Abstract
Background
Respiratory syncytial virus (RSV) is a major cause of hospitalization for bronchiolitis and pneumonia in infancy. In Japan, limited data are publicly available on RSV epidemiology and clinical characteristics among infants.
Methods
This retrospective study described RSV incidence, seasonality, patient characteristics, resource use, and clinical outcomes among Japanese children <2 years from January 2017 through December 2018. The RSV cases were identified using the Japanese Medical Data Center database.
Results
In the database, 9,711 and 8,509 RSV patients <2 years were identified in 2017 and 2018, respectively. Of these, 25% required hospitalization. Ninety percent of hospitalized patients did not have a known RSV risk factor. Nineteen percent of hospitalized patients experienced dehydration, and 12% had acute respiratory failure. Hospitalization lasted 1 week on average and 7% required some type of mechanical ventilation. The peak of hospitalizations occurred at 2 months. The incidence of RSV hospitalization in children <2 years was 23.2 per 1,000 person‐years, which increased to 35.4 per 1,000 for infants <6 months. This age group accounted for 40% of all RSV‐associated hospitalizations among children <2 years.
Conclusions
Roughly one‐fourth of all RSV patients <2 years were hospitalized. Ninety percent of these did not have an underlying risk condition. This underscores that RSV can cause serious disease among all young children. Three to four out of every 100 Japanese children <6 months were hospitalized for RSV, and this age group accounted for ~40% of all RSV‐associated hospitalizations. Novel and broad‐based RSV prevention strategies, especially those targeting young infants, are needed.
Keywords: epidemiology, Japan, respiratory syncytial virus
Respiratory syncytial virus (RSV) is a major cause of hospitalization for bronchiolitis and pneumonia among infants worldwide, and is the second leading cause of mortality, following malaria, among infants. 1 Among children younger than 5 years of age, an estimated 3 million RSV‐related hospitalizations and at least 60 000 deaths occur globally each year. 2 Nearly half of these hospitalizations and deaths occur among children under 6 months of age. 2
Respiratory syncytial virus can be spread through contact with respiratory droplets from infected individuals or contaminated surfaces and objects. It is highly communicable, and humans are the only known reservoir. Despite 50% of infants becoming infected during their first year of life and almost 100% by their second year, lifetime immunity is not achieved following these initial infections. 3 The risk of severe or even fatal disease is higher among preterm children and children with chronic cardiac and respiratory conditions, immunodeficiency, or specific genetic abnormalities. However, most of the severe cases of RSV infection occur among full‐term children and those without pre‐existing diseases. 4 , 5 , 6 , 7 , 8
In Japan, RSV infection is defined as a Category V infectious disease and is monitored under the National Epidemiology Surveillance of Infectious Diseases (NESID) program. Respiratory syncytial virus infection is reported from the pediatric sentinel surveillance system. The NESID program provides the Infectious Diseases Weekly Report (IDWR) and the Infectious Agents Surveillance Report (IASR) by the National Institute of Infectious Diseases (NIID). These reports contain information on the occurrence of RSV infections in the population covered by the approximately 3,000 pediatric sentinel sites across Japan, as well as some patient characteristics. Despite the existence of nationwide RSV surveillance, 7 more granular data describing the burden of RSV, including clinical features, resource use, and outcomes are needed. This study describes the national epidemiology and clinical features of RSV infection among children in Japan using a nationwide healthcare claims database.
