Abstract
BACKGROUND
Hyperactive cranial neuropathies refractory to medical management can often be debilitating to patients. While microvascular decompression (MVD) surgery can provide relief to such patients when an aberrant vessel is compressing the root entry zone (REZ) of the nerve, the arteries of elderly patients over 65 years of age can be less amenable to manipulation because of calcifications and other morphological changes. A dolichoectatic vertebral artery (DVA), in fact, can lead to multiple cranial neuropathies; therefore, a strategy for MVDs in elderly patients is useful.
OBSERVATIONS
A 76-year-old man presented with medically refractory trigeminal neuralgia (TN) and hemifacial spasm (HFS). A DVA was the conflicting vessel at the left REZs of the trigeminal and facial nerves. The authors performed a retrosigmoid craniotomy for MVD of the DVA with Teflon padding at both REZs in approximately 1 hour of operative time. The patient was free of facial pain and spasm immediately after surgery and at follow-up.
LESSONS
The authors described the case of an elderly patient with both TN and HFS caused by compression of a DVA. Simultaneous MVD with Teflon padding at both REZs provided symptomatic relief with limited surgical time. This can be a particularly useful and straightforward surgical strategy in the elderly population.
Keywords: hemifacial spasm, trigeminal neuralgia, microvascular decompression
ABBREVIATIONS : CN = cranial nerve, DVA = dolichoectatic vertebral artery, HFS = hemifacial spasm, MVD = microvascular decompression, REZ = root entry zone, TN = trigeminal neuralgia
Trigeminal neuralgia (TN) and hemifacial spasm (HFS) refractory to medical management can commonly be the result of direct contact by an aberrant vessel compressing the root entry zone (REZ) of the trigeminal and facial nerves, respectively. Microvascular decompression (MVD) has been shown to provide lasting relief.1 In TN, the offending vessel is usually the superior cerebellar artery, whereas in HFS, it is usually the anterior inferior cerebellar artery. There are instances, however, in which an enlarged or dolichoectatic vertebral artery (DVA) can be the offending vessel2 and can cause both TN and HFS as well as other hyperactive cranial nerve (CN) syndromes,3 such as glossopharyngeal neuralgia.3,4 In this study, we present an elderly patient with both TN and HFS refractory to medical management. The offending vessel in this case was a DVA compressing the REZ of the respective nerves. We describe the surgical technique of simultaneous microvascular decompression of both the trigeminal nerve and the facial nerve, using only Teflon patties to pad and achieve adequate decompression and separation in a short operative time of approximately 40 minutes. The use of MVD for combined CN pathologies is a rare and effective strategy, particularly in elderly patients with DVAs.4–8
Illustrative Case
A 76-year-old man with left-sided HFS and TN that were both refractory to medical management presented to our outpatient clinic for evaluation. Constructive interference in steady state magnetic resonance imaging revealed a DVA in conflict with the REZ of the facial and trigeminal nerves (Figs. 1 and 2). The patient’s case was discussed at our institution’s multidisciplinary hemifacial pain and spasm conference. Because of the failure of conservative management, open surgery for MVD of both the facial and trigeminal nerves was recommended.
FIG. 1.
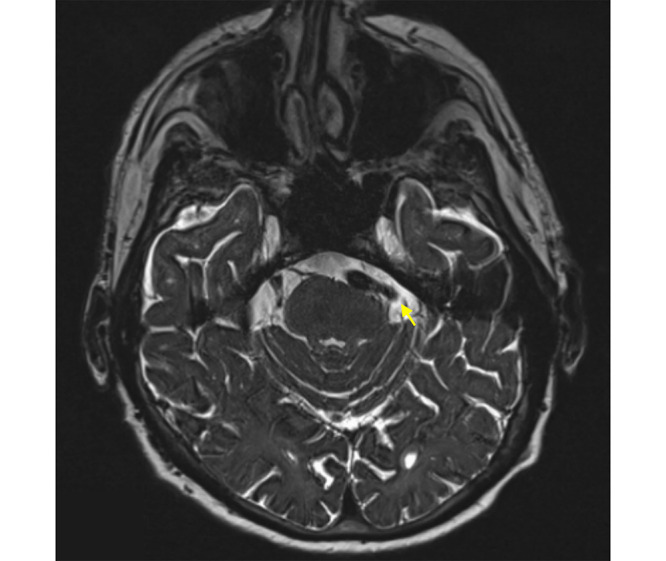
Constructive interference in steady state (CISS) magnetic resonance imaging (MRI) showing a DVA compressing the REZ of CN V (yellow arrow).
