Abstract
Aim
Maintaining ≥20 teeth is a public health goal worldwide. Healthy aging, which includes psychological and social well‐being, as well as physical indicators, has attracted a great deal of attention with the progression of aging societies. However, no studies have examined the association between the number of remaining teeth and healthy aging. This study aimed to investigate the association between the number of remaining teeth and healthy aging.
Methods
This community‐based longitudinal cohort study included 8300 Japanese people aged ≥65 years who were free of disability and depression in the baseline survey in 2006. The participants were categorized into four groups according to the number of remaining teeth at baseline: 0–9, 10–19, 20–24 and ≥25. The primary outcome was healthy aging (defined as meeting all four of the following criteria: free of disability, free of depression, high health‐related quality of life and high life satisfaction), as assessed by a questionnaire survey carried out in 2017. Multiple logistic regression was used to calculate the corresponding odds ratios and 95% confidence intervals.
Results
During about 11 years of follow‐up, 621 (7.5%) participants attained healthy aging. Participants with ≥20 remaining teeth showed a higher healthy aging rate. Compared with participants with 0–9 teeth, the multivariate‐adjusted odds ratios (95% confidence intervals) for 10–19, 20–24 and ≥25 teeth were 0.98 (0.77–1.26), 1.28 (1.01–1.63) and 1.59 (1.24–2.03), respectively.
Conclusions
These findings suggest that maintaining ≥20 teeth was associated with healthy aging. Geriatr Gerontol Int 2022; 22: 68–74.
Keywords: healthy aging, longitudinal study, oral health, remaining teeth, successful aging
Introduction
With population aging, “successful aging” or “healthy aging” has attracted a great deal of attention worldwide, because people have begun to seek well‐being during aging rather than mere longevity and absence of disability. 1 , 2
The concept of “successful aging” was first proposed by Rowe and Kahn, and they defined successful aging as, “low probability of disease and disease‐related disability and related risk factors,” “high cognitive and physical functional capacity” and “active engagement with life”. 3 , 4 The concept of successful aging has been further developed, and the World Health Organization in 2015 began using the term “healthy aging,” defined as “the process of developing and maintaining the functional ability that enables well‐being in older age”. 5 This definition recognizes the enhanced importance of promoting well‐being among the aged, which includes domains, such as happiness, satisfaction and fulfillment. 5 Thus, our definition of healthy aging, included not only physiological indicators (i.e. free of disability), but also factors regarding psychological and social well‐being (i.e. free of depression, high health‐related quality of life [HRQOL] and high life satisfaction). 1
Good oral health has been shown to be associated with better physical or cognitive function. 6 , 7 In addition, systematic reviews have reported that maintaining natural teeth is associated with decreased risks of dementia 8 and depression. 9 The World Health Organization reported that oral health is an important component of general health and quality of life, 10 and the goal of increasing the percentage of individuals with functional dentition (i.e. ≥21 remaining teeth) was advocated in Global Goals for Oral Health 2020. 11 Furthermore, the goal of Health Japan 21, the national health promotion strategy implemented by the Ministry of Health, Labour and Welfare of Japan, is to increase the percentage of individuals maintaining ≥20 remaining teeth until the age of 80 years from 25% in 2005 to 50% by 2022. 12 However, there is no clear evidence that ≥20 remaining teeth are required for good health. Additionally, to our knowledge, no studies have examined the association between number of remaining teeth and healthy aging.
Therefore, the present study aimed to investigate the association between number of remaining teeth and healthy aging using data from a community‐based longitudinal cohort study on older people in Japan. We defined healthy aging as not only physical capability, but also a broad domain of well‐being, including free of depression, high HRQOL and high life satisfaction.
Methods
Study participants
Baseline survey
The design of the Ohsaki Cohort 2006 Study has been described in detail elsewhere. 13 In brief, the source population was composed of all citizens aged ≥65 years living in Ohsaki city in northeastern Japan (n = 31 694). The baseline survey was carried out between 1 and 15 December 2006. A questionnaire was distributed to individual households by the heads of individual administrative districts and then collected by mail. Among the source population, 23 091 persons who provided valid responses formed the study cohort. We further excluded 6333 people who did not provide written consent for review of their long‐term care insurance (LTCI) information, 1979 who had already been certified as having a disability by the LTCI system before follow up, five who had died or moved out of the district before follow up and 4827 who had depressive symptoms or whose responses regarding depression were missing at baseline. Finally, 9947 participants were followed from 16 December 2006 to 30 November 2017 (Fig. 1).