Methods
Study design and population
This retrospective study described the incidence and seasonality of medically attended RSV episodes among Japanese children <2 years of age from January 1, 2017 through December 31, 2018. Among those with RSV, patient characteristics, resource use (e.g. hospitalization, mechanical ventilation, intensive care unit admission), and clinical outcomes (average length of stay and death) were described. Respiratory syncytial virus cases were identified using the Japanese Medical Data Center (JMDC) database. The JMDC database provides anonymized inpatient, outpatient, and pharmacy claims from health insurance associations in Japan, 9 through a panel of approximately seven million beneficiaries since 2005 to the present, 10 which accounts for about 5.5% of the entire Japanese population. Diagnosis codes used to identify RSV (B348, J121, J205, J210) and underlying conditions, and procedure codes for RSV‐associated clinical outcomes, are provided in the supplementary material (Appendix Table S1‐S4). Risk status for RSV infection was defined based on having at least one record with a diagnosis of any of five specified risk factors: prematurity, bronchopulmonary dysplasia (BPD), Down syndrome, congenital heart disease (CHD), or immunodeficiency. Associated diseases were also identified, and these included the five specified risk factors as well as other medical conditions frequently observed with RSV infections. 11 , 12
Ethics approval and informed consent
This study used de‐identified claims data compiled by JMDC, which were classified as anonymously processed information under the Act on the Protection of Personal information. 13
Statistical analysis
Patient characteristics, clinical outcomes, and resource use for patients with RSV were described using descriptive statistics. To describe seasonality of RSV infections, numbers of RSV cases in outpatient and inpatient settings were calculated per calendar month for each study period. Respiratory syncytial virus incidence was calculated per 1,000 person‐years (PYs) with 95% confidence intervals. The incidence rate was defined as the number of patients with an RSV infection observed during the study period divided by the sum of time at risk of RSV infection. Time at risk for RSV infection was defined as the time to the first RSV infection, time until reaching age 2, or time until the end of the study period (based on whichever occurred first). End of follow up occurred at the first of any of the following: death, 23 months of age, loss to follow up, end of the study period.
Results
In the JMDC database, 9,711 and 8,509 RSV patients <2 years of age were identified in 2017 and 2018, respectively. Of these, 25% were hospitalized, Fifty‐five percent of all RSV patients were male (Table 1). Most (90%) hospitalized patients did not have risk conditions for RSV. The two most frequent RSV risk factors for RSV hospitalization were prematurity (5%) and CHD (4%). On average, a hospital stay for RSV infection lasted 1 week, ranging from 6.1 to 7.4 days (Table 2). Nineteen percent of hospitalized patients experienced dehydration, and 12% had acute respiratory failure. Bronchial asthma, acute bronchitis, and asthmatic bronchitis were also consistently observed in the 10 most frequently occurring RSV‐associated diseases (Appendix Tables S8 and S9).
Table 1.
Demographic and clinical characteristics for RSV patients <2 years of age in the JMDC population
| 2017 | 2018 | |||||
|---|---|---|---|---|---|---|
|
All RSV patients† (n = 9,711) |
Only outpatients‡ (n = 7,238) |
Inpatients§ (n = 2,473) |
All RSV patients† (n = 8,509) |
Only outpatients‡ (n = 6,426) |
Inpatients§ (n = 2,083) |
|
| Male (n, %) | 5,347 (55.1) | 3,967 (54.8) | 1,380 (55.8) | 4,654 (54.7) | 3,487 (54.3) | 1,167 (56.0) |
| Any RSV risk factor (n, %) | 651 (6.7) | 422 (5.8) | 229 (9.3) | 621 (7.3) | 407 (6.3) | 214 (10.3) |
| Prematurity (n, %) | 356 (3.7) | 233 (3.2) | 123 (5.0) | 327 (3.8) | 215 (3.3) | 112 (5.4) |
| BPD (n, %) | 12 (0.1) | 6 (0.1) | 6 (0.2) | 10 (0.1) | 6 (0.1) | 4 (0.2) |
| Down syndrome (n, %) | 25 (0.3) | 13 (0.2) | 12 (0.5) | 31 (0.4) | 17 (0.3) | 14 (0.7) |
| CHD (n, %) | 275 (2.8) | 177 (2.4) | 98 (4.0) | 269 (3.2) | 176 (2.7) | 93 (4.5) |
| Immunodeficiency (n, %) | 47 (0.5) | 27 (0.4) | 20 (0.8) | 59 (0.7) | 30 (0.5) | 29 (1.4) |
†All RSV patients: patients with only outpatient visit or hospitalization.
‡Only outpatients: patients with only outpatient visit.
§Inpatients: patients with hospitalization.
BPD: bronchopulmonary dysplasia; CHD: congenital heart disease; JMDC: Japan Medical Data Center; RSV: respiratory syncytial virus.
Table 2.
Length of hospital stay among RSV inpatients in the JMDC population
| Age group (months) | 0–2 | 3–5 | 6–11 | 12–23 | ||||
|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2017 | 2018 | 2017 | 2018 | 2017 | 2018 | |
| Total RSV inpatients† | 514 | 481 | 474 | 426 | 576 | 472 | 979 | 771 |
| Number of hospitalizations‡ | 516 | 484 | 447 | 398 | 569 | 467 | 979 | 774 |
| Length of hospital stay (days) | ||||||||
| Mean | 7.4 | 7.0 | 6.2 | 6.7 | 6.5 | 6.8 | 6.1 | 6.5 |
| Median | 6 | 6 | 5 | 5 | 6 | 6 | 5 | 6 |
†Total RSV inpatients: the number of inpatients diagnosed with RSV.
