Abstract
Background
Problems with anger and aggression affect many veterans who have deployed to a warzone, resulting in serious impairment in multiple aspects of functioning. Controlled studies are needed to improve treatment options for these veterans. This randomized controlled trial compared an individually delivered cognitive behavioral therapy adapted from Novaco's Anger Control Therapy to a manualized supportive therapy to control for common therapeutic factors.
Methods
Ninety‐two post‐911 veterans deployed during Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), or Operation New Dawn (OND) with moderate to severe anger problems were randomized to receive the cognitive behavioral intervention (CBI) or the supportive intervention (SI). Anger, aggression, multiple areas of functioning and quality of life were assessed at multiple time points inclu\ding 3‐ and 6‐month follow‐up.
Results
Hierarchical linear modeling (HLM) analyses showed significant treatment effects favoring CBI for anger severity, social and interpersonal functioning, and quality of life. The presence of a PTSD diagnosis did not affect outcomes.
Conclusions
CBI is an effective treatment for OEF/OIF/OND veterans with anger problems following deployment, regardless of PTSD diagnosis.
Keywords: aggression, anger, trauma, treatment, veterans
1. INTRODUCTION
Increased anger and difficulty managing its expression is a common and serious problem in veterans who have served in a warzone. This has been true for veterans of earlier wars (e.g., Grinker & Spiegel, 1945; Kulka et al., 1990), and now is well documented in post‐911 veterans including those serving in Afghanistan (Operation Enduring Freedom, OEF) and Iraq (Operation Iraqi Freedom, OIF). For example, problems with anger and aggression following deployment were endorsed by 67% of Army soldiers (Wright et al., 2012) and 57% of combat veterans receiving VA medical care (Sayer et al., 2010). A sizable number have specifically reported acts of aggression including threats of and actual physical violence (Thomas et al., 2010). Consequences of anger and aggression in veterans include marital problems and divorce, parenting problems, domestic violence, and job instability (Evans et al., 2003; Kulka et al., 1990; Roberge et al., 2016), as well as increased suicidal ideation (Wilks et al., 2019), and poorer response to treatment for posttraumatic stress disorder (PTSD) (e.g., Forbes et al., 2008; Lloyd et al., 2014).
There are several reasons that might explain the frequency of anger and aggression in combat veterans. Hyperarousal symptoms, which are common in combat veterans with and without PTSD, contribute to postwar aggression (Lasko et al., 1994). Military training focuses on responding to threat with aggression; aggression is likely further associated with survival in combat experiences—a powerful reinforcer. Chemtob et al. (1997) proposed a model involving a “survival mode” of functioning that when triggered preempts all other cognitive processing, increases more rapid reactions requiring less evidence of threat, and decreases capacity to regulate arousal level. Persistence of the survival mode of processing beyond the warzone results in impaired ability to regulate responses to threat, and excessive anger and aggression in situations perceived as threatening where there is no real threat.
Despite the magnitude of the problem, there are no clear guidelines for treating anger and aggression in veterans. One approach would be to use empirically validated treatments for PTSD, since anger is a symptom of PTSD. However, problematic anger and aggression are common in OIF/OEF veterans without PTSD (e.g., Sayer et al., 2010) for whom PTSD treatments would not be indicated. Furthermore, among those with and without PTSD, anger is the most common problem that veterans report wanting help with (Rosen et al., 2013; Sayer et al., 2010). Also, while there are small to moderate decreases in anger and aggression following PTSD treatment, 78% of veterans treated with Cognitive Processing Therapy (Miles et al., 2020) and 80% treated with PE (Schnurr & Lunney, (2019) endorsed continuing problems with anger after treatment.
The alternative is to use treatment approaches developed specifically for treating anger. There are surprisingly few controlled studies of such treatments in veterans. Further, existing studies are limited by small samples (Chemtob et al., 1997; Donahue et al., 2017; Elgoben et al., 2021; Shea et al., 2013), or no control group (Donahue et al., 2017; Gerlock, 1994; Kalkstein et al., 2018; Linkh & Sonnek, 2003; Morland et al., 2010). In a prior study (Shea et al., 2013) we piloted a cognitive‐behavioral treatment (Novaco, 2001) that we adapted for OEF/OIF veterans (cognitive behavioral intervention—CBI) and found that CBI showed significantly more improvement than an active supportive therapy control group. These promising findings led to the current study (ClinicalTrials.gov ID: NCT02157779), a randomized controlled trial (RCT), designed to test the effectiveness of CBI compared to the supportive therapy intervention (SI) in a larger sample of OEF/OIF veterans on primary outcome measures of anger and aggression, and on secondary outcomes of functioning, quality of life, and PTSD symptoms (Shea et al., 2018). We hypothesized that CBI would show more improvement compared to SI on all outcome measures. We also proposed an exploratory hypothesis that CBI would be superior to SI for those with and without PTSD. To our knowledge, except for our pilot study (Shea et al., 2013), this is the first RCT of anger treatment in veterans using an active control for therapeutic common factors. It is also unique among anger treatment studies in its focus on a sample consisting exclusively of previously deployed post‐911 veterans, and among studies of individually delivered anger treatments to include veterans with and without PTSD.
2. METHOD
2.1. Design
This two‐arm single‐blind RCT was conducted from March 2015 to February 2019. The study was approved by the local VA Institutional Review Board and all participants provided informed consent. Participants were randomly assigned (1 to 1 ratio) to CBI or SI using urn randomization, a stratified randomization technique that systematically biases the randomization in favor of balance among the treatment condition on stratification variables (Stout et al., 1994; Wei, 1978). Balancing factors were gender, PTSD diagnosis, and time since return from deployment (≤2 years vs. >2 years).
2.2. Participants
Participants were referred by mental health clinicians from the local VA mental health service or were self‐referred in response to brochures or postings describing the study. Inclusion criteria included having served as a member of the military (Active Duty, National Guard or Reserve) in a post‐911 deployment, experiencing one or more DSM‐5 Criterion A traumatic events while deployed, reporting moderate to severe problems with anger, and at least two additional symptoms of hyperarousal. We required deployment trauma and hyperarousal symptoms in order to capture a sample with anger and aggression consistent with the survival mode model. Participants also had to agree to refrain from treatment for PTSD or anger during the study treatment phase, and if taking psychotropic medication, a stable dose for at least 4 weeks was required. Exclusion criteria included severe substance use disorder, psychotic symptoms, or a manic episode within the 3 previous months, current suicidal or homicidal ideation requiring hospitalization, and severe cognitive impairment that would preclude the ability to comprehend interview and self‐report questions.
2.3. Procedures
Participants who passed initial screening were scheduled for an interview to describe the study, obtain informed consent, and be assessed for inclusion/exclusion criteria. Eligible participants then completed the baseline assessment. Participants were compensated for assessments.
