Abstract
More than 8 billion tonnes of plastic were produced between 1950 and 2015, that is 1 tonne for every man, woman and child on our planet. Global plastic production has been growing exponentially with an annual growth rate of 8.4% since 1950, equating to approximately 380 million tonnes per annum. A further 50 kg of plastic is now being produced for each person every year with production continuing to accelerate. Here, we discuss the human and planetary health hazards of all that plastic. We consider each step in the journey of these complex and pervasive industrial materials: from their synthesis predominantly from fossil fuel feedstocks, through an often‐brief consumer use as plastic products, and onto waste streams as fuel, permanent landfill or as unmanaged waste in our environment, food, air and bodies.
Keywords: environment, environmental pollution, public health, population health, plastics, polymers
Key Points.
Global plastic production has been growing and has diverse and concerning effects on human and planetary health.
As consumers, we can ask where the plastic comes from, what is in it, and where it goes.
As health professionals, we can educate ourselves about the harms of plastic, and advocate for recyclable, safer plastic to rescue the health of future generations and of the planet.
Hazards of Plastic Production
What are plastics?
Consumer plastics are highly complex industrial materials, incorporating a polymer matrix mixed with a diverse array of additives and processing agents, plus impurities, by‐products, breakdown products and contaminants. 1 , 2 More than 10 500 monomers, additives and processing agents are registered for production internationally, with nearly 40% produced at high volumes 2 at a total of 25 million tonnes annually. 1 Additives comprise approximately 7% of plastic products by weight, 1 and include plasticisers, flame retardants, antioxidants, UV stabilisers and pigments that are mixed with the polymer to produce specific products, 1 , 2 , 3 or as fillers. 1 Additives are not typically bonded to the polymer and leach out over time and with use. 3 , 4 , 5
Raw materials
While plastic waste is a visible environmental problem, there is less consumer awareness of the significant environmental impact of plastic production. 6 , 7 , 8 Plastic polymers and additives are overwhelmingly synthesised from ‘virgin’ petrochemicals. Plastic production starts with the extraction, transport and refinement of crude oil, with environmental damage at the site of extraction, risk of crude‐oil spillage during extraction and transportation, contamination of groundwater due to fracking, and air pollution from flaring (burning off excess gasses at extraction), transportation emissions and refinement 9 , 10 (Fig. 1).
Fig. 1.
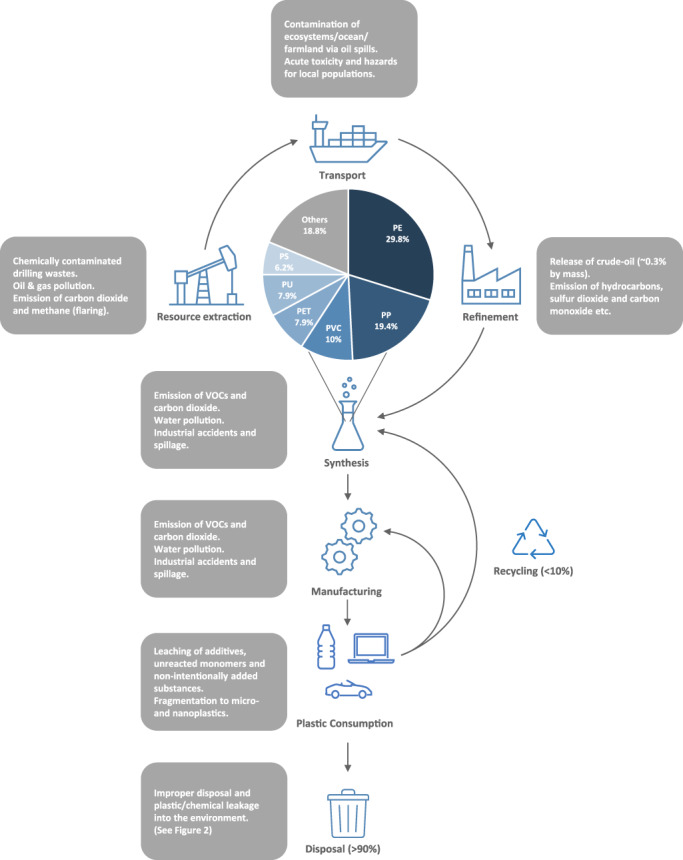
Plastic supply chain and potential hazards for planetary and human health and share of main polymers for plastic production. PE, polyethylene; PET, polyethylene terephthalate; PP, polypropylene; PS, polystyrene; PU, polyurethanes; PVC, polyvinyl chloride; VOCs = volatile organic compounds.
Manufacture
Refined petrochemicals such as ethylene, propylene or benzene are used to synthesise plastic monomers, which are bonded together as polymers. Similar to refinement, this is energy‐intensive and produces significant amounts of carbon dioxide. 9 Additionally, the vast majority of these processes use hazardous chemicals, including the monomers themselves (such as propylene, styrene, vinyl chloride and butadiene), intermediates in monomer production (such as benzene and toluene), processing agents and by‐products. 9 Additives follow a similar process of chemical synthesis through multiple intermediates. These pose occupational as well as environmental hazards, through emission of gases/vapours, contamination of waterways or soils by chemical waste mismanagement, or through industrial accidents 9 (Figs 1, 2).
Fig. 2.
