Abstract
Many states expanded their Medicaid programs to low-income adults under the Affordable Care Act (ACA). These expansions increased Medicaid coverage among low-income parents and their children. Whether these improvements in coverage and healthcare use lead to better health outcomes for parents and their children remains unanswered. We used longitudinal data on a large, nationally representative cohort of elementary-aged children from low-income households from 2010–2016. Using a difference-in-differences approach in state Medicaid policy decisions, we estimated the effect of the ACA Medicaid expansions on parent and child health. We found that parents’ self-reported health status improved significantly post-expansion in states that expanded Medicaid through the ACA by 4 percentage points (p < 0.05), a 4.7% improvement. We found no significant changes in children’s use of routine doctor visits or parents’ assessment of their children’s health status. We observed modest decreases in children’s body mass index (BMI) of about 2% (p < 0.05), especially for girls.
INTRODUCTION
Previous research documents that the ACA Medicaid expansions have increased health insurance coverage among low-income parents.1–5 Though children in low-income households were already eligible for health insurance coverage through Medicaid, the ACA Medicaid expansions also increased health insurance coverage of these children through parents’ increased awareness of their children’s eligibility for existing Medicaid coverage.6 Evidence is also building showing the spillover effects of these expansions onto other parental outcomes including financial well-being1,7 and psychological distress.1 Emerging research suggests that children also benefit from adult Medicaid expansions in the form of more preventive care use8 and improved children’s reading skills.9
Less is known about how these increases in health insurance coverage and preventive care have spillover effects on the health outcomes of parents and children, specifically. In general, correlational research shows a positive relationship between parental insurance coverage and children’s health in low-income families.10–13 Causal research on whether health insurance coverage affects overall health, however, is mixed.14–20
Although much research has shown improvements in health outcomes among the low-income adult population from the ACA Medicaid expansions,21 it is important to distinguish between adults without dependent children and parents given that parents are more likely to subsequently influence children. Existing research that does not include parents may be missing a feature of the ACA Medicaid expansion effects, namely spillover effects on children already eligible for Medicaid coverage. Understanding the effects on children’s healthcare utilization and health outcomes is important in documenting the impact of public health insurance eligibility for low-income parents on their children’s development.
In this study, we examine the spillover effects of public health insurance expansions for low-income adults on parent and child health, extending the prior literature that showed positive effects of parental health insurance expansions on children’s health insurance outcomes.22,23 We pair longitudinal data on a representative sample of children from low-income households with a quasi-experimental design that leverages state variation in Medicaid expansion between 2010–2016. We also examine heterogeneity in the findings by child race and ethnicity, child sex, and family income due to potential differences in the spillover effects related to these demographic characteristics. For example, due to the timing of maturation and differences in body composition and healthcare needs, there may be differences in the role of parental public health insurance access on health between girls and boys. Our findings document how changes in state Medicaid policies regarding adult eligibility affect the health of parents and their children.
METHODS
Data
We analyze data from the Early Childhood Longitudinal Study, Kindergarten class of 2010–11 (ECLS-K:2011), a nationally representative cohort of U.S. children who entered kindergarten in the fall of 2010. ECLS-K:2011 is sponsored by the National Center for Education Statistics (NCES) within the Institute of Education Sciences (IES) of the U.S. Department of Education. Follow up data on children, parents, and teachers were done 1–2 times per year between 2011 and 2016. The ECLS-K:2011 provides significant strengths in answering the research questions; the data are nationally representative, were collected in multiple languages, and there is a sizable subsample of the population of interest, low-income families. The ECLS-K:2011 contains strong measurement with parent reports of parent health, child health, and child health care utilization, and direct assessments of children’s body mass index (BMI). Most importantly, there are several waves of data collected both before and after the ACA Medicaid expansions. Multiple studies have utilized the ECSL-K:2011 to study child and parent health.24–26
We limit the analytical sample to households with incomes less than 138 percent of the federal poverty line (FPL) in 2013 to focus on the households most likely to be eligible for the ACA’s expansion to low-income adults. We follow this group of children/parents pre- and post-expansion—enabled by the longitudinal nature of data—to estimate the ACA impacts post-expansion. Of the 14,530 children eligible for inclusion in spring 2016 data collection, 11,440 responded in spring 2016. Of these, 4,270 children were from low-income households who resided in the same state across all waves.1 To account for the complex survey design and non-random attrition across waves, we include post-stratification weights. In all, after accounting for missing data on key variables of interest and zero longitudinal weights, our analytical sample size is approximately 2,500 children across 7 waves, totaling 10,000–16,800 child-wave observations (the exact sample size varies slightly across models). Thus, our results are generalizable to children in low-income households in the U.S. who attended kindergarten in fall 2010. Additional detail regarding the ECLS-K:2011’s study design is available from the NCES. We obtained Penn State Institutional Review Board approval for the study.
Measures
Our analysis is conducted at the child-wave level. The primary outcomes of interest follow the previous literature that has explored the impact of public health expansions for children in the 1990s on children’s health status and health utilization.27,28 In addition, we include a measure of overall parental health status in our analysis. Specifically, we assess the following:
Parent Health. Parents reported on their overall health status on a 5-point scale (1= Excellent, 2=Very Good, 3=Good, 4=Fair, and 5 = Poor) in each wave. Following past literature,27 we convert this measure to a binary variable to indicate whether the parent is in good health or better (over 80% of parents fall into this category).
Child Health. Parents also reported on their children’s overall health status on a 5-point scale (1= Excellent, 2=Very Good, 3=Good, 4=Fair, and 5 = Poor) in each wave. Similar to the parental health measure, we convert this measure to a binary variable to indicate whether the child is in good health or better (over 90% of children fall into this category).
Child health utilization for routine care. To investigate the effect of public health insurance expansions on children’s healthcare utilization, we assess whether a child had any doctor visits for routine care in the past year. We focus on utilization that is explicitly routine in nature to avoid confounding between healthcare access and sickness, following previous literature.28 Specifically, in each wave, parents were asked “How long has it been since [child’s] last visit to a clinic, health center, hospital, doctor’s office, or other place for routine care?”. Parents reported on a 5-point scale (1 = Never, 2 = Less than 6 months, 3 = 6–12 months, 4 = 1–2 years, 5= greater than 2 years). Because the AAP recommends children have at least one preventative/routine doctor’s visit per year,29 we recode this variable as binary equaling 1 if the child had at least 1 doctor visit in the past year, and zero otherwise.
