Abstract
The high lethality of ovarian cancer in the United States and associated complexities of the patient journey across the cancer care continuum warrant an assessment of current practices and barriers to quality care in the United States. The objectives of this study were to identify and assess key components in the provision of high‐quality care delivery for patients with ovarian cancer, identify challenges in the implementation of best practices, and develop corresponding quality‐related recommendations to guide multidisciplinary ovarian cancer programs and practices. This multiphase ovarian cancer quality‐care initiative was guided by a multidisciplinary expert steering committee, including gynecologic oncologists, pathologists, a genetic counselor, a nurse navigator, social workers, and cancer center administrators. Key partnerships were also established. A collaborative approach was adopted to develop comprehensive recommendations by identifying ideal quality‐of‐care program components in advanced epithelial ovarian cancer management. The core program components included: care coordination and patient education, prevention and screening, diagnosis and initial management, treatment planning, disease surveillance, equity in care, and quality of life. Quality‐directed recommendations were developed across 7 core program components, with a focus on ensuring high‐quality ovarian cancer care delivery for patients through improved patient education and engagement by addressing unmet medical and supportive care needs. Implementation challenges were described, and key recommendations to overcome barriers were provided. The recommendations emerging from this initiative can serve as a comprehensive resource guide for multidisciplinary cancer practices, providers, and other stakeholders working to provide quality‐directed cancer care for patients diagnosed with ovarian cancer and their families.
Keywords: biomarkers, chemotherapy, delivery of health care, diagnosis, health equity, immunotherapy, ovarian neoplasms, patient care management, quality of health care, radiotherapy
Short abstract
Quality‐directed recommendations for ovarian cancer care delivery are developed across 7 core program components, with a focus on ensuring high‐quality care delivery by addressing unmet medical and supportive care needs. These recommendations can serve as a comprehensive resource guide for multidisciplinary cancer practices, providers, and other stakeholders working to provide quality‐directed cancer care for patients diagnosed with ovarian cancer and their families.
Introduction
Ovarian cancer is a biologically diverse disease with multiple histologic and molecular subtypes. 1 , 2 , 3 It is the leading cause of gynecologic cancer mortality in the United States and ranks fifth in cancer deaths among women. 4 Despite declining incidence rates over the past 30 years in the United States, 5 ovarian cancer remains a significant public health issue, with estimates of 21,410 incident cases and 13,770 deaths in 2021. 4 Advanced‐stage diagnosis is a particular challenge 6 driving a poor prognosis 5 and a 5‐year overall survival rate <50% for those diagnosed with epithelial ovarian cancer. 5 Delivering guideline‐concordant care is an important driver of improved patient survival. 7 , 8 , 9 , 10
Emerging evidence supports routine genetic testing early in the cancer care continuum 11 , 12 to identify biomarkers, guide treatment decisions, and identify at‐risk family members who may benefit from prevention strategies. 13 Genetic testing includes germline testing for BRCA1, BRCA2, and other ovarian cancer‐susceptibility gene mutations and somatic testing for BRCA1 and BRCA2 pathogenic or likely pathogenic variants. 13 , 14 Testing strategies are rapidly evolving, with new recommendations including expanded multiplex gene panels to test for both hereditary and somatic mutations; the use of novel molecular assays to measure homologous recombination deficiency (HRD) status in ovarian tumors; and sequencing of the ATM, RAD51C, RAD51D, BRIP1, NBN, PALB2, and STK11 genes in the absence of germline targets. 13 Gene mutations in the DNA mismatch‐repair genes MLH1, MSH2, MSH6, PMS2, and EPCAM are associated with Lynch syndrome and, although less commonly associated with ovarian cancer, can influence treatment decisions and risk communication. 13 Despite its importance, testing in many settings, including specialized centers, remains low 15 , 16 , 17 and was estimated to be 34.3% in an evaluation within the National Cancer Institute's Surveillance, Epidemiology, and End Results program records. 17 Improved surgical and survival outcomes have been documented when a gynecologic oncologist is involved in ovarian cancer care; however, such consultation is not always routine practice 10 nor is the receipt of guideline‐concordant care from diagnosis onward. 7 , 8 , 9 , 10 , 18 Also critical to ovarian cancer care delivery are determination of surgical suitability, eligibility for targeted therapies, and pathologic evaluation, 19 with care delivery ideally involving surgery and chemotherapy as initial therapy. 13
Given the high disease burden, the toxicity associated with treatment, the heterogeneous nature of the malignancy, and the complexities of treatment planning, receiving high‐quality care remains challenging across the ovarian cancer care continuum. These challenges emphasize the importance of a multidisciplinary team approach to care delivery in this disease site; therefore, it is vital to evaluate current practices and identify recommendations for defining the key areas of quality care to help guide multidisciplinary ovarian cancer practices. In 2019, the Association of Community Cancer Centers (ACCC) launched a multiphase, stakeholder‐driven initiative to improve care for patients diagnosed with ovarian cancer in the United States that included 3 primary components: 1) development and administration of a workshop application survey to identify the needs of patients diagnosed with ovarian cancer across several cancer programs; 2) recruitment for and execution of quality‐improvement initiatives with 3 selected ACCC member programs on topics specific to ovarian cancer care delivery, spanning diagnosis through survivorship; and 3) dissemination of findings through a curated, comprehensive resource library hosted by the ACCC and dedicated to patient‐specific and provider‐specific ovarian cancer educational resources. As part of an evidence‐based approach, key components in the provision of high‐quality care delivery for patients with ovarian cancer, including malignancies arising in the ovaries, peritoneum, and fallopian tubes, were identified, and recommendations that could serve as a comprehensive yet succinct resource for multidisciplinary ovarian cancer practices and providers in the United States were developed.
Methods
The ovarian cancer quality‐care initiative was guided by a multidisciplinary expert steering committee that included gynecologic oncologists, pathologists, a genetic counselor, a nurse navigator, social workers, and cancer center administrators across the United States. Furthermore, key partnerships were established with the Society of Gynecologic Oncology, the National Society of Genetic Counselors, and the Association for Molecular Pathology. Patient advocacy was represented through a partnership with the Ovarian Cancer Research Alliance. This multidisciplinary expert group provided recommendations based on available evidence in structural improvements that can improve the quality of care for patients with ovarian cancer.
