Summary
The competency-based undergraduate curriculum reform at the University of Medicine and Pharmacy at Ho Chi Minh City, Faculty of Medicine (UMP-FM) is detailed and reviewed in reference to the instructional and institutional reforms, and enabling actions recommended by the Lancet 2010 Commission for Health Professional Education. Key objectives are to: revise the overall 6-year curriculum to be more integrated and competency-based; reinforce students’ knowledge application, problem-solving, clinical competence, self-directed learning and soft skills; develop a comprehensive and performance-based student assessment programme; and establish a comprehensive quality monitoring programme to facilitate changes and improvements. New features include early introduction to the practice of medicine, family- and community-based medicine, professionalism, interprofessional education, electives experiences, and a scholarly project. Institutional reform introduces a faculty development programme, joint planning mechanism, a “culture of critical inquiry”, and a transparent faculty reward system. Lessons learnt from the curriculum reform at UMP-FM could be helpful to medical schools from low- and middle-income countries considering transitioning from a traditional to a competency-based curriculum.
Funding
This work receives no external funding.
Keywords: Medical education reform, Curriculum development, Curriculum implementation, Curriculum governance, Institutional governance, Organisational structure, Faculty development, Clinical competence, Competency-based education, Health professional education
Background and rationale
Modern medical education in Viet Nam started in the early twentieth century. Historically, this followed Flexner's model,1 and was centred around science-based education, focused on theory and hospital-based practice, was teacher-centred, and had no integration between basic and clinical science.
An important strength of the pre-reform curriculum at UMP-FM was the start of clinical experiences in the second year of medical school. Weaknesses in the preclinical years included a lack of integrated curriculum and an overloaded curriculum. There was a heavy reliance on traditional lectures and passive learning that was predominantly teacher-focused. Furthermore, there was no specific emphasis on students’ abilities to use and apply knowledge towards problem-solving.
The pre-reform clinical curriculum relied on multiple short clinical subspecialities courses, focussed more on in-hospital than community/outpatient care, and had a high student-to-faculty ratio. There was a lack of emphasis on soft skills such as professionalism, communication, doctor-patient relationship, teamwork, lifelong learning, and medical ethics. These, coupled with the lack of a comprehensive and efficient monitoring and assessment system, resulted in an inability to assess adequately and ensure the validity of students’ learning and clinical competence. Finally, there were no student electives, and teaching of certain topics was compulsory in Viet Nam such as National Defence, Marxist-Leninist philosophy, and Ho Chi Minh's ideology.
Although medical curriculum reform at University of Medicine and Pharmacy at Ho Chi Minh City, Faculty of Medicine (UMP-FM) was not based on the Lancet Commission for Health Professional Education “Reforms for a second century”,2 several reform processes/activities are consistent with the Commission's recommendations. This case study uses recommendations regarding instructional and institutional reforms, enabling actions2 and intended goals as a framework to review components of curriculum reform at UMP-FM, and evaluates progress at twelve years after conception, development and implementation.
The goal was to transition from a discipline- and knowledge-based curriculum to an integrated, system- and competency-based curriculum. Key features include: vertical and horizontal curriculum integration; student-centred approach; emphasis on primary care, professionalism and interprofessional education; more practice- (versus theory-) based training; expansion from hospital-based to hospital- and community-based practice; self-directed learning process; reducing curriculum overload; increasing time for self-directed learning; formative and summative performance-based assessment; and just-in-time faculty feedback to evaluate student competencies.
Context, event, and strategic plan
Over the past 20 years, with the support of the Vietnamese Ministry of Health (MoH), several international medical institutions and organisations have initiated various projects in collaboration with medical universities in Viet Nam, including the development of expected learning outcomes for medical school graduates,3 and the expansion of primary care and family medicine curriculum programmes.4,5 However, these programmes were not truly implemented and integrated into the existing curricula. Possible explanations include not integrating the changes within each institution's “bottom-up and top-down inputs”, not utilising “active involvement of stakeholders” and motivational strategies,3 and/or being consistent with factors considered to favour successful curricular changes.6
Timeline
In 2000, the UMP-FM's Vision and Strategic Development Plan Towards 2020 affirmed the need for medical curriculum innovation.7 In June 2010, a faculty conference was held to review the progress of medical education improvement at UMP since 2000. The then UMP President called on the faculty to renew the medical curriculum because both faculty and students considered it to be unnecessarily overloaded and redundant. Most importantly, it was recognised that UMP needed to review and renew itself to uphold the quality of its training.
Efforts to initiate the curriculum review process started with visits by the Medical Education Core Group to Gadjah Mada University (GMU) and Padjadjaran University (PU) in Indonesia (2010), Harvard Medical School (HMS, 2011) and the University of Geneva Faculty of Medicine (UGFM, 2012). There, UMP leaders observed and discussed their curriculum reform model and processes,8,9 and explored directions and potential partnerships. The decision to proceed with curriculum reform was reached after several conferences and a decisive meeting with the HMS faculty in September 2012. Subsequently, an international consultant from UGFM was recruited. Next, UMP-FM and the Health Advancement in Viet Nam (HAIVN) consulting group organised a conference with HMS and UGFM consultants in October 2013 to present the needs and key changes of a curriculum reform to the faculty to secure their understanding and support. The conference concluded with the MoH's full support and the faculty voting for curriculum reform. Later in 2013, a Project Management Unit was established, and UMP-FM decided to work towards overall reform of its 6-year medical education curriculum, supported by faculty members, institution leadership, and relevant stakeholders.