2.4. Assessment of inclusion criteria
The Clinician‐Administered PTSD Scale for DSM‐5 (CAPS‐5), a widely used structured interview with strong psychometrics (Weathers et al., 2018) was used to assess the presence of a deployment criterion A event, and symptoms of hyperarousal. The Structured Clinical Interview for DSM‐5 (SCID‐5; American Psychiatric Association, 2013) was used to rule out current severe substance use disorder or psychotic symptoms.
2.5. Primary outcome measures
Primary outcome measures include the Anger Expression Index (AX Index) from the State‐Trait Anger Inventory‐2 (STAXI‐2; Spielberger, 1999) and the Aggression (AGG) score from the Overt Aggression Scale‐Modified (OAS‐M; Coccaro, 2000). The STAXI‐2 is a self‐report questionnaire with six scales (state anger, trait anger, anger control‐in, anger control‐out, anger expression‐in, and anger expression‐out) and an overall measure of the expression and control of anger (AX Index) with a score range from 0 to 96. It has substantial psychometric evidence (Speilberger, 1999). Internal consistency α for the STAXI‐2 AX in the current study was 0.87.
The OAS‐M (Coccaro, 2000) is a semistructured interview designed to evaluate various manifestations of aggressive behaviors in outpatients. Four subcomponents (verbal aggression, aggression against objects, aggression against others, and aggression against self) comprise the overall aggression (AGG) score. Subcomponent scores are determined by multiplying the number and severity level of aggressive behaviors of each type during the prior week. Additional scores include the total number of all aggressive behaviors and a Global Anger and Aggression (GAA) score composed of two item ratings (subjective experience of anger, overt expression of anger). The OAS‐M has been shown to be reliable and valid, with good psychometric properties (Coccaro et al., 2000, Coccaro, 2020). Both the STAXI‐2 and the OAS‐M were administered at baseline, after the fourth and eighth treatment sessions, at the end of treatment, and at 3‐ and 6‐month posttreatment follow‐up assessments.
2.6. Secondary outcome measures
The interview‐based Longitudinal Interval Follow‐up Evaluation (LIFE; Keller et al., 1987) was used to assess occupational and social functioning, each on a five‐point scale ranging from 1 (no impairment, very good) to 5 (severe impairment, markedly impaired), respectively. The occupation score incorporated ratings as applicable for employment, household duties, and student work (Leon et al., 1999).
The Outcome Questionnaire (OQ), a 45‐item self‐report questionnaire developed to assess psychotherapy outcome (Lambert et al., 1997) includes three subscales (symptom distress, interpersonal relations, and social role) and a total score range from 0 to 180. Psychometrics are strong (Lambert et al., 1996). Internal consistency for the total score in the current study was 0.93.
The psychological domain scale of the WHO Quality of Life—BREF measure, also an established measure with strong psychometrics (Skevington et al., 2004) assesses satisfaction with life and oneself. Scores can range from 8 to 32. Internal consistency in the current study was .81. The CAPS‐5 (described above) symptom severity score (range of 0–80) was also included as a secondary outcome measure. Secondary measures were administered at baseline, end of treatment, and 3‐ and 6‐month follow‐up assessments.
2.7. Interviewer training and reliability
Clinical interviewers had masters or doctoral level training in psychology or social work. Training included rating previously recorded interviews and conducting practice interviews. Early study interviews for each interviewer were reviewed and rated by an experienced trainer, with feedback to interviewers. Monthly meetings were held to discuss ratings of recorded interviews to prevent drift. Intraclass correlations (Shrout & Fleiss, 1979), based upon 26 randomly selected interviews rated by a range of four to six interviewers, were as follows: OAS‐M aggression scale, 0.99; CAPS severity score, 0.81; CAPS hyperarousal items, range of 0.70–0.94; LIFE occupational functioning, 0.78; LIFE social functioning, 0.52. The lower reliability for social functioning is likely due to a restricted range of ratings; 82% of ratings were either a 3 (fair) or 4 (poor) on this five‐point scale. When examined by ratings within one point on the scale, there was 100% agreement. Clinical Interviewers were blinded to treatment conditions.
2.8. Treatment conditions
Both treatment conditions consisted of 12 weekly individual sessions, 75 min in length. The use of the term intervention rather than therapy was intended to reduce the possible military‐related stigma associated with receiving mental health treatment, with the goal of increasing acceptability and enhancing recruitment.
2.9. CBI
CBI is an adaptation of a psychotherapy developed specifically for the treatment of anger (Novaco, 2001) that conceptualizes anger in terms of interacting regulatory deficits in arousal, cognitive, and behavioral domains. Key elements include (1) psychoeducation about responses to trauma including anger and aggression following deployment in a war‐zone; (2) arousal reduction (e.g., diaphragmatic breathing); (3) cognitive restructuring of anger schemas; (4) behavioral coping strategies (e.g., training in communication, assertiveness); and (5) inoculation training (practicing cognitive, arousal, and behavioral coping skills while visualizing progressively more intense anger‐arousing scenes from personal hierarchies). For the current study, we added psychoeducation about responses to war‐zone experiences using “Battlemind” (Adler et al., 2009), which conceptualizes anger and other symptoms within the context of adaptive function in the warzone that becomes nonadaptive at home. We also increased the emphasis on arousal reduction through the introduction of multiple methods of relaxation training and reorganized the manual to increase ease of use.
2.10. Supportive intervention
The SI manual was adapted from a present‐centered therapy (PCT) manual used as an active control condition for a previous multisite study of treatment of PTSD in female veterans (Schnurr et al., 2007; Shea et al., 2003). PCT was designed to control for nonspecific treatment factors such as therapeutic relationship and support, enhancement of hope, and motivation to address problems. The manual was adapted for the current study specifically to fit the population of military personnel with post‐911 deployments. SI included the same psychoeducation as CBI. Except for the first two sessions, which include the rationale for SI and psychoeducation, the content of the sessions is determined by the patient. Interventions were supportive and problem focused. Cognitive‐behavioral interventions were proscribed.
2.11. Therapist training and supervision
Five licensed and credentialed therapists with prior training in cognitive behavioral therapy and experience treating veterans delivered both interventions. Training for both CBI and SI included a detailed review of the manual, illustration, and examples of interventions, and a review of proscribed interventions (SI only). Each therapist had one CBI training case, with supervision based on recorded sessions. A training case was not required for SI, as therapists were experienced in providing supportive therapy. One to two randomly selected sessions from early cases of both treatments were monitored for adherence and quality, and feedback provided as needed. Group supervision meetings were held weekly to discuss cases and provide feedback, transitioning to monthly meetings mid‐way through the study.
