Abstract
Background
Evidence supports the contribution of various stigma-related constructs to help-seeking. These constructs have yet to be tested in a single model among college students, a group highly affected by mental illness.
Aims
Using data from 153 college students this study examines factors contributing to help seeking for mental illness.
Method
Using path analysis, the current study evaluated a model of the relationship between level of familiarity, personal stigma, desired social distance, label avoidance, attitudes towards treatment seeking, and intentions to seek treatment.
Results
Findings support a model of help-seeking describing the relationship between familiarity with mental illness, personal stigma, social distance, label avoidance, attitudes and intentions to seek treatment.
Conclusions
Findings suggest label avoidance, attitudes towards treatment seeking and intentions to seek treatment might be augmented through interventions aimed at increasing college students’ levels of familiarity, or intimate contact, with individuals with mental illness. Additional implications for practice and further research are addressed.
Keywords: stigma, label avoidance, help seeking, college students, level of familiarity
Introduction
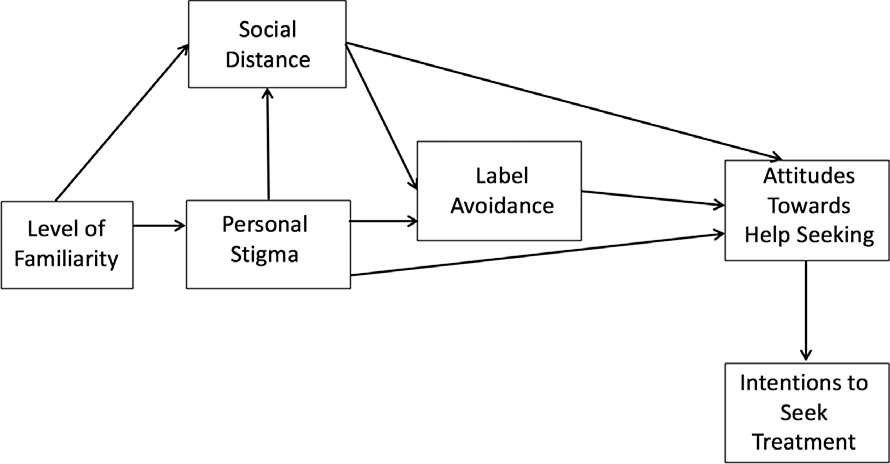
College campuses are a place where many students find themselves struggling with mental illness (Auerbach et al., 2018). The impact of mental illness on student outcomes such as graduation from college (Arria et al., 2013; Eisenberg, Golberstein & Hunt, 2009; Hunt, Eisenberg, & Kilbourne, 2010; Kessler, Foster & Saunders, 1995), employment (Ettner, Frank, & Kessler, 1997), experiences with substance use disorders (Weitzman, 2004), and social outcomes (Kessler et al., 1997; Kessler, Walters, & Forthofer, 1998) is well documented and profound. Research on mental illness in the general adult population, indicates the stigma related to mental illness—defined as negative stereotypes, prejudices with regard to individuals with mental illness, and the resulting discrimination experienced by people with mental illness (Corrigan, 2000; Corrigan & Kosyluk, 2014)—is one of the greatest barriers individuals with mental illness face in achieving life goals (Corrigan, Larson, & Rusch, 2009). Treatment participation for individuals with mental illness is an important factor contributing to recovery; however, the stigma associated with mental illness causes many individuals to avoid seeking mental health treatment (Corrigan, Druss, & Perlick, 2014). Eisenberg, Hunt, Speer, and Zivin (2011) report only about 36% of students experiencing a mental health condition sought services within the previous year. This statistic is perplexing given college campuses are one of the only locations where mental health treatments are frequently available at zero cost to the consumer. Though some research suggests that rates of intention to seek treatment for mental health concerns may be increasing over time (Oswalt, Lederer, Chestnut-Steich, Day, Halbritter, & Ortiz, 2019), it is likely perceptions of and experiences with stigma continue to negatively impact mental health help-seeking among college students. While research has provided evidence to support a model of the impact of stigma on help-seeking attitudes and behaviors among the adult population, this model has yet to be tested among the college student population. To address this gap, we set out to test a model (see figure 1) implicating mental illness stigma-related constructs in predicting treatment seeking among college students.
Figure 1.
Hypothesized model of the relationship between personal stigma, social distance, label avoidance, attitudes towards treatment seeking, and intentions to seek treatment.
Conceptual Model
Anagnostopoulos and Hantzi (2011) found level of familiarity with mental illness influences personal stigma and desired social distance. The greater one’s level of familiarity, or intimate knowledge of mental illness, the lower their level of personal stigma and desired social distance. Therefore, we propose a model where level of familiarity exerts exogenous influence on personal stigma and desired social distance from individuals with mental illness.
Previous work has shown personal stigma predicts desired social distance from individuals with mental illness, a proxy of discrimination (Anagnostopoulos & Hantzi, 2011; Corrigan et al., 2003; Link et al., 1999). The construct of discrimination is of particular interest as advocates agree improving attitudes towards individuals with mental illness is important, however the ultimate goal is to change behaviors (reduce discrimination) toward individuals with mental illness. Our model frames personal stigma as a predictor of desired social distance.