In May 2014, the World Bank (WB) approved a loan to the MoH to support health professional education reform.10,11 This provided a timely opportunity for UMP-FM to apply for the financial support needed for its curriculum reform.11 Based on its 2014 strategic plan, the application addressed the national needs to train a new generation of Vietnamese physicians to meet the country's future healthcare needs, increasing demand for equal access to quality care, and the International Cebu Declaration towards an ASEAN Community in 2015.12
Events
Several events reinforced UMP-FM curriculum reform initiatives. In May 2015, MoH released the Basic Competency Standards for General Practitioners (Table S1) and detailed its intention to introduce a Vietnamese, national and standardised medical certification examination by 2028. This alignment of the national and institutional priorities supported UMP-FM to make its “Plan of Medical Education Quality Improvement” a key institutional development project for 2014–2020. UMP-FM collaborated with international consultants at UGFM and HMS-HAIVN to develop a master plan for curriculum reform.
The concordant timelines of UMP-FM institutional initiatives for curriculum reform, MoH national schemes and support of healthcare training, international support and collaborations, and the WB loan to Viet Nam's project Heath Professionals Education and Training for Health System Reform (HPET), all played a crucial part in facilitating the reform process at UMP-FM. In contrast to other projects, a large proportion of the grant money was used to prepare and train faculty and staff to curriculum changes (rather than invested in capital purchases, such as equipment). Through the HPET project, we were able to create and train a group of local experts who in turn could work together with international experts to help other medical schools to reform their curriculum.
Plan
The Curriculum Reform Master Plan included the following principles:
-
1.
Innovating the 6-year medical education programme based on an integrated, system- and competency-based curriculum, and hospital- and community-based practice.
-
2.
Developing students’ standard clinical competencies and soft skills.
-
3.
Developing a systematic and comprehensive competency-based assessment programme.
-
4.
Developing lecturers’ teaching capacity.
-
5.
Building infrastructure to support activities of the renewed programme.
-
6.
Establishing a comprehensive internal and external quality assurance to facilitate required changes and continuous improvements.
-
7.
Developing necessary institutional reforms and organisational structures to lead, support, promote, implement and sustain the reform activities and processes.
Based on the experience at UGFM and HMS, we adopted Kotter's eight steps of leading change13 to create a climate of change, engage and enable the organisation, and implement and sustain institutional changes.
Implementation
Instructional reform
Competency-based and integrated curriculum
The reform objectives are to: (1) revise the 6-year curriculum to be more integrated, system- and competency-based; (2) reinforce students’ knowledge application, problem-solving, clinical competence, interprofessional teamwork and soft skills; (3) provide early introduction to the practice of medicine; (4) focus on family/community medicine to address Viet Nam healthcare needs;14 and (5) develop a comprehensive, performance-based student assessment programme.
There are several reasons for UMP-FM to adopt an integrated system- and competency-based curriculum: 1) it is consistent with the national “Basic competency standards for General Practitioners” (MoH, 2015);15 2) it supports the goal of creating competent physicians to serve and advance Viet Nam healthcare system; and 3) it allows consultants from UGFM and HMS to share their expertise and experiences with similar curricula. The competency-based medical education (CBME) curriculum was developed based on five competency domains outlined by the MoH: medical knowledge/skills, patient care, medical ethics/professionalism, communication/collaboration, and system-based practice.15
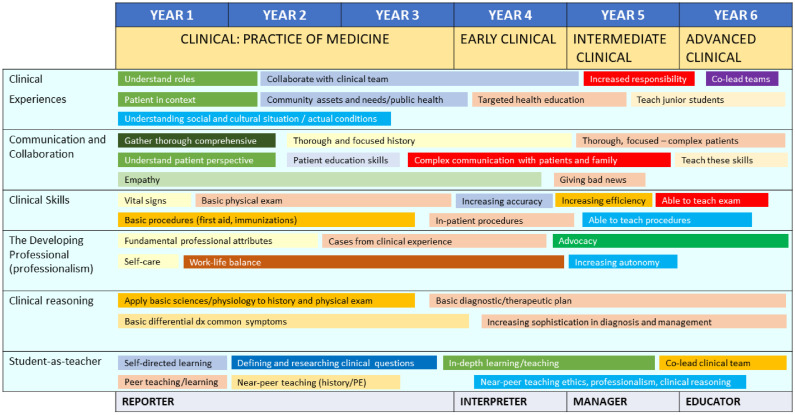
The 6-year programme includes a preclinical and clinical phase (three years each). The new curriculum includes eleven expected learning outcomes (ELOs) (Table 1). The curriculum is matched with the ELOs in a matrix, with competencies built up over time using the RIME (Reporter, Investigator, Manager, and Educator) model (Figure 1).16
Table 1.