Child Body Mass Index (BMI). In addition to the self/parent-reported measures of health and healthcare utilization, we include an objectively assessed measure of child health: child BMI. To ensure accurate measurements, children’s weight and height measurements were carried out twice. Composite BMI measures (calculated as weight in kilograms divided by height in meters squared) were provided for each wave in the data. Because we are using a longitudinal model to assess within-child changes in BMI, we use the composite BMI measures in our main analyses.2
Table 1 shows the weighted and unweighted descriptive characteristics of the key measures from our analytic sample.
Table 1.
Descriptive Statistics in Low-Income Households (< 138% FPL)
| All States | Non-Expansion States | Expansion States | Non-Expansion States | Expansion States | |||
|---|---|---|---|---|---|---|---|
| N a | Mean | SD | Mean | Mean | Weighted Mean | Weighted Mean | |
| Parental Health | |||||||
| Overall Health Status (Good or better) | 14,870 | 0.815 | 0.388 | 0.795 | 0.834 | 0.786 | 0.848 |
| Child Health Utilization | |||||||
| At least 1 Routine Doctor Visit in past year | 15,880 | 0.888 | 0.315 | 0.900 | 0.876 | 0.902 | 0.875 |
| Child Health | |||||||
| Overall Health Status (Good or better) | 21,930 | 0.953 | 0.212 | 0.947 | 0.959 | 0.949 | 0.963 |
| BMI | 25,930 | 18.501 | 4.176 | 18.613 | 18.392 | 18.835 | 18.497 |
| Family and Child Characteristics | |||||||
| Male | 26,900 | 0.514 | 0.499 | 0.522 | 0.506 | 0.527 | 0.501 |
| Black | 26,900 | 0.159 | 0.366 | 0.226 | 0.096 | 0.262 | 0.130 |
| Hispanic | 26,900 | 0.466 | 0.498 | 0.430 | 0.500 | 0.374 | 0.459 |
| White | 26,900 | 0.252 | 0.434 | 0.265 | 0.239 | 0.287 | 0.300 |
| Child age (in months) | 26,900 | 96.723 | 22.506 | 96.514 | 96.922 | 98.127 | 98.553 |
| Parent age (in years) | 26,900 | 32.067 | 7.752 | 31.696 | 32.474 | 31.972 | 32.776 |
| Parent has high school diploma or more | 26,900 | 0.328 | 0.469 | 0.331 | 0.323 | 0.358 | 0.345 |
| Time-varying State Characteristics | |||||||
| Unemployment rate | 26,900 | 7.331 | 2.163 | 6.849 | 7.789 | 6.721 | 7.580 |
| EITC rate | 26,900 | 0.073 | 0.154 | 0.020 | 0.123 | 0.021 | 0.119 |
| TANF/SNAP max. benefits for family of 3 ($) | 26,900 | 942.50 | 183.46 | 809.00 | 1069.16 | 811.39 | 1052.16 |
| Minimum wage | 26,900 | 7.615 | 0.792 | 7.208 | 8.002 | 7.098 | 7.976 |
Notes: The difference between expansion and non-expansion states is statistically significant at p < .05 for all variables. Sampling weights are used in the last two columns to adjust for nonresponse and differential attrition across waves in the sampling
Sample sizes (in child-waves) are rounded to the nearest 10 as per dataset guidelines.
As noted in the table, we find considerable differences between children and parents from low-income households (less than 138% FPL) residing in the expansion states and non-expansion states.3 Past literature has shown that the states that expanded were more progressive; these statistical differences underscore the need to use an appropriate identification strategy in our analysis to account for these differences. Indeed, we use a difference-in-differences (DD) approach precisely to ensure that these differences in levels can be accounted for by focusing on the differences in the trends of these outcomes pre- and post-ACA between expansion and non-expansion states. We describe our analytical approach below.
Analytic Method
Although the ACA was originally a federal mandate, in 2012, the Supreme Court allowed states to opt out of the Medicaid expansion requirement. As a result, some states opted to expand Medicaid to all adults with household incomes less than 138% FPL, while some states did not. In our analytic sample, children (and parents) who reside in twenty-five states are coded as 1 to denote expansion and those in the remaining sixteen states are coded as 0. Table S1 shows details of states’ expansion decisions. Due to ECLS-K:2011’s clustered sampling framework, there were no children sampled from 10 states.
Using a child’s state of residence and the date in which that state expanded Medicaid through the ACA, we employ a DD approach to estimate the impact of the public health insurance expansions for low-income adults on parents’ health, children’s health, and children’s use of routine health services (see Appendix for supplemental information regarding the models and methods). Specifically, we compare the changes in health outcomes of children (and parents) from before the Medicaid expansion (waves 1–4, when children entered kindergarten through the spring of second grade) and after the expansion in January 2014 (waves 5–7, when children were in third through fifth grades) between the expansion and non-expansion states. Children are coded as being in the treatment group (post-expansion) if their state of residence expanded during or after 2014. Although most states expanded their Medicaid programs to low-income adults in 2014, some states expanded early, and some expanded late. Early expanders are treated as if they expanded in 2014 based on the effective date of expansion, meaning all time points prior to 2014 (waves 1–4) are coded as not yet expanded. We use 2014 as the effective date of expansion even for the early expanders, as is standard in the past ACA literature, because full implementation took place only 2014-onwards.20,21 We also include child fixed effects, which adjust for all time-invariant factors related to the outcomes of interest, including a child’s sex, race/ethnicity, parent education, and other constant household characteristics and unobserved features.
In addition, we adjust for several time-varying state characteristics that may have differentially affected the health and healthcare utilization outcomes across states in low-income households. Because these factors may also be correlated with a state’s decision to expand Medicaid for low-income adults, adjusting for these factors helps reduce time-varying confounds. Specifically, we include the following characteristics: state unemployment rates, state Earned Income Tax Credit (EITC) rates, state minimum wages, and the maximum Temporary Assistance for Needy Family (TANF) and Supplemental Nutrition Assistance Program (SNAP) combined benefits for a family of three at the state-year level.
We use Ordinary Least Squares (OLS) estimation for all our models. Because the dependent variables, other than BMI, are all binary, they are linear probability models in such cases and the reported coefficient can be interpreted as marginal effects (i.e., percentage point changes in outcomes in expansion states post-expansion). All statistical analyses are weighted to adjust for sampling procedures, nonresponse, differential attrition, and standard errors are clustered at the state level, the level at which treatment status varies.32
RESULTS
Figure 1 shows the summarized health trajectories over the study period for parents and children in the expansion states relative to non-expansion states among low-income households. Across these dependent variables, we observe largely parallel trends prior to the expansion (January 2014). We test this more rigorously in the appendix, where we provide (1) results from regression-adjusted models that show that the linear pre-trends in our models are not statistically different between the two groups of states prior to the expansion (see Table S2); and event-study graphs (see Figure S1) that provide further confidence in the DD identification strategy.