Details of the quality‐improvement projects, including design, implementation, and site‐specific results and the associated impact, have been published. 20 In summary, genetic counseling and testing, the availability of and/or enrollment in clinical trials, and multidisciplinary team care were identified as key areas for quality improvement. At each of the 3 participating sites, key stakeholders were identified, and goals were established and executed through staged project design and review at months 1, 3, and 6. Furthermore, an ovarian cancer quality‐care document was developed using a collaborative approach informed by the expert steering committee and real‐world inputs from multidisciplinary teams, physician champions, and quality‐improvement workshop participants. The steering committee drafted quality‐directed components, implementation barriers, and comprehensive recommendations for the ideal management of advanced epithelial ovarian cancer aimed at providing evidence‐based guidance and best practices to ovarian cancer programs in the United States. Multiple teleconferences and reviews were conducted to search for published standards, articles, and guidelines. A PubMed literature search was conducted to identify articles published dating back 10 years from the search date that included the search terms ovarian cancer, quality, and care. In addition, oncology professional association websites, such as the American Society of Clinical Oncology, the National Comprehensive Cancer Network, and the Centers for Medicare and Medicaid Services, were searched for Merit‐Based Incentive Payment System Programs/Quality Payment Program–type quality metrics specifically for ovarian cancer and/or gynecologic oncology diagnoses. The quality document was discussed in depth during steering committee meetings, which included in‐person and virtual sessions, and subsequently was approved. This review article addresses the core components in ovarian cancer care, including care coordination and patient education, prevention and screening, diagnosis and initial management, treatment planning, disease surveillance, equity in care, and quality of life (QoL). Implementation challenges and system‐level recommendations for addressing each challenge are described. This document is intended for broad dissemination as a quality‐directed program resource spanning the ovarian cancer care continuum.
Results
The steering committee developed and endorsed quality recommendations targeting 7 key components of ovarian cancer care delivery: care coordination and patient education, prevention and screening, diagnosis and initial management, treatment planning, disease surveillance, equity in care, and QoL (Table 1).
TABLE 1.
Implementation Barriers and Key Recommendations for the Provision of High‐Quality Ovarian Cancer Care Delivery
| Domain | Implementation Barriers | Key Recommendations |
|---|---|---|
| 1. Care coordination and patient education | a. Limited physician time to address nonmedical needs of patients with ovarian cancer | a. Identifying and uniformly advising patients and caregivers of available local, regional, and/or online resources |
| b. Ensuring all cancer center resources are equally available to all patients with cancer, including those diagnosed with gynecologic cancer | ||
| c. Incorporating dedicated patient navigation (clinical or lay) services that are specific to caring for this population and that promote patient participation in shared decision‐making | ||
| 2. Prevention and screening | a. Low rate of prophylactic and risk‐reducing surgery | a. Identifying local champions within health systems for ovarian cancer risk reduction |
| b. Continuing education of gynecologists, surgeons, pathologists, and oncologists on the role of risk‐reducing surgery | ||
| c. Thorough pathologic evaluation (SEE‐FIM) of specimens after risk‐reducing surgery to detect occult tubal carcinomas and precursor lesions | ||
| 3. Diagnosis and initial management | a. Lack of access to specialists accompanied by fragmented and siloed care across hospital departments | a. Identifying a local/regional gynecologic oncologist, where necessary, for referrals |
| b. Identifying ways to overcome patient‐level barriers (gas cards and bus vouchers to alleviate inequities) | ||
| c. Ensuring complete pathologic evaluation, including accurate diagnosis and harvest of sufficient tumor tissue for potential molecular testing, before treatment initiation | ||
| d. Engaging patient navigators to ensure timely referrals and assistance with overcoming barriers to evaluation | ||
| e. Bridging cancer center support to ensure resources are equally available to all patients with cancer | ||
| f. Engaging a gynecologic cancer patient advocate within the health system to liaise with the cancer center and ensure that services are available for patients with gynecologic cancer | ||
| Evaluation | a. Limited number of gynecologic oncologists with expertise to adequately evaluate and manage newly diagnosed ovarian cancers | a. Centralizing surgical expertise within health systems and regions and considering a new ovarian cancer diagnosis as an urgent new diagnosis with flexibility within the system to add on surgery and chemotherapy and with formal processes for urgent referrals, telemedicine options for gynecologic oncology consultations, and provider education |
| b. Limited access to gynecologic oncologist because of transportation barriers | b. Incentivizing and standardizing gynecologic oncology referrals by medical or surgical oncologists before treatment initiation | |
| c. Limited access to genetic counseling and oncofertility services | c. Engaging and using patient navigators to ensure referrals to gynecologic oncologists | |
| d. Centralizing genetic counseling services within health systems and regions to ensure access for patients with newly diagnosed ovarian cancer | ||
| e. Providing alternate care delivery, including telemedicine and group genetic counseling | ||
| f. Employing checklists or other reminder systems to ensure all patients are referred to and receive genetic testing and/or counseling | ||
| g. Identifying a local champion for oncofertility or providing appropriate educational materials | ||
| 4. Treatment planning | ||
| General | a. Limited availability of clinical trials for patients with ovarian cancer | a. Identifying local champions to introduce and accrue patients to clinical trials |
| b. Inadequate enrollment of elderly patients and those from historically under‐represented racial and ethnic groups | b. Ensuring all physicians and team members are up to date on clinical trial availability | |
| c. Cancer center support for clinical trials that may not cross departments and extend to gynecology | c. Engaging research staff in clinical discussions (such as tumor boards) to encourage cross‐talk between clinical and research staff to optimize the identification of eligible patients | |
| d. Patient reluctance to participate in clinical trials | d. Ensuring organizational support for all cancer clinical trials regardless of cancer type | |
| e. Engaging patient navigators across visits and encouraging provider recommendations of clinical trials | ||
| Standard therapy (frontline adjuvant or primary systemic chemotherapy, other targeted therapy) and maintenance therapy | a. Low rate of PARP inhibitor prescription | a. Educating patients and physicians on the benefits of targeted agents and PARP inhibitors with or without bevacizumab and their appropriate place in therapy |
| b. Financial toxicity associated with oral chemotherapy | b. Engaging financial navigators during diagnosis to assist with prior authorizations, copays, and other out‐of‐pocket costs associated with oral anticancer agents | |
| 5. Disease surveillance | a. Historical overuse of imaging for posttreatment cancer surveillance | a. Educating physicians, team members, and patients on the risks and benefits of false‐positive imaging |
| b. Using quality metrics for physicians that involve the use of evidence‐based surveillance | ||
| 6. Equity in care | a. Limited access to health insurance and care for nonmajority racial and ethnic groups and implicit bias among health care providers | a. Ensuring peer or nursing navigation for all patients with ovarian cancer |
| b. Establishing institutional policies to reduce implicit bias | ||
| c. Measuring quality metrics by self‐described race with the goal of reducing racial health inequities | ||
| 7. Quality of life | a. Patient reluctance to discuss these issues with their clinician or other members of the health care team and a limited comfort level with these topics and/or lack of available resources from physicians and other team members | a. Identifying and uniformly advising cancer care team members and patients of available local, regional, and/or online resources |
| b. Partnering with patient advocacy partners to create and curate patient and provider resources (also identified in the Survivorship Care Plan) | ||
| c. Identifying specific timepoints during a patient's care to discuss advanced directives and goals of care |
Abbreviations: PARP, poly(adenosine diphosphate‐ribose) polymerase; SEE‐FIM, sectioning and extensive examination of the fimbriated end.