Expected learning outcomes (ELOs) for a medical doctor.
| KNOWLEDGE | |
|---|---|
| ELO1 | Apply basic medical scientific knowledge, basic medicine and clinical medicine in healthcare practice |
| ELO2 | Apply evidence-based medicine in medical practice |
| ELO3 | Apply knowledge of health promotion and disease prevention in individual and community healthcare |
| SKILL | |
|---|---|
| ELO4 | Perform physical examination, a clinical history interview, synthesise and interpret clinical and paraclinical information to make accurate diagnosis of common diseases |
| ELO5 | Establish a comprehensive and appropriate treatment plan, following the patient-centred principle |
| ELO6 | Perform first aid and treat patients in accordance with the role and functions of medical doctors: ensure continuous, safe and effective care |
| ELO7 | Identify common health problems in the community, and plan and propose appropriate solutions |
| ELO8 | Communicate and coordinate effectively with patients and the patient's relatives, colleagues and community in healthcare practice |
| ELO9 | Organise, manage and maintain a professional work environment in a safe and effective manner |
| ATTITUDE | |
|---|---|
| ELO10 | Comply with legal regulations and professional ethical standards in medical practice |
| ELO11 | Demonstrate professionalism and continuous career development in healthcare practice |
Figure 1.
Application of the RIME (reporter, investigator, manager, and educator) model to curriculum reform. PE, physical examination.
Integrated basic sciences
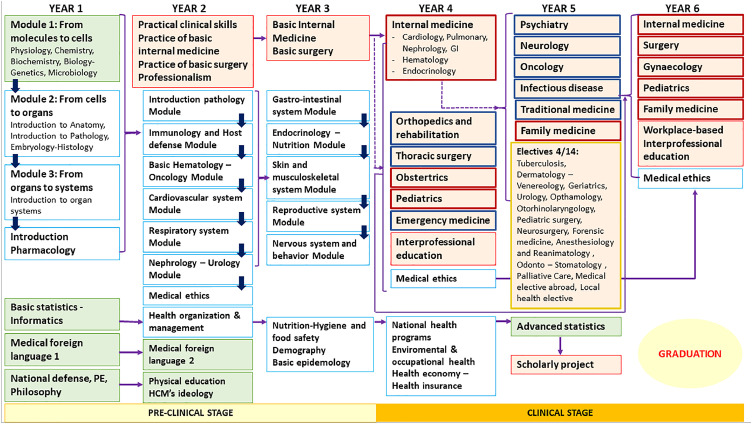
In the reformed curriculum, preclinical basic medical sciences disciplines are integrated into “levels of biology organisation” then “organ system” modules to provide a more relevant clinical learning context (Figure 2). To reinforce “joint planning” and “culture of critical inquiry”,2 curriculum development, organisation and teaching were performed by clinical and basic science faculty.
Figure 2.
New curriculum map. GI, gastro-intestinal system; HCM, Ho Chi Minh; PE, physical examination. Green box: general education; blue box: basic medical education; orange box: medical education; dark blue arrow: horizontally integrated; purple arrow: vertically integrated; continuous line: directly relevant; broken line: indirectly relevant. dark red borders: core clerkship; dark blue borders: secondary clerkship; dark yellow borders: electives.
Practice of medicine (POM)
The new POM module was introduced early in the second year and taught over two years. Firstly, students learn POM of internal medicine and general surgery at the Centre for Advanced Training in Clinical Simulation (https://atcs.ump.edu.vn), including basic skills in medical history taking, physical examination and professionalism. Next, they advance to real-world practice in community health centres and district hospitals.
Professionalism
This topic was introduced for the first time. To maximize its relevance, professionalism is integrated within the medical ethics, POM, inter-professional education, family medicine, and scholarly project modules. The objective is to improve students’ attitude and soft skills such as altruism, accountability, commitment to excellence, integrity, respect for others, leadership, empathy, and confidentiality.
Interprofessional education (IPE)
Although different health professions often work together in clinical practice, they are not specifically trained to do so. IPE nurtures teamwork in a healthcare environment, effective communication, mutual respect, professional approach/attitude and leadership skills. To emphasise “joint planning” and “culture of critical inquiry”,6 the IPE course was designed and taught by faculty from medicine, nursing, pharmacy, and rehabilitation.
Integrated clinical clerkship
In the pre-reform curriculum, clinical clerkships consisted of five core specialties and nineteen short subspecialties courses. Most courses had limited clinical activities and exposures to the content and practice were often not synchronised. In the new programme, clinical activities within each clerkship are coordinated and reinforced. The revised curriculum was reorganised into six core primary and eight secondary clerkships, and fourteen clinical electives (students would choose four) (Figure 2).
The main objectives of the redesigned clinical curriculum were to reinforce existing core clinical clerkships by integrating relevant subspecialties to reduce the number of short subspecialty courses. They are also to introduce Family Medicine as a new core clerkship to address the needs of Viet Nam primary care, reorganise the teaching of several subspecialties into electives, and rearrange clinical teaching and supervision to accommodate large student numbers. The new curriculum has better faculty-student ratios of 1:5 instead of 1:12–15 as before. To achieve these objectives, UMP-FM must negotiate with hospitals the needed institutional governance and organisation changes to facilitate implementation of the revised curriculum.
Electives
Electives in year 5 provide students with the opportunity to expand their knowledge, experience in different subjects, and study abroad. The restructure consists of integrating the “need to know” basic content and competencies into the family medicine clerkship, and the “good to know” advanced content and competencies to the electives.