Personal stigma has been shown to be a significant predictor of college students’ attitudes towards seeking professional help for mental health concerns (Eisenberg, Downs, Golberstein, & Zivins, 2009). Therefore, we frame personal stigma and the related construct of social distance as predictors of attitudes towards help seeking for mental health concerns, such that the more personal stigma one holds and the more one desires social distance from individuals with mental illness, the more likely one is to have negative attitudes about seeking mental health treatment. Another type of stigma that may be of particular relevance to examining mental health service engagement in the college population is label avoidance (Corrigan & Kosyluk, 2014). Label avoidance involves an awareness of the general public’s stigma surrounding mental illness (perceived stigma) and efforts to evade this label by avoiding situations and places (e.g. a counselor’s office) that might prime this categorization (Corrigan, 2000; Corrigan & Kosyluk, 2014; Rusch, Angermeyer, & Corrigan, 2005). Findings of a meta-analysis conducted by Nam and colleagues (2013) suggest that label avoidance may be the most significant barrier to seeking mental health care among college students. Previous work suggests that personal stigma is a significant predictor of label avoidance (Bathje & Pryor, 2011). We hypothesize that personal stigma and desired social distance predict label avoidance among college students.
Finally, previous work has provided support for a fully mediated model where personal stigma predicts label avoidance, label avoidance predicts attitudes towards help seeking, and attitudes towards help seeking predicts intentions to seek treatment among adults with mental illness (Vogel, Wade, & Hackler, 2007; Bathje & Pryor, 2011). In line with this previous work, we sought to evaluate a model of help seeking among college students accounting for all of these previously established relationships between variables. Our hypothesized model frames level of familiarity as a predictor of personal stigma and desired social distance, personal stigma and desired social distance as a predictors of label avoidance and attitudes towards help seeking, label avoidance as a predictor of attitudes towards help seeking, and attitudes towards help seeking as a predictor of intentions to seek treatment among a sample of college students.
Materials and Methods
Participants
Adults (age 18+) enrolled at a four-year private, technology-focused, research university offering undergraduate and graduate degrees in engineering, science, architecture, business, design, human sciences, applied technology, and law in metropolitan Chicago were recruited for this study. In total, 198 adults were solicited for the study and all 198 agreed to participate and completed all measures. Of these 198 participants, 153 participants reported that they had not previously received treatment or support for mental illness. We conducted our analyses using these 153 participants to avoid any bias that might be introduced by previous experience with mental health services. Table 1 provides participant demographics for these 153 participants. The average age of the sample was 21.10 years (standard deviation [SD] = 4.81). About 63% of the sample was male and 60.8% of participants were single. About thirty nine percent of participants were White/Caucasian, with 17.6% of the sample identifying as Hispanic/Latino. The racial and gender profile of study participants appears to be similar to that of the student body of the university. Demographics specific to college students and to mental illness were also collected from participants. There were fairly even numbers of Freshmen, Sophomores, Juniors, and Seniors who participated in the study. With regard to mental health status, 3.3% of the sample reported that they had been diagnosed with a mental illness.
Table 1.
Demographic Characteristics
| Total | |
|---|---|
| N | 153 |
| Age (SD) | 21.10 (4.81) |
| Gender (%) | |
| Male | 97 (63.40) |
| Female | 54 (35.30) |
| Transgender | 1 (0.70) |
| Prefer not to answer | 1 (0.70) |
| Race- N (%) | |
| American Indian/Alaskan Native | 3 (1.96) |
| Asian/Asian American | 57 (37.25) |
| African American/Black | 18 (11.76) |
| Pacific Islander | 1 (0.65) |
| White/Caucasian | 60 (39.22) |
| Arab/Middle Eastern | 2 (1.31) |
| Other | 30 (19.61) |
| Hispanic/Latino- N (%) | |
| Yes | 27 (17.60) |
| No | 126 (82.40) |
| Diagnosed Mental Illness- N (%) | |
| Yes | 5 (3.30) |
| No | 142 (92.80) |
| Unsure | 6 (3.90) |
| Current Relationship Status- N (%) | |
| Single | 93 (60.80) |
| In a relationship | 56 (36.60) |
| Married or domestic partnership | 2 (1.30) |
| Divorced | 1 (0.70) |
| Widowed | 1 (0.70) |
| Year in Degree Program- N (%) | |
| Freshman | 36 (23.50) |
| Sophomore | 43 (28.10) |
| Junior | 31 (20.30) |
| Senior | 27 (17.60) |
| 5th Year or Greater | 7 (4.60) |
| Master’s | 5 (3.30) |
| Doctoral | 1 (0.70) |
| Other | 3 (2.00) |
Procedures
Participants were recruited through advertisements in the university’s weekly newsletter, the psychology student subject pool, and from campus fraternities and sororities. Recruitment language framed this research broadly as a study of student attitudes towards mental illness. Participants interested in enrolling in the study either completed an online form to indicate their availability or directly emailed the research team. All participants provided informed consent to participate. Participants completed measures of level of familiarity with mental illness, personal stigma, desired social distance (a proxy of discrimination), label avoidance, attitudes towards treatment seeking, and intentions to seek treatment (from formal and informal sources). All surveys were completed via the Qualtrics online survey platform. Approval for this study was obtained from the Institutional Review Board of the University at which the study was conducted (Protocol #2014–002).