Figure 1.
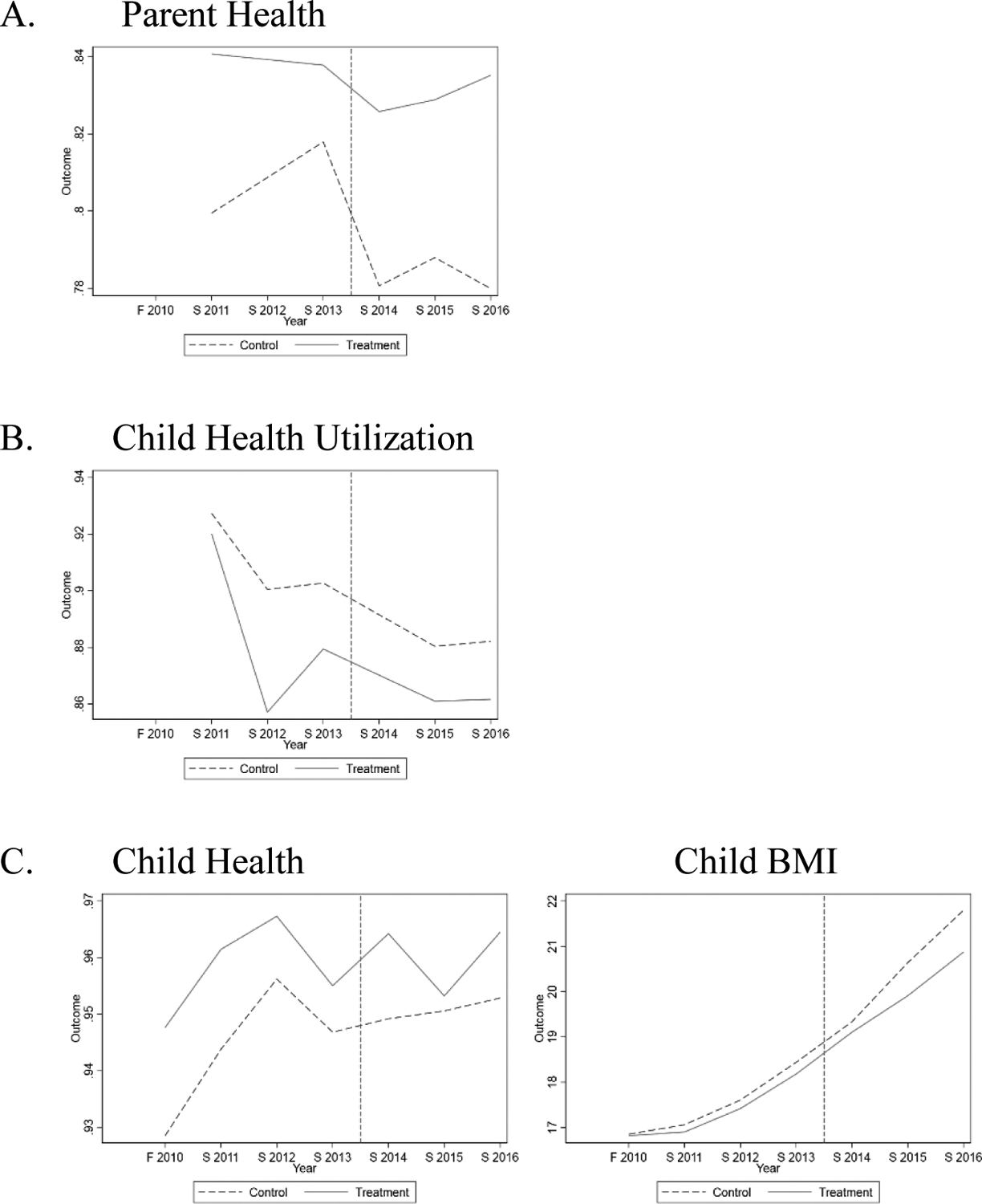
Raw Trends in Variables of Interest
Notes: Data from ECLS:K 2011. Expansion states are the treatment states, and non-expansion states are the control states. The x-axis (Year) represents the survey wave, F=fall and S=spring. The vertical line represents January 2014, when the ACA Medicaid expansions were largely implemented. Sample is limited to children in households with incomes below 138% FPL. Parent health and child health utilization were not available in the F 2010 wave of data collection.
Table 2 reports the main estimates of the effect of the ACA’s public health insurance expansions to low-income adults on parent and child health outcomes. Model 1 (column 1) includes child fixed effects, wave fixed effects, and the time-varying expansion status at the state level (see Table S1 for the expansion status). In Model 2 (column 2), we add the time-varying state-level covariates to the DD regression models.
Table 2.
Impact of the ACA Medicaid Expansion on Health Outcomes in Low-Income Households (< 138% FPL)
| A. Parent Health | Overall Health | |||
|---|---|---|---|---|
| (1) | (2) | |||
| Expansion | 0.039*** (0.010) | 0.034* (0.013) | ||
| Mean of DV | 0.829 | 0.829 | ||
| Time Varying State Covariates | No | Yes | ||
| Observationsa | 10,760 | 10,760 | ||
| R-squared (within-child) | 0.004 | 0.005 | ||
| B. Child Health Utilization | Doctor Visits | |||
| (1) | (2) | |||
| Expansion | −0.003 (0.013) | 0.011 (0.014) | ||
| Mean of DV | 0.92 | 0.92 | ||
| Time Varying State Covariates | No | Yes | ||
| Observationsa | 11,160 | 11,160 | ||
| R-squared (within-child) | 0.008 | 0.009 | ||
| C. Child Health | Overall Health | BMI | ||
| (1) | (2) | (1) | (2) | |
| Expansion | −0.007 (0.007) | −0.004 (0.009) | −0.443** (0.133) | −0.334* (0.142) |
| Mean of DV | 0.94 | 0.94 | 16.88 | 16.88 |
| Time Varying State Covariates | No | Yes | No | Yes |
| Observationsa | 15,300 | 15,300 | 16,840 | 16,840 |
| R-squared (within-child) | 0.002 | 0.002 | 0.471 | 0.473 |
Notes: Each column of each panel corresponds to a different OLS regression model. Each model includes wave and child fixed effects and sampling weights. Expansion represents β1 from equation (1) as shown in appendix, and measures the average effect of the Medicaid expansions after it took place. Mean of each dependent variable (DV) provides the within-child average of the DV after controlling for just wave fixed effects. Heteroscedasticity-robust standard errors, in parentheses, are clustered at the state level.