Scholarly project
The reformed curriculum includes a four-week scholarly project module, designed to familiarise students with scientific research methodology, and cultivate their critical research thinking, problem-solving, decision-making, continuous improvement mindset, and teamwork.
Teaching/learning format
A student-centred approach is central and implemented throughout the curriculum using multiple teaching/learning formats, including lectures, flipped-classroom, team-based learning, case-based learning, bedside teaching, work-based teaching and supervision, and provision of regular feedback/debriefing.
Assessment
The new curriculum includes a transition from knowledge-based to competency-based assessment. It utilises a multiple-formats approach to assess the desired ELOs such as performance-based to address assessment of competencies, and work-based assessment in the clinical years to approximate assessment in the real working environment. For assessment of knowledge, the revised curriculum follows the Bloom taxonomy principles. For assessment of practice, Miller's pyramid was used to assess competences. Student assessments include formative and summative. Formative assessments are conducted continuously and regularly during the courses/modules using a variety of tools (Table S2). Summative assessments are conducted at the end of each course/module via several different methods (Table S2). Timely feedback is provided. To graduate, sixth-year students need to successfully complete their five rotational clerkships (medicine, surgery, obstetrics/gynaecology, paediatrics and family medicine) before the final exam. Students can submit claims or request an appeal. However, the number of these was low over the last 5 years, and only 8.5% of test scores were changed.
Institutional reform
This refers mainly to the governance, management and organisational structures that need to be in place to ensure effectiveness of curriculum reform and delivery. These include:
-
1.
The development, adaptation and implementation of intra-institutional and inter-institutional policies to organise commissions and working groups, and to facilitate the reform process;
-
2.
Instituting training and reward programmes for faculty/staff who actively participate and contribute to the reform;
-
3.
Establishing investment strategies to build human and technical resource capacity;
-
4.
Introducing programme monitoring and evaluation, and facilitating timely changes;
-
5.
Establishing strong and regular communications with stakeholders, students and faculty; and,
-
6.
Establishing sustainable collaborative exchanges with international institutions/consultants.
These key actions have been described by Frenk et al. as joint planning, academic systems, global networks, and a culture of critical inquiry.2 They are also reflected in Kotter's 8-step process for leading change in institutional reform. It includes building a guiding coalition, forming strategic visions and initiatives, enlisting a volunteer (faculty) army, enabling action by removing barriers, sustaining acceleration, and instituting change.13
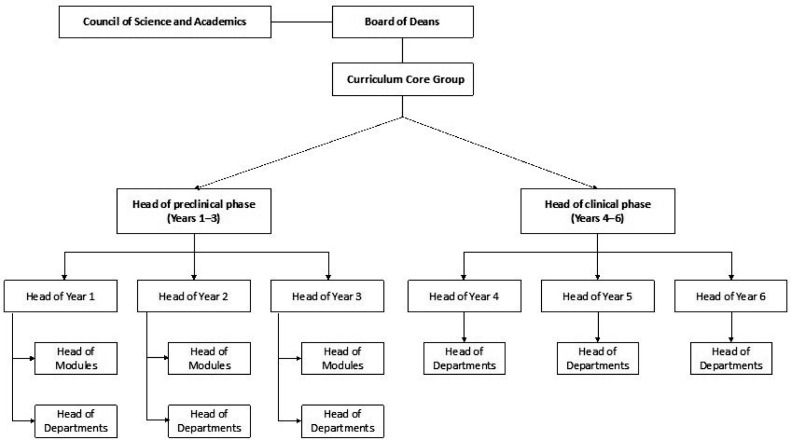
Organisational structure, management and governance
The highest level of academic management at UMP-FM is the Board of Deans, alongside the Council of Science and Academics. The newly created Curriculum Core Group (CCG) is designed to facilitate development of the integrated CBME curriculum and manage academic activities (Figure 3) while facilitating “joint planning” and “the culture of critical inquiry”.2 It includes heads of the preclinical (years 1–3) and clinical (years 4–6) phases, all reporting to the CCG then the Board of Deans. Under the Phase heads are heads for each study year; both groups worked closely with heads of modules/departments to help build the new curriculum. Specific development of each module is carried out by the head of module and its multidisciplinary working group.
Figure 3.
Structure of the new faculty.
All heads are identified and nominated by the President (UMP) and Dean (UMP-FM) based on several criteria, mainly commitment and participation in the reform process, ability to work with different people in different situations, and ability to lead and be respected by his/her peers. Nominated faculty members were then trained on complementary skills through the in-house leadership course, and some attended the Harvard Macy Institute course on ‘Leading Innovations in Health Care and Education’.17 Module heads could also be appointed as the head of curriculum phases/years, and work as part of the CCG.
Institutional culture
Resistance to change is inevitable and part of any change process. To facilitate and initiate change, UMP-FM first secured support from the university and then from FM leadership. However, a leadership coalition within the university was not sufficient to trigger organisational change. We also worked hard to gain support from other stakeholders, including senior faculty, MoH leadership, administrative staff, and international partners. When project momentum had been achieved, we advocated again for reform within the faculty. It has been suggested that paying attention to how institutional change occurs is at least, if not more, important than focusing on the curriculum elements that need to change to implement CBME. Therefore, institutional culture plays a key role and it is crucial to encourage innovation in an environment that is supportive and safe.18 Another important aspect of our institutional culture is to nurture the culture of critical inquiry, which facilitates the mobilisation of “scientific knowledge, ethical deliberation, and public reasoning and debate to generate enlightened social transformation”.6 UMP leadership has encouraged creative, innovative and critical inquiry through delegating to talented and responsible faculty members. These cultural elements have supported the spirit of change that is spreading through UMP-FM and have made the curriculum reform a comprehensive institutional project by unifying the workforce around a common goal.
