity.
Results
Although a linear relationship was observed between and oxCCO during ischemia, both exhibited a nonlinear relationship with respect to CBF. In contrast, linear correlation was sufficient to characterize the relationships between and CBF and between the two metabolic markers during reduced metabolic demand.
Conclusions
The observed relationship between and oxCCO during periods of restricted oxygen delivery and lower metabolic demand indicates that the two metabolic markers are strongly correlated.
Keywords: near-infrared spectroscopy, diffuse correlation spectroscopy, cerebral blood flow, brain metabolism, cytochrome-c-oxidase
1. Introduction
The importance of adequate oxygen metabolism for maintaining cerebral health and function is well recognized considering the high energy demands of the brain—consuming 20% of the body’s total energy budget—and its reliance on blood flow for a constant supply of oxygen and glucose due to a lack of energy stores.1 Because of this dependency, inadequate oxygen delivery due to ischemia is a major cause of secondary brain injury in critical care patients recovering from life-threatening neurological emergencies, such as severe traumatic brain injury and subarachnoid hemorrhage.2,3 Independent of inadequate cerebral blood flow (CBF), another cause of secondary brain injury is mitochondrial dysfunction resulting from a hypoxic-ischemic insult. Mitochondrial dysfunction is also a major pathophysiological mechanism of neonatal encephalopathy and the neurologic sequela following cardiac arrest.4,5
Since its initial inception, one of the primary motivations for using near-infrared spectroscopy (NIRS) as a bedside neuromonitoring device has been to assess oxygen metabolism.6 The most frequently used parameter is tissue oxygen saturation (), although it is not a direct marker of metabolism because blood oxygenation also depends on CBF.7 Based on the Fick principle, the cerebral metabolic rate of oxygen () can be determined by combining , CBF, and arterial oxygen saturation () measurements. Initial applications used bolus-tracking methods to measure CBF;8,9 however, the emergence of diffuse correlation spectroscopy (DCS) has enabled continuous monitoring.10,11 The combination of NIRS and DCS has been used to measure CBF and in clinical studies involving neonatal and adult patient populations.12–16
Due to the unique light-absorbing properties of cytochrome-c-oxidase (CCO), NIRS offers an alternative approach for assessing oxygen metabolism by measuring changes in the oxidation state of CCO (oxCCO).17 This metabolic marker is directly related to mitochondrial ATP production and has the advantage of not requiring separate measurements of CBF and , nor does it depend on assuming a fixed arteriovenous blood volume ratio required to convert to venous oxygen saturation as required to determine .18,19 Another advantage of the oxCCO is that its concentration is much higher in the brain than in extracerebral tissues; therefore, it is less sensitive to extracerebral layers contamination than the hemoglobin signals. The challenge with monitoring oxCCO is that the in vivo concentration of CCO is at least an order of magnitude lower than the hemoglobin concentration.
Broadband or hyperspectral NIRS (hsNIRS) has proven to be the most reliable approach for measuring oxCCO changes accurately,20 even in the face of larger oxy- and deoxyhemoglobin signals ( and Hb, respectively). The absorption spectrum of the oxCCO is relatively broad (720 to 920 nm) without any strong features, and it overlaps with the hemoglobins’ spectra. Consequently, the multiwavelength approach improves the reliability of the measured oxCCO changes. Clinical studies have shown the ability of hsNIRS to detect oxCCO changes associated with neonatal hypoxic-ischemic encephalopathy, preterm birth, and cardiac surgery.21–25
A disadvantage with measuring oxCCO is the lack of a suitable commercial monitor given the requirement of hyperspectral measurements to minimize crosstalk between chromophores. In contrast, a number of NIRS/DCS devices, some of which are available commercially, have been developed to quantify CBF and .26,27 Considering that and the redox state of CCO both reflect cellular oxygen metabolism, it is reasonable to expect that these two parameters should be correlated, provided the electron transport chain has a ready supply of electrons from substrates (primarily NADH, nicotinamide adenine dinucleotide (NAD) + hydrogen (H)), and there is no change in CCO concentration.28 To test this hypothesis, this study consisted of two experiments aimed at altering cerebral oxygen metabolism. Both sets of experiments were conducted in newborn piglets to avoid signal contamination from extracerebral tissues. In the first set, carotid occlusion was used to restrict oxygen delivery to the brain, which causes a corresponding decrease in metabolism.29 In the second set, cerebral metabolic demand was reduced without impeding CBF by altering the anesthetics administered to the animals.8 Experiments were performed using a hybrid hsNIRS/DCS system capable of collecting CBF, , Hb, and oxCCO data simultaneously. In addition, absolute baseline CBF was measured by a bolus-tracking method to convert DCS measurements into physiological units of blood flow.30
2. Methods
2.1. Instrumentation
All data were collected using an in-house built hsNIRS/DCS system that incorporated a multiplexing shutter system to cycle between data acquisition from the two subsystems.23,24 The NIRS light source was a 20-W halogen bulb (Hl-2000-HP, Ocean Optics) that was filtered from 600 to 1000 nm and coupled into a custom optical fiber bundle (active diameter 2.4 mm, fiber core , , Loptek, Germany) to direct the light to the head. Reflected broadband light from the interrogated tissue was collected at a source–detector distance of 3 cm by three fiber bundles (bundle active diameter 2 mm, fiber core diameter , , Loptek, Germany) that were linearly aligned at the entrance of the spectrometer (iDus 420, to 1085 nm, ; Andor, Oxford Instruments, Canada).