2.12. Adherence ratings
All therapy sessions were recorded. Approximately 10% of sessions within each condition were randomly chosen and rated by two clinical psychologists using previously developed scales (Shea et al., 2013). Both adherence raters rated a common set of sessions followed by discussion and consensus ratings to calibrate ratings. For the 44 CBI sessions rated, 86% of required session elements were rated as present. The average rating for therapist skill (based upon a four‐point scale with 1 = poor, 2 = fair, 3 = good, 4 = excellent) was 2.98 (0.38). Of 39 SI sessions rated, adherence was high for the two key SI interventions (89% for problem‐solving and 95% for praise and support). No proscribed elements were rated as present. The mean rating for therapist skill for SI was 3.20 (0.39).
2.13. Data analysis
Outcome variables were screened for inconsistent or abnormal values, and continuous measures were assessed for skewness and outliers. As is characteristic of the OAS‐M (Coccoro, 2020), the OAS‐M AGG score was highly skewed; thus, the AGG and subcomponent scores were winsorized and log base 10 transformed to improve normality. χ 2 analyses and analysis of variance (ANOVA) for discrete and continuous variables, respectively, were used to test for differences by treatment on baseline demographic and clinical variables. Hierarchical linear modeling (HLM) for repeated measures was used to test for differences due to treatment conditions in outcome measures, covarying for the baseline score (Raudenbush & Bryk, 2002). Analyses included all participants with at least one post‐baseline assessment (4 and 8 weeks, posttreatment, 3‐ and 6‐month follow‐ups for the OAS‐M and STAXI‐2; posttreatment, 3‐ and 6 months for the other outcome measures). We used Full Information Maximum Likelihood (Dempster et al., 1977) to account for missing data. The treatment group main effect over time was designated as the primary significance test. Hypothesis tests were two‐tailed with an α level of .025 as a partial adjustment for the number of variables tested; α levels between .025 and .05 were interpreted as trends. Effects sizes (Cohen, 1992) were calculated to illustrate between‐treatment effects. On measures with subscales, supplementary HLM analyses were conducted to help interpret findings on the total scores. HLM for repeated measures was also used to examine comparative treatment effects for participants with and without PTSD, by adding effects for PTSD diagnosis and the PTSD diagnosis by treatment group interaction to the model.
Power estimates for the repeated measures design (Faes et al., 2009) were based on detection of medium effects with a two‐tailed α of .025 as described above. Analyses indicated that a sample of 90 with 20% projected attrition would provide 83% power to detect a medium effect size of 0.60.
3. RESULTS
3.1. Descriptive analyses
Ninety‐two participants were randomized, including 47 to CBI and 45 to SI. Participants (Table 1) were predominantly male (96%), White (87%) and non‐Hispanic (79%), with a mean age of 35.9. Most had more than high school education (76%), were employed (63%), and were married or living with a partner (57%). There were no significant differences by treatment condition on any of the baseline demographic or clinical variables.
Table 1.
Demographic and clinical characteristics
| Variable | Total Sample (n = 92) | CBI (n = 47) | SI (n = 45) |
|---|---|---|---|
| % | N% | N% | |
| Male | 89 (97) | 46 (98) | 43 (96) |
| Race | |||
| Black | 6 (7) | 1 (2) | 5 (11) |
| White | 80 (87) | 42 (89) | 38 (84) |
| Native American | 5 (5) | 1 (2) | 4 (9) |
| Asian | 1 (1) | 1 (1) | 0 (0) |
| Multiracial | 5 (5) | 2 (4) | 3 (7) |
| Other | 6 (7) | 4 (9) | 2 (4) |
| Ethnicity: Hispanic | 19 (21) | 7 (15) | 12 (27) |
| Married/live tog | 52 (57) | 26 (55) | 26 (58) |
| Education | |||
| High school or less | 22 (24) | 11 (23) | 11 (24) |
| Some college | 54 (59) | 30 (64) | 24 (53) |
| Bachelors or more | 16 (17) | 6 (13) | 10 (22) |
| Employment | |||
| Full‐time | 49 (53) | 22 (47) | 27 (60) |
| Part‐time | 9 (10) | 6 (13) | 3 (7) |
| Unemployed | 29 (32) | 14 (30) | 15 (33) |
| Retired | 5 (5) | 5 (11) | 0 (0) |
| Service connection | |||
| Any | 70 (76) | 34 (72) | 36 (80) |
| PTSD | 42 (46) | 21 (45) | 21 (47) |
| Diagnoses | |||
| Current PTSD | 60 (65) | 31 (66) | 29 (64) |
| Current MDD | 46 (50) | 21 (45) | 25 (56) |
| Current AUD | 15 (16) | 9 (19) | 6 (13) |
| Current SUD | 15 (16) | 9 (19) | 6 (13) |
| Psychotropic meds | 44 (48) | 18 (38) | 26 (58) |
| Age (mean, SD) | 35.89 (9.38) | 35.30 (9.09) | 36.40 (9.75) |
| Deployments (mean, SD) | |||
| Number of | 1.61 (.84) | 1.64 (.87) | 1.58 (.81) |
| Years since last (mean, SD) | 7.06 (3.29) | 6.88 (3.08) | 7.25 (3.50) |
Abbreviations: AUD, alcohol use disorder; MDD, major depressive disorder; PTSD, posttraumatic stress disorder; SUD, substance use disorder.
One participant in each condition dropped from the study before starting treatment (Figure 1). Of the 90 participants attending at least one session, 57 (63%) completed at least 11 sessions. Significantly fewer CBI (n = 23, 50%) than SI (n = 34, 77%) participants completed (χ 2 (1, 92) = 6.91, p = .009), and CBI participants had significantly fewer sessions (CBI: M = 7.66, SD = 4.62, SI: M = 9.71, SD = 4.07); t (1, 90) = 2.26; p = .026). Seventy‐three participants (79.3%) completed at least one post‐baseline assessment.
Figure 1.