‡Number of hospitalizations: the number of times patients were hospitalized due to RSV.
JMDC: Japan Medical Data Center; RSV: respiratory syncytial virus.
Among hospitalized children, 0.1% were admitted into the ICU and 7% required artificial respiration or mechanical ventilation (Table 3). Infants <6 months of age accounted for 41% of RSV‐related hospitalizations among those <2 years (Fig. 1). Of those who required mechanical ventilation, approximately half (52% in 2017; 50% in 2018) were <6 months old. The peak of hospitalizations occurred at age 2 months, with this age group accounting for 10% of all hospitalized patients (Fig. 1).
Table 3.
RSV‐associated clinical outcomes in the JMDC population
| 2017 | 2018 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age (months) | All (0–23) | 0–2 | 3–5 | 6–11 | 12–23 | All (0–23) | 0–2 | 3–5 | 6–11 | 12–23 |
| RSV hospitalization (%) | 2,473 (100.0) | 518 (20.9) | 447 (18.1) | 565 (22.8) | 943 (38.1) | 2,083 (100.0) | 488 (23.4) | 395 (19.0) | 453 (21.7) | 747 (35.9) |
| ICU admissions (%) | 3 (0.1) | 1 (0.2) | 0 (0.0) | 0 (0.0) | 2 (0.2) | 1 (0.0) | 1 (0.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Ventilator use (%) | 164 (6.6) | 46 (8.9) | 40 (8.9) | 52 (9.2) | 26 (2.8) | 168 (8.1) | 39 (8.0) | 45 (11.4) | 60 (13.2) | 24 (3.2) |
| RSV mortality | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
ICU: intensive care unit; JMDC: Japan Medical Data Center; RSV: respiratory syncytial virus.
Fig. 1.
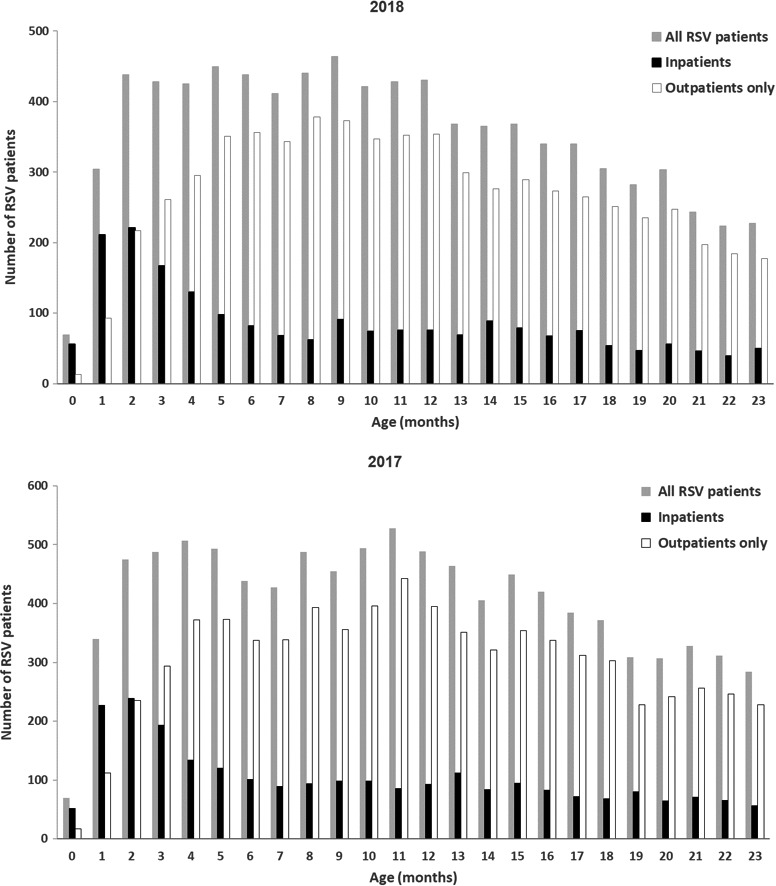
Number of RSV patients in the JMDC population by age in months and care setting for 2018 and 2017. JMDC: Japan Medical Data Center; RSV: respiratory syncytial virus; All RSV patients: patients with only outpatient visit or hospitalization; Only Outpatients: patients with only outpatient visit; Inpatients: patients with hospitalization. ( ): All RSV patients; (■): Inpatients; (□): Outpatients only.