Care Coordination and Patient Education
Effective care coordination across the cancer care continuum has important ramifications for patient health outcomes. 21 , 22 These include facilitating patient education on various facets of ovarian cancer care delivery, including the importance of genetic testing and shared decision‐making, especially when new and complex treatments are involved and patients have limited or no prior experience with ovarian cancer care. 23 Patients with ovarian cancer report the so‐called little big things (scheduling, wait times, pharmacy, transportation, parking, finances, insurance, and discharge) and a lack of care coordination as significant burdens, and they report human contact as a comfort. 24 All patients should: 1) receive education on ovarian cancer, staging, prognosis, possible treatment side effects, and response expectations before therapy initiation by a multidisciplinary cancer care team member; 2) participate in shared decision‐making concerning their comprehensive cancer care plan; 3) have access to multidisciplinary cancer care team members who can answer questions and assess and address possible barriers to treatment success, including financial, housing, transportation, and treatment costs and prediagnosis comorbidities; and 4) have ongoing access to a multidisciplinary cancer care team member who can answer questions regarding emotional, psychosocial, and/or spiritual care concerns and needs.
Limited physician time to address the nonmedical needs of patients, such as psychosocial supportive care, 25 , 26 is often challenging, including identifying and uniformly advising patients and caregivers of available local, regional, and/or online resources and ensuring that all cancer center resources are equally available to all patients with cancer, including those diagnosed with gynecologic cancer. Ideally, patient navigation services should be available and should encompass the provision of individualized assistance to patients, families, and caregivers to meet medical needs, help overcome health care system barriers, and facilitate timely access to quality health and psychosocial care from the initial consult/evaluation/prediagnosis through all phases of the cancer experience. 27 , 28 Figure 1 illustrates the core characteristics and functional competencies of such services. 27 , 29
Figure 1.
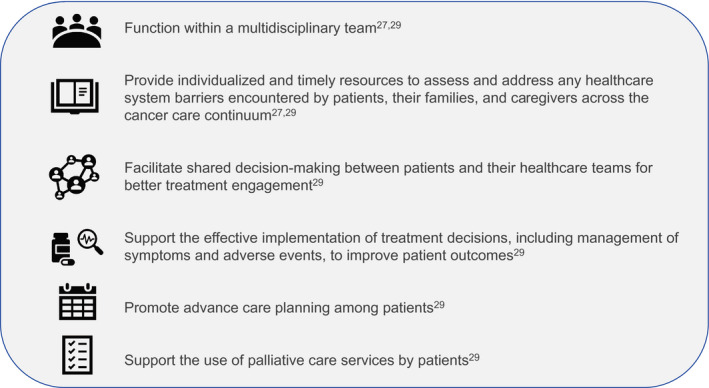
Core characteristics and functional competencies involved in patient navigation in the oncology care setting are illustrated (see Oncology Nursing Society; Association of Oncology Social Work; National Association of Social Workers. Oncology Nursing Society, the Association of Oncology Social Work, and the National Association of Social Workers joint position on the role of oncology nursing and oncology social work in patient navigation. Oncol Nurs Forum. 2010;37:251‐252 27 ; and Oncology Nursing Society. 2017 Oncology Nurse Navigator Core Competencies. 29 https://www.ons.org/sites/default/files/2017‐05/2017_Oncology_Nurse_Navigator_Competencies.pdf).
Prevention and Screening
Routine screening for individuals at an average or high risk of ovarian cancer is not currently recommended because the risks outweigh the benefits. 13 , 30 Regarding prevention or risk reduction, 2 key components are identified. First, opportunistic salpingectomy at the time of hysterectomy, other pelvic surgery, or in lieu of tubal ligation in individuals at an average risk of ovarian cancer is recommended; and risk‐reducing salpingo‐oophorectomy is recommended for patients at increased genetic risk of ovarian cancer (family history; BRCA1, BRCA2, and other inherited mutations) at the completion of childbearing or at an age determined by family history or specific mutations and before menopause. For high‐risk patients aged 30 to 35 years who do not elect to undergo risk‐reducing salpingo‐oophorectomy, transvaginal ultrasound with cancer antigen 125 may be considered. 13 A pathologic examination protocol that uses sectioning and extensive examination of the fimbriated end 31 , 32 of the grossly normal fallopian tubes and ovaries in patients with such mutations to identify occult tubal cancer and precancers designated as serous tubal intraepithelial carcinomas has been endorsed. 2 , 33 , 34 The relation between serous tubal intraepithelial carcinoma lesions and high‐grade serous and endometrioid cancers is supported by the ubiquitous presence of TP53 mutations and their typical location within the fimbriated end of the fallopian tube. 32 , 35 , 36 , 37 The implementation of prophylactic and risk‐reducing surgery remains a challenge. 38 , 39 , 40 , 41 Identifying local champions within health systems for ovarian cancer risk reduction and engaging with gynecologists, nongynecologic surgeons, pathologists, and primary care providers on the role of risk‐reducing surgery are recommended.
Diagnosis and Initial Management
The peritoneal spread of ovarian cancer typically results in an insidious onset of symptoms, with the ultimate diagnosis made typically as late‐stage disease. Before treatment initiation, recommendations for initial workup will ideally include: 1) evaluation by a gynecologic oncologist; 2) tumor marker assessment (cancer antigen 125, carcinoembryonic antigen, and/or cancer antigen 19‐9), as clinically indicated before therapy initiation; 3) complete pathologic evaluation; 4) decision for and timing of surgery determined by a gynecologic oncologist; 5) nutrition analysis and referral; 6) emotional distress/support screening, psychosocial needs referral, and/or spiritual care referral; and 7) referral to a concurrent, supportive oncologist/palliative care specialist when appropriate. Challenges include a lack of access to specialists and fragmented and siloed care across hospital departments in which psychosocial support and related services may not be extended to patients with gynecologic cancer. 22 Identifying a local/regional gynecologic oncologist for referrals; identifying and engaging with gynecologic cancer patient advocates within the health system to liaise with the cancer center and ensure that services, such as social work support, are available for patients to help overcome patient‐level barriers (eg, gas cards and bus vouchers to alleviate inequities); engaging patient navigators/patient advocates to ensure timely referrals and assistance with overcoming barriers to evaluation; and bridging cancer center support with national nonprofit support programs to ensure resources are equally available to all cancer patients are recommended.