Measures
Measures included in this study corresponded with constructs in the path model shown in figure 1. Cronbach’s alphas for all scales for the present study are provided in Table 2.
Table 2.
Means, Standard Deviations, Zero-order Correlations, and Cronbach’s Alphas of Scales
| Measure | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | Cronbach’s Alpha of Scale |
|---|---|---|---|---|---|---|---|---|---|
| 1. Level of Familiaritya | 6.17 | 2.71 | 1 | −.25** | −.28** | .01 | .08 | .07 | N/A |
| 2. Personal Stigma (α=0.67) | 29.15 | 9.30 | 1 | .69** | .38** | .21* | −.16* | 0.63 | |
| 3. Social Distance (α=0.93) | 16.80 | 4.08 | 1 | .37** | −.20* | −.15 | 0.89 | ||
| 4. Label Avoidance (α=0.89) | 25.51 | 7.97 | 1 | −.57** | 0.90 | ||||
| 5. Attitudes Towards Help Seeking (α=0.62) | 26.26 | 4.36 | 1 | 0.75 | |||||
| 6. Intentions to Seek Treatment (α=0.87) | 52.23 | 17.68 | 0.88 |
Note: The Level of Familiarity scale is a checklist and therefore we do not have data on the reliability of the scale.
p<.05
p<.01
Level of familiarity
Familiarity with mental illness was assessed using the Level of Familiarity Scale (Corrigan, Edwards & Green, et al., 2001; Corrigan, Green, Lundin, Kubiak & Penn, 2001; Holmes, Corrigan & Williams et al., 1999). The Level of Contact Report lists 11 situations that vary in intimacy with persons with mental illness. These situations were adapted from other scales used in stigma research (Holmes, Corrigan & Williams et al., 1999; Link, 1987; Penn et al., 1994), and varied from least intimate contact (“I have never observed a person that I was aware had a severe mental illness”), to medium intimacy (“I have worked with a person who had a severe mental illness at my place of employment”), to high intimacy (“I have a severe mental illness”). The index for contact is the rank score of the most intimate contact situation indicated and ranges from 1 (least intimate contact) to 11 (most intimate contact). The Level of Familiarity Scale is a checklist and therefore there is no data on the reliability or validity of the scale.
Desired social distance
The Social Distance Scale was used as a proxy of discrimination for the purpose of this study. The SDS comprises seven items (e.g., “How would you feel about renting a room in your home to a person with severe mental illness?”). Participants rate items on a 0- to 3- point willingness scale (3 = definitely unwilling). The SDS has good internal consistency (α = 0.75) and validity (moderate to large positive correlation with perceived dangerousness; see Penn et al. [1994]) for a fuller discussion of the SDS psychometrics).
Personal stigma
Personal stigma was measured using the 9-item version of the Attribution Questionnaire (AQ-9). A vignette precedes the scale and was modified slightly for the college population for the purpose of this study (“Jamie is a 20-year old college student who has been hospitalized three times for mental illness.”). The AQ-9 includes nine questions answered on a nine point Likert scale (9 = very much). An example item is, “How dangerous would you feel Jamie is?” The AQ-9 has been found to have strong internal consistency (α = 0.73), test-retest reliability (r = 0.73), validity (moderate negative correlations with beliefs about self-determination, empowerment, and recovery among people with mental illness), and sensitivity to change (Corrigan, Powell & Michaels, 2014)
Label avoidance
A consequence of personal stigma is that people who might benefit from mental health services do not seek help to avoid being labeled with a mental illness. Vogel, Wade, and Haake (2006) refer to this as the self-stigma of seeking psychological help. While their definition of self-stigma differs from Corrigan’s conceptualization, the measure is consistent with how Corrigan defines the construct of label avoidance. Corrigan (2004) defines label avoidance as “avoid[ing] the stigma altogether by denying [one’s] group status [mental illness] and by avoiding the institutions that mark [one as mentally ill] (i.e. mental health care).” The Self-Stigma of Seeking Help Scale (SSOSH) was used in this study to assess label avoidance. The SSOSH is a 10-item scale with items such as “I would feel inadequate if I went to a therapist for psychological help.” Items are rated on a five-point Likert scale (5= strongly agree). The SSOSH has been shown to have a unidimensional factor structure and demonstrated validity (strong negative correlation with attitudes towards help seeking, and moderate to strong positive correlation with the social stigma of seeking help) and internal consistency (α = 0.91; Vogel, Wade & Haake, 2006).
Attitudes towards treatment seeking
The 10-item version of the Attitudes Towards Seeking Professional Psychological Help Scale (ATSPPHS) was used to assess participants’ attitudes towards seeking professional psychological help. An example item is, “Considering the time and expense involved in psychotherapy, it would have doubtful value for a person like me.” Items are rated on a four-point Likert scale (4 = agree). The scale has a demonstrated strong internal consistency (α = 0.84), test-retest reliability (r = 0.84), and validity (Fischer & Farina, 1995).
