Abstract
Background:
Malnutrition among under-five children (U5C) in India is a major public health problem due to double burden caused by nutritional transition. WHO cut-offs are adopted as global growth standards which define how children should grow in condition of optimal nutrition and health. Growth references which are representative of population-specific existing growth patterns need to be updated regularly which is cumbersome; hence, the author’s group published ‘synthetic growth references’ for Indian children of age 0–18 years.
Objectives:
The objective of this study is to field test the new synthetic growth references in U5C for height-for-age, weight-for-age and body mass index (BMI)-for-age against WHO charts in urban and rural Indian children to estimate prevalence of various indices of malnutrition.
Methods:
A cross-sectional anthropometric assessment of apparently healthy rural and urban Indian U5C attending vaccination centre was performed using standard protocols. They were converted to Z-scores using WHO and Indian synthetic growth references. The equality of proportion of parameters of malnutrition was tested by McNemar’s test and P value <0.05 was considered significant.
Results:
WHO charts significantly overestimated stunting and malnutrition as compared to synthetic references with difference in sensitivity of 7.2% and 8.5%, respectively, and converse for over-nutrition by 2.1%. The most commonly affected parameter of malnutrition was underweight. Stunting was significantly higher in rural population using both cut-offs (P < 0.05).
Conclusion:
The synthetic references limit the spread of weight and BMI and do not overestimate stunting and wasting. They may be more useful for identification of malnutrition and may thus be recommended for routine screening in Indian U5C.
Keywords: Malnutrition, obesity, stunting, synthetic, WHO
INTRODUCTION
The World Health Organization (WHO) defines malnutrition as deficiencies, excesses or imbalances in a person’s intake of energy and/or nutrients. Approximately 45% of deaths among children under 5 years of age have been linked to under-nutrition.[1] The United Nations Children’s Fund with WHO and World Bank Group Joint Child Malnutrition Estimates in its key findings of the 2020 edition states that, globally, 144 million children (21.3%) under 5 years were stunted and 47 million (6.9%) were wasted, of which 14.3 million were severely wasted and 38.9 million (5.6%) were overweight or obese. Malnutrition rates remain alarming with stunting declining slowly from 2000 to 2019 (32.4% to 21.3%) while overweight rates increased from 4.9% to 5.7% in the same duration. The low- and middle-income countries are facing the challenge of double burden of malnutrition consisting of both under-nutrition and overweight and obesity. Majority of all stunted (54%), wasted (69%) and overweight (45%) children under 5 years of age live in Asia. The south-east Asia region performs worse than global average with rates of stunting, wasting and overweight being 24.7%, 8.2% and 7.5%, respectively.[2]
Malnutrition among under-5 children is a major public health problem in India. The burden of under-nutrition among under-5 children remains the same despite various intervention programs. Further, changing dietary patterns have resulted in increased prevalence of obesity. It is well known that assessment of growth using anthropometric methods is critical to assess nutritional status of children. The WHO growth standards for children under the age of 5 years were published in 2006 and have been adopted as a global single standard of childhood growth for under-5 children in many countries including India. They are growth standards and thus define how a population of children should grow in condition of optimal nutrition and health. However, they may over-diagnose underweight and stunting in a number of apparently normal children in developing countries like India.[3] Thus, a growth reference which is representative of population-specific existing growth pattern may provide a more accurate estimate.
The data collection for updating growth references is expensive and cumbersome; hence, the author’s group published ‘synthetic growth references’ as a more feasible alternative for Indian children of age 0–18 years.[4] Although these synthetic charts have been constructed robustly and are compared with the lambda-mu-sigma (LMS) references and Indian Academy of Paediatrics (IAP) 2015 charts in 5–18-year age range, there are no data on how they perform in comparison with the WHO growth standards in children under 5 years. Further, it is essential to understand how interpretation of growth parameters differs between references generated by synthesizing population-specific anthropometry and the WHO standards in urban as well as rural children.