Sample sizes (in child-years) are rounded to the nearest 10 as per dataset guidelines.
p < 0.05,
p < 0.01,
p < 0.001.
First, we find that parents who reside in expansion states reported overall better health post-expansion. On average, we observe a 3.9 percentage point increase of parents who report “good”, “very good”, or “excellent” health as compared to those in non-expansion states. These health effects persist in model 2 despite inclusion of other potential time-varying confounding variables. Relative to the mean value of 0.829, this increase represents an improvement of about 4.7 percent.
Next, we examine if these effects extend to children’s health utilization and health. Panel B reports no statistically significant changes in routine doctor visits for children or parents’ assessment of their child’s overall health. In contrast, as shown in Panel C, we observe significant decreases in children’s BMI. These effects are modest (about 2%). Interestingly, we observe that the BMI decreases are driven by girls (see Table S3 for more heterogenous effects).
SENSITIVITY ANALYSES
To confirm that omitted variables are not driving the main results, we next perform a placebo check. We conduct the same difference-in-differences analysis using a sample of households with household incomes above 400% FPL. We do not expect parents and children in these households to be affected by the Medicaid expansions since the adults in the households were not eligible due to their higher incomes. Indeed, Table 3 reports no significant effects for any of the health or healthcare use outcomes for this high-income sample.
Table 3.
Impact of the ACA Medicaid Expansion on Health Outcomes in High-Income Households (> 400% FPL)
| A. Parent Health | Overall Health | |||
|---|---|---|---|---|
| (1) | (2) | |||
| Expansion | −0.004 (0.007) | −0.009 (0.007) | ||
| Mean of DV | 0.963 | 0.963 | ||
| Time Varying State Covariates | No | Yes | ||
| Observationsa | 11,730 | 11,730 | ||
| R-squared (within-child) | 0.002 | 0.003 | ||
| B. Child Health Utilization | Doctor Visits | |||
| (1) | (2) | |||
| Expansion | −0.004 (0.015) | 0.014 (0.017) | ||
| Mean of DV | 0.94 | 0.93 | ||
| Time Varying State Covariates | No | Yes | ||
| Observationsa | 11,910 | 11,910 | ||
| R-squared (within-child) | 0.013 | 0.015 | ||
| C. Child Health | Overall Health | BMI | ||
| (1) | (2) | (1) | (2) | |
| Expansion | 0.007 (0.004) | 0.006 (0.004) | 0.021 (0.091) | 0.153 (0.117) |
| Mean of DV | 0.98 | 0.98 | 16.26 | 16.26 |
| Time Varying State Covariates | No | Yes | No | Yes |
| Observationsa | 16,590 | 16,590 | 18,190 | 18,190 |
| R-squared (within-child) | 0.001 | 0.002 | 0.445 | 0.449 |
Notes: Each column of each panel corresponds to a different OLS regression model. Each model includes wave and child fixed effects, state-level covariates, and sampling weights. Expansion represents β1 from equation (1) as shown in appendix, estimated for sub-sample of higher-income (> 400%FPL households only), and measures the average effect of the Medicaid expansions after it took place. Mean of each dependent variable (DV) provides the within-child average of the DV after controlling for just wave fixed effects. Heteroscedasticity-robust standard errors, in parentheses, are clustered at the state level.
Sample sizes (in child-years) are rounded to the nearest 10 as per dataset guidelines.
p < 0.05,
p < 0.01,
p < 0.001.
Next, we perform a similar analysis on a more precise subset of households in states that expanded. Specifically, we limit the sample to households with incomes between each state’s pre-ACA parental eligibility income thresholds and 138% FPL. Unlike the main analysis, in which we treat all households with incomes under 138% FPL in expansion states as being “treated,” in this analysis we focus only on parents who were most likely to be newly eligible under the ACA due to their parental status. On average, the Medicaid eligibility threshold for parents in expansion states increased from about 105% in 2011 (unweighted average across expansion states) to at least 138% in 2014 under the ACA (see Appendix Table S5 for details on the thresholds we used). We also include more details regarding the models and methods for this robustness analysis in the appendix.
As this is a more precise sample, we expect the effects to be tighter. Parents and children in low-income households (<138% FPL) residing in states that did not expand Medicaid through the ACA consist of the control group, as before. Children whose parents were eligible for Medicaid based on pre-ACA income thresholds in expansion and non-expansion states are dropped. All other elements remain the same as in the main estimation. Table 4 reports results from this analysis. Because we have more limited sample size and fewer treatment clusters here, we also report wild cluster bootstrapped p-values here.33,34
Table 4.
Impact of the ACA Parental Income Eligibility Expansion on Impact of the ACA Medicaid Expansion on Health Outcomes in Low-Income Households (<138% FPL)
| A. Parent Health | Overall Health | |||
|---|---|---|---|---|
| (1) | (2) | |||
| Expansion | 0.063*** (0.018) | 0.062*** (0.017) | ||
| Mean of DV | 0.839 | 0.839 | ||
| Time Varying State Covariates | No | Yes | ||
| Observationsa | 5,240 | 5,240 | ||
| R-squared (within-child) | 0.005 | 0.006 | ||
| Wild Cluster Bootstrap p-value | 0.055 | 0.029 | ||
| B. Child Health Utilization | Doctor Visits | |||
| (1) | (2) | |||
| Expansion | −0.025 (0.018) | −0.010 (0.020) | ||
| Mean of DV | 0.94 | 0.94 | ||
| Time Varying State Covariates | No | Yes | ||
| Observationsa | 5,390 | 5,390 | ||
| R-squared (within-child) | 0.010 | 0.013 | ||
| Wild Cluster Bootstrap p-value | 0.807 | 0.812 | ||
| C. Child Health | Overall Health | BMI | ||
| (1) | (2) | (1) | (2) | |
| Expansion | −0.002 (0.009) | 0.007 (0.009) | −0.444* (0.183) | −0.486* (0.192) |
| Mean of DV | 0.95 | 0.95 | 16.91 | 16.91 |
| Time Varying State Covariates | No | Yes | No | Yes |
| Observationsa | 7,430 | 7,430 | 8,140 | 8,140 |
| R-squared (within-child) | 0.002 | 0.002 | 0.458 | 0.459 |
| Wild Cluster Bootstrap p-value | 0.817 | 0.631 | 0.048 | 0.066 |
Notes: Each column of each panel corresponds to a different OLS regression model. Each model includes wave and child fixed effects and sampling weights. Expansion represents β from equation (2), as shown in appendix, and measures the average effect of the Medicaid expansions after it took place. Mean of each dependent variable (DV) provides the within-child average of the DV after controlling for just wave fixed effects. Heteroscedasticity-robust standard errors, in parentheses, are clustered at the state level.