): All RSV patients; (■): Inpatients; (□): Outpatients only.
The incidence rate of medically attended RSV among Japanese children <2 years of age was 85.2 per 1,000 person‐years. The incidence rate of RSV hospitalization in children <2 years was 23.2 per 1,000 person‐years, which increased to 35.4 per 1,000 person‐years for infants <6 months (Table 4). Regarding seasonality of RSV infections, 2017 and 2018 seasonality patterns were similar. The highest number of RSV cases, for both 2017 and 2018, was in September (Fig. 2).
Table 4.
RSV incidence in the JMDC population per 1000 by age group and setting of care for 2017 to 2018
| Age (months) | 0–2 | 3–5 | 6–11 | 12–23 | 0–5 | 0–11 | 0–23 | |
|---|---|---|---|---|---|---|---|---|
| All† | No. of RSV infections | 1,845 | 3,052 | 4,489 | 3,160 | 4,897 | 9,386 | 12 546 |
| Total PY | 29 121 | 28 099 | 45 016 | 44 947 | 57 220 | 102 236 | 147 183 | |
| Incidence per 1,000 PY (95% CI) | 63.4 (60.5–66.3) | 109.0 (104.8–112.5) | 100.0 (96.8–102.6) | 70.0 (67.9–72.8) | 85.6 (83.2–88.0) | 91.8 (90.0–93.7) | 85.2 (83.8–86.7) | |
| Outpatients‡ | No. of RSV infections | 1,543 | 2,941 | 4,376 | 3,010 | 4,484 | 8,860 | 11 870 |
| Total PY | 29 143 | 28 186 | 45 211 | 45 265 | 57 329 | 102 540 | 147 805 | |
| Incidence per 1,000 PY (95% CI) | 52.9 (50.3–55.6) | 104.3 (100.6–108.1) | 96.8 (93.9–99.7) | 66.5 (64.1–68.9) | 78.2 (75.9–80.5) | 86.4 (84.6–88.2) | 80.3 (78.9–81.8) | |
| Inpatients§ | No. of RSV infections | 1,087 | 953 | 850 | 693 | 2,040 | 2,890 | 3,583 |
| Total PY | 29 146 | 28 446 | 47 049 | 49 533 | 57 592 | 104 641 | 154 174 | |
| Incidence per 1,000 PY (95% CI) | 37.3 (35.1–39.5) | 33.5 (31.4–35.6) | 18.1 (16.9–19.3) | 14.0 (13.0–15.0) | 35.4 (33.9–37.0) | 27.6 (26.6–28.6) | 23.2 (22.5–24.0) | |
†All: patients with outpatient visit only or hospitalization.
‡Outpatient: patients with any outpatient visits – i.e. outpatient visits only and outpatients who were subsequently hospitalized.
§Inpatients: patients with any hospitalization – i.e. hospitalization only and outpatients after hospitalization.
CI: confidence interval; JMDC: Japan Medical Data Center; PY: person‐years; RSV: respiratory syncytial virus.
Fig. 2.