Intentions to seek treatment
The General Help-Seeking Questionnaire (GHSQ) assesses future help-seeking behavioral intentions over the next four weeks. This measure was used in addition to the ATSPPHS in order to assess intentions to seek help, a precursor of behavior. The instructions for this instrument read, “Below is a list of people who you might seek help from if you were experiencing a personal or emotional problem. Please circle the number that shows how likely it is that you would seek help from each of these people for a personal or emotional problem during the next 4 weeks.” Future help-seeking intentions are measured by listing a number of potential help sources and asking participants to indicate how likely it is that they would seek help from the source for a specified problem on a seven-point scale (7= extremely likely). The measure was designed so that specific sources of help, the future time-period specified, and the type of problem can be modified to be appropriate to the particular research objectives. For example, one of the sources of help included for the purpose of this study with college students was the Resident Assistant. Help-seeking intentions can be reported as a total scale score or as three sub-scales: level of intention for seeking informal help; level of intention for seeking formal help; and level of intention to seek help from no-one. For the purpose of this study we elected to use the GHSQ total scale score. The GHSQ has demonstrated good internal consistency (α = 0.85), test-retest reliability (r=.92), and validity (modest positive correlation with actual help-seeking behaviors [r=.20]) in previous studies (Rickwood, Deane, Wilson & Ciarrochi, 2005).
Results
Preliminary Analysis
Variables included in the model were examined for missing data and no cases were found (N=198). Missing data were avoided through the use of the request response function within the Qualtrics survey platform. This function reminds participants of any unanswered questions before proceeding to the next page of the survey. Participants have the option to proceed without answering questions or to respond to unanswered questions before proceeding. Each variable was examined for presence of outliers (Tabachnick & Fidell, 2001). One univariate outlier was found and dropped from subsequent analyses. Examination for multivariate outliers was conducted using the Mahalanobis distances among the variables (Tabachnick & Fidell, 2001), resulting in detection of two multivariate outliers at p < .001 (Mahalanobis distance > 34.53) and these two cases were dropped from subsequent analyses. Thus, after excluding any participants who reported previous use of mental health treatment or support, remaining analyses were conducted with a sample size of 153. Table 2 shows means, standard deviations, zero-order correlations, and Cronbach’s alphas for overall scales. All constructs correlated as expected.
Path analysis with maximum likelihood estimation in the AMOS 25 program was used to examine model fit. Five indices were used to assess goodness of fit of the resulting model. These included chi-square (χ2), comparative fit index (CFI), non-normed fit index/Tucker–Lewis index (NNFI/TLI), root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). Of these indices, only chi-square provides evidence of statistical significance. Unlike most tests of statistical significance associated with chi-square, however, support for a proposed model is demonstrated with a nonsignificant value. Specifically, a nonsignificant value (p > .05) for a particular model indicates that the observed and reproduced variance–covariance matrices are not significantly different from one another. The remaining indices are interpreted relative to common “rules of thumb” (Kline, 2015). For the present study, these rules of thumb were CFI and NNFI/TLI (.95 or greater), RMSEA (.05 or less), and SRMR (.08 or less). Because the maximum likelihood procedures used to test the hypothesized model assumes normality, we examined the multivariate normality of the observed variables. Specifically, we focused on values of multivariate kurtosis as multivariate kurtotic data are seen to be particularly problematic for SEM (Byrne, 2010; Raykov & Marcoulides, 2010). West, Finch, and Curran (1995) consider rescaled β2 values equal to or greater than 7 to indicate early departure from normality. Using this value as a guide, our data did not violate the assumption of multivariate normality.
Model Testing
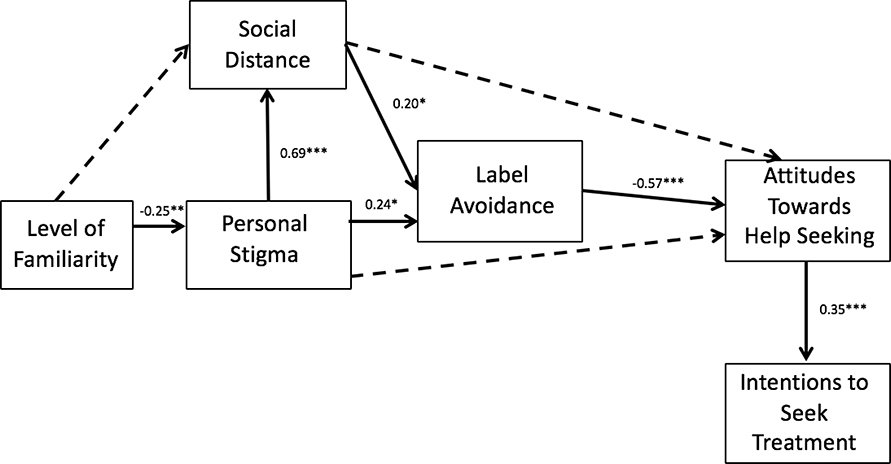
Upon running the hypothesized model (in figure 1), the path between personal stigma and attitudes towards help seeking was not found to be significant and so this path was dropped from the model. Likewise, the path between social distance and attitudes towards help seeking was not found to be significant and so this path was dropped from the model. The path between level of familiarity and social distance was also non-significant and was therefore dropped. Having made these modifications to the hypothesized model, we moved from a confirmatory to exploratory analysis (Schreiber, Nora, Stage, Barlow, & King, 2006) of Model 2 (see figure 2). The respecified model with non-significant paths from our hypothesized model constrained to zero, resulted in a non-significant chi-square. The chi-square difference test was then used to compare these two nested models to determine which model best fit our data. A nonsignificant chi-square difference, Δχ2 (3) = 3.47, p = .32, indicated no differences between these two models. On the basis of the principle of parsimony, the respecified model (Model 2) was selected as the best model (Raykov & Marcoulides, 1999). Corresponding fit indices for Model 2 showed good fit to the data, χ2 (9) = 12.64, p = .18, CFI = .98, NNFI = .95, TLI= .97, SRMR = .05, RMSEA = .05. The standardized path coefficients for the model can be found in figure 2. The direct effects for this model indicate that level of familiarity predicts personal stigma. Personal stigma predicts social distance and social distance predicts label avoidance, as does personal stigma. Label avoidance predicts attitudes towards treatment seeking, which in turn predicts intentions to seek treatment (see Figure 2).