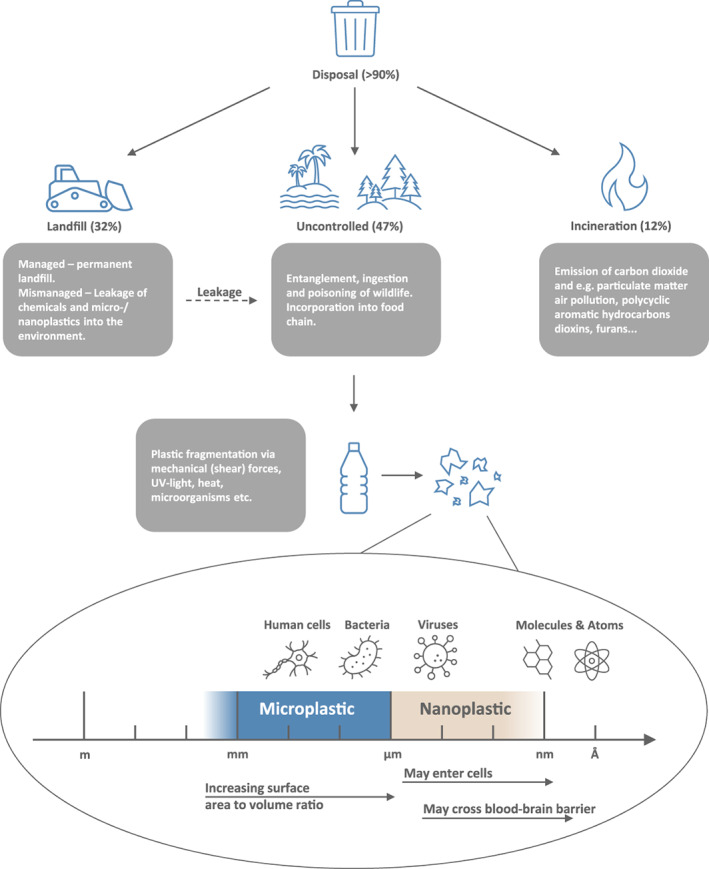
Potential hazards for planetary and human health from different forms of plastic disposal (top) and fragmentation of plastic products into micro‐ and nanoplastics (bottom).
For example, antimony is used as a catalyst during monomer synthesis and remains in the process stream during polymerisation and manufacturing of, for example, drinking bottles and textiles. Insufficient wastewater treatment or leaching from plastic products leads to antinomy pollution of rivers near polyethylene terephthalate production sites which threatens local drinking water supplies. 11
Human health implications of plastic production
Environmental hazards of plastic production affect human health directly and indirectly (Fig. 3). The contribution of plastics production to both global carbon emissions and particulate air pollution is of growing concern. Throughout the supply chain, plastic contributes approximately 4% of total global greenhouse emissions. 12 Urgent changes to global emissions are critical to avoid a disastrous 1.5°C increase in anthropogenic warming. 13 The human health effects of climate change alone are profound, and already being felt. 14 Outdoor fine particulate matter (PM2.5) – such as produced during flaring, from transportation diesel and in crude oil refinement – is the fifth leading death risk factor world‐wide 15 and underscores the risk of such a large‐scale industry dependent on petrochemical feedstock.
Fig. 3.
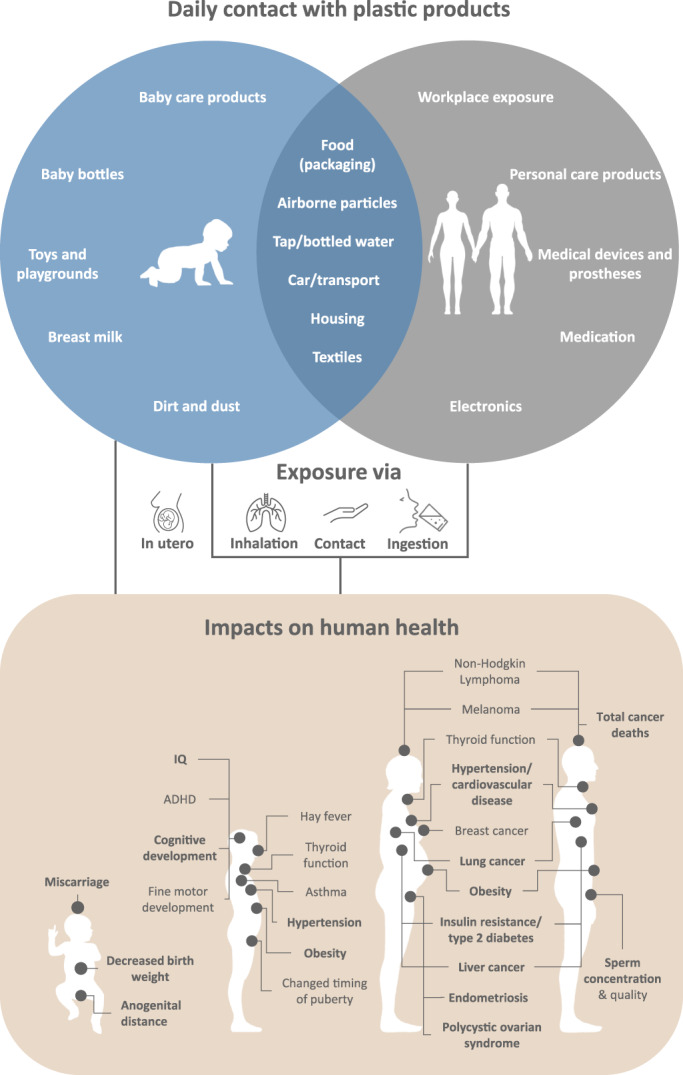
Common routes of plastic exposure for children and adults (top) and impacts on human health based on systematic review with meta‐analysis (bottom). See text for references.
Hazards of Plastic Use
The next step in the plastic supply chain is the use of manufactured plastic products, the largest markets being packaging (38%), building and construction (16%) and textiles (15%), 1 but with diverse applications across almost every aspect of our lives (Fig. 3). The volumes at which plastics are produced reflect a growing dependence on these products including household goods, food processing and packaging, personal care products and medical applications, both external and internal. In each application, including food packaging, 4 we are exposed to a complex mixture of chemicals. With use, degradation products are also formed and plastic itself fragments to micro‐ and nanoplastics (Fig. 3).
The primary hazard during direct consumer exposure to plastic is chemicals that leach out from the plastic, 3 , 4 , 5 and which may enter food and drink during processing or from packaging. Some of the smallest and most volatile chemicals can also be absorbed transdermally or dispersed into the air and inhaled (in each case bypassing first‐pass metabolism). Young children have additional exposure through oral exploratory behaviour and/or non‐nutritional ingestion, including their toys and accumulated chemicals in household dust and soil.