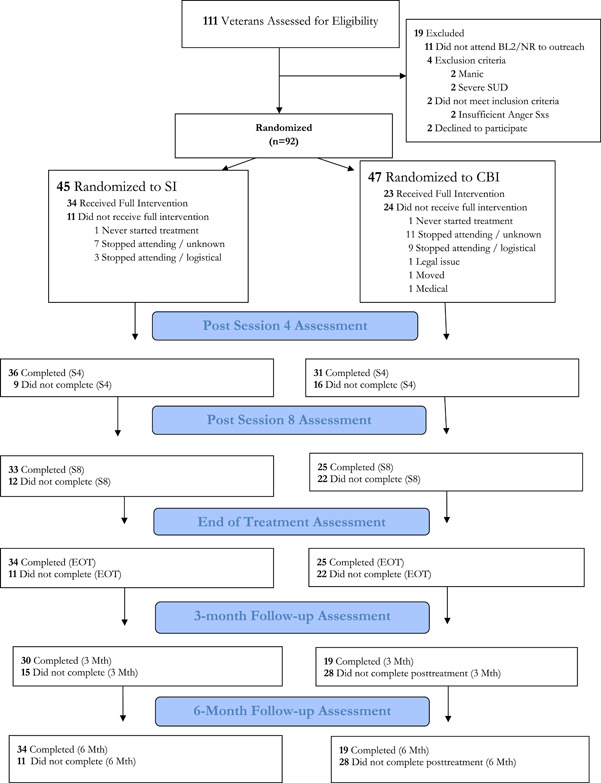
Consort diagram. CBI, cognitive‐behavioral intervention; SI, supportive intervention
Twenty‐four percent of participants received one or more nonstudy individual psychotherapy sessions during the treatment phase, 31% during the 3 month and 38% during the 6‐month follow‐up phases. A small proportion of participants participated in group (6%−7%) or family/couples therapy (5%−11%) during the study or follow‐up phases. Rates of psychiatric medications were 52% (n = 34) during the study phase, 61% (n = 30) during the 3 month, and 62% (n = 33) during the 6‐month follow‐up phase intervals. CBI and SI did not differ significantly on the proportion receiving nonstudy individual psychotherapy during the treatment phase (χ 2 (1, 59) = 0.44, p = .51), 3 month (χ 2 (1, 49) = 0.57, p = .45), or 6‐month follow‐up (χ 2 (1, 53) = 0.24, p = .62), or on group or marital therapy at any time point. There were also no significant differences on psychiatric medication use during the treatment phase (χ 2 (1, 65) = 1.21, p = .27), 3‐month (χ 2 (1, 49) = 0.15, p = .70) or 6‐month follow‐up (χ 2 (1, 53) = 1.17, p = .28).
3.2. Primary outcome measures
HLM analyses showed significantly greater improvement in CBI compared to SI on the STAXI‐2 Anger Index (F(1,182) = 5.77, p = .017) (Table 2). As can be seen in Figure 2 and Table 3 (effect sizes over time) the largest separation between the treatments were at session eight and at the end of treatment, with the difference decreasing over the follow‐up. CBI and SI did not differ significantly on OAS‐M aggression (AGG) score (F (1, 209) = 1.79, p = .17). Supplementary HLM analyses of subscales showed that for the STAXI‐2, the Anger Expression Out scale differed significantly with more improvement in CBI (F (1, 193) = 9.87, p = .002); there were no significant treatment differences on the Anger Expression In, Anger Control Out, or Anger Control In subscales. Although the OAS‐M AGG score did not differ by treatment, CBI improved more on aggressive outbursts (F (1, 209) = 5.43, p = .021), with trends toward significantly more improvement on aggression against objects (F (1, 209) = 4.44, p = .036), and global anger/aggression (GAA) scores (F (1, 209) = 4.56, p = .034).
Table 2.
Differences of least‐square means from repeated measures analyses of covariance
| Adjusted means across follow‐upa | ||||||
|---|---|---|---|---|---|---|
| Dependent variable | CBI | SI | Estimated differenceb | 95% CI | p | d c |
| STAXI‐2 | 41.42 | 47.09 | −5.67 | −10.32, −1.01 | .017 | −0.36 |
| Anger Index | ||||||
| OAS‐M | 1.00 | 1.14 | −0.14 | −0.33, 0.06 | .17 | −0.19 |
| Aggressiond | ||||||
| Outcome quest | 60.69 | 72.34 | −11.65 | −22.20, −1.09 | .031 | −0.49 |
| Total score | ||||||
| LIFE Global | 2.85 | 3.28 | −0.42 | −0.75, −0.09 | .011 | −0.54 |
| Social Func | ||||||
| LIFE Global | 2.78 | 3.04 | −0.26 | −0.63, 0.11 | .16 | −0.29 |
| Work Func | ||||||
| WHO QOL | 13.64 | 12.09 | 1.56 | 0.51, 2.60 | .004 | 0.50 |
| Psychological | ||||||
| CAPS severity | 22.56 | 24.71 | −2.15 | −7.37, 3.07 | .40 | −0.14 |
Abbreviations: CAPS, Clinician Rated PTSD Scale; LIFE, Longitudinal Interval Follow‐up Evaluation; OAS‐M, Overt Aggression Scale Modified; STAXI, State‐Trait Anger Inventory; WHO, World Health Organization.
Means are adjusted for BL scores and time effects.
A negative difference means that the adjusted mean for CBI is numerically lower than that for SI. For most measures, a higher score indicates higher severity/poorer functioning. Exceptions: WHO QOL.
Cohen's effect size d.
OAS‐M scores are log10 transformed.
Figure 2.
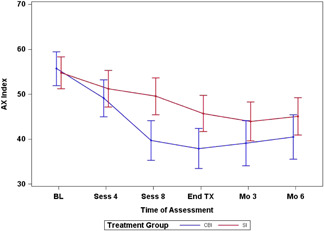
STAXI‐2 Anger Index by Treatment with 95% confidence intervals. AX, Anger Expression Index; CBI, cognitive behavioral intervention; SI, supportive intervention
Table 3.
Unadjusted means by treatment condition and between group effect sizes for all time points
| CBI | SI | |||||
|---|---|---|---|---|---|---|
| Measurea | Time | Mean | SD | Mean | SD | d b |
| STAXI‐2 AX | Baseline | 55.67 | 12.98 | 54.77 | 11.86 | 0.07 |
| Week 4 | 49.16 | 15.30 | 52.88 | 12.82 | −0.11 | |
| Week 8 | 40.33 | 17.95 | 49.61 | 13.89 | −0.48 | |
| End of TX | 37.50 | 16.68 | 46.00 | 13.64 | −0.39 | |
| Month 3 | 40.31 | 14.07 | 43.81 | 13.85 | −0.22 | |
| Month 6 | 42.06 | 15.27 | 44.61 | 14.20 | −0.21 | |
| OASM AGGc | Baseline | 1.335 | 0.525 | 1.396 | 0.500 | −0.12 |
| Week 4 | 1.234 | 0.486 | 1.285 | 0.541 | −0.02 | |
| Week 8 | 0.953 | 0.639 | 1.148 | 0.638 | −0.16 | |
| End of TX | 0.909 | 0.608 | 1.103 | 0.662 | −0.19 | |
| Month 3 | 0.908 | 0.448 | 1.024 | 0.728 | −0.06 | |
| Month 6 | 0.946 | 0.758 | 1.117 | 0.549 | −0.23 | |
| OQ total | Baseline | 82.73 | 27.04 | 89.71 | 22.59 | −0.28 |
| End of TX | 60.96 | 29.37 | 72.04 | 25.70 | −0.24 | |
| Month 3 | 56.76 | 28.19 | 76.55 | 26.64 | −0.57 | |
| Month 6 | 61.17 | 28.82 | 70.71 | 27.60 | −0.50 | |
| LIFE Social | Baseline | 3.57 | 0.54 | 3.64 | 0.71 | −0.11 |
| End of TX | 2.92 | 0.64 | 3.38 | 0.78 | −0.53 | |
| Month 3 | 2.95 | 0.78 | 3.27 | 0.78 | −0.39 | |
| Month 6 | 2.79 | 0.79 | 3.06 | 0.92 | −0.38 | |
| LIFE occupation | Baseline | 3.17 | 1.22 | 2.98 | 1.08 | 0.16 |
| End of TX | 2.88 | 0.88 | 3.21 | 1.07 | −0.38 | |
| Month 3 | 3.05 | 0.85 | 3.00 | 0.95 | −0.20 | |
| Month 6 | 2.84 | 0.90 | 2.71 | 0.97 | −0.09 | |
| WHO QOL psychological | Baseline | 11.54 | 3.17 | 10.97 | 2.61 | 0.20 |
| End of TX | 14.11 | 2.50 | 11.70 | 3.26 | 0.61 | |
| Month 3 | 13.92 | 2.32 | 11.39 | 3.30 | 0.43 | |
| Month 6 | 13.59 | 2.73 | 12.24 | 2.98 | 0.17 | |
| CAPS severity | Baseline | 30.02 | 10.62 | 32.38 | 9.52 | −0.21 |
| End of TX | 22.40 | 11.99 | 24.24 | 10.58 | −0.08 | |
| Month 3 | 22.37 | 12.73 | 24.93 | 12.54 | −0.16 | |
| Month 6 | 21.89 | 11.58 | 23.38 | 12.41 | −0.23 |
Abbreviations: CAPS, Clinician Rated PTSD Scale; LIFE, Longitudinal Interval Follow‐up Evaluation; OAS‐M AGG, Overt Aggression Scale Modified, Aggression Score; STAXI‐2 AX, State‐Trait Anger Inventory, Anger Index; TX, Treatment; WHO QOL, World Health Organization Quality of Life.
