Abstract
Background
Undernutrition and overnutrition have been considered separate challenges caused by the distinct factors in distinct settings. The double burden of malnutrition is defined as the coexistence of both undernutrition and overnutrition, which has now spread globally, especially in low‐ and middle‐income countries. In Kenya, the double burden of malnutrition is present in the capital city but the situation in rural areas currently remains unknown. The aim of this study was therefore to analyze nutritional status in rural Kenya.
Methods
Data from height and weight measurements conducted by teachers in the third term of school year 2013 were collected from primary schools. Teachers were trained by experts before starting the measurements. The Z‐scores of height‐for‐age, weight‐for‐age, and body mass index‐for‐age were calculated using AnthroPlus, and nutritional status was defined according to the World Health Organization guidelines.
Results
Data analyzed from 7,447 pupils (3,763 boys and 3,684 girls) showed that 12.4% were stunted and 7.8% were underweight among those ≤120 months old, and 11.7% were thin among those >120 months old. Boys were more likely to be stunted than girls. Boys were more likely to be underweight and girls were more likely to be overweight in the older age group.
Conclusion
The double burden of malnutrition was not found, and undernutrition was still common among schoolchildren in the study area. However, it is important to monitor nutritional status due to adverse effects of rapid urbanization. Height and weight measurements in schools may be useful for monitoring the nutritional status of schoolchildren.
Keywords: double burden of malnutrition, Kenya, overweight, school health, underweight
Malnutrition, including both undernutrition and overnutrition, has remained a global challenge 1 , 2 and is present in both adults and children. 3 , 4 , 5 As of 2014, more than 1.9 billion adults aged 18 years and older were overweight, and 462 million were underweight. 6 In 2019, 38 million children under 5 years old were overweight, 144 million were stunted, and 47 million were suffering wasting worldwide. 4 In high‐income countries such as the USA, overnutrition has been a problem as a cause of non‐communicable diseases (NCDs). In low‐ and middle‐income countries (LMICs), too, overnutrition has been increasing as a problem, even though the problem of undernutrition still remains. 2 , 3
Malnutrition has a big impact on health. Overweight and obesity can be linked to diet‐related NCDs such as cardiovascular diseases and diabetes mellitus. 7 , 8 Undernutrition is linked to around 45% of deaths among children under 5 years old. 9 Although it may not be a direct cause among the principal causes of death in young children, undernutrition is responsible for 60.7% of deaths from diarrhea, 52.3% of deaths from pneumonia, 44.8% of deaths from measles, and 57.3% of deaths from malaria. 10 Moreover, malnutrition in childhood affects both physical and mental development, which later influence adulthood in terms of body size, motor ability, and learning ability, among other factors, and may also relate to the completion of schooling. 11
Over the past decades, the landscape of global nutrition has gradually changed to one of a “double burden of malnutrition,” which is defined as the coexistence of undernutrition and overweight, obesity, or diet‐related NCDs within individuals, households, and populations and across the course of life. 2 , 12 Before this concept was established, undernutrition and overnutrition were considered separate challenges in different populations with contrasting factors, such as poverty and food insecurity for undernutrition, and affluence and diet richness for overnutrition. However, the double burden of malnutrition can now be seen globally, especially in LMICs. 13 , 14 , 15 , 16 , 17 , 18 Countries in the highest quartiles of income among LMICs were the typical regions affected by the double burden of malnutrition in the 1990s, but recently, however, the level of this double burden has become much more severe in LMICs in the lowest income quartile, including countries in South Asia, East Asia, and Sub‐Saharan Africa. 17 Rapid urbanization has been occurring in developing regions, especially in Africa, which has undergone the most rapid urbanization at 3.7% annually from 2010 to 2015. Nevertheless, income levels are much lower than those in other regions at similar levels of urbanization. 19 This urban poor setting contributes to increased food insecurity, more street food vendors, and more reliance on staple foods and processed foods, which are associated with higher intake of fat, sugars, and energy. 20 Thus, this rapid urbanization is linked to dietary changes and may consequently contribute to increasing overweight and obesity among low‐income countries and populations. 21