For the vast majority of plastic additives, we know little about the degree of human exposure or possible human health impacts. There are limitations of in vitro and animal studies to evaluate effects of low‐dose, long‐term human exposure, and there is no systematic process for post‐marketing surveillance, as there is for pharmaceuticals or pesticides. This issue is compounded for non‐intentionally added substances where identity is unknown or not disclosed. 4 Indeed, of approximately 10 500 known plastic monomers, chemical additives and processing aids, approximately 4100 lack any reported hazard classifications. 2 Of the 6436 chemicals for which hazard data are available, 3950 have been identified as substances of low concern; of the remaining 2486 chemicals, 1232 are of medium concern and 1254 are of high concern. 2
Knowledge of direct human health effects is limited to a small subset where techniques have been independently developed to measure the chemical or its metabolites in human bio‐samples, and observational studies have then evaluated the association between individual exposure and health outcomes. Examples include certain bisphenol monomers, phthalate plasticisers, organohalide flame retardants and polyfluoroalkyl processing aids. The key findings evaluated by meta‐analysis of multiple individual study populations are summarised in Figure 3.
Bisphenols
Bisphenols are used to make polycarbonates and epoxy resins, including plastic food and beverage containers or their linings. Bisphenol A (BPA) has attracted the most research with adverse associations including: anogenital distance in newborn girls, 16 hypertension, 17 cardiovascular disease, 18 polycystic ovary syndrome, 19 insulin resistance, 20 type 2 diabetes, 17 , 21 , 22 obesity and increased waist circumference. 17 , 21 , 22 There are no global treaties relating to BPA or other bisphenols; regulations vary from country to country. Driven by consumer pressure, industry has reduced BPA use but BPA has largely been replaced by other bisphenols with very similar biological activity in vitro and in animal studies. 23
Phthalates (ortho‐phthalate diesters)
Phthalates are the main plasticisers used to increase the flexibility of plastics. Exposure is usually measured as a metabolite in urine. Adverse associations include: miscarriage, 24 anogenital distance in newborn boys 25 and sperm concentration. 26 Additional concerns for harm, but with differing findings for different phthalates, include birthweight in newborns, 27 asthma, 28 , 29 psychomotor development, 30 cognitive development and IQ, 30 precocious puberty in girls, 31 , 32 increased blood pressure in children, 27 insulin resistance, 20 , 33 type 2 diabetes, 20 thyroid function, 34 obesity and waist circumference, 21 , 27 endometriosis 35 and additional sperm quality measures. 26 There are no global treaties relating to phthalates.
Halogenated flame retardants
Halogenated flame retardants used in plastics include polychlorinated biphenyls (PCBs) and polybrominated diphenyl ethers (PBDEs). Adverse health effects associated with PCBs include: reduced birthweight, 36 , 37 death from certain cancers, 38 , 39 cardiovascular disease, 18 type 2 diabetes 20 , 40 and endometriosis. 41 , 42 Adverse health effects associated with PBDEs include: reduced birthweight, 43 cognitive development and IQ. 44 Additional concerns include: insulin resistance, 20 infant bronchitis, 45 several cancers 38 , 39 , 42 , 46 , 47 , 48 , 49 for PCBs and thyroid function 17 for PBDEs. PCBs and certain PBDEs are regulated under the Stockholm Convention as Persistent Organic Pollutants (POPs), but replacements include other brominated flame retardants, some with strong structural similarities.
Per‐ and polyfluoroalkyl substances
Per‐ and polyfluoroalkyl substances (PFAS) are used in firefighting foams, as protective coatings for food packaging, textiles and furniture, but also in the manufacture of fluoropolymer plastics for non‐stick cookware and waterproof fabrics. There are more than 9000 PFAS, 50 but only a handful have been studied for human exposure and health effects. Adverse health effects associated with PFAS include: decreased birthweight and length in newborns 51 , 52 , 53 and obesity in children. 54 Additional concerns include: neurodevelopment, 55 allergic rhinitis in children 56 and thyroid function. 57 Some PFAS are regulated under the Stockholm Convention as POPs, but otherwise regulation varies from country to country.
Other monomers, additives, processing aids and non‐intentionally added substances
The small number of chemicals studied across the above categories only captures a tiny fraction of over 10 500 chemicals in plastics, 2 leaving considerable uncertainty regarding health effects of other high‐volume production additives. ‘Non‐targeted’ approaches to identify other chemicals leaching from consumer products, 58 , 59 in food, 60 household environmental samples, 61 or indeed in human biospecimens, 62 , 63 are starting to identify a much more extensive range of plastic chemical exposure, including organophosphate flame retardants, UV filters and stabilisers and non‐phthalate plasticisers, 58 , 59 , 60 , 61 , 62 , 63 for which human health effects are unknown.
Hazards of Plastic Waste
Waste streams and recycling
Global plastic waste management has lagged behind waste production with only approximately 9% being recycled. 1 Traditional mechanical recycling methods largely yield down‐cycled plastic of inferior quality, more limited application and reduced recycling options. 64 Emerging chemical recycling technologies provide potential recycling of the same plastic, 65 , 66 but need further development to address high cost and energy requirements. A greater proportion (12%) is incinerated in purpose‐built facilities. This provides an option for lower grade non‐recyclable plastic, but releases the embedded carbon as carbon dioxide. In the absence of controlled incineration, open burns are common, releasing toxic airborne pollutants alongside embedded carbon. 67 The vast majority (79%) of plastic waste is discarded. 1 Even in the best‐case scenario, processing and landfill results in accumulation because anaerobic conditions limit degradation. 68 Of all plastics produced annually, nearly half is mismanaged, 69 with littering or leaking from landfills resulting in pollution of land, freshwater waterways and the ocean. 70
Macro, micro‐ and nanoplastic waste
The visible components of plastic waste are macroplastics including plastic products that retain sufficient integrity to be recognisable and initial fragmentation products. Progressive weathering and fragmentation lead to ever smaller fragments, namely microplastics (<5 mm) 71 and nanoplastics (typically defined either as <1 μm or <100 nm). 5 , 71
Macroplastics present certain physical hazards to humans such as injury and substantive hazards to marine life. 72 There is strong public awareness of these environmental hazards, especially for marine life, but less so of micro‐ and nanoplastics. 6 , 7
Micro‐ and nanoplastics present very different hazards, with four key areas of concern being: leaching of additives; plastic particles as vectors for environmental contaminants and micro‐organisms; indirect effects through actions at the lining of our guts or lungs; and, for particles small enough to pass through biological barriers, direct effects within tissues.