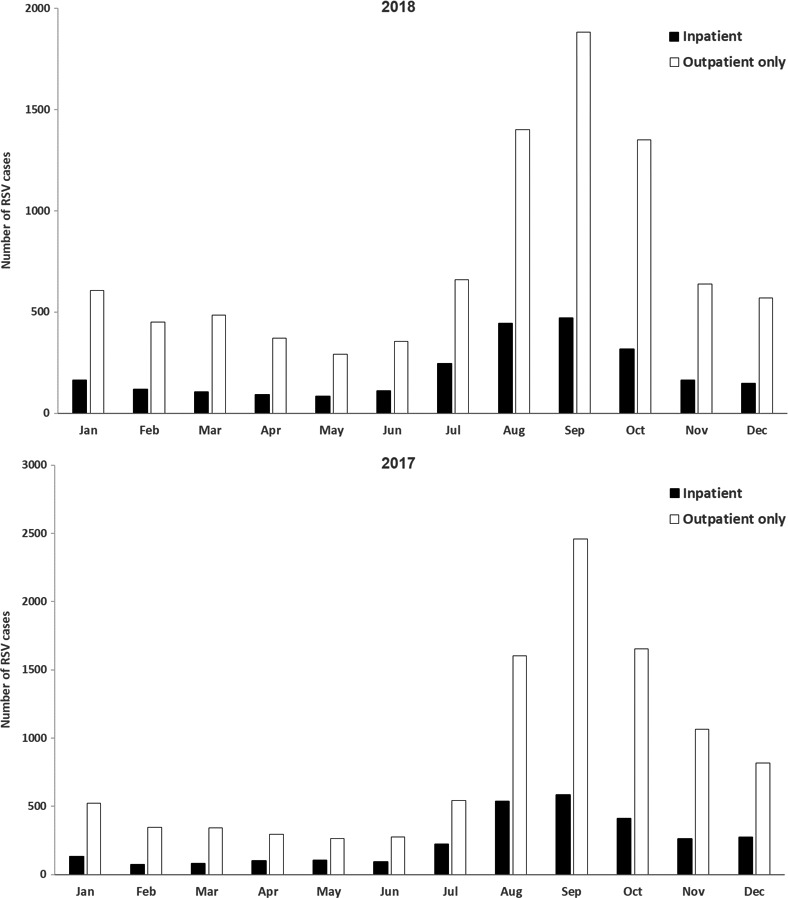
Numbers of RSV cases (<2 years) in the JMDC population for 2018 and 2017 by calendar month. JMDC: Japan Medical Data Center; RSV: respiratory syncytial virus; Outpatient Only: patients with only outpatient visit; Inpatient: patients with hospitalization; (■): Inpatients; (□): Outpatients only.
Discussion
This study confirms the high burden of RSV infection among infants and young children in Japan. Extrapolating the number of patients with JMDC into the Japanese population suggests that an estimated 119 000 to 138 000 RSV‐related diagnoses occur in Japan among children <2 years of age each year. Roughly one‐fourth of all RSV patients <2 years were hospitalized (Appendix Table S5). Although certain conditions do put infants at increased risk of RSV disease, 6 , 14 this study showed that 90% of children <2 years of age hospitalized with RSV infection did not have an underlying risk condition for RSV infection. This underscores that RSV can cause serious disease among all young children. This finding is consistent with previous reports in Japan 15 , 16 and the USA. 14
Regarding associated diseases, 47% of RSV all patients had acute bronchitis and 7.5% had dehydration. These disorders were frequently reported in all age groups (0–23 months of age). In addition, 7% of all RSV patients aged 0–2 months had acute respiratory failure (Appendix Table S8). On the other hand, 19% of RSV hospitalized patients had dehydration and 12% had respiratory failure. These disorders were frequently reported in all age groups (0–23 months of age; Appendix Table S9). On average, patients stayed for about 1 week in the hospital across age groups. This result is consistent with other reports in the Japanese setting 16 , 17 , 18 , 19 and highlights the impact of RSV on patients and the health system. Although <1% were admitted to the ICU, 7% required artificial respiration or mechanical ventilation. The proportion of ICU admissions in a previous report was slightly higher but this difference may be due to the data source for the previous study being tertiary hospital‐based, which tends to involve more severe cases. 16
Extrapolating the number of RSV patients in the JMDC by month of age to the Japanese population by month of age described the same tendency as in Appendix Figure S1 (Appendix Tables S6 and S7).
Japanese children aged <6 months accounted for 41% of RSV‐related hospitalizations among children <2 years of age. This is similar to findings in other developed countries, 2 , 14 , 20 and another study previously conducted in Japan 14 where the inpatient burden is disproportionately shifted towards the very young. The peak of hospitalization for RSV infection occurred at 2 months of age, consistent with previous reports in multiple settings highlighting that most hospitalizations occur in the first 90 days of life. 6 , 14 , 21 Infants <6 months also had more severe disease. For example, while only 7% of children hospitalized for <24 months for RSV infection required mechanical ventilation, roughly 50% of all mechanical ventilation occurred in infants <6 months old. This further highlights the disproportionate burden of RSV in very young patients.
Among children <2 years of age in the JMDC population, the rate of RSV was 85 per 1,000. The rate of hospitalized RSV decreased as age increased from 37 per 1,000 among infants <2 months of age to 14 per 1,000 among children 12–23 months of age. Rates found in this study were consistent with those in the US 20 and developed countries globally 2 and in other Japanese studies (e.g., Tochigi prefecture). 22
Current peaks of RSV infections, for both 2017 and 2018, were in September. This is consistent with the NIID sentinel report (IASR 2018). 7 While the majority of studies covering previous years indicated December as the peak for cases in Japan, 18 , 23 , 24 , 25 , 26 , 27 these data suggest an evolution of the epidemiology of RSV infection with cases occurring earlier in the year and not being confined to the winter months.
