Abstract
Objective
To evaluate work‐related issues (WRIs) and their determinants in patients with axial spondyloarthritis (SpA) across Europe.
Methods
The European Map of Axial Spondyloarthritis is a cross‐sectional online survey (2017–2018) of unselected patients with self‐reported axial SpA from 13 European countries. Participants were classified as active or inactive members of the labor force according to the International Labor Organization standards. Those employed reported WRIs due to axial SpA in the past 12 months. Sociodemographic characteristics and patient‐reported outcomes were compared between patients with and without WRIs. Stepwise regression analysis was conducted to identify independent determinants of WRIs.
Results
The sample comprised 2,846 patients with axial SpA, 1,653 were active members of the labor force, 1,450 were employed, and of those employed, 67.7% reported at least 1 WRI. The most frequently reported WRIs were taking sick leave (56.3%), difficulty fulfilling working hours (44.6%), and missing work for doctor’s appointments (34.6%). Of the total sample, 74.1% declared that they had faced or would face difficulties finding a job due to axial SpA. Patients with WRIs were more often female, were less likely to be married or in a relationship, and had a higher educational level, poorer patient‐reported outcomes, and a greater prevalence of anxiety and depression. Multivariable regression showed that WRIs were associated with a higher Bath Ankylosing Spondylitis Disease Activity Index score (odds ratio [OR] 1.30 [95% confidence interval (95% CI) 1.16–1.45]) and the 12‐item General Health Questionnaire score (OR 1.15 [95% CI 1.09–1.22]), and were negatively associated with inflammatory bowel disease (OR 0.58 [95% CI 0.36–0.91]).
Conclusion
Approximately two‐thirds of employed patients experienced WRIs due to axial SpA. Association between disease activity and psychological distress with WRIs suggests the need to ensure that axial SpA patients receive the required support to cope with their working life.
INTRODUCTION
Axial spondyloarthritis (SpA) is a chronic inflammatory disease usually affecting the axial skeleton, including the sacroiliac and spinal joints. Currently, axial SpA comprises patients with nonradiographic axial SpA and radiographic axial SpA, also known as ankylosing spondylitis (1).
SIGNIFICANCE & INNOVATIONS.
This study presents data on a large sample of patients with axial spondyloarthritis (SpA) from 13 European countries, reducing territorial and cultural biases present in other published studies.
Traditionally, studies on rheumatic diseases have focused on the medical or clinical parameters, while this study focuses on patient‐reported outcomes, contributing to the growing interest in the scientific literature for the patient’s perspective.
To provide reliable and robust data on unemployment, we calculated the unemployment rate following the International Labor Organization standards on active and inactive populations, to compare the rate of unemployment in the countries to that of their respective general populations.
Additionally, to the best of our knowledge, this is the first study to report reliable unemployment rates of axial SpA patients of a group of countries that are not frequently the focus of research.
Axial SpA has a great impact on working life, a key sphere within overall quality of life. Previous studies have shown that persistent patterns of high disease activity among axial SpA patients are associated with loss of work productivity (2) and increased probability of work disability (3). Patients with axial SpA are also known to experience significant career development limitations as a result of their condition (4). Experiencing problems at work also predicts poor out‐of‐work functioning and psychological issues (5, 6). Certain psychosocial factors such as social deprivation, depression, anxiety, and reduced self‐efficacy are associated with increased presenteeism and absenteeism (7), thereby highlighting the bidirectional relationship between workplace and psychosocial functioning.
Access to health care is essential to avoid a progressive worsening of functional, work, and psychological and social health and the attendant consequences for the individual, society, and the economy. This fact is supported by the Assessment of SpondyloArthritis international Society/European Alliance of Associations for Rheumatology, which expressly recommend that work productivity loss should be taken into account when assessing the cost‐effectiveness of treatments (8).
Interactions between disease activity, psychosocial factors, and disruption of patients' working lives stimulate the focus on the development of comprehensive and holistic management for axial SpA (9). Consequently, evaluating the working life of patients with axial SpA in all respects is important: employment status, unemployment rates, and work‐related issues (WRIs), as well as the association of these problems with sociodemographic characteristics of patients and their patient‐reported outcomes. Unfortunately, methodologic differences when defining the employment ratio in different studies has led to inconsistent conclusions, often within the same population (7, 10, 11).
One of the objectives of the European Map of Axial Spondyloarthritis (EMAS) is to provide reliable and standard indicators, collected using the same methodology, on all aspects related to the lives of patients living with axial SpA, and further, to allow comparisons between countries across Europe (12). The aim of the present analysis was to assess the working life of patients with axial SpA, including WRIs and their determinants in Europe.