In Kenya, 26% of children under 5 years are stunted and 11% are underweight. Nevertheless, 33% of women aged 15–49 years are overweight or obese. Stunting among children under five is more common in rural areas (29%) than urban areas (20%), and overweight and obesity among women are more common in urban areas (43%) than rural areas, although the prevalence in rural areas is still high at 26%. 22 In previous studies conducted in 2008–2010 in an urban poor setting in Nairobi, Kenya, almost half of the children under five were stunted (46–47%), 11–12% were underweight, 2.5–2.6% were wasting, and 9% were overweight or obese. 23 , 24 Meanwhile, 32% of their mothers were overweight or obese and 7.5% were underweight. 24
There have been various reports on the nutritional status of school‐aged children. One study targeting 4‐ to 11‐year‐old children in public primary schools reported that 24.5% were stunted, 14.9% were underweight, and 9.7% were wasting. 25 Another study targeting 9‐ to 11‐year‐old children in both public and private primary schools showed that 3.7% were underweight, 14.4% were overweight, and 6.4% were obese. 26 One study targeting 10‐ to 15‐year‐old children indicated that pupils in private schools were more likely to be overweight/obese than those in public schools. The prevalence of overweight and obesity was 16.7% and 6.9%, respectively, in private schools but 5.7% and 1.6% in public schools. 27
The above studies were conducted in urban settings, especially in slums in Nairobi Province. However, the situation in rural areas has remained unknown thus far. In recent years, it has been assumed that changes in dietary habits have diffused through rural areas in Africa. Energy‐dense foods with minimal nutritional value, such as processed foods and sugar‐sweetened beverages, have become available at relatively cheap prices in rural areas along with modernization and urbanization. 2 , 17 , 28 Thus, the aim of this study was to describe the nutritional status of schoolchildren in Mbita Sub‐county, which is a relatively rural area in Homa‐bay County, Kenya.
Methods
Study site
This study was conducted in four locations: Gembe East, Gembe West, Rusinga East, and Rusinga West in Mbita Sub‐county, Homa‐bay County, Kenya. A school health project was conducted in these areas by the Institute of Tropical Medicine, Nagasaki University (NUITM), which was funded by the Japan International Cooperation Agency (JICA). The population of the study site was 68 319 as of 2018. 29 All four locations are located along the shores of Lake Victoria, and the main source of income is fisheries.
Study sample
The study sample comprised all pupils who went to public or private primary schools (n = 102) in the study area that participated in the school health project.
Height and weight measurements
Height and weight measurements were introduced to primary schools by the school health project as one of the activities. First, officers from the Ministry of Education and Ministry of Health in Mbita Sub‐county were trained as trainers for the measurement and recording of height and weight, its importance, and how to use the results. The training was provided during a 2 day workshop by officers from the central government and Japanese experts. Next, three teachers from each primary school in the study area were trained by these trainers under the supervision of central government officers and the Japanese experts. Height and weight scales and record sheets were provided by the project. Height and weight measurements in schools have been conducted during each school term (three terms per year) since 2013.
Data collection
Data on height and weight measurements obtained by trained teachers in each school were used for this study. The record sheets were collected from the schools once a year for data entry by the project team. The data collected in the third term of the 2013 school year were used to analyze nutritional status among the primary school children at the study sites. The students’ dates of birth were confirmed by the Health and Demographic Surveillance System (HDSS) of NUITM.
Data analysis
Anthropometric indices, height‐for‐age, weight‐for‐age, and body mass index (BMI)‐for‐age were calculated based on the growth standards promulgated by the World Health Organization (WHO) using AnthroPlus v1.0.4 (WHO, Geneva, Switzerland). According to the recommendations of WHO, weight‐for‐age was used for children up to 120 months old, whereas BMI‐for‐age was used for children over 10 years old. 30 Height‐for‐age was used for all pupils. Other statistical analyses, including descriptive analysis and comparison of a frequency distribution by χ2 testing, were conducted using STATA 16.1 (StataCorp LLC, College Station, TX, USA). A Z‐score of height‐for‐age (HAZ) <−2 SD of the WHO Reference 2007 was defined as stunting. A Z‐score of weight‐for‐age (WAZ) <−2 SD of the WHO Reference 2007 was defined as underweight, a Z‐score of BMI‐for‐age (BAZ) <−2 SD of the WHO Reference 2007 was defined as thinness, and WAZ >2 SD of the WHO Reference 2007 or BAZ > 1 SD of the WHO Reference 2007 was defined as overweight according to the WHO guidelines. 31
Ethical considerations
This study was approved by the Scientific and Ethics Review Unit of the Kenya Medical Research Institute (SSC Protocol No. 2916). Permission for research activity in schools was given by the local education office. The data used for this study were secondary data, so consent forms were not obtained from any of the individuals.