Figure 2.
Model 2 of the relationship between level of familiarity, personal stigma, social distance, label avoidance, attitudes towards treatment seeking, and intentions to seek treatment.
Note. All path coefficients are standardized values.
*p < .05. ** p < .01. *** p<.001
Discussion
Using path analysis, the current study evaluated an exploratory model of the relationship between level of familiarity, personal stigma, desired social distance, label avoidance, attitudes towards treatment seeking, and intentions to seek treatment among college students. Results indicate that the respecified, exploratory model is supported by the data. Greater familiarity with mental illness predicts lower levels of personal stigma. Personal stigma positively predicts desired social distance and label avoidance. Greater desire for social distance from individuals with mental illness positively predicts label avoidance. Label avoidance negatively predicts attitudes towards treatment seeking, and attitudes towards treatment seeking in turn positively predict intentions to seek treatment.
The present findings build upon other work in the area of college mental health and treatment engagement, which suggests that personal stigma (Eisenberg, Downs &Golberstein, et al., 2009), and label avoidance (Nam, 2013; Bathje & Pryor, 2011) may be associated with college student attitudes towards seeking help for mental health concerns. This model adds to the existing literature by examining the contribution of level of familiarity and social distance to models of treatment seeking for mental health concerns among college students.
These findings have several implications for practice. Most importantly, the model suggests that increasing one’s level of familiarity with mental illness should positively impact stigma and social distance. This is in line with previous research with the general adult population suggesting that contact, or face-to-face interactions with individuals with mental illness, is the most effective form of stigma change (Corrigan, Morris, Michaels, Rafacz & Rüsch, 2012). In the academic setting this can be done using a variety of mechanisms (e.g. coursework, bringing in guest speakers with lived experience, field learning experiences to mental health service organizations etc.) Other work examining the impact of contact- and education-based anti-stigma interventions among college students also supports the notion that increasing level of familiarity should decrease stigma and social distance (Kosyluk et al., 2016). In their randomized controlled trial of contact and education-based stigma change programs in the college setting, Kosyluk and colleagues (2016) found both contact and education-based interventions were effective for reducing stigma and social distance and improving attitudes towards help seeking and intentions to seek help from formal sources of support compared with a control condition. Such interventions can be delivered in a variety of venues with the intention to reduce stigma and improve treatment seeking. One example of a national student organization that has been successful at reducing stigma using peer-to-peer contact is Active Minds (McKinney, 2009; Sontag-Padilla et al., 2018). Supporting such organizations on college campuses may positively impact stigma and help seeking.
The model also suggests label avoidance, attitudes towards treatment seeking, and intentions to seek treatment might be augmented through interventions aimed at increasing college students’ levels of familiarity, or intimate contact, with individuals with mental illness. An example of such an intervention is This Is My Brave (www.thisismybrave.org), which facilitates contact through storytelling surrounding mental illness and recovery with the goal of encouraging treatment engagement. This intervention has been demonstrated effective for improving willingness to seek treatment (Kosyluk et al., 2018; Kosyluk et al., in review). Interventions such as This Is My Brave, where individuals with lived experience with mental illness disclose their stories of challenges with mental illness and recovery, are in line with the disclosure-based approach to stigma reduction put forth by Corrigan, Kosyluk, and Rüsch (2013). Other work suggests programs meant to assist people with mental illness grapple with disclosure decisions and learn to strategically tell their stories of lived experience with mental illness may be helpful in reducing the negative impact of stigma and improving help-seeking, specifically among young people (Mulfinger et al., 2018). Corrigan and colleagues (2016) conducted a study to determine whether such programs would be desirable to college students with mental health concerns, concluding that some college students may find programs aiding in disclosure useful in assisting them to achieve their desire to disclose their mental illness. The model tested here suggests that there is merit to considering the use of disclosure-based programs with college students with mental illness.