MATERIALS AND METHODS
The EMAS project is promoted by the Axial Spondyloarthritis International Federation and by the Spanish Federation of Spondyloarthritis Associations (CEADE). The project is led by the Health and Territory Research group of the University of Seville and a steering committee composed of patient representatives and internationally recognized rheumatologists and psychologists specialized in axial SpA.
Design and survey development
EMAS was an observational, cross‐sectional online survey of unselected patients self‐reporting as having axial SpA from Austria, Belgium, France, Germany, Italy, The Netherlands, Norway, Russia, Slovenia, Sweden, Switzerland, and the UK. The questionnaire was adapted from the Spanish Atlas of Axial Spondyloarthritis 2017 (13), a patient survey held from January to March 2016, promoted by Health and Territory Research and CEADE with the support of the Max Weber Institute and Novartis Farmacéutica Spain. Data from the Atlas of Axial Spondyloarthritis in Spain 2017 (14) were retrospectively added to the EMAS database.
The EMAS patient questionnaire included 108 items related to 12 different areas: sociodemographic and anthropometric characteristics, disability assessment, work life, daily life, lifestyle habits, diagnostic journey, health care resource utilization, treatment, comorbidities (including extraarticular manifestations), psychological health, disease outcomes, and patient disease‐related attitudes. The EMAS questionnaire was originally developed in Spanish and subsequently translated into English, followed by Dutch, French, German, Italian, Russian, Swedish, and Slovenian. Prior to the start of data collection, participating countries were asked to assess and modify questions for local relevance, with guidance to only make essential changes in order to maintain consistency on an international level.
Sample selection and recruitment
Detailed information on the design and procedures of the EMAS study can be found elsewhere (12). Briefly, European patients with a self‐reported clinician‐provided diagnosis of axial SpA (radiographic or nonradiographic), age ≥18 years, who had visited a health care professional for axial SpA in the 12 months prior to participation were included in the survey.
Participants were recruited between July 2017 and March 2018 by the global research agency Ipsos SA, formerly GfK, through their existing online panel. In Austria, France, Spain, Norway, Slovenia, Sweden, The Netherlands, Italy, Russia, and Switzerland, patient organizations also supported recruitment by distributing the survey to their associated members (Figure 1). All patients agreed to their participation through informed consent and were asked to provide explicit opt‐in consent prior to participating in the EMAS survey. Participant data were anonymized.
Figure 1.
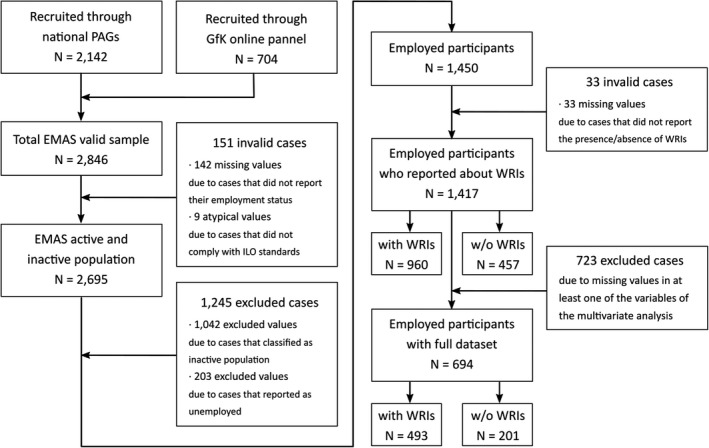
European Map of Axial Spondyloarthritis (EMAS) flow diagram of patient recruitment and selection. ILO = International Labor Organization; PAGs = patient advocacy groups; w/o = without; WRIs = work‐related issues.
Labor force and employment rates
Participants were asked about their employment status through a multiple‐choice question in which they could choose 1 option from the following: employed, unemployed, on temporary sick leave, on permanent sick leave, retired, early retirement, student, or homemaker. Using this information, patients were classified as part of the labor force (active population) or the economically inactive population according to the International Labor Organization standards (15, 16). Those considered active, or in the labor force, included the employed and unemployed of working age (15–64 years). Participants who reported being on temporary sick leave, permanent sick leave, retired, having taken early retirement, or being a student or homemaker were considered part of the inactive population. Figure 1 shows the sample selection process for the study data analysis. Employment and unemployment rates were calculated comparing employed and unemployed participants within the labor force.