In addition to degradation of waste macroplastics, micro‐ and nanoplastics are also intentionally added, for example as abrasives in personal care products, 73 , 74 , 75 , 76 or released from plastic products during daily use, including synthetic clothing, 73 , 75 , 77 plastic food containers and even baby bottles. 78 Most research has focused on larger microplastics >10 μm that are visible with microscopy techniques. There are concerning knowledge gaps regarding nanoplastics which, because of their smaller size, are anticipated to pose greater hazards for human toxicity. 5 The smallest microplastics (<10 μm) and nanoplastics are too small to detect with microscopy techniques used for larger microplastics, and their small size poses additional analytical challenges, 5 with techniques only beginning to emerge.
Human exposure
Microplastics have been detected in almost every part of the environment, 75 , 76 , 79 including freshwater and air, 73 , 75 , 76 in drinking water and a diverse range of foods and beverages including honey, milk, seafood, table salt and beer. 73 , 74 , 75
Ingestion and local effects in the gut
Estimates of microplastic ingested are imprecise, but could be as high as approximately 200 000 microplastic particles/day or 0.1–5 g/week. 80 Microplastics are present in stools of humans and also many animals. 81 Animal studies have reported multiple local effects of engineered nano‐ and microplastics in the gut, including inflammation, barrier function deterioration and gut microbiota changes. 76
Inhalation and local effects in the lung
Airborne microplastics are prevalent even in very remote planetary regions. 82 Inhalation of airborne microplastics is modelled to be a major route of human exposure, 73 , 83 with evidence for plastic fibres in human lung tissue. 82 , 84 There are multiple sources of airborne microplastics including microplastic fibres from synthetic textiles and the synthetic textile industry 82 , 83 and microplastic degradation products from vehicle tyres. 82 ‘Tyre crumb’ alone is a substantive component of overall PM2.5 and PM10 particulate air pollution, 82 although the overall contribution of microplastics is unknown. 82
Occupationally exposed textile workers may experience a range of interstitial lung disease 82 , 83 : lung biopsies reveal inflammation, fibrosis and granuloma formation. 82 , 83 In vitro studies in human lung cell lines have separately reported pro‐inflammatory, cytotoxic or pro‐apoptotic effects of engineered nano‐ and microplastics. 82
Internal exposure and detection in tissues
The likelihood of uptake of micro‐ and nanoplastics through gastrointestinal and alveolar epithelium differs by size. 5 , 73 Animal and in vitro models of human biological barriers show translocation of microplastics below 5–10 μm from the gut into the circulatory and/or lymphatic systems. 73 , 75 , 85 In animal models, in vitro and in a human placental perfusion study, engineered nanoplastics cross cell membranes as well as specialist biological barriers such as the mammalian placental barrier and blood–brain barrier. 73 , 75
To date, microplastics have been detected in human faeces, 86 lung 82 , 84 and colectomy samples 87 as well as placenta 88 , 89 although the latter requires further confirmation. Techniques to directly detect nanoplastics in human tissue are yet to be established.
It is not known what the direct biological effects of micro‐ and nanoplastic fragments may be in the diverse tissues and organs but there is the potential, as shown in animal models and human in vitro studies, to disrupt fundamental processes across multiple cell types and trigger, for example, inflammation and oxidative stress. 75 , 85 , 90
Vectors for additives, environmental toxins and micro‐organisms
Not only do micro‐ and nanoplastics contain complex mixtures of additives and other chemicals from their initial manufacture, but there is growing evidence that once in contaminated environments, like our ocean, toxic chemicals including POPs 75 , 77 and heavy metals 77 accumulate through adsorption. Decreasing particle size results in increasing surface‐area‐to‐volume ratio, providing greater opportunity for diffusion of additives from the plastic, or adsorption and subsequent release of chemicals from the environment. 5 Nanoplastics are of particular concern because the combination of available surface‐area for exchange and tissue penetration due to their small size could deliver locally high doses of leached compounds. 5
Environmental microplastics may also be coated with a biofilm or ‘eco‐corona’, 5 of particular concern due to mixing between microplastics and human effluent in sewerage. 77 There is evidence that biofilms carry pathogenic bacteria, some with microbial resistance. 72 , 75 , 77
Conclusion
Not simple, not cheap, not convenient, not inert and not sustainable
We need to fundamentally re‐think plastics. Consumers perceive plastics to be cheap, convenient and recyclable. 7 But plastics are complex mixtures of industrial chemicals, and our review uncovers an intricate set of hazards that we poorly understand and are currently failing to manage. Not only are plastics rarely recycled to keep them out of waste streams and turn the virgin plastic production tap off, but they are also largely not recyclable with existing technology. As with other fossil fuel commodities, market forces are not factoring in the cost of managing hazards to human and planetary health, and current generations are effectively passing responsibility for the problem onto future generations who do not have a voice.
What can you do?
As consumers, we can value the full cost of the plastic we use each day, ‘choose to refuse’ and reduce use. We can be curious and ask questions about where the plastic comes from, what is in it and where it goes.
As medical professionals, we have expertise to share the science and the respected voice to advocate for the health of future generations and the planet that they depend on. We can use that voice to advocate with regulators so that industry takes responsibility for the hazards of their products, and to empower consumers to demand this of industry, regulators and brands.
Opportunity for change
Change is possible. Plastics can be simpler, safer and recyclable. This will require improved recycling technology to turn off the tap on virgin plastic, 91 redesign of the plastics themselves and redesign plastic chemical regulation. Working with industry to introduce extended producer responsibility for plastic use and waste management will require intervention by policy‐makers to reduce demand for plastics, for example by banning unnecessary plastic applications, and to level the economic playfield for sustainable circular plastic, for example by taxing virgin fossil fuel‐based feedstocks and introducing minimum recycled content standards. A mechanism for post‐marketing surveillance, just as with pharmaceuticals or pesticides, is also critical. We should not be producing vast quantities of chemicals of unknown human toxicity if we cannot detect human exposure nor monitor health effects. Transparency around additives and non‐intentionally added substances in plastics is therefore essential, as are methods for detecting plastic chemicals in ongoing biomonitoring programmes. Investment in techniques to measure nanoplastics and study their health effects is also critical.