Thus, the aim of our study was to field test the new synthetic growth references in children under 5 years of age. The specific objectives were (1) to compare standard deviation (SD) scores (Z-scores) of children’s height-for-age, weight-for-age and body mass index (BMI)-for-age as computed based on the WHO charts against the synthetic references in urban and rural children, and (2) to compare prevalence of various indices of malnutrition as judged by both the references.
METHODS
Subjects and design
This cross-sectional, observational study was performed from October 2020 to April 2021 from rural and urban areas of Pune district of Maharashtra (Western India). Apparently healthy children between the ages of 0 and 60 months attending an urban health centre and a rural primary health centre for vaccination were included in this study. Children who appeared syndromic (assessed by trained medical personnel) or were on any medication besides multivitamins were not included in this study. Written informed consent was obtained from the parents before measurements were made. An ethical approval was obtained from the institutional ethics committee. Sample size of 1252 was sufficient to achieve 80% power of study at 5% level of significance (alpha) and 10% margin of error (delta) using National Family Health Survey (NFHS-5) data published in 2019–2020 on prevalence of malnutrition.[5]
Anthropometry
We measured recumbent length for children less than 2 years and standing height thereafter based on the Participant Manual for Facility Based Care of Severe Acute Malnutrition given by Ministry of Health and Family Welfare, Government of India, 2013.[6] Length was measured using an infantometer (Medsor Impex) with a headboard and sliding foot piece placed on a stable, level table covered with a thin cloth. One person stood behind the headboard and positioned the child lying on his back on the measuring board, supporting the head and placing it against the headboard. The crown of the head was placed against the headboard, compressing the hair by holding the head with two hands and tilting upwards until the eyes looked straight up, and the line of sight was perpendicular to the measuring board. The other person placed one hand on the shins or knees and pressed gently but firmly and placed the foot piece firmly against the feet. The soles of the feet were placed flat on the foot piece with toes pointing up. The length was measured up to the last completed 0.1 cm and recorded. Height (Seca Portable stadiometer, Hamburg, Germany up to 0.1 cm accuracy) and body weight (Seca 876 Flat scale, Hamburg, Germany, up to 100 g accuracy) were measured using standard protocols. BMI was computed using the following formula: BMI = weight (kg)/height (m) 2.
Z-score calculation
The Z scores for WHO references were calculated using the WHO AnthroPlus app.[7] The synthetic charts were produced by computing means using non-linear regression equations for height, weight and BMI at all ages from birth to 18 years using equations described by Hermanussen from the means at key ages (birth, school entry and adult height) followed by creation of percentiles. The Z scores for synthetic references were calculated using synthesized anthropometry LMS values.[4]
Classification of malnutrition
Malnutrition was classified using WHO classification of nutritional status of infants and children as shown in Table 1.[8,9]
Table 1.
WHO definition of parameters of nutritional status
| Nutritional status | Definition |
|---|---|
| Stunted | Length/Height for age <2SD |
| Severely stunted | Length/Height for age <3SD |
| Underweight | Weight for age <2SD |
| Severely underweight | Weight for age <3SD |
| Moderate acute malnutrition | BMI-for-age <2SD and >3SD |
| Severe acute malnutrition | BMI-for-age <3SD |
| Overweight | BMI-for-age >2SD and <3SD |
| Obese | BMI-for-age >3SD |
SD: Standard deviation, BMI: body mass index
Difference in sensitivity
The difference in the proportion of patients classified by any parameter of malnutrition according to synthetic or WHO growth standards/references was calculated by the following equation: difference in sensitivity = (ns − nw)/N, where ns is the number of children classified by synthetic charts and nw is the number of children classified by WHO references and N is the total.
Statistical analysis
Data were analysed using SPSS 25.0 for Windows (IBM SPSS, Bangalore, India). Descriptive statistics for demographic and anthropometric characteristics were calculated by gender and rural or urban background. Differences in means among children were calculated using independent sample t test. Sensitivity of various parameters of malnutrition was calculated using both WHO and synthetic references. The equality of the proportions classified by various parameters of malnutrition according to synthetic and WHO growth references was evaluated based on gender and socioeconomic status using the McNemar test. P value less than 0.05 was considered significant.