Impact on working life
Those in employment were also asked to report WRIs due to axial SpA in the 12 months prior to participating in the EMAS survey via a yes/no question. Those reporting “yes” were asked to choose the WRIs applicable to them from the following list: 1) I asked for some days off/leave of absence, 2) I took sick leave, 3) I reduced my working hours, 4) I missed work only for the time my doctor’s appointment took, 5) It has been difficult for me to fulfill working hours, 6) I have occasionally changed my work shift, 7) My professional life has suffered (e.g., missed promotion), or 8) I had to give up my previous job.
Furthermore, all participants were asked the following yes/no questions: 1) Do you think it is or would be difficult for you to find a job because of your spondylitis/spondyloarthritis? 2) Do you think your current or past work choice was in any way determined by your spondylitis/spondyloarthritis?
Other patient‐reported outcomes
In addition, the following patient‐reported outcomes were also collected in the EMAS questionnaire (12).
Bath Ankylosing Spondylitis Disease Activity Index (BASDAI)
The BASDAI is a validated self‐administered questionnaire assessing disease activity in patients with axial SpA, capturing symptoms of fatigue, spinal pain, peripheral arthritis, enthesitis, and the intensity and duration of morning stiffness. Possible scores range from 0 (no activity) to 10 (maximum activity) (17).
Spinal Stiffness Index
This index assesses the self‐reported degree of stiffness experienced by patients in the spinal column, distinguishing between the cervical, dorsal, and lumbar areas. The index is the result of adding an unweighted degree of stiffness in these 3 spinal regions on a scale of lesser to greater effect (from 3 to 12): where a value of 3 would imply no stiffness, 4–6 mild stiffness, 7–9 moderate stiffness, and 10–12 significant stiffness. This index showed an acceptable internal reliability (Cronbach’s α = 0.79) (13).
Functional Limitation Index
This index, developed specifically for this study, assesses the degree of functional limitation in 18 daily life activities (dressing, bathing, showering, tying shoe laces, moving about the house, climbing stairs, getting out of bed, using the bathroom, shopping, preparing meals, eating, household tasks, walking down the street, using public transportation, driving, going to the doctor, doing physical exercise, and having intimate relations). The score is generated by adding the nonweighted degree of functional limitation of all activities, using a score of 0–3 (0 = no limitation, 1 = low limitation, 2 = medium limitation, and 3 = high limitation), with a total result between 0 and 54. Thus, a functional limitation value of 0–18 would imply low limitation, 18–36 medium limitation, and 36–54 high limitation. Cronbach’s α = 0.97, demonstrating excellent internal reliability (13).
12‐item General Health Questionnaire (GHQ‐12)
This questionnaire measures psychological distress, using 12 items (18), which are then transformed into a dichotomous score (0‐0‐1‐1) called the GHQ‐12 score. The cutoff point of 3 implies those experiencing a risk of psychological distress (19).
Statistical analysis
The sociodemographic variables included in this analysis were age, sex, educational level, marital status, and income level and patient‐reported outcomes including the BASDAI, spinal stiffness and functional limitation, the presence of both physical and psychological comorbidities, extraarticular manifestations such as uveitis and inflammatory bowel disease (IBD), and psychological distress as measured by the GHQ‐12.
The distribution of all variables was compared between patients with and without WRIs using Mann‐Whitney and chi‐square tests (for scale and categorical variables, respectively). A univariate logistic regression was carried out to explain the presence of the WRIs individually for each variable (including sociodemographic characteristics, patient‐reported outcomes, and psychological health). To identify independent determinants of WRIs, a multivariate stepwise regression analysis with candidate variables that showed an association with the WRIs in the univariate analysis was conducted.
RESULTS
Labor force
There were 2,846 participants in the EMAS survey, of which 2,704 reported their employment status. Nine patients were excluded from the analysis (making a total of 2,695) because they reported being employed or unemployed and age >65 years and therefore could not be considered as either part of the labor force or the inactive population following International Labor Organization classification. Of the selected sample, 1,653 (61.3%) were part of the labor force, while 1,042 (38.7%) were economically inactive. Among those inactive, 29.2% were on temporary sick leave, 28.0% on permanent sick leave, 22.1% retired, 10.9% homemakers, 5.7% students, and 4.1% on early retirement (Table 1). Approximately 90% of participants with axial SpA on sick leave, either temporary or permanent, declared that their condition was the cause of their employment status. Two‐thirds of early retired participants reported axial SpA as the cause for their retirement. Within the labor force, 1,450 (87.7%) were employed, and 203 (12.3%) unemployed.
Table 1.
