Abstract
Introduction
Systemic lupus erythematosus (SLE) is characterized by early atherothrombosis. Pulse wave velocity (PWV) is a promising tool for the diagnosis of early vascular remodelling and initial atherosclerotic plaque formation. Our objective was to evaluate PWV and its relationship with coronary atherosclerosis and thrombotic biomarkers in patients with SLE.
Material and methods
In 26 patients with SLE with stable clinical conditions, mean age of 39.1 ±11.7 years and without a history of coronary artery disease, multidetector computed tomography (MDCT)-based coronary calcium scoring (CACS) was performed and PWV measured.
Laboratory evaluation included serum levels of anticardiolipin and anti-β2-glycoprotein antibodies (anti-β2-GPI), lupus anticoagulant (LA), D-dimers, thrombin–antithrombin complexes (TAT), and von Willebrand factor (vWF).
Results
Multidetector computed tomography revealed coronary calcifications in 8 (30.8%) patients and the median CACS was 52.4 HU (range 2–843.2). The mean PWV was 9.0 ±3.2 m/s and was higher in patients aged > 50 years (+33.7% vs. < 50 years), those with positive LA (+28.2% vs. LA negative), TAT ≥ 10 μg/l (+18.1% vs. < 10 μg/l), vWF ≥ 200 IU/dl (+51.8% vs. < 200 IU/dl) and with coronary atherosclerosis (CACS > 0; +21.4% vs. CACS = 0).
In contrast, the duration of the disease, D-dimers, anticardiolipin, and anti-β2-GPI antibodies did not influence PWV. In the group without atherosclerosis (CACS = 0, n =18), patients with vWF ≥ 200 IU/dl had a 19.3% higher PWV compared to the rest.
Conclusions
In patients with SLE, PWV was associated with the presence of coronary atherosclerotic lesions in MDCT. Furthermore, arterial stiffness was higher in patients with markers of endothelial dysfunction and a prothrombotic state, suggesting their contribution to the early stages of arterial remodelling in SLE.
Keywords: systemic lupus erythematosus, autoimmune diseases, pulse wave velocity, coronary calcification
Introduction
Objectives
Systemic lupus erythematosus (SLE) is a generalized autoimmune disease in which diffuse chronic inflammation plays an important role. Today, survival in patients with SLE is limited by the increased occurrence of serious cardiovascular complications [1].
Risk factors for coronary artery disease (hypertension, hyperlipidaemia, diabetes, tobacco use, and sedentary lifestyle) do not explain the increased risk of atherosclerosis and cardiovascular complications in patients with SLE [2]. One of the possible mechanisms includes chronic, generalized inflammation, as well as the presence of antiphospholipid antibodies (aPL). Elevated levels of aPL are associated with an increased risk of thrombosis in the arteries and microcirculation [3, 4]. This co-existence meets the criteria for the diagnosis of antiphospholipid syndrome (APS) [5], which occurs in one-third of patients with SLE [6].
Non-invasive methods of measuring vascular parameters are used to assess the risk of development and progression of cardiovascular diseases. The loss of elasticity of the arterial walls, in particular the aorta, is believed to be a marker of early changes that may lead to the development of atherosclerosis and a wide spectrum of its complications (e.g. myocardial infarction, ischaemic stroke, limb ischaemia) [7]. Pulse wave velocity (PWV) is used to detect an early increase in aortic wall stiffness and is valued by the European Society of Cardiology as a marker of early atherosclerotic damage [8].
There is abundant evidence in the literature of a high predictive value of carotid-femoral pulse wave velocity (cfPWV) in the evaluation of the risk of cardiovascular complications in the elderly [9], in patients with arterial hypertension [7], type 2 diabetes [10] or end-stage renal disease [11]; cfPWV also allows independent evaluation of cerebrovascular risk in healthy subjects [12].
Von Willebrand factor (vWF), produced by the endothelium, plays a role in platelet activation and aggregation. Its blood concentration increases in endothelial damage, especially in diseases that accelerate atherosclerosis, such as arterial hypertension, hyperlipidaemia, and nicotinism [6, 13]. Although elevated blood vWF concentration can also be found during pregnancy and after physical activity in otherwise healthy subjects, vWF is considered a good marker of endothelial damage [14, 15]. The general advantage of vWF as an indicator of endothelial damage is that it is produced only by the endothelium and its level remains stable for weeks [14].