FIG. 2.

CISS MRI showing a DVA compressing the REZ the CN VII/VIII complex (yellow arrow).
The patient was given the option of surgery versus continued conservative management and/or Gamma Knife radiosurgery for TN. He underwent a left retrosigmoid craniotomy for combined decompression of the trigeminal and facial nerves. Neurophysiology monitoring of the trigeminal and facial nerves as well as brainstem auditory evoked response and somatosensory evoked potentials was performed. The patient was placed supine with his head fixed in the three-pin Mayfield head holder and turned to the right, tucked at the neck and extended toward the floor. We made a curvilinear incision behind his ear and performed a small retrosigmoid craniotomy inferior to the asterion with the dura opened and reflected beneath the junction of the transverse and sigmoid sinus. Cerebrospinal fluid was released, which allowed for retractorless surgery. The operating microscope was used, and the arachnoid overlying the cerebellopontine angle was subsequently sharply dissected and the trigeminal and facial nerves were identified. We visualized the DVA looped underneath the REZ of both the trigeminal and facial nerves (Fig. 3), and it was mobilized and dissected away from both nerves. Although the stiffness of the vertebral artery was appreciated, the vessel was able to be safely elevated and manipulated. Several Teflon patties were used to create separation between the vertebral artery and the REZs of the trigeminal and facial nerves (Fig. 4). Excellent decompression was achieved, and the disappearance of lateral spread of the facial nerve on neurophysiological monitoring was appreciated.
FIG. 3.
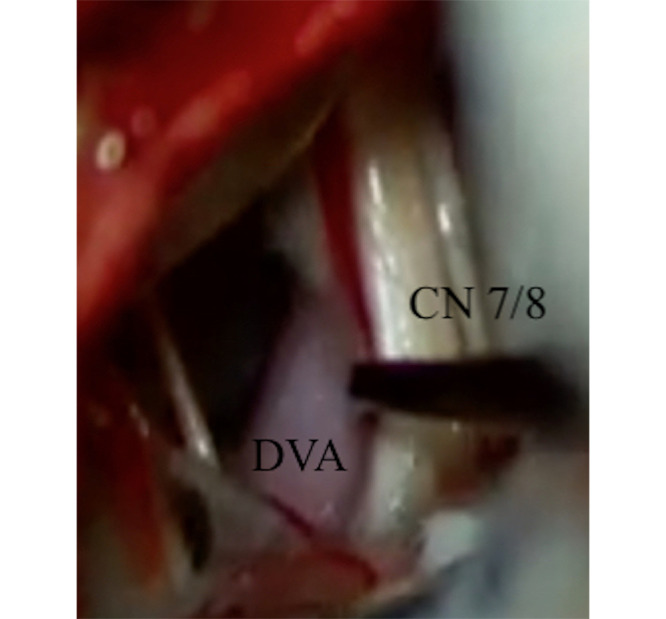
Intraoperative photograph showing the DVA in relation to the CN VII/VIII complex.
FIG. 4.
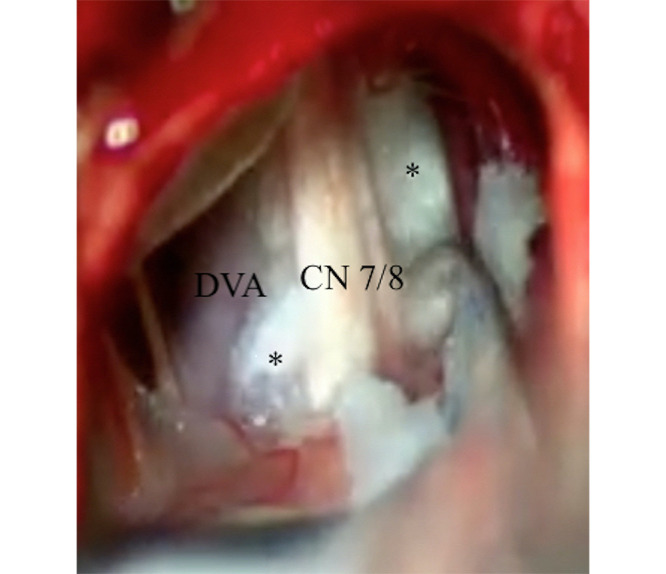
Intraoperative photograph showing the DVA decompressed with Teflon patties (*).