Sample sizes (in child-years) are rounded to the nearest 10 as per dataset guidelines.
p < 0.05,
p < 0.01,
p < 0.001. We also report wild cluster bootstrapped p-values in the last row within each panel created using “boottest” command in STATA with 1,000 replications, which provides more conservative standard errors for inference in Table 4 (Cameron & Miller, 2008; 2015).
As expected, we find larger effects on self-reported overall parental health. Specifically, using this approach, we find an improvement in self-reported overall health by about 6 percentage points (~7% compared to ~4.7% in the main analysis). The effects on children’s BMI (Panel C) are approximately the same size (3%), and the insignificant findings for doctor visits and overall child health remain. Despite a reduction in precision when adjusted for fewer clusters, the results on parent health and child BMI are qualitatively similar (ps <0.10).
We also include event-study graphs below. Essentially, in this model, we include indicator variables to denote whether a child/parent from a low-income household (<138% FPL) resided in a state that expanded Medicaid at time t-j, for all integers j representing the number of years since the expansion. All coefficients are normalized to the year before the expansion (i.e. “−1” indicator). Again, all other model specifications are similar to (1), and include child fixed effects and sampling weights.
Although limited by the sample size and a relatively short post-expansion time period, we observe some interesting trends. First, we observe non-significant pre-trends further bolstering confidence in our identification strategy. Second, we find that the effects on parental health are larger and significant in the immediate years post-expansion and wane over time in our sample. In contrast, the effects on children’s BMI seems to grow over time. However, we interpret these effects with caution given the lack of precision in these dynamic effects.
Finally, we conducted a variety of other robustness checks such as (1) alternative coding/operationalization of the primary outcomes of interest; (2) alternative sample exclusions and fixed effects specifications; (3) and the examination of the role of staggered treatment timing on our baseline estimates. While we do not find any statistically significant effects on children’s classification of being overweight, underweight, or obese; our baseline results on parent health and child BMI are robust and qualitatively similar to alternative sample selections (such as households with less than 100% FPL, households where parents do not have a college-degree) and the exclusion of individual fixed effects (see Table S6). Finally, we find that 92 percent of our DD estimate of parent health and 93.5 percent of our DD estimate on child BMI comes from comparisons of treated and never treated cohorts. This reduces the concerns regarding the role of staggered treatment timing in our sample that the latest methodological advances in the applied DD literature have highlighted (See Appendix for more details).
DISCUSSION
We investigated how recent public health insurance expansions for adults in low-income households through the ACA affected the health of parents and their children. Using longitudinal data on a large, nationally representative cohort of kindergarteners from low-income households from 2010–2016, we found that parents’ self-reported health status improved significantly post-expansion in states that expanded their Medicaid programs to low-income adults. However, we did not observe any significant changes in children’s healthcare utilization (measured by a routine doctor visit in the past year) or parents’ assessment of their children’s health status. We also observed modest significant decreases in children’s BMI, especially for girls. We first contextualize the parental health effects and discuss the likely mechanisms that might be at play, and then turn our focus to interpreting the child health effects on BMI.
Although some low-income parents were eligible for public health insurance prior to the ACA based on varying state eligibility rules, many gained eligibility as a result of the ACA. Specifically, Medicaid/CHIP insurance rates among low-income parents in expansion states increased by about 12 percentage points by 2015 (in the first two years post-ACA).18 Research has also documented increased financial security from such insurance coverage and better parent health.18,35 Studies examining the impact of greater access to Medicaid in the 1990s and 2000s for low-income parents found improvements in parental use of preventive medical care36 and their reports of mental health.37 Unfortunately, the data do not allow us to examine the impact of ACA expansions on health insurance coverage among low-income parents; nevertheless, our results on improved parental health is consistent with prior research. By extending data in our sample through the spring of 2016, we find that the immediate positive parental health effects (albeit not significant)18 found in the ACA literature seem to be sustained beyond the initial years post-ACA implementation. Whether these effects are sustained in the longer-term is an important empirical question for future research given we see a regression to the mean towards the end of our sample time-period. We also find that the effects are stronger among Black, and below-median income households in this low-income sample (see Appendix Table S3). However, we interpret these heterogeneous findings with caution given low sample size for subsamples.
With respect to the spillovers on children’s health utilization and overall health status, we do not find significant changes. It is important to note that all children in our sample were likely eligible for public health insurance for multiple years prior to the ACA unlike their parents. With over 90 percent of these children receiving the recommended doctor visits and reporting good health status, it is perhaps not surprising to see that the parental health insurance expansions through the ACA did not have additional extensive margin effects on healthcare utilization or parent-rated overall child health status. Further, because we adjust for child fixed effects, only within-child variation pre- and post-ACA in these outcomes are captured in our final models which also exert some ceiling effects. Finally, because both these measures are parent-reported, we also note the limitations regarding their subjective nature despite their widespread use in past literature.27,28
Yet, in an objectively measured health outcome—childhood BMI, previously unexplored in the ACA literature—we document small protective effects of parental Medicaid eligibility. Specifically, the ACA Medicaid expansions reduced BMI, especially among girls. These effects are important since preventing excessive weight gain for school-aged children has been a focus of school-based public health interventions,38 due to its links to adult obesity and other deleterious effects across life-course.39,40 However, research has also shown that factors outside schools—specifically, parents and home environments—play a more prominent role in BMI changes for school-aged children.26,41,42 Parents may be making improved nutritional dietary choices and food-related routines for themselves and their children due to reduced stress.33,34 Suggestive evidence of improvements in children’s BMI over time warrants much closer attention as well. Future research on childhood obesity should examine the dynamic links between family functioning and BMI. Improvements in family income and economic well-being as a result of Medicaid coverage7,18 might also enable low-income households to afford healthier food purchases.35 Indeed, family income is considered a key social determinant of childhood obesity.36 We also examined sex differences in the effects of the expansions on children’s BMI because of documented sex differences in the social and behavioral risk factors for overweight and obesity in childhood.44 We found stronger BMI declines among girls relative to boys. These results coincide with existing research finding a stronger association between food insecurity and childhood BMI for girls,45,46 perhaps due to sex differences in response to stress and parental feeding practices.47,48
Our study has some limitations. Although we did not randomly assign Medicaid eligibility to parents in the sample as in a randomized control trial, we used a quasi-experimental design to isolate the effect of adult Medicaid eligibility. Because there may be omitted, time-varying variables that are correlated with both our health outcomes and whether a state expanded their Medicaid program, we use a variety of robustness checks to address this concern—including the use of both child fixed effects and wave fixed effects (so that only within-child variation, before and after the expansion could be driving the results), alternative sample exclusion strategy to identify precise set of parents who likely became newly eligible for Medicaid under the ACA, and placebo checks.