Figure 1.
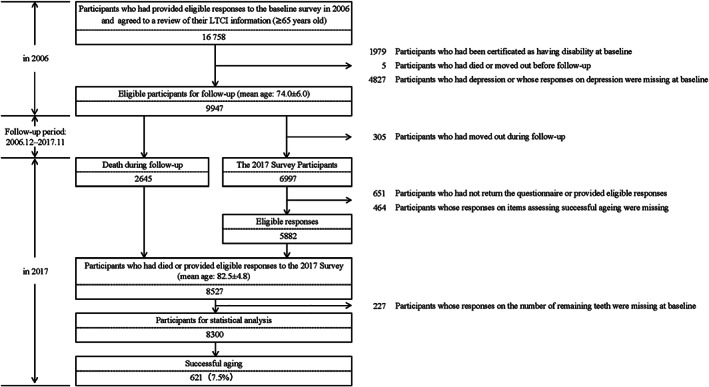
Flowchart of study participants. LTCI, long‐term care insurance.
Healthy aging assessment survey (2017 Survey)
During the follow‐up period, 2645 participants died and 305 were lost because of moving out of the study area. Among the remaining 6997 survivors, we carried out a health‐related questionnaire survey in November 2017 (2017 Survey). The questionnaire included self‐report questions regarding depression, HRQOL and life satisfaction, which were the components used to assess healthy aging. We further excluded 651 participants who did not return a questionnaire or provide eligible responses, 464 whose responses on components assessing healthy aging were missing, and 227 whose answers on the number of remaining teeth were missing at baseline. Finally, 8300 participants, consisting of 2645 who died during follow up and 5655 who provided valid responses in the 2017 Survey, were included in the statistical analysis (Fig. 1).
Number of remaining teeth (exposure)
In the baseline questionnaire, we asked the respondents to classify their number of remaining teeth into the following six categories: all (28 teeth), most (25–27 teeth), moderate (20–24 teeth), about half (10–19 teeth), few (1–9 teeth) and none (0 teeth). Then, we divided the respondents into the following four groups according to quartiles of the categorization of the number of remaining teeth: 0–9 teeth, 10–19 teeth, 20–24 teeth and ≥25 teeth.
We also asked the respondents whether they used dentures. Then, we combined the responses regarding number of teeth and denture use, and divided the respondents into the following six groups: 0–9 teeth, 10–19 teeth without dentures, 10–19 teeth with dentures, 20–24 teeth without dentures, 20–24 teeth with dentures and ≥25 teeth. The respondents who answered 0–9 teeth and ≥25 teeth were not classified based on whether they used dentures, because those who had 0–9 teeth mostly did (94.0%), and those who had ≥25 teeth mostly did not (86.1%).
Healthy aging (outcome)
Definition of healthy aging
The primary outcome of the present study was healthy aging, which consisted of the following four components according to our previous study 1 : (i) free of functional disability; (ii) free of depression; (iii) high HRQOL; and (iv) high life satisfaction. Only participants who met all four criteria were considered to have healthy aging. Participants who did not meet all four criteria were categorized as having normal aging, even if they had missing values for some of the components.
Functional disability ascertainment
In the present study, we defined incident functional disability as certification under the LTCI system in Japan (Support Level 1 or higher), which uses a nationally uniform standard of functional disability. 14 , 15 LTCI in Japan is a mandatory social insurance system that is meant to help frail older individuals carry out activities of daily living. LTCI certification was found to be associated with the ability to carry out activities of daily living in a community‐based study, and has previously been used as a measure of incident functional disability among older individuals in epidemiological studies. 16 Data regarding incident functional disability, death or emigration during follow up were transferred from the Ohsaki City Government under the agreement on Epidemiologic Research and Privacy Protection.