For patients undergoing surgical management as their initial intervention, the evaluation should include: 1) comprehensive surgical staging that incorporates International Federation of Gynecology and Obstetrics or American Joint Committee on Cancer (eighth edition) guidelines and includes an accurate pathologic diagnosis with histologic subtype characterization for all patients undergoing initial surgery for presumed early stage disease, 42 2) harvesting of sufficient treatment‐naive tumor tissue for biomarker testing during diagnostic biopsy in patients undergoing neoadjuvant chemotherapy, 3) cytoreductive surgery for patients with advanced‐stage disease who are deemed fit to undergo surgery with a high likelihood of successful resection to <1 cm of residual disease, 4) genetic risk evaluation and testing coordination (germline mutation testing, somatic mutation testing, HRD testing, and additional testing) for all patients, and 5) a fertility‐preservation discussion with care team member(s) or referral to a reproductive endocrinology and infertility/oncofertility service before surgery, if relevant. The limited availability of gynecologic oncologists who have the expertise to adequately evaluate and manage newly diagnosed ovarian cancer is a challenge. 43 , 44 Health systems should ensure that organizational support for all clinical cancer care, including navigation and advocacy, extends to all disease sites, providing opportunities for expedited care. Additional recommendations include centralizing surgical expertise within health systems and regions; consideration of a new ovarian cancer diagnosis as an urgent diagnosis with flexibility within the system to add on consultation, surgery, chemotherapy, and formal processes for urgent referrals; telemedicine options for gynecologic oncology consultations when in‐person visits are not available or feasible; and education of physicians, providers, and hospital administration on both the signs and symptoms of ovarian cancer and the importance of timely and expedited treatment initiation. Access to a gynecologic oncologist for evaluation tends to be most limited for patients living in rural regions where transportation barriers are high. 44 Incentivizing and standardizing gynecologic oncology referrals should be considered to optimize the chances that all patients with ovarian cancer are appropriately evaluated. Engaging and using health system‐based oncology patient navigators and advocates can facilitate and ensure appropriate referrals to gynecologic oncologists and their care teams. Other challenges include the limited availability of genetic counseling 45 , 46 and oncofertility services. 47 , 48 Recommendations include centralizing genetic counseling services within health systems and regions to ensure access for patients with newly diagnosed ovarian cancer; alternative care delivery, including telemedicine and group genetic counseling; electronic medical record checklists or other reminder systems to ensure that all patients and their family members are referred to and receive genetic testing and/or counseling; and the identification of a local champion for oncofertility or provision of appropriate educational materials.
Treatment Planning
After an ovarian cancer diagnosis, treatment must be individualized based on the patient's performance status, care goals, and germline and somatic genetic testing results. Components of a general treatment plan include: 1) a multidisciplinary review of the treatment plan for consensus recommendations; 2) evaluation for clinical trials in the upfront and recurrent settings to be considered first; 3) a care plan, compliant with the 13 components in the Institute of Medicine's Care Management Plan (Table 2), 22 provided to patients before receiving the first therapeutic modality; and 4) early integration of supportive and palliative care services. The limited availability of clinical trials for patients with ovarian cancer and the inadequate enrollment of elderly patients and those from historically under‐represented racial and ethnic groups pose challenges. 49 , 50 , 51 To improve clinical trials enrollment with a health care system, identifying and incentivizing local champions to introduce and accrue patients to clinical trials, ensuring that all physicians and team members are up to date on clinical trial availability, and engaging research staff in clinical discussions, such as tumor boards, to encourage cross‐talk between clinical and research staff to optimize the identification of eligible patients are recommended. Another challenge is that cancer center support for clinical trials may not cross departments and extend to gynecologic oncology divisions—perhaps a feature of the cancer center administrative structure that unintentionally influences resource allocation decisions, including clinical trial support, toward nongynecologic disease sites. Patients may be reluctant to participate in clinical trials 52 ; however, physician involvement is a key determinant of patient enrollment in clinical trials. Organizational and physician factors can be optimized to facilitate patient enrollment. 53 Health care systems can ensure that physicians have access to support staff to help screen and enroll patients as well as to set expectations for minimum accrual. The engagement of patient navigators familiar with clinical trial availability can also improve enrollment. 54 , 55 , 56 , 57
TABLE 2.
Components of a Cancer Care Plan to be Developed in Collaboration With Patients a
| Components |
|---|
| 1. Patient information |
| 2. Diagnosis‐related information, including tissue, biomarkers, and stage |
| 3. Prognosis |
| 4. Treatment goals (curative, life‐prolonging, symptom control, palliative care) |
| 5. Initial plan for treatment and proposed duration, including chemotherapy (drugs, doses, schedule), surgery, and radiation therapy |
| 6. Expected response to treatment |
| 7. Treatment benefits and harms, including toxicity management, and short‐term and late effects of treatment |
| 8. Quality of life and patients' likely experience with treatment |
| 9. Responsible persons for specific aspects of a patient's care (eg, cancer care team, primary care/geriatrics care team, or other care teams) |
| 10. Advanced care plans, including advanced directives and other legal documents |
| 11. Estimated total and out‐of‐pocket costs of cancer treatment |
| 12. Psychosocial health needs plan comprising psychological, nutritional, vocational, disability, legal, or financial concerns and their management |
| 13. Survivorship plan comprising treatment, recommended follow‐up activities, surveillance, and risk reduction, and health‐promotion activities |
Institute of Medicine. Delivering High‐Quality Cancer Care: Charting a New Course for a System in Crisis. The National Academies Press; 2013. 22 Reproduced with permission from the National Academy of Sciences, Courtesy of the National Academies Press; Washington, DC.
Select patients with early stage or low‐grade cancers may not require chemotherapy, and surgery alone with follow‐up evaluation may suffice as primary treatment. 13 However, for most patients with ovarian cancer, initial treatment involves systemic chemotherapy and often includes other targeted therapy as standard and maintenance therapies. 13 The initiation of frontline adjuvant or primary systemic chemotherapy within 42 days after cytoreduction is recommended for all eligible patients, with ≥80% of patients receiving a National Comprehensive Cancer Network‐recommended treatment regimen for advanced epithelial ovarian cancer, including the administration of carboplatin/paclitaxel with or without bevacizumab, followed by consideration of maintenance therapy with bevacizumab, a poly(adenosine diphosphate–ribose) polymerase (PARP) inhibitor, or a bevacizumab plus PARP inhibitor combination in selected patients who have a partial or complete response to frontline chemotherapy. 13 If clinical trials are available, they should be offered. If the patient declines or the patient does not meet eligibility criteria, shared decision making based on their genetic testing results, somatic testing, tumor histology, medical comorbidities, and patient goals of care should determine maintenance therapy initiation.
Most patients with ovarian cancer will ultimately recur. Prognosis and treatment have been driven by the platinum‐free interval. For patients who have a platinum‐resistant recurrence (<6 months since the last platinum‐based chemotherapy), single‐agent chemotherapy with or without bevacizumab is recommended. 58 For patients with platinum‐sensitive, recurrent disease, doublet platinum and other chemotherapy agents, with or without bevacizumab, are recommended. 59 PARP inhibitors should also be considered in the following settings for recurrent disease: 1) as maintenance treatment for platinum‐sensitive, recurrent disease in patients who have at least a partial response to platinum‐based chemotherapy; and 2) as a treatment option for patients who have deleterious germline and/or somatic BRCA‐mutated disease or evidence of HRD after from 2 to ≥3 lines of chemotherapy (based on the agent chosen). 13 The efficacy of PARP inhibitor therapy in previously treated patients is currently unknown. Among eligible patients, more than one‐half do not receive a PARP inhibitor maintenance prescription. 60 Educating patients and physicians about the available treatment options, associated side‐effect profiles, and their appropriate place in therapy may lead to the increased use of available therapies. Engaging financial navigators during treatment to assist with prior authorizations, copays, and other out‐of‐pocket costs and to support patients with financial assistance application submissions may help alleviate the financial toxicity associated with chemotherapy, particularly oral agents, which often carry high out‐of‐pocket costs. 61
Disease Surveillance
Posttreatment surveillance encompasses the detection of disease recurrence and late treatment side effects. Both oncology and primary care providers can ensure appropriate patient follow‐up through a comprehensive history and physical examination with symptom review, education on signs or symptoms of recurrence, and other aspects, such as promotion of bone, brain, cardiovascular, and sexual health. 62 , 63 Standardizing surveillance protocols that include a history and physical examination 63 with an assessment of tumor markers, if indicated (visits every 2‐4 months for the first 2 years, every 3‐6 months for next 3 years, and annually after 5 years), is recommended. Routine imaging is not recommended but should be prompted by the onset of disease‐related symptoms or by an increase in a tumor marker. Computed tomography is recommended for imaging, with positron emission tomography reserved for specific circumstances. Survivorship care plans should be developed for patients with surgically resected ovarian cancer who are treated with curative intent. A challenge related to this recommendation is the historical overuse of routine imaging, including computed tomography scans, for posttreatment cancer surveillance in patients with ovarian and other gynecologic cancers, with implications of increased patient anxiety, risks of overtreatment, and increased health care costs despite limited impact on detecting disease recurrence and no improvement in overall survival. 64 , 65 , 66 Recommendations to mitigate the overuse of imaging include educating physicians, team members, and patients on the risks and benefits of false‐positive imaging and applying quality metrics for physicians that include adherence to evidence‐based surveillance.