Limitations
One limitation of this study is the fact that intentions to seek treatment, as opposed to actual treatment seeking, were examined as the ultimate outcome of interest. Future studies should consider research designs that capture actual treatment seeking to see if the model continues to hold. There may be additional limitations related to the operationalization of intentions to seek treatment. We used the General Help Seeking Questionnaire to approximate this construct. This measure may actually capture other information such as level of distress, as opposed to or in addition to intentions to seek treatment. Future research may consider alternative ways to operationalize intentions to seek treatment.
This model was evaluated using cross-sectional data. Therefore, we are limited in the causal statements we can make about the relationships between variables and should interpret these findings with caution. Future work should strive to adopt longitudinal designs allowing the testing of causality. After constraining non-significant paths in our originally hypothesized model to zero, we evaluated a respecified model and moved from confirmatory to exploratory analysis. Though the exploratory model still makes theoretical sense, these results nonetheless need to be interpreted with caution and future research is called for to confirm our supported exploratory model.
An additional limitation of the study concerns the language used in recruitment materials. It is possible that by explicitly using the terms “mental illness” and “attitudes” we may have obtained a sample who already held more positive attitudes towards mental illness. Such range restriction in our stigma-related variables may contribute to weaker relationships between variables. Despite this potential limitation we did find support for a model of the relationship between level of familiarity, stigma-related constructs, and help seeking.
As mentioned earlier, some research suggests intentions to seek treatment may be improving over time (Oswalt, Lederer, Chestnut-Steich, Day, Halbritter, & Ortiz, 2019). Such improvements may be attributable to stigma reduction work taking place on college campuses. Increasing rates of treatment seeking for mental health concerns may present new challenges for engaging students in mental health care. As college counseling center services face greater demand, longer wait times may serve as a greater barrier to care. Future research needs to consider issues of access in combination with stigma as barriers to college student mental health treatment.
Additional future research directions include investigating the roles other relevant variables (e.g. race and ethnicity) may play in this model. Through comparing the model across different populations, we may gain better understanding of differences in help seeking behaviors and factors influencing help seeking across cultures. Unfortunately, the current sample was not large enough to allow for adequate examination of the influence of such factors on the model’s fit. Finally, future research may want to examine relevance of the model for other types of disabilities, particularly other concealable disabilities.
Acknowledgements
This study was funded by grant # P20MH085981 from the National Institute of Mental Health.
Declaration of Interest: This study was supported by grant P20 MH085981 from the National Institute of Mental Health. There are no known conflicts of interest to report.
Declaration of Interest: This work was supported by grant P20 MH085981 from the National Institute of Mental Health. There are no known conflicts of interest to report.
Footnotes
Disclosure statement: No financial interest or benefit has arisen from the direct application of this research.
Data availability statement: The data that support the findings of this study are available from the corresponding author, KK, upon reasonable request.
Contributor Information
Kristin A Kosyluk, University of South Florida, Department of Mental Health Law and Policy, 13301 Bruce B. Downs Blvd, MHC 2735, Tampa, Florida 33612.
Kyaien Conner, University of South Florida, Department of Mental Health Law and Policy, 13301 Bruce B. Downs Blvd, Tampa, Florida 33612.
Maya Al-Khouja, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
Andrea Bink, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
Blythe Buchholz, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
Sarah Ellefson, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
Konadu Fokuo, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
David Goldberg, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
Dana Kraus, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
Adeline Leon, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
Karina Powell, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
Annie Schmidt, University of North Carolina
Patrick Michaels, Louis Stokes Cleveland Department of Veterans Affairs Medical Center
Patrick W. Corrigan, Illinois Institute of Technology, 3424 S. State Street, Chicago, Illinois 60616
References
- Anagnostopoulos F, & Hantzi A (2011). Familiarity with and social distance from people with mental illness: Testing the mediating effects of prejudiced attitudes. Journal of Community & Applied Social Psychology,21(5), 451–460. DOI: 10.1002/casp.1082 [DOI] [Google Scholar]