Thrombin–antithrombin III complexes (TAT) are formed when thrombin, generated by thrombotic pathways, is inactivated by circulating antithrombin III. High levels of TAT are associated with high prothrombotic activity and may be found in clinical conditions such as myocardial infarction, atrial fibrillation, or pulmonary embolism [16]. On the other hand, chronic anticoagulation leads to a decrease in serum TAT levels [16]. Thrombin–antithrombin III complex represents a short-lived marker of prothrombotic activity and is widely used in studies on coagulation disorders [6].
The increase in aortic stiffness assessed with cfPWV well reflects the increased risk of cerebrovascular and cardiovascular diseases [8]. Although vessel wall stiffening is primarily related to ageing, many studies have shown an acceleration in vascular stiffness in patients with risk factors for cardiovascular disease [7]. Changes in the structure of the vessel wall become the basis for the development of atherosclerosis, which, as an inflammatory process, is also intensified in systemic inflammatory diseases [17].
Purpose of the study
The purpose of the study was to assess pulse wave velocity in patients with SLE and to evaluate its relationship with markers of thrombosis and coronary atherosclerosis.
Material and methods
This prospective single-centre study was carried out in 26 consecutive patients treated for SLE in the Department of Internal Medicine of the Jagiellonian University Medical College, Krakow. All patients met at least 4 ACR classification criteria for SLE [18].
Inclusion and exclusion criteria
The inclusion criterion was a stable clinical condition of SLE (no need to intensify immunosuppressive therapy, that is, an increase in current doses of immunosuppressive drugs or the introduction of an additional immunosuppressive drug in the last three months).
Exclusion criteria were the following: a history of coronary artery disease, known cancer, clinical symptoms of heart failure (New York Heart Association III or IV class), renal failure (creatinine clearance < 30 ml/min) and/or respiratory failure.
Pulse wave velocity
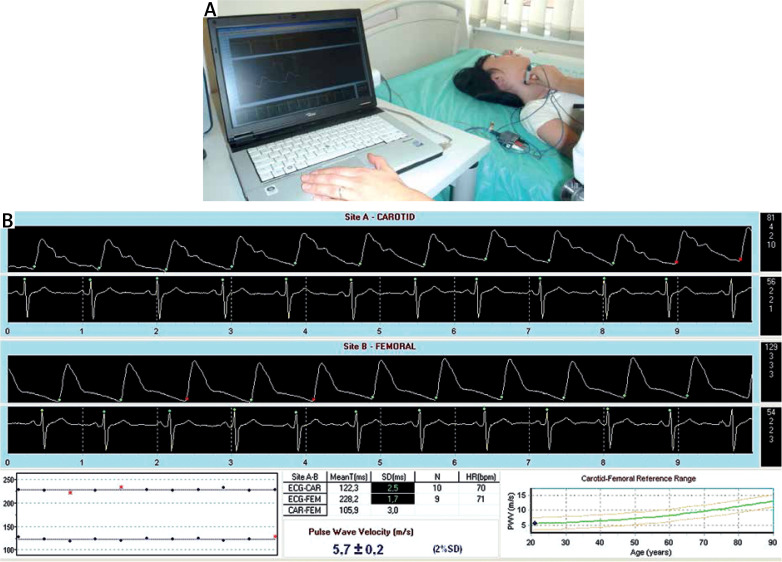
Pulse wave velocity was measured transcutaneously in the right common carotid artery and in the right femoral artery independently, using SphygmoCor. The applanation tonometer (Millar®) was applied first to the common carotid artery and then to the femoral. The measurement of PWV was performed simultaneously with the ECG examination (Fig. 1 A). The propagation time is expressed as the difference between the beginning of pulse waves in both arteries and the contraction of the left ventricle, represented by the wave R in the ECG. This method neglects the fact that the wave in both arteries comes from two separate cycles of the heart cycle. It is believed that with a sufficiently short period of time between both measurements, possible changes in heart rate or isovolumetric left ventricular contraction time do not significantly affect pulse wave velocity and are negligible (Fig. 1 B) [19].