Measurement of depression
Depression was measured both at baseline and in the 2017 Survey through the Depression and Suicide Screen. The Depression and Suicide Screen, which was developed in Japanese by Fujisawa et al., is a brief screening instrument for depression and suicidal ideation for the aged. 17 This instrument is composed of the following five items: (1) “Is your life pretty full?”; (2) “Do you still enjoy doing the things you used to do?”; (3) “Do you think it is too much trouble to do the things you used to do?”; (4) “Do you feel that you are a useful person who is needed by others?”; and (5) “Do you feel tired without any specific reason?”. For items 1, 2) and 4, responses of “yes” are scored 0 and responses of “no” are scored 1, whereas for items 3 and 5, responses of “yes” are scored 1 and responses of “no” are scored 0. The cut‐off value of 1 (≤1 vs >1) produced satisfactory sensitivity and specificity in detecting depression (i.e. 70.5% and 72.9%, respectively), so we defined a Depression and Suicide Screen score of <2 as “free of depression”. 17
Measurement of HRQOL
HRQOL was evaluated using the three‐level version of the European Quality of Life‐5 Dimensions (EQ‐5D‐3L) in the 2017 Survey. 18 The EQ‐5D‐3L consists of the following five dimensions: (1) mobility; (2) self‐care; (3) usual activities; (4) pain/discomfort; and (5) anxiety/depression. The Japanese version of the EQ‐5D‐3L was developed by Tsuchiya et al. 19 The results were coded and converted to a utility value score ranging from −0.111 to 1.000. An EQ‐5D‐3L score of 1.000 represents a state of full health; we defined this score as “high HRQOL”.
Measurement of life satisfaction
Life satisfaction was assessed in the 2017 Survey using the Satisfaction With Life Scale developed by Diener et al. 20 ; we used the Japanese version, the reliability and validity of which were verified by Sumino. 21 The Satisfaction With Life Scale is composed of five items, each of which is scored from 1 to 7 to indicate agreement, with a possible range from 5 (low satisfaction) to 35 (high satisfaction). We defined an Satisfaction With Life Scale score of ≥25 as “high life satisfaction”.
Covariates
Body mass index was calculated as the self‐reported body weight (kg) divided by the square of the self‐reported body height (m2).
The Kihon Checklist was developed by the Ministry of Health, Labour and Welfare of Japan to predict functional decline in community‐dwelling older individuals. With regard to the cognitive function score in the Kihon Checklist, respondents were asked about their current cognitive function status using three binary questions, yielding a total score ranging from 0 to 3 points. The validity of the cognitive function score in the Kihon Checklist was confirmed in a previous study using the Clinical Dementia Rating as the gold standard. 22 According to previous studies, we classified individuals with a score of 0 as having better cognitive function. 22
Statistical analysis
The participants' baseline characteristics were evaluated using the χ2‐test for variables of proportion and one‐factor analysis of variance for continuous variables. We used these methods to compare variables among groups with varying numbers of teeth.
Next, we used multiple logistic regression models to calculate the odds ratios (ORs) and 95% confidence intervals (CIs). Participants having 0–9 teeth were used as a reference category. Dummy variables were created for each multicategorical covariate for the corresponding model. For cases where values for a covariate were missing, we created a separate category for missing values and included this in the model. The following model was used to analyze the association between number of remaining teeth and healthy aging. The model was adjusted for sex, age, smoking status (current, former, never, or missing), drinking status (current, former, never, or missing), time spent walking (≥1, 0.5–1, or <0.5 h/day or missing), sleep duration (≤6, 7–8, or ≥9 h/day, or missing), education level (≤15, 16–18 or ≥19 years, or missing), history of disease (stroke, hypertension, myocardial infarction, cancer, or diabetes [yes or no for each term]), cognitive function score (0, ≥1 or missing) and social participation (volunteering, hobby activities, or activities in neighborhood association [yes or no for each term]), because the above variables were associated with health status.
We also carried out two sets of sensitivity analyses. First, we replaced the exposure by combining the number of teeth and whether they used dentures. Second, we replaced the outcome with survival and four components of healthy aging using the same multiple logistical regression model, respectively.
All statistical analyses were carried out using the sas software package (version 9.4; SAS Institute, Cary, NC, USA). All statistical tests were two‐sided, and P‐values <0.05 were considered significant.
Ethical issues
We considered the return of a completed questionnaire to imply consent to participate in the study involving the baseline survey data, subsequent follow up for death and emigration, and the 2017 Survey data. The Ethics Committee of the Tohoku University Graduate School of Medicine (Sendai, Japan) reviewed and approved the study protocols (Ohsaki Cohort 2006 Study: 2006–206; 2017 Survey: 2017‐1‐631).