For the DCS module, light from a continuous laser with a long coherence length () emitting at (DL785-100s, CrystaLaser) was coupled into a single fiber (fiber core diameter , , Loptek, Germany). On the detection side, light was collected at a source–detector distance of 2 cm by single-mode fibers (core diameter , , Loptek, Berlin, Germany) coupled to a four-channel single-photon counting module (SPCM-AQR-15-FC, Excelitas Technologies, Canada). Each counting module generated TTL pulses sent to an edge-detecting photon counter on a PCIe6612 counter/timer data acquisition board (National Instrument).27,31 Photon counts were recorded and processed using in-house developed software written in LabVIEW (2017 SP1, National Instruments) and MATLAB (2016b, MathWorks). Intensity autocorrelation curves were generated for each detector at 40 delay times () ranging from 1 to .32
2.2. Animal Preparation
Animal experiments were conducted in accordance with the guidelines of the Canadian Council of Animal Care (CCAC) and approved by the Animal Care Committee at Western University. Young piglets (age ranged from 12 to 216 h) were initially anesthetized with 5% isoflurane, which was reduced to 3% for surgical procedures and maintained at 2% to 3% during the experiment. Piglets were tracheotomized and mechanically ventilated on an oxygen-medical air mixture. Incisions were made lateral to the trachea, and vascular occluders (In Vivo Metric, California were placed around the carotid arteries posterior to the clavicle. Catheters were inserted into both ear veins for injections and into a femoral artery to collect arterial blood samples for gas and glucose analyses and for monitoring arterial blood pressure. Vital signs [heart rate (HR), , end-tidal tension, respiratory rate, blood pressure, and temperature] were monitored continuously (SurgiVet, Smiths Medical, Minnesota). Piglets were placed in the prone position with the hsNIRS and DCS probes secured to the top of the head using an in-house three-dimensional-printed probe holder.
2.3. Experimental Procedure
After a stabilization period of following surgery, a bolus of propofol () was administered intravenously to reduce cerebral energy metabolism.33 After a second delay of to allow propofol effects to wear off, the carotid occluders were inflated to reduce global CBF and released after 10 min to restore normal blood flow. The hybrid system was used to collect broadband and DCS data throughout the two procedures continuously. The shutter system cycled between the hsNIRS and DCS systems in 3-s intervals with an additional 0.5-s delay added between intervals to account for shutter transition times and avoid any cross contamination between the two systems. For both systems, data were acquired at 4 Hz during each 3-s interval, which were subsequently averaged to generate a single measurement every 7 s. The final step was to measure absolute CBF by dynamic contrast-enhanced NIRS. The protocol consisted of an intravenous bolus injection of indocyanine green (ICG, ). The rapid passage of the dye through the brain was recorded by continuous hsNIRS acquisition at a temporal resolution of 250 ms. The corresponding time-varying arterial ICG concentration, required for flow quantification, was measured using a dye densitometer attached to a front paw (DDG 2001, Nihon Kohden, Japan).
2.4. Data Analysis
2.4.1. Hyperspectral NIRS analysis
Details of the hsNIRS data analysis have been described previously.29 For each animal, a reference spectrum () and a dark count spectrum () were acquired at the beginning of each experiment. A baseline reflectance spectrum was determined from spectra () collected prior to propofol infusion using the following:
| (1) |
The first and second derivatives of were fit with the solution to the diffusion approximation for a semi-infinite homogeneous medium34 to generate estimates of the tissue water fraction, and Hb concentrations, and two scattering parameters [wavelength-dependent power and the reduced scattering coefficient () at 800 nm].24 Fitting was performed using a constrained minimization algorithm based on the MATLAB function fminsearchbnd. The estimates of and Hb concentrations were used to calculate baseline tissue oxygen saturation ().
A modified Beer–Lambert law based on the UCLn algorithm was used to calculate subsequent changes in Hb, , and oxCCO concentrations.17 For this analysis, the differential pathlengths for each animal were calculated by fitting the second derivative of the average baseline to the second derivative of the water absorption spectrum35 and correcting for the wavelength dependence of the pathlength.36 The UCLn algorithm was performed twice. First, to quantify changes in oxCCO concentration () from attenuation changes between 770 and 906 nm.17 This wavelength range is optimized for oxCCO as it avoids the large deoxyhemoglobin absorption feature at .37 Next, the analysis was repeated for the wavelength range between 680 and 850 nm to determine changes in Hb and concentrations.38 It was previously shown that this range provides a good assessment of tissue saturation because absorption changes are dominated by oxy and deoxyhemoglobin.39 Tissue oxygen saturation at each time point was determined by combining the relative changes derived from the UCLn algorithm with the absolute baseline value obtained by derivative spectroscopy. The resulting times series of , , and were smoothed with a zero-phase digital filter (filtfilt, MATLAB, 2016b, MathWorks).
2.4.2. DCS analysis
Normalized intensity autocorrelations functions were converted to electric field autocorrelation data using the Siegert relation.40 Each autocorrelation function was subsequently fit with the solution to the diffusion approximation for a semi-infinite homogenous medium. The fitting incorporated coherence factor () dynamic measurements obtained by hsNIRS and assuming .41 An assumed value of was used instead of the estimate from the analysis of the hsNIRS data, as differential spectral analysis has been shown to underestimate .34 The fitting variable was a blood flow index (BFi) based on modelling tissue perfusion as a pseudo-Brownian motion.10 Fitting was performed across all correlation times from 1 to . The resulting BFi time courses were smoothed with the same filter (zero-phase digital filtering, filtfilt, MATLAB, 2016b, MathWorks) as the hsNIRS data.
2.4.3. Dynamic contrast-enhanced NIRS
Baseline CBF was quantified by relating the time-varying arterial concentration of ICG, , to the corresponding brain concentration curve, :
| (2) |
where is the impulse residue function and ∗ refers to the convolution operator. The product CBF · was extracted by deconvolution,42 from which CBF was determined by the initial value, for by definition equals 1. The same fitting algorithm used to determine the baseline optical properties was used to determine with ICG concentration as the only fitting parameter.