Results
Characteristics of participants
Height and weight measurements were recorded for 9,892 pupils (5,003 boys and 4,889 girls). The dates of birth were available for 7,452 of these pupils (3,766 boys and 3,686 girls) from the HDSS data. Furthermore, five pupils were excluded because they were beyond the age suitable for calculating anthropometric indices using AnthroPlus. Ultimately, data from 7,447 pupils (3,763 boys and 3,684 girls), 6,180 (3,138 boys and 3,042 girls) in public schools and 1,267 (625 boys and 642 girls) in private schools were analyzed. The mean ages were 139.5 ± 30.6 months for all pupils, 141.7 ± 30.2 months for the boys, and 128.5 ± 30.4 months for the girls (Table 1).
Table 1.
Characteristics of the study participants (N = 7,447)
| Characteristic | School type | Total | |
|---|---|---|---|
| Public | Private | ||
| Sex, n (%) | |||
| Boys | 3,138 (50.8) | 625 (49.3) | 3,763 (50.5) |
| Girls | 3,042 (49.2) | 642 (50.7) | 3,684 (49.5) |
| Age, months, mean (SD) | 141.7 (30.2) | 128.5 (30.4) | 139.5 (30.6) |
Nutritional status
Overall, 12.4% of the pupils were stunted, 7.8% were underweight among those less than or equal to 120 months old, and 11.7% were considered thin among those more than 120 months old (Table 2). HAZ and BAZ showed significant differences between the boys and girls (P < 0.001 for both), whereas WAZ did not show any difference between them. Boys were more likely to be stunted than girls. In the older age group, boys were more likely to be thin, and girls were more likely to be overweight (Table 2). HAZ tended to decrease along with age (Fig. 1).
Table 2.
Distribution of Z‐scores of height‐for‐age (HAZ), weight‐for‐age (WAZ), and BMI‐for‐age (BAZ) by sex
| Sex | HAZ (N = 7,437) | WAZ (N = 7,437) | BAZ (N = 5,180) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stunting <−2 SD | −2 SD≤ ≤2 SD | 2 SD< | P‐value | Underweight <−2 SD | −2 SD≤ ≤2 SD | Overweight 2 SD< | P‐value | Thinness <−2 SD | −2 SD≤ ≤1 SD | Overweight 1 SD< | P‐value | |
| Boys, n (%) | 573 (15.2) | 3,044 (81.0) | 142 (3.8) | <0.001 | 88 (8.0) | 993 (89.7) | 26 (2.3) | 0.972 | 345 (13.0) | 2,266 (85.5) | 40 (1.5) | <0.001 |
| Girls, n (%) | 573 (15.2) | 3,044 (81.0) | 142 (3.8) | – | 89 (7.7) | 1,035 (90.0) | 26 (2.3) | – | 261 (10.3) | 2,156 (85.3) | 112 (4.4) | – |
| Total, n (%) | 919 (12.4) | 6,243 (83.9) | 275 (3.7) | – | 177 (7.8) | 2,028 (89.9) | 52 (2.3) | – | 606 (11.7) | 4,422 (85.4) | 152 (2.9) | – |
BMI, body mass index.
Fig. 1.
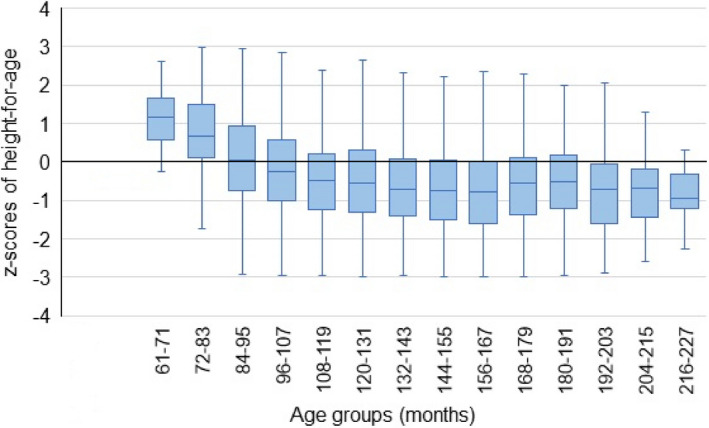
Z‐scores of height‐for‐age (HAZ) by age.