Results
In the present study, 8300 participants (48.3% men; mean [standard deviation] age at baseline in 2006, 73.3 [5.7] years) were included in the statistical analysis. During approximately 11 years of follow up, 621 (7.5%) participants met all the criteria for healthy aging, and 5746 (69.2%) survived.
Table 1 shows the characteristics of the study participants according to the number of remaining teeth. Those who had fewer teeth showed lower rate of healthy aging, were older, were likely to be women, were current smokers, spent less time walking, slept longer and had a lower education level.
Table 1.
Baseline characteristics of the study participants according to number of remaining teeth (n = 8300)
| No. remaining teeth | P‐values | ||||
|---|---|---|---|---|---|
| 0–9 | 10–19 | 20–24 | ≥25 | ||
| (n = 3414) | (n = 2017) | (n = 1652) | (n = 1217) | ||
| No. healthy aging (%) | 154 (4.5) | 131 (6.5) | 171 (10.4) | 165 (13.6) | <0.001 |
| Mean age, years (SD) | 75.4 (5.9) | 72.8 (5.3) | 71.5 (4.8) | 70.8 (4.7) | <0.001 |
| Sex (%) | |||||
| Men | 44.9 | 48.6 | 52.5 | 51.9 | <0.001 |
| Women | 55.1 | 51.4 | 47.5 | 48.2 | |
| Body mass index, kg/m2 (%) | |||||
| ≤18.4 | 5.3 | 3.9 | 2.5 | 3.7 | <0.001 |
| 18.5–24.9 | 66.4 | 66.3 | 64.7 | 63.3 | |
| ≥25.0 | 28.3 | 29.8 | 32.8 | 33.0 | |
| Smoking status (%) | |||||
| Current | 15.1 | 14.6 | 11.5 | 9.3 | <0.001 |
| Former | 28.6 | 27.8 | 27.7 | 26.9 | |
| Never | 56.3 | 57.6 | 60.8 | 63.8 | |
| Drinking status (%) | |||||
| Current | 34.8 | 43.0 | 49.1 | 48.5 | <0.001 |
| Former | 11.0 | 10.2 | 7.5 | 9.1 | |
| Never | 54.2 | 46.8 | 43.4 | 42.4 | |
| Time spent walking, h/day (%) | |||||
| ≥1.0 | 29.1 | 31.7 | 31.4 | 31.7 | <0.001 |
| 0.5–1.0 | 36.5 | 38.9 | 40.4 | 43.5 | |
| <0.5 | 34.4 | 29.4 | 28.2 | 24.8 | |
| Sleep duration, h/day (%) | |||||
| ≤6 | 17.5 | 19.6 | 19.9 | 19.8 | <0.001 |
| 7–8 | 58.5 | 61.0 | 63.0 | 65.3 | |
| ≥9 | 24.0 | 19.4 | 17.1 | 14.9 | |
| Education level † (%) | |||||
| ≤15 years | 31.4 | 25.1 | 23.9 | 18.7 | <0.001 |
| 16–18 years | 43.7 | 43.7 | 44.5 | 45.8 | |
| ≥19 years | 24.9 | 31.2 | 31.6 | 35.5 | |
| History of disease (%) | |||||
| Stroke | 2.2 | 2.5 | 2.2 | 2.1 | 0.785 |
| Hypertension | 42.4 | 42.8 | 43.6 | 42.2 | 0.820 |
| Myocardial infarction | 4.9 | 4.1 | 3.4 | 3.4 | 0.026 |
| Diabetes mellitus | 11.7 | 11.0 | 9.4 | 10.3 | 0.091 |
| Cancer | 8.4 | 8.1 | 8.1 | 8.1 | 0.963 |
| Better cognitive function ‡ (%) | 67.4 | 72.0 | 75.5 | 75.7 | <0.001 |
| Social participation (%) | |||||
| Volunteering | 31.3 | 39.2 | 44.8 | 43.0 | <0.001 |
| Hobby activities | 46.3 | 54.9 | 61.8 | 61.4 | <0.001 |
| Activities in neighborhood association | 49.5 | 55.9 | 59.8 | 59.0 | <0.001 |
Age at last school graduation.
Cognitive function score in Kihon Checklist <1.
We used the χ2‐test for variables of proportion and one‐factor anova for continuous variables (missing value excluded).