Equity in Care
Significant disparities exist in access to and receipt of guideline‐adherent, high‐quality ovarian cancer care among patients from historically under‐represented racial and ethnic groups and those with lower socioeconomic status. 67 , 68 , 69 Black and Hispanic patients are less likely to receive guideline‐adherent care compared with White patients, with or without a gynecologic oncologist consultation 5 , 67 , 68 , 70 , 71 ; uninsured patients or those who are publicly insured are less likely to receive guideline‐adherent care compared with those who have private insurance or managed care 68 ; Asian patients have a higher 5‐year disease‐specific survival rate compared with White patients 72 ; regional differences exist in ovarian cancer incidence between American Indian/Alaska Native women and White women in the same US geographic region 73 ; and Black and Hispanic patients are under‐represented in ovarian cancer clinical trials compared with the incident US population. 74 These inequities in care delivery translate to an overall survival disadvantage for many patients from historically under‐represented racial and ethnic groups as well as those with low socioeconomic status. 8 , 68 , 70 , 75 With improvements in treatment, the survival advantage for non‐Hispanic White patients with ovarian cancer has widened because access to guideline‐adherent care increases the likelihood of improved outcomes. 5 Limited access to health insurance and care for under‐represented racial and ethnic groups 67 , 68 , 69 and implicit racial bias among health care providers in the case of racially discordant interactions 76 continue to be challenges to equity in ovarian cancer care. Ensuring peer or nursing navigation for all patients with ovarian cancer, establishing institutional policies to reduce implicit bias, and measuring and stratifying quality metrics by self‐described race, with the goal of reducing racial health inequities, are recommended.
Quality of Life
Health‐related QoL is an important consideration for patients diagnosed with ovarian cancer because of the side effects of therapeutic interventions, including fatigue, bloating, pain, peripheral neuropathy after taxane‐based chemotherapy, sexual dysfunction, and morbidity from disease‐related symptoms. 77 Recommendations include referrals by oncologists and primary care providers to clinic‐based or community‐based exercise programs because higher health‐related QoL (including physical functioning) is associated with overall survival 78 ; the inclusion of advanced directives in visits involving changes in the treatment plan; and caregiver support, including meetings with caregivers or family members to provide details on diagnosis, treatment, and off‐treatment transition. Patients may be reluctant or uncomfortable discussing these topics with their clinician or health care staff, and limited available resources pose a challenge. 19 , 79 , 80 Identifying and uniformly advising cancer care team members and patients of available local, regional, and/or online resources; collaborating with patient advocacy partners to create and curate patient and provider resources (also identified in the Survivorship Care Plan); and identifying specific timepoints during a patient's care to discuss advanced directives and care goals can improve the QoL of patients with ovarian cancer.
Discussion and Conclusion
Through the initiative spearheaded by the multidisciplinary expert steering committee, core components were identified in the provision of high‐quality care delivery for patients diagnosed with ovarian cancer, including care coordination and patient education, prevention and screening, diagnosis and initial management, treatment planning, disease surveillance, equity in care, and QoL. Informed by components and potential barriers to effective implementation, a comprehensive set of recommendations for high‐quality advanced epithelial ovarian cancer management were compiled. Because limited numbers of gynecologic oncologists currently are trained and practice in the United States, strategies for sharing the care of these patients with other multidisciplinary team members must be identified locally to ensure that a full spectrum of cancer care is available for patients with ovarian cancer. Key concerns to ensure the provision of quality care for these patients include patient education and engagement on available treatment options; addressing the psychosocial support needs of patients, their families, and caregivers; and structural barriers within the health care system. Given the heterogeneity of ovarian cancer, with its multiple and varied tumor subtypes, and the evolving treatment management landscape, a single model cannot be used to describe ovarian cancer care delivery for patients across different settings. 19 , 81 The recommendations provided by this task force can be used by cancer programs as a quality‐directed resource spanning the ovarian cancer care continuum. Navigator‐driven and person‐centric programs are the need of the hour, with emphasis on critical aspects, such as multidisciplinary team‐based care, access to clinical trials, and provision of ancillary services, including genetic counseling, supportive care, fertility preservation, and nutritional counseling, all of which can significantly help improve the lives of patients affected by ovarian cancer. 82 The recommendations provided by this task force thus will be widely disseminated through the ACCC community (https://www.accc‐cancer.org/projects/ovarian‐cancer‐quality‐care/overview; accessed February 25, 2021) of >28,000 health care professionals across all disciplines in oncology, along with the network of 21 state societies that are managed by the ACCC, the partner organizations, and the multidisciplinary steering committee involved in this initiative.
In conclusion, the recommendations for advanced epithelial ovarian cancer management provided here address the inadequacies of structural provisions independent of the effective patient‐level guidelines commonly used. Our recommendations exceed the scope of current guidelines, highlighting areas of prevention, health equity, and implementation barriers, and provide key recommendations to address these barriers. These recommendations, along with the complementary article, 20 provide a useful resource to improve organizational support, can support data benchmarking for ovarian cancer or gynecologic oncology work by cancer programs, and, in doing so, can improve ovarian cancer care.
Funding Support
Funding support from AstraZeneca and Merck was provided to the Association of Community Cancer Centers, and funding for medical writing support paid to Cactus Communications was contracted and compensated by AstraZeneca.