RESULTS
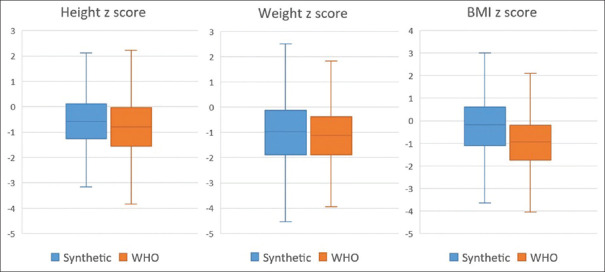
Of the 1252 children who were enrolled in this study, 2 were excluded for erroneous data as the height and weight were either below or above 5SD score.[10] A total of 1250 (666 boys) children were included in this study and their data were analysed. Based on the area of residence, 800 children (448 boys) belonged to urban areas of Pune and 450 (218 boys) were rural children. The mean and SD of height Z score, weight Z score and BMI Z score of entire study group are − 0.5 ± 1.1, −1 ± 1.3 and − 0.3 ± 1.3 for synthetic cut-offs while they are − 0.7 ± 1.2, −1.1 ± 1.1 and − 0.9 ± 1.2, respectively, for WHO cut-offs. Figure 1 shows comparison of these values by both cut-offs. On performing paired t-test, there is significant difference between these values (P < 0.05).
Figure 1.
Comparison of mean height Z score, weight Z score and BMI Z score by WHO and synthetic growth references
Table 2a illustrates the demographic and mean anthropometric characteristics of children as per area of residence (urban vs. rural). No significant differences were noted between genders and urban/rural groups except rural girls who had lower mean weight and BMI than rural boys. The mean and SD scores of children from different socioeconomic groups based on the WHO charts and synthetic growth charts are illustrated in Table 2b. There were no significant differences in mean anthropometric parameters between urban and rural subjects of either gender. No significant differences were noted in the 0–2-year and 2–5-year age groups.
Table 2a.
Demographic and anthropometric measures
| Parameter | Boys | Girls | ||
|---|---|---|---|---|
|
|
|
|||
| Urban | Rural | Urban | Rural | |
| Age (months) | 47.8±7.2 | 48.9±7.8 | 48.6±7.2 | 47.9±7.6 |
| Weight (kg)* | 14.4±2.7 | 14.4±2.3 | 14.2±2.4 | 13.8±2.5 |
| Height/Length (cm) | 100.0±6.4 | 100.3±6.6 | 99.9±6.1 | 99.1±6.4 |
| BMI (kg/m2)* | 14.3±1.6 | 14.2±1.2 | 14.1±1.5 | 14.0±1.3 |
*Statistically significant difference between rural girls and rural boys at P<0.05
Table 2b.
Mean Z scores of rural/urban children on WHO standards and synthetic growth charts for the appropriate age and sex
| Charts | Sex | Height | Weight | BMI | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Urban | Rural | Urban | Rural | Urban | Rural | ||
| WHO | Boys | −0.7±1.1 | −0.7±1.4 | −1.1±1.2 | −1.1±1.1 | −0.9±1.3 | −0.9±1.0 |
| Girls | −0.6±1.0 | −0.7±1.4 | −1.0±1.1 | −1.1±1.1 | −0.9±1.2 | −1.0±1.0 | |
| Synthetic | Boys | −0.5±1.0 | −0.5±1.2 | −1.1±1.4 | −1.1±1.3 | −0.3±1.5 | −0.2±1.1 |
| Girls | −0.4±0.9 | −0.5±1.2 | −0.8±1.2 | −0.9±1.3 | −0.2±1.3 | −0.3±1.1 | |
WHO: World Health Organization. No significant difference noted in mean anthropometric measures by gender or area of residence using either growth chart cut-offs
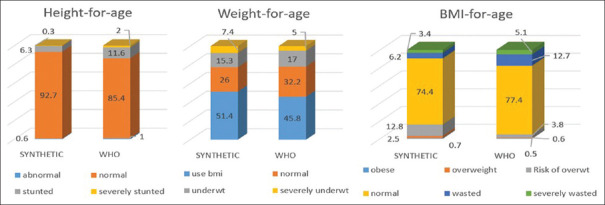
As shown in Figure 2, there was a significant difference (P < 0.05) in children classified as within reference range, stunted and severely stunted with WHO classifying more subjects as stunted compared to synthetic chart references. In weight-for-age categories however, there was no difference in classifying as underweight but WHO charts significantly (P < 0.05) normalized weight as compared to synthetic charts. Among the BMI-for-age categories, both cut-offs identified obese and normal similarly but synthetic charts significantly (P < 0.05) identified overweight and risk of overweight higher than WHO charts while converse was observed for wasting.