Our measures include parental self-report of their own health status and that of their children. While we acknowledge the potential bias in self-report, this single item self-rating of global health status has been used extensively in national surveys across multiple countries and shows strong reliability and discriminant validity in terms of health conditions, use of health services, and mortality.49 We also include direct assessments of children’s BMI, which is less subject to desirable response bias. Additionally, because the ECLS-K survey focuses on children, parental health measures that are consistently included across waves are limited to self-rated health. Future research should examine other parental health outcomes as well. Finally, we have three post-expansion waves in the dataset. Therefore, our results reflect only the short-term effects. Longer-term effects may be compounded given the importance of childhood health and the role of parents’ health in long-term gains.
Despite these limitations, these findings are important given the ongoing policy debates regarding changes to the ACA and the precarious and uncertain nature of the post-COVID-19 pandemic job market and the role of employer-sponsored health care. In particular, understanding the scope of the domains and populations in which the Medicaid expansions reach is important for accurately documenting the costs and benefits of Medicaid. Finally, this research also provides further evidence of a spillover of adult public health insurance eligibility onto children.
CONCLUSION
We document that the ACA’s Medicaid expansions for low-income adults improved parents’ self-rated health and children’s BMI. Given the health disparities that persist across the socioeconomic spectrum and the compounding nature of health improvements in childhood, the Medicaid program likely serves to shrink these gaps within states that expanded their Medicaid programs. These findings also indicate that there is the potential to reduce similar health disparities in states that have not yet expanded their Medicaid programs to low-income adults through the ACA.
Supplementary Material
Figure 2.
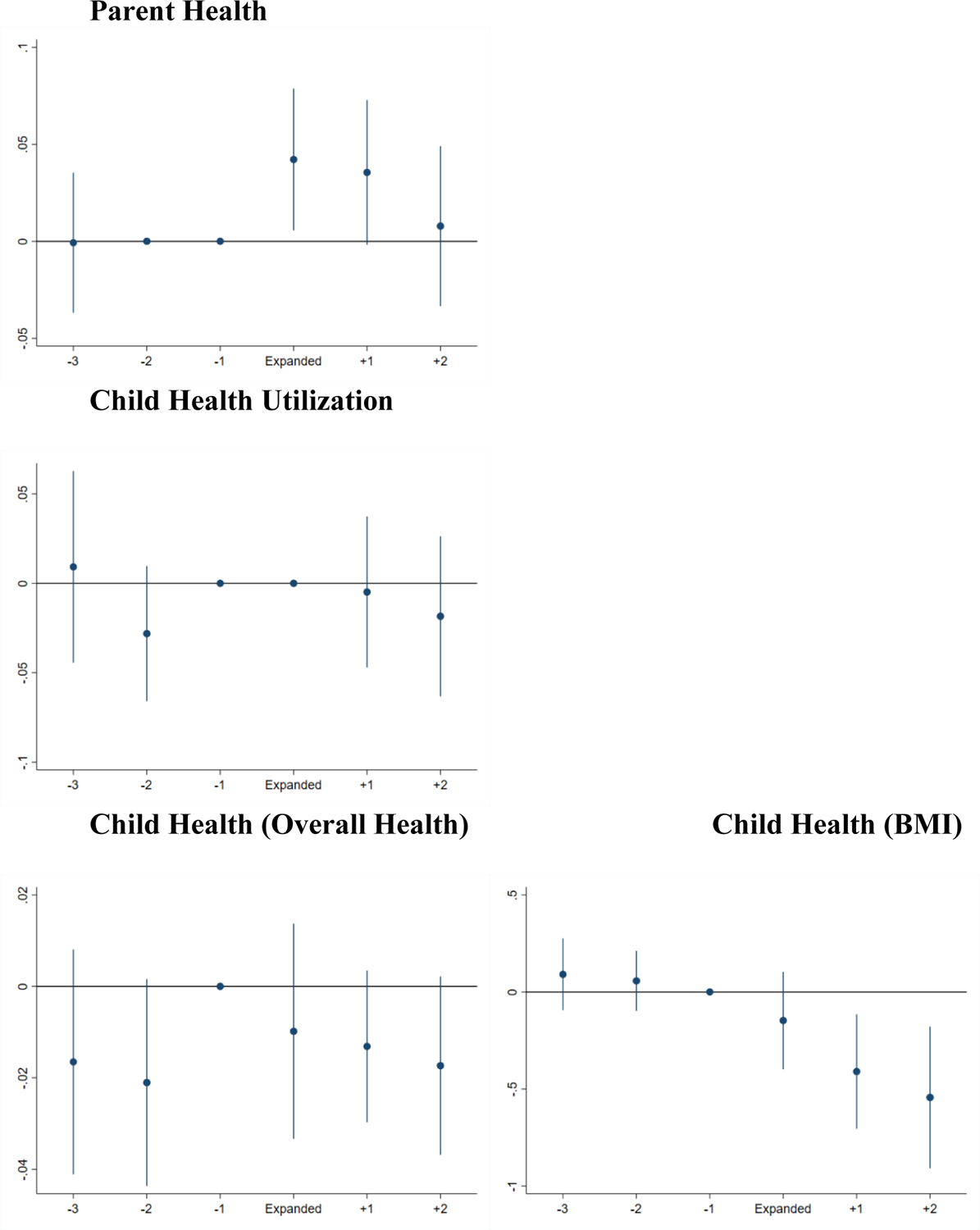
Event-Study Graphs
Notes: Each bar represents the 95 percent confidence internal (constructed with standard errors clustered at the state level), and the center of the bar represents the point estimate. The coefficient for the group “−1” (i.e. the one year prior to the Medicaid expansion) is normalized to zero. Similarly, coefficients for years in which the outcome is not measured in the sample is also reported as zero. Sample is limited to children in households with incomes below 138% FPL.
Highlights.
The Affordable Care Act (ACA) expanded eligibility to Medicaid programs among low-income parents in some states.
Quasi-experimental analysis of national data used to estimate the effect of the ACA Medicaid expansions on health outcomes.
Parents’ self-reported health improved significantly in states that expanded Medicaid through the ACA by 4 percentage points.
No significant changes in children’s use of routine doctor visits or parents’ assessment of their children’s health status.
Modest decreases in children’s body mass index (BMI) of about 2%, especially for girls, observed.
This study highlights the spillover effects of parental public health insurance eligibility onto children.
Funding/Support:
We acknowledge the restricted-use data access and a seed grant provided by the Population Research Institute at Penn State University, which is supported by an infrastructure grant by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD041025), to Gopalan.