Fig. 1.
Pulse wave velocity measurement. An applanation tonometer (Millar®) is applied to the common carotid artery (A). The pulse wave graph is recorded by the SphygmoCor®, simultaneously with the ECG examination (B).
Pulse wave velocity (PWV) is defined as the ratio of a distance (s) between test points to the time (Δt) needed to travel this distance (PWV = s/Δt). The space between the two measurement points was evaluated above the body surface with a measuring tape and adjusted to the precise vascular anatomy [8]. Pulse wave velocity is expressed in metres per second (m/s). The average of three consecutive measurements was adopted as the final result.
Coronary calcium score
Coronary calcium scoring was performed using a multidetector computed tomography scanner (Somatom Definition, Siemens, Germany). Images were ECG-triggered with 3-mm thick sections covering the whole heart. Coronary artery calcifications were defined as lesions with attenuation greater than 130 Hounsfield units (HU) in more than four adjacent pixels. To quantify coronary calcium, the 3D Leonardo application (Siemens, Germany) was used. The number of atherosclerotic plaques and their volume in particular coronary arteries were evaluated. The Agatston calcium score was calculated [20].
Laboratory tests
Routine laboratory investigations were measured using standard methods. Serum levels of anticardiolipin (aCL) and anti-β2-GPI antibodies (of both IgG and IgM classes) were measured using a homemade ELISA with the Sapporo standard for the measurement of anti-β2-GPI antibodies (HCAL for IgG, EY2C9 for IgM) [13].
Values exceeding the 99th percentile of a healthy population sample were considered positive, that is, > 20 RU/ml for aCL IgG; > 30 RU for aCL IgM; > 3 RU/ml for anti-β2-GPI IgG and > 3 RU/ml for anti-β2-GPI IgG.
The presence of lupus anticoagulant (LA) was tested in accordance with the three step procedure recommended by the International Society on Thrombosis and Haemostasis [21].
Thrombin–antithrombin III complexes and vWF levels were assessed in citrate plasma using commercial kits (Siemens, Germany). The detailed assay methodology was in accordance with the manufacturer’s instructions.
Statistical analysis
Statistical analysis was performed using the Statistica Six Sigma software. The study was powered to have an 80% chance of detecting a 10% difference in PWV at the 0.05 significance level. To demonstrate such a difference or greater, 12 subjects or more were required in each group based on the values of a previous study [22].
All numerical data were expressed as mean values ± standard deviations for the normal distribution or as the median and interquartile range (IQR) for the non-normal distribution. Continuous variables were compared using the t-test. The χ2 test was used to examine the differences in proportion. The level of statistical significance was predetermined at p < 0.05.
Bioethical standards
Before inclusion in the study, informed consent was obtained from each patient. The study protocol conformed to the ethical guidelines of the Declaration of Helsinki of 1975 and was approved by the Bioethical Committee of the Jagiellonian University in Krakow.
Results
Characteristics of the patients
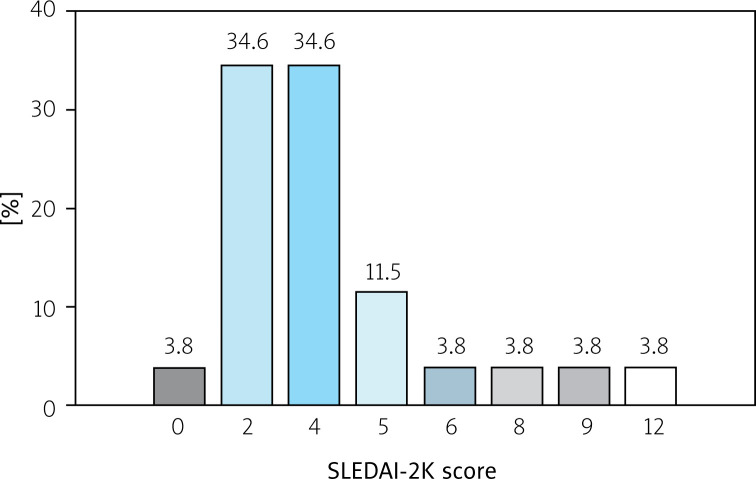
Our study included 26 patients (among them n = 23, 88% women), mean age 39.1 ±11.7 years. The mean duration of the disease at the time of examination was 15.5 (range 2 to 32 years). The severity of SLE according to the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) score [23] is shown in Figure 2.