Recently, high‐risk children have been receiving palivizumab prophylactically during the RSV season, which has also been reported in surveys evaluating patient information in Japanese hospitals. 28 , 29 However, many children are still hospitalized for RSV infection given that – as seen in this study – the vast majority of hospitalizations are in children without underlying medical conditions. Furthermore, some patients are still hospitalized even after receiving prophylactic palivizumab during the peak of the RSV season. 29 Thus, new and broader preventive strategies for RSV infections in young children are needed, including licensure of new vaccines and monoclonal antibodies in the future or administration of palivizumab, which is currently available, earlier in the year prior to the start of the RSV season. 29 , 30
This study has limitations. The definition of RSV infection in this study was based on ICD10 codes and thus not necessarily test‐confirmed RSV positivity. Recent studies in other developed settings found RSV ICD‐10 code specificity to be very high (>99%), although there was inconsistency in sensitivity estimates suggesting that study results could underestimate the RSV burden. 20 , 31 , 32 Moreover, JMDC database includes employees and their family members from only medium‐ to large‐scale companies and does not include employees of small companies and public/government employees. This could also point to an underestimation of the RSV burden as a US study showed that rates were much higher among children who relied on government assistance programs. 20 Despite these limitations, results on seasonality of RSV infections align with the data from the NESID program, which require stringent laboratory confirmation for inclusion. The number of hospital days from admission date was also truncated at the end of the study period and this could have underestimated the average length of hospital stay in some cases. Strengths of this study include the large number of patients, even among very young age groups, and the description of up‐to‐date, nationwide, and detailed information on patient characteristics, resource use, and clinical outcomes that have not been previously described.
Conclusions
Roughly one‐fourth of all RSV patients <2 years were hospitalized. Ninety percent of children <2 years of age hospitalized with RSV infection did not have an underlying risk condition. This underscores that RSV can cause serious disease among all young children. Three to four out of every 100 Japanese children aged <6 months were hospitalized for RSV, and this age group accounted for approximately 40% of all RSV‐associated hospitalizations. Novel and broad‐based prevention strategies against RSV infection, especially those targeting young infants, are needed.
Disclosures
This study was sponsored by Pfizer Japan Inc. All authors are employees of Pfizer Japan Inc. and Pfizer Inc. Dr Togo and Mr Kobayashi report personal fees from Pfizer Japan Inc., stock from Pfizer Inc., during the conduct of the study. Dr McLaughlin and Dr Agosti report personal fees and stock from Pfizer Inc. during the conduct of the study.
Authors contributions
Y.K conceptualized and designed the study, instructed the data analysis, and drafted the initial manuscript. K.T. conducted statistical analysis and critically reviewed and revised the manuscript. J.M. and Y.A. contributed significantly to the interpretation of the data and revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Supporting information
Table S1. JMDC standard diagnosis names and ICD‐10 codes for RSV infections.
Table S2. JMDC standard diagnosis names and ICD‐10 codes for baseline underlying conditions.
Table S3. JMDC procedure codes for ICU admissions.
Table S4. JMDC procedure codes for ventilator use.
Table S5. Estimated number of RSV patients <2 years in the Japanese population by age in year and setting of care for 2017 and 2018.
Table S6. Estimated numbers of RSV and Palivizumab patients in Japan by age group and setting of care for 2017.
Table S7. Estimated numbers of RSV and palivizumab patients in Japan by age group and setting of care for 2018.
Table S8. Ten most frequent associated diseases among all RSV patients in the JMDC population by age group
Table S9. Top associated diseases among RSV inpatients in the JMDC population.
Fig. S1. Estimated numbers of RSV cases in the Japanese population for 2018 and 2017, by calendar month. RSV, Respiratory syncytial virus.
Acknowledgments
The authors acknowledge Dr Bennett Lee (Pfizer Japan Inc) for his useful advice on this study.
The JMDC provided the claims data and aggregation service. Medical writing support was provided by Jihen Mahjoub MS and Ver Bilano PhD, from Creativ‐Ceutical.