Weight‐for‐age showed a statistical difference between the public schools and private schools. Pupils in the public schools tended to be underweight compared to those in the private schools, with a prevalence of 8.9% and 4.7%, respectively (P = 0.005, Table 3). As very few of the pupils in the older group attended private schools, BAZ and HAZ were not compared.
Table 3.
Distribution of Z‐scores of weight‐for‐age (WAZ) by school type
| Characteristic | WAZ (N = 2,257) | P‐value | ||
|---|---|---|---|---|
| Underweight <−2 SD | ‐2 SD≤ ≤2 SD | Overweight 2 SD< | ||
| Public, n (%) | 151 (8.9) | 1,508 (88.8) | 40 (2.3) | 0.005 |
| Private, n (%) | 26 (4.7) | 520 (93.2) | 12 (2.1) | |
| Total, n (%) | 177 (7.8) | 2,028 (89.9) | 52 (2.3) | |
Discussion
In this study, the double burden of malnutrition was not found in the study area. Undernutrition was still common but girls were more likely to be overweight than boys in the older age group. Boys were also more likely to be stunted than girls in the study area. Public school children were more likely to be underweight than private school children in the lower age group.
Undernutrition is usually a result of poor dietary intake or disease. In addition, the following two scenarios are conceivable: (i) the problem of low weight due to lack of nutrition is increasing; (ii) the weight gain is not keeping up with the height increase accompanying growth. Regarding scenario 2, it may disappear as it grows, but scenario 1, it may have serious problems. The study area was a rural area in a relatively poor setting. 29 Aside from Mbita township, most of the remaining areas are extremely rural, and it is very difficult to access the town to buy junk food. The residents usually planted maize (as a staple food in Kenya) at home for self‐consumption. Around 2011–2012, a severe drought affected East‐African countries, including Kenya, 32 which resulted in food insecurity. The human intestinal parasite Schistosoma mansoni is also very common in the study area. 33 , 34 These conditions might relate to the nutritional status of children in the area.
Although the double burden of malnutrition was not found in the study area, it is still important to monitor nutritional situation. Rapid urbanization in LMICs has caused overweight and obesity among various age groups of low socio‐economic populations due to changes in the food system and lifestyles. 2 , 5 , 17 , 21 , 26 , 35 Previous studies in Kenya reported that the double burden of malnutrition in children has been seen in urban slum settings. 24 , 26 According to the Kenya housing and population census in 2009 and 2019, the Kenyan population rose from 37.7 million to 47.6 million in this 10‐year period, and the population in Homa‐bay County in 2019 was 1.2 times the 2009 population. 29 , 36 Rapid population growth and rapid urbanization have led to slums and urban poor.
Town areas in the study area have been expanding due to population growth and a main road that connects to the capital of Homa‐bay County, which was paved with asphalt in the middle of the 2010s. Thus, residents in the study area have much easier access to cheaper processed food. This study was conducted in late 2013, so it might not have caught the change in nutritional status that may have occurred with these background changes.
The girls in the older group (>120 months old) showed a greater tendency toward overweight than the boys in the study area. This result is consistent with previous studies that targeted schoolchildren or adults (>15 years old) in African countries. 37 , 38 , 39 , 40 One cause of overweight is an imbalance of energy between calories ingested and calories expended. Some causes of energy imbalance are an increased intake of energy‐dense foods and increased physical inactivity. A study in Nairobi, Kenya, indicated that boys aged 9–11 years were more likely to engage in physical activities than girls. 26 The Kenya demographic and health survey of 2014 reported that 61% of women aged 15–19 years did not engage in any physical activity at all, whereas 36% of males in the same age group did not do any physical exercise. 22
In contrast, a study in Brazil reported that boys aged 12–18 years were more overweight than girls, 41 and a study in Indonesia showed no difference of overweight prevalence between boys and girls aged 8–10 years. 42 Our study also found that the younger age group did not show any difference in WAZ between boys and girls. This inconsistent phenomenon might be related to the difference of child growth patterns between boys and girls due to the variation of age range of the study samples. In addition, differences of environmental and sociocultural factors might contribute to this inconsistent phenomenon among countries. The present study also found that boys were more likely to be stunted than girls. This finding is consistent with several other studies 43 , 44 , 45 , 46 , 47 but the reason for this result is still unknown. Male sex has been considered a risk factor for preterm infants, 43 , 48 which might affect later body size.