2.4.4. Calculating the cerebral metabolic rate of oxygen
The final step was to calculate the (ml ), which was based on the standard mass balance equation relating to CBF and :32,43
| (3) |
where is the oxygen-carrying capacity of hemoglobin (1.39 ml of per g Hb);44 tHb is the total hemoglobin concentration, which was determined from the baseline arterial blood sample; and is the venous volume fraction, which was set to 0.75.32,43 The CBF time series in physiological units of blood flow (i.e., ) was generated by scaling BFi data by baseline CBF measured by contrast-enhanced NIRS.
2.5. Statistical Analysis
All data are presented as mean standard error, and statistical significance was defined as .
The relationships between changes in each metabolic parameter and CBF and between the two metabolic parameters were assessed using a least-squares algorithm to fit a power-law relationship:
| (4) |
where is a scaling factor, is the power exponent, was either the change in () or , and was either the change in CBF () or . For this analysis, time series were converted into bins that had a width of when was the independent variable and when was the independent variable. A paired -test was used to determine if the mean value of for each test was statistically different from one. Linear regression was used in cases in which the difference did not reach significance.
3. Results
Data were acquired from six piglets. Relevant baseline physiological parameters are provided in Table 1. Each experiment, including both procedures, took on average to complete. Average baseline CBF and measured by dynamic contrast-enhanced NIRS were and , respectively.
Table 1.
Physiological parameters.
| Parameter | Piglet no. | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Sex | Female | Male | Male | Female | Female | Female |
| Age (h) | 216 | 12 | 60 | 48 | 24 | 12 |
| Weight (kg) | 4.1 | 1.9 | 2.7 | 2.5 | 1.7 | 2.0 |
| Blood pressure (mmHg) | 46 | 40 | 38 | 44 | 45 | 34 |
| HR () | 166 | 146 | 138 | 169 | 163 | 129 |
| (%) | 95 | 99 | 98 | 98 | 98 | 99 |
| tHb (g/dl) | 4.5 | 6.1 | 8.0 | 7.2 | 6.3 | 6.7 |
| Temperature (°C) | 37.7 | 38.6 | 37.9 | 38.5 | 38.5 | 37.9 |
| (mmHg) | 35.3 | 37.7 | 40.0 | 36.6 | 37.7 | 35.9 |
| (mmHg) | 265 | 263 | 260 | 186 | 260 | 324 |
| Respiratory rate () | 42 | 55 | 51 | 51 | 55 | 45 |
| Glucose (mM) | 10.5 | 7.7 | 5.2 | 7.1 | 5.5 | 6 |
| () | 51.5 | 57.0 | 59.8 | 57.7 | 46.2 | 44.9 |
| () | 1.29 | 3.19 | 1.73 | 1.44 | 0.55 | 0.76 |
, arterial oxygen saturation; , arterial partial pressure of carbon dioxide; , arterial partial pressure of oxygen; tHb, total hemoglobin concentration; , baseline cerebral blood flow; , baseline cerebral metabolic rate of oxygen.
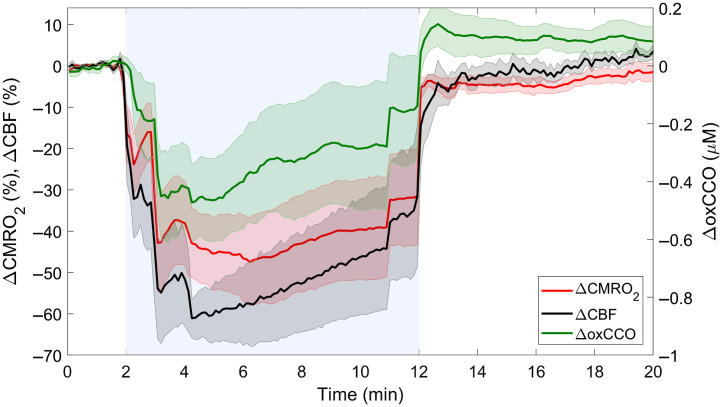
Figure 1 presents average changes in CBF, , and oxCCO during carotid occlusion. All three parameters exhibited rapid changes at the beginning and end of the occlusion period. The biphasic responses observed at these transition periods were a consequence of sequential inflating/releasing of the occluders. Complete carotid occlusion resulted in a maximum CBF reduction of or relative to baseline. The corresponding nadir was or , and the maximum reduction in oxCCO was .
Fig. 1.
Average temporal changes in CBF, , and oxCCO in response to carotid occlusion, which is indicated by the blue region between 2 and 12 min. Time courses were averaged across animals, and shading surrounding each line represents the standard error of the mean.
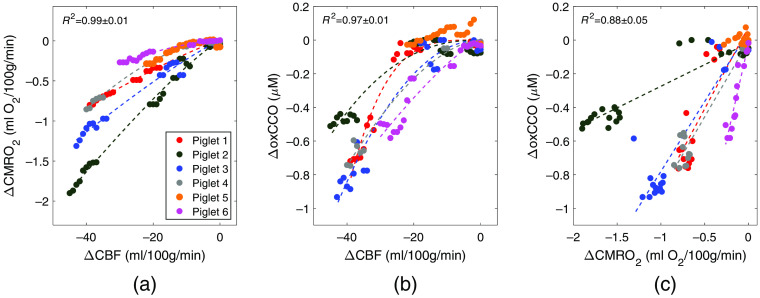
Figure 2 presents the results of the regression analysis used to determine the relationships among the three parameters during carotid occlusion: (a) and , (b) and , and (c) and . The analysis was conducted for each animal separately, and all changes are relative to preocclusion values. The results from one animal (piglet 5, orange symbols in Fig. 2) were not included in the regression analysis as the reduction in CBF was modest () compared with the other animals () with no appreciable change in oxCCO, which was likely due to insufficient occlusion. To investigate the potential influence of inter-subject variability in the physiological parameters (Table 1) on the reconstructed CBF changes, linear regression was conducted between each physiological parameter and , and no statistically significant relationship was found for any of the parameters. Based on the remaining five animals, the average exponent of the power law () was for versus and for versus . These values were significantly greater than one but not significantly different from each other. In contrast, the mean value of characterizing the relationship between and was not statistically different from one, and therefore linear regression was used to characterize this relationship. Results of the regression analysis for each animal, including the coefficient of determination, are presented in Table 2.