Fig. 2.
Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) score in study patients.
Two patients had previously been diagnosed with APS according to the revised APS classification criteria [5]. One of the two had a history of pulmonary embolism. There were two patients with arterial hypertension and a history of smoking. The results of peripheral blood count, serum sodium, potassium, glucose, creatinine, and urine, as well as ECG recordings at rest, were normal in all patients.
Immunosuppressive treatment included: methylprednisolone (n = 14, 53.8%; 4 mg to maintain clinical stability), prednisone (n = 2, 7.7%), chloroquine derivative (n = 3, 11.5%), azathioprine (n =2, 7.7%), cyclophosphamide (n = 1, 3.8%) and methotrexate (n = 1, 3.8%). The remaining patients did not use any immunosuppressive drugs in the last 12 months of observation.
Other pharmacotherapy included angiotensin-converting enzyme inhibitors in 3 (11.5%) subjects, a β-receptor antagonist in 1 (3.8%) and a calcium channel antagonist in 1 (3.8%). Antiphospholipid syndrome patients were treated with anticoagulant (warfarin, n = 1) or antiplatelet therapy (aspirin, n = 1).
Coronary artery calcium score
Multidetector computed tomography revealed coronary calcifications in 8 (30.8%) patients. The median number and volume of atherosclerotic calcified plaques were 3 (2–23) and 27.6 mm3 (4–761.8 mm3), respectively. The calcium score (CACS) was 52.4 (2–843.2).
Thrombotic biomarkers
The TAT level was 3.7 ±3.5 μg/l, vWF level 143.0 ±47.5 IU/dl, the D-dimer level was 0.73 ±0.92 mg/l. Lupus anticoagulant was present in 5 (19.2%) patients. The concentration of anticardiolipin autoantibodies was as follows: IgM 13.9 ±12.1 RU/ml and IgG 12.3 ±9.0 RU/ml. Regarding anti-β2-GPI antibodies, IgM and IgG levels were 2.2 ±4.3 RU/ml and 1.4 ±1.3 RU/ml, respectively.
Pulse wave velocity
The mean PWV was 9.0 ±3.2 m/s. Pulse wave velocity was higher in patients older than 50 years, those with positive LA, TAT ≥ 10 μg/l, and vWF ≥ 200 IU/dl and with coronary atherosclerosis (CACS > 0). In contrast, disease duration, D-dimers and anticardiolipin and anti-β2-GPI antibodies levels did not influence the PWV (Table I).
Table I.
Influence of coronary artery calcium score and thrombotic biomarkers on pulse wave velocity (PWV) in patients with SLE (n = 26)
| Parameters | PWV [m/s] | p-value |
|---|---|---|
| Age < 50 years | 8.3 ±1.6 | 0.04 |
| Age ≥ 50 years | 11.1 ±5.9 | |
| Duration of the disease < 10 years | 8.1 ±1.8 | NS |
| Duration of the disease ≥ 10 years | 8.8 ±0.4 | |
| LA negative | 8.5 ±1.7 | 0.04 |
| LA positive | 10.9 ±6.6 | |
| D-dimers < 250 mg/l | 9.1 ±1.9 | NS |
| D-dimers ≥ 250 mg/l | 8.9 ±3.6 | |
| vWF < 200 IU/dl | 8.3 ±1.5 | 0.01 |
| vWF ≥ 200 IU/dl | 12.6 ±6.9 | |
| TAT < 10 μg/l | 8.3 ±1.6 | 0.04 |
| TAT ≥ 10 μg/l | 9.8 ±0.7 | |
| CACS = 0 | 8.4 ±1.7 | 0.04 |
| CACS > 0 | 10.2 ±5.2 |
CACS – coronary artery calcium score, LA – lupus anticoagulant, NS – non-significant, TAT – thrombin–antithrombin complexes, vWF – von Willebrand factor.
In the group without atherosclerosis (CACS = 0, n = 18), patients with vWF ≥ 200 IU/dl had 26.8% higher PWV compared to the rest (Table II). We did not observe an association between PWV and other thrombotic markers in this subgroup.