Role of Funder/Sponsor (if any):
Our funders had no role in the design and conduct of the study.
Footnotes
Conflict of Interest Disclosures: The authors have no conflicts of interest relevant to this article to disclose.
To keep the comparisons clean we drop the children who moved across state lines across waves in our data. Only 30 movers had non-missing responses on our key variables of interest precluding any independent analysis of the subsample of movers.
See appendix for results and discussion on why BMI z-scores (calculated using age- and sex-specific CDC growth charts) are not well-suited for this analysis.30,31
These statistical differences persist even in the weighted means comparisons. It is however important to note that the sampling weights primarily adjust for nonresponse bias and differential attrition in the survey sample design. So, these weights are not intended to balance the treatment and comparison means to account for selection bias.
REFERENCES
- 1.McMorrow S, Gates JA, Long SK, Kenney GM. Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Affairs. 2017;36(5):808–818. [DOI] [PubMed] [Google Scholar]
- 2.Kaestner R, Garrett B, Chen J, Gangopadhyaya A, Fleming C. Effects of ACA Medicaid expansions on health insurance coverage and labor supply. Journal of Policy Analysis and Management. 2017;36(3):608–642. doi: 10.1002/pam.21993 [DOI] [PubMed] [Google Scholar]
- 3.Johnston EM, Strahan AE, Joski P, Dunlop AL, Adams EK. Impacts of the Affordable Care Act’s Medicaid expansion on women of reproductive age: differences by parental status and state policies. Women’s Health Issues. 2018;28(2):122–129. doi: 10.1016/j.whi.2017.11.005 [DOI] [PubMed] [Google Scholar]
- 4.Johnston EM, McMorrow S, Thomas TW, Kenney GM. ACA Medicaid Expansion and Insurance Coverage Among New Mothers Living in Poverty. Pediatrics. 2020;145(5). doi: 10.1542/peds.2019-3178 [DOI] [PubMed] [Google Scholar]
- 5.Wherry LR. State Medicaid Expansions for Parents Led to Increased Coverage and Prenatal Care Utilization among Pregnant Mothers. Health Services Research. 2018;53(5):3569–3591. doi: 10.1111/1475-6773.12820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hudson JL, Moriya AS. Medicaid Expansion For Adults Had Measurable ‘Welcome Mat’ Effects On Their Children. Health Affairs. 2017;36(9):1643–1651. doi: 10.1377/hlthaff.2017.0347 [DOI] [PubMed] [Google Scholar]
- 7.Wisk LE, Peltz A, Galbraith AA. Changes in Health Care–Related Financial Burden for US Families With Children Associated With the Affordable Care Act. JAMA Pediatrics. 2020;174(11):1032–1040. doi: 10.1001/jamapediatrics.2020.3973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venkataramani M, Pollack CE, Roberts ET. Spillover Effects of Adult Medicaid Expansions on Children’s Use of Preventive Services. Pediatrics. 2017;140(6). doi: 10.1542/peds.2017-0953 [DOI] [PubMed] [Google Scholar]
- 9.Bullinger LR, Gopalan M, Lombardi C. Impacts of Publicly Funded Health Insurance for Adults on Children’s Academic Achievement.; in prep. [DOI] [PMC free article] [PubMed]
- 10.Davidoff A, Dubay L, Kenney G, Yemane A. The effect of parents’ insurance coverage on access to care for low-income children. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2003;40(3):254–268. [DOI] [PubMed] [Google Scholar]
- 11.Gifford EJ, Weech-Maldonado R, Short PF. Low-Income Children’s Preventive Services Use: Implications of Parents’ Medicaid Status. Health Care Financ Rev. 2005;26(4):81–94. Accessed March 15, 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4194911/ [PMC free article] [PubMed] [Google Scholar]
- 12.DeVoe JE, Tillotson CJ, Wallace LS. Children’s Receipt of Health Care Services and Family Health Insurance Patterns. The Annals of Family Medicine. 2009;7(5):406–413. doi: 10.1370/afm.1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wallace J, Sommers BD. Health Insurance Effects on Preventive Care and Health: A Methodologic Review. American Journal of Preventive Medicine. 2016;50(5, Supplement 1):S27–S33. doi: 10.1016/j.amepre.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 14.Cotti C, Nesson E, Tefft N. Impacts of the ACA Medicaid expansion on health behaviors: Evidence from household panel data. Health Economics. 2019;28(2):219–244. doi: 10.1002/hec.3838 [DOI] [PubMed] [Google Scholar]
- 15.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health. Southern Economic Journal. 2018;84(3):660–691. doi: 10.1002/soej.12245 [DOI] [Google Scholar]
- 16.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Effects of the Affordable Care Act on Health Care Access and Self-Assessed Health After 3 Years. INQUIRY. 2018;55:0046958018796361. doi: 10.1177/0046958018796361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Effects of the Affordable Care Act on Health Behaviors After 3 Years. Eastern Econ J. 2019;45(1):7–33. doi: 10.1057/s41302-018-0119-4 [DOI] [Google Scholar]
- 18.McMorrow S, Gates JA, Long SK, Kenney GM. Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Affairs. 2017;36(5):808–818. [DOI] [PubMed] [Google Scholar]
- 19.Simon K, Soni A, Cawley J. The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions. J Pol Anal Manage. 2017;36(2):390–417. doi: 10.1002/pam.21972 [DOI] [PubMed] [Google Scholar]
- 20.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in Self-reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act. JAMA. 2015;314(4):366–374. doi: 10.1001/jama.2015.8421 [DOI] [PubMed] [Google Scholar]
- 21.Soni A, Wherry LR, Simon KI. How Have ACA Insurance Expansions Affected Health Outcomes? Findings From The Literature. Health Affairs. 2020;39(3):371–378. doi: 10.1377/hlthaff.2019.01436 [DOI] [PubMed] [Google Scholar]
- 22.Dubay L, Kenney G. Expanding public health insurance to parents: effects on children’s coverage under Medicaid. Health Services Research. 2003;38(5):1283–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamersma S, Kim M, Timpe B. The Effect of Parental Medicaid Expansions on Children’s Health Insurance Coverage. Contemporary Economic Policy. 2019;37(2):297–311. [Google Scholar]