Fig. 2.
Correlation plots showing the relationship between changes in the two metabolic parameters ( and ) and corresponding changes in CBF () in response to carotid occlusion: (a) versus and (b) versus . Plot (c) presents the relationship between and . Each color indicates data from an individual animal. Dashed lines represent the best-fit lines of the power law in (a) and (b) and linear regression in (c).
Table 2.
Best-fit estimates of the power law exponent () from individual animals. Results from linear regression for are also presented.
| Animal no. | |||||||
|---|---|---|---|---|---|---|---|
| Slope | Intercept | ||||||
| 1 | 1.18 | 1.00 | 3.71 | 0.98 | 0.97 | 0.08 | 0.81 |
| 2 | 1.17 | 1.00 | 2.37 | 0.96 | 0.26 | −0.02 | 0.88 |
| 3 | 1.15 | 0.99 | 2.07 | 0.97 | 0.83 | 0.05 | 0.88 |
| 4 | 1.79 | 1.00 | 1.71 | 0.99 | 0.89 | −0.01 | 0.95 |
| 6 | 1.67 | 0.99 | 1.27 | 0.96 | 2.28 | −0.03 | 0.88 |
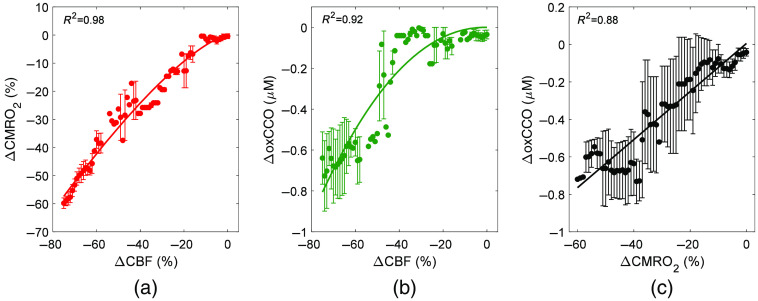
Figure 3 shows the relationships between the three parameters during carotid occlusion averaged across animals. Relative changes are presented to remove the variability observed between animals in Fig. 2. Best-fit estimates of were 1.37 for versus and 2.14 for versus . Linear regression revealed a strong correlation between and with a slope of per % and an intercept of .
Fig. 3.
Relationship between relative metabolic and blood flow changes in response to carotid occlusion: (a) versus , (b) versus , and (c) versus . Data were averaged across five animals, and the solid lines represent the best fit of either the power law in (a) and (b) or linear regression in (c). Error bars represent the standard deviation across animals.
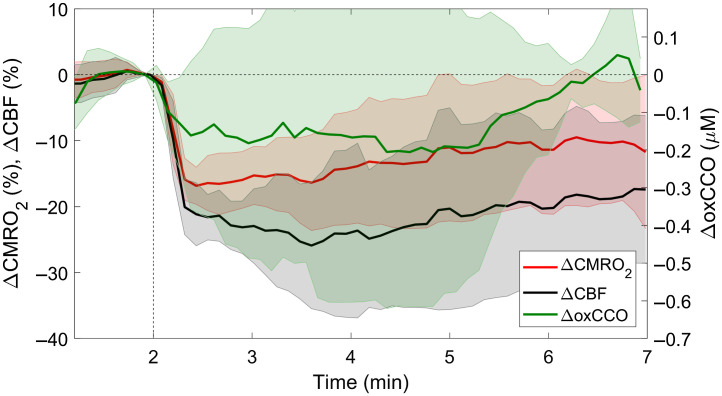
Figure 4 presents average changes in CBF, , and oxCCO in response to propofol injection. The maximum CBF reduction was (), with a corresponding decrease in of () and oxCCO of .
Fig. 4.
Average changes in CBF, , and oxCCO in response to a bolus injection of propofol () administered at the 2-min mark (indicated by the vertical dashed line). Each time course was averaged across six animals, and the shading surrounding each line represents the standard error of the mean.
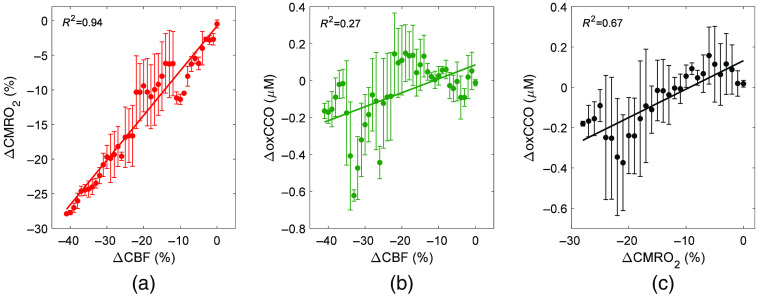
Compared with carotid occlusion, the decreases in CBF, , and oxCCO following propofol injection were relatively small. Consequently, linear regression analysis was used to characterize the relationship between the metabolic parameters and CBF instead of the power law (Fig. 5). The analysis revealed a strong correlation between changes in CBF and ; however, only a weak-to-moderate relationship was observed between and . Finally, a moderate-to-strong linear relationship was found between and .
Fig. 5.
Correlation plots of the relationship between (a) and , (b) and , and (c) and in response to propofol injection. The solid lines represent the results of linear regression: (a) , , (% ); (b) , , ; and (c) , , . Error bars represent the standard deviation across animals.
4. Discussion
The motivation for this study was to investigate the relationship between the two metabolic markers that can be assessed by NIRS: the cerebral metabolic rate of oxygen and the oxidation state of cytochrome-c-oxidase. The main finding was that and remained coupled when oxygen delivery to the brain was restricted and when the cerebral metabolic demand was lowered.