Change is starting. Global bodies such as the Organisation for Economic Co‐operation and Development are reviewing our relationship with plastics, 92 as are influential regional regulatory bodies such as the European Union. 93 , 94 Canada has defined plastics as toxic, 95 acknowledging the environmental impact of plastic and its harm to human health. Adding the authoritative voice of medical professions to advocate for the health of future generations is a critical element that adds weight to the urgent need to regulate and redesign plastic.
Acknowledgements
This work was funded by the Minderoo Foundation, Perth. We thank Louise Goodes, Joanne Webb, Meredith Ryland and Lisa Hooyer, Plastics & Human Health – Minderoo Foundation, and Dominic Charles, No Plastic Waste – Minderoo Foundation, for their comments.
Conflict of interest: The authors are employed by the Minderoo Foundation, a modern philanthropic organisation https://www.minderoo.org/about/#overview.
References
- 1. Geyer R, Jambeck JR, Law KL. Production, use, and fate of all plastics ever made. Sci. Adv. 2017; 3: e1700782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wiesinger H, Wang Z, Hellweg S. Deep dive into plastic monomers, additives, and processing aids. Environ. Sci. Technol. 2021; 55: 9339–51. [DOI] [PubMed] [Google Scholar]
- 3. Hahladakis JN, Velis CA, Weber R, Iacovidou E, Purnell P. An overview of chemical additives present in plastics: Migration, release, fate and environmental impact during their use, disposal and recycling. J. Hazard. Mater. 2018; 344: 179–99. [DOI] [PubMed] [Google Scholar]
- 4. Muncke J, Andersson A‐M, Backhaus T et al. Impacts of food contact chemicals on human health: A consensus statement. Environ. Health 2020; 19: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gigault J, El Hadri H, Nguyen B et al. Nanoplastics are neither microplastics nor engineered nanoparticles. Nat. Nanotechnol. 2021; 16: 501–7. [DOI] [PubMed] [Google Scholar]
- 6. Heidbreder LM, Bablok I, Drews S, Menzel C. Tackling the plastic problem: A review on perceptions, behaviors, and interventions. Sci. Total Environ. 2019; 668: 1077–93. [DOI] [PubMed] [Google Scholar]
- 7. Dilkes‐Hoffman L, Ashworth P, Laycock B, Pratt S, Lant P. Public attitudes towards bioplastics – Knowledge, perception and end‐of‐life management. Resour. Conserv. Recycl. 2019; 151: 104479. [Google Scholar]
- 8. Barbir J, Leal Filho W, Salvia AL et al. Assessing the levels of awareness among European citizens about the direct and indirect impacts of plastics on human health. Int. J. Environ. Res. Public Health 2021; 18: 3116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Azoulay D, Villa P, Arellano Y et al. Plastic and Health – The Hidden Costs of a Plastic Planet; Washington DC: Center for International Environmental Law, 2019. Available from: https://www.ciel.org/wp-content/uploads/2019/02/Plastic-and-Health-The-Hidden-Costs-of-a-Plastic-Planet-February-2019.pdf [accessed 23 September 2021]. [Google Scholar]
- 10. Epstein PR, Selber J (eds). Oil: A Life Cycle Analysis of Its Health and Environmental Impacts. Boston, MA: The Center for Health and the Global Environment, Harvard Medical School, 2002. Available from: http://oneplanetfellows.pbworks.com/f/Oil_Impacts.pdf [accessed 23 September 2021]. [Google Scholar]
- 11. Chu J, Hu X, Kong L et al. Dynamic flow and pollution of antimony from polyethylene terephthalate (PET) fibers in China. Sci. Total Environ. 2021; 771: 144643. [DOI] [PubMed] [Google Scholar]
- 12. Zheng J, Suh S. Strategies to reduce the global carbon footprint of plastics. Nat. Clim. Change 2019; 9: 374–8. [Google Scholar]
- 13. Masson‐Delmotte V, Zhai P, Pirani A, Connors SL, Péan C, Berger S, Caud N, Chen Y, Goldfarb L, Gomis MI, Huang M, Leitzell K, Lonnoy E, Matthews JBR, Maycock TK, Waterfield T, Yelekçi O, Yu R, Zhou B, editors. Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge (UK): Cambridge University Press; In Press. IPCC, 2021: Summary for Policymakers; [41 p.]. Available from: https://www.ipcc.ch/report/ar6/wg1/downloads/report/IPCC_AR6_WGI_SPM.pdf [accessed 23 September 2021]. [Google Scholar]
- 14. World Health Organisation . COP24 special report: health and climate change. Geneva Switzerland: World Health Organization; 2018. Available from: https://apps.who.int/iris/handle/10665/276405 [accessed 11 October 2021]. [Google Scholar]
- 15. Cohen AJ, Brauer M, Burnett R et al. Estimates and 25‐year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the global burden of diseases study 2015. Lancet 2017; 389: 1907–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nelson W, Liu D‐Y, Yang Y, Zhong Z‐H, Wang Y‐X, Ding Y. In utero exposure to persistent and nonpersistent endocrine‐disrupting chemicals and anogenital distance. A systematic review of epidemiological studies. Biol. Reprod. 2020; 102: 276–91. [DOI] [PubMed] [Google Scholar]
- 17. Rancière F, Lyons JG, Loh VHY et al. Bisphenol A and the risk of cardiometabolic disorders: A systematic review with meta‐analysis of the epidemiological evidence. Environ. Health 2015; 14: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fu X, Xu J, Zhang R, Yu J. The association between environmental endocrine disruptors and cardiovascular diseases: A systematic review and meta‐analysis. Environ. Res. 2020; 187: 109464. [DOI] [PubMed] [Google Scholar]
- 19. Hu Y, Wen S, Yuan D et al. The association between the environmental endocrine disruptor bisphenol A and polycystic ovary syndrome: A systematic review and meta‐analysis. Gynecol. Endocrinol. 2018; 34: 370–7. [DOI] [PubMed] [Google Scholar]