- 24.Diep CS, Baranowski T, Kimbro RT. Acculturation and weight change in Asian-American children: Evidence from the ECLS-K:2011. Prev Med. 2017;99:286–292. doi: 10.1016/j.ypmed.2017.03.019 [DOI] [PubMed] [Google Scholar]
- 25.Bednar S, Rouse K. The effect of physical education on children’s body weight and human capital: New evidence from the ECLS-K:2011. Health Econ. 2020;29(4):393–405. doi: 10.1002/hec.3990 [DOI] [PubMed] [Google Scholar]
- 26.von Hippel PT, Workman J. From Kindergarten Through Second Grade, U.S. Children’s Obesity Prevalence Grows Only During Summer Vacations. Obesity (Silver Spring). 2016;24(11):2296–2300. doi: 10.1002/oby.21613 [DOI] [PubMed] [Google Scholar]
- 27.Thompson O. The long-term health impacts of Medicaid and CHIP. Journal of Health Economics. 2017;51:26–40. doi: 10.1016/j.jhealeco.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 28.Currie J, Decker S, Lin W. Has public health insurance for older children reduced disparities in access to care and health outcomes? Journal of Health Economics. 2008;27(6):1567–1581. doi: 10.1016/j.jhealeco.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 29.AAP COMMITTEE ON PRACTICE AND AMBULATORY MEDICINE, AAP BRIGHT FUTURES PERIODICITY SCHEDULE WORKGROUP. 2017 Recommendations for Preventive Pediatric Health Care. Pediatrics. 2017;139(4):e20170254. doi: 10.1542/peds.2017-0254 [DOI] [PubMed] [Google Scholar]
- 30.Berkey CS, Colditz GA. Adiposity in Adolescents: Change in Actual BMI Works Better Than Change in BMI z Score for Longitudinal Studies. Annals of Epidemiology. 2007;17(1):44–50. doi: 10.1016/j.annepidem.2006.07.014 [DOI] [PubMed] [Google Scholar]
- 31.Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z -score or BMI centile? European Journal of Clinical Nutrition. 2005;59(3):419–425. doi: 10.1038/sj.ejcn.1602090 [DOI] [PubMed] [Google Scholar]
- 32.Bertrand M, Duflo E, Mullainathan S. How Much Should We Trust Differences-in-Differences Estimates? The Quarterly Journal of Economics. 2004;119(1):249–275. Accessed September 11, 2018. https://www.jstor.org/stable/25098683 [Google Scholar]
- 33.Cameron A, Gelbach J, Miller D. Bootstrap-Based Improvements for Inference with Clustered Errors. The Review of Economics and Statistics. 2008;90(3):414–427. Accessed May 10, 2021. https://econpapers.repec.org/article/tprrestat/v_3a90_3ay_3a2008_3ai_3a3_3ap_3a414-427.htm [Google Scholar]
- 34.Cameron AC, Miller DL. A Practitioner’s Guide to Cluster-Robust Inference. J Human Resources. 2015;50(2):317–372. doi: 10.3368/jhr.50.2.317 [DOI] [Google Scholar]
- 35.Brantley E, Darden M, Ku L. Associations of Expanding Parental Medicaid Eligibility and Parental Health and Family Functioning. Academic Pediatrics. Published online July 26, 2021. doi: 10.1016/j.acap.2021.07.017 [DOI] [PubMed] [Google Scholar]
- 36.Busch SH, Duchovny N. Family coverage expansions: Impact on insurance coverage and health care utilization of parents. Journal of Health Economics. 2005;24(5):876–890. [DOI] [PubMed] [Google Scholar]
- 37.McMorrow S, Kenney GM, Long SK, Goin DE. Medicaid Expansions from 1997 to 2009 Increased Coverage and Improved Access and Mental Health Outcomes for Low-Income Parents. Health Serv Res. 2016;51(4):1347–1367. doi: 10.1111/1475-6773.12432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Story M, Kaphingst KM, French S. The role of schools in obesity prevention. Future Child. 2006;16(1):109–142. doi: 10.1353/foc.2006.0007 [DOI] [PubMed] [Google Scholar]
- 39.Whitaker RC, Pepe MS, Wright JA, Seidel KD, Dietz WH. Early adiposity rebound and the risk of adult obesity. Pediatrics. 1998;101(3):E5. doi: 10.1542/peds.101.3.e5 [DOI] [PubMed] [Google Scholar]
- 40.Wilson SE, Crosnoe R, Daniels K. Introduction to Special Issue on Obesity and the Family across the Life Course. Economics & Human Biology. 2012;10(4):329–332. doi: 10.1016/j.ehb.2012.05.003 [DOI] [PubMed] [Google Scholar]
- 41.von Hippel PT, Powell B, Downey DB, Rowland NJ. The Effect of School on Overweight in Childhood: Gain in Body Mass Index During the School Year and During Summer Vacation. Am J Public Health. 2007;97(4):696–702. doi: 10.2105/AJPH.2005.080754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anderson PM. Parental employment, family routines and childhood obesity. Economics & Human Biology. 2012;10(4):340–351. doi: 10.1016/j.ehb.2012.04.006 [DOI] [PubMed] [Google Scholar]
- 43.Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in Obesity Prevalence by Demographics and Urbanization in US Children and Adolescents, 2013–2016. JAMA. 2018;319(23):2410–2418. doi: 10.1001/jama.2018.5158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wisniewski AB, Chernausek SD. Gender in childhood obesity: Family environment, hormones, and genes. Gender Medicine. 2009;6:76–85. doi: 10.1016/j.genm.2008.12.001 [DOI] [PubMed] [Google Scholar]
- 45.Casey PH, Simpson PM, Gossett JM, et al. The Association of Child and Household Food Insecurity With Childhood Overweight Status. Pediatrics. 2006;118(5):e1406–e1413. doi: 10.1542/peds.2006-0097 [DOI] [PubMed] [Google Scholar]
- 46.Speirs KE, Fiese BH, STRONG Kids Research Team. The Relationship Between Food Insecurity and BMI for Preschool Children. Matern Child Health J. 2016;20(4):925–933. doi: 10.1007/s10995-015-1881-0 [DOI] [PubMed] [Google Scholar]
- 47.Faith MS, Scanlon KS, Birch LL, Francis LA, Sherry B. Parent-Child Feeding Strategies and Their Relationships to Child Eating and Weight Status. Obesity Research. 2004;12(11):1711–1722. doi: 10.1038/oby.2004.212 [DOI] [PubMed] [Google Scholar]
- 48.Jyoti DF, Frongillo EA, Jones SJ. Food Insecurity Affects School Children’s Academic Performance, Weight Gain, and Social Skills. The Journal of Nutrition. 2005;135(12):2831–2839. doi: 10.1093/jn/135.12.2831 [DOI] [PubMed] [Google Scholar]
- 49.Bowling A. Just one question: If one question works, why ask several? Journal of Epidemiology & Community Health. 2005;59(5):342–345. doi: 10.1136/jech.2004.021204 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