For most measures, a higher score indicates higher severity/poorer functioning. Exceptions: WHO QOL.
Negative effect size indicates larger effect for CBI, except for WHO QOLwhere positive effect size indicates larger effect for CBI.
OAS‐M scores are log10 transformed.
3.3. Secondary outcome measures
CBI also showed significantly more improvement than SI on the LIFE social adjustment global score (F (1, 95) = 6.49, p = .011), and on the QOL psychological domain score (F (1, 88) = 8.79, p = .004) (Table 2). Between group effects sizes across all time points were −0.54 for social functioning and 0.50 for QOL psychological score (Table 2), both favoring CBI. Differences were close to significance on the OQ total score (F (1, 77) = 4.83, p = .031), with more change in CBI (d = −0.49). The treatments did not differ significantly on the LIFE occupational functioning score (F (1, 95) = 1.96, p = .165) or on PTSD severity (F = 0.67, p = .40). Supplemental analyses of the OQ subscales showed more improvement for CBI only on the scale of the interpersonal relations (F (1, 83) = 5.35, p = .023); symptom distress and social role did not differ significantly. There were no significant differences on the other WHO QOL‐BREF subscales (physical, social, and environmental).
3.4. Outcome by PTSD diagnosis
There were no main effects for PTSD diagnosis (all p > .10) or significant interactions between PTSD diagnosis and treatment condition (all p > .28) for any of the outcome measures.
3.5. Supplementary analyses
Due to the significantly higher noncompletion rate in CBI, further analyses were conducted to rule out possible responder bias. GLM analyses examining termination (completer versus noncompleter), treatment condition, and the interaction of termination status and treatment condition were conducted for baseline scores on all primary and secondary outcome measures. There were no interactions close to significance, and examination of the mean scores of noncompleters showed no indication of higher severity for CBI versus SI noncompleters. Similar analyses were conducted for a measure completed at each treatment session (dimensions of anger reactions [DAR]; Forbes et al., 2004). All participants who started treatment had one or more DARs completed. Examining the last available DAR score for all participants showed a significant effect for treatment favoring CBI (F(1,86) = 5.79, p = .018), and for termination status (higher scores for non‐completers (F(1,86) = 10.93, p = .001). There were no significant differences between non‐completers in CBI and those in SI; the mean DAR score for CBI noncompleters (12.17, SD = 6.8) was numerically lower (less severe) than for SI (14.00, SD = 6.1).
4. DISCUSSION
The purpose of this study was to test the effectiveness of CBI in reducing anger and aggression, and secondarily in improving functioning and quality of life and reducing PTSD symptoms in veterans with post‐911 deployments. We found that compared to our active supportive intervention control, CBI had a significantly greater reduction in anger severity as measured by the STAXI‐2 index but did not differ in aggression as measured by the OAS‐M AGG score. Findings of superiority of CBI on the STAXI‐2 index are consistent with the two smaller RCTs of individually delivered cognitive behavioral therapy, including the pilot for the current study (Shea et al., 2013) and Chemtob et al. (1997) who tested an earlier version of the current treatment (Novaco, 1999).
Analyses of the subscales of the primary outcome measures showed that while the overall OAS‐M AGG score did not differ, CBI was superior to SI in reduction of number of aggressive outbursts, aggression toward objects, and on the global anger/aggression (GAA) score. The lack of difference on the overall AGG score was likely influenced by the very low endorsement rates on the OAS‐M subscale AA‐self (physically aggressive behaviors towards the self) at all time points. Coccoro (2020) also found the AGG score to be less sensitive to change than the GAA score and suggested it may be better to exclude AA‐self from the total aggression (AGG) score. On the STAXI‐2, although CBI scores decreased more than SI scores on all subscales, the difference was statistically significant only on the anger expression out scale, suggesting that CBI may have its strongest effects in reducing outward expression as opposed to inward experience of anger.
Findings from our secondary outcome measures showed the superiority of CBI for social functioning and psychological quality of life, and interpersonal functioning as measured by the OQ, but no treatment differences in occupational functioning, or improvement in PTSD symptoms. The findings for PTSD might have been expected, since not all the participants met the criteria for PTSD and, except for anger and hyperarousal, CBI does not focus specifically on PTSD symptoms. CBI was also found to be more effective than SI in reducing anger and improving social and interpersonal functioning and quality of life, irrespective of PTSD diagnosis. This is the first study to our knowledge that has examined whether PTSD affects outcomes of anger treatment and suggests that CBI is comparably effective for both groups. Given that anger problems have been shown to be the most frequently reported problem following return from deployment for OEF/OIF veterans with and without PTSD (Sayer et al., 2010), empirical support for CBI as an effective anger treatment is important for both groups. For those with PTSD, however, an important question is whether starting with a trauma‐focused treatment like prolonged exposure or cognitive processing therapy would provide broader benefits beyond improvement in anger.
