Abstract
The novel coronavirus disease (COVID-19) has generated great confusion around the world, affecting people’s lives and producing a large number of deaths. The development of portable and wearable devices is of great importance in several fields such as point-of-care medical applications and environmental monitoring. Wearable devices with an ability to collect various types of physiological records are progressively becoming incorporated into everyday life of people. Physiological indicators are essential health indicators and their monitoring could efficiently enable early discovery of disease. This would also help decrease the number of extra severe health problems, in disease avoidance, and lower the overall public sector health cost. Protective clothing is nowadays a main part of textiles classified as technical or industrial textiles. Protective clothing aims to protect its wearer from the harsh environmental impacts that may result in injury or death. Providing protection for the common population has also been taken seriously considering the anticipated disaster due to virus attacks. This review highlights the properties of the materials that are used in wearable health care device and medical textiles.
Keywords: COVID-19, wearable device, health care device, nanomaterials, medical textile, smart textile, sensors, face mask
Introduction
The novel coronavirus disease (COVID-19) pandemic appeared in Wuhan, China, in December 2019 and has become a serious public health problem worldwide. As the COVID-19 pandemic continues to grow, researchers worldwide have been working to better understand its spread, mitigate, and suppress it. The main areas of research include studying the transmission of COVID-19 and facilitating its detection, developing possible vaccines and treatments, and understanding the social and economic impacts of the pandemic.1–5 Also researchers worldwide have been working to provide clothing and protective tools for doctors as well as the nursing staff to provide protection from disease transmission as well as providing comfort and flexibility for ease of work.4–6 In addition to provide tools for patients for ease of household insulation, such as devices for measuring temperature, respiration and pressure.
Wearable devices are devices that can be worn directly on the skin in different parts of the body. These devices have gained great attention due to their ease of collection of important information in real-time regarding a wearer’s health, both continuously and non-invasively.7–9 The usage of wearable health care devices also encourages people to take more interest in their own health care in a more useful and cheaper way, thereby improving their compliance. Wearable devices are becoming smaller and more mobile with time, opening novel alternatives to traditional methods that providers have cooperated with patients, carried out tests, collected data, and delivered treatments. Wearable devices come in many forms; there are smart wristbands, watches shirts, shoes, headbands, eyeglasses, shirts, shoes, and necklaces. Most of them have sensors that collect raw data that is fed into a database or software application for analysis. Analysis usually triggers a response that would, for example, alert a physician to contact a patient who is experiencing abnormal symptoms.10–12 By frequent detection of the level of physical markers, for example, body temperature and pressure pulses using different sensing techniques, wearable devices can provide one of the most comprehensive feedback on human health state.13–15
Textile materials contain fibers, yarns, filaments, and different structures of fabrics that are made from natural or synthetic fibrous materials. The applications of textile materials in various fields have significantly enlarged with the development of new fibers and manufacturing technologies for yarns and fabrics. One of the most essential applications of textile materials is in the medical textile industry. In recent years, the results from the tremendous research in the field of material, surface, aerosol science, and engineering have enhanced the textile materials with properties crucial for successful prevention of the spread of infectious diseases, for example, improved filtration, antibacterial and antiviral activity, and breathability.16 Materials science plays an important role in the effective protection against COVID-19 by numerous means, for instance, disinfection, isolation, and inactivation.17,18 Personnel protective equipment kits, such as face shields, masks, gloves, protective suits, and goggles, help in physically isolating the human body from viral infection to stop the spreading of COVID-19.19,20 This fact is placing textiles on the front line in the battle against the current pandemic. The textile industry is an important player since many textile companies are presently implementing the production of protective masks and protective clothing using their production facilities. Another specification of COVID-19 is the exponential growth in the number of new cases that can easily lead to systemic health care failure. Therefore, the World Health Organization (WHO) recommends patients with mild symptoms and without cardinal chronic conditions to be cared for at home while keeping a communication link with the health care personnel. At this time, the smart textile role for sensing and monitoring of body physiological parameters as part of telemedicine could play an essential role. Smart textiles and nanotechnology are promising in tackling the pandemic.21,22 In this article, we discuss how advanced materials can contribute to the development of medical textiles as well as wearable health care devices.
Wearable health care devices
Wearable health care devices are a major branch that gradually evolved with the development of wearable devices.23 It mainly uses multimedia, wireless communication, and sensor technology to collect various physiological parameters of the human body to achieve monitoring of various physical signs of the human body.24 Wearable devices have features such as wearability, mobility, and sustainability that can overcome these shortcomings of traditional medical devices.25
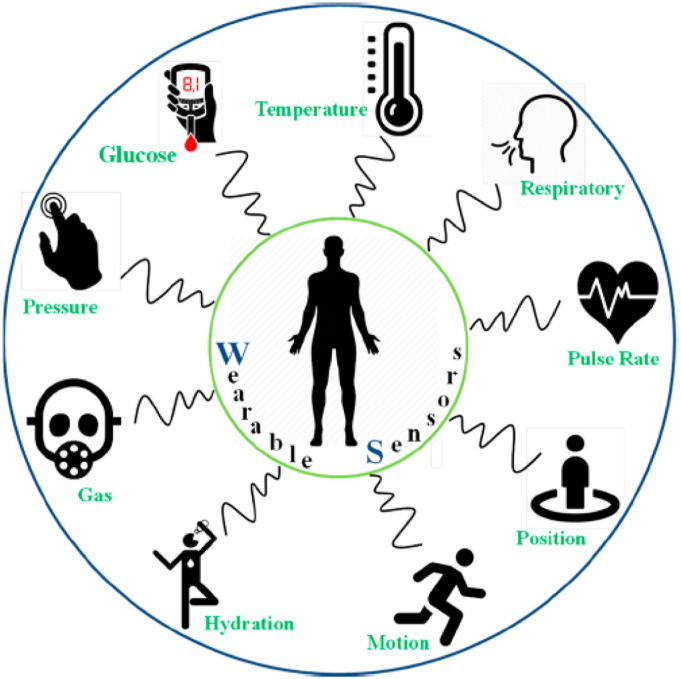
Smart wearable systems are designed to be the next generation of personal mobile devices for remote health monitoring.26 Wearable electronics technology is one of the most important recent innovations that are regularly becoming abundant. Wearable technologies engaged in the health care sector for monitoring physiological parameters include body temperature, physical pressure, blood pressure, respiratory rate, humidity, heart rate (HR), skin conductance, and body movements.27 Some representative examples are mentioned in the schematic of Figure 1.28 Flexible sensing electronics will change conventional diagnosis methods and revolutionize medical instruments by bestowing them with portable, wearable, remote, and timely features.26
Figure 1.
Schematic representation of wearable health care sensing devices.28
Currently, accurately acquiring real-time health signals has been realized in medical institutions, which helps a lot in diagnosing disease and selecting proper medical measures. But, most medical institutions are highly concentrated in central hospitals, making health care services laborious and time-consuming when people were there in large numbers. Patients, especially the ones in the developing areas, may feel more pain and even death for the lack of timely and actual treatment. Moreover, the high cost of purchasing, using, and maintaining these medical facilities also brings heavy economic burden to hospital and patients, which can further hinder the diagnosis and treatment of diseases. Developing wearable sensors for health care-related applications faces a multitude of challenges, which include the selection of suitable substrates, biocompatible materials, and manufacturing techniques, as well as the instantaneous monitoring of different analysts, the washability, and uninterrupted signal display circuits.28
The flexible/stretchable sensors involve three basic components: containing substrate, active element, and electrode/interconnect. The organic materials have excessive mechanical flexibility and chemical stability, but very few of them expose favorable active characters. While, traditional inorganic electronic materials are sensitive to many stimuli, but not competent to mechanical compliance due to their rigidity and frangibility. So, the collaboration between different materials can be a solution to compacting high measuring performance, flexibility/stretchability, and mechanical robustness in one device. The novel approaches in material preparation, such as scaling down measurement and manufacturing composites, can be useful in device development. The next parts will focus on the commonly used materials and their participation in substrate, active element, and electrode.29
Materials selection for wearable health care devices
In the past few years, the configurations of wearable systems with unique sensing materials and device structures have proved to be highly sensitive in simulating human somatosensory systems and to be able to easily and non-invasively track biophysical and biochemical signals such as body temperature, body movements, blood pressure, metabolites, functional proteins, and oligonucleotides.30,31 In addition, these wearable health care systems can not only improve health status, but also contribute greatly to the development of medical technology by collecting human health information into a system and collecting large amounts of data.32
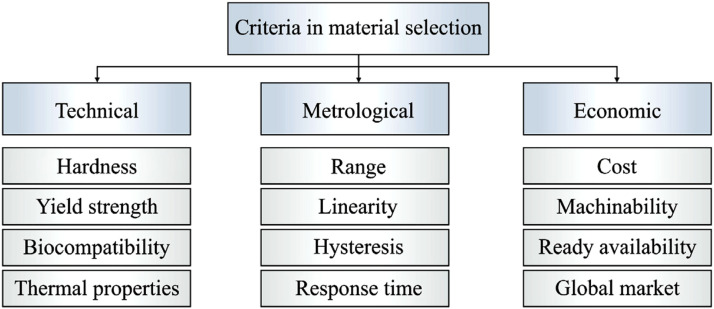
However, compared with the rapidly growing wearable device market, the development of wearable health care systems used in practical applications is slow, which can be attributed to the following challenges. Firstly, the health care system must be wearable, combined with skin or human body surface, with compatibility, durability, and abrasion resistance.33 Hence, brittle materials and integrated circuit technology usually used in semiconductor industry are not feasible. Secondly, the human body has very complex attributes. Recently, several good overviews have been reported on the advanced achievements in wearable sensors for health monitoring.34 Although material selection is an important issue in fabrication of different types of sensor, it has found a crucial role in fabrication of wearable health sensors. Owing to the applications of wearable health sensors, material selection significantly affects the performance of the sensor. Literature investigation indicates that different types of materials have been proposed for fabrication of prototypes suitable for different applications. It is noteworthy that based on the diversity of sensor technologies, sometimes demands can be answered via more than one type of sensor. This issue can affect the research and planning of wearable sensor materials, though this material selection ought to satisfy not only technical and metrological features but also economic criteria. In Figure 2, main criteria and some relevant sub-criteria in material selection of wearable health sensors are shown. It includes technical properties of the material, metrological, and economic issues. However, based on application of the sensor, other properties, such as elastic linearity, accuracy, and manufacturing aspects must be considered.35
Figure 2.