- 20. Song Y, Chou EL, Baecker A et al. Endocrine‐disrupting chemicals, risk of type 2 diabetes, and diabetes‐related metabolic traits: A systematic review and meta‐analysis. J. Diabetes 2016; 8: 516–32. [DOI] [PubMed] [Google Scholar]
- 21. Ribeiro CM, Beserra BTS, Silva NG et al. Exposure to endocrine‐disrupting chemicals and anthropometric measures of obesity: A systematic review and meta‐analysis. BMJ Open 2020; 10: e033509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wu W, Li M, Liu A et al. Bisphenol A and the risk of obesity a systematic review with meta‐analysis of the epidemiological evidence. Dose Response 2020; 18: 1559325820916949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen D, Kannan K, Tan H et al. Bisphenol analogues other than BPA: Environmental occurrence, human exposure, and toxicity—A review. Environ. Sci. Technol. 2016; 50: 5438–53. [DOI] [PubMed] [Google Scholar]
- 24. Zhang H, Gao F, Ben Y, Su Y. Association between phthalate exposure and risk of spontaneous pregnancy loss: A systematic review and meta‐analysis. Environ. Pollut. 2020; 267: 115446. [DOI] [PubMed] [Google Scholar]
- 25. Dorman DC, Chiu W, Hales BF et al. Systematic reviews and meta‐analyses of human and animal evidence of prenatal diethylhexyl phthalate exposure and changes in male anogenital distance. J. Toxicol. Environ. Health B Crit. Rev. 2018; 21: 207–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cai H, Zheng W, Zheng P et al. Human urinary/seminal phthalates or their metabolite levels and semen quality: A meta‐analysis. Environ. Res. 2015; 142: 486–94. [DOI] [PubMed] [Google Scholar]
- 27. Golestanzadeh M, Riahi R, Kelishadi R. Association of exposure to phthalates with cardiometabolic risk factors in children and adolescents: A systematic review and meta‐analysis. Environ. Sci. Pollut. Res. 2019; 26: 35670–86. [DOI] [PubMed] [Google Scholar]
- 28. Li M‐C, Chen C‐H, Guo YL. Phthalate esters and childhood asthma: A systematic review and congener‐specific meta‐analysis. Environ. Pollut. 2017; 229: 655–60. [DOI] [PubMed] [Google Scholar]
- 29. Wu W, Wu C, Ji C et al. Association between phthalate exposure and asthma risk: A meta‐analysis of observational studies. Int. J. Hyg. Environ. Health 2020; 228: 113539. [DOI] [PubMed] [Google Scholar]
- 30. Lee D‐W, Kim M‐S, Lim Y‐H, Lee N, Hong Y‐C. Prenatal and postnatal exposure to di‐(2‐ethylhexyl) phthalate and neurodevelopmental outcomes: A systematic review and meta‐analysis. Environ. Res. 2018; 167: 558–66. [DOI] [PubMed] [Google Scholar]
- 31. Wen Y, Liu S‐D, Lei X, Ling Y‐S, Luo Y, Liu Q. Association of PAEs with precocious puberty in children: A systematic review and meta‐analysis. Int. J. Environ. Res. Public Health 2015; 12: 15254–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Golestanzadeh M, Riahi R, Kelishadi R. Association of phthalate exposure with precocious and delayed pubertal timing in girls and boys: A systematic review and meta‐analysis. Environ Sci Process Impacts 2020; 22: 873–94. [DOI] [PubMed] [Google Scholar]
- 33. Shoshtari‐Yeganeh B, Zarean M, Mansourian M et al. Systematic review and meta‐analysis on the association between phthalates exposure and insulin resistance. Environ. Sci. Pollut. Res. 2019; 26: 9435–42. [DOI] [PubMed] [Google Scholar]
- 34. Kim MJ, Moon S, Oh B‐C, Jung D, Choi K, Park YJ. Association between diethylhexyl phthalate exposure and thyroid function: A meta‐analysis. Thyroid 2019; 29:183–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cai W, Yang J, Liu Y, Bi Y, Wang H. Association between phthalate metabolites and risk of endometriosis: A meta‐analysis. Int. J. Environ. Res. Public Health 2019; 16: 3678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Govarts E, Nieuwenhuijsen M, Schoeters G et al. Birth weight and prenatal exposure to polychlorinated biphenyls (PCBs) and dichlorodiphenyldichloroethylene (DDE): A meta‐analysis within 12 European birth cohorts. Environ. Health Perspect. 2012; 120: 162–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zou H, Lin Y, Yang L et al. Neonatal weight and prenatal exposure to polychlorinated biphenyls: A meta‐analysis. Asian Pac. J. Cancer Prev. 2019; 20: 3251–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Li M‐C, Chen P‐C, Tsai P‐C et al. Mortality after exposure to polychlorinated biphenyls and polychlorinated dibenzofurans: A meta‐analysis of two highly exposed cohorts. Int. J. Cancer 2015; 137: 1427–32. [DOI] [PubMed] [Google Scholar]
- 39. Zani C, Ceretti E, Covolo L, Donato F. Do polychlorinated biphenyls cause cancer? A systematic review and meta‐analysis of epidemiological studies on risk of cutaneous melanoma and non‐Hodgkin lymphoma. Chemosphere 2017; 183: 97–106. [DOI] [PubMed] [Google Scholar]
- 40. Wu HW, Bertrand KA, Choi AL et al. Persistent organic pollutants and type 2 diabetes: A prospective analysis in the nurses' health study and meta‐analysis. Environ. Health Perspect. 2013; 121: 153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cano‐Sancho G, Ploteau S, Matta K et al. Human epidemiological evidence about the associations between exposure to organochlorine chemicals and endometriosis: Systematic review and meta‐analysis. Environ. Int. 2019; 123: 209–23. [DOI] [PubMed] [Google Scholar]