Table II.
Influence of thrombotic biomarkers on pulse wave velocity (PWV) in patients with SLE without coronary calcifications (n = 18)
| Parameters | PWV [m/s] | p-value |
|---|---|---|
| vWF < 200 IU/dl | 8.2 ±1.7 | 0.01 |
| vWF ≥ 200 IU/dl | 10.4 ±0.1 | |
| TAT < 10 μg/l | 8.3 ±1.9 | NS |
| TAT ≥ 10 μg/l | 9.9 ±0.8 |
NS – non-significant, PWV – pulse wave velocity, TAT – thrombin–antithrombin complexes, vWF – von Willebrand factor.
Discussion
Our study confirms that PWV is related to subclinical coronary atherosclerosis in patients with SLE. Furthermore, we observed increased arterial stiffness in patients with positive lupus anticoagulant and elevated TAT and vWF.
Pulse wave velocity in patients with SLE included in our study was 9.0 ±3.2 m/s. The results are similar to those reported in the literature [24, 25]. In a study by Yildiz et al. [24] conducted among young women with SLE and mean age 33.6 ±9.6 years, similar values of pulse wave velocity were obtained (8.98 ±2.05 m/s). Furthermore, Kocabay et al. [25] reported that 22 patients with newly diagnosed SLE aged 35 ±2.5 years achieved an average PWV value of 9.3 ±2.5 m/s.
In the study by Bjarnegråd et al. [26] conducted among 27 women with SLE at an average age of 60 years, women with SLE had a higher pulse wave velocity (9.8 m/s) than patients in the age-matched control group (8.2 m/s), which confirms the influence of age on arterial stiffness, as was also observed in our study.
Our findings on increased arterial stiffness in patients with SLE are consistent with the results of the recent meta-analysis of 18 studies among 943 patients with SLE [27].
As the body ages, significant morphological and functional changes occur in the arterial walls, especially in the middle (media) and subendothelial (intima) layers. Endothelial function is impaired, leading to a reduction in the bioavailability of vasodilating nitric oxide [17]. Disturbances in its production result in an increase in the resting tone of vascular smooth muscle cells, then lead to an increase in arterial stiffness, and finally cause an increase in blood pressure. Additionally, elastin fibres gradually fragment and disappear. They are replaced by more rigid, and thus less prone to stretching, collagen fibres. The amount of intercellular matrix increases and calcium deposits accumulate [17].
Mitchel et al. [9] conducted PWV studies in a population without risk factors for cardiovascular diseases. They divided the study group into four groups according to age (< 50, 50–59, 60–69, > 70 years) and found a significant increase in PWV with age.
An interesting study by Sutton-Tyrrell et al. [28] showed that in older patients (the age of the study group was > 70 years), increased PWV was strongly associated with the occurrence of adverse cardiovascular events and increased mortality.
In our study, we observed a positive correlation between PWV and the presence of coronary calcifications. A higher PWV was found in patients with coronary atherosclerosis (10.2 ±5.2 m/s; +21.4%) compared to patients without coronary calcifications. A similar correlation was previously reported in patients without SLE. Kullo et al. [29] found that PWV was significantly associated with the presence and quantity of coronary artery calcium in patients without a history of myocardial infarction or stroke, while in the study by Liu et al. [30], PWV correlated well with coronary atherosclerosis in a large group of 654 participants.
Modification of lifestyle was the therapeutic intervention that prevented the progression of arterial stiffness. It was also reported that the more advanced ischaemic heart disease was, the higher the PWV values were [22]. In the study of 92 patients who qualified for invasive coronary diagnostics, it was found that PWV was significantly higher in patients with coronary artery lesions (11.13 ±0.91 m/s in single vessel disease, 15.22 ±1.11 m/s in twovessel disease and 19.30 ±2.05 m/s in threevessel disease) than in subjects with normal coronary vessels (8.14 ±1.25 m/s) [22].
The correlation of arterial stiffness, as a marker of early atherosclerosis, with the severity of systemic inflammation has been studied [31, 32], but the studies are not consistent. Blann et al. [31] found that arterial stiffness was not related to inflammation. But his research was conducted among patients with stable coronary artery disease.