Figure 2.
Anthropometric characteristics assessed on WHO and synthetic charts
As seen in Figure 3, on performing related samples McNemar’s test, we found no significant difference in the two methods in identifying underweight (weight for age). However, the WHO charts significantly overestimated stunting as compared to synthetic references (P < 0.05) on McNemar’s test with difference in sensitivity of 7.2%. On using the BMI-for-age charts, WHO references identified significantly higher proportion as malnourished as compared to synthetic references and vice versa for over-nutrition with difference in sensitivity of 8.5% and 2.1%, respectively (P < 0.05).
Figure 3.
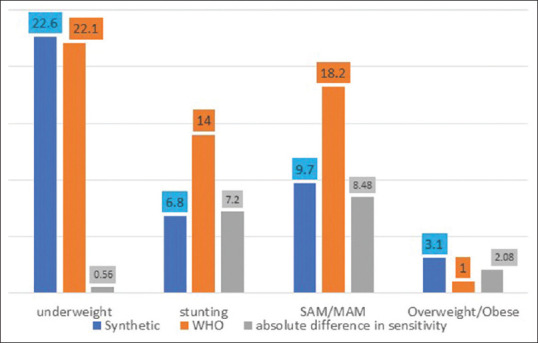
Sensitivity of WHO and synthetic growth references in identifying malnourishment in 0–5-year-old Indian children
Table 3a illustrates comparison of various parameters of malnutrition based on synthetic and WHO references. We noted a significantly higher prevalence of severe acute malnutrition in urban population as compared to rural population by using both WHO and synthetic references and vice versa for moderate acute malnutrition by only WHO cut-offs. We also found a significantly higher prevalence of moderate stunting among rural populations by both references.
Table 3a.
Comparison of prevalence of various parameters of malnutrition based on synthetic and WHO references
| Parameter | WHO | Synthetic | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Urban (%) | Rural (%) | Total (%) | Urban (%) | Rural (%) | Total (%) | |
| BMI | ||||||
| SAM*+ | 7.10 | 1.80 | 5.20 | 5.10 | 0.40 | 3.40 |
| MAM+ | 10.90 | 16.70 | 13 | 5.90 | 6.90 | 6.20 |
| Overweight | 0.80 | 0.20 | 0.60 | 3 | 1.60 | 2.50 |
| Obese | 0.50 | 0.40 | 0.50 | 0.80 | 0.40 | 0.60 |
| Weight | ||||||
| Severely underweight | 4.90 | 5.30 | 5.00 | 6.90 | 8.40 | 7.40 |
| Moderately underweight | 16.40 | 18.20 | 17.10 | 15.10 | 15.30 | 15.20 |
| Height | ||||||
| Severely stunted | 1.50 | 2.90 | 2 | 0.40 | 0.20 | 0.30 |
| moderately stunted*+ | 9.60 | 16.20 | 12 | 5 | 9.10 | 6.50 |
*Statistically significant difference by synthetic Z scores. +Statistically significant difference by WHO Z scores
On assessing these parameters segregated by gender, we found no significant differences in prevalence of acute malnutrition in both urban and rural populations. Overall, we found a significantly higher prevalence of malnutrition by synthetic references in urban populations than in rural. Stunting was significantly higher in rural population than in urban population in both genders using the WHO cut-offs (P < 0.05 for both). No such differences were noted in either gender using synthetic references; however, overall higher prevalence of chronic malnutrition was noted in the rural population [Table 3b].