1Vaccine Medical Affairs, 2Health & Value, Pfizer Japan Inc, Tokyo, Japan, 3Viral Vaccines, 4Pipeline Vaccines, Pfizer Inc, Collegeville, PA, USA
References
- 1. Leader S, Kohlhase K. Respiratory syncytial virus‐coded pediatric hospitalizations, 1997 to 1999. Pediatr. Infect. Dis. J. 2002; 21: 629–32. [DOI] [PubMed] [Google Scholar]
- 2. Shi T, McAllister DA, O'Brien KL et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: A systematic review and modelling study. Lancet. 2017; 390: 946–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dudas RA, Karron RA. Respiratory syncytial virus vaccines. Clin. Microbiol. Rev. 1998; 11: 430–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mazur NI, Bont L, Cohen AL et al. Severity of respiratory syncytial virus lower respiratory tract infection with viral coinfection in HIV‐uninfected children. Clin. Infect. Dis. 2017; 64: 443–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sigurs N, Gustafsson PM, Bjarnason R et al. Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am. J. Resp. Crit Care. 2005; 171(2): 137–41. [DOI] [PubMed] [Google Scholar]
- 6. American Academy of Pediatrics Committee on Infectious D, American Academy of Pediatrics Bronchiolitis Guidelines C . Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 2014; 134: e620–38. [DOI] [PubMed] [Google Scholar]
- 7. Infectious Agents Surveillance Report (IASR) . Respiratory syncytial virus infection, January 2014‐September 2018. Vol. 39 No. 32 (No. 466). National Institute of Infectious Diseases, 2018; 207–9. [Google Scholar]
- 8. Sockrider M, Katkin J. What is respiratory syncytial virus (RSV)? Am. J. Resp. Crit. Care. 2015; 191: P3–4. [DOI] [PubMed] [Google Scholar]
- 9. Sato K, Ohno T, Ishii T, Ito C, Kaise T. The prevalence, characteristics, and patient burden of severe asthma determined by using a japan health care claims database. Clin. Ther. 2019; 41: 2239–51. [DOI] [PubMed] [Google Scholar]
- 10. Japan Medical Data Company . JMDC Database; 2020. [Google Scholar]
- 11. Okada K, Mizuno M, Moriuchi H et al. The Working Group for Revision of "Guidelines for the Use of Palivizumab in Japan": A Committee Report. Pediatr. Int. 2020; 62(11): 1223–9. [DOI] [PubMed] [Google Scholar]
- 12. AbbVie . Package Insert of Palivizumab in Japan, Revised March 2019 (6th edn.) (In Japanese).
- 13. Act on the protection of personal information (Act No. 57 of 2003, Amendment of Act No. 65 of 2015). http://www.japaneselawtranslation.go.jp/law/detail/?id=2781&vm=2&re=02
- 14. Hall CB, Weinberg GA, Blumkin AK et al. Respiratory syncytial virus‐associated hospitalizations among children less than 24 months of age. Pediatrics 2013; 132: e341–8. [DOI] [PubMed] [Google Scholar]
- 15. Fujita S, Hirose S, Hamada H, Fujimori M, Yasukawa K, Takanashi J. Epidemic season of respiratory syncytial virus infection is shifting to midsummer in Chiba, Japan: A single center study for clinical characteristics of hospitalized patients in summer, compared with those in winter. J. Jpn. Soc. Emerg. Pediatr. 2019; 18: 16–21. (In Japanese). [Google Scholar]
- 16. Sruamsiri R, Kubo H, Mahlich J. Hospitalization costs and length of stay of Japanese children with respiratory syncytial virus: A structural equation modeling approach. Medicine (Baltimore). 2018; 97: e11491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Inagaki K, Morikawa H, Kito A et al. Trends and clinical studies of respiratory syncytial virus infection in our hospital. Igaku Kensa. 2009; 58: 7–10. (In Japanese). [Google Scholar]
- 18. Moriyama Y, Hamada H, Okada M et al. Distinctive clinical features of human bocavirus in children younger than 2 years. Eur. J. Pediatr. 2010; 169(9): 1087–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Okubo Y, Morisaki N, Michihata N, Matsui H, Fushimi K, Yasunaga H. Dose‐dependent relationships between weight status and clinical outcomes among infants hospitalized with respiratory syncytial virus infections. Pediatr. Pulm. 2018; 53: 461–6. [DOI] [PubMed] [Google Scholar]