On the other hand, Tuttolomondo et al. [32] detected a positive relationship between PWV and some circulating mediators (e.g. vWF) in patients with an acute cardiovascular or cerebrovascular event. In our study, we examined patients with higher levels of inflammatory markers caused by general inflammatory diseases, probably the reason for our positive results.
In patients with SLE, traditional risk factors for atherosclerosis may predict an increased risk of cardiovascular events. However, they do not significantly explain the accelerated progression of atherosclerosis in this group. The primary contribution to both the initiation and progression of atherosclerosis has been attributed to a malfunctioning immune system and, more specifically, to intensified autoimmune responses [2]. This concept was confirmed by Mendoza-Pinto et al. [27], who demonstrated that inflammatory markers influence arterial vessel stiffness in patients with SLE.
The high level of prothrombotic activity in SLE was also described as an important factor that contributes to an increased risk of cardiovascular events [15]. It is suggested to be associated with endothelial damage and autoinflammation [27].
It appears that the rapid progression of atherosclerosis, a result of the pro-inflammatory state in rheumatic disorders, may also increase the probability of thrombotic events. Many studies have shown a correlation between prothrombotic activity and endothelial dysfunction, one of the early stages of atherosclerosis [15, 33]. Thrombin formation has been shown to increase matrix metalloproteinase (MMS) enzymatic activity, contributing to the stiffness of the extracellular matrix of arteries [34].
Furthermore, the degradation of the extracellular matrix by MMS remains a link between arterial vessel remodelling, arterial stiffness, atherosclerotic plaque progression, and destabilization [35]. Platelet activation, expressed by a higher vWF, may not only lead to thrombotic complications in patients with atherosclerosis, but may also contribute to arterial stiffness [36].
Our study supports this thesis, but also indicates that for the early stages of arterial remodelling, endothelial dysfunction (vWF level), prothrombotic activity (TAT concentration), and presence of lupus anticoagulant may constitute significant causal factors of atherosclerosis. Interestingly, it was observed not only in patients with coronary calcifications, but also in those without calcified atherosclerosis in the coronary vessels.
Study limitations
Our study has several limitations. First, the sample size was relatively small; however, the study was adequately powered to detect differences in PWV between the study groups. Second, noninvasively measured PWV tends to overestimate PWV obtained by invasive measurements by about 20% due to the anatomical structure of individual patients and the degree of tortuosity of the aorta [37]. Third, since we evaluated a limited number of thrombotic and inflammatory biomarkers in SLE, the results of our study are hypothesis-generating. Fourth, the statistical association presented does not necessarily mean a cause-and-effect relationship.
Conclusions
In patients with systemic lupus erythematosus, PWV is related to the presence of coronary atherosclerotic lesions. In addition, arterial stiffness is higher in patients with positive lupus anticoagulant and higher levels of vWF and TAT. Lupus anticoagulant presence, endothelial dysfunction, or prothrombotic activity, manifested by higher levels of vWF and TAT, influences the early stages of arterial remodelling and atherosclerosis in SLE.
Footnotes
The authors declare no conflicts of interest.
This study was supported by the grant N40201231/0460 from the Polish Ministry of Science and Higher Education.