Thirty‐seven percent of participants did not complete treatment. Prior studies have also shown that veterans with anger problems show poorer treatment engagement, lower session attendance, and higher rates of noncompletion (Morland et al., 2012; Rosen et al.,2001). Additionally, OEF/OIF veterans may have higher rates of dropout than veterans of other eras (Chard et al., 2010). Most notable, however, is that CBI participants were more than twice as likely to fail to complete treatment than those in SI (50% vs. 23%). The dropout rate was similarly high in the two prior studies of this treatment approach: 50% for Chemtob et al. (1997) and 42% for Shea et al. (2013) as well as in most other studies of cognitive‐behavioral treatments (Morland et al., 2012). In the current study, most dropouts from CBI (n = 11) stopped attending for unknown reasons and did not respond to outreach. Nine cited logistical problems such as transportation difficulties, childcare responsibilities, or lack of time due to increased demands of work, school, or parenting. SI was similar in terms of reasons for dropout, but with lower frequencies (seven unknown and three logistical problems).
The finding of significantly lower attrition for SI, which is an adapted version of PCT, is consistent with findings from several studies of cognitive‐behavioral trauma‐focused treatments that have used PCT as an active control (Belsher et al., 2019; Imel et al., 2013). SI contains the same elements of psychoeducation, support, and informal problem‐solving strategies as PCT. It might be assumed that higher drop‐out in trauma‐focused treatments is due to the focus on trauma, but the absence of a focus on trauma in CBI suggests other factors are likely involved. One difference between cognitive behavioral therapies more generally and both PCT and SI is the degree of structure in the sessions. PCT and SI are nondirective and allow the patient to determine the focus of sessions, in contrast to cognitive‐behavioral approaches that involve explicit agendas for each session. Homework requirements are considerably more demanding in CBT approaches and require high levels of motivation and treatment engagement, known to be lower in veterans with anger. Understanding whether these or other factors are associated with dropout in CBT approaches, and ways to ameliorate relevant factors might extend the efficacy of these treatments to a larger proportion of patients. Adding a motivational enhancement component may be one way to increase engagement (Murphy et al., 2002). Alternatively, it may be that some patients are not well suited for cognitive‐behavioral approaches; if so, being able to identify such patients and offer alternative approaches is important.
Strengths of this study include the randomized design, multiple assessment points, interviewers blinded to treatment condition, assessment of treatment adherence, and the use of an active control condition. SI was used to provide common therapeutic factors of therapy, including a rationale, psychoeducation, and therapist support, validation, and encouragement. Controlling for such factors that are known to influence outcome allows a strong test of the effects of the treatment's unique interventions.
Limitations include our low rate of women and racial minorities, reducing the generalizability of the findings to these important groups. Both groups are underrepresented in our recruitment settings, and despite our efforts to broaden or target recruitment sources (e.g., the women's primary care clinic), we were unsuccessful in achieving a more diverse sample. Since we focused only on post‐911 veterans who experienced warzone‐related trauma, the extent to which these findings apply to other veterans with anger problems is unknown. We should also note that the current study included veterans who were able to be treated on an outpatient basis. While our sample was quite similar to those of other published treatment trials of veterans treated for anger in the severity of symptoms and indicators of functional status (e.g., marital status, education level, and employment), veterans who require inpatient or residential treatment or who are incarcerated due to anger problems may need more intensive, longer‐term and/or alternative types of treatment. This is an important area for future study. Finally, the high dropout rate in CBI is a disappointment and perhaps a limitation, but at the same time is an outcome that warrants further investigation.
In conclusion, the present study provides evidence of the effectiveness of a specific cognitive‐behavioral psychotherapy for the treatment of anger problems in veterans who have deployed to a warzone. Despite high attrition, CBI was associated with significantly more improvement in anger as well as interpersonal aspects of functioning and quality of life. This study is unique in examining whether veterans with and without PTSD respond similarly, demonstrating that CBI is effective regardless of PTSD diagnosis. Further research is needed to determine if and how attrition can be reduced in veterans receiving cognitive‐behavioral treatments for anger.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENTS
This study was supported by Grant Number 5I01RX001146, from the Department of Veterans Affairs Rehabilitation Research and Development Program. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. Material has also been reviewed by the Walter Reed Army Institute of Research. There is no objection to its presentation and/or publication. The opinions or assertions contained herein are the private views of the author, and are not to be construed as official, or as reflecting true views of the Department of the Army or the Department of Defense. The investigators have adhered to the policies for protection of human subjects as prescribed in AR 70–25. We are grateful to the following persons who provided important contributions to the study: Laura Fabricant, Shauna L. Finley, Samantha Collum, Emily Gentes, Jennifer Primack, Sidney Brigido, and Mackay Kanaley.
Tracie Shea, M. , Stout, R. L. , Reddy, M. K. , Sevin, E. , Presseau, C. , Lambert, J. , & Cameron, A. (2022). Treatment of anger problems in previously deployed post‐911 veterans: A randomized controlled trial. Depression and Anxiety, 39, 274–285. 10.1002/da.23230
DATA AVAILABILITY STATEMENT
The data that support the findings of this study may be available upon reasonable request following all relevant regulations.
REFERENCES
- Adler, A. B. , Bliese, P. D. , McGurk, D. , Hoge, C. W. , & Castrol, C. A. (2009). Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: Randomization by platoon. Journal of Consulting and Clinical Psychology, 77(5), 928–940. 10.1037/a0016877 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (DSM‐5®). American Psychiatric Pub.