Main criteria in material selection for wearable health sensors.35
Materials used for wearable health care devices
In the recent years, the application of brittle and hard metals and silicon in wearable device needing large deformation has been limited. Table 1 includes a representative list of well-known, traditional materials that have been used in biomedical systems. A stretchable sensor with high performance and elastic mechanical response is an ideal choice for the next generation of health care applications.36 Commonly, metal foils, rubber, and elastic polymers are widely chosen as substrates because of their great mechanical elasticity, good chemical resistance, and thermal stability.37,38 For flexible wearable sensors, utilizing a flexible substrate is necessary in order to impart stability to the active material. In this respect, polyurethane, polydimethylsiloxane (PDMS), polyethylene naphthalate (PEN), polyethylene terephthalate (PET), and polyimide (PI) are most commonly used flexible substrates in wearable sensors for health monitoring.39 Most of the polymeric materials are soft, lightweight, RF-transparent, and low cost, and hence can address the current challenges associated with metallic and ceramic materials for implantable electronics.40
Table 1.
A summary of the traditional materials with applications in bioelectronics.36
| Materials | Properties | Device component | Applications |
|---|---|---|---|
| Silicon | Compatible with microfabrication | Substrate | Intraocular pressure and cardiovascular monitoring |
| Silicon | Compatible with microfabrication | Structural diaphragm | Blood pressure and shunt pressure sensor |
| Silicon oxide | High-quality factor | Structural diaphragm and substrate | Surface acoustic wave blood pressure sensor |
| Silicon nitride | Thermally stable | Dielectric layer | Orthopedic sensor |
| Silicon nitride | Thermally stable | Insulation layer | Cerebrospinal fluid flow monitoring |
| Stainless steel | Compatible with stents | Substrate | Capacitive pressure sensor |
Table 2 summarizes the list of applications of several important polymeric materials in flexible electronics. In addition to synthetic substrates, some natural materials have also been opened for manufacture of wearable system substrates. Biomaterial is the largest material system in nature. It has good biocompatibility, biodegradability, versatility, sustainability, and low cost.41 Fibers and textiles are ideal for wearable sensing systems because they are supposed to be the closest natural materials to human skin. For instance, natural silks are not only an abundant and attractive biomaterial, but also satisfy the mechanical requirements of irregular deformation.42 The next generation of wearable devices is expected to perform functions including recording more accurately. Therefore, all kinds of advanced materials will promote the innovation of wearable equipment with unique functions quickly, continuously, and predictably. Appropriate assembly methods and materials are essential for acquiring wearable sensors with good stability, high sensitivity, and strain range. In recent years, different kinds of materials, including nanowires (NWs,) metal nanoparticles (MNPs), conductive polymers (CPs), and carbon materials, have been widely used to manufacture wearable health care devices due to their remarkable mechanical and electrical characteristics.43–45 Compared with other candidates, advanced carbon-based materials such as carbon black nanoparticles (CBNPs), carbon-based nanofibers, graphene, and CNTs have unique advantages, including high chemical and thermal stability, good electrical conductivity, and easy to be functionalized, which give them great potential in wearable electronic products and applications.46,47 Graphene is another important carbon-based material for developing wearable health care systems. Because of its small size, strong mechanical properties, and excellent electrical conductivity, it can be used as an active sensing material for flexible sensors.48 Inorganic nanomaterials with strong adaptability, large surface area, excellent sensing performance, and compatibility with low-cost manufacturing process are widely used as components for the development of wearable sensors.49,50
Table 2.
Summary of organic materials with applications in biomedical devices.
| Materials | Properties | Device component | Applications |
|---|---|---|---|
| PDMS | Low modulus, high dielectric strength, and low chemical reactivity | Dielectric layer | Pressure and oxygen sensor in blood |
| Substrate layer | Physiological recording | ||
| PVDF | Piezoelectricity | Structural diaphragm | Intracranial and endovascular pressure monitoring |
| Polyimide (PI) | High heat resistance | Substrate layer | Intraocular and cardiovascular pressure monitoring |
| Structural diaphragm | Intraocular pressure monitoring |
PDMS: polydimethylsiloxane; PVDF: polyvinylidene fluoride.36
Metal possesses excellent electrical conductivity and has been widely used in wearable sensors. Specific to active material, metal often appears in the following forms: (1) nanowires or particles; (2) flexible or stretchable configurations; and (3) liquid state at room temperature. Nanowires (NWs) and nanoparticles (NPs) are often taken advantage of as fillers to prepare piezoresistive composites and conductive ink. Currently, a wide variety of nanomaterials have been used in fabrication of wearable temperature sensors. More in deep, graphene, conductive polymers, CNTs, nickel, and copper metal nanoparticles have been utilized as thermal sensing element.51–54 For flexible wearable sensors, utilizing a flexible substrate is necessary in order to impart stability to the active material. In this respect, polyurethane, PDMS, polyethylene terephthalate, Ecoflex, and polyethylene naphthalate are the most commonly used flexible substrate in wearable sensors for health monitoring.39 As most of the wearable health sensors are in connection with human skin, utilizing biocompatible materials is a vital issue. In this area, both inorganic piezoelectric materials (e.g., zinc oxide, lead zirconate titanate, and lithium niobate) and organic ones (e.g., poly-l-lactic acid, polyvinylidene fluoride, and poly-d-lactic acid) are biocompatible. These have been used in fabrication of piezoelectric sensors.55,56 It is notable that piezoelectric polymers have garnered noteworthy attention because of low-cost and ease of use. In wearable electromechanical sensors, polyvinylidene fluoride is the most extensively used flexible piezoelectric material. This material offers unique physical properties and semi-crystallinity, to its compact linear molecular structure. In addition to the mentioned inorganic and organic piezoelectric materials, silk is a flexible, natural, and great material for utilizing in textile-based wearable sensors. Based on piezoelectric property of silk, it can be used in different types of wearable sensors.55Table 3 (which is relevant throughout the previous paper) contains a condensed summary of details extracted from the literature, including information on materials, properties, general applications, and fabrication process.28
Table 3.