The present study also showed that among the lower age group, pupils in the public schools had a tendency to be underweight compared to those in the private schools. This result is consistent with a previous study in Nairobi, Kenya, 27 although it reported a much greater incidence of overweight pupils in private schools than in public schools. In the study area, neither public nor private schools offered school lunch. Unlike private schools in urban areas, most of the private schools in Mbita do not have such a positive environment, but they could collect some contributions from parents / guardians of pupils and offer porridge to pupils as a 10 o'clock snack. This might be one reason for this phenomenon.
This study used data obtained by teachers in schools. It is unclear how accurate the teachers' measurements were, and this might be a limitation of this study. Studies in the USA showed that the measurements of height and weight by school staff and school nurses were accurate enough to screen students' BMI. 49 , 50 In addition, teachers in our study were all trained by central government officers and Japanese experts. We therefore considered the quality of the data to be good enough to screen the study children's nutritional status. In Japan, the measurement of height and weight and health checkups have been conducted in schools since the late 1800s, and the data have been used to grasp the dynamics of nutritional status among schoolchildren. 51 , 52
There are some concerns about conducting height and weight measurements in schools. In the USA, it has been discussed that BMI measurements in schools might bring harmful consequences such as bullying and low self‐esteem among malnourished children, and overreactions of parents. 53 , 54 In fact, some teachers in this study reported that even if the pupils were screened for malnutrition, it was difficult to consult or give advice to them and their guardians because of their economic situation – i.e., the guardians could not provide enough food for their children because of a lack of money or food insecurity.
However, according to the teachers in the participating schools, the pupils were interested in measuring their height and weight, which is a good entry point to developing an interest in their own health from a health education perspective. Thus, the measurement of height and weight in schools would appear to have merit for children’s health. Another difficulty faced during the study was the confirmation of the schoolchildren’s dates of birth. Most of the pupils did not know their dates of birth, and therefore, HDSS data were used to confirm them in this study. If height and weight measurements are introduced to schools, it will be necessary to consider how to accurately confirm dates of birth.
Conclusions
The double burden of malnutrition was not found in the study area in 2013, but undernutrition was still common among schoolchildren. However, rapid urbanization and rapid population growth have been occurring in the area, making it important to longitudinally monitor nutritional status. Height and weight measurements in schools may be useful tools for monitoring schoolchildren’s nutritional status.
Disclosure
This study was supported by a Grant for the National Center for Global Health and Medicine (30‐4). The sponsor did not play any role in this study.
Author contributions
R.T. and J.K. designed the study. R.T., S.T., T. As., T. Ak., H.K., A.M., and B.W. performed training for the measurements. R.T. and H.K. performed data collection. R.T. performed data analysis. S.M.N., D.W.N., Y.K., and J.K. provided technical advice. R.T. drafted the manuscript. S.T., T. As., and J.K. critically reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgment
This work is a part of the JICA partnership project, “Supporting Health from School to Community in Mbita Sub‐county, Homa‐bay County,” which is supported by the Japan International Cooperation Agency (JICA). We are grateful to Professor Masaaki Shimada and Professor Yoshio Ichinose for their support and encouragement. Many thanks are given to the officers of the Ministry of Education and Ministry of Health in Mbita and all of the field staff. We appreciate all the teachers and pupils who participated in this study. This paper has been published with the permission of the Director General, Kenya Medical Research Institute. This work was supported by JSPS KAKENHI Grant Number JP19K21756.