Faculty development
Faculty play a key role in the successful implementation of CBME. Continued support for programme leaders and faculty requires central resources (i.e., time, expertise, and financial support) and coordination of numerous iterative processes.19 At UMP this was facilitated by the HPET project with a clear funding strategy and allocation that were supported by the Board of Deans. It has three complementary types of faculty support and development.
The first was started early to build the needed workforce capacity and coalition, the “preliminary curriculum core group”. During this period, UMP-FM had several faculty development activities with Ludwig Maximilian University of Munich and DUKE-National University of Singapore. The second type of support/development was provided by HAIVN. This included bringing experts from HMS to Viet Nam to provide training workshops and support other UMP-FM initiatives, while selected UMP faculty undertook a short in-depth training session at HMS. One faculty member undertook a Master of Medical Sciences in Medical Education programme at HMS and now heads the UMP-FM Medical Education Centre (MEC). This centre, restructured in 2019, trains faculty in the process of curriculum reform and develops faculty competence in curriculum design, teaching, assessment, research, and leadership. Thirdly, a memorandum of understanding for a 5-year Collaborative Education Programme (CEP) between Texas Tech University Health Sciences Centre at El Paso (TTU) and UMP was signed in January 2017 to establish a Faculty Development Unit (FDU) and a simulation centre at UMP-FM. Subsequently, in June 2017, several faculty (who later became the CCG) travelled to TTU to study the establishment and operation of a simulation centre, and acquire techniques in simulation-based teaching and learning. The CEP delivered a Faculty Development Programme (FDP) to core faculty members and facilitated the creation of the FDU (Table 2), which is now an important element of the MEC. In addition, there is a monitoring and evaluation programme to follow faculty after graduation from the FDP and determine how they were assessed by their department head. There is also a mentoring programme where high-achieving graduates are invited to contribute to the training of other faculty members.
Table 2.
Topics covered by faculty development programme (FDP). ATCS, Centre for Advanced Training in Clinical Simulation; CBME, competency-based medical education; EBPE, evidene-based practice education.
| Themes | Topics | |
|---|---|---|
| 1 | Teaching | Competency-Based Medical Education |
| Principles of adult learning | ||
| Adult learning and effective teaching | ||
| Reform the medical education to support the healthcare in Viet Nam | ||
| Audience Interactive Response System | ||
| How to apply adult learning and prepare a good lecture | ||
| Web-based learning & cloud storage in medical education | ||
| Turning point | ||
| How to improve your oral presentation | ||
| How to develop, implement & assess active learning of the learners | ||
| Evidence-based medicine (EBM), integration of EBM into medical education | ||
| 2 | Assessment | Workshop on standardised patients (SP) & objective-structured clinical examination (OSCE) |
| Workshop on writing case scenario | ||
| Workshop on debriefing techniques | ||
| Workshop on writing standardised questions | ||
| Workshop on interprofessional education and practice to improve patient safety | ||
| 3 | Research | Basic data analysis |
| Mobile computing platform in the teaching and practice of EBM | ||
| How to develop & conduct research in medical education | ||
| Workshop: How to organise and conduct an EBM-format journal club | ||
| 4 | Developing clinical skills | How to organise a lesson in simulation centre |
| Introduction to ATCS regulations and documentation | ||
| ATCS Centre equipment | ||
| Development & integration of clinical simulation into medical education | ||
| One-minute preceptor: micro-skills of clinical teaching | ||
| EBPE: the vital signs and vascular system | ||
| EBPE: examination of the heart and hand-on training: Littmann 3200 | ||
| Workshop on interpretation of chest radiograph | ||
| EBPE of the abdomen | ||
| EBPE of the respiratory system | ||
| EBPE of the central nervous system | ||
| Integration of EBPE into the preclinical curriculum & clinical rotation | ||
| 5 | Leadership | The seven habits of highly effective people |
| Principles for negotiation & conflict resolution | ||
| Introduction to mentoring program | ||
| The essential principles for effective leadership | ||
| Develop and implement a faculty mentoring programme | ||
| Developing and becoming the leader within you | ||
| Team work | ||
| Effective time management |
Faculty teaching and teaching-related reward
A faculty teaching and teaching-related evaluation and recognition process are part of the new structure. Each year, 360-degree assessment is used to evaluate the performance of each faculty member. A faculty reward mechanism recognises outstanding contribution to the development and implementation of the new CBME, and publications in international journals. Rewards include being nominated as ‘Teacher of The Year’, overseas study grants, and/or attendance at international medical education conferences and training.