The mean CBF time course shown in Fig. 1 illustrates the expected decrease in global cerebral perfusion caused by carotid occlusion. On average, CBF decreased by , corresponding to an average value of at its nadir. This value is within the range reported for the ischemic threshold,45 although brain injury from this type of whole-brain insult typically requires durations longer than 10 min and the combination of hypoxia and ischemia.46 Nevertheless, the correlation plots in Figs. 2 and 3 demonstrate that the impact on oxygen delivery was significant enough to cause sizable reductions in and oxCCO. Power law analysis revealed that both decreases in and oxCCO exhibited a nonlinear relationship with respect to concurrent decreases in CBF. Similar findings have been previously reported for during middle cerebral artery occlusion in pigs and for oxCCO in a piglet model of hypoxia-ischemia and in patients during cardiac surgery.23,29,47 The dampened metabolic responses reflect the compensatory increase in oxygen extraction that occurs in an effort to match energy demands.48 In contrast, a strong linear correlation between decreases in and oxCCO was found (), indicating that impeding oxygen delivery had a similar effect on both markers. The results presented in Fig. 2 showed a large variation in the dynamic relationship between the two metabolic markers. Two extrema can be observed (animals 2 and 6) in which the amplitudes of the responses were opposite for the two metabolic markers. The values given in Table 1 show that these two animals also had the lowest (#6) and highest (#2) baseline values. To investigate the potential influence of the baseline oxygen consumption on the relationship between the two metabolic markers, we conducted a linear regression between and the slopes given in Table 2. A moderate-to-strong linear relationship was found (), but it did not reach statistical significance (). These results suggest that the metabolic response in the brain to reduced oxygen delivery does depend on the initial baseline metabolic rate.
The reduction in brain activity caused by injecting the anesthetic propofol resulted in a different relationship between cerebral perfusion and metabolism compared with that observed during carotid occlusion. In this case, the lower metabolic demand was matched by a similar reduction in CBF, as evident by the strong linear correlation between CBF and (Fig. 5; ). This finding of proportional decreases in CBF and following propofol infusion agrees with previous studies.33,49 Overall, the effects of propofol were small compared with carotid occlusion, with roughly 50% smaller reductions in CBF, , and oxCCO. Most likely, the background isoflurane anesthesia tempered the effects of propofol. Only a weak correlation was found between and () due to the considerable variability observed in the data (Fig. 4) as the small magnitude of the changes was close to the precision limits of the measurements. It is possible that the direct effects of propofol on oxidative substrate levels could have counteracted the reduction in oxCCO50,51 caused by lowering cerebral energy demands. However, the decreases in oxCCO for the two sets of experiments were similar for the same change in CBF. Despite the weak correlation between and , a moderate-to-strong correlation () was found between and . In agreement with these experimental results, a model designed to simulate the regulation of brain hemodynamics and metabolism predicts a linear relationship between and oxCCO during modest changes in energy demands (i.e., changes in ).28
The results of this study should not be interpreted as suggesting that and oxCCO are always coupled. Indeed, previous studies have illustrated conditions in which changes in oxCCO occur with no measurable difference in . The treatment of patent ductus arteriosus in preterm infants by the cyclooxygenase inhibitor indomethacin reduces oxCCO52 but does not affect despite the vasodilatory effects of the drug.14,53 Likewise, moderate hypercapnia increases oxCCO,54 along with CBF, but is generally considered not to alter .32,55 These discrepancies indicate that some conditions can lead to fluctuations in intracellular oxygen tension that are not sufficient to affect the mitochondrial respiratory rate. A more complete understanding of the intricate relationship between and oxCCO should account for other variables that can influence the oxCCO signal, including the availability of respiratory electrons and the rate of ATP utilization.17 Imaging of glucose metabolism could be used to gauge substrate supply and phosphorus magnetic resonance spectroscopy to assess the rate of ATP hydrolysis.56,57
A limitation of this study was the small sample size. Five successful experiments were sufficient to show that the relationship between the two metabolic parameters and CBF during carotid occlusion were better characterized by the power law than linear regression. However, the study did not have sufficient power to determine if the two responses were different as suggested by their exponents ( for and for ). Based on these average and standard deviations values, power analysis indicated that an additional five data sets would be required to assess statistical difference between the metabolic markers. The higher exponent for agrees with the concept that low oxygen tension is required to reduce CCO.58 In terms of , a potential confounding factor could be applying the Fick principle [i.e., Eq. (3)], which assumes a steady-state, to dynamic CBF and data. Furthermore, possible changes in the assumed venous fraction (), which was fixed to 0.75, would also affect the accuracy of the measurements.19
5. Conclusions
In summary, combining hsNIRS with DCS provided a means of assessing the relationship between and oxCCO. Moderate-to-strong linear correlations were found between the two metabolic parameters in response to reductions in global CBF and brain activity. These results indicate that, under these conditions, and oxCCO provided similar information regarding cerebral energy metabolism. More studies are required to determine if this agreement would extend to clinically relevant conditions such as perinatal hypoxia-ischemia, considering mitochondrial dysfunction is a major contributor to delayed brain injury.19,21 Given the differences in technologies required to monitor and oxCCO, it would be valuable to determine which metric, or perhaps the combination, could help detect early evidence of cerebral metabolic distress.
Acknowledgments
The authors would like to thank Drs. Chris E. Cooper and Ilias Tachtsidis for their helpful discussions regarding interpreting the oxCCO signals. This work was funded through grants from the Canadian Institutes of Health Research (130391) and the Natural Sciences and Engineering Research Council of Canada (R3592A02002).
Biographies
Daniel Milej is a research associate at Lawson Health Research Institute in London, Canada. He received his PhD in biomedical engineering from the Nalecz Institute of Biocybernetics and Biomedical Engineering, Polish Academy of Sciences, in 2014. His current research focuses on designing, developing, and implementing sophisticated optoelectronic medical and clinical instrumentation, specifically brain imaging using time-domain diffuse optics and diffuse correlation spectroscopy.