Table 3b.
Comparison of prevalence of various parameters of malnutrition by gender and area of residence based on synthetic and WHO references
| Parameter | WHO | Synthetic | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Boys | Girls | Boys | Girls | |||||
|
|
|
|
|
|||||
| Urban (%) | Rural (%) | Urban (%) | Rural (%) | Urban (%) | Rural (%) | Urban (%) | Rural (%) | |
| Stunting* | 11.60 | 20.60 | 10.50 | 17.70 | 4.90 | 8.70 | 6.00 | 9.90 |
| Underweight | 22.80 | 22.50 | 19.30 | 24.60 | 25.40 | 25.20 | 17.60 | 22.40 |
| MAM/SAM | 19.40 | 14.70 | 16.20 | 22.00 | 11.40 | 6.90 | 10.50 | 7.80 |
| Overweight/Obese | 1.80 | 0.90 | 0.60 | 0.40 | 3.80 | 2.30 | 3.70 | 1.70 |
*Statistically significant (P<0.05) using WHO Z scores
DISCUSSION
We report that prevalence of stunting, wasting, underweight and overweight by WHO and synthetic cut-offs were 14% and 6.8%, 18.2% and 9.7%, 22.1% and 22.6%, 1% and 3.1%, respectively. The most commonly affected parameter of malnutrition was underweight (weight for age). Overall, the prevalence of stunting (height for age) was significantly higher in rural population than in urban population and converse for severe wasting. No significant gender-wise differences were noted in any malnutrition parameters. Upon comparing the percentage abnormal using the WHO and synthetic cut-offs, we found no significant difference in weight-for-age cut-offs; however, the WHO cut-offs overestimate stunting with difference of sensitivity of 7.2%. Moreover, upon comparing the BMI-for-age cut-offs, the WHO references identify a significantly higher proportion as acutely malnourished as compared to synthetic references by 8.5% and vice versa for over-nutrition with difference in sensitivity of 2.1%.
The percentage of various parameters of malnutrition reported by us is lower than the national average as reported in the recently published NHFS-5 (2019–2020) data, although the prevalence and urban versus rural trend of underweight, overweight and wasting (malnutrition) are similar. Similar to our study, the NHFS-5 reports higher prevalence of underweight (27.3% vs. 33.8%) and wasting (18.5% vs. 19.5%) in rural population while higher rates of over-nutrition (4.2% vs. 3.2%) in urban population.[5] The same trend is reported for the state of Maharashtra in the NFHS-5 data with higher prevalence rates. In reference to stunting, we report much lower rate of stunting than the national and Maharashtra estimates as per the NHFS-5 report; however, similar to our study, they also identify rural children under the age of 5 years to be more stunted than urban ones.[5] A review article on malnutrition among under-5 children in India and strategies for control has reported a wide range of prevalence of underweight, stunting and wasting ranging from 39% to 75%, 15.4% to 74% and 10.6% to 42.3%, respectively.[10] Very few studies have been conducted to assess the prevalence of overweight or obesity among under-5 children, with results showing prevalence up to 4.5%.[11] Similar to our study, a study on children under 5 years in Chennai found prevalence of underweight, stunting, wasting and overweight to be 19.9% (95% CI 15.9–24.4), 17.1% (95% CI 13.3–21.4), 21.6% (95% CI 17.4–26.2) and 1.4%, respectively, with no significant gender difference.[12] In contrast to our results, another study from Maharashtra reports stunting as the commonest form of under-nutrition observed.[13] This observed difference in prevalence rates of under-nutrition and over-nutrition between national and local studies may be due to the difference in the methodology adopted, operational definitions, instruments used, sample size studied and the geographical area involved in this study.[10]
We note difference in sensitivity of 7.2% between WHO and synthetic cut-offs in identifying stunting (height/length for age or chronic malnutrition) with WHO cut-offs overestimating stunting. Studies have shown a higher prevalence of short stature as per WHO charts compared to IAP 2015 in privileged school children around Pune in 5–18-year olds.[14] Another Indian study also suggests that IAP 2015 criteria have better diagnostic accuracy in identifying short stature in Indian children as compared to use of WHO criteria which causes unwarranted work-up in a substantial number of subjects.[15] Underweight and stunting are likely to be over-diagnosed in a large number of apparently normal children in developing countries such as India upon using WHO references.[16] A study of comparison of WHO growth standards with IAP growth charts of under-5 children in a rural area of Puducherry showed no significant difference in prevalence of underweight but WHO references estimated a significantly higher prevalence of stunting.[17] Marked mismatch exists between WHO standards and country-specific synthetic height and weight data from Indonesia and Romania which necessitated the development of synthetic charts in these countries.[18,19] This is perhaps related to the fact that population height is more genetically determined at all ages and Asians are known to be short when compared to WHO standards at all ages.