References
- 1.Schmidt W, Pawlak-Buś K, Leszczyński P. Historia diagnostyki i leczenia tocznia rumieniowatego układowego. Rheumatol Forum 2021; 7: 71–77, DOI: 10.5603/FR.2021.0012. [DOI] [Google Scholar]
- 2.Pons-Estel GJ, González LA, Zhang J, et al. Predictors of cardiovascular damage in patients with systemic lupus erythematosus: data from LUMINA (LXVIII), a multiethnic US cohort. Rheumatology (Oxford) 2009; 48: 817–822, DOI: 10.1093/rheumatology/kep102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arad A, Proulle V, Furie RA, et al. β2-Glycoprotein-1 autoanti-bodies from patients with antiphospholipid syndrome are sufficient to potentiate arterial thrombus formation in a mouse model. Blood 2011; 117: 3453–3459, DOI: 10.1182/blood-2010-08-300715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tripodi A, de Groot PG, Pengo V. Antiphospholipid syndrome: laboratory detection, mechanisms of action and treatment. J Intern Med 2011; 270: 110–122, DOI: 10.1111/j.1365-2796.2011.02362.x. [DOI] [PubMed] [Google Scholar]
- 5.Miyakis S, Lockshin MD, Atsumi T, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 2006; 4: 295–306, DOI: 10.1111/j.1538-7836.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 6.Bugała K, Mazurek A, Gryga K, et al. Influence of autoimmunity and inflammation on endothelial function and thrombosis in systemic lupus erythematosus patients. Clin Rheumatol 2018; 37: 2087–2093, DOI: 10.1007/s10067-018-4104-4. [DOI] [PubMed] [Google Scholar]
- 7.Kopeć G, Podolec M, Dziedzic H, Sobień B. [The concept of arterial stiffness in cardiovascular disease prevention]. Kardiol Pol 2010; 68: 364–368 [In Polish]. [PubMed] [Google Scholar]
- 8.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018; 39: 3021–3104, DOI: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell GF, Parise H, Benjamin EJ, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension 2004; 43: 1239–1245, DOI: 10.1161/01.HYP.0000128420.01881.aa. [DOI] [PubMed] [Google Scholar]
- 10.Cruickshank K, Riste L, Anderson SG, et al. Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation 2002; 106: 2085–2090, DOI: 10.1161/01.cir.0000033824.02722.f7. [DOI] [PubMed] [Google Scholar]
- 11.Blacher J, Safar ME, Guerin AP, et al. Aortic pulse wave velocity index and mortality in end-stage renal disease. Kidney Int 2003; 63: 1852–1860, DOI: 10.1046/j.1523-1755.2003.00932.x. [DOI] [PubMed] [Google Scholar]
- 12.Mattace-Raso FUS, van der Cammen TJM, Hofman A, et al. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation 2006; 113: 657–663, DOI: 10.1161/CIRCULATIONAHA.105.555235. [DOI] [PubMed] [Google Scholar]
- 13.Swadzba J, De Clerck LS, Stevens WJ, et al. Anticardiolipin, anti-beta(2)-glycoprotein I, antiprothrombin antibodies, and lupus anticoagulant in patients with systemic lupus erythematosus with a history of thrombosis. J Rheumatol 1997; 24: 1710–1715. [PubMed] [Google Scholar]
- 14.Denis CV, Susen S, Lenting PJ. von Willebrand disease: what does the future hold? Blood 2021; 137: 2299–2306, DOI: 10.1182/blood.2020008501. [DOI] [PubMed] [Google Scholar]
- 15.Mazurek A, Gryga K, Bugala K, et al. Influence of statin therapy on antiphospholipid antibodies and endothelial dysfunction in young patients with coronary artery disease and systemic lupus erythematosus. Arch Med Sci 2022; 18: 18–24, DOI: 10.5114/aoms.2019.9027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drabik L, Konieczyńska M, Undas A. Clot Lysis Time Predicts Stroke During Anticoagulant Therapy in Patients with Atrial Fibrillation. Can J Cardiol 2020; 36: 119–126, DOI: 10.1016/j.cjca.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Wang M, Monticone RE, Lakatta EG. Arterial aging: a journey into subclinical arterial disease. Curr Opin Nephrol Hypertens 2010; 19: 201–207, DOI: 10.1097/MNH.0b013e3283361c0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith EL, Shmerling RH. The American College of Rheumatology criteria for the classification of systemic lupus erythematosus: strengths, weaknesses, and opportunities for improvement. Lupus 1999; 8: 586–595, DOI: 10.1191/096120399680411317. [DOI] [PubMed] [Google Scholar]