Ajay Rajaram received his BSc degree in medical physics from McMaster University and his PhD in medical biophysics from Western University in Canada. He is currently a postdoctoral fellow at Boston Children’s Hospital and Harvard Medical School. His research focuses on the clinical translation of optical neuromonitoring and imaging tools for early detection of brain development and injury in neonatal populations.
Marianne Suwalski is a PhD candidate in the Department of Medical Biophysics at Western University. She received her MD from the Medical University of Warsaw in Warsaw, Poland. Her current research focuses on monitoring the brain with broadband near-infrared spectroscopy and diffuse correlation spectroscopy during cardiothoracic surgery.
Leena N. Shoemaker is a postdoctoral associate at Western University in London, Canada. She received her PhD in cerebrovascular and exercise physiology from Otago University in Dunedin, New Zealand, in 2020. Her current research focuses on utilizing a combination of imaging methods (including ultrasound and optical monitoring systems) to elucidate the vascular mechanics of the cerebral micro- and macrovasculature. She is particularly interested in the role of exercise in dampening age-related declines in cerebrovascular and cognitive function.
Keith St. Lawrence is a professor in the Department of Medical Biophysics at Western University. His research focuses on developing quantitative methods of imaging cerebral blood flow and energy metabolism. His research encompasses a number of modalities, including diffuse optics, functional near-infrared spectroscopy, magnetic resonance imaging, and positron emission tomography.
Laura B. Morrison: Biography is not available.
Disclosures
The authors of this paper report no relevant financial interests or other potential conflicts of interest to disclose.
Contributor Information
Daniel Milej, Email: dmilej@uwo.ca.
Ajay Rajaram, Email: Ajay.Rajaram@childrens.harvard.edu.
Marianne Suwalski, Email: msuwalsk@uwo.ca.
Laura B. Morrison, Email: lmorriso@lawsonimaging.ca.
Leena N. Shoemaker, Email: lshoemak@uwo.ca.
Keith St. Lawrence, Email: kstlaw@lawsonimaging.ca.
Code, Data, and Materials Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Rolfe D. F. S., Brown G. C., “Cellular energy utilization and molecular origin of standard metabolic rate in mammals,” Physiol. Rev. 77(3), 731–758 (1997). 10.1152/physrev.1997.77.3.731 [DOI] [PubMed] [Google Scholar]
- 2.Posti J. P., Raj R., Luoto T. M., “How do we identify the crashing traumatic brain injury patient: the neurosurgeon’s view,” Curr. Opin. Crit. Care 27, 87–94 (2021). 10.1097/MCC.0000000000000799 [DOI] [PubMed] [Google Scholar]
- 3.Miller C., et al. , “Monitoring of cerebral blood flow and ischemia in the critically ill,” Neurocrit. Care 21, 121–128 (2014). 10.1007/s12028-014-0021-9 [DOI] [PubMed] [Google Scholar]
- 4.Davidson J. O., et al. , “Update on mechanisms of the pathophysiology of neonatal encephalopathy,” Semin. Fetal Neonatal Med. 26, 101267 (2021). 10.1016/j.siny.2021.101267 [DOI] [PubMed] [Google Scholar]
- 5.Sekhon M. S., Ainslie P. N., Griesdale D. E., “Clinical pathophysiology of hypoxic ischemic brain injury after cardiac arrest: a ‘two-hit’ model,” Crit. Care 21, 90 (2017). 10.1186/s13054-017-1670-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jöbsis F. F., “Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters,” Science 198(4323), 1264–1267 (1977). 10.1126/science.929199 [DOI] [PubMed] [Google Scholar]
- 7.Boas D. A., Franceschini M. A., “Haemoglobin oxygen saturation as a biomarker: the problem and a solution,” Philos. Trans. R. Soc. A: Math. Phys. Eng. Sci. 369(1955), 4407–4424 (2011). 10.1098/rsta.2011.0250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tichauer K. M., et al. , “Measurement of cerebral oxidative metabolism with near-infrared spectroscopy: a validation study,” J. Cereb. Blood Flow Metab. 27(4), 873–873 (2006). 10.1038/sj.jcbfm.9600397 [DOI] [PubMed] [Google Scholar]
- 9.Yoxall C. W., Weindling A. M., “Measurement of cerebral oxygen consumption in the human neonate using near infrared spectroscopy: cerebral oxygen consumption increases with advancing gestational age,” Pediatr. Res. 44, 283–290 (1998). 10.1203/00006450-199809000-00004 [DOI] [PubMed] [Google Scholar]
- 10.Durduran T., Yodh A. G., “Diffuse correlation spectroscopy for non-invasive, micro-vascular cerebral blood flow measurement,” Neuroimage 85, 51–63 (2014). 10.1016/j.neuroimage.2013.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Durduran T., et al. , “Diffuse optical measurement of blood flow, blood oxygenation, and metabolism in a human brain during sensorimotor cortex activation,” Opt. Lett. 29(15), 1766 (2004). 10.1364/OL.29.001766 [DOI] [PubMed] [Google Scholar]