- 42. Roy D, Morgan M, Yoo C et al. Integrated bioinformatics, environmental epidemiologic and genomic approaches to identify environmental and molecular links between endometriosis and breast cancer. Int. J. Mol. Sci. 2015; 16: 25285–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zhao X, Peng S, Xiang Y et al. Correlation between prenatal exposure to polybrominated diphenyl ethers (PBDEs) and infant birth outcomes: A meta‐analysis and an experimental study. Int. J. Environ. Res. Public Health 2017; 14: 268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lam J, Lanphear BP, Bellinger D et al. Developmental PBDE exposure and IQ/ADHD in childhood: A systematic review and meta‐analysis. Environ. Health Perspect. 2017; 125: 086001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gascon M, Sunyer J, Casas M et al. Prenatal exposure to DDE and PCB 153 and respiratory health in early childhood: A meta‐analysis. Epidemiology 2014; 25: 544–53. [DOI] [PubMed] [Google Scholar]
- 46. Zani C, Toninelli G, Filisetti B, Donato F. Polychlorinated biphenyls and cancer: An epidemiological assessment. J. Environ. Sci. Health C 2013; 31: 99–144. [DOI] [PubMed] [Google Scholar]
- 47. Leng L, Li J, Luo X et al. Polychlorinated biphenyls and breast cancer: A congener‐specific meta‐analysis. Environ. Int. 2016; 88: 133–41. [DOI] [PubMed] [Google Scholar]
- 48. Catalani S, Donato F, Tomasi C, Pira E, Apostoli P, Boffetta P. Occupational and environmental exposure to polychlorinated biphenyls and risk of non‐Hodgkin lymphoma: A systematic review and meta‐analysis of epidemiology studies. Eur. J. Cancer Prev. 2019; 28: 441–50. [DOI] [PubMed] [Google Scholar]
- 49. Zhang J, Huang Y, Wang X, Lin K, Wu K. Environmental polychlorinated biphenyl exposure and breast cancer risk: A meta‐analysis of observational studies. PLoS One 2015; 10: e0142513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. United States Environmental Protection Agency . CompTox Chemicals Dashboard, PFASMASTER Chemicals. PFAS List of Master Substances (Version 2). 2021. Available from: https://comptox.epa.gov/dashboard/chemical_lists/PFASMASTER [accessed 23 September 2021].
- 51. Johnson PI, Sutton P, Atchley DS et al. The navigation guide—Evidence‐based medicine meets environmental health: Systematic review of human evidence for PFOA effects on fetal growth. Environ. Health Perspect. 2014; 122: 1028–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Negri E, Metruccio F, Guercio V et al. Exposure to PFOA and PFOS and fetal growth: A critical merging of toxicological and epidemiological data. Crit. Rev. Toxicol. 2017; 47: 489–515. [DOI] [PubMed] [Google Scholar]
- 53. Steenland K, Barry V, Savitz D. Serum perfluorooctanoic acid and birthweight: An updated meta‐analysis with bias analysis. Epidemiology 2018; 29: 765–76. [DOI] [PubMed] [Google Scholar]
- 54. Liu P, Yang F, Wang Y, Yuan Z. Perfluorooctanoic acid (PFOA) exposure in early life increases risk of childhood adiposity: A meta‐analysis of prospective cohort studies. Int. J. Environ. Res. Public Health 2018; 15: 2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Forns J, Verner M‐A, Iszatt N et al. Early life exposure to perfluoroalkyl substances (PFAS) and ADHD: A meta‐analysis of nine European population‐based studies. Environ. Health Perspect. 2020; 128: 057002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Luo Y, Deji Z, Huang Z. Exposure to perfluoroalkyl substances and allergic outcomes in children: A systematic review and meta‐analysis. Environ. Res. 2020; 191: 110145. [DOI] [PubMed] [Google Scholar]
- 57. Kim MJ, Moon S, Oh B‐C et al. Association between perfluoroalkyl substances exposure and thyroid function in adults: A meta‐analysis. PLOS ONE 2018; 13: e0197244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. García Ibarra V, Rodríguez Bernaldo de Quirós A, Paseiro Losada P, Sendón R. Non‐target analysis of intentionally and non intentionally added substances from plastic packaging materials and their migration into food simulants. Food Packag. Shelf Life 2019; 21: 100325. [Google Scholar]
- 59. Zimmermann L, Bartosova Z, Braun K, Oehlmann J, Völker C, Wagner M. Plastic products leach chemicals that induce in vitro toxicity under realistic use conditions. Environ. Sci. Technol. 2021; 55: 11814–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tian L, Zheng J, Goodyer CG, Bayen S. Non‐targeted screening of plastic‐related chemicals in food collected in Montreal, Canada. Food Chem. 2020; 326: 126942. [DOI] [PubMed] [Google Scholar]
- 61. Dubocq F, Kärrman A, Gustavsson J, Wang T. Comprehensive chemical characterization of indoor dust by target, suspect screening and nontarget analysis using LC‐HRMS and GC‐HRMS. Environ. Pollut. 2021; 276: 116701. [DOI] [PubMed] [Google Scholar]
- 62. Wang A, Abrahamsson DP, Jiang T et al. Suspect screening, prioritization, and confirmation of environmental chemicals in maternal‐newborn pairs from San Francisco. Environ. Sci. Technol. 2021; 55: 5037–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Caballero‐Casero N, Castro G, Bastiaensen M et al. Identification of chemicals of emerging concern in urine of Flemish adolescents using a new suspect screening workflow for LC‐QTOF‐MS. Chemosphere 2021; 280: 130683. [DOI] [PubMed] [Google Scholar]
- 64. Schyns ZOG, Shaver MP. Mechanical recycling of packaging plastics: A review. Macromol. Rapid Commun. 2021; 42: 2000415. [DOI] [PubMed] [Google Scholar]
- 65. Zhu J‐B, Watson EM, Tang J, Chen EY‐X. A synthetic polymer system with repeatable chemical recyclability. Science 2018; 360: 398–403. [DOI] [PubMed] [Google Scholar]
- 66. King S, Hutchinson SA, Boxall NJ. Advanced Recycling Technologies to Address Australia's Plastic Waste. Canberra, Australia: Commonwealth Scientific and Industrial Research Organisation; 2021. [Google Scholar]
- 67. Powrie W, Velis C, Cook E, Ingham H. Open uncontrolled burning of solid waste undermines human health: Time to act. Waste Manag. Res. 2021; 39: 1–2. [DOI] [PubMed] [Google Scholar]