- Belsher, B. E. , Beech, E. , Evatt, D. , Smolenski, D. J. , Shea, M. T. , Otto, J. L. , Rosen, C. S. , & Schnurr, P. P. (2019). Present‐centered therapy (PCT) for post‐traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews, 2019(11), CD012898. 10.1002/14651858.CD012898.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chard, K. M. , Schumm, J. A. , Owens, G. P. , & Cottingham, S. M. (2010). A comparison of OEF and OIF veterans and Vietnam veterans receiving cognitive processing therapy. Journal of Traumatic Stress, 23, 25–32. 10.1002/jts.20500 [DOI] [PubMed] [Google Scholar]
- Chemtob, C. , Novaco, R. W. , Hamada, R. S. , & Gross, D. M. (1997). Cognitive‐behavioral treatment for severe anger in posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 65, 184–189. 10.1037/0022-006X.65.1.184 [DOI] [PubMed] [Google Scholar]
- Coccaro, E. (2020). The Overt Aggression Scale Modified (OAS‐M) for clinical trials targeting impulsive aggression and intermittent explosive disorder: Validity, reliability, and correlates. Journal of Psychiatric Research, 124, 50–57. 10.1016/j.jpsychires.2020.01.007 [DOI] [PubMed] [Google Scholar]
- Coccaro, E. F. , Harvey, P. D. , Kupsaw, L. E. , Herbert, J. L. , & Bernstein, D. P. (2000). Overt Aggression Scale‐Modified (OAS‐M). In American Psychiatric Association (Ed.), American Psychiatric Association Task Force for the Handbook of Psychiatric Measures (pp. 699–702). Washington DC: American Psychiatric Association. [Google Scholar]
- Cohen, J. (1992). A power primer. Psychological Bulletin, 122, 155–159. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Dempster, A. P. , Laird, N. M. , & Rubin, D. B. (1977). Maximum likelihood estimation from incomplete data via the EM algorithm. Journal of the Royal Statistical Society, Series B, 39, 1–38. 10.1111/j.2517-6161.1977.tb01600.x [DOI] [Google Scholar]
- Donahue, J. J. , Santanello, A. , Marsiglio, M. C. , & Van Male, L. M. (2017). Acceptance and commitment therapy for anger dysregulation with military veterans: A pilot study. Journal of Contemporary Psychotherapy, 47, 233–241. 10.1007/s10879-017-9361-z [DOI] [Google Scholar]
- Elgoben, E. G. , Aralis, H. , Cassiello‐Robbins, C. F. , Lester, P. , Saltzman, W. , & Barish, G. (2021). Integrating mobile technology and social support with cognitive behavioral therapy for anger in veterans with PTSD: A pilot study. Military Behavioral Health, 9(1), 17–26. [Google Scholar]
- Evans, L. , McHugh, T. , Hopwood, M. , & Watt, C. (2003). Chronic posttraumatic stress disorder and family functioning of Vietnam veterans and their partners. Australian and New Zealand Journal of Psychiatry, 37, 765–772. 10.1080/2Fj.1440-1614.2003.01267.x [DOI] [PubMed] [Google Scholar]
- Faes, C. , Molenberghs, G. , Aerts, M. , Verbeke, G. , & Kenward, M. G. (2009). The effective sample size and an alternative small‐sample degrees‐of‐freedom method. The American Statistician, 63(4), 389–399. 10.1111/j.2517-6161.1977.tb01600 [DOI] [Google Scholar]
- Forbes, D. , Hawthorne, G. , Elliott, P. , McHugh, T. , Biddle, D. , Creamer, M. , & Novaco, R. W. (2004). A concise measure of anger in combat‐related posttraumatic stress disorder. Journal of Traumatic Stress, 17, 249–256. 10.1080/21635781.2020.1768972 [DOI] [PubMed] [Google Scholar]
- Forbes, D. , Parslow, R. , Creamer, M. , Allen, N. , McHugh, T. , & Hopwood, M. (2008). Mechanisms of anger and treatment outcome in combat veterans with posttraumatic stress disorder. Journal of Traumatic Stress, 21, 142–149. 10.1002/jts.20315 [DOI] [PubMed] [Google Scholar]
- Gerlock, A. (1994). Veterans' responses to an anger management intervention. Issues in Mental Health Nursing, 16, 393–408. 10.3109/01612849409006916 [DOI] [PubMed] [Google Scholar]
- Grinker, R. R. , & Spiegel, J. P. (1945). Men Under Stress. Philadelphia: Blakiston. [Google Scholar]
- Imel, Z. E. , Laska, K. , Jakcupcak, M. , & Simpson, T. L. (2013). Meta‐analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 394–404. 10.1037/a0031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkstein, S. , Scott, J. C. , Smith, R. V. , & Cruz, J. (2018). Effectiveness of an anger control program among veterans with PTSD and other mental health issues: A comparative study. Journal of Clinical Psychology, 74, 1422–1430. 10.1002/jclp.22631 [DOI] [PubMed] [Google Scholar]
- Keller, M. B. , Lavori, P. W. , Friedman, B. , Nielson, E. , Endicott, J. , McDonald‐Scott, P. , & Andreason, N. C. (1987). The longitudinal interval follow‐up evaluation. Archives of General Psychiatry, 44, 540–548. 10.1001/archpsyc.1987.01800180050009 [DOI] [PubMed] [Google Scholar]
- Kulka, R. , Schlenger, W. E. , Fairbank, J. A. , Hough, R. L. , Jordan, B. K. , Marmar, C. R. , & Weiss, D. S. (1990). Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. Brunner/Mazel. [Google Scholar]
- Lambert, M. J. , Burlingame, G. M. , Umphress, V. , Hansen, N. B. , Vermeersch, D. A. , Clouse, G. C. , & Yanchar, S. C. (1996). The reliability and validity of the Outcome Questionnaire. Clinical Psychology & Psychotherapy: An International Journal of Theory and Practice. 3, 4(249–258). [Google Scholar]
- Lasko, N. B. , Gurvits, T. V. , Kuhne, A. A. , Orr, S. P. , & Pitman, R. K. (1994). Aggression and its correlates in Vietnam veterans with and without chronic posttraumatic stress disorder. Comprehensive Psychiatry, 35(5), 373–381. [DOI] [PubMed] [Google Scholar]
- Leon, A. C. , Solomon, D. A. , Mueller, T. I. , Turvey, C. L. , Endicott, J. , & Keller, M. B. (1999). The Range of Impaired Functioning Tool (LIFE–RIFT): A brief measure of functional impairment. Psychological Medicine, 29(4), 869–878. 10.1017/S0033291799008570 [DOI] [PubMed] [Google Scholar]
- Linkh, D. , & Sonnek, S. M. (2003). An application of cognitive‐behavioral anger management training in a military/occupational setting: Efficacy and demographic factors. Military Medicine, 168(6), 475–478. 10.1093/milmed/168.6.475 [DOI] [PubMed] [Google Scholar]
- Lloyd, D. , Nixon, R. D. V. , Varker, T. , Elliott, P. , Perry, D. , Bryant, R. A. , Creamer, M. , & Forbes, D. (2014). Comorbidity in the prediction of cognitive processing therapy treatment outcomes for combat‐related posttraumatic stress disorder. Journal of Anxiety Disorders, 28, 237–240. 10.1016/j.janxdis.2013.12.002 [DOI] [PubMed] [Google Scholar]