Employment status of participants in the labor force and economically inactive population (n = 2,695)*
| Population, employment status | No. (%) |
|---|---|
| Active population (n = 1,653 [61.3%]) | |
| Employed | 1,450 (87.7) |
| Unemployed | 203 (12.3) |
| Total | 1,653 (100.0) |
| Inactive population (n = 1,042 [38.7%]) | |
| Temporary sick leave | 304 (29.2) |
| Permanent sick leave | 292 (28.0) |
| Retired | 230 (22.1) |
| Homemaker | 114 (10.9) |
| Student | 59 (5.7) |
| Early retirement | 43 (4.1) |
| Total | 1,042 (100.0) |
Based on International Labor Organization criteria, which define the active population or labor force as the sum of persons ages 15–64 years who are employed, plus those who are unemployed.
A total 65.3% of participants with axial SpA who were unemployed reported that the disease had been the main cause of their unemployment, compared to 34.7% who reported that it had not influenced their joblessness. Notably, unemployment rates across axial SpA patients in the labor force (n = 1,653) varied greatly between the different EMAS participating countries, ranging from 0.4% in Norway to 21.7% in Spain, with average values nearing 11.8%, as in France (Figure 2).
Figure 2.
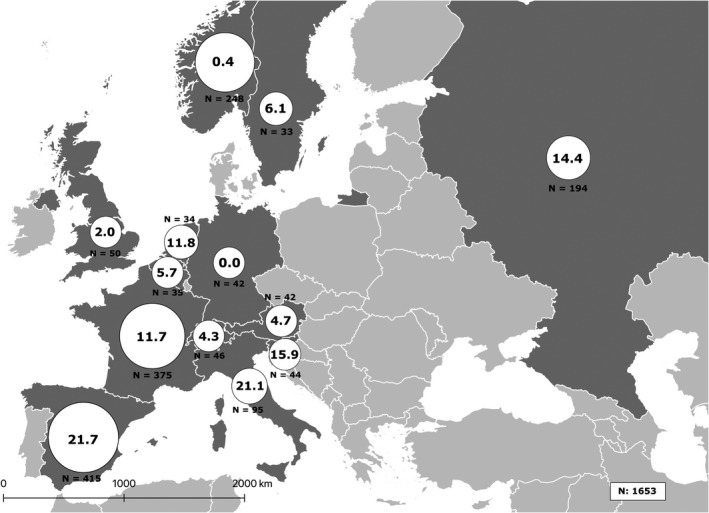
Unemployment rates reported by axial SpA patients in the labor force by country (n = 1,653).
WRI‐related issues and their determinants
Of all participants who were either part of the labor force (active population) or the inactive population (n = 2,695), 1,967 reported whether they had faced or would face difficulties finding a job due to axial SpA (1,457 [74.1%] declared “yes”). Additionally, participants were asked whether their present or past work choice was determined by their condition. In all, 45.1% (1,084 of 2,405 participants who answered the survey item) reported “yes.”
Of the 1,450 active and employed participants in the EMAS sample, 960 (67.7%) reported experiencing at least 1 WRI due to axial SpA in the past 12 months. Overall, 56.3% took sick leave, 44.6% had difficulties fulfilling working hours, 34% missed work due to doctor’s appointments, 31.6% requested days off, 25.7% reduced their working hours, 18.9% changed work shift occasionally, 16.7% saw their professional life suffer, and 8.8% had to give up a previous job because of their axial SpA.
Active and employed patients with WRIs were more often female, more likely to have obtained a university education, and less likely to be married or in a relationship compared to active and employed patients without WRIs. Those with WRIs had higher disease activity (BASDAI) and higher levels of spinal stiffness, functional limitation, and psychological distress (GHQ‐12). Furthermore, the presence of WRIs was associated with physical and psychological comorbidities (anxiety, depression). Patients with WRIs had a lower prevalence of IBD, while there was no difference in the prevalence of uveitis. No information on the presence of psoriasis was gathered across all of the EMAS‐participating countries (Table 2).
Table 2.