A Chinese study reports higher prevalence of stunting, underweight and wasting using the Chinese national growth charts as compared to WHO references and vice versa for overweight.[20] Various studies have reported that growth charts in different countries are different from the WHO references with respect to height of children. As children on whom Japanese growth charts were constructed were shorter than the WHO growth standards, the prevalence of stunting is expected to be higher when the WHO growth standards are used in these populations.[21] As the WHO height/length standards are much higher than the country-specific height references and wasting is a ratio of weight for height, wasting by WHO standards is much higher for the local population. Authors’ group in a previous study has reported higher prevalence of overweight/obesity with better accuracy by using IAP BMI charts as compared to WHO growth references for 5–18-year-old Indian children.[22] The difference in the assessments between the WHO growth standards and local growth references may be due to environmental, genetic or epigenetic factors and that local growth charts may be more suitable for individual growth monitoring.[23]
Ours is the first study where the Indian national synthetic charts have been field-tested for parameters of malnutrition as compared to WHO growth standards in children less than 5 years age. The strength of this study is that children from both rural and urban areas have been studied and a comparison has been made between the WHO and synthetic references. However, this study has limitation of including data from a single centre, and although healthy children were selected for this study, no investigations were carried out to assess ill health.
To conclude, our field-testing study showed that prevalence of stunting was higher while overweight was lower in under-5 Indian children while using WHO growth standards as compared to Indian synthetic growth references. The synthetic references have a narrower range for both weight and BMI; they may be more useful for screening for obesity. Synthetic references can be created using minimal data and are useful in updating growth references in place of collecting data on large number of children. Our study suggests that synthetic growth references may be used for routine screening of malnutrition in rural and urban Indian children less than 5 years age. Larger studies are required to confirm these observations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1. [Last accessed on 2022 Jan 03]. Available from:https://www.who.int/news-room/fact-sheets/detail/malnutrition .
- 2.United Nations Children's Fund (UNICEF), World Health Organization, International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition:Key Findings of the 2020 Edition of the Joint Child Malnutrition Estimates. Geneva: World Health Organization; 2020. [Google Scholar]
- 3.Khadilkar VV, Khadilkar AV, Chiplonkar SA. Growth performance of affluent Indian preschool children:A comparison with the new WHO growth standard. Indian Pediatr. 2010;47:869–72. doi: 10.1007/s13312-010-0147-6. [DOI] [PubMed] [Google Scholar]
- 4.Khadilkar V, Khadilkar AV, Kajale N. Indian growth references from 018 yearold children and adolescents-A comparison of two methods. Indian J Endocr Metab. 2019;23:635–44. doi: 10.4103/ijem.IJEM_555_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NFHS-5 National Family Health Survey (NFHS-5) 2019-20 India. Int Inst Popul Sci ICF. 2017. [Last accessed on 2022 Jan 03]. pp. 1–192. Available from:http://rchiips.org/NFHS/NFHS-4Reports/India.pdfhttp://rchiips.org/nfhs/NFHS-5_FCTS/India.pdf .
- 6. [Last accessed on 2022 Jan 03]. Available from:https://www.nhm.gov.in/images/pdf/programmes/child-health/IEC-materials/PARTICIPANT-MANUAL_FBCSA- Malnutrition.pdf .