- Miles, S. R. , Dillon, K. H. , Jacoby, V. M. , Hale, W. J. , Dondanville, K. A. , Wachen, J. S. , Yarvis, J. S. , Peterson, A. L. , Mintz, J. , Litz, B. T. , Young‐McCaughan, S. , & Resick, P. A. (2020). Changes in anger and aggression after treatment for PTSD in active duty military. Journal of Clinical Psychology, 76, 493–507. 10.1002/jclp.22878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland, L. A. , Greene, C. J. , Rosen, C. S. , Foy, D. , Reilly, P. , Shore, J. , He, Q. , & Frueh, B. C. (2010). Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: A randomized noninferiority trial. Journal of Clinical Psychiatry, 71, 855–863. 10.4088/JCP.09m05604blu [DOI] [PubMed] [Google Scholar]
- Morland, L. A. , Love, A. R. , Mackintosh, M. , Greene, C. J. , & Rosen, C. S. (2012). Treating anger and aggression in military populations: research updates and clinical implications. Clinical Psychology: Science and Practice, 19, 305–302. 10.1111/cpsp.12007 [DOI] [Google Scholar]
- Murphy, R. T. , Rosen, C. S. , Cameron, R. P. , & Thompson, K. E. (2002). Development of a group treatment for enhancing motivation to change PTSD symptoms. Cognitive and behavioral practice, 9(4), 308–316. 10.1016/S1077-7229(02)80025-6 [DOI] [Google Scholar]
- Novaco, R. W. (1999). Stress inoculation treatment for anger control: therapist procedures (1993‐1994 Modifications) . National Centre for War‐related Posttraumatic Stress Disorder. [Google Scholar]
- Novaco, R. (2001). Stress inoculation therapy for anger control: therapist procedures . University of California. [Google Scholar]
- Raudenbush, S. W. , & Bryk, A. S. (2002). Hierarchical linear models: Applications and data analysis methods (volume 1). Sage Publications. [Google Scholar]
- Roberge, E. M. , Allen, N. J. , Taylor, J. W. , & Bryan, C. J. (2016). Relationship functioning in Vietnam veteran couples: The roles of PTSD and anger. Journal of Clinical Psychology, 72(9), 966–974. 10.1002/jclp.22301 [DOI] [PubMed] [Google Scholar]
- Rosen, C. S. , Adler, E. , & Tiet, Q. (2013). Presenting concerns of veterans entering treatment for posttraumatic stress disorder. Journal of Traumatic Stress, 26, 640–643. 10.1002/jts.21841 [DOI] [PubMed] [Google Scholar]
- Rosen, C. S. , Murphy, R. T. , Chow, H. C. , Drescher, K. D. , Ramirez, G. , Ruddy, R. , & Gusman, F. (2001). Posttraumatic stress disorder patients’ readiness to change alcohol and anger problems. Psychotherapy: Theory, Research, Practice, Training, 38(2), 233–244. 10.1037/0033-3204.38.2.233 [DOI] [Google Scholar]
- Sayer, N. A. , Noorbaloochi, S. , Frazier, P. , Carlson, K. , Gravely, A. , & Murdoch, M. (2010). Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatric Services, 61, 589–597. 10.1176/ps.2010.61.6.589 [DOI] [PubMed] [Google Scholar]
- Schnurr, P. P. , Friedman, M. J. , Engel, C. C. , Foa, E. B. , Shea, M. T. , Chow, B. K. , Resick, P. A. , Thurston, V. , Orsillo, S. M. , Haug, R. , Turner, C. , & Bernardy, N. (2007). Cognitive behavioral therapy for posttraumatic stress disorder in women. A randomized controlled trial. Journal of the American Medical Association, 297, 820–830. 10.1001/jama.297.8.820 [DOI] [PubMed] [Google Scholar]
- Schnurr, P. P. , & Lunney, C. A. (2019). Residual symptoms following prolonged exposure or present‐centered therapy in female veterans and soldiers. Depression and Anxiety, 36, 162–169. 10.1002/da.22871 [DOI] [PubMed] [Google Scholar]
- Shea, M. T. , Bernardy, N. , Howard, J. , Key, F. , & Lambert, J. Present Centered Therapy Manual. Unpublished manual, 2003.
- Shea, M. T. , Lambert, J. , & Reddy, M. K. (2013). A randomized pilot study of anger treatment for Iraq and Afghanistan Veterans. Behavior Research and Therapy, 51, 607–613. 10.1016/j.brat.2013.05.013 [DOI] [PubMed] [Google Scholar]
- Shea, M. T. , Lambert, J. , Reddy, M. K. , Presseau, C. , Sevin, E. , & Stout, R. L. (2018). Treatment of trauma related anger in operation enduring freedom, operation Iraqi Freedom, and Operation New Dawn veterans: Rationale and study protocol. Contemporary Clinical Trials Communications, 12, 26–31. 10.1016/j.conctc.2018.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout, P. E. , & Fleiss, J. L. (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428. 10.1037/0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- Skevington, S. M. , Lotfy, M. , & O'Connell, K. A. (2004). The World Health Organization's WHOQOL‐BREF quality of life assessment: Psychometric properties and results of the international field trail. A report from the WHOQOL group. Quality of Life Research, 13(2), 299–310. 10.1023/B:QURE.0000018486.91360.00 [DOI] [PubMed] [Google Scholar]
- Spielberger, C. D. (1999). STAXI‐2: State‐Trait Anger Expression Inventory‐2: Professional manual. Odessa (FL): Psychological Assessment Resources. [Google Scholar]
- Spielberger, C. D. (1999). STAXI‐2 Stait‐Trait Anger Expression Inventory‐2 Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc. [Google Scholar]
- Stout, R. , Wirtz, P. , Carbonari, J. P. , & Del Boca, F. (1994). Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, 12, 70–75. 10.15288/jsas.1994.s12.70 [DOI] [PubMed] [Google Scholar]
- Thomas, J. L. , Wilk, J. E. , Riviere, L. A. , McGurk, D. , Castro, C. A. , & Hoge, C. W. (2010). Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry, 67(6), 614–623. 10.1001/archgenpsychiatry.2010.54 [DOI] [PubMed] [Google Scholar]
- Weathers, F. W. , Bovin, M. J. , Lee, D. J. , Sloan, D. M. , Schnurr, P. P. , Kaloupek, D. G. , Keane, T. M. , & Marx, B. P. (2018). The Clinician‐Administered PTSD Scale for DSM–5 (CAPS‐5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei, L. J. (1978). An application of an urn model to the design of sequential controlled clinical trials. Journal of the American Statistical Association, 73, 559–563. [Google Scholar]
- Wilks, C. R. , Morland, L. A. , Dillon, K. H. , Mackintosh, M. A. , Blakey, S. M. , Wagner, H. R. , V. A., Mid‐Atlantic MIRECC Workgroup, & Elbogen, E. B. (2019). Anger, social support, and suicide risk in U.S. military veterans. Journal of Psychiatric Research, 109, 139–144. 10.1016/j.jpsychires.2018.11.026 [DOI] [PubMed] [Google Scholar]
- Wright, K. M. , Foran, H. M. , Wood, M. D. , Eckford, R. D. , & McGurk, D. (2012). Alcohol problems, aggression, and other externalizing behaviors after return from deployment: Understanding the role of combat exposure, internalizing symptoms, and social environment. Journal of Clinical Psychology, 68, 782–800. 10.1002/jclp.21864 [DOI] [PubMed] [Google Scholar]
- Lambert, M. J. , Finch, A. A. , Okiishi, J , Burlingame, G.M. , McKelvey, C. , & Reiseinger, C. W. (1997). Administration and scoring manual for the Outcome Questionnaire Short Form. Stevenson, MD: American Professional Credentialing Services, [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study may be available upon reasonable request following all relevant regulations.