Conflict of Interest Disclosures
Sarah M. Temkin reports consulting fees from Cancer Expert Now and payment or honoraria from Clovis Oncology outside the submitted work. Leigh M. Boehmer reports personal fees from Pfizer outside the submitted work. Leigha Senter reports personal fees and honoraria from AstraZeneca outside the submitted work. Destin R. Black reports payment or honoraria for the Ovarian Cancer Workshop to Willis‐Knighton Medical Center and participation on the Gynecologic Oncology Group Investigator Council outside the submitted work. Stephanie V. Blank reports research collaboration and institutional contracts with Glaxo Smith Kline, Roche, AstraZeneca, Seattle Genetics, Merck, AkesoBio, and NRG Oncology; participation on an Aravive data safety and monitoring board; and a leadership or fiduciary role with the Society of Gynecologic Oncology (unpaid), the American Board of Obstetrics and Gynecology, SHARE (unpaid), and the National Ovarian Cancer Coalition (unpaid) all outside the submitted work. Anna Yemelyanova reports personal fees and honoraria from Roche Diagnostics and meeting/travel support from AstraZeneca outside the submitted work. Anthony M. Magliocco reports honoraria from AstraZeneca, Roche, Merck, Bristol Myers Squibb, and Lilly; payment from the Department of Justice Office of the Inspector General for expert testimony; meeting/travel support from AstraZeneca; and is an employee of Protean BioDiagnostics and owns equity in the company all outside the submitted work. Mollie A. Finkel reports personal fees from AstraZeneca outside the submitted work. Premal H. Thaker reports institutional grants or contracts from AstraZeneca, Merck, Glaxo Smith Kline, Novocure, Aravive, and Clovis; personal fees from AstraZeneca, Glaxo Smith Kline, Stryker, Seagen, Celsion, Immunogen, and Aravive; honoraria from AstraZeneca, Merck, and Glaxo Smith Kline; payment for expert testimony; payment for participation on a data safety monitoring board or advisory board from Novocure, Glaxo Smith Kline, AstraZeneca, Celsion, Novocure, and Iovance; and owns stock options in Celsion all outside the submitted work. Matthew P. Smeltzer, Monique D. Dawkins, Tracy E. Moore made no disclosures.
Temkin SM, Smeltzer MP, Dawkins MD, Boehmer LM, Senter L, Black DR, Blank SV, Yemelyanova A, Magliocco AM, Finkel MA, Moore TE, Thaker PH. Improving the quality of care for patients with advanced epithelial ovarian cancer: Program components, implementation barriers, and recommendations. Cancer.2022. 10.1002/cncr.34023
We thank the Society of Gynecologic Oncology, the National Society of Genetic Counselors, the Association for Molecular Pathology, and the Ovarian Cancer Research Alliance, which were partner organizations in this initiative; Drs. Nashwa Kabil and Kathleen Reed from AstraZeneca for reviewing a draft of the article; and Melissa Furtado, MPH, and Juliane Moloney, PhD, of Cactus Life Sciences (part of Cactus Communications) for writing support. The authors retained full control over the content of the article and approved the final version for submission.
This article was prepared before Sarah M. Temkin's employment at the National Institutes of Health. The opinions expressed in this article are the author's own and do not reflect the views of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
References
- 1. Kurman RJ. Origin and molecular pathogenesis of ovarian high‐grade serous carcinoma. Ann Oncol. 2013;24(suppl 10):x16‐x21. [DOI] [PubMed] [Google Scholar]
- 2. Kurman RJ, Shih IM. The dualistic model of ovarian carcinogenesis: revisited, revised, and expanded. Am J Pathol. 2016;186:733‐747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wentzensen N, Poole EM, Trabert B, et al. Ovarian cancer risk factors by histologic subtype: an analysis from the Ovarian Cancer Cohort Consortium. J Clin Oncol. 2016;34:2888‐2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7‐33. [DOI] [PubMed] [Google Scholar]
- 5. Torre LA, Trabert B, DeSantis CE, et al. Ovarian cancer statistics, 2018. CA Cancer J Clin. 2018;68:284‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Howlader N, Noone AM, Krapcho M, et al, eds. SEER Cancer Statistics Review, 1975‐2012. National Cancer Institute; 2015. [Google Scholar]
- 7. Cliby WA, Powell MA, Al‐Hammadi N, et al. Ovarian cancer in the United States: contemporary patterns of care associated with improved survival. Gynecol Oncol. 2015;136:11‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bristow RE, Chang J, Ziogas A, Campos B, Chavez LR, Anton‐Culver H. Sociodemographic disparities in advanced ovarian cancer survival and adherence to treatment guidelines. Obstet Gynecol. 2015;125:833‐842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin JJ, Egorova N, Franco R, Prasad‐Hayes M, Bickell NA. Ovarian cancer treatment and survival trends among women older than 65 years of age in the United States, 1995‐2008. Obstet Gynecol. 2016;127:81‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Warren JL, Harlan LC, Trimble EL, Stevens J, Grimes M, Cronin KA. Trends in the receipt of guideline care and survival for women with ovarian cancer: a population‐based study. Gynecol Oncol. 2017;145:486‐492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jervis S, Song H, Lee A, et al. Ovarian cancer familial relative risks by tumour subtypes and by known ovarian cancer genetic susceptibility variants. J Med Genet. 2014;51:108‐113. [DOI] [PubMed] [Google Scholar]
- 12. Soegaard M, Frederiksen K, Jensen A, et al. Risk of ovarian cancer in women with first‐degree relatives with cancer. Acta Obstet Gynecol Scand. 2009;88:449‐456. [DOI] [PubMed] [Google Scholar]
- 13. National Comprehensive Cancer Network (NCCN) . NCCN Clinical Practice Guidelines in Oncology: Ovarian Cancer/Fallopian Tube Cancer/Primary Peritoneal Cancer. NCCN; 2021. Accessed February 25, 2021. https://www.nccn.org/guidelines/guidelines‐detail?category=1&id=1453 [Google Scholar]
- 14. Daly MB, Pilarski R, Berry M, et al. NCCN Guidelines insights: genetic/familial high‐risk assessment: Breast and ovarian, version 2.2017. J Natl Compr Canc Netw. 2017;15:9‐20. [DOI] [PubMed] [Google Scholar]
- 15. Gross AL, Blot WJ, Visvanathan K. BRCA1 and BRCA2 testing in medically underserved Medicare beneficiaries with breast or ovarian cancer. JAMA. 2018;320:597‐598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kurian AW, Ward KC, Howlader N, et al. Genetic testing and results in a population‐based cohort of breast cancer patients and ovarian cancer patients. J Clin Oncol. 2019;37:1305‐1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kurian AW, Ward KC, Abrahamse P, et al. Time trends in receipt of germline genetic testing and results for women diagnosed with breast cancer or ovarian cancer, 2012‐2019. J Clin Oncol. 2021;39:1631‐1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rim SH, Hirsch S, Thomas CC, et al. Gynecologic oncologists involvement on ovarian cancer standard of care receipt and survival. World J Obstet Gynecol. 2016;5:187‐196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Committee on the State of the Science in Ovarian Cancer Research ; Board on Health Care Services ; Institute of Medicine; National Academies of Sciences, Engineering, and Medicine . Ovarian Cancers: Evolving Paradigms in Research and Care. National Academies Press (US); 2016. [PubMed] [Google Scholar]