Association between sociodemographic characteristics, patient‐reported outcomes, and WRIs in active and employed participants*
| Variable |
WRIs (n = 960) |
Without WRIs (n = 457) |
P |
|---|---|---|---|
| Sociodemographic | |||
| Age, years | 41.2 ± 9.5 | 42.2 ± 10.3 | 0.085 |
| Male, no. (%) | 361 (37.6) | 218 (47.7) | <0.001 |
| Education level university, no. (%) | 584 (60.8) | 259 (56.7) | 0.002 |
| Married or with partner, no. (%) | 772 (80.8) | 377 (82.7) | 0.406 |
| Monthly income, € | 1,219.4 ± 944.3 | 1,196.7 ± 920.3 | 0.945 |
| Axial spondyloarthritis related | |||
| Disease duration, years | 15.0 ± 10.6 | 15.3 ± 10.8 | 0.666 |
| BASDAI (0–10) (n = 1,303) | 5.4 ± 1.8 | 4.0 ± 2.0 | <0.001 |
| Spinal Stiffness Index (3–12) (n = 1,349) | 7.5 ± 2.4 | 6.3 ± 2.5 | <0.001 |
| Functional Limitation Index (0–54) (n = 1,396) | 17.8 ± 15.4 | 16.5 ± 16.4 | 0.002 |
| GHQ‐12 (0–12) (n = 1,337) | 5.1 ± 4.0 | 2.6 ± 3.3 | <0.001 |
| Uveitis (n = 1,298), no. (%) | 168 (19.1) | 75 (17.9) | 0.581 |
| Inflammatory bowel disease (n = 982), no. (%) | 86 (13.0) | 64 (20.1) | 0.003 |
| Comorbidities, no. (%) | |||
| At least 1 physical comorbidity (n = 1,372)† | 570 (61.2) | 205 (46.6) | <0.001 |
| Anxiety (n = 1,361) | 298 (32.3) | 71 (16.2) | <0.001 |
| Depression (n = 1,364) | 241 (26.1) | 49 (11.1) | <0.001 |
Values are the mean ± SD unless indicated otherwise. BASDAI = Bath Ankylosing Spondylitis Disease Activity Index. GHQ‐12 = 12‐Item General Health Questionnaire; WRI = work‐related issues.
Physical comorbidities considered were any severe infections requiring antibiotics in the past 12 months, any severe infections requiring inpatient hospital admission, atherosclerosis, cataracts, coronary artery disease, diabetes mellitus, episcleritis, fibromyalgia, genital lesions, glaucoma, gout, heart failure, hypercholesterolemia, hypertension, irregular heartbeat, kidney failure, liver disease, obesity, pacemaker fitted, psoriasis, psoriatic arthritis, and spinal or other fractures.
The multivariate stepwise regression identified the following variables as an independent determinant of the WRIs in active and employed patients with axial SpA: higher BASDAI score (disease activity) and higher GHQ‐12 score (psychological distress) (Table 3). Notably, cases included in the regression analysis were slightly older, had longer disease duration, and were more likely to have at least 1 physical comorbidity as compared to those excluded because of missing values of the explanatory variables. However, both samples had similar sociodemographic characteristics and patient‐reported outcomes such as BASDAI or GHQ‐12 scores.
Table 3.
Univariate and multivariate stepwise logistic regression of the association between sociodemographic characteristics, patient‐reported outcomes, and WRIs in active and employed participants*
| Variable | Univariate logistic regression | Multivariate stepwise logistic regression |
|---|---|---|
| Age | 0.99 (0.98–1.00) | NA |
| Female | 1.51 (1.21–1.90)† | 0.81 (0.61–1.08) |
| Education level, university | 1.27 (1.07–1.50)† | NA |
| Marital status, married or with partner | 0.88 (0.66–1.18) | NA |
| Monthly income, € | 1.00 (1.00–1.00) | NA |
| BASDAI (0–10) | 1.46 (1.36–1.56)† | 1.30 (1.16–1.45)† |
| Spinal Stiffness Index (3–12) | 1.22 (1.16–1.28)† | 0.96 (0.89–1.04) |
| GHQ‐12 (0–12) | 1.21 (1.16–1.25)† | 1.15 (1.08–1.22)† |
| Functional Limitation Index (0–54) | 1.01 (1.00–1.01) | 0.99 (0.98–1.01) |
| Uveitis | 1.09 (0.81–1.47) | 0.88 (0.56–1.39) |
| Inflammatory bowel disease | 0.59 (0.41–0.84)† | 0.58 (0.36–0.91)† |
| Any physical comorbidities | 1.81 (1.44–2.27)† | 0.98 (0.67–1.43) |
| Anxiety | 2.47 (1.85–3.29)† | 1.28 (0.76–2.14) |
| Depression | 2.83 (2.03–3.94)† | 0.99 (0.55–1.77) |
Values are the odds ratio (95% confidence interval). BASDAI = Bath Ankylosing Spondylitis Disease Activity Index; GHQ‐12 = 12‐item General Health Questionnaire; NA = not applicable; WRIs = work‐related issues.