- Arria AM, Caldeira KM, Vincent KB, Winick ER, Baron RA, & O’Grady KE (2013). Discontinuous college enrollment: Associations with substance use and mental health. Psychiatric Services, 64(2): 165–172. DOI: 10.1176/appi.ps.201200106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, … & Murray E (2018). WHO World Mental Health Surveys International College Student Project: prevalence and distribution of mental disorders. Journal of abnormal psychology, 127(7), 623–638.. DOI: 10.1037/abn0000362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bathje GJ, & Pryor JB (2011). The relationships of public and self-stigma to seeking mental health services. Journal of Mental Health Counseling, 33(2), 161. DOI: 10.17744/mehc.33.2.g6320392741604l1 [DOI] [Google Scholar]
- Byrne BM (2013). Structural equation modeling with AMOS: Basic concepts, applications, and programming. Routledge. [Google Scholar]
- Corrigan P (2004). How stigma interferes with mental health care. American psychologist, 59(7), 614–625. DOI: 10.1037/0003-066X.59.7.614 [DOI] [PubMed] [Google Scholar]
- Corrigan PW (2000). Mental health stigma as social attribution: Implications for research methods and attitude change. Clinical Psychology: Science and Practice, 7(1), 48–67. DOI: 10.1093/clipsy.7.1.48 [DOI] [Google Scholar]
- Corrigan PW, Druss BG, & Perlick DA (2014). The impact of mental illness stigma on seeking and participating in mental health care. Psychological Science in the Public Interest, 15(2), 37–70. DOI: 10.1177/1529100614531398 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Edwards AB, Green A, Diwan SL, & Penn DL (2001). Prejudice, social distance, and familiarity with mental illness. Schizophrenia Bulletin, 27(2), 219. DOI: 10.1093/oxfordjournals.schbul.a006868 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Green A, Lundin R, Kubiak MA, & Penn DL (2001). Familiarity with and social distance from people who have serious mental illness. Psychiatric services, 52: 953–8. DOI: 10.1176/appi.ps.52.7.953 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, & Kosyluk K (2014). Mental Illness Stigma: Types, Constructs, and Vehicles for Change. In Corrigan. (Ed.), Stigma of Disease and Disability: Understanding Causes and Overcoming Injustices. Washington, DC: American Psychological Association (APA). [Google Scholar]
- Corrigan PW, Kosyluk KA, Markowitz F, Brown RL, Conlon B, Rees J, … & Al-Khouja M (2016). Mental illness stigma and disclosure in college students. Journal of Mental Health, 25(3), 224–230. DOI: 10.3109/09638237.2015.1101056 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Kosyluk KA, & Rüsch N (2013). Reducing self-stigma by coming out proud. American journal of public health, 103(5), 794–800. DOI: 10.2105/AJPH.2012.301037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Larson JE, & Rüsch N (2009). Self‐stigma and the “why try” effect: impact on life goals and evidence‐based practices. World Psychiatry, 8(2), 75–81. DOI: 10.1002/j.2051-5545.2009.tb00218.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan P, Markowitz FE, Watson A, Rowan D, & Kubiak MA (2003). An attribution model of public discrimination towards persons with mental illness. Journal of health and Social Behavior, 162–179. DOI: 10.2307/1519806 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, & Rüsch N (2012). Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatric services, 63(10), 963–973. DOI: 10.1176/appi.ps.201100529 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Powell KJ, & Michaels PJ (2014). Brief battery for measurement of stigmatizing versus affirming attitudes about mental illness. Psychiatry research, 215(2), 466–470. DOI: 10.1016/j.psychres.2013.12.006 [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Downs MF, Golberstein E, & Zivin K (2009). Stigma and help seeking for mental health among college students. Medical Care Research and Review, 66(5), 522–541. DOI: 10.1177/1077558709335173 [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Golberstein E, & Hunt JB (2009). Mental health and academic success in college. The BE Journal of Economic Analysis & Policy, 9(1), 1–35. DOI: 10.2202/1935-1682.2191 [DOI] [Google Scholar]
- Eisenberg D, Hunt J, Speer N, & Zivin K (2011). Mental health service utilization among college students in the United States. The Journal of nervous and mental disease, 199(5), 301–308. [DOI] [PubMed] [Google Scholar]
- Ettner SL, Frank RG, & Kessler RC (1997). The impact of psychiatric disorders on labor market outcomes. Industrial & Labor Relations Review, 51(1), 64–81. DOI: 10.1177/001979399705100105 [DOI] [Google Scholar]
- Fischer EH, & Farina A (1995). Attitudes toward seeking professional psychological help: A shortened form and considerations for research. Journal of College Student Development, 36(4), 368–373. [Google Scholar]
- Holmes EP, Corrigan PW, Williams P, Canar J, & Kubiak MA (1999). Changing attitudes about schizophrenia. Schizophrenia Bulletin,25(3), 447–456. DOI: 10.1093/oxfordjournals.schbul.a033392 [DOI] [PubMed] [Google Scholar]
- Hunt J, Eisenberg D, & Kilbourne AM (2010). Consequences of receipt of a psychiatric diagnosis for completion of college. Psychiatric Services, 61, 399–404. DOI: 10.1176/ps.2010.61.4.399 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Foster CL, Saunders WB, Stang PE, & Walters EE (1997). Social consequences of psychiatric disorders, II: Teenage parenthood. American Journal of Psychiatry, 154(10), 1405–1411. DOI: 10.1176/ajp.154.10.1405 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Foster CL, Saunders WB, & Stang PE (1995). Social consequences of psychiatric disorders, I: Educational attainment. American Journal of Psychiatry, 152(7), 1026–1032. DOI: 10.1176/ajp.152.7.1026 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Walters EE, & Forthofer MS (1998). The social consequences of psychiatric disorders, III: probability of marital stability. American Journal of Psychiatry, 155, 1092–1096. DOI: 10.1176/ajp.155.8.1092 [DOI] [PubMed] [Google Scholar]