- 19.Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605, DOI: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 20.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15: 827–832, DOI: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 21.Pengo V, Tripodi A, Reber G, et al. Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anti-coagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost 2009; 7: 1737–1740, DOI: 10.1111/j.1538-7836.2009.03555.x. [DOI] [PubMed] [Google Scholar]
- 22.Alarhabi AY, Mohamed MS, Ibrahim S, et al. Pulse wave velocity as a marker of severity of coronary artery disease. J Clin Hypertens (Greenwich) 2009; 11: 17–21, DOI: 10.1111/j.1751-7176.2008.00061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bombardier C, Gladman DD, Urowitz MB, et al. Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 1992; 35: 630–340, DOI: 10.1002/art.1780350606. [DOI] [PubMed] [Google Scholar]
- 24.Yildiz M, Yildiz BS, Soy M, Tutkan H. Impairment of arterial distensibility in premenopausal women with systemic lupus erythematosus. Kardiol Pol 2008; 66: 1191–1194; discussion 1200-1201. [PubMed] [Google Scholar]
- 25.Kocabay G, Hasdemir H, Yildiz M. Evaluation of pulse wave velocity in systemic lupus erythematosus, rheumatoid arthritis and Behçet’s disease. J Cardiol 2012; 59: 72–77, DOI: 10.1016/j.jjcc.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Bjarnegråd N, Bengtsson C, Brodszki J, et al. Increased aortic pulse wave velocity in middle aged women with systemic lupus erythematosus. Lupus 2006; 15: 644–650, DOI: 10.1177/0961203306071402. [DOI] [PubMed] [Google Scholar]
- 27.Mendoza-Pinto C, Rojas-Villarraga A, Molano-González N, et al. Endothelial dysfunction and arterial stiffness in patients with systemic lupus erythematosus: A systematic review and meta-analysis. Atherosclerosis 2020; 297: 55–63, DOI: 10.1016/j.atherosclerosis.2020.01.028. [DOI] [PubMed] [Google Scholar]
- 28.Sutton-Tyrrell K, Najjar SS, Boudreau RM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation 2005; 111: 3384–3390, DOI: 10.1161/CIRCULATIONAHA.104.483628. [DOI] [PubMed] [Google Scholar]
- 29.Kullo IJ, Bielak LF, Turner ST, et al. Aortic pulse wave velocity is associated with the presence and quantity of coronary artery calcium: a community-based study. Hypertension 2006; 47: 174–179, DOI: 10.1161/01.HYP.0000199605.35173.14. [DOI] [PubMed] [Google Scholar]
- 30.Liu C-S, Li C-I, Shih C-M, et al. Arterial stiffness measured as pulse wave velocity is highly correlated with coronary atherosclerosis in asymptomatic patients. J Atheroscler Thromb 2011; 18: 652–658, DOI: 10.5551/jat.7021. [DOI] [PubMed] [Google Scholar]
- 31.Blann AD, Kuzniatsova N, Lip GY. Inflammation does not influence arterial stiffness and pulse-wave velocity in patients with coronary artery disease. J Hum Hypertens 2013; 27: 629–634, DOI: 10.1038/jhh.2013.17. [DOI] [PubMed] [Google Scholar]
- 32.Tuttolomondo A, Di Raimondo D, Pecoraro R, et al. Immune-inflammatory markers and arterial stiffness indexes in subjects with acute ischemic stroke. Atherosclerosis 2010; 213: 311–318, DOI: 10.1016/j.atherosclerosis.2010.08.065. [DOI] [PubMed] [Google Scholar]
- 33.Kotyla P. Różnice w rozwoju autoimmunizacji u kobiet i mężczyzn. Rheumatol Forum 2020; 6: 131–138, DOI: 10.5603/FR.2020.0017. [DOI] [Google Scholar]
- 34.Watanabe N, Ikeda U. Matrix metalloproteinases and atherosclerosis. Curr Atheroscler Rep 2004; 6: 112–120, DOI: 10.1007/s11883-004-0099-1. [DOI] [PubMed] [Google Scholar]
- 35.Lyle AN, Raaz U. Killing Me Unsoftly: Causes and Mechanisms of Arterial Stiffness. Arterioscler Thromb Vasc Biol 2017; 37: e1–e11, DOI: 10.1161/ATVBAHA.116.308563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yamasaki F, Furuno T, Sato K, et al. Association between arterial stiffness and platelet activation. J Hum Hypertens 2005; 19: 527–533, DOI: 10.1038/sj.jhh.1001861. [DOI] [PubMed] [Google Scholar]
- 37.Van Bortel LM, Laurent S, Boutouyrie P, et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens 2012; 30: 445–448, DOI: 10.1097/HJH.0b013e32834fa8b0. [DOI] [PubMed] [Google Scholar]