Infrastructure/educational resources
Information technology (IT) to empower learning is an important focus of the UMP-FM curriculum reform project because this was a weak component compared with some Western medical schools. Therefore, IT facilities, including e-learning infrastructure, were introduced and regularly updated. The Information Technology and Communication Centre (ITC), created in 2011, provides IT software and services. The following have been set up to meet teaching needs: two virtual learning rooms (140 computers each and a data server system); nine smart classrooms (>500 seats) for active learning; one seminar room (>60 seats); two computer laboratories (430 computers); and many large lecture halls. The library web portal was also upgraded, providing students and lecturers with easy on-site and remote access.
As proposed in the HPET curriculum reform grant, the Centre for Advanced Training in Clinical Simulation (ATCS) has been established to support the education programme and improve students’ clinical competence. This includes a clinical skills laboratory and clinical simulation area where students learn basic clinical skills in patient communication, patient history taking and physical exam. The Centre received provisional accreditation in 2019 and full accreditation in 2021 by the Society for Simulation in Healthcare (https://www.ssih.org/Credentialing/Accreditation).
Global networks
Collaborations with diverse international partners have played a central role in the development and implementation of UMP-FM curriculum reform. Initially (2010–2013), international collaboration helped institutional leaders explore the direction and decide on potential partners for the reform process. These collaborations also served as triggers and “advance organisers” for envisioning the required changes and reinforcing the readiness to change. From 2013 to 2014, collaborations between UMP-FM and UGFM and HMS allowed curriculum reform ideas to be translated into a solid project and submitted to the WB-HPET call for proposals.11 The third phase (2014–2022) includes collaborations regarding the development and implementation of the curriculum reform activities detailed in the grant, and supports the faculty to develop resources and implement the HPET project.
International experts of Vietnamese origin were essential because they have a better understanding of the local context/culture, and speak the local language. Furthermore, having organisations such as HAIVN and its IMPACT-MED project available on-site is strategically important for our reform endeavour. Local collaborations with HAIVN facilitated exchanges/collaborations with HMS faculty and HMS-affiliated teaching hospitals. Furthermore, on-site HAIVN staff have repeatedly and readily provided technical and organisational support.20
Enabling actions
Programme quality and accreditation
The Faculty Quality Assurance and Improvement (QAI) programme, supported by the Quality Assurance Unit established in 2017, is a new structure to ensure the quality, efficiency and sustainability of the curriculum. It ensures that the curriculum is being continuously reviewed and improved based on the Plan–Do–Check–Act approach.21 Feedback is collected from students and faculty members, alumni, employers, and professional associations (Table S3). Minor revisions can be implemented at the end of each module/course/clerkship, moderate revisions can be implemented every 3 years, while major revisions can be undertaken every 6 years. Any relevant guidance issued since the initial curriculum reform process (e.g. from the Ministry of Education and Training in 202122) will also be incorporated into subsequent curriculum revisions.
For UMP-FM, as specified in the HPET grant, it was important that all teaching activities are benchmarked against World Federation for Medical Education (WFME) accreditation standards, and periodic reviews are performed to align graduate attributes with the curriculum ELOs. This facilitates continuous improvement of the curriculum and learning/teaching activities. In addition, the development, implementation and maintenance of standard operating procedures ensures the consistency of the designed curriculum and delivered activities.
As part of its external quality assurance initiative, UMP-FM applied to the ASEAN University Network-Quality Assurance Organisation for accreditation of its basic medical education programme. Full accreditation for the reformed programme was received in June 2021, and UMP-FM is now working towards WFME accreditation.
Mobilise leadership
This is an important aspect of enabling the reform process. As part of our reforms there were three levels of leadership:
-
•
Internal: The leaders of the reform process had to change the mindset of the leadership of the Faculty of Medicine and senior faculty members.
-
•
National: The leaders of the reform process had to convince the MoH about the urgent need for medical education curriculum reform in Viet Nam (note that this was achieved because the MoH agreed to support the process by facilitating the HPET project).
-
•
International: The leaders of the reform process mobilised the support of international experts to facilitate the reform process.
Impact
The new curriculum at UMP-FM is the first integrated and CBME programme in Viet Nam, and the first class of students is graduating in 2022. Intended outcomes are for the graduates to be ready and able to pursue postgraduate education, and capable of delivering effective, efficient and quality healthcare that meets the needs of the population. However, the impact of CBME is much wider than this. It also raises awareness of the new education model in Viet Nam, the need to build the capacity of local experts, and the need to facilitate interaction between medical education centres and their affiliated teaching clinics/hospitals. Dentistry and nursing education programmes at UMP and four other medical schools in Viet Nam are now undergoing competency-based curriculum reform. Medical education initiatives at UMP have gained recognition, and the MoH has appointed UMP to build a licensing exam centre for the qualification and certification of medical graduates, with the objective of ensuring patient safety.
Lessons learnt
The lessons learnt through the curriculum reform process at UMP may be helpful to other medical schools in low- and middle-income countries that are considering transforming from a traditional to a CBME curriculum. These are:
-
1.
Start with a sense of urgency and a consensus decision-making, and make curriculum reform an institutional-wide project. This motivates wide support from faculty members and stakeholders, and strengthens a common determination and commitment to change.
-
2.
There is no such thing as a perfect curriculum. Having this mindset allows us to take risks and apply an innovative approach. It also allows us to apply a continuous evaluation, adaptation and self-questioning approach to challenges.
-
3.