- 20. McLaughlin JM, Khan F, Schmitt HJ et al. Respiratory syncytial virus‐associated hospitalization rates among US infants: A systematic review and meta‐analysis. J. Infect. Dis. 2020. 10.1093/infdis/jiaa752. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Winterstein AG, Knox CA, Kubilis P, Hampp C. Appropriateness of age thresholds for respiratory syncytial virus immunoprophylaxis in moderate‐preterm infants: A cohort study. JAMA Pediatr. 2013; 167(12): 1118–24. [DOI] [PubMed] [Google Scholar]
- 22. Suzumura H, Takahashi N, Yamazaki Y et al. Infantile respiratory syncytial virus infection‐associated hospitalization rate by gestational week. Jpn. J. Pediatr. 2011; 64: 2021–6. (In Japanese). [Google Scholar]
- 23. Akiyoshi K, Tamura T, Haruta T, Infulenza Examination Team of Kobe Institute of Health . Virus‐related lower respiratory inflammation: Detection of human metapneumovirus from severe pneumonia cases with A/H1N1pdm virus. Jpn. J. Infect. Dis. 2011; 64: 89–91. [PubMed] [Google Scholar]
- 24. Hara M, Takao S, Shimazu Y, Nishimura T. Three‐year study of viral etiology and features of febrile respiratory tract infections in Japanese pediatric outpatients. Pediatr. Infect. Dis. J. 2014; 33: 687–92. [DOI] [PubMed] [Google Scholar]
- 25. Mizuta K, Abiko C, Aoki Y et al. Seasonal patterns of respiratory syncytial virus, influenza A virus, human metapneumovirus, and parainfluenza virus type 3 infections on the basis of virus isolation data between 2004 and 2011 in Yamagata, Japan. Jpn. J. Infect. Dis. 2013; 66(2): 140–5. [DOI] [PubMed] [Google Scholar]
- 26. Nishimura T, Suzue J, Kaji H. Breastfeeding reduces the severity of respiratory syncytial virus infection among young infants: A multi‐center prospective study. Pediatr. Int. 2009; 51: 812–6. [DOI] [PubMed] [Google Scholar]
- 27. Shobugawa Y, Saito R, Sano Y et al. Emerging genotypes of human respiratory syncytial virus subgroup A among patients in Japan. J. Clin. Microbiol. 2009; 47: 2475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kusuda S, Takahashi N, Saitoh T et al. Survey of pediatric ward hospitalization due to respiratory syncytial virus infection after the introduction of palivizumab to high‐risk infants in Japan. Pediatr. Int. 2011; 53: 368–73. [DOI] [PubMed] [Google Scholar]
- 29. Yanagisawa T, Nakamura T. Survey of hospitalization for respiratory syncytial virus in Nagano, Japan. Pediatr. Int. 2018; 60: 835–8. [DOI] [PubMed] [Google Scholar]
- 30. Seimiya A, Morioka I, Okahashi A, Nagano N, Yoda H. Survey of infants hospitalized for respiratory syncytial virus disease in Tokyo, 2018. Pediatr. Int. 2021; 63: 219–21. [DOI] [PubMed] [Google Scholar]
- 31. Cai W, Tolksdorf K, Hirve S et al. Evaluation of using ICD‐10 code data for respiratory syncytial virus surveillance. Influenza Other Resp. 2020; 14: 630–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pisesky A, Benchimol EI, Wong CA et al. Incidence of hospitalization for respiratory syncytial virus infection amongst children in Ontario, Canada: A population‐based study using validated health administrative data. PLoS One 2016; 11: e0150416. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. JMDC standard diagnosis names and ICD‐10 codes for RSV infections.
Table S2. JMDC standard diagnosis names and ICD‐10 codes for baseline underlying conditions.
Table S3. JMDC procedure codes for ICU admissions.
Table S4. JMDC procedure codes for ventilator use.
Table S5. Estimated number of RSV patients <2 years in the Japanese population by age in year and setting of care for 2017 and 2018.
Table S6. Estimated numbers of RSV and Palivizumab patients in Japan by age group and setting of care for 2017.
Table S7. Estimated numbers of RSV and palivizumab patients in Japan by age group and setting of care for 2018.
Table S8. Ten most frequent associated diseases among all RSV patients in the JMDC population by age group
Table S9. Top associated diseases among RSV inpatients in the JMDC population.
Fig. S1. Estimated numbers of RSV cases in the Japanese population for 2018 and 2017, by calendar month. RSV, Respiratory syncytial virus.