- 20. Thaker PH, Smeltzer MP, Dawkins M, et al. Improving the quality of care for persons with advanced epithelial ovarian cancer. Oncol Issues. 2021;36:36‐48. [Google Scholar]
- 21. Weaver SJ, Jacobsen PB. Cancer care coordination: opportunities for healthcare delivery research. Transl Behav Med. 2018;8:503‐508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Institute of Medicine . Delivering High‐Quality Cancer Care: Charting a New Course for a System in Crisis. National Academies Press (US); 2013. [PubMed] [Google Scholar]
- 23. Katz SJ, Belkora J, Elwyn G. Shared decision making for treatment of cancer: challenges and opportunities. J Oncol Pract. 2014;10:206‐208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Roche KL, Angarita AM, Cristello A, et al. “Little Big Things”: a qualitative study of ovarian cancer survivors and their experiences with the health care system. J Oncol Pract. 2016;12:e974‐e980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Epstein RM, Street RL Jr. Patient‐Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. NIH Publication No. 07‐6225. US Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2007. [Google Scholar]
- 26. Institute of Medicine (US) Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting ; Adler NE, Page AEK, eds. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. National Academies Press (US); 2008. [PubMed] [Google Scholar]
- 27. Oncology Nursing Society; Association of Oncology Social Work; National Association of Social Workers. Oncology Nursing Society, the Association of Oncology Social Work, and the National Association of Social Workers joint position on the role of oncology nursing and oncology social work in patient navigation. Oncol Nurs Forum. 2010;37:251‐252. [PubMed] [Google Scholar]
- 28. Kline RM, Rocque GB, Rohan EA, et al. Patient navigation in cancer: the business case to support clinical needs. J Oncol Pract. 2019;15:585‐590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Oncology Nursing Society . 2017 Oncology Nurse Navigator Core Competencies. Accessed February 25, 2021. https://www.ons.org/sites/default/files/2017‐05/2017_Oncology_Nurse_Navigator_Competencies.pdf
- 30. Schorge JO, Modesitt SC, Coleman RL, et al. SGO white paper on ovarian cancer: etiology, screening and surveillance. Gynecol Oncol. 2010;119:7‐17. [DOI] [PubMed] [Google Scholar]
- 31. Clarke BA, Crum CP, Nucci MR, Oliva E, Cooper K; members of the Cancer Committee, College of American Pathologists . Protocol for the Examination of Specimens From Patients With Carcinoma of the Fallopian Tube. College of American Pathologists; 2013. Accessed February 25, 2021. https://webapps.cap.org/apps/docs/committees/cancer/cancer_protocols/2013/FallopianTube_13protocol_3101.pdf [Google Scholar]
- 32. Medeiros F, Muto MG, Lee Y, et al. The tubal fimbria is a preferred site for early adenocarcinoma in women with familial ovarian cancer syndrome. Am J Surg Pathol. 2006;30:230‐236. [DOI] [PubMed] [Google Scholar]
- 33. Kuhn E, Kurman RJ, Shih IM. Ovarian cancer is an imported disease: fact or fiction? Curr Obstet Gynecol Rep. 2012;1:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kurman RJ, Shih IM. Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer—shifting the paradigm. Hum Pathol. 2011;42:918‐931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Piek JM, van Diest PJ, Zweemer RP, et al. Dysplastic changes in prophylactically removed fallopian tubes of women predisposed to developing ovarian cancer. J Pathol. 2001;195:451‐456. [DOI] [PubMed] [Google Scholar]
- 36. Callahan MJ, Crum CP, Medeiros F, et al. Primary fallopian tube malignancies in BRCA‐positive women undergoing surgery for ovarian cancer risk reduction. J Clin Oncol. 2007;25:3985‐3990. [DOI] [PubMed] [Google Scholar]
- 37. Carcangiu ML, Radice P, Manoukian S, et al. Atypical epithelial proliferation in fallopian tubes in prophylactic salpingo‐oophorectomy specimens from BRCA1 and BRCA2 germline mutation carriers. Int J Gynecol Pathol. 2004;23:35‐40. [DOI] [PubMed] [Google Scholar]
- 38. Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616‐1622. [DOI] [PubMed] [Google Scholar]
- 39. Kauff ND, Domchek SM, Friebel TM, et al. Risk‐reducing salpingo‐oophorectomy for the prevention of BRCA1‐ and BRCA2‐associated breast and gynecologic cancer: a multicenter, prospective study. J Clin Oncol. 2008;26:1331‐1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kauff ND, Satagopan JM, Robson ME, et al. Risk‐reducing salpingo‐oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002;346:1609‐1615. [DOI] [PubMed] [Google Scholar]
- 41. Rebbeck TR, Kauff ND, Domchek SM. Meta‐analysis of risk reduction estimates associated with risk‐reducing salpingo‐oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst. 2009;101:80‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Movahedi‐Lankarani S, Krishnamurti U, Bell DA, et al; College of American Pathologists (CAP) Cancer and CAP Pathology Electronic Reporting Committees. Protocol for the Examination of Specimens From Patients With Primary Tumors of the Ovary, Fallopian Tube, or Peritoneum. Version 1.1.0.0. College of American Pathologists; 2018. Accessed February 25, 2021. https://documents.cap.org/protocols/cp‐femalereproductive‐ovary‐fallopian‐18protocol‐1100.pdf [Google Scholar]
- 43. Stewart SL, Cooney D, Hirsch S, et al. The effect of gynecologic oncologist availability on ovarian cancer mortality. World J Obstet Gynecol. 2014;3:71‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ricci S, Tergas AI, Roche KL, et al. Geographic disparities in the distribution of the U.S. gynecologic oncology workforce: a Society of Gynecologic Oncology study. Gynecol Oncol Rep. 2017;22:100‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Petzel SV, Vogel RI, McNiel J, Leininger A, Argenta PA, Geller MA. Improving referral for genetic risk assessment in ovarian cancer using an electronic medical record system. Int J Gynecol Cancer. 2014;24:1003‐1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sweet KM, Bradley TL, Westman JA. Identification and referral of families at high risk for cancer susceptibility. J Clin Oncol. 2002;20:528‐537. [DOI] [PubMed] [Google Scholar]
- 47. Goldfarb SB, Kamer SA, Oppong BA, et al. Fertility preservation for the young breast cancer patient. Ann Surg Oncol. 2016;23:1530‐1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chin HB, Howards PP, Kramer MR, Mertens AC, Spencer JB. Which female cancer patients fail to receive fertility counseling before treatment in the state of Georgia? Fertil Steril. 2016;106:1763‐1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lewis JH, Kilgore ML, Goldman DP, et al. Participation of patients 65 years of age or older in cancer clinical trials. J Clin Oncol. 2003;21:1383‐1389. [DOI] [PubMed] [Google Scholar]
- 50. Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race‐, sex‐, and age‐based disparities. JAMA. 2004;291:2720‐2726. [DOI] [PubMed] [Google Scholar]