Table S1 shows the characteristics of the study participants according to healthy aging or non‐healthy aging. Those who attained healthy aging were younger, likely to have a higher education level, had better cognitive function and has a higher rate of social participation.
Table 2 shows the association between the number of remaining teeth and healthy aging. Participants with ≥20 remaining teeth showed higher rates for healthy aging. Compared with participants with 0–9 teeth, the multivariate‐adjusted ORs (95% CIs) were 0.98 (0.77–1.26) for 10–19 teeth, 1.28 (1.01–1.63) for 20–24 teeth and 1.59 (1.24–2.03) for ≥25 teeth. The ORs for healthy aging did not increase linearly with the number of remaining teeth, rather it became significant for those having ≥20 teeth.
Table 2.
Association between the number of remaining teeth and healthy aging (n = 8300)
| No. remaining teeth | ||||
|---|---|---|---|---|
| 0–9 | 10–19 | 20–24 | ≥25 | |
| (n = 3414) | (n = 2017) | (n = 1652) | (n = 1217) | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| No. healthy aging (%) | 154 (4.5) | 131 (6.5) | 171 (10.4) | 165 (13.6) |
| Model † | 1.00 (Ref.) | 0.98 (0.77–1.26) | 1.28 (1.01–1.63) | 1.59 (1.24–2.03) |
Adjustment items: sex, age (65–69, 70–74, 75–79, 80–84 or ≥85 years), smoking status (current, former, never or missing), drinking status (current, former, never or missing), time spent walking (≥1, 0.5–1 or <0.5 h/day, or missing), sleep duration (≤6, 7–8, or ≥9 h/day or missing), education level (≤15, 16–18 or ≥19 years, or missing), history of disease (stroke, hypertension, myocardial infarction, cancer or diabetes [yes or no for each term]), cognitive function score (0, ≥1 or missing) and social participation (volunteering, hobby activities or activities in neighborhood association [yes or no for each term]).
CI, confidence interval; OR, odds ratio; Ref., referent values.
This relationship did not differ when exposure was replaced with the combined number of teeth and use of dentures. The multivariate‐adjusted ORs (95% CIs) for 10–19 teeth without dentures, 10–19 teeth with dentures, 20–24 teeth without dentures, 20–24 teeth with dentures and ≥25 teeth were 0.97 (0.65–1.47), 0.98 (0.75–1.28), 1.18 (0.90–1.56), 1.46 (1.06–2.00) and 1.58 (1.23–2.03), respectively (Table 3).
Table 3.
Association between the number of remaining teeth and without/with dentures and healthy aging (n = 8220)
| No. remaining teeth and use of dentures | ||||||
|---|---|---|---|---|---|---|
| 0–9 † | 10–19 | 20–24 | ≥25 † | |||
| without dentures | with dentures | without dentures | with dentures | |||
| (n = 3404) | (n = 481) | (n = 1523) | (n = 1017) | (n = 606) | (n = 1189) | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| No. healthy aging (%) | 154 (4.5) | 31 (6.4) | 99 (6.5) | 102 (10.0) | 67 (11.1) | 162 (13.6) |
| Model ‡ | 1.00 (Ref.) | 0.97 (0.65–1.47) | 0.98 (0.75–1.28) | 1.18 (0.90–1.56) | 1.46 (1.06–2.00) | 1.58 (1.23–2.03) |
The respondents who answered 0–9 teeth and ≥25 teeth were not classified based on whether they used dentures, because those who had 0–9 teeth mostly did (94.0%), and those who had ≥25 teeth mostly did not (86.1%).
Adjustment items: sex, age (65–69, 70–74, 75–79, 80–84 or ≥85 years), smoking status (current, former, never or missing), drinking status (current, former, never or missing), time spent walking (≥1, 0.5–1 or <0.5 h/day, or missing), sleep duration (≤6, 7–8 or ≥9 h/day, or missing), education level (≤15, 16–18 or ≥19 years, or missing), history of disease (stroke, hypertension, myocardial infarction, cancer or diabetes [yes or no for each term]), cognitive function score (0, ≥1 or missing) and social participation (volunteering, hobby activities or activities in neighborhood association [yes or no for each term]).
CI, confidence interval; OR, odds ratio; Ref., referent values.