Summary of representative materials, substrates, mechanisms, and fabrication procedures.28
| Sensor type | Materials | Substrates | Mechanism | Fabrication |
|---|---|---|---|---|
| Respiratory/breath | Graphite, SiO2
Graphite Silicon-nanocrystal CNTs PVDF-TrFE ZnO, Au |
Cellulose
Acetate Paper PI PDMS PDMS PI (nanoporous) |
Humidity Conductometric Humidity Strain Piezoelectric Impedance |
Hand-painting Hand-painting Spin coating Laser Scribing Molding E-beam, Sputtering |
| Temperature | CaCl2, Aliphatic Diols Graphene, Ag, PDMS Graphene/PEDOT-PSS |
PLA PET Polyurethane |
Conductometric Resistive Resistive |
Injection Transfer Printing Inkjet Printing |
| Pressure and strain | MWCNTs, Al2O3, Cu, CNTs Conductive self-healing hydrogel SWCNT/paper, Au, PDMS |
PI PDMS PDMS PI |
Pressure/TFTs Piezoresistive Piezoresistive Piezoresistive |
ALD Vacuum Deposition Casting 3D printing E-beam evaporation |
| Hydration | Graphene, Ag/AgCl Ag, PDMS Ag/AgCl |
PMMA PDMS PET |
Impedance Impedance Electrochemical |
Wet transfer, Dry Patterning Drop Casting Screen Printing |
| Pulse rate | Graphene
oxide PEDOT-PSS, PVDF-TrFE PVDF-TrFE, Al, Ag Graphene oxide, Au |
PET, PI PEN PI Fabric (facemask) |
Conductometric Piezoelectric Piezoelectric Humidity |
Transfer printing Screen printing LBL Drop casting |
| Gas sensors | AgNPs, Carbon, CNT Reduced graphene Oxide Ag, Au |
Silk PET PI |
Chemirsistive Chemirsistive Chemirsistive |
Spray and Drop Coating Drop casting, Spin coating Inkjet printing |
| Alcohol/acetone | ZnO, TiO2, Cu Au, ZnO ITO, ZnO |
Alumina PI PET |
Chemiresistive Chemiresistive Chemiresistive |
Screen printing E-Bean, sputtering Drop casting, Laser ablation |
| Motion and activity Monitoring |
Carbon black Carbon, Ag MWCNT, Cu MWCNTs, |
Polyurethane
PDMS,Cotton PDMS Polyurethane |
Strain, conductivity
Strain Strain Piezoresistive |
Drop and dry
Impregnation, Casting Casting 3D printing |
Wearable health care devices and COVID-19
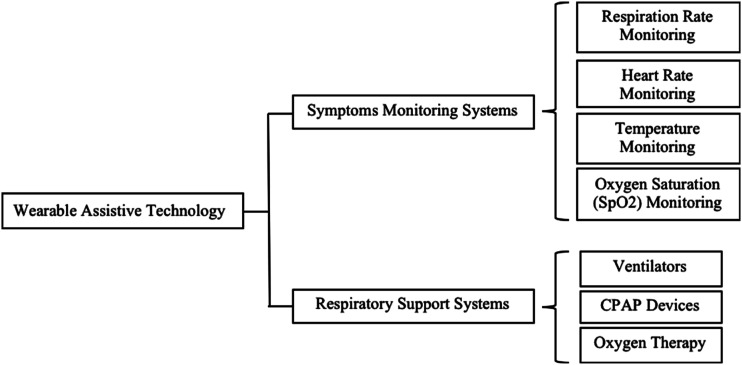
In the COVID-19 pandemic, wearable health care devices and nano-biosensors have gained significant publicity because of the contactless-based health care instructions. The wearable sensors are capable of measuring vital signals of the human physical body, for example, body temperature, respiratory rate, heart rate, blood pressure, skin coloration, sleep duration, and body motion. These measured parameters are clinically essential and can be gained through contactless processes.57 The wearable technology achieves a substantial role in the discovery of COVID-19 symptoms to assist the patients infected by this unusual virus. There are three signs that can be considered as key of coronavirus symptoms. These are respiratory distress/difficulty, fever, and cough.58 These signs are universal to all the clinical demonstrations of COVID-19. Hence, it is vital to assess respiratory, cardiovascular monitoring, and estimation of other parameters as body temperature and oxygen saturation (SpO2). Various investigations have been conducted based on the usage of wearable health care devices to handle the COVID-19 pandemic. Figure 3 offers an overview of the wearable assistive technology for the patients infected by COVID-19.59–64
Figure 3.
Overview of the wearable assistive technology for the patients infected with COVID-19.
Temperature measurement is very important for COVID-19 detection and has been used by many countries as an instant test to conclude if citizens have been infected with COVID-19. Many researchers have already offered wearable health care devices for continuous body temperature monitoring which can be intended for COVID-19 patients. Liu et al.65 offered a wearable device as a physiological monitoring system that monitors body temperature, electrocardiography (ECG), blood pressure, and some other physiological parameters. The proposed device is easy to use, and especially developed for home application that can be used for COVID-19 patients. Song et al.66 suggested a wearable system based on multiple artificial neural networks which monitors the body temperature very precisely with squatter reaction time. Zakaria et al.67 established the Internet of Things (IoT)-based body temperature monitoring, particularly for infants. The proposed device is lightweight, very small in size, and continuously monitors the body temperature and can be comfortably used by the baby. Kulkarni et al.68 proposed another IoT-based device named Health Companion using wearable computing which monitors the temperature and pulse. This proposed device aims to determine and collect different parameters of the human body. This assists the users to monitor their physical condition and aids the doctors to closely study the patients’ ailments. This device can be used for fever tracking for the period of illness.
Respiration rate (RR) for respiratory assessment is one of the greatest crucial parameters in COVID-19 infection finding as the virus has a severe effect on the lungs area. Liu et al.69 suggested an RR system which is used to be located on the upper lip which is mainly a flexible epidermal respiratory system based on the thermal convection. Charlton et al.70 suggested a system for RR estimation from electrocardiography (ECG) and photoplethysmogram (PPG) which improved the estimation accuracy. The advantage of the system is that it can be incorporated into commercial wearable health care devices, thus adding RR monitoring functionality in existing systems. Therefore, this technology would be very efficient for COVID-19 patients to monitor their RR. Tamilselvi et al.71 suggested a system for health monitoring which can monitor primary metrics of a patient, for example, body temperature, heart rate, eye movement, and percentage of oxygen saturation. Xue et al.72 established a wearable health care device that continuously monitors SpO2 and body temperature in real-time. Jarchi et al.73 proposed a wearable health care device for heart rate variability (HRV) and SpO2 estimation which used commercial wrist-worn pulse oximeter for attaining accurate results. Mujawar et al.62 discuss the nano material-based biosensor for health care monitoring and diagnosis of COVID-19 in supposed patients. The nano-biosensors contain the geno sensor and immuno sensor that are embedded on-chip to execute assessment of COVID-19 patients. The data collected from the sensors are additionally analyzed through artificial intelligence (AI) supported data processing and analysis algorithms. Interfacing of nano sensor-based bio chip with the IoT is identified as the Internet of Bio-Nano Things (IoBNT). This IoBNT can be used in many ways, for example, data sharing with other medical and health care centers across the globe, contact tracing, faster assessment of COIVD-19 infection, quarantine management, and targeted COIVD-19 patient sensing.
Wearable technologies enable the continuous monitoring of human physical activities and behaviors as well as physiological and biochemical parameters during daily life. Hence, wearable technologies have demonstrated a tremendous ability in dealing with infectious diseases like the new corona virus. There is no doubt wearable technologies can not only act as an early warning but also as lifesaving devices. When we go out from this crisis, it is very important that we should continue our undivided attention and research into these paradigm changes and technologies.
Medical textiles
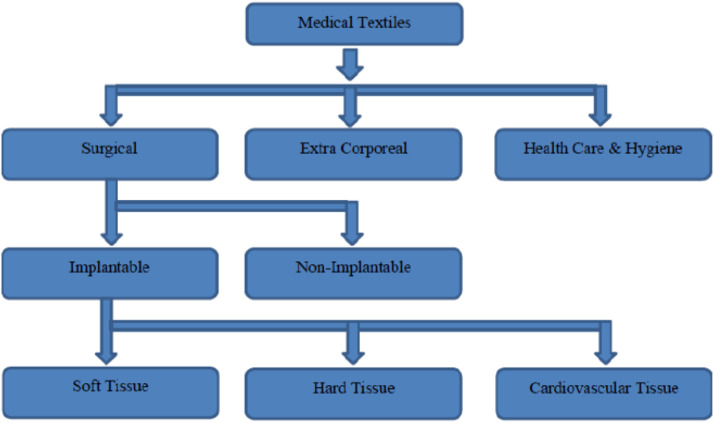
Medical textiles refer to a textile structure, which has been produced for use in any of a variety of medical applications. Medical textiles are a major growing area within the scope of technical textiles, which is defined as textile materials and products manufactured mainly for their technical performance and functional properties rather than their esthetic or decoration characteristics. Technical textiles include, in addition to medical textiles, marine, military, aerospace, industrial, safety, and transport textiles.74 Generally, textile materials have many special characteristics, for example, air permeability, strength, extensibility, flexibility, and availability in three-dimensional structures, variety in fiber length, fineness, cross-sectional shape, and absorbency. These features sort them suitable materials for medical applications. On the other hand, in some cases, different designs and characteristics or a combination of several features are required.75 Hence, it is necessary to develop the characteristics of a product based on its end use. High surface areas, absorbency characteristics, and large diversities in product forms donate to the emergence of additional smart products in the medical textile industry.
A number of surface modification and finishing techniques can considerably enhance some specific characteristics of textile materials such as blood coagulation, wound healing, anticoagulation, water and blood absorption, antimicrobial, and so on. Moreover, by using these modern technologies, we can impart improved multifunctional properties to a certain textile-based product. There are different applications for medical textiles including the application such as wound dressing, hygienic, and personal care products. In addition, hospital textiles such as bedding, clothing, surgical gowns, and hospital cloths are expected to fulfill comfort and hygienic properties such as moisture management, thermal conductivity, breathability, antimicrobial activity, and odor resistance.76,77 The classification of medical textile is denoted in Figure 4.78 Extensive progress in tissue engineering and nanotechnology has had a great influence on advanced medical textile products in these areas. On the other hand, the developments of biomaterials, nanomaterials, and biotechnology have led to fabrication of new polymers, hydrogels, composites, and fibrous structures with unique characteristics for different medical applications. Subsequently, with these developments in textile and medical industry, the risk of health care associated-infection and contagious diseases will decline. In contrast, patient compliance with medication and treatment and standard of living will grow.79
Figure 4.
Classification of medical textiles.78
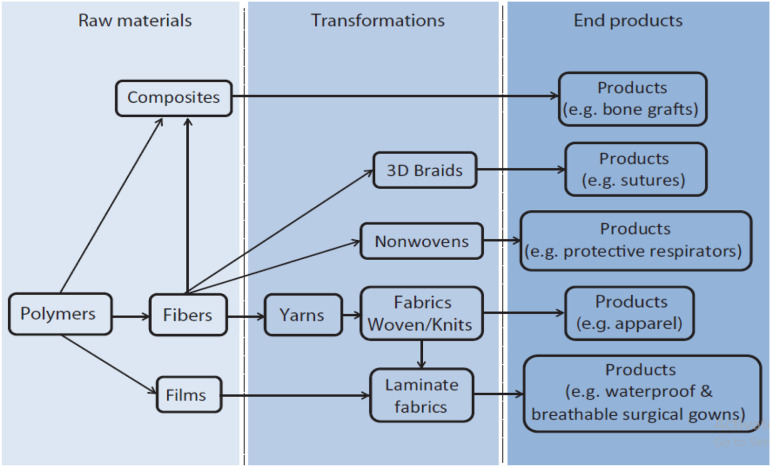
The market for functional textiles is steadily increasing due to the increased interest among people in personal health and hygiene products and a decrease in disposable time. On most of the occasions, natural fibers such as cotton, silk, lyocell, and other regenerated fibers are used to make the medical textiles. Due to the limitations of natural fibers in medical textiles, synthetic fibers were used for durable applications in the medical industry. Recently, the most widely used synthetic fibers in medical textiles are polyester, viscose, polyamides, and polypropylene. They are enormously improving and their blends are used for developing new products. Figure 5 shows that a chain of traditional textile transformation processes fibers composed of natural or synthetic polymers are turned into yarns, followed by being woven or knitted into fabrics and additional fabricated into specific products, containing apparel.78
Figure 5.
Process of medical textile production from polymers.78
New production methods have also been developed to create fibrous structures other than woven and knit. For example, nonwoven technology has aided the manufacturing of fabrics without the yarn spinning process, which not only significantly reduces production cost but also causes the end products to have porous and greatly absorbent structures to meet the requirement of hygiene products. The technology of electrospinning permits the production of ultrafine fibers in the size of nanometers, which is way beyond the capacity of traditional fiber spinning technology. Mixture of a fibrous material and another material such as polymer, metal, or ceramic helps produce various kinds of composite materials that will bring about a synergy between two dissimilar materials.80,81 Nanoparticles of metal oxides and ceramics have been used to vary surface properties and to impart textile functions. Photocatalytic activity of metal oxide nanoparticles such as TiO2 and MgO can destroy toxic chemicals and decompose organic matters in the air such as odor molecules, bacteria, and viruses. Moreover nanoparticles can convert fabrics into sensor-based materials, thus assisting them to convert exerted mechanical forces into electric signals and can therefore be used to monitor bodily functions such as heart rhythm and pulse if worn next to the skin.82 Nanotechnology deals the possibility of representation textiles certain properties that protect humans and their natural environment. Nanotechnology use in textiles further allows for the control of crystal structure, enhanced mechanical properties, enhanced resistance to chemicals, microbes, flame and heat, enhanced electrical properties, enhanced coloration, and production of self-cleaning clothing.83
Textiles have been improved using polymeric nanocomposites and metallic and inorganic nanostructured materials. Preceding researches have revealed bulk modification of filament yarns by various concentrations of nanocomposites fillers like Ag–Zn and Ag–TiO2, and various polymer powders by using different mixing methods. Nano titanium dioxide has been used to develop wrinkle resistance of cotton fabrics.84 Earlier, resin was used to impart wrinkle resistance, but it causes a reduction in abrasion resistance, tensile strength, and water absorbency. ZnO nanoparticles have been used to remove the UV component of sunlight, thereby decreasing the fading rate of the dyes used for textiles.85 TiO2 nanoparticles have been used with Ag to produce bactericidal textiles. The fabric modified with TiO2 is treated at a specific temperature to activate the bactericidal property and Ag was deposited on the activated cotton or polyester. This increases the bonding capacity of TiO2 and Ag with the textile surface by the induction of surface oxygen functionalities. Biocidal cotton bandages coated with CuO nanoparticles revealed killing of E. coli bacteria. Nanoactive materials have been confirmed to not only adsorb but also destroy a variety of chemicals containing chemical and biological warfare (CWA) and its simulants. New materials and methods for combining protective chemical additives into advanced fabrics are being established and tested for new-generation protective clothing that will provide barrier protection and detection, trapping, and decontamination of toxic particles, liquids, and vapors that contact these advanced fabrics.86
Smart textiles for medicine and health care
Current advances in nanotechnology, electronics, materials science, and the collaboration between scientists in these fields have caused the development of intelligent or smart textiles that can sense and/or respond to mechanical, light, thermal, chemical, electrical, and magnetic stimuli. This is possible because of, these stimuli are able to change the appearances (e.g., color) and/or structures of the smart materials integrated into the textiles during their fabrication, these changes will produce a warning signal (e.g., a flashing light). Smart textiles might have application in such end uses as sports/recreation or special work wear for first responders or for consumption in extreme environments (e.g., space exploration), where early signals of distress would aid timely interventions. Smart textiles for health care contain textile sensors, actuators, and wearable electronics systems implanted into textiles that enable registration and transmission of physiological data and wireless communication between the wearer and the operator, for example, patient and medical personnel. Such systems make sure patients’ mobility, thereby providing a greater level of psycho-physiological comfort, especially when a long-term bio-monitoring is required. Table 4 summarizes main applications fields of smart medical textiles.87,88 Smart devices made from intelligent textiles are estimated to provide remote monitoring of a patient’s physiological and physical data and signs through non-invasive sensors implanted in clothing materials. These data or signs may be used to support diagnosis and personalized management of chronic diseases like diabetes, arthritis, lung and heart disease, and hypertension. Such technologies allow patients to be treated at home instead of hospitals; they also allow quick detection of diseases and timely treatment.89,90
Table 4.
Applications of smart textiles for medicine and health care.89
| Application | In vitro | In vivo |
|---|---|---|
| Surgery | Bandages Wound care |
Sutures Soft tissues Orthopedic implants Cardiovascular implants |
| Hygiene | Uniform for medical personnel hospital textiles | — |
| Drug-release systems | Smart bandages and plasters | — |
| Bio-monitoring | Cardiovascular and hemodynamic
activity Neural activity Muscle activity and kinematics Respiratory activity Thermoregulation |
— |
| Therapy and wellness | Electrical stimulation
therapy Physiotherapy Auxiliary systems Active thermoregulation systems |
— |
Smart materials
Smart materials find application in hospital textiles and clothing for medical personnel. Moreover, functionality of these textiles can be obtained by different approaches according to specific applications. For this type of medical textiles though, functional textiles bring most solutions. For hospital textiles, those normally are textile materials with antimicrobial and antibacterial properties or low friction coating. Clothing for medical personnel is also made of functional textiles that assure efficient moisture transport and biological protection. However, conductive textile materials are more often used in fabricating of heating textiles that find applications in blankets for operating rooms. Moreover, conductive textile materials can be a benefit in improvement of distanced communication between medical personnel and patients through wearable technologies integrated into clothing. In addition, smart textiles deal solution for decubitus prophylaxis and associated health disorders which are a significant problem in the hospital environment. Currently, there are already a number of developments that contribute in managing these difficulties through innovative and smart textile solutions. Namely, those can be instigated by stimulating blood flow in sensitive areas through textile-based sensors and systems, optimizing and controlling moisture management through textile sensors.87 The most communally used materials for the sensor implementation are conductive textile materials. These materials can be yarns that ensure manufacturing of textile electrodes through such conventional textile manufacturing technologies as weaving, knitting, and embroidery. Another approach offers solutions implemented through inkjet and screen printing and thin film technologies such as sol–gel and sputtering methods.91 The textile electrodes fabricated by the mentioned conventional techniques demonstrate via higher efficiency in performance and usage (washing).
Medical textiles and COVID-19
From the time when the coronavirus outbreak started, the demand for personal protective equipment (PPE) has increased.92 PPE like protective suits, masks, gloves, face shields, and goggles aids in physically isolating the human body from viral infection. PPE is considered an important infection control measure.93,94 It has become a new normal in many societies in the COVID-19 pandemic. The surge in demand for surgical masks and respirators has led to a global shortage of resource and raw materials. Therefore, many people have resorted to produce their own masks, recycling used masks, or settling for masks providing less protection than actually needed. Researchers and industry actors have been working hard to address the issue of shortage as well as to enhance the protection afforded by existing mask models. These efforts include sourcing and engineering alternative materials with sufficient filtering capacity, engineering the design of masks and respirators for better protection, and user comfort, emergent and engineering multifunctional masks and materials with hydrophobic, self-disinfecting, antimicrobial and even sensing properties, and exploring novel technologies for efficient production and customization of masks.95,96
Materials science plays an essential role in the effective protection against COVID-19 virus by different means like isolation, disinfection, and inactivation.4 In the recent years, several studies have stated the filtration performance of natural polymer-based electrospun nanofiber membranes which established their potential to be used for filtration applications. Akduman et al.97 informed that as the fiber diameter decreases, the most penetrating particle size decreases and the capture efficiency of the utmost penetrating particle size rises. Nanofibers could be the main elements for filter materials in face masks or respirators. They have very great surface area per unit mass that improves capture efficiency and other surface area-dependent phenomena that might be engineered into the fiber surfaces. They might improve filter charactarestics for capture of naturally occurring nanoparticles such as viruses, as well as micron-sized particles such as bacteria.
Zhu et al.98 stated that the filtration membrane developed with chitosan-based natural biopolymer displayed excellent air and microbial filtration, while the addition of silica nanoparticles to the membrane improved the roughness, which more enhanced the filtering efficiency. Ahne et al.99 stated 99.8% filtration efficiency of the electrospun cellulose-based nanofiber. Leong et al.100 proposed cellulose-based nanofiber as a viable filtration medium over N95 masks. Soybean protein-based nanofiber textile was settled by Souzandeh et al.101 Desai et al.102 established chitosan and polyethylene oxide-based filter media using the electrospinning process whereby the properties were considered as a function of varying chitosan fiber content and fiber diameter. The investigation revealed that the size and content of the chitosan fibers were the dominant factors that influenced the filtration performance. Wang et al.103 compared the characteristics of silk nanofiber air filter membrane to the commercially existing KN90 respirator as well as the polypropylene nanofiber membrane. The silk nanofiber membrane revealed the same filtration characteristics as the commercially existing filter membranes. The findings of the study suggested the use of silk nanofiber as a suitable alternative to the petroleum-derived polypropylene for fabricating the air filter medium. Furthermore, some investigations reported the use of hybrid nanofibres in air filter applications in the current years.104,105 Developing a hybrid natural polymer-based biodegradable filter medium can boost the filtering properties and also help to achieve the preferred water resistance, microbial resistance, and mechanical strength properties.106 These findings establish the potential of the natural polymer-based nanofibres for use in air filtration applications that also may be considered to construct the filter material for face masks. Konda et al.107 verified multiple layers of silk, chiffon, and observed enhancement in filtration efficiency when more layers were stacked. They also tested several types of hybrid samples and establish that filtration efficiency enhanced slightly when cotton was used in combination with chiffon or silk, while the benefits from using polypropylene or cotton quilt were more noteworthy.
Hao et al.108 studied household air filters, vacuum bags, and coffee filters in adding to cloth materials. They detected that the performance of multiple layers of household air filter was comparable to N95 respirators or KN95 masks in terms of both filtration efficiency and flow resistance for particles in the range of 10–600 nm size. Drewnick et al.109 also stated that the performance of vacuum bag for particles in the range of 0.02–10 mm size was comparable to N95 respirators among the 44 household materials tested in their investigation. Zhang et al.110 fabricated an efficient air filter based on ionic liquid polymer (ILP) composite that was dispersed on the spongy network of melamine-formaldehyde (MF). Such type of masks retains nanofibrous filter which may filter out even nano sized particulates and let clean air for comfort in breath. In another investigation, a specialized mask was fabricated by combining a layer of cotton along with a layer of chargeable natural silk.111 The removal mechanism involves the combined action of mechanical and electrostatic filtration.
In recent times, we faced the problem of shortage of PPE kits for the duration of COVID-19 pandemic. Hence, the development of reusable masks, gloves, and other PPE is in continuous thrust. Tebyetekerwa et al.112 suggested the use of durable and yet reliable electrospun nonwoven filters with very small fiber diameters. The filter may be processed by suitable disinfection methods and protocols to achieve reuse without compromising the filtration efficiency. Beyond these, future face masks need to be antiviral as well as veridical. The present electrospinning technology is mature making the recommended strategy relatively low-cost with mass production capacity.
The surface treatment or the surface coating offers self-cleaning ability to the gloves, masks, and protective suits and consequently, made these protective tools reusable.113,114 Therefore, the filter of gloves, masks, and protective gown can be coated by graphene oxide to disinfect the virus. More recently, it has been stated that graphene coating increases the hydrophobicity of the surface of masks that restricts the viability of the virus on its surface. Furthermore, such type of graphene-coated masks can be reusable due to its excellent photothermal properties that make these masks self-sterilized in the exposure of sunlight.114 Atab et al.113 manufactured a polymeric membrane made of polyamide with intrinsic hydrophobicity which may easily bounce off the aqueous droplets of virus. Apart from hydrophobic surfaces, sunlight sterilization feature was also incorporated in a membrane, as settled by Zhong et al.35 For this purpose, graphene-coated masks have been prepared with highly hydrophobic surface and excellent photothermal properties, due to which the temperature of the outer layer of mask reaches 80°C and accordingly becomes sterilized in sunlight.114
Recent efforts have demonstrated the potential of reusable mask development enabled by material innovation and technology advancement in addressing the mask shortage while reducing the greenhouse gas (GHG) emissions and negative environmental impact. However, continuous efforts are needed to ensure feasible developments can be transit to existing manufacturing facilities. In addition, there are more scientific opportunities to progress new and environmentally friendly mask materials with functions of interests, such as self-sanitizing and degradable materials, and to develop a low energy consumption technique or process for a nonwoven fiber that could replace a carbon-intensive melt-blown process in the near future.96
Summary
The novel coronavirus disease (COVID-19) has caused great confusion around the world, affecting people’s lives and producing a large number of deaths. The development of portable and wearable devices is of great importance in several fields such as point-of-care medical applications and environmental monitoring. Wearable technologies employed in the health care sector for monitoring physiological parameters include body temperature, physical pressure, blood pressure, respiratory rate, humidity, heart rate (HR), skin conductance, and body movements. High performance and reliable wearable health care monitoring system requires flexible/stretchable sensors with different performances, containing the basic ones (sensitivity, linearity, hysteresis, response time, and durability) and specific ones (self-power, wireless communication, biocompatibility, and biodegradability). Continuing progress in the enhancement and combination of these properties has been further exciting the wearable sensors to appear in more health care applications. However, some challenges still exist in the intellectualization, the systematization, and mass production of wearable health care devices. The application of natural materials may afford more low-budget options and further diminish the economic burden. Wearable technologies allow the continuous monitoring of human physical activities and behaviors, as well as physiological and biochemical parameters during daily life. Hence, wearable technologies have demonstrated a tremendous ability in dealing with infectious diseases like the new corona virus. There is no doubt wearable technologies can not only act as an early warning but also as lifesaving devices. When we go out from this crisis, it is very important that we should continue our undivided attention and research into these paradigm changes and technologies.
In recent years, the results from the tremendous research in the field of material, surface, aerosol science, and engineering have enriched the textile materials with properties ( improved filtration, antibacterial and antiviral activity, breathability, etc.) crucial for successful prevention of the spread of infectious diseases. This fact is placing textiles on the front line in the fight against the current pandemic, and the textile industry is an important player since many textile companies are currently implementing the production of protective masks and protective clothing using their production facilities. Another specification of COVID-19 is the exponential growth in the number of new cases that can easily lead to systemic health care failure. Therefore, WHO recommends patients with mild symptoms and without cardinal chronic conditions to be cared for at home while keeping a communication link with the health care personnel. Here, the smart textile role for sensing and monitoring of body parameters as part of telemedicine could play an important role. Nanotechnology and smart textiles are promising in tackling the pandemic. Nanotechnology offers the possibility of rendering textiles certain properties that protect humans and their natural environment. Nanotechnology use in textiles further allows for the control of crystal structure, enhanced mechanical properties, enhanced resistance to chemicals, microbes, flame and heat, enhanced electrical properties, enhanced coloration, and production of self-cleaning clothing. Smart textiles find multiplicity applications and own sensing and actuating functions that can be professionally used in medicine. Finally, smart devices made from intelligent textiles are estimated to provide remote monitoring of a patient’s physiological and physical data and signs through non-invasive sensors implanted in clothing materials. These data or signs can be used to support diagnosis and personalized management of chronic diseases such as diabetes, arthritis, lung and heart disease, and hypertension. These technologies permit patients to be treated at home in its place instead of hospitals; they also let early detection of diseases and timely treatment.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Dalia Saber https://orcid.org/0000-0002-7349-1723
References
- 1.Shurbaji S, Ibrahim M, El-Sherbiny N, et al. Nitric oxide releasing hydrogel nanoparticles decreases epithelial cell injuries associated with airway. Reopening” Front Bioeng Biotechnol 2021; 8: 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nathan L, Plaskasovitis C, Stokes C, et al. 3D tissue models as an effective tool for studying viruses and vaccine development. Front Bioeng Biotechnol 2021; 8: 2021. [Google Scholar]
- 3.Sandhu A, Hany R, Hirohata A, et al. Global snapshot of the effects of the COVID-19 pandemic on the research activities of materials scientists between Spring and Autumn 2020. Sci Technol Adv Mater 2021; 22(1): 173–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abhinav S, Deepak K, Swati A, et al. Recent advances in materials science: a reinforced approach toward challenges against COVID-19. Emergent Mater 2021; 4: 57–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-qaness MA, Ewees AA, Fan H, et al. Optimization method for forecasting confirmed cases of COVID-19 in China. J Clin Med 2020; 9: 674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuminori T, Yukiko U, Soichi A, et al. Increased adhesion of methicillin-resistant Staphylococcus aureus to the surface of personal protective clothing damaged by friction during nursing action. Am J Infect Control 2020; 48: 416–419. [DOI] [PubMed] [Google Scholar]
- 7.Trung TQ, Ramasundaram S, Hwang BU, et al. An all-elastomeric transparent and stretchable temperature sensor for body-attachable wearable electronics. Adv Mater 2016; 28: 502–509. [DOI] [PubMed] [Google Scholar]
- 8.Ajami S, Teimouri F. Features and application of wearable biosensors in medical care. J Res Med Sci 2015; 20: 1208–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson EC, Verhagen T, Noordzij ML. Health empowerment through activity trackers: An empirical smart wristband study. Comput Hum Behav 2016; 62: 364–374. [Google Scholar]
- 10.Chuah HW, Rauschnabel PA, Krey N, et al. Wearable technologies: The role of usefulness and visibility in Smartwatch adoption. Comput Hum Behav 2016; 65: 276–284. [Google Scholar]
- 11.Constant N, Douglas-Prawl O, Johnson S, Mankodiya K.Pulse-Glasses: An unobtrusive,, wearable HR monitor with Internet-of-Things functionality. In: 2015 IEEE 12th International Conference on Wearable and Implantable Body Sensor Networks (BSN), 2015, pp. 1–5. doi: 10.1109/BSN.2015.7299350. [DOI] [Google Scholar]
- 12.Khandwalla RM, Birkeland K, Zimmer R, et al. Predicting heart failure events with home monitoring: Use of a novel wearable necklace to measure stroke volume, cardiac output and thoracic impedance. J Am Coll Cardiol 2016; 67: 1296. [Google Scholar]
- 13.Solovei D, Žák J, Majzlíková P, et al. Chemical sensor platform for noninvasive monitoring of activity and dehydration. Sensors 2015, 15: 1479–1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gao R, Emaminejad S, Nyein HYY, et al. Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis. Nature 2016; 529: 509–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bandodkar AJ, Wang J. Non-invasive wearable electrochemical sensors. A Review. Trends Biotechnol 2014; 32: 363–371. [DOI] [PubMed] [Google Scholar]
- 16.Huang H., Fan C., Li M., et al. COVID-19: A call for physical scientists and engineers. ACS Nano 2020; 14(4): 3747–3754. [DOI] [PubMed] [Google Scholar]
- 17.Weiss C., Carriere M., Fusco L., et al. Toward nanotechnology enabled approaches against the COVID-19 Pandemic. ACS Nano 2020; 14: 6383–6406. [DOI] [PubMed] [Google Scholar]
- 18.Yu Y.Y., Bu F., Zhou H., et al. Biosafety materials: an emerging new research direction of materials science from the COVID-19 outbreak. Mater Chem Front 1930; 4:2020. [Google Scholar]
- 19.Tang Z., Kong N., Zhang X., et al. A materials-science perspective on tackling COVID-19. Nat Rev Mater 2020; 5: 847–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chua MH, Cheng W, Kong J, et al. Face masks in the new COVID-19 normal: materials, testing, and perspectives. Research 2020; 7286735: 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goel S., Hawi S., Goel G., et al. Resilient and agile engineering solutions to address societal challenges such as coronavirus pandemic. Mater Today Chem 2020; 17: 100300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ivanoska-Dacikj A, Stachewicz U. Smart textiles and wearable technologies opportunities offered in the fight against pandemics in relation to current COVID-19 state. Rev Adv Mater Sci 2020; 59(487–505): 133. [Google Scholar]
- 23.Costa J, Adams AT, Jung MF. EmotionCheck “A wearable device to regulate anxiety through false heart rate feedback” Getmobile Mob. Comput Commun 2017; 21(2). 22–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flaura KW, Winston ACY. Wearable health device dermatitis: A case of acrylate-related contact allergy. Cutis 2017; 100: 97–99. [PubMed] [Google Scholar]
- 25.Xiqiu Hu A, Jingrong Cao B, Wua H, et al. A wearable device for collecting multi-signal parameters of newborn. Computer Commun 2020; 154: 269–277. [Google Scholar]
- 26.Wang X, Zheng L, Zhang T. Flexible sensing electronics wearable/attachable health monitoring. Small 2017; 13: 1602790. [DOI] [PubMed] [Google Scholar]
- 27.Sreenilayam SP, Inam U, Nicolosi V, et al. Advanced materials of printed wearables for physiological parameter monitoring. Mater Today 2020; 32: 147. [Google Scholar]
- 28.Khan S, Ali S, Berma A. Recent Developments in Printing Flexible and Wearable Sensing Electronics for Healthcare Applications. Sensors 2019; 19: 1230. 10.3390/s19051230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Y, Wang H, Zhao W, et al. Stretchable sensors for wearable health monitoring: sensing mechanisms, materials, fabrication strategies and features. Sensors 2018; 18: 645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu Q., Tai H., Yuan Z., et al. A high‐performances flexible temperature sensor composed of polyethyleneimine/reduced graphene oxide bilayer for real‐time monitoring. Adv Mater Technol 2019; 4: 115. [Google Scholar]
- 31.Tian X, Lee PM, Tan YJ, et al. Wireless body sensor networks based on metamaterial textiles. Nat Electron 2019; 2: 243–251. [Google Scholar]
- 32.Nightingale AM, Leong CL, Burnish RA, et al. Monitoring biomolecule concentrations in tissue using a wearable droplet microfluidic-based sensor. Nat Comm 2019; 10(12): 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Acar G, Ozturk O, Golparvar AJ, et al. Wearable and flexible textile electrodes for biopotential signal monitoring. A review. Electronics 2019; 8: 479. [Google Scholar]
- 34.Zheng Loua D, Wangb L, Jiang K, et al. Reviews of wearable healthcare systems: Materials, devices and system integration. Mater Sci Eng R 2020; 140: 147. [Google Scholar]
- 35.Nasiri S, Reza M, Khosravani R. Progress and challenges in fabrication of wearable sensors for health monitoring. Sensors Actuators A 2020; 312: 112105. [Google Scholar]
- 36.Chen Y, Kim Y-S, Tillman BW., et al. Recent low-profile implantable bioelectronics. Adv Mater 2018; 11: 522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Munief W-M, Lanche R, Lu X, et al. Wafer-scale fabrication of microelectrode arrays on optically transparent polymer foils for the integration of flexible nanoscale devices. Flexible Printed Electron 2018; 3: 044001. [Google Scholar]
- 38.Maghsoudi K, Vazirinasab E., Jafari R., et al. Evaluating the effect of processing parameters on the replication quality in the micro compression molding of silicone rubber. Mater Manuf Process 2020; 35(14): 1567–1575. [Google Scholar]
- 39.Kim S., Zhang X., Daugherty R., et al. Design and implementation of electrostatic micro-actuators inultrasonic frequency on a flexible substrate. PEN (Polyethylenenaphthalate)” Sens Actuators A 2013; 195: 198–205. [Google Scholar]
- 40.Go M, Hwang B, Lim S. Highly reliable mulberry paper (Hanji)-based electrode with printed silver nanowire/zinc oxide hybrid for. Soft Electronics. Mater Manuf Process 2019; 34(14): 1605–1611. [Google Scholar]
- 41.Wang L, Chen D, Jiang K, et al. New insights and perspectives into biological materials for flexible electronics. Chem Soc Rev 2017; 46: 6764–6815. [DOI] [PubMed] [Google Scholar]
- 42.Fan S, Zhang Y, Huang X, et al. Silk materials for medical, electronic and optical applications. Sci China Technol Sci 2019; 62: 903–918. [Google Scholar]
- 43.Liu Z, Xu J, Chen D, et al. Flexible electronics based on inorganic nanowires. Chem Soc Rev 2015; 44: 161–192. [DOI] [PubMed] [Google Scholar]
- 44.Lou Z, Shen G. Flexible Electronics: Flexible Photodetectors Based on 1D Inorganic Nanostructures. Adv Sci 2016; 3: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hu X, Li G, Zhu P, et al. Facile and scalable fabrication of self-assembled Cu architecture with superior antioxidative properties and improved sinterability as a conductive ink for flexible electronics. Nanotechnology 2019; 30: 127. [DOI] [PubMed] [Google Scholar]
- 46.Singh E, Meyyappan M, Nalwa HS. Flexible graphene-based wearable gas and chemical sensors. ACS Appl Mater Int 2017; 9: 34544–34586. [DOI] [PubMed] [Google Scholar]
- 47.Zhilyaeva MA, Shulga EV, Shandakov SD, et al. A novel straightforward wet pulling technique to fabricate carbon nanotube fibers. Carbon 2019; 15069–75. [Google Scholar]
- 48.Wang C, Xia K, Wang H, et al. Advanced Carbon for Flexible and Wearable Electronics. Adv Mater 2019; 31. [DOI] [PubMed] [Google Scholar]
- 49.Gai M, LI L, Song Y. Inkjet printing wearable electronic devices. J Mater.Chem C 2017; 5: 2971–2993. [Google Scholar]
- 50.Nasei S, Song Y, Wang Y, et al. Micro additive manufacturing of glucose biosensors: A feasibility study. Anal Chim Acta 20181043: 142–149. [DOI] [PubMed] [Google Scholar]
- 51.Lou Z, Chen S, Wang L, et al. Ultra sensitive and ultra flexible e-skins with dual functionalities forwearable electronics. Nano Energy 2017; 38: 28–35. [Google Scholar]
- 52.Tang Z, Yao D, Hu S, et al. Highly conductive, washable and super-hydrophobic wearable carbonnanotubes e-textile for vacuum pressure sensors. Sens Actuators A 2020; 303: 112. [Google Scholar]
- 53.Jin Y, Boon EP, Le LT, et al. Fabric-infused array of reduced grapheneoxide sensors for mapping of skin temperatures. Sens Actuators A 2012; 280: 92–98. [Google Scholar]
- 54.Shaikh TN, Chaudhari SB, Pate H, et al. Gauging performance of biosynthesized silver nanoparticles loaded polypropylene nonwoven based textile electrodes for 3-lead health monitoring electro cardiogram on analogous system. J Ind Textiles 2021; 13: 227. [Google Scholar]
- 55.Ma X, Zhang X, Fang P. Flexible film-transducers based on Polypropylene piezo electrets: fabrication, properties, and applications in wearable devices. Sens Actuators A 2017; 256: 35–42. [Google Scholar]
- 56.Hamid HMA, Celik Butler Z. Characterization and performance analysis of Li-doped ZnO nanowire as a nano-sensor and nano-energy harvesting element. Nano Energy 2018; 50: 159–168. [Google Scholar]
- 57.Krishnamurthi R, Gopinathan D, Kumar A.(2021) Wearable Devices and COVID-19: State of the Art, Framework, and Challenges. In: Al-Turjman F, Devi A, Nayyar A. (eds) Emerging Technologies for Battling Covid-19. Studies in Systems, Decision and Control, vol 324. Cham: Springer. [Google Scholar]
- 58.Liu Y, Yan L-M, Wan L, et al. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis 2020; 20; 656–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nilashi M, Asadi S, Abumalloh RA, et al. Intelligent recommender systems in the COVID-19 outbreak: The case of wearable healthcare devices. J Soft Comput Decis Support Syst 2020; 7(48–12): 119. [Google Scholar]
- 60.Tripathy AK, Mohapatra AG, Mohanty SP, et al. EasyBand: a wearable for safety-aware mobility during pandemic outbreak. IEEE Consum Electron Mag 2020; 47: 777–780. [Google Scholar]
- 61.Mohammed MN, Syamsudin H, Al-Zubaidi S, et al. Novel COVID-19 detection and diagnosis system using IOT based smart helmet. Int J Psychosoc Rehabil 2020; 24(7). [Google Scholar]
- 62.Mujawar MA, Gohel H, Bhardwaj SK, et al. Aspects of nano-enabling biosensing systems for intelligent healthcare; towards COVID-19 management. Mater Today Chem 2020; 17: 100306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alwashmi MF. The use of digital health in the detection and management of COVID-19. Int J Environ Res Public Health 2020; 17(8): 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Islam M, Mahmud S, Muhammad LJ, et al. Wearable technology to assist the patients infected with novel coronavirus (COVID-19)” SN COMPUT. SCI 2020; 1: 320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu B, Zhang Y, Liu Z. Wearable monitoring system with multiple physiological parameters5th International Summer School and Symposium on Medical Devices and Biosensors. IEEE 2008; 268–271: 2008. [Google Scholar]
- 66.Song C, Zeng P, Wang Z, et al. Wearable continuous body temperature measurement using multiple artificial neural networks. IEEE Trans Ind Inf 2018; 14: 4395–4406. [Google Scholar]
- 67.Zakaria NA, Mohd Saleh FNB, Razak MAA. IoT (internet of things) based infant body temperature monitoring. In: 2nd International Conference on BioSignal Analysis, Processing and Systems (ICBAPS). IEEE2018; 148–153. [Google Scholar]
- 68.Kulkarni C, Karhade H, Gupta S, et al. Health companion device using IoT and wearable computing. In: International Conference on Internet of Things and Applications (IOTA). IEEE2016; 152–156. [Google Scholar]
- 69.Liu Y, Zhao L, Avila R, et al. Epidermal electronics for respiration monitoring via thermo-sensitive measuring. Mater Today Phys 2016; 13: 100199. [Google Scholar]
- 70.Charlton PH, Birrenkott DA, Bonnici T, et al. Breathing rate estimation from the electrocardiogram and photoplethysmogram: a review. IEEE Rev Biomed Eng 2018; 11(2–20): 245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tamilselvi V, Sribalaji S, Vigneshwaran P, et al. IoT based health monitoring system. In: 2020 6th International Conference on Advanced Computing and Communication Systems (ICACCS). IEEE2020; 386–389. [Google Scholar]