- 51. Talarico L, Chen G, Pazdur R. Enrollment of elderly patients in clinical trials for cancer drug registration: a 7‐year experience by the US Food and Drug Administration. J Clin Oncol. 2004;22:4626‐4631. [DOI] [PubMed] [Google Scholar]
- 52. Moorcraft SY, Marriott C, Peckitt C, et al. Patients' willingness to participate in clinical trials and their views on aspects of cancer research: results of a prospective patient survey. Trials. 2016;17:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Jacobs SR, Weiner BJ, Reeve BB, Weinberger M, Minasian LM, Good MJ. Organizational and physician factors associated with patient enrollment in cancer clinical trials. Clin Trials. 2014;11:565‐575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wells KJ, Valverde P, Ustjanauskas AE, Calhoun EA, Risendal BC. What are patient navigators doing, for whom, and where? A national survey evaluating the types of services provided by patient navigators. Patient Educ Couns. 2018;101:285‐294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Fouad MN, Acemgil A, Bae S, et al. Patient navigation as a model to increase participation of African Americans in cancer clinical trials. J Oncol Pract. 2016;12:556‐563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cartmell KB, Bonilha HS, Simpson KN, Ford ME, Bryant DC, Alberg AJ. Patient barriers to cancer clinical trial participation and navigator activities to assist. Adv Cancer Res. 2020;146:139‐166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Holmes DR, Major J, Lyonga DE, Alleyne RS, Clayton SM. Increasing minority patient participation in cancer clinical trials using oncology nurse navigation. Am J Surg. 2012;203:415‐422. [DOI] [PubMed] [Google Scholar]
- 58. Pujade‐Lauraine E, Hilpert F, Weber B, et al. Bevacizumab combined with chemotherapy for platinum‐resistant recurrent ovarian cancer: the AURELIA open‐label randomized phase III trial [erratum in J Clin Oncol. 2014;32:4025]. J Clin Oncol. 2014;32:1302‐1308. [DOI] [PubMed] [Google Scholar]
- 59. Pfisterer J, Shannon CM, Baumann K, et al. Bevacizumab and platinum‐based combinations for recurrent ovarian cancer: a randomised, open‐label, phase 3 trial. Lancet Oncol. 2020;21:699‐709. [DOI] [PubMed] [Google Scholar]
- 60. Garofalo D, Aydin E, Labrador M, et al. Real‐world data analysis of ovarian cancer (OC) maintenance utilization among maintenance eligible patients. J Clin Oncol. 2019;37:5579. [Google Scholar]
- 61. Siddiqui M, Rajkumar SV. The high cost of cancer drugs and what we can do about it. Mayo Clin Proc. 2012;87:935‐943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Faubion SS, MacLaughlin KL, Long ME, Pruthi S, Casey PM. Surveillance and care of the gynecologic cancer survivor. J Womens Health (Larchmt). 2015;24:899‐906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Salani R, Khanna N, Frimer M, Bristow RE, Chen LM. An update on post‐treatment surveillance and diagnosis of recurrence in women with gynecologic malignancies: Society of Gynecologic Oncology (SGO) recommendations. Gynecol Oncol. 2017;146:3‐10. [DOI] [PubMed] [Google Scholar]
- 64. Esselen KM, Cronin AM, Bixel K, et al. Use of CA‐125 tests and computed tomographic scans for surveillance in ovarian cancer. JAMA Oncol. 2016;2:1427‐1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Armstrong A, Otvos B, Singh S, Debernardo R. Evaluation of the cost of CA‐125 measurement, physical exam, and imaging in the diagnosis of recurrent ovarian cancer. Gynecol Oncol. 2013;131:503‐507. [DOI] [PubMed] [Google Scholar]
- 66. Rimel BJ, Burke WM, Higgins RV, Lee PS, Lutman CV, Parker L. Improving quality and decreasing cost in gynecologic oncology care. Society of Gynecologic Oncology recommendations for clinical practice. Gynecol Oncol. 2015;137:280‐284. [DOI] [PubMed] [Google Scholar]
- 67. Bandera EV, Lee VS, Rodriguez‐Rodriguez L, Powell CB, Kushi LH. Racial/ethnic disparities in ovarian cancer treatment and survival. Clin Cancer Res. 2016;22:5909‐5914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Howell EA, Egorova N, Hayes MP, Wisnivesky J, Franco R, Bickell N. Racial disparities in the treatment of advanced epithelial ovarian cancer. Obstet Gynecol. 2013;122:1025‐1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Karanth S, Fowler ME, Mao X, et al. Race, socioeconomic status, and health‐care access disparities in ovarian cancer treatment and mortality: systematic review and meta‐analysis. JNCI Cancer Spectr. 2019;3:pkz084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Bristow RE, Powell MA, Al‐Hammadi N, et al. Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. J Natl Cancer Inst. 2013;105:823‐832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Cronin KA, Howlader N, Stevens JL, Trimble EL, Harlan LC, Warren JL. Racial disparities in the receipt of guideline care and cancer deaths for women with ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2019;28:539‐545. [DOI] [PubMed] [Google Scholar]
- 72. Fuh KC, Shin JY, Kapp DS, et al. Survival differences of Asian and Caucasian epithelial ovarian cancer patients in the United States. Gynecol Oncol. 2015;136:491‐497. [DOI] [PubMed] [Google Scholar]
- 73. Singh SD, Ryerson AB, Wu M, Kaur JS. Ovarian and uterine cancer incidence and mortality in American Indian and Alaska Native women, United States, 1999‐2009. Am J Public Health. 2014;104(suppl 3):S423‐S431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Mishkin G, Minasian LM, Kohn EC, Noone AM, Temkin SM. The generalizability of NCI‐sponsored clinical trials accrual among women with gynecologic malignancies. Gynecol Oncol. 2016;143:611‐616. [DOI] [PubMed] [Google Scholar]
- 75. Terplan M, Schluterman N, McNamara EJ, Tracy JK, Temkin SM. Have racial disparities in ovarian cancer increased over time? An analysis of SEER data. Gynecol Oncol. 2012;125:19‐24. [DOI] [PubMed] [Google Scholar]
- 76. Penner LA, Dovidio JF, Gonzalez R, et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol. 2016;34:2874‐2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Chase DM, Wenzel L. Health‐related quality of life in ovarian cancer patients and its impact on clinical management. Expert Rev Pharmacoecon Outcomes Res. 2011;11:421‐431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Zhou Y, Cartmel B, Gottlieb L, et al. Randomized trial of exercise on quality of life in women with ovarian cancer: Women's Activity and Lifestyle Study in Connecticut (WALC). J Natl Cancer Inst. 2017;109:djx072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Gunnarsdottir S, Donovan HS, Serlin RC, Voge C, Ward S. Patient‐related barriers to pain management: the Barriers Questionnaire II (BQ‐II). Pain. 2002;99:385‐396. [DOI] [PubMed] [Google Scholar]
- 80. Passik SD, Kirsh KL, Donaghy K, et al. Patient‐related barriers to fatigue communication: initial validation of the fatigue management barriers questionnaire. J Pain Symptom Manage. 2002;24:481‐493. [DOI] [PubMed] [Google Scholar]
- 81. Lheureux S, Braunstein M, Oza AM. Epithelial ovarian cancer: evolution of management in the era of precision medicine. CA Cancer J Clin. 2019;69:280‐304. [DOI] [PubMed] [Google Scholar]
- 82. University of Alabama Birmingham (UAB) Medicine . Comprehensive Ovarian Cancer Program. Accessed February 25, 2021. https://www.uabmedicine.org/web/medicalprofessionals/comprehensive‐ovarian‐cancer‐program