Identify core faculty members and assemble a group with shared commitment. Collaborations played an important role in developing core faculty members who started the reform process while undergoing personal development.
-
4.
Identify and use momentum effectively. This allowed us to move forward with a stronger commitment and to overcome resistance.
-
5.
Be flexible. This allowed us to take input and feedback from stakeholders, and encouraged innovation and engagement.
-
6.
Effective communication. This supported us to achieve a wide range of engagement.
-
7.
Change requires material and spiritual investment. A variety of resources need to be mobilised, sceptics need to be tolerated and engaged with, and emotional frustration is part of the process.
-
8.
Stay focused on the vision and champion an entrepreneurial approach. To innovate and advance the project, it is crucial to recognise paths and opportunities that will lead to realisation of the vision.23
-
9.
International collaboration is critical, and there are different levels/types of collaborations that are each valuable at different phases of the reform process. The transformation would not have been possible without our international partners.
-
10.
The alignment of national and institutional initiatives is essential to the success of instructional and institutional reforms, and facilitates the institution's motivation and projects to move forward. This synchronisation is probably critical in developing countries.
-
11.
Follow Kotter's eight steps in leading change.13
Future directions
As the UMP FM curriculum reforms move forward, one of the biggest challenges remaining is the development and improvement of teaching in the clinical years. This includes improving the quality of the clinical teaching workforce, providing more access to practical training and experiences in hospitals/community clinics, and the collaboration framework between UMP and “affiliated” hospitals/community clinics. We are considering and reviewing various models of Academic Health Centre (AHC) organisation,24, 25 which were introduced in the US in the late 1940s and are now used in the Netherlands, Australia, and United Kingdom.24 “The defining feature of these complex organisations is a tripartite mission of high quality research, medical education and clinical care”,24 characterised by high-quality clinical services, involvement with basic and clinical science, and a permanent commitment to high-quality education and training. The Viet Nam MoH is currently trying to allocate more autonomy to UMPs and hospitals. In addition, in 2017 the Prime Minister issued the decree on "Provisions of practical training in the field of healthcare service”26 that outlined specific regulations on the relationship-cooperation between medical universities and hospitals. In this context, AHC models could be reviewed and adapted for UMP-FM.
Despite progress to date, several challenges remain. Although reduced, student workload remains quite high and there is a commitment to continue to undertake short- and long-term revision processes to make the curriculum more concise. We are also developing mechanisms to determine whether students are ready to graduate and have attained the required competencies after completing the new curriculum. Furthermore, it is important to move from the current manual management systems to a more digital-based system. Finally, we need to continue to foster and improve collaboration between teaching hospitals and community clinics. By implementing all these aspects, and proactively addressing any new issues, that today's reforms can continue to be tomorrow's successes.
Conclusions and recommendations
The goal of CBME curriculum reform is to equip graduates with the competence to serve the Viet Nam healthcare system. The process has covered and implemented, to a certain extent, several recommendations and enabling actions outlined by the Lancet 2010 Commission for Health Professional Education.2 Success of the curriculum reform process at UMP-FM is due to the availability of both external and internal resources and support, and the internal drive for reform. International collaborations have also played an important role in the success of the current reform process.
Given the short time we had to get a six-year curriculum up and running, and with a faculty overstretched in their teaching, administrative and clinical responsibilities, a highly effective FDP and teaching recognition and reward system were critical to successful curriculum reform. In addition, to ensure the programme's quality and sustainability, it is essential that a continuous quality assurance process is implemented throughout the reform process. Finally, good leadership and an energetic, dedicated, generous and motivated faculty/staff are key contributors to successful curriculum reform.
Contributor
Substantial contributions to the conception, design of the work; the acquisition, analysis, interpretation of data for the work: TDT, PMV, HTMP, LNA, HPD, HTTD, NH, QTVH, BKL, DQN, HTMN, KDN, NAN, PHN, TAN, TCT, HNC, LNV, and NVV.
Drafting the work, revising it critically for important intellectual content: TDT, PMV, HTMP, LNV, NVV.
Final approval of the version to be published: TDT, PMV, HTMP, LNA, HPD, HTTD, NH, QTVH, BKL, DQN, HTMN, KDN, NAN, PHN, TAN, TCT, HNC, LNV, and NVV.
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: TDT, PMV, HTMP, LNA, HPD, HTTD, NH, QTVH, BKL, DQN, HTMN, KDN, NAN, PHN, TAN, TCT, HNC, LNV, and NVV.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
We would like to thank all faculty members and staff of UMP-FM, and our international partners, for their dedication to the curriculum reform process.
Funding
This work receives no external funding.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100543.
Appendix. Supplementary materials
References
- 1.Flexner A. Updyke; Boston, MA: 1910. A Report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. [Google Scholar]
- 2.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 3.Hoat LN, Yen NB, Wright EP. Participatory identification of learning objectives in eight medical schools in Viet Nam. Med Teach. 2007;29(7):683–690. doi: 10.1080/01421590701361189. [DOI] [PubMed] [Google Scholar]
- 4.Montegut AJ, Cartwright CA, Schirmer JM, Cummings S. An international consultation: the development of family medicine in Viet Nam. Fam Med. 2004;36(5):352–356. [PubMed] [Google Scholar]
- 5.Schirmer JM, Le NH. The Viet Nam family medicine development project: a cross-cultural collaboration. Families, Syst Health. 2002;20(3):303–310. [Google Scholar]
- 6.Bland CJ, Starnaman S, Wersal L, Moorehead-Rosenberg L, Zonia S, Henry R. Curricular change in medical schools: how to succeed. Acad Med. 2000;75(6):575–594. doi: 10.1097/00001888-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 7.UMP-FM. The long-term strategic plan of the University of Medicine and Pharmacy at Ho Chi Minh City towards 2020. (2010) (Unpublised document).