Table 4 shows the association between the number of remaining teeth and each component of healthy aging (survival, free of disability, free of depression, high HRQOL and high life satisfaction). Participants with ≥20 remaining teeth showed higher rates for each component of healthy aging; the corresponding multivariate‐adjusted ORs (95% CIs) for 10–19 teeth, 20–24 teeth and ≥25 teeth were 0.98 (0.77–1.26), 1.28 (1.01–1.63) and 1.59 (1.24–2.03), respectively, in survival; 0.95 (0.74–1.22), 1.20 (0.94–1.53) and 1.44 (1.12–1.85), respectively, in free of disability; 0.92 (0.71–1.19), 1.13 (0.88–1.44) and 1.31 (1.02–1.70), respectively, in free of depression; 0.92 (0.71–1.19), 1.14 (0.89–1.46) and 1.37 (1.06–1.77), respectively, in high HRQOL; and 0.93 (0.72–1.20), 1.14 (0.89–1.47) and 1.35 (1.05–1.75), respectively, in high life satisfaction.
Table 4.
Association between the number of remaining teeth and survival and four components of healthy aging
| No. remaining teeth | ||||
|---|---|---|---|---|
| 0–9 | 10–19 | 20–24 | ≥25 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Survival | ||||
| Percentages of participants that survived | 60.5 | 70.0 | 77.2 | 81.7 |
| Model † | 1.00 (Ref.) | 0.98 (0.77–1.26) | 1.28 (1.01–1.63) | 1.59 (1.24–2.03) |
| Free of disability | ||||
| Percentages of participants free of disability | 56.0 | 66.6 | 74.2 | 76.5 |
| Model † | 1.00 (Ref.) | 0.95 (0.74–1.22) | 1.20 (0.94–1.53) | 1.44 (1.12–1.85) |
| Free of depression | ||||
| Percentages of participants free of depression | 47.5 | 52.8 | 61.1 | 66.5 |
| Model † | 1.00 (Ref.) | 0.92 (0.71–1.19) | 1.13 (0.88–1.44) | 1.31 (1.02–1.70) |
| High HRQOL | ||||
| Percentages of participants with high HRQOL | 24.2 | 27.9 | 33.5 | 39.8 |
| Model † | 1.00 (Ref.) | 0.92 (0.71–1.19) | 1.14 (0.89–1.46) | 1.37 (1.06–1.77) |
| High life satisfaction | ||||
| Percentages of participants with high life satisfaction | 35.3 | 36.6 | 42.0 | 42.3 |
| Model † | 1.00 (Ref.) | 0.93 (0.72–1.20) | 1.14 (0.89–1.47) | 1.35 (1.05–1.75) |
Adjustment items: sex, age (65–69, 70–74, 75–79, 80–84 or ≥85 years), smoking status (current, former, never or missing), drinking status (current, former, never or missing), time spent walking (≥1, 0.5–1 or <0.5 h/day, or missing), sleep duration (≤6, 7–8 or ≥9 h/day, or missing), education level (≤15, 16–18 or ≥19 years, or missing), history of disease (stroke, hypertension, myocardial infarction, cancer or diabetes [yes or no for each term]), cognitive function score (0, ≥1 or missing) and social participation (volunteering, hobby activities, or activities in neighborhood association [yes or no for each term]).
CI, confidence interval; OR, odds ratio; Ref., referent values.
Discussion
To our knowledge, this is the first study to examine the association between the number of remaining teeth and healthy aging. When 0–9 teeth was used as the reference category, the category “10–19 teeth” was not statistically significant, but the categories “20–24 teeth” and “≥25 teeth” were significantly associated with healthy aging, regardless of whether they used dentures. These results suggest that having ≥20 natural teeth in older age is important to achieve healthy aging. The present findings would serve as evidence for the public health goal, such as Global Goals for Oral Health 2020 11 and Health Japan 21. 12
Previous studies have reported that maintaining more natural teeth is significantly associated with survival, 23 independence in carrying out activities of daily living, 6 better mental health 9 and a high quality of life. 24 These findings were consistent with those in the present study. Having a sufficient number of teeth helps maintains the chewing function, leading pleasurable eating of a variety of foods and taking enough nutrition. 25 In addition, in terms of aesthetics, having enough teeth has been suggested as being essential for actively talking and laughing. 26 , 27 From the aforementioned, it has been clarified that a sufficient number of teeth affects not only the physical aspect, but also the mental aspect. Therefore, the number of teeth could be a predictor of healthy aging, including happiness, satisfaction and fulfillment advocated by the World Health Organization.