References
- 1. World Health Organization . Global nutrition policy review 2016‐2017: country progress in creating enabling policy environments for promoting healthy diets and nutrition. Geneva: World Health Organization; 2018. Licence: CC BY‐NC‐SA 3.0 IGO. [Google Scholar]
- 2. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012; 70: 3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. NCD Risk Factor Collaboration (NCD‐RisC) . Trends in adult body‐mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population‐based measurement studies with 19.2 million participants. Lancet 2016; 387: 1377–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. UNICEF/WHO/World Bank . Level and trends in child malnutrition: joint child malnutrition estimates. Key findings of the 2017 edition. Geneva: United Nations Children's Fund (UNICEF)/World Health Organization (WHO)/World Bank; 2018. http://www.who.int/nutgrowthdb/estimates2017/en/ [Google Scholar]
- 5. NCD Risk Factor Collaboration (NCD‐RisC) . Worldwide trends in body‐mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population‐based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017; 390: 2627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization [homepage on the internet]. Nutrition: Double burden of malnutrition. [Cited 9 Dec 2020]. Available from: https://www.who.int/nutrition/double‐burden‐malnutrition/en/ [Google Scholar]
- 7. World Health Organization . Global Report on Diabetes. World Health Organization, Geneva, 2016. http://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf?sequence=1 [Google Scholar]
- 8. Greenberg H, Deckelbaum RJ. Chapter 2.3 Diet and non‐communicable diseases: An urgent need for new paradigms. In: Eggersdorfer M, Kraemer K, Cordaro JB et al. (eds). Good Nutrition: Perspectives for the 21st Century. Karger, Basel, 2016; 105‐18. https://www.karger.com/Article/PDF/452379 [Google Scholar]
- 9. World Health Organization [homepage on the internet]. Malnutrition. [Cited 9 Dec 2020]. Available from: https://www.who.int/news‐room/fact‐sheets/detail/malnutrition [Google Scholar]
- 10. Caulfield LE, De Onis M, Blössner M, Black RE. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am. J. Clin. Nutr. 2004; 80: 193–8. [DOI] [PubMed] [Google Scholar]
- 11. Alderman H, Hoddinott J, Kinsey B. Long‐term consequences of early childhood malnutrition. Oxf. Econ. Pap. 2006; 58: 450–74. [Google Scholar]
- 12. World Health Organization . The Double Burden of Malnutrition: Policy Brief. World Health Organization, Geneva, 2017. https://apps.who.int/iris/bitstream/handle/10665/255413/WHO‐NMH‐NHD‐17.3‐eng.pdf?ua=1 [Google Scholar]
- 13. Global Nutrition Report Stakeholder Group . 2020 Global Nutrition Report: Action on equity to end malnutrition. Development Initiatives, Bristol, 2020. https://globalnutritionreport.org/reports/2020‐global‐nutrition‐report/ [Google Scholar]
- 14. Black RE, Victora CG, Walker SP et al. Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet 2013; 382: 427–51. [DOI] [PubMed] [Google Scholar]
- 15. Tzioumis E, Adair LS. Childhood dual burden of under‐ and overnutrition in low‐ and middle‐income countries: A critical review. Food Nutr. Bull. 2014; 35: 230–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Caleyachetty R, Thomas GN, Kengne AP et al. The double burden of malnutrition among adolescents: Analysis of data from the Global School‐Based Student Health and Health Behavior in School‐Aged Children surveys in 57 low‐ and middle‐income countries. Am. J. Clin. Nutr. 2018; 108: 414–24. [DOI] [PubMed] [Google Scholar]
- 17. Popkin BM, Corvalan C, Grummer‐Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020; 395: 65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wells JC, Sawaya AL, Wibaek R et al. The double burden of malnutrition: Aetiological pathways and consequences for health. Lancet 2020; 395: 75–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. United Nations Human Settlements Programme . World cities report 2020: The value of sustainable urbanization. United Nations Human Settlements Programme, Nairobi, 2020. https://unhabitat.org/sites/default/files/2020/10/wcr_2020_report.pdf [Google Scholar]