- 68. Quecholac‐Piña X, Hernández‐Berriel MD, Mañón‐Salas MD, Espinosa‐Valdemar RM, Vázquez‐Morillas A. Degradation of plastics under anaerobic conditions: A short review. Polymers 2020; 12: 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lebreton L, Andrady A. Future scenarios of global plastic waste generation and disposal. Palgrave Commun. 2019; 5: 6. [Google Scholar]
- 70. Jambeck JR, Geyer R, Wilcox C et al. Plastic waste inputs from land into the ocean. Science 2015; 347: 768–71. [DOI] [PubMed] [Google Scholar]
- 71. Hartmann NB, Hüffer T, Thompson RC et al. Are we speaking the same language? Recommendations for a definition and categorization framework for plastic debris. Environ. Sci. Technol. 2019; 53: 1039–47. [DOI] [PubMed] [Google Scholar]
- 72. Landrigan PJ, Stegeman JJ, Fleming LE et al. Human health and ocean pollution. Ann. Glob. Health 2020; 86: 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Kannan K, Vimalkumar KA. Review of human exposure to microplastics and insights into microplastics as obesogens. Front. Endocrinol. 2021; 12: 978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Revel M, Châtel A, Mouneyrac C. Micro(nano)plastics: A threat to human health? Curr. Opin. Environ. Sci. Health 2018; 1: 17–23. [Google Scholar]
- 75. Prata JC, da Costa JP, Lopes I, Duarte AC, Rocha‐Santos T. Environmental exposure to microplastics: An overview on possible human health effects. Sci. Total Environ. 2020; 702: 134455. [DOI] [PubMed] [Google Scholar]
- 76. Huang Z, Weng Y, Shen Q, Zhao Y, Jin Y. Microplastic: A potential threat to human and animal health by interfering with the intestinal barrier function and changing the intestinal microenvironment. Sci. Total Environ. 2021; 785: 147365. [DOI] [PubMed] [Google Scholar]
- 77. Mendoza LMR, Karapanagioti H, Álvarez NR. Micro(nanoplastics) in the marine environment: Current knowledge and gaps. Curr. Opin. Environ. Sci. Health 2018; 1: 47–51. [Google Scholar]
- 78. Li D, Shi Y, Yang L et al. Microplastic release from the degradation of polypropylene feeding bottles during infant formula preparation. Nat. Food 2020; 1: 746–54. [DOI] [PubMed] [Google Scholar]
- 79. Stubbins A, Law KL, Muñoz SE, Bianchi TS, Zhu L. Plastics in the earth system. Science 2021; 373: 51–5. [DOI] [PubMed] [Google Scholar]
- 80. Senathirajah K, Attwood S, Bhagwat G, Carbery M, Wilson S, Palanisami T. Estimation of the mass of microplastics ingested – A pivotal first step towards human health risk assessment. J. Hazard. Mater. 2021; 404: 124004. [DOI] [PubMed] [Google Scholar]
- 81. Schwabl P, Köppel S, Königshofer P et al. Detection of various microplastics in human stool. Ann. Intern. Med. 2019; 171: 453–7. [DOI] [PubMed] [Google Scholar]
- 82. Amato‐Lourenço LF, dos Santos Galvão L, de Weger LA, Hiemstra PS, Vijver MG, Mauad T. An emerging class of air pollutants: Potential effects of microplastics to respiratory human health? Sci. Total Environ. 2020; 749: 141676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Gasperi J, Wright SL, Dris R et al. Microplastics in air: Are we breathing it in? Curr. Opin. Environ. Sci. Health 2018; 1: 1–5. [Google Scholar]
- 84. Pauly JL, Stegmeier SJ, Allaart HA et al. Inhaled cellulosic and plastic fibers found in human lung tissue. Cancer Epidemiol. Biomarkers Prev. 1998; 7: 419–28. [PubMed] [Google Scholar]
- 85. Yong CQJ, Valiyaveettil S, Tang BL. Toxicity of microplastics and nanoplastics in mammalian systems. Int. J. Environ. Res. Public Health 2020; 17(5):1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Pérez‐Guevara F, Kutralam‐Muniasamy G, Shruti VC. Critical review on microplastics in fecal matter: Research progress, analytical methods and future outlook. Sci. Total Environ. 2021; 778: 146395. [DOI] [PubMed] [Google Scholar]
- 87. Ibrahim YS, Tuan Anuar S, Azmi AA et al. Detection of microplastics in human colectomy specimens. JGH Open 2021; 5: 116–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Ragusa A, Svelato A, Santacroce C et al. Plasticenta: First evidence of microplastics in human placenta. Environ. Int. 2021; 146: 106274. [DOI] [PubMed] [Google Scholar]
- 89. Braun T, Ehrlich L, Henrich W et al. Detection of microplastic in human placenta and meconium in a clinical setting. Pharmaceutics 2021; 13: 921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Rahman A, Sarkar A, Yadav OP, Achari G, Slobodnik J. Potential human health risks due to environmental exposure to nano‐ and microplastics and knowledge gaps: A scoping review. Sci. Total Environ. 2021; 757: 143872. [DOI] [PubMed] [Google Scholar]
- 91. Charles D, Kimman L, Saran N. The Plastic Waste Makers Index – Revealing the Source of the Single‐Use Plastics Crisis. Perth, Australia: Minderoo Foundation; 2021. [Google Scholar]
- 92. Environment Directorate Chemicals and Biotechnology Committee . ENV/CBC/RM(2021)6; Organisation for Economic Co‐operation and Development. 2021.
- 93. European Chemicals Agency . Mapping exercise – Plastic additives initiative – ECHA. Available from: https://echa.europa.eu/mapping-exercise-plastic-additives-initiative [accessed 23 September 2021].
- 94. European Chemicals Agency . Plastic additives initiative – ECHA. Available from: https://echa.europa.eu/da/plastic-additives-initiative [accessed 23 September 2021].
- 95. Health Canada . Science Assessment of Plastic Pollution. Ottawa, ON: Government of Canada; 2020. Available from: https://www.canada.ca/en/environment-climate-change/services/evaluating-existing-substances/science-assessment-plastic-pollution.html [accessed 23 September 2021]. [Google Scholar]