Statistically significant.
DISCUSSION
The unemployment ratio of EMAS survey participants (12.3%) was almost double that of the European Union–28 zone for the year 2017 (6.8%), according to Eurostat (20). This trend is supported by other studies that compare employment rates and absenteeism in patients with axial SpA to those of the general population (21). Despite the general trend for the whole of Europe indicated in this study, highlighting the disparity across the labor market in participating EMAS countries is important, with Mediterranean countries showing higher unemployment rates than those of Central and Northern Europe. As being unemployed is associated with worse health outcomes for patients with axial SpA, both in their physical and psychosocial health status (7, 22) as well as their financial status, this situation points to the importance of national policies to prevent harmful consequences associated with diseases such as axial SpA.
Some studies have reported that the rate of withdrawal from work is 3 times higher among patients with axial SpA than in the general population (23). The fact that more than one‐half of EMAS participants of the inactive population reported either being on temporary or permanent sick leave reinforces the significant individual disability burden caused by axial SpA and its associated economic cost to society.
Furthermore, nearly two‐thirds of the active employed population with axial SpA reported WRIs due to axial SpA. In more than one‐half of the cases, patients took sick leave, approximately one‐third missed work because of doctor appointments, one‐fourth indicated that they had reduced their working hours, and nearly one‐half reported difficulties in fulfilling working hours. These data support the fact that axial SpA is a disease that impacts significantly on working life, producing a variety of problems regarding absenteeism and presenteeism, compromising work productivity, and involving substantial direct and indirect costs to society (21).
Worse patient‐reported outcomes, both physical and psychological, were associated with WRIs. In particular, higher disease activity as assessed by the BASDAI, and a higher level of psychological distress reflected by GHQ‐12 scores, were identified as 2 independent predictors of WRIs in the multivariate regression analysis. Given the extensive research on the subject (2, 4), the role of psychological distress (GHQ‐12), which emerged as an important factor closely behind disease activity, is insufficiently explored (9). The relationship between physical and psychological health is complex and most likely bidirectional (24). In fact, an association between the BASDAI and GHQ‐12 has been found in other studies (25). Most probably, disease activity by itself facilitates the triggering of WRIs while generating enough psychological distress to lead to greater WRIs.
Interestingly, the presence of IBD was negatively associated with the presence of WRIs, which may be related to a higher probability of being treated with biologic therapies in the presence of IBD, which could have had a positive impact on axial SpA activity. However, since no detailed information on current treatment was gathered, this possibility remains conjecture.
The present findings highlight the need for a holistic and interdisciplinary approach to axial SpA and related conditions in European countries, where health care should not focus solely on the clinical treatment of the disease. Stakeholders should recognize that patients with axial SpA take the disease to work and into their family and social life, all of which are also affected by it (26). Caring about the working life of axial SpA patients, providing workplace adaptations, and ensuring flexibility at work will lead to better health outcomes and ultimately a higher quality of life for those with this chronic condition.
This study is not without limitations. First, we acknowledge that it did not use previously validated scales or indices in assessing the impact on work or functional impairment. The decision was taken during the preliminary phase of the survey development, when patients expressed concern about the limitations of existing measures that did not capture all aspects of their disease; therefore, the survey questions may reflect other, but relevant, issues for the patients not reported in previous studies. Second, the study may be subject to sample bias, since data from some countries concentrated a high percentage of the total participants, such as Spain, France, or Norway. In any case, these countries represent a wide range of possible unemployment outcomes in Europe, so this effect is probably counter‐weighted. Furthermore, a higher proportion of female participants in some countries might reflect a higher proportion of female members in the patient organization and not necessarily in the axial SpA population.
Approximately 50% of the patients were excluded from the multivariable analysis due to missing values of those variables included in the model, which represents another potential source of a sample bias. At the same time, the main sociodemographic characteristics and patient‐reported outcome parameters were similar across excluded and included patients, which makes the risk of the bias rather low. Finally, despite the bidirectional nature of associations reported, another limitation of this study is the inability to establish causality using this cross‐sectional approach. In fact, assessing the cause of WRIs is difficult, whether due to the problems related to the disease, the underlying inflammatory processes, or other factors associated with this chronic pathology (spinal stiffness or functional limitations in daily life). We can only conclude that relationships exist between these variables. To establish causality, we would need to carry out longitudinal studies regarding the evolution of physical and psychological variables and their relationship to work productivity or vice versa. Finally, the possible effect of pharmacologic treatments on work productivity could have influenced the results of our study in ways we had not anticipated.
Axial SpA has a substantial impact on working life, with disease‐associated WRIs reported by two‐thirds of the active employed population in this study. High disease activity and significant levels of psychological distress were 2 major independent determinants of WRIs. Overall, there is a need for a holistic approach to axial SpA care to ensure that patients have the support needed to remain part of the workforce and retain autonomy over their professional future.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Garrido‐Cumbrera had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Garrido‐Cumbrera, Bundy, Navarro‐Compán, Makri, Mahapatra, Delgado‐Domínguez, Poddubnyy.
Acquisition of data
Garrido‐Cumbrera, Bundy, Navarro‐Compán, Makri, Sanz‐Gómez, Christen, Mahapatra, Delgado‐Domínguez, Poddubnyy.
Analysis and interpretation of data
Garrido‐Cumbrera, Bundy, Navarro‐Compán, Makri, Sanz‐Gómez, Christen, Mahapatra, Delgado‐Domínguez, Poddubnyy.
ROLE OF THE STUDY SPONSOR
Novartis Pharma AG had no role in the study design or in the collection, analysis, or interpretation of the data, the writing of the manuscript, or the decision to submit the manuscript for publication. Publication of this article was not contingent upon approval by Novartis Pharma AG.
Supported by Novartis Pharma AG.
Dr. Garrido‐Cumbrera has received honoraria from Novartis Pharma AG (less than $10,000). Dr. Bundy has received honoraria from Novartis Pharma AG, AbbVie, Celgene, Janssen, Eli Lilly and Company, Novartis, and Pfizer (less than $10,000 each). Dr. Navarro‐Compán has received honoraria from Novartis Pharma AG, AbbVie, Bristol Myers Squibb, Eli Lilly and Company, MSD, Novartis, Pfizer, Roche, and UCB (less than $10,000 each). Dr. Makri has received honoraria from Novartis Pharma AG, Bayer, and GlaxoSmithKline (less than $10,000 each). Mr. Sanz‐Gómez has received honoraria from Novartis Pharma AG (less than $10,000). Ms. Christen has received honoraria from Novartis Pharma AG (less than $10,000). Dr. Mahapatra has received honoraria from Novartis Pharma AG (less than $10,000). Dr. Delgado‐Domínguez has received honoraria from Novartis Pharma AG (less than $10,000). Dr. Poddubnyy has received honoraria from Novartis Pharma AG, AbbVie, Bristol Myers Squibb, Celgene, Janssen, Eli Lilly and Company, MSD, Novartis, Pfizer, Roche, and UCB (less than $10,000 each) and has received research grants from AbbVie, MSD, Novartis, and Pfizer. No other disclosures relevant to this article were reported.
REFERENCES
- 1. Sieper J, Poddubnyy D. Axial spondyloarthritis. Lancet 2017;390:73–84. [DOI] [PubMed] [Google Scholar]
- 2. Espahbodi S, Bassett P, Cavill C, Freeth M, Hole J, Sengupta R. Fatigue contributes to work productivity impairment in patients with axial spondyloarthritis: a cross‐sectional UK study. Clin Exp Rheumatol 2017;35:571–8. [PubMed] [Google Scholar]
- 3. Molto A, Tezenas du Montcel S, Wendling D, Dougados M, Vanier A, Gossec L. Disease activity trajectories in early axial spondyloarthritis: results from the DESIR cohort. Ann Rheum Dis 2017;76:1036–41. [DOI] [PubMed] [Google Scholar]
- 4. Ramonda R, Marchesoni A, Carletto A, Bianchi G, Cutolo M, Ferraccioli G, et al. Patient‐reported impact of spondyloarthritis on work disability and working life: the ATLANTIS survey. Arthritis Res Ther 2016;18:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Haglund E, Petersson IF, Bremander A, Bergman S. Predictors of presenteeism and activity impairment outside work in patients with spondyloarthritis. J Occup Rehabil 2015;25:288–95. [DOI] [PubMed] [Google Scholar]
- 6. Hooge M de, Ramonda R, Lorenzin M, Frallonardo P, Punzi L, Ortolan A, et al. Work productivity is associated with disease activity and functional ability in Italian patients with early axial spondyloarthritis: an observational study from the SPACE cohort. Arthritis Res Ther 2016;18:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Healey EL, Haywood KL, Jordan KP, Garratt A, Packham JC. Impact of ankylosing spondylitis on work in patients across the UK. Scand J Rheumatol 2011;40:34–40. [DOI] [PubMed] [Google Scholar]
- 8. Van der Heijde D, Ramiro S, Landewé R, Baraliakos X, Van Den Bosch F, Sepriano A, et al. 2016 update of the ASAS‐EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 2017;76:978–91. [DOI] [PubMed] [Google Scholar]
- 9. Packham J. Optimizing outcomes for ankylosing spondylitis and axial spondyloarthritis patients: a holistic approach to care. Rheumatology (Oxford) 2018;57:vi29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chorus AM, Boonen A, Miedema HS, van der Linden S. Employment perspectives of patients with ankylosing spondylitis. Ann Rheum Dis 2002;61:693–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Montacer Kchir M, Mehdi Ghannouchi M, Hamdi W, Azzouz D, Kochbati S, Saadellaoui K, et al. Impact of the ankylosing spondylitis on the professional activity. Jt Bone Spine 2009;76:378–82. [DOI] [PubMed] [Google Scholar]
- 12. Garrido‐Cumbrera M, Poddubnyy D, Gossec L, Gálvez‐Ruiz D, Bundy C, Mahapatra R, et al. The European Map of Axial Spondyloarthritis: capturing the patient perspective. An analysis of 2846 patients across 13 countries. Curr Rheumatol Rep 2019;21:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garrido‐Cumbrera M, Navarro‐Compán V, Zarco P, Collantes‐Estévez E, Gálvez‐Ruiz D, Braçe O, et al. Atlas of axial spondyloarthritis in Spain 2017: study design and population. Reumatol Clin 2019;15:127–32. [DOI] [PubMed] [Google Scholar]
- 14. Garrido Cumbrera M, Gálvez Ruiz D, Chacón García J, Braçe O, Villoro Valdés R, Merino Ventosa M, et al. Atlas of axial spondyloarthritis in Spain 2017: profile of the disease. Heidelberg: Max Weber Institute; 2017. [Google Scholar]
- 15. International Labour Organization . Labour force. 2019. URL: https://www.ilo.org/global/statistics‐and‐databases/statistics‐overview‐and‐topics/WCMS_470304/lang‐‐en/index.htm.
- 16. Pasteels JM. ILO Projections of the economically active population: revised methodology of the 2011 edition. 2012. URL: https://www.ilo.org/wcmsp5/groups/public/‐‐‐dgreports/‐‐‐stat/documents/publication/wcms_213752.pdf.
- 17. Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 1994;21:2286–91. [PubMed] [Google Scholar]
- 18. Goldberg DP, Williams P. A user’s guide to the General Health Questionnaire. Berkshire (UK): NFER‐Nelson; 1988. [Google Scholar]
- 19. Cano A, Sprafkin RP, Scaturo DJ, Lantinga LJ, Fiese BH, Brand F. Mental health screening in primary care: a comparison of 3 brief measures of psychological distress. Prim Care Companion J Clin Psychiatry 2001;3:206–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. EUROSTAT . Employment statistics. 2018. URL: http://ec.europa.eu/eurostat/statistics‐explained/index.php/Employment_statistics.
- 21. Boonen A. A review of work‐participation, cost‐of‐illness and cost‐effectiveness studies in ankylosing spondylitis. Nat Clin Pract Rheumatol 2006;2:546–53. [DOI] [PubMed] [Google Scholar]
- 22. Marengo MF, Schneeberger EE, Citera G, Cocco JA. Work status among patients with ankylosing spondylitis in Argentina. J Clin Rheumatol 2008;14:273–7. [DOI] [PubMed] [Google Scholar]
- 23. Boonen A, van der Linden SM. The burden of ankylosing spondylitis. J Rheumatol Suppl 2006;78:4–11. [PubMed] [Google Scholar]
- 24. Jang JH, Green CE, Assassi S, Reveille JD, Ward MM, Weisman MH, et al. The contribution of disease activity on functional limitations over time through psychological mediators: a 12‐month longitudinal study in patients with ankylosing spondylitis. Rheumatology (Oxford) 2011;50:2087–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Garrido‐Cumbrera M, Delgado‐Domínguez CJ, Gálvez‐Ruiz D, Blanch Mur C, Navarro‐Compán V. The impact of axial spondyloarthritis on mental health: results from the Atlas. J Rheumatol 2019;46:1284–9. [DOI] [PubMed] [Google Scholar]
- 26. Ward MM, Reveille JD, Learch TJ, Davis JC Jr, Weisman MH. Impact of ankylosing spondylitis on work and family life: comparisons with the US population. Arthritis Rheum 2008;59:497–503. [DOI] [PubMed] [Google Scholar]