- Kline RB (2015). Principles and practice of structural equation modeling. Guilford publications. [Google Scholar]
- Kosyluk KA, Al-Khouja M, Bink A, Buchholz B, Ellefson S, Fokuo JK, … Corrigan PW (2016). Challenging the Stigma of Mental Illness Among College Students: A Randomized Controlled Trial. Journal of Adolescent Health, 59(60), 325–331. DOI: 10.1016/j.jadohealth.2016.05.005 [DOI] [PubMed] [Google Scholar]
- Kosyluk K, Marshall J, Macias DR, Andrus D, Guerra D, Robinson M, … & Chapman S (2018). Examining the impact of this is my brave on mental illness stigma and willingness to seek help: A pilot study. Community mental health journal, 54(3), 276–281. DOI: 10.1007/s10597-018-0238-8 [DOI] [PubMed] [Google Scholar]
- Kosyluk KA, Marshall J, Macias DR, Macias S, Conner KO, Beekman BM, Her J (In Review). Challenging the Stigma of Mental Illness through Creative Storytelling: A Randomized Controlled Trial of This Is My Brave. Community Mental Health Journal. [DOI] [PubMed] [Google Scholar]
- Link BG (1987). Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review, 52, 96–112. DOI: 10.2307/2095395 [DOI] [Google Scholar]
- Link BG, Phelan JC, Bresnahan M, Stueve A, & Pescosolido BA (1999). Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American journal of public health, 89(9), 1328–1333. DOI: 10.2105/AJPH.89.9.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney KG (2009). Initial evaluation of active minds: A student organization dedicated to reducing the stigma of mental illness. Journal of college student psychotherapy, 23(4), 281–301. [Google Scholar]
- Mulfinger N, Müller S, Böge I, Sakar V, Corrigan PW, Evans‐Lacko S, … & Ruckes C (2018). Honest, Open, Proud for adolescents with mental illness: pilot randomized controlled trial. Journal of Child Psychology and Psychiatry, 59(6), 684–691. DOI: 10.1111/jcpp.12853 [DOI] [PubMed] [Google Scholar]
- Nam SK, Choi SI, Lee JH, Lee MK, Kim AR, & Lee SM (2013). Psychological factors in college students’ attitudes toward seeking professional psychological help: A meta-analysis. Professional Psychology: Research and Practice, 44(1), 37. DOI: 10.1037/a0029562 [DOI] [Google Scholar]
- Oswalt SB, Lederer AM, Chestnut-Steich K, Day C, Halbritter A, & Ortiz D (2019). Trends in college students’ mental health diagnoses and utilization of services, 2009–2015. Journal of American College Health, 1–11. [DOI] [PubMed] [Google Scholar]
- Penn DL, Guynan K, Daily T, Spaulding WD, Garbin CP, & Sullivan M (1994). Dispelling the stigma of schizophrenia: what sort of information is best? Schizophrenia bulletin, 20(3), 567–578. DOI: 10.1093/schbul/20.3.567 [DOI] [PubMed] [Google Scholar]
- Raykov T, & Marcoulides GA (1999). On desirability of parsimony in structural equation model selection. Structural Equation Modeling: A Multidisciplinary Journal, 6(3), 292–300. DOI: 10.1080/10705519909540135 [DOI] [Google Scholar]
- Raykov T, & Marcoulides GA (2010). Group comparisons in the presence of missing data using latent variable modeling techniques. Structural equation modeling, 17(1), 134–149. DOI: 10.1080/10705510903439136 [DOI] [Google Scholar]
- Rickwood D, Deane FP, Wilson CJ, & Ciarrochi J (2005). Young people’s help-seeking for mental health problems. Australian e-journal for the Advancement of Mental health, 4(3), 218–251. DOI: 10.5172/jamh.4.3.218 [DOI] [Google Scholar]
- Rüsch N, Angermeyer MC, & Corrigan PW (2005). Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. European psychiatry, 20(8), 529–539. DOI: 10.1016/j.eurpsy.2005.04.004 [DOI] [PubMed] [Google Scholar]
- Schreiber JB, Nora A, Stage FK, Barlow EA, & King J (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of educational research, 99(6), 323–338. [Google Scholar]
- Sontag-Padilla L, Dunbar MS, Ye F, Kase C, Fein R, Abelson S, … & Stein BD (2018). Strengthening college students’ mental health knowledge, awareness, and helping behaviors: the impact of Active Minds, a peer mental health organization. Journal of the American Academy of Child & Adolescent Psychiatry, 57(7), 500–507. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS, & Osterlind SJ (2001). Using multivariate statistics.
- Vogel DL, Wade NG, & Hackler AH (2007). Perceived public stigma and the willingness to seek counseling: The mediating roles of self-stigma and attitudes toward counseling. Journal of Counseling Psychology, 54(1), 40–50. DOI: 10.1037/0022-0167.54.1.40 [DOI] [Google Scholar]
- Vogel DL, Wade NG, & Haake S (2006). Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology, 53(3), 325–337. DOI: 10.1037/0022-0167.53.3.325 [DOI] [Google Scholar]
- Weitzman ER (2004). Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. The Journal of nervous and mental disease, 192(4), 269–277. DOI: 10.1097/01.nmd.0000120885.17362.94 [DOI] [PubMed] [Google Scholar]
- West SG, Finch JF, & Curran PJ (1995). Structural equation models with nonnormal variables. Structural equation modeling: Concepts, issues, and applications, 56–75. [Google Scholar]