- 20. FAO, IFAD, UNICEF, WFP, WHO . The State of Food Security and Nutrition in the World 2020. Transforming food systems for affordable healthy diets. Food and Agriculture Organization, Rome; 2020. 10.4060/ca9692en [DOI] [Google Scholar]
- 21. FAO . Globalization of food systems in developing countries: impact on food security and nutrition. FAO, Rome, 2004. http://www.fao.org/3/a‐y5736e.pdf [PubMed] [Google Scholar]
- 22. Kenya National Bureau of Statistics . Kenya Demographic and Health Survey 2014. Kenya National Bureau of Statistics, Nairobi, 2015. https://www.knbs.or.ke/?wpdmpro=2014‐kenya‐demographic‐and‐health‐survey&wpdmdl=3580 [Google Scholar]
- 23. Olack B, Burke H, Cosmas L et al. Nutritional status of under‐five children living in an informal urban settlement in Nairobi, Kenya. J. Health Popul. Nutr. 2011; 29: 357–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kimani‐Murage EW, Muthuri SK, Oti SO, Mutua MK, van de Vijver S, Kyobutungi C. Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. PLoS One 2015; 10: e0129943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mwaniki EW, Makokha AN. Nutrition status and associated factors among children in public primary schools in Dagoretti, Nairobi, Kenya. Afr. Health Sci. 2013; 13: 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Muthuri SK, Wachira LJ, Onywera VO, Tremblay MS. Correlates of objectively measured overweight/obesity and physical activity in Kenyan school children: Results from ISCOLE‐Kenya. BMC Public Health 2014; 14: 436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kamau JW, Wanderi MP, Njororai WWS, Wamukoya EK. Prevalence of overweight and obesity among primary school children in Nairobi province, Kenya. Afr. J. Phys. Health Educ. 2011; 17: 312–27. 10.4314/ajpherd.v17i2.67668 [DOI] [Google Scholar]
- 28. Food and Agriculture Organization, Economic Commission for Africa, African Union Commission . 2019 Africa regional overview of food security and nutrition. Accra: FAO; 2020. 10.4060/CA7343EN [DOI] [Google Scholar]
- 29. Kenya National Bureau of Statistics . 2019 Kenya population and housing census volume II: Distribution of population by administrative units. Kenya National Bureau of Statistics, Nairobi. 2020. https://www.knbs.or.ke/?wpdmpro=2019‐kenya‐population‐and‐housing‐census‐volume‐ii‐distribution‐of‐population‐by‐administrative‐units [Google Scholar]
- 30. World Health Organization . WHO AnthroPlus for personal computers manual: Software for assessing growth of the world's children and adolescents. World Health Organization, Geneva, 2009. http://www.who.int/growthref/tools/en/ [Google Scholar]
- 31. World Health Organization . Nutrition landscape information system (NLIS) country profile indicators: interpretation guide. World Health Organization, Geneva, 2010. https://www.who.int/nutrition/nlis_interpretation_guide.pdf [Google Scholar]
- 32. United Nations Office for the Coordination of Humanitarian Affairs [homepage on the internet]. Eastern Africa Drought Humanitarian Report No. 3, 10 June 2011. reliefweb.int. [Cited 23 Dec 2020]. Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/OCHA%20Eastern%20Africa%20Humanitarian%20Report%20No.%203%20‐%20Drought%20May%202011%20FINAL.pdf [Google Scholar]
- 33. Nagi S, Chadeka EA, Sunahara T et al. Risk factors and spatial distribution of schistosoma mansoni infection among primary school children in Mbita district, Western Kenya. PLoS Negl. Trop. Dis. 2014; 8: e2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Takeuchi R, Njenga SM, Ichinose Y, Kaneko S, Estrada CA, Kobayashi J. Is there a gap between health education content and practice toward schistosomiasis prevention among schoolchildren along the shores of Lake Victoria in Kenya? PLOS Negl. Trop. Dis. 2019; 13: e0007572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ziraba AK, Fotso JC, Ochako R. Overweight and obesity in urban Africa: A problem of the rich or the poor? BMC Public Health 2009; 9: 465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kenya National Bureau of Statistics . 2009 Kenya population and housing census: Population distribution by sex, number of households, area and density by county and district. Kenya National Bureau of Statistics, Nairobi, 2017. https://www.knbs.or.ke/?wpdmpro=population‐distribution‐by‐sex‐number‐of‐households‐area‐and‐density‐by‐county‐and‐district [Google Scholar]