The patient tolerated the procedure well. In the immediate postoperative period, the patient was pain and spasm free without detectable facial weakness or hearing loss. He was discharged home in excellent condition on postoperative day 2. At the 5-month follow-up, the patient continues to be free of facial pain and spasm.
Discussion
Observations
Surgery for MVD to treat TN was first described by Peter Janetta in 1983.9 Given its level of success for this pathology, MVD was later expanded to treat other hyperactive CN syndromes, including HFS and glossopharyngeal neuralgia.3,4
Albeit rare, patients can suffer from more than one hyperactive CN syndrome due to the same conflicting vessel4,5,7,8 and often, a dolichoectatic vertebrobasilar arterial system is the culprit.3,6 Indeed, the pathophysiology of a dolichoectatic vertebrobasilar system is most commonly observed in the setting of long-standing hypertension causing disruption of the inner layers of the vessel, leading to elongation and distention of the vessel. This also results in increased muscularity of the offending vessel, rendering it potentially less compliant and more challenging to mobilize during MVD. In cases in which the offending vessel is a DVA, the patients are usually over 60 years of age.10 Therefore, surgical considerations such as prolonged time under anesthesia are necessary.
Although various nuances to MVD surgical techniques have been introduced over the years, the basic principle of creating separation between the offending vessel and hyperactive nerve remains the same. In the description of the MVD for treatment of multiple CN neuropathies, single Teflon patties are often used to achieve decompression of the affected nerve.11 In our case, we used multiple Teflon patties to maintain adequate decompression of the DVA from the REZs of CNs V and VII. Each Teflon patty was shaped by the lead surgeon to fit in the appropriate space and achieve maximal decompression. Although we did encounter a rather noncompliant vertebral artery, the use of Teflon patties alone was sufficient to maintain adequate decompression in a relatively short operative time. This is important when operating on elderly patients, who usually present with this pathology.10
Recent reports have also shown a clip sling technique to be effective in less compliant arteries, such as the vertebral artery, whereby a Teflon sling is fashioned around the offending vertebral artery.3,12,13 An aneurysm clip can be used to keep the sling in place in conjunction with individual Teflon patties. Indeed, the use of the clip sling technique, and variations thereof, may potentially provide a more durable, long-term solution when dealing with compression of multiple CNs. One of the larger studies, with 41 patients, in which the clip sling technique was used for TN alone showed that most patients were pain free at a mean follow-up of 16 months.13 With respect to multiple hyperactive cranial neuropathies, a large series examined 44 patients treated with the clip sling technique and found that 43 of them received a clinical cure within 1 month of surgery and only 3 patients showed recurrence during a mean follow-up time of 40 months.14 However, when considering the elderly population in particular, a more straightforward approach without increased operative time for dissection and the additional use of the clip sling technique may be sufficient to achieve adequate decompression and improvement in quality of life for patients with potentially shorter lifespans.
Lessons
We describe the case of simultaneous MVD for trigeminal neuralgia and hemifacial spasm caused by a single dolichoectatic vertebral artery in an elderly patient. Microdissection around the offending artery, with mobilization and placement of multiple Teflon patties at both REZs, without the use of a sling, can achieve maximal decompression and symptomatic relief in a relatively short operative time. We suggest that this straightforward approach is a safe and effective one, particularly for the elderly population, in whom DVAs may cause multiple hyperactive cranial syndromes.
Disclosures
Dr. Moliterno reported personal fees from BK Medical outside the submitted work. No other disclosures were reported.
Author Contributions
Conception and design: Moliterno, Marianayagam, Jalal. Acquisition of data: Marianayagam, Qureshi, Vasandani, Vetsa, Wu. Analysis and interpretation of data: Marianayagam, Qureshi, Vasandani, Jalal, Wu. Drafting the article: Marianayagam, Vasandani, Jalal. Critically revising the article: Marianayagam, Qureshi, Vasandani, Vetsa, Jalal. Reviewed submitted version of manuscript: Marianayagam, Qureshi, Jalal. Approved the final version of the manuscript on behalf of all authors: Moliterno. Administrative/technical/material support: Vetsa, Jalal, Wu. Study supervision: Moliterno.