- 12.Buckley E. M., et al. , “Early postoperative changes in cerebral oxygen metabolism following neonatal cardiac surgery: effects of surgical duration,” J. Thorac. Cardiovasc. Surg. 145, 196–203 (2013). 10.1016/j.jtcvs.2012.09.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dehaes M., et al. , “Cerebral oxygen metabolism in neonatal hypoxic ischemic encephalopathy during and after therapeutic hypothermia,” J. Cereb. Blood Flow Metab. 34(1), 87–94 (2014). 10.1038/jcbfm.2013.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diop M., et al. , “Development of a combined broadband near-infrared and diffusion correlation system for monitoring cerebral blood flow and oxidative metabolism in preterm infants,” Biomed. Opt. Express 6(10), 3907–3918 (2015). 10.1364/BOE.6.003907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker W. B., et al. , “Continuous non-invasive optical monitoring of cerebral blood flow and oxidative metabolism after acute brain injury,” J. Cereb. Blood Flow Metab. 39(8), 1469–1485 (2019). 10.1177/0271678X19846657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zavriyev A. I., et al. , “The role of diffuse correlation spectroscopy and frequency-domain near-infrared spectroscopy in monitoring cerebral hemodynamics during hypothermic circulatory arrests,” JTCVS Tech. 7(C), 161–177 (2021). 10.1016/j.xjtc.2021.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bale G., Elwell C. E., Tachtsidis I., “From Jöbsis to the present day: a review of clinical near-infrared spectroscopy measurements of cerebral cytochrome-c-oxidase,” J. Biomed. Opt. 21(9), 091307 (2016). 10.1117/1.JBO.21.9.091307 [DOI] [PubMed] [Google Scholar]
- 18.Watzman H. M., et al. , “Arterial and venous contributions to near-infrared cerebral oximetry,” Anesthesiology 93(4), 947–953 (2000). 10.1097/00000542-200010000-00012 [DOI] [PubMed] [Google Scholar]
- 19.Tichauer K. M., et al. , “Using near-infrared spectroscopy to measure cerebral metabolic rate of oxygen under multiple levels of arterial oxygenation in piglets,” J. Appl. Physiol. 109(3), 878–885 (2010). 10.1152/japplphysiol.01432.2009 [DOI] [PubMed] [Google Scholar]
- 20.Matcher S. J., et al. , “Performance comparison of several published tissue near-infrared spectroscopy algorithms,” Anal. Biochem. 227(1), 54–68 (1995). 10.1006/abio.1995.1252 [DOI] [PubMed] [Google Scholar]
- 21.Bale G., et al. , “Oxygen dependency of mitochondrial metabolism indicates outcome of newborn brain injury,” J. Cereb. Blood Flow Metab. 39(10), 2035–2047 (2019). 10.1177/0271678X18777928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harvey-Jones K., et al. , “Role of optical neuromonitoring in neonatal encephalopathy—current state and recent advances,” Front. Pediatr. 9, 653676 (2021). 10.3389/fped.2021.653676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rajaram A., et al. , “Optical monitoring of cerebral perfusion and metabolism in adults during cardiac surgery with cardiopulmonary bypass,” Biomed. Opt. Express 11(10), 5967–5981 (2020). 10.1364/BOE.404101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rajaram A., et al. , “Perfusion and metabolic neuromonitoring during ventricular taps in infants with post-hemorrhagic ventricular dilatation,” Brain Sci. 10(7), 452 (2020). 10.3390/brainsci10070452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rajaram A., et al. , “Assessing cerebral blood flow, oxygenation and cytochrome c oxidase stability in preterm infants during the first 3 days after birth,” Sci. Rep. 12, 181 (2022). 10.1038/s41598-021-03830-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen T. N., et al. , “Hyperspectral near-infrared spectroscopy assessment of the brain during hypoperfusion,” J. Biomed. Opt. 24(3), 035007 (2019). 10.1117/1.JBO.24.3.035007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Milej D., et al. , “Characterizing dynamic cerebral vascular reactivity using a hybrid system combining time-resolved near-infrared and diffuse correlation spectroscopy,” Biomed. Opt. Express 11(8), 4571 (2020). 10.1364/BOE.392113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Banaji M., et al. , “A model of brain circulation and metabolism: NIRS signal changes during physiological challenges,” PLoS Comput. Biol. 4, e1000212 (2008). 10.1371/journal.pcbi.1000212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rajaram A., et al. , “Simultaneous monitoring of cerebral perfusion and cytochrome c oxidase by combining broadband near-infrared spectroscopy and diffuse correlation spectroscopy,” Biomed. Opt. Express 9(6), 2588–2603 (2018). 10.1364/BOE.9.002588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diop M., et al. , “Calibration of diffuse correlation spectroscopy with a time-resolved near-infrared technique to yield absolute cerebral blood flow measurements,” Biomed. Opt. Express 2(7), 2068–2081 (2011). 10.1364/BOE.2.002068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khalid M., et al. , “Development of a stand-alone DCS system for monitoring absolute cerebral blood flow,” Biomed. Opt. Express 10(9), 4607–4620 (2019). 10.1364/BOE.10.004607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Milej D., et al. , “Direct assessment of extracerebral signal contamination on optical measurements of cerebral blood flow, oxygenation, and metabolism,” Neurophotonics 7(4), 045002 (2020). 10.1117/1.NPh.7.4.045002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Narciso L., et al. , “A noninvasive method for quantifying cerebral metabolic rate of oxygen by hybrid PET/MRI: validation in a Porcine model,” J. Nucl. Med. 62(12), 1789–1796 (2021). 10.2967/jnumed.120.260521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kewin M., et al. , “Evaluation of hyperspectral NIRS for quantitative measurements of tissue oxygen saturation by comparison to time-resolved NIRS,” Biomed. Opt. Express 10(9), 4789 (2019). 10.1364/BOE.10.004789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Matcher S. J., Cope M., Delpy D. T., “Use of the water absorption spectrum to quantify tissue chromophore concentration changes in near-infrared spectroscopy,” Phys. Med. Biol. 39(1), 177–196 (1994). 10.1088/0031-9155/39/1/011 [DOI] [PubMed] [Google Scholar]
- 36.Essenpreis M., et al. , “Wavelength dependence of the differential pathlength factor and the log slope in time-resolved tissue spectroscopy,” Adv. Exp. Med. Biol. 333, 9–20 (1993). 10.1007/978-1-4899-2468-1_2 [DOI] [PubMed] [Google Scholar]