- 37. Muthuri SK, Francis CE, Wachira LJ et al. Evidence of an overweight/obesity transition among school‐aged children and youth in Sub‐Saharan Africa: A systematic review. PLoS One 2014; 9: e92846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Toselli S, Gualdi‐Russo E, Boulos DN et al. Prevalence of overweight and obesity in adults from North Africa. Eur. J. Public Health. 2014; 24(Suppl 1): 31–9. [DOI] [PubMed] [Google Scholar]
- 39. Price AJ, Crampin AC, Amberbir A et al. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub‐Saharan Africa: a cross‐sectional, population‐based study in rural and urban Malawi. Lancet. Diabetes Endocrinol. 2018; 6: 208–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Maruf FA, Aronu U, Chukwuegbu K, Aronu AE. Influence of gender on prevalence of overweight and obesity in Nigerian schoolchildren and adolescents. Tanzan J Health Res. 2013; 15: 247–51. [DOI] [PubMed] [Google Scholar]
- 41. Carneiro CS, Peixoto MDRG, Mendonça KL et al. Overweight and associated factors in adolescents from a Brazilian capital. Rev. Bras. Epidemiol. 2017; 20: 260–73. [DOI] [PubMed] [Google Scholar]
- 42. Soekirman H, Jus'at I, Jahari AB. Regional study of nutritional status of urban primary schoolchildren. 2. West Jakarta and Bogor, Indonesia. Food Nutr. Bull. 2002; 23: 31–40. [DOI] [PubMed] [Google Scholar]
- 43. Wamani H, Astrøm AN, Peterson S, Tumwine JK, Tylleskär T. Boys are more stunted than girls in sub‐Saharan Africa: a meta‐analysis of 16 demographic and health surveys. BMC Pediatr. 2007; 7: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Goon DT, Toriola AL, Shaw BS et al. Anthropometrically determined nutritional status of urban primary schoolchildren in Makurdi, Nigeria. BMC Public Health 2011; 11: 769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Saltzman E, Schlossman N, Brown CA et al. Nutrition status of primary school students in two rural regions of Guinea‐Bissau. Food Nutr. Bull. 2017; 38: 103–14. [DOI] [PubMed] [Google Scholar]
- 46. Ayogu RNB, Afiaenyi IC, Madukwe EU, Udenta EA. Prevalence and predictors of under‐nutrition among school children in a rural South‐eastern Nigerian community: A cross sectional study. BMC Public Health 2018; 18: 587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jonah CMP, Sambu WC, May JD. A comparative analysis of socioeconomic inequities in stunting: a case of three middle‐income African countries. Arch. Public Health. 2018; 76: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Elsmén E, Pupp HI, Hellström‐Westas L. Preterm male infants need more initial respiratory and circulatory support than female infants. Acta Paediatr. 2004; 93: 529–33. [DOI] [PubMed] [Google Scholar]
- 49. Thompson HR, Linchey JK, King B, Himes JH, Madsen KA. Accuracy of school staff‐measured height and weight used for body mass index screening and reporting. J. Sch. Health. 2019; 89: 629–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Stoddard SA, Kubik MY, Skay C. Is school‐based height and weight screening of elementary students private and reliable? J. Sch. Nurs. 2008; 24: 43–8. [DOI] [PubMed] [Google Scholar]
- 51. Japan Society of School Health [homepage on the internet]. History of school health (3). [Cited 25 Dec 2020]. Available from: https://www.gakkohoken.jp/column/archives/69 (in Japanese). [Google Scholar]
- 52. Ministry of Education, Culture, Sports, Science and Technology, Japan [homepage on the internet]. School health statistical survey: outline. [Cited 25 Dec 2020]. Available from: https://www.mext.go.jp/b_menu/toukei/chousa05/hoken/gaiyou/chousa/1268648.htm (in Japanese). [Google Scholar]
- 53. Eating Disorders Coalition . [homepage on the internet]. Facts and concerns about school‐based BMI screening, surveillance and reporting. Eating Disorders Coalition. [Cited 25 Dec 2020]. Available from: http://eatingdisorderscoalition.org.s208556.gridserver.com/couch/uploads/file/School%20Based%20BMI.pdf [Google Scholar]
- 54. Ikeda JP, Crawford PB, Woodward‐Lopez G. BMI screening in schools: helpful or harmful. Health Educ. Res. 2006; 21: 761–9. [DOI] [PubMed] [Google Scholar]