References
- 1. Barker FG, 2nd, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 1996;334(17):1077–1083. doi: 10.1056/NEJM199604253341701. [DOI] [PubMed] [Google Scholar]
- 2.Wilkins R. Facial nerve decompression for hemifacial spasm. In: Apuzzo MLJ, editor. Brain Surgery Complication Avoidance and Management. Churchill Livingstone; 1993. pp. 2115–2143. [Google Scholar]
- 3. Perez-Roman RJ, Chen SH, Sur S, Leon-Correa R, Morcos JJ. A unique case of microvascular triple decompression for combined simultaneous trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia because of the dolichoectatic vertebrobasilar system. Oper Neurosurg (Hagerstown) 2020;18(6):692–697. doi: 10.1093/ons/opz205. [DOI] [PubMed] [Google Scholar]
- 4. Wang YN, Zhong J, Zhu J, et al. Microvascular decompression in patients with coexistent trigeminal neuralgia, hemifacial spasm and glossopharyngeal neuralgia. Acta Neurochir (Wien) 2014;156(6):1167–1171. doi: 10.1007/s00701-014-2034-8. [DOI] [PubMed] [Google Scholar]
- 5. Eidelman BH, Nielsen VK, Møller M, Jannetta PJ. Vascular compression, hemifacial spasm, and multiple cranial neuropathy. Neurology. 1985;35(5):712–716. doi: 10.1212/wnl.35.5.712. [DOI] [PubMed] [Google Scholar]
- 6. Jia Y, Wenhua W, Quanbin Z. A single microvascular decompression surgery cures a patient with trigeminal neuralgia, hemifacial spasm, tinnitus, hypertension, and paroxysmal supraventricular tachycardia caused by the compression of a vertebral artery. Neurol India. 2013;61(1):73–75. doi: 10.4103/0028-3886.108016. [DOI] [PubMed] [Google Scholar]
- 7. Yang KH, Na JH, Kong DS, Park K. Combined hyperactive dysfunction syndrome of the cranial nerves. J Korean Neurosurg Soc. 2009;46(4):351–354. doi: 10.3340/jkns.2009.46.4.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kobata H, Kondo A, Iwasaki K, Nishioka T. Combined hyperactive dysfunction syndrome of the cranial nerves: trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia: 11-year experience and review. Neurosurgery. 1998;43(6):1351–1362. doi: 10.1097/00006123-199812000-00052. [DOI] [PubMed] [Google Scholar]
- 9. Jannetta PJ. Hemifacial spasm: treatment by posterior fossa surgery. J Neurol Neurosurg Psychiatry. 1983;46(5):465–466. doi: 10.1136/jnnp.46.5.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ubogu EE, Zaidat OO. Vertebrobasilar dolichoectasia diagnosed by magnetic resonance angiography and risk of stroke and death: a cohort study. J Neurol Neurosurg Psychiatry. 2004;75(1):22–26. [PMC free article] [PubMed] [Google Scholar]
- 11. Broggi G, Broggi M, Ferroli P, Franzini A. Surgical technique for trigeminal microvascular decompression. Acta Neurochir (Wien) 2012;154(6):1089–1095. doi: 10.1007/s00701-012-1324-2. [DOI] [PubMed] [Google Scholar]
- 12. Lee SH, Park JS, Ahn YH. Bioglue-coated teflon sling technique in microvascular decompression for hemifacial spasm involving the vertebral artery. J Korean Neurosurg Soc. 2016;59(5):505–511. doi: 10.3340/jkns.2016.59.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Steinberg JA, Sack J, Wilson B, et al. Tentorial sling for microvascular decompression in patients with trigeminal neuralgia: a description of operative technique and clinical outcomes. J Neurosurg. doi: 10.3171/2017.10.JNS17971. Published online April 20, 2018. doi: 10.3171/2017.10.JNS17971. [DOI] [PubMed] [Google Scholar]
- 14. Cao J, Jiao J, Du Z, et al. Combined hyperactive dysfunction syndrome of the cranial nerves: a retrospective systematic study of clinical characteristics in 44 patients. World Neurosurg. 2017;104:390–397. doi: 10.1016/j.wneu.2017.05.020. [DOI] [PubMed] [Google Scholar]