- 7.WHO AnthroPlus for Personal Computers Manual:Software for Assessing Growth of the World's Children and Adolescents. Geneva: WHO; 2009. [Last accessed on 2021 Dec 29]. Available from:http://www.who.int/growthref/tools/en/ [Google Scholar]
- 8.World Health Organization. Guideline:assessing and managing children at primary health-care facilities to prevent overweight and obesity in the context of the double burden of malnutrition. [PubMed] [Google Scholar]
- 9.Mansourian M, Marateb HR, Kelishadi R, Motlagh ME, Aminaee T, Taslimi M, et al. First growth curves based on the World Health Organization reference in a nationally representative sample of pediatric population in the Middle East and North Africa (MENA):The CASPIAN-III study. BMC Pediatr. 2012;12:149. doi: 10.1186/1471-2431-12-149. doi:10.1186/1471-2431-12-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sahu SK, Kumar SG, Bhat BV, Premarajan KC, Sarkar S, Roy G, et al. Malnutrition among under-five children in India and strategies for control. J Nat Sci Biol Med. 2015;6:18–23. doi: 10.4103/0976-9668.149072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar HN, Mohanan P, Kotian S, Sajjan BS, Kumar SG. Prevalence of overweight and obesity among preschool children in semi urban South India. Indian Pediatr. 2008;45:497–49. [PubMed] [Google Scholar]
- 12.Sundari S. A Study on the prevalence and pattern of malnutrition among children under five years in Chennai. Int J Pharm Bio Sci. 2017;8:(B):135–9. [Google Scholar]
- 13.Murarkar S, Gothankar J, Doke P, Pore P, Lalwani S, Dhumale G, et al. Prevalence and determinants of undernutrition among under-five children residing in urban slums and rural area, Maharashtra, India:A community-based cross-sectional study. BMC Public Health. 2020;20:1–9. doi: 10.1186/s12889-020-09642-0. doi:10.1186/s12889-020-09642-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lohiya N, Khadilkar V, Pawar S, Khadilkar A, Chiplonkar S, Jahagirdar R. Field testing of IAP 2015 growth charts. Indian J Pediatr. 2018;85:723–8. doi: 10.1007/s12098-018-2621-4. [DOI] [PubMed] [Google Scholar]
- 15.Patel R, Bajpai A. Evaluation of short stature in children and adolescents. Indian J Pediatr. 2021;88:1196–202. doi: 10.1007/s12098-021-03880-9. [DOI] [PubMed] [Google Scholar]
- 16.Khadilkar V, Khadilkar A. Growth charts:A diagnostic tool. Indian J Endocrinol Metabol. 2011;15(Suppl 3):S166. doi: 10.4103/2230-8210.84854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.John J. Comparison of World Health Organization growth standards with Indian academy of pediatrics growth charts of under-five children in a rural area of Puducherry. Med J Dr. DY Patil Univ. 2017;10:22. [Google Scholar]
- 18.Pulungan AB, Julia M, Batubara JRL, Hermanussen M. Indonesian national synthetic growth charts. Acta Sci Paediatr. 2018;1:20–34. [Google Scholar]
- 19.Pascanu I, Pop R, Barbu CG, Dumitrescu CP, Gherlan I, Marginean O, et al. Development of synthetic growth charts for Romanian population. Acta Endocrinologica (Bucharest) 2016;12:309. doi: 10.4183/aeb.2016.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang Z, Duan Y, Ma G, Yang X, Yin S. Comparison of the China growth charts with the WHO growth standards in assessing malnutrition of children. BMJ Open. 2015;5:e006107. doi: 10.1136/bmjopen-2014-006107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lucas A. Growth and later health:A general perspective. Nestle Nutr Workshop Ser Pediatr Program. 2010;65:1–9. doi: 10.1159/000281107. discussion 9-11. doi:10.1159/000281107. [DOI] [PubMed] [Google Scholar]
- 22.Oza C, Khadilkar V, Gondhalekar K, Kