Abstract
Purpose
This study aimed to investigate the effect of orthokeratology (OK) on accommodative function and aberrations, to explore the correlations between them and determine what role they play in myopia control.
Methods
In this prospective case‐controlled study, 61 children were divided into an OK (n = 30) and a single‐vision spectacles (SVS) (n = 31) group. Accommodation and ocular wavefront aberrations in the OK group were measured at baseline and after 1, 3, 6, 9 and 12 months of OK wear, and again at 1 month after stopping OK (13th month). The same procedure was performed in the SVS group at baseline and at 3, 6 and 12 months. Axial length (AL), accommodative lag area and aberrations including spherical aberration (SA), coma and total higher‐order aberrations (HOAs) were analysed.
Results
During OK wear, the accommodative lag area at each visit was lower than the baseline level (all p < 0.01); all aberrations at each visit were higher than pre‐treatment (all p < 0.001). After 1 month of OK treatment, changes in accommodative lag area and SA did not show significant correlation (p = 0.16), but after OK cessation these changes were correlated (p = 0.01). In the OK group, multivariate regression analysis showed changes in accommodative lag area were associated with AL progression in the first 6 months but not in the 1‐year analysis. For the SVS group, there were no significant changes in the accommodative lag area or any aberrations during the study period.
Conclusions
Increased HOAs and improved accommodative accuracy were observed during OK treatment, but began to regress after the cessation of OK. A significant positive correlation between improved accommodative accuracy and slowed axial elongation was only observed during the first 6 months of treatment.
Keywords: aberrations, accommodation, myopia progression, orthokeratology
Key points:
This study aimed to explore the association between accommodative function and aberrations during orthokeratology (OK) treatment for myopia control.
Accommodative accuracy improved during OK, but regressed after the cessation of treatment. Spherical aberration also tended to revert towards pre‐treatment levels.
An association between improved accommodative accuracy and retarded axial elongation was observed during the initial 6 months of OK wear.
INTRODUCTION
While myopia is a global health concern, the prevalence of myopia in East Asian countries is the highest in the world. 1 , 2 In China, up to 90% of teenagers and young adults are myopic. 3 By the year 2050, 49.8% of the world's population will have myopia and 9.8% will have high myopia. 4 High myopia increases the risk of developing blinding complications such as retinal detachment, glaucoma and other deleterious conditions. 5 To reduce the prevalence of high myopia, it is imperative to slow the progression of myopia in children.
Orthokeratology (OK) is one of the most effective interventions for slowing myopia progression in children. 6 A meta‐analysis reported that OK could reduce axial elongation by an estimated 0.19 mm per year compared to conventional single‐vision spectacles (SVS). 7 Thus, because of the effectiveness of OK, it is well accepted as a clinical treatment modality.
Peripheral hyperopic defocus has been implicated as a contributor to myopia progression. 8 Accommodative lag has also been regarded as a risk factor for myopia progression, as it produces hyperopic defocus, 8 , 9 but this relationship remains controversial given the findings of longitudinal studies exploring the relationships between accommodative lag and myopia progression. 10 , 11 , 12 Some researchers observed that accommodative accuracy improved after OK treatment and proposed that it plays a role in myopia control by reducing hyperopic defocus. 13 , 14 , 15 , 16 , 17 However, there are no longitudinal studies to explore the possible effects of these accommodative changes on myopia control in OK‐treated eyes.
In addition to improving accommodation, corneal reshaping by OK increases corneal and ocular higher‐order aberrations (HOAs), principally coma and spherical aberration (SA). 18 , 19 However, greater changes in corneal SA were observed than ocular SA; thus it was considered that accommodation might compensate for corneal aberrations. 19 For example, Batres et al. believed changes in internal aberration were linked to increases in the accommodative response; however, they did not find a significant correlation between changes in internal aberration and the increases in accommodative response. 20 Other longitudinal studies have investigated the impact of HOAs on axial growth although no consensus was achieved. 21 , 22
To date, any associations between accommodative accuracy and ocular higher‐order aberrations (such as coma, SA, total HOAs) in patients treated with OK are unclear. This study aimed to compare the effects of OK lenses versus SVS on accommodative accuracy and ocular HOAs in myopic children, and to determine the role of each during myopia control.
METHODS
Subjects and study design
This analysis was conducted on data derived from a single‐site, 1‐year, prospective, non‐randomized, non‐masked myopia control clinical trial. Myopic children (n = 61) were recruited from the Eye Hospital of Wenzhou Medical University, China. Inclusion criteria required subjects to be between 8 and 13 years old, with spherical refraction between −1.00 and −5.00 D, astigmatism not more than 0.75 D, anisometropia less than 1.00 D and monocular best spectacle‐corrected visual acuity of 0.10logMAR (6/7.5) or better. Exclusion criteria were a history of strabismus or binocular vision abnormalities and ocular or systemic disease. Patients with a previous history of myopia control were also excluded. According to the personal willingness of the children and their guardians, 30 children were fitted with OK lenses (Emerald series; Euclid, euclidsys.com), and 31 received SVS. Children were instructed to wear the OK lenses for at least 8 h at night, or in the case of the SVS group, to wear them during the day. After initial enrolment, subjects in the OK group were assessed at baseline (before wearing the OK lenses), 1, 3, 6, 9 and 12 months, and at 1 month (13th month) after OK discontinuance. Subjects in the SVS group were assessed at baseline, 3, 6 and 12 months. Ophthalmic examinations were performed at each follow‐up visit. In the OK group, measurements were recorded within 3 h of lens removal. Additionally, all measurements were completed in the morning. This was a prospective case‐controlled study that followed the tenets of the Declaration of Helsinki, was approved by the Ethics Committee of the Eye Hospital (KYK [2016]38), and registered with the Chinese Clinical Trial Registry (ChiCTR1800018564). Written assent and informed consent were obtained from the children and their parents or guardians before participation.
Measurements
Ophthalmic examinations in each group included subjective refraction and slit‐lamp observation by an experienced optometrist. Monocular uncorrected visual acuity was measured first to ensure good correction by the OK lenses. This was followed by subjective over‐refraction. Accommodation measurements were performed under monocular viewing conditions. In the OK group, accommodation of subjects was measured at baseline and at the last visit (1 month after OK discontinuance) using trial frames with full correction; however, accommodation was measured unaided for other follow‐up visits. All accommodation measurements in the SVS group were performed on the right eye while wearing trial frames with full correction. Details of the accommodative stimulus‐response curves (ASRC) measurements and calculation methods, such as vertex correction, were described previously. 23 A modified Badal system mounted on the Grand Seiko autorefractor (WAM‐5500; Grand Seiko, grandseiko.com) provided a wide and continuous range of accommodative stimuli (−1.61 D to approximately +14.83 D). 23 Subjects were required to fixate on a 3*3 array of 6/9 “E” letters at 4.5‐metre during the examination. The accommodative response was measured with the WAM‐5500 at a sampling speed of 5 Hz and recorded by the lab computer software. Three repeated measurements were obtained from the right eye of each subject over a stimulus range between −1.61 D and +14.83 D (Figure 1). The ASRC was fitted with a 3‐D polynomial equation, and the one with the highest R 2 value was chosen for analysis. The accommodative lag area was calculated as the area between the 1:1 line from 0 D to 6 D and the ASRC over the same stimulus range (Figure 1).
FIGURE 1.
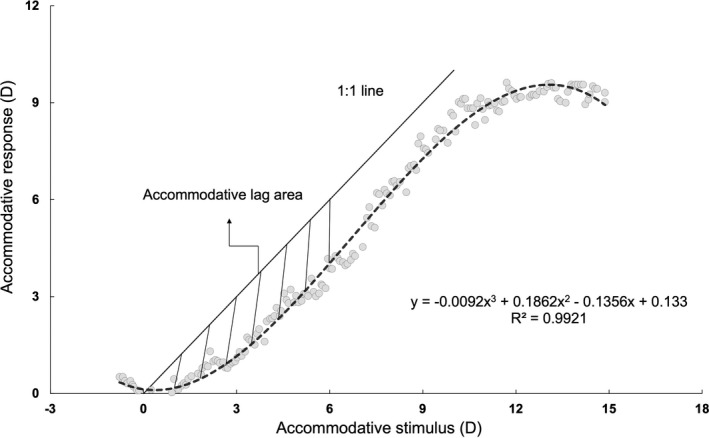
Representative example of a child's accommodative stimulus‐response curve and accommodative lag area. The curve was fitted with a 3‐D polynomial equation (dashed line). The solid black line indicates the 1:1 response to the accommodative stimulus. The shaded area represents the accommodative lag area between the dashed line and the solid line from 0 to 6 D Badal stimulus. D, dioptre
Ocular wavefront aberration analysis was performed through the natural pupils in a dark room using the Wavefront Analysis‐Supported Customized Ablation system (WASCA; Carl Zeiss Meditec, zeiss.com). Measurements were repeated at least three times from the right eye of each subject, and the three best‐focused images were chosen and averaged for analysis. All data were analysed up to the 7th order with a 4‐mm pupil diameter. SA ( and combined), coma ( combined) and HOAs (3rd to 7th orders) were evaluated and compared. 22
Measurements under cycloplegia were carried out at baseline, 6 months and at the last visit in both groups (13 and 12 months for the OK and SVS group, respectively). Thirty minutes after instillation of one drop of 0.5% proparacaine and two drops of 1% cyclopentolate administered 5 min apart, three measurements of spherical equivalent refractive error (SER) were obtained using the WAM‐5500, and measurements of axial length (AL) were obtained with the Lenstar LS 900 (Haag‐Streit, haag‐streit.com).
Statistical analysis
Data were calculated as means (standard deviation) and analysed using statistical software (SPSS version 24.0; IBM, ibm.com). Unpaired t‐tests were used to compare baseline data between groups. Differences in the gender ratio between groups were assessed with the Chi‐square test. Repeated measures analysis of variance (ANOVA) was performed to test changes in accommodation and aberrations followed by post‐hoc, least significant difference tests between baseline and the follow‐up visits. Associations between the changes in accommodation and aberrations over time were analysed by Pearson correlation. Univariate and multivariate regression analyses were used to evaluate factors associated with axial elongation in both groups. Variables with a p value ≤0.10 in the univariate analysis were included in the stepwise multivariate analysis. The statistical significance threshold was set at p < 0.05.
RESULTS
Changes in axial length (AL) and spherical equivalent refraction (SER)
At baseline, there were no significant differences between the OK and SVS groups for age, gender, SER and axial length (Table 1). After 1 year, the mean (SD) change in AL for the OK group, i.e., 0.28 (0.17) mm, was 24% smaller than the value for the SVS group of 0.37 (0.18) mm (t = −2.15, p = 0.04). The change in SER for the OK group, −0.37 (0.42) D, was 47% lower than that of the control group −0.70 (0.42) (t = 3.32, p < 0.01).
TABLE 1.
Baseline characteristics of subjects in the OK and SVS groups
| Parameters | OK | SVS | p Value |
|---|---|---|---|
| Total | N = 30 | N = 31 | |
| Age (y) | 10.3 (1.3) | 10.1 (1.0) | 0.53 |
| Gender, Male/Female | 13/17 | 17/14 | 0.37 |
| SER (D) | −2.63 (0.71) | −2.69 (0.71) | 0.73 |
| Axial length (mm) | 24.88 (0.91) | 24.83 (0.70) | 0.79 |
Figures in brackets indicate 1 standard deviation.
D, dioptre; OK, orthokeratology; SER, spherical equivalent refraction; SVS, single‐vision spectacles; y, years of age.
Accommodative function over time
The accommodative lag area for the OK group showed significant changes over time (ANOVA, F(1,29) = 906.30, p < 0.001). The 1‐month follow‐up findings were significantly lower than baseline (t‐test, p < 0.001) as was the case at each subsequent visit (t‐test, all p < 0.05, Figure 2a). After ceasing OK treatment, accommodative lag area increased but still did not reach the baseline value (t‐test, p < 0.01). In the SVS group, accommodation was stable throughout the study period (ANOVA test, F(1,30) = 1515.09, p = 0.26, Figure 2b).
FIGURE 2.
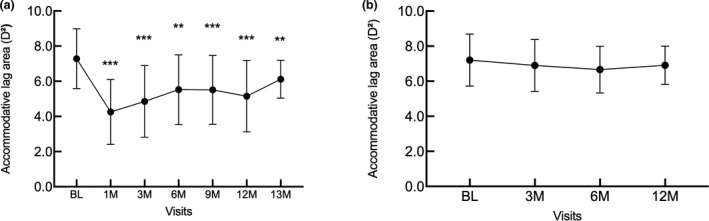
Accommodative lag area over time in the OK (a) and SVS groups (b). OK, orthokeratology; SVS, single‐vision spectacles; D, dioptre; M, months; BL, baseline; Error bars indicate one standard deviation; ** and *** indicate significance of p < 0.01 and p < 0.001, respectively
Ocular aberrations over time
At the 13 month visit, 28 subjects in the OK group had completed the ocular aberration measurements. SA, coma and total HOAs in the OK group increased significantly after 1 month of OK treatment (t‐test, all p < 0.001). Furthermore, the measurements remained significantly greater than baseline at each follow‐up visit during OK treatment (t‐test, all p < 0.001, Figure 3a). After stopping OK lens wear for 1 month (i.e., the 13 month visit), coma, SA and total HOAs remained higher than the baseline (t‐test, all p < 0.01). In the SVS group, all HOAs were stable and did not deviate significantly from the baseline values (ANOVA, all p > 0.05, Figure 3b).
FIGURE 3.
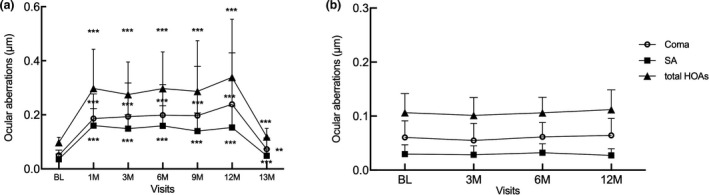
Ocular aberrations over time in the OK (a) and SVS groups (b). OK, orthokeratology; SVS, single‐vision spectacles; SA, spherical aberration; BL, baseline; HOAs, higher‐order aberrations; Error bars indicate one standard deviation; ** and *** indicate significance of p < 0.01 and p < 0.001, respectively
Correlation between changes in aberrations and accommodation in the orthokeratology (OK) group
After 1 month of OK wear, the accommodative lag area tended to decrease more with larger increases of SA, but this correlation was not significant (Figure 4a). However, at 13 months, the negative correlation between recovery of accommodative lag area (i.e., the difference between the 13 and 12 month values) and SA was significant (r = −0.47, p = 0.01, Figure 4b). Furthermore, the decrease in accommodative lag area after 1 month of OK lens wear was also negatively correlated with the baseline accommodative lag area (Pearson correlation, r = −0.70, p < 0.001, Figure 4c). Other changes in aberrations were not correlated with accommodation shifts.
FIGURE 4.
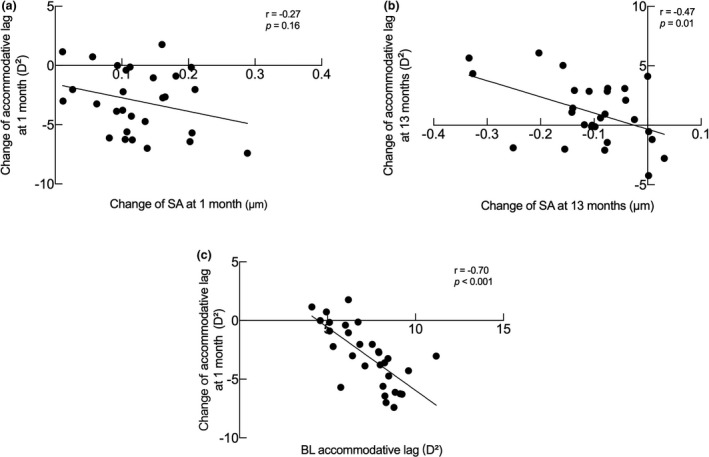
Correlation analysis of accommodation changes in the OK group. (a) Scatter plot for changes of SA against accommodative lag area changes at 1 month of OK treatment. (b) Scatter plot for changes of SA against accommodative lag area changes after ceasing OK treatment. (c) Scatter plot for accommodative lag area at baseline against changes at 1 month. Change at 1 month, difference between 1 month and baseline; change at 13 months, difference between 13 months and 12 months. BL, baseline; D, dioptre; OK, orthokeratology; SA, spherical aberration
Factors associated with axial length (AL) elongation
In the OK group, based on univariate analysis, changes in accommodative lag area after 6 and 12 months were associated with axial elongation (B = 0.02, p = 0.03; B = 0.03, p = 0.02, respectively, Table 2). Age was negatively correlated with axial growth at 1 year (p < 0.01). Variables with a p value ≤ 0.10 in the univariate analysis were then entered into a multivariate regression analysis. At 6 months, changes in accommodative lag area remained in the model (B = 0.02, p = 0.03). However, at 1 year, only the age variable remained in the model (B = −0.07, p < 0.01). In the univariate regression analysis of the SVS group, no variables were associated with axial elongation at either 6 or 12 months (all p > 0.05) (see Table S2).
TABLE 2.
Factors associated with AL elongation in the OK group
| Variables | 6 months | 1 year | ||
|---|---|---|---|---|
| B (95% CI) | p | B (95% CI) | p | |
| Univariate analysis | ||||
| Age (years) | −0.03 (−0.06, 0.001) | 0.06 | −0.07 (−0.11, −0.02) | <0.01** |
| SER (D) | −0.03 (−0.08, 0.03) | 0.33 | −0.06 (−0.15, 0.03) | 0.21 |
| Initial AL (mm) | −0.02 (−0.06, 0.03) | 0.43 | −0.04 (−0.11, 0.03) | 0.26 |
| BL accommodative lag area (D2) | −0.02 (−0.04, 0.004) | 0.10 | −0.03 (−0.07, 0.01) | 0.14 |
| △ Accommodative lag area (D2) | 0.02 (0.002, 0.03) | 0.03* | 0.03 (0.01,0.06) | 0.02* |
| △SA (μm) | 0.12 (−0.51, 0.74) | 0.71 | 0.03 (−0.07, 0.12) | 0.56 |
| △Coma (μm) | 0.22 (−0.20, 0.65) | 0.29 | 0.12 (−0.46, 0.69) | 0.68 |
| △total HOAs (μm) | 0.11 (−0.27, 0.49) | 0.54 | 0.08 (−0.44, 0.59) | 0.77 |
| Multivariate analysis | ||||
| Age (years) | – | – | −0.07 (−0.11, 0.02) | <0.01** |
| △ Accommodative lag area (D2) | 0.02 (0.002, 0.03) | 0.03* | – | – |
OK, orthokeratology; SER, spherical equivalent refraction; D, dioptre; AL, axial length; ∆, difference between weighted average after OK treatment within half a year or 1 year and baseline (e.g. 1‐year △Coma = ‐ , i for visit during OK wear, for the time interval between two consecutive visits); BL, baseline; SA, spherical aberration; HOAs, higher‐order aberrations. * and ** indicate significance of p < 0.05 and p < 0.01, respectively.
DISCUSSION
The present study showed that OK slowed axial elongation by 0.09 mm and refractive error by 0.37 D when compared with the SVS group. Ocular accommodative accuracy improved during OK treatment, and this change may be related to the changes in SA. Moreover, the association between improved accommodative accuracy and slowed axial elongation was only present during the first 6 months of the study. In the SVS group, no significant changes were observed in either accommodation or aberrations during the study period, and we hypothesize that they are not involved in the natural progression of myopia (see Figure S1).
Orthokeratology caused a dramatic increase in ocular aberrations over the baseline values. HOAs, coma and SA increased by 3, 4 and 5 times, respectively, but remained stable in the SVS group. These findings are generally consistent with the results of earlier studies. 19 , 21 , 22 Due to many factors that affect aberrations, such as pupil size, 18 contact lens design 24 and duration of wear, 25 the measured change in aberrations varies amongst previous studies. Stillitano et al. followed their subjects for 1 year, and found that most optical aberrations induced by OK remained stable after 1 week of lens wear. 26 We also found that the aberrations remained stable after the increases that became evident in the early stages of OK wear.
After discontinuing OK for 1 month, coma, SA and total HOAs remained higher than the baseline levels, which was not consistent with our expectations and previous studies. 27 , 28 For example, Hiraoka et al. found HOAs returned to baseline level 1 week after ending treatment. 27 Lorente‐Velázquez et al. suggested corneal reshaping was completely reversible 1 month after OK cessation. 28 Indeed, analysis of corneal aberrations here showed that the cornea had reverted to pre‐treatment values 1 month after OK cessation (see Figure S2). However, at the 13 month visit, ocular HOAs in the OK group remained higher than baseline. This may be due to changes in ocular shape or the crystalline lens. Zhang et al. suggested that spectacle lenses designed to create myopic defocus for myopia control may alter the overall shape of the retina. 29 Therefore, it is reasonable to speculate that wearing OK lenses based on this same peripheral defocus principle may also change the ocular shape after 1 year of wear, as well as induce changes in HOAs. In the present study, changes in crystalline lens were not documented as we did not monitor either the shape of the lens or the ciliary muscle. Future studies could employ anterior segment optical coherence tomography (OCT) to observe changes in the shape of the crystalline lens and ciliary muscle, both of which could affect accommodation. In contrast, aberrations remained stable in the SVS control group during the 1 year monitoring period. Thus, aberrations were not affected by age or refractive development during that period.
In this study, to reflect the actual accommodative status, accommodation measurements during OK treatment were conducted without additional optical correction. Additionally, we replaced the traditional accommodative lag measurement at a single stimulus level with the accommodation lag area using stimuli from 0 to 6 D. This approach reflects the accommodative performance under real‐time conditions where working distances vary during multi‐visual tasks. Nevertheless, in line with previous studies using a single accommodative stimulus, 13 , 14 we found that accommodative lag decreased during OK treatment. We speculate that the improvement in accommodative accuracy with OK was not due to refractive overcorrection, even though overcorrection may increase the accommodative response. These current findings show that the average degree of overcorrection was low (see Table S1 ), and thus was likely to have a minimal effect on accommodation. In a previous investigation, 20 accommodative lag when assessed with OK lenses providing full correction was significantly smaller than the baseline level, consistent with our proposal. We excluded the possibility that the improvement in accommodative response was due to an increase in accommodative demand because it was equivalent in this investigation (0–6 D). A reasonable suggestion is compensation for the increase in positive corneal SA by OK. 20 SA shifts in the negative direction with accommodation, and this can partly neutralize the OK induced positive increase in corneal SA. 30 Batres et al. reported that accommodative accuracy improved and internal SA decreased after OK wear, and speculated a link between these changes. 20 However, due to the limitations of the measuring device, no information was reported regarding the internal SA. After ceasing OK treatment, we found that a larger reversion of SA was associated with a greater increase in accommodative lag area. Additionally, after 1 and 12 months of OK wear, the decrease in accommodative lag area tended to be negatively associated with the increase in SA, although the association was not statistically significant (see Figure S3). We speculate that those subjects showing larger increases in SA will have a greater improvement in accommodative accuracy.
OK reduced axial elongation by 24% and myopia progression by 47% compared with SVS in this study. This difference between axial elongation and myopia progression could be attributed to subjects having physiological axial elongation. However, axial length is the preferred metric for monitoring the progression of myopia. 31 Our findings of slowed axial elongation are similar to those of He et al. (28.9%), 32 but poorer than other studies. 33 , 34 , 35
Regarding accommodative function and myopia progression in the OK group, multivariate regression analysis revealed that changes in accommodative lag area were associated with AL progression during the first 6 months, but not in the 1‐year analysis. This implies that improved accommodative accuracy is associated with slowed axial growth in the short term. This could explain why clinical optical interventions that aim to reduce accommodative lag do not achieve satisfactory control of myopia progression. 36 One‐year multivariate regression results indicated that older children had slower axial growth. Other investigations have also reported that AL elongation in older children (9–10 years) treated with OK was slower than for younger children (7–8 years) or axial elongation in children undergoing OK therapy was negatively correlated with the age of the wearer according to regression analysis, 37 , 38 while the similar trend between age and myopia progression was found among untreated children. 39 However, the R 2 value for the model at six months and 1‐year was low (R 2 = 0.16 and 0.25, respectively), suggesting that there may be other stronger factors affecting myopia control, such as peripheral myopic defocus. 40
We did not find that ocular aberrations were associated with AL elongation in the OK group. Recently, Lau et al. reported that, after adjusting for confounding factors, a higher level of positive ocular SA was associated with slower AL elongation in 103 children receiving OK treatment for over 2 years. 22 However, the range of myopic corrections in Lau et al.’s investigation, i.e., −8.63 D to −0.38 D, was much greater than that of the present study (−1.25 D to −4.00 D), which increased the change in aberrations. 41 These small changes in aberrations may account for our negative finding. Indeed, contact lenses designed with positive SA have been found to only slow myopia progression during the initial 6 months of wear. We suggest that SA may be linked with myopia control through changes in accommodative accuracy. In short, whether SA plays a role in myopia control, and the mechanisms by which it might potentially work, requires further investigation.
A limitation of the present study is that it was not a double‐masked randomized trial design. Although it is currently difficult to perform a masked trial using OK, a gold standard randomized masked trial still needs to be conducted to avoid potential bias and provide more solid evidence. Another limitation was that the 1‐year axial elongation measurements of the OK group were obtained at 13 months (i.e., 1 month after OK cessation). While 1 month of axial growth is likely to be minimal, it could possibly affect the results.
In conclusion, for myopic children treated with SVS, accommodation and aberrations remained stable throughout the study period, and exhibited no association with myopia progression. In contrast, children who wore OK lenses had improved accommodative function, and the changes were significantly correlated with changes in SA after OK cessation. The improvement in accommodative accuracy was greater for those individuals with poorer baseline accommodative accuracy. Additionally, this correlation between improved accommodative accuracy and slowed axial elongation was only evident during the initial 6 months of OK wear.
CONFLICT OF INTEREST
All authors declared that there is no conflict of interest.
AUTHOR CONTRIBUTION
Chenglu Ding: Data curation (lead); Formal analysis (lead); Methodology (equal); Writing – original draft (lead); Writing – review & editing (lead). Yunyun Chen: Investigation (equal); Methodology (lead); Project administration (lead). Xue Li: Data curation (lead); Resources (equal); Visualization (equal). Yingying Huang: Conceptualization (equal); Methodology (lead); Resources (equal). Hao Chen: Funding acquisition (lead); Investigation (lead). Jinhua Bao: Supervision (lead); Validation (lead); Writing – review & editing (lead).
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
None.
Ding C, Chen Y, Li X, et al. The associations of accommodation and aberrations in myopia control with orthokeratology. Ophthalmic Physiol Opt 2022;42:327–334. 10.1111/opo.12930
Chenglu Ding and Yunyun Chen contributed equally to this work.
Funding information
This work was supported by the Leading Science and Technology Innovation Talent of Zhejiang Provincial Ten Thousand Talent Project (grant no. 2017R52050).
Contributor Information
Hao Chen, Email: chenhao@mail.eye.ac.cn.
Jinhua Bao, Email: baojessie@163.com.
REFERENCES
- 1. He M, Zeng J, Liu Y, et al. Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci 2004;45:793–9. [DOI] [PubMed] [Google Scholar]
- 2. Jung S, Lee J, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19‐year‐old male conscripts in Seoul, South Korea. Invest Ophthalmol Vis Sci 2012;53:5579–83. [DOI] [PubMed] [Google Scholar]
- 3. Dolgin E. The myopia boom. Nature 2015;519:276–8. [DOI] [PubMed] [Google Scholar]
- 4. Holden B, Fricke T, Wilson D, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016;123:1036–42. [DOI] [PubMed] [Google Scholar]
- 5. Saw SM, Gazzard G, Shih‐Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt 2005;25:381–91. [DOI] [PubMed] [Google Scholar]
- 6. Huang J, Wen D, Wang Q, et al. Efficacy comparison of 16 interventions for myopia control in children: a network meta‐analysis. Ophthalmology 2016;123:697–708. [DOI] [PubMed] [Google Scholar]
- 7. Li S, Kang M, Wu S, et al. Efficacy, safety and acceptability of orthokeratology on slowing axial elongation in myopic children by meta‐analysis. Curr Eye Res 2016;41:600–8. [DOI] [PubMed] [Google Scholar]
- 8. Smith E, Hung L, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res 2009;49:2386–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gwiazda J, Thorn F, Bauer J, Held R. Myopic children show insufficient accommodative response to blur. Invest Ophthalmol Vis Sci 1993;34:690–4. [PubMed] [Google Scholar]
- 10. Allen P, O'Leary D. Accommodation functions: co‐dependency and relationship to refractive error. Vision Res 2006;46:491–505. [DOI] [PubMed] [Google Scholar]
- 11. Lan W, Yang Z, Liu W, Chen X, Ge J. A longitudinal study on the relationship between myopia development and near accommodation lag in myopic children. Ophthalmic Physiol Opt 2008;28:57–61. [DOI] [PubMed] [Google Scholar]
- 12. Aleman A, Schaeffel F. Lag of accommodation does not predict changes in eye growth in chickens. Vision Res 2018;149:77–85. [DOI] [PubMed] [Google Scholar]
- 13. Yang Y, Wang L, Li P, Li J. Accommodation function comparison following use of contact lens for orthokeratology and spectacle use in myopic children: a prospective controlled trial. Int J Ophthalmol 2018;11:1234–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Han X, Xu D, Ge W, et al. A comparison of the effects of orthokeratology lens, medcall lens, and ordinary frame glasses on the accommodative response in myopic children. Eye Contact Lens 2018;44:268–71. [DOI] [PubMed] [Google Scholar]
- 15. Tarrant J, Liu Y, Wildsoet CF. Orthokeratology can decrease the accommodative lag in myopes. Invest Ophthalmol Vis Sci 2009;50:4294. ARVO E‐Abstract 4294. [Google Scholar]
- 16. Gifford K, Gifford P, Hendicott P, Schmid K. Zone of clear single binocular vision in myopic orthokeratology. Eye Contact Lens 2020;46:82–90. [DOI] [PubMed] [Google Scholar]
- 17. Song Y, Zhu S, Yang B, et al. Accommodation and binocular vision changes after wearing orthokeratology lens in 8‐ to 14‐year‐old myopic children. Graefes Arch Clin Exp Ophthalmol 2021;259:2035–45. [DOI] [PubMed] [Google Scholar]
- 18. Hiraoka T, Matsumoto Y, Okamoto F, et al. Corneal higher‐order aberrations induced by overnight orthokeratology. Am J Ophthalmol 2005;139:429–36. [DOI] [PubMed] [Google Scholar]
- 19. Gifford P, Li M, Lu H, et al. Corneal versus ocular aberrations after overnight orthokeratology. Optom Vis Sci 2013;90:439–47. [DOI] [PubMed] [Google Scholar]
- 20. Batres L, Peruzzo S, Serramito M, Carracedo G. Accommodation response and spherical aberration during orthokeratology. Graefes Arch Clin Exp Ophthalmol 2020;258:117–27. [DOI] [PubMed] [Google Scholar]
- 21. Hiraoka T, Kakita T, Okamoto F, Oshika T. Influence of ocular wavefront aberrations on axial length elongation in myopic children treated with overnight orthokeratology. Ophthalmology 2015;122:93–100. [DOI] [PubMed] [Google Scholar]
- 22. Lau J, Vincent S, Cheung S, Cho P. Higher‐order aberrations and axial elongation in myopic children treated with orthokeratology. Invest Ophthalmol Vis Sci 2020;61:22. 10.1167/iovs.61.2.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen Y, Jin W, Zheng Z, et al. Comparison of three monocular methods for measuring accommodative stimulus‐response curves. Clin Exp Optom 2017;100:155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kang P, Gifford P, Swarbrick H. Can manipulation of orthokeratology lens parameters modify peripheral refraction? Optom Vis Sci 2013;90:1237–48. [DOI] [PubMed] [Google Scholar]
- 25. Lian Y, Shen M, Huang S, et al. Corneal reshaping and wavefront aberrations during overnight orthokeratology. Eye Contact Lens 2014;40:161–8. [DOI] [PubMed] [Google Scholar]
- 26. Stillitano I, Schor P, Lipener C, Hofling‐Lima A. Long‐term follow‐up of orthokeratology corneal reshaping using wavefront aberrometry and contrast sensitivity. Eye Contact Lens 2008;34:140–5. [DOI] [PubMed] [Google Scholar]
- 27. Hiraoka T, Okamoto C, Ishii Y, Okamoto F, Oshika T. Recovery of corneal irregular astigmatism, ocular higher‐order aberrations, and contrast sensitivity after discontinuation of overnight orthokeratology. Br J Ophthalmol 2009;93:203–8. [DOI] [PubMed] [Google Scholar]
- 28. Lorente‐Velázquez A, Madrid‐Costa D, Nieto‐Bona A, González‐Mesa A, Carballo J. Recovery evaluation of induced changes in higher order aberrations from the anterior surface of the cornea for different pupil sizes after cessation of corneal refractive therapy. Cornea 2013;32:e16–20. [DOI] [PubMed] [Google Scholar]
- 29. Zhang H, Lam C, Tang W, Leung M, To C. Defocus incorporated multiple segments spectacle lenses changed the relative peripheral refraction: a 2‐year randomized clinical trial. Invest Ophthalmol Vis Sci 2020;61:53. 10.1167/iovs.61.5.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ke B, Mao X, Jiang H, et al. The relationship between high‐order aberration and anterior ocular biometry during accommodation in young healthy adults. Invest Ophthalmol Vis Sci 2017;58:5628–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in myopia control. Prog Retin Eye Res 2021;83:100923. 10.1016/j.preteyeres.2020.100923 [DOI] [PubMed] [Google Scholar]
- 32. He M, Du Y, Liu Q, et al. Effects of orthokeratology on the progression of low to moderate myopia in Chinese children. BMC Ophthalmol 2016;16:126. 10.1186/s12886-016-0302-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vincent SJ, Cho P, Chan KY, et al. CLEAR – orthokeratology. Cont Lens Anterior Eye 2021;44:240–69. [DOI] [PubMed] [Google Scholar]
- 34. Swarbrick H, Alharbi A, Watt K, Lum E, Kang P. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology 2015;122:620–30. [DOI] [PubMed] [Google Scholar]
- 35. Chen C, Cheung S, Cho P. Myopia control using toric orthokeratology (TO‐SEE study). Invest Ophthalmol Vis Sci 2013;54:6510–7. [DOI] [PubMed] [Google Scholar]
- 36. Wildsoet C, Chia A, Cho P, et al. IMI – interventions myopia institute: interventions for controlling myopia onset and progression report. Invest Ophthalmol Vis Sci 2019;60:M106–M31. [DOI] [PubMed] [Google Scholar]
- 37. Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2‐year randomized clinical trial. Invest Ophthalmol Vis Sci 2012;53:7077–85. [DOI] [PubMed] [Google Scholar]
- 38. Zhong Y, Chen Z, Xue F, Miao H, Zhou X. Central and peripheral corneal power change in myopic orthokeratology and its relationship with 2‐year axial length change. Invest Ophthalmol Vis Sci 2015;56:4514–9. [DOI] [PubMed] [Google Scholar]
- 39. Donovan L, Sankaridurg P, Ho A, et al. Myopia progression rates in urban children wearing single‐vision spectacles. Optom Vis Sci 2012;89:27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hu Y, Wen C, Li Z, et al. Areal summed corneal power shift is an important determinant for axial length elongation in myopic children treated with overnight orthokeratology. Br J Ophthalmol 2019;103:1571–5. [DOI] [PubMed] [Google Scholar]
- 41. Hiraoka T, Okamoto C, Ishii Y, et al. Mesopic contrast sensitivity and ocular higher‐order aberrations after overnight orthokeratology. Am J Ophthalmol 2008;145:645–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