In Japan, the 8020 Campaign advocating to maintain ≥20 teeth until the age of 80 years has been widespread across the nation, and the percentage of individuals maintaining ≥20 remaining teeth until the age of 80 years has increased from 25.0% in 2005 to 51.2% in 2016. 28 Globally, the prevalence of dental caries is decreasing, but periodontal disease is increasing. 29 Therefore, to realize a healthy aging society on a global scale, strategies for improving oral health are indispensable.
The present study had a number of strengths. First, we used a relatively large population‐based cohort with 8300 older participants. Second, for our definition of healthy aging, we considered not only physiological, but also psychological indicators.
However, the present study also had several limitations. First, although we excluded participants with depressive symptoms, we could not obtain information about HRQOL and life satisfaction at baseline. Second, misclassification of the number of teeth as a result of self‐reporting might have occurred. However, the validity of the self‐reported number of teeth has been confirmed in a previous study. 30
In conclusion, the results of the present study suggest that maintaining ≥20 teeth is associated with healthy aging in older people in Japan. This finding would serve as evidence for the public health goal of having older people around the world maintain ≥20 teeth to achieve healthy aging.
Disclosure statement
The authors declare no conflict of interest.
Supporting information
Table S1 Baseline characteristics of the study participants according to healthy aging (n = 8300).
Acknowledgements
The authors thank Yoshiko Nakata for her technical assistance. This work was supported by JSPS KAKENHI Grant Number JP17H04130, and by a grant‐in‐aid from the Ministry of Health, Labour and Welfare, Health and Labor Sciences research grants, Japan (Comprehensive Research on Cardiovascular and Life‐Style Related Diseases: 19FA2001, 20FA1002).
Matsuyama S, Lu Y, Aida J, Tanji F, Tsuji I. Association between number of remaining teeth and healthy aging in Japanese older people: The Ohsaki Cohort 2006 Study. Geriatr. Gerontol. Int. 2022;22:68–74. 10.1111/ggi.14320
Data Availability Statement
Research data are not shared.
References
- 1. Lu Y, Matsuyama S, Tanji F, Otsuka T, Tomata Y, Tsuji I. Social participation and healthy aging among the elderly Japanese: the Ohsaki Cohort 2006 Study. J Gerontol A Biol Sci Med Sci 2021. 10.1093/gerona/glab101 [DOI] [PubMed] [Google Scholar]
- 2. Gopinath B, Russell J, Kifley A, Flood VM, Mitchell P. Adherence to dietary guidelines and successful aging over 10 years. J Gerontol A Biol Sci Med Sci 2016; 71: 349–355. [DOI] [PubMed] [Google Scholar]
- 3. Rowe JW, Kahn RL. Human aging: usual and successful. Science 1987; 237: 143–149. [DOI] [PubMed] [Google Scholar]
- 4. Rowe JW, Kahn RL. Successful aging. Gerontologist 1997; 37: 433–440. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization . World Report on Ageing and Health, Geneva, Switzerland: World Health Organization, 2015. [Google Scholar]
- 6. Aida J, Kondo K, Hirai H et al. Association between dental status and incident disability in an older Japanese population. J Am Geriatr Soc 2012; 60: 338–343. [DOI] [PubMed] [Google Scholar]
- 7. Kato H, Takahashi Y, Iseki C et al. Tooth loss‐associated cognitive impairment in the elderly: a community‐based study in Japan. Intern Med 2019; 58: 1411–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fang WL, Jiang MJ, Gu BB et al. Tooth loss as a risk factor for dementia: systematic review and meta‐analysis of 21 observational studies. BMC Psychiatry 2018; 18: 345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cademartori MG, Gastal MT, Nascimento GG, Demarco FF, Correa MB. Is depression associated with oral health outcomes in adults and elders? A systematic review and meta‐analysis. Clin Oral Investig 2018; 22: 2685–2702. [DOI] [PubMed] [Google Scholar]
- 10. Petersen PE. World Health Organization global policy for improvement of oral health ‐ World Health Assembly 2007. Int Dent J 2008; 58: 115–121. [DOI] [PubMed] [Google Scholar]