- 37.Cooper C. E., et al. , “Use of mitochondrial inhibitors to demonstrate that cytochrome oxidase near-infrared spectroscopy can measure mitochondrial dysfunction noninvasively in the brain,” J. Cereb. Blood Flow Metab. 19(1), 27–38 (1999). 10.1097/00004647-199901000-00003 [DOI] [PubMed] [Google Scholar]
- 38.Matcher S. J., et al. , “Absolute quantification methods in tissue near-infrared spectroscope,” Proc. SPIE 2389, 486–495 (1995). 10.1117/12.209997 [DOI] [Google Scholar]
- 39.Kovacsova Z., et al. , “Absolute quantification of cerebral tissue oxygen saturation with multidistance broadband NIRS in newborn brain,” Biomed. Opt. Express 12(2), 907 (2021). 10.1364/BOE.412088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Verdecchia K., et al. , “Assessment of the best flow model to characterize diffuse correlation spectroscopy data acquired directly on the brain,” Biomed. Opt. Express 6(11), 4288 (2015). 10.1364/BOE.6.004288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Milej D., et al. , “Quantification of cerebral blood flow in adults by contrast-enhanced near-infrared spectroscopy: validation against MRI,” J. Cereb. Blood Flow Metab. 40(8), 1672–1684 (2020). 10.1177/0271678X19872564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brown D. W., et al. , “Quantitative near infrared spectroscopy measurement of cerebral hemodynamics in newborn piglets,” Pediatr. Res. 51(5), 564–570 (2002). 10.1203/00006450-200205000-00004 [DOI] [PubMed] [Google Scholar]
- 43.Verdecchia K., et al. , “Quantifying the cerebral metabolic rate of oxygen by combining diffuse correlation spectroscopy and time-resolved near-infrared spectroscopy,” J. Biomed. Opt. 18(2), 027007 (2013). 10.1117/1.JBO.18.2.027007 [DOI] [PubMed] [Google Scholar]
- 44.Dominguez de Villota E. D., et al. , “Equality of the in vivo and in vitro oxygen-binding capacity of haemoglobin in patients with severe respiratory disease,” Br. J. Anaesth. 53(12), 1325–1328 (1981). 10.1093/bja/53.12.1325 [DOI] [PubMed] [Google Scholar]
- 45.Bandera E., et al. , “Cerebral blood flow threshold of ischemic penumbra and infarct core in acute ischemic stroke,” Stroke 37(5), 1334–1339 (2006). 10.1161/01.STR.0000217418.29609.22 [DOI] [PubMed] [Google Scholar]
- 46.Tichauer K. M., et al. , “Assessing the severity of perinatal hypoxia-ischemia in piglets using near-infrared spectroscopy to measure the cerebral metabolic rate of oxygen,” Pediatr. Res. 65(3), 301–306 (2009). 10.1203/PDR.0b013e318194faa6 [DOI] [PubMed] [Google Scholar]
- 47.Cooper J. A., et al. , “Continuous monitoring of absolute cerebral blood flow by near-infrared spectroscopy during global and focal temporary vessel occlusion,” J. Appl. Physiol. 110(6), 1691–1698 (2011). 10.1152/japplphysiol.01458.2010 [DOI] [PubMed] [Google Scholar]
- 48.Cooper C. E., Delpy D. T., Nemoto E. M., “The relationship of oxygen delivery to absolute haemoglobin oxygenation and mitochondrial cytochrome oxidase redox state in the adult brain: a near-infrared spectroscopy study,” Biochem. J. 332(3), 627–632 (1998). 10.1042/bj3320627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oshima T., Karasawa F., Satoh T., “Effects of propofol on cerebral blood flow and the metabolic rate of oxygen in humans,” Acta Anaesthesiol. Scand. 43, 42–43 (2002). 10.1034/j.1399-6576.2002.460713.x [DOI] [PubMed] [Google Scholar]
- 50.Banaji M., “A generic model of electron transport in mitochondria,” J. Theor. Biol. 243, 501–516 (2006). 10.1016/j.jtbi.2006.07.006 [DOI] [PubMed] [Google Scholar]
- 51.Kajimoto M., et al. , “Propofol compared with isoflurane inhibits mitochondrial metabolism in immature swine cerebral cortex,” J. Cereb. Blood Flow Metab. 34, 514–521 (2014). 10.1038/jcbfm.2013.229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mccormick D. C., et al. , “Effect of indomethacin on cerebral oxidized cytochrome oxidase in preterm infants,” Pediatr. Res. 33(6), 603–608 (1993). 10.1203/00006450-199306000-00015 [DOI] [PubMed] [Google Scholar]
- 53.Arora R., et al. , “Preservation of the metabolic rate of oxygen in preterm infants during indomethacin therapy for closure of the ductus arteriosus,” Pediatr. Res. 73(6), 713–718 (2013). 10.1038/pr.2013.53 [DOI] [PubMed] [Google Scholar]
- 54.Kolyva C., et al. , “Cytochrome c oxidase response to changes in cerebral oxygen delivery in the adult brain shows higher brain-specificity than haemoglobin,” Neuroimage 85, 234–244 (2014). 10.1016/j.neuroimage.2013.05.070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jain V., et al. , “Rapid magnetic resonance measurement of global cerebral metabolic rate of oxygen consumption in humans during rest and hypercapnia,” J. Cereb. Blood Flow Metab. 31(7), 1504–1512 (2011). 10.1038/jcbfm.2011.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bale G., et al. , “Multimodal measurements of brain tissue metabolism and perfusion in a neonatal model of hypoxic-ischaemic injury,” Adv. Exp. Med. Biol. 1269, 203–208 (2021). 10.1007/978-3-030-48238-1_32 [DOI] [PubMed] [Google Scholar]
- 57.Zhu X. H., et al. , “Quantitative imaging of energy expenditure in human brain,” Neuroimage 60, 2107–2117 (2012). 10.1016/j.neuroimage.2012.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cooper C. E., Springett R., “Measurement of cytochrome oxidase and mitochondrial energetics by near-infrared spectroscopy,” Philos. Trans. R. Soc. B Biol. Sci. 352, 669–676 (1997). 10.1098/rstb.1997.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]