- 72.Xue J, Huang Y, Du X, et al. Design of a wearable device for monitoring SpO2 continuously. In: 2015 IEEE 12th Intl Conf on Ubiquitous Intelligence and Computing and 2015 IEEE 12th Intl Conf on Autonomic and Trusted Computing and 2015 IEEE 15th Intl Conf on Scalable Computing and Communications and Its Associated Workshops (UIC-ATC-ScalCom). IEEE2015; 1253–1257. [Google Scholar]
- 73.Jarchi D, Salvi D, Velardo C, et al. Estimation of HRV and SpO2 from wrist-worn commercial sensors for clinical settings. In: 2018 IEEE 15th International Conference on Wearable and Implantable Body Sensor Networks (BSN). IEEE2018; 144–147. [Google Scholar]
- 74.Denton MJ. Textile Terms and Definitions”. 11th EdManchester, UK: Textile Institute, 2002. [Google Scholar]
- 75.Kandhavadivu P, Vigneswaran C, Ramachandran T, et al. Development of polyester-based bamboo charcoal and lyocell-blended union fabrics for healthcare and hygienic textiles”. J Ind Textiles 2002; 41(2): 142–159. [Google Scholar]
- 76.Czajka R. Development Medical Textile Market. Fibre Text East Eur 2005; 13(1): 1–49. [Google Scholar]
- 77.Anahita RS, Alireza N. “Medical Textiles” Advances in Functional and Protective Textiles. Manchester, UK: Woodhead Publishing, 2020. [Google Scholar]
- 78.Akter S, Abu Yousuf Md, Abdullah Al. Faruque “Medical Textiles: Significance And Future Prospect In Bangladesh”. Eur Scientific J 2014; 10(12 I): 54. [Google Scholar]
- 79.Janarthanan M, Kumar MS. The properties of bioactive substances obtained from seaweeds and their applications in textile industries”. J Ind Textiles 2018; 48(1): 361–401. [Google Scholar]
- 80.Mao N. Methods for characterisation of nonwoven structure, property, and performance. In: Kellie G. (ed). Advances in Technical Nonwovens. Amsterdam: Elsevier; 2016. ch 6. [Google Scholar]
- 81.Hutten IM. Handbook of Nonwoven Filter Media. Oxford: Elsevier, 2016. ch.8. [Google Scholar]
- 82.Wong YWH, Yuen CWM, Leung MYS, et al. Selected applications of nanotechnology in textiles. AUTEX Res J 2006; 61–8. [Google Scholar]
- 83.Jaworek A, Krupa A, Lackowski M, et al. Nanocomposite fabric formation by electrospinning and electrospraying technologies. J Electrostat 2009; 67: 435–438. [Google Scholar]
- 84.Dastjerdi R, Mojtahedi MRM, Shoshtari AM, et al. Fiber to fabric processability of silver/zinc loaded nanocomposite yarns. Text Res J 2009; 79(12): 1099. –1107. [Google Scholar]
- 85.Suna L, Rippona JA, Cookson PG, et al. Effects of undoped and manganese-doped zinc oxide nanoparticles on the colour fading of dyed polyester fabrics. Chem Eng J 2009; 147: 391–398. [Google Scholar]
- 86.Richard Chandrasekaran YZ, Ramakrishna S. An update on nanomaterials-based textiles for protection and decontamination. J Am Ceram Soc 2010; 93(12): 3955–3975. [Google Scholar]
- 87.Lenting H. Seminar: Medical Smart Textiles” Chances, Challenges and Medical Needs. November 15, 2012. Multifunctional Medical Textiles for Wound Prevention and Improved Decubitus Wound Healing: Research Results and Experiences on the Road of Implementation Aachen: Insitut fuer Textiltechnik, 2010. [Google Scholar]
- 88.Li H, Yang H, Li E, et al. Wearable sensors in intellegent clothing for measuring human body temperature based on fiber bragg grating. Opitics Express 201220: 11. [DOI] [PubMed] [Google Scholar]
- 89.Viktorija M, Hoerr M, Krieviņš I, et al. Smart textiles for healthcare: applications and technologies. Jelgava 2014; 7:802. [Google Scholar]
- 90.Cherenack K, van Peterson L.Smart textiles: Challenges opportunities. J Appl Phys 2012; 112: 1–14. [Google Scholar]
- 91.Xie L, Yang G, Xu L, et al. Characterization of dry biotential electrodes. In 35th Annual International Conference of the IEEE EMBS.Osaka, Japan. 2013, pp. 1478–1482. [DOI] [PubMed] [Google Scholar]
- 92.Willsher K, Holmes O, McKernan B, et al. US hijacking mask shipments in rush for coronavirus protection. The Guardian. Guardian News & Media Limited London, April 3, 2020 https://www.theguardian.com/world/2020/apr/02/global-battle-coronavirus-equipment-masks-tests [Google Scholar]
- 93.Leung NHL, Chu DKW, Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med 2012; 26(5): 676–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Eikenberry SE, Mancuso M, Iboi E, et al. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis Model 2020; 5: 293–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Swennen GRJ, Pottel L, Haers PE. Custom-made 3D-printed face masks in case of pandemic crisis situations with a lack of commercially available FFP2/3 masks. Int J Oral Maxillofacial Surg 2020; 49(5): 673–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chua MH, Cheng W, Simin Goh S, et al. Face masks in the new COVID-19 normal: Materials, testing, and perspectives. AAAS Res 2020; 7286735: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Akduman C, Akcakoca Kumbasar EP. Nanofibers in face masks and respirators to provide better protection. In 18th World Textile Conference. AUTEX; 2018. [Google Scholar]
- 98.Zhu M, Xiong R., Huang C.Bio-based and photocrosslinked electrospun antibacterial nanofibrous membranes for air filtration Carbohydr. Polym 2019; 55: 205. [DOI] [PubMed] [Google Scholar]
- 99.Ahne J, Li Q, Croiset E, et al. Electrospun cellulose acetate nanofibers for airborne nanoparticle filtration. Text. Res J 2019; 89: 3137. [Google Scholar]
- 100.“Regeneration of α-Cellulose Nanofibers Derived from Vegetable Pulp Waste to Intercept Airborne Microparticulates”, In IRC-SET 2018; Springer Singapore, 2019; pp. 235. [Google Scholar]
- 101.Souzandeh H, Johnson K. S, Wang Y, et al. Soy-protein-based nanofabrics for highly efficient and multifunctional air filtration. ACS Appl Mater Int 2016; 8: 20023–20031. [DOI] [PubMed] [Google Scholar]
- 102.Desai K, Kit K, Li J, et al. Nanofibrous chitosan non-wovens for filtration applications. Polymer 2009; 50: 3661. [Google Scholar]
- 103.Wang C, Wu S, Jian M, et al. Silk nanofibers as high efficient and lightweight air filter. Nano Res 2016; 9: 2590–2597. [Google Scholar]
- 104.Hamid S, Molki B, Zheng M, et al. Cross-linked protein nanofilter with antibacterial properties for multifunctional air filtration. ACS Appl Mater Inter 2017; 9(27): 22846–22855. [DOI] [PubMed] [Google Scholar]
- 105.Souzandeh H, Scudiero L, Wang Y, et al. A disposable multi-functional air filter: Paper towel/protein nanofibers with gradient porous structures for capturing pollutants of broad species and sizes. ACS Sustain Chem Eng 2017; 5: 6209–6217. [Google Scholar]
- 106.Souzandeh H, Wang Y, Netravali A. N, et al. Towards sustainable and multifunctional air-filters: A review on biopolymer-based filtration materials. Polym Rev 2019; 59: 651. [Google Scholar]
- 107.Konda A, Prakash A, Moss GA, et al. Response to letters to the editor on aerosol filtration efficiency of common fabrics used in respiratory cloth masks: Revised and expanded results. ACS Nano 2020; 14(9): 10764–10770. [DOI] [PubMed] [Google Scholar]
- 108.Hao W, Parasch A, Williams S, et al. Filtration performances of non-medical materials as candidates for manufacturing facemasks and respirators. Int J Hyg Environ Health 2020; 229: 113582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Drewnick F, Pikmann J, Fachinger F, et al. Aerosol filtration efficiency of household materials for homemade face masks: Influence of material properties, particle size, particle electrical charge, face velocity, and leaks. Aerosol Sci Technol 2021; 55(163–67): 123. [Google Scholar]
- 110.Zhang GH, Zhu Q-H, Zhang L, et al. High-performance particulate matter including nanoscale particle removal by a self- powered air filter. Nat Commun 2020; 11: 1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Konda A, Prakash A, Moss GA, et al. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano 2020; 14: 6339–6347. [DOI] [PubMed] [Google Scholar]
- 112.Tebyetekerwa M, Xu Z, Yang S, et al. Electrospun nanofibers-based face masks. Adv Fiber Mater 2020; 2: 161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Atab EN, Qaiser N, Badghaish HS, et al. A flexible nanoporous template for the design and development of reusable anti-COVID-19 hydrophobic face masks. ACS Nano 2020; 14: 7659–7665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhong H, Zhu Z, Lin J, et al. Reusable and recyclable graphene masks with outstanding superhydrophobic and photothermal performances. ACS Nano 2020; 14: 6213–6221. [DOI] [PubMed] [Google Scholar]