- 11. Hobdell M, Petersen PE, Clarkson J, Johnson N. Global goals for oral health 2020. Int Dent J 2003; 53: 285–288. [DOI] [PubMed] [Google Scholar]
- 12. Ministry of Health, Labour and Welfare of Japan . Health Japan 21. 2012. [Cited 20 Dec 2019.] Available from URL: https://www.mhlw.go.jp/bunya/kenkou/dl/kenkounippon21_01.pdf
- 13. Kuriyama S, Nakaya N, Ohmori‐Matsuda K et al. The Ohsaki Cohort 2006 Study: design of study and profile of participants at baseline. J Epidemiol 2010; 20: 253–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ministry of Health, Labour and Welfare of Japan . Long‐Term Care, Health and Welfare Services for the Elderly. 2016. [Cited 20 Dec 2019.] Available from URL: https://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/index.html
- 15. Tsutsui T, Muramatsu N. Care‐needs certification in the long‐term care insurance system of Japan. J Am Geriatr Soc 2005; 53: 522–527. [DOI] [PubMed] [Google Scholar]
- 16. Arai Y, Zarit SH, Kumamoto K, Takeda A. Are there inequities in the assessment of dementia under Japan's LTC insurance system? Int J Geriatr Psychiatry 2003; 18: 346–352. [DOI] [PubMed] [Google Scholar]
- 17. Fujisawa D, Tanaka E, Sakamoto S, Neichi K, Nakagawa A, Ono Y. The development of a brief screening instrument for depression and suicidal ideation for elderly: the depression and suicide screen. Psychiatry Clin Neurosci 2005; 59: 634–638. [DOI] [PubMed] [Google Scholar]
- 18. Group TE . EuroQol ‐ a new facility for the measurement of health‐related quality of life. Health Policy 1990; 16: 199–208. [DOI] [PubMed] [Google Scholar]
- 19. Tsuchiya A, Ikeda S, Ikegami N et al. Estimating an EQ‐5D population value set: the case of Japan. Health Econ 2002; 11: 341–353. [DOI] [PubMed] [Google Scholar]
- 20. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess 1985; 49: 71–75. [DOI] [PubMed] [Google Scholar]
- 21. Sumino Z. Development of Japanese version of the satisfaction with life scale (SWLS). Paper presented at the 36th Annual Convention of the Japanese Association of Educational Psychology Review., 1994.
- 22. Meguro K, Team. KP . The validity of the basic checklist in the old‐old population: the Kurihara project. Jpn J Geriatr Psychiatry 2012; 23: 725–730. [Google Scholar]
- 23. Goto Y, Wada K, Uji T et al. Number of teeth and all‐cause and cancer mortality in a Japanese community: the Takayama study. J Epidemiol 2020; 30: 213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Haag DG, Peres KG, Balasubramanian M, Brennan DS. Oral conditions and health‐related quality of life: a systematic review. J Dent Res 2017; 96: 864–874. [DOI] [PubMed] [Google Scholar]
- 25. Wright FAC, Law GG, Milledge KL et al. Chewing function, general health and the dentition of older Australian men: the Concord health and ageing in men project. Community Dent Oral Epidemiol 2019; 47: 134–141. [DOI] [PubMed] [Google Scholar]
- 26. Miura H, Yamasaki K, Morizaki N, Moriya S, Sumi Y. Factors influencing oral health‐related quality of life (OHRQoL) among the frail elderly residing in the community with their family. Arch Gerontol Geriatr 2010; 51: e62–e65. [DOI] [PubMed] [Google Scholar]
- 27. Petersen PE. Global policy for improvement of oral health in the 21st century ‐ implications to oral health research of World Health Assembly 2007, World Health Organization. Community Dent Oral Epidemiol 2009; 37: 1–8. [DOI] [PubMed] [Google Scholar]
- 28. Ministry of Health, Labour and Welfare of Japan . Health Japan 21 middle evaluation report. 2018. [Cited 18 May 2021.] Available from URL: https://www.mhlw.go.jp/content/000378318.pdf
- 29. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392: 1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Matsui D, Yamamoto T, Nishigaki M et al. Validity of self‐reported number of teeth and oral health variables. BMC Oral Health 2016; 17: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Baseline characteristics of the study participants according to healthy aging (n = 8300).
Data Availability Statement
Research data are not shared.