- 8.Bonvin R, Nendaz M, Frey P, Schnabel KP, Huwendiek S, Schirlo C. Looking back: twenty years of reforming undergraduate medical training and curriculum frameworks in Switzerland. GMS J Med Educ. 2019;36(5):Doc64. doi: 10.3205/zma001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vu NV, Bader CR, Vassalli JD. In: Advances in Medical Education. Scherpbier AJJA, van der Vleuten CPM, Rethans JJ, editors. Kluwer Academic Publishers; Dordrecht: 1997. The redesigned undergraduate medical curriculum at the University of Geneva. [Google Scholar]
- 10.Le SM. The windy journey of medical education in Viet Nam. Available from: https://blogs.worldbank.org/health/windy-journey-medical-education-Viet_Nam. Accessed 31 January 2022.
- 11.The World Bank. Health professionals education and training for health system reforms. Available from: https://projects.worldbank.org/en/projects-operations/project-detail/P131825. Accessed 11 January 2022.
- 12.Association of Southeast Asian Nations. Cebu declaration on the acceleration of the establishment of an ASEAN community by 2015. Available from: https://asean.org/cebu-declaration-on-the-acceleration-of-the-establishment-of-an-asean-community-by-2015/. Accessed 11 January 2022.
- 13.Kotter JP. Leading change: why transformation efforts fail. Harvard Business Review May-June 1995. Available from: https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2. Accessed 11 January 2022.
- 14.VMGUS Publication, No 052009. Viet Namese medical education and development of family medicine in Viet Nam.
- 15.Ministry of Health. Ministry of Health. Basic competency standards for General Practioners” (Decision No. 1854/QĐ-BYT, dated 18 May 2015).
- 16.DeWitt D, Carline J, Paauw D, Pangaro L. Pilot study of a ‘RIME’-based tool for giving feedback in a multi-specialty longitudinal clerkship. Med Educ. 2008;42(12):1205–1209. doi: 10.1111/j.1365-2923.2008.03229.x. [DOI] [PubMed] [Google Scholar]
- 17.Harvard Macy Institute. Annual Harvard Macy institute programs. Available from:https://harvardmacy.org/images/course_content/2017_hce2-0/Health_Care_Education_2017.pdf. Accessed 15 March 2022.
- 18.Mejicano GC, Bumsted TN. Describing the journey and lessons learned implementing a competency-based, time-variable undergraduate medical education curriculum. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S42–S48. doi: 10.1097/ACM.0000000000002068. [DOI] [PubMed] [Google Scholar]
- 19.Dagnone D, Stockley D, Flynn L, et al. Delivering on the promise of competency based medical education - an institutional approach. Can Med Educ J. 2019;10(1):e28–e38. [PMC free article] [PubMed] [Google Scholar]
- 20.Duong DB, Phan T, Trung NQ, et al. Innovations in medical education in Viet Nam. BMJ Innovations. 2021;7(suppl 1):s23–s29. [Google Scholar]
- 21.UMP-FM. Faculty of medicine web page. Available from: https://med.ump.edu.vn/dao-tao/chuong-trinh-doi-moi-khoa-y. Accessed 15 March 2022.
- 22.Ministry of Education and Training. Circular: providing for standards and formulation, appraisal and promulgation of training progams of higher education (22 Jun 2021). Available from:https://thuvienphapluat.vn/van-ban/EN/Giao-duc/Circular-17-2021-TT-BGDDT-standards-and-formulation-training-programs-of-higher-education/480403/tieng-anh.aspx. Accessed 27 June 2022.
- 23.Neck HM, Neck CP, Murray EL. Entrepeneurship: The Practice and Mindset. SAGEPublications; 2021. Creating and recognizing new opportunities; pp. 56–76.https://uksagepubcom/sites/default/files/upm-assets/107801_book_item_107801pdf Available from: Accessed 15 March 2022. [Google Scholar]
- 24.French CE, Ferlie E, Fulop NJ. The international spread of Academic Health Science Centres: a scoping review and the case of policy transfer to England. Health Policy. 2014;117(3):382–391. doi: 10.1016/j.healthpol.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Weiner BJ, Culbertson R, Jones RF, Dickler R. Organizational models for medical school-clinical enterprise relationships. Acad Med. 2001;76(2):113–124. doi: 10.1097/00001888-200102000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Decree No. 111/2017/ND-CP dated October 05, 2017 of the Government on the provisions of practical training in the field of healthcare service [in Viet Namese]. Available from: https://thuvienphapluat.vn/van-ban/Giao-duc/Nghi-dinh-111-2017-ND-CP-quy-dinh-to-chuc-dao-tao-thuc-hanh-trong-dao-tao-khoi-nganh-suc-khoe-363410.aspx. Accessed 12 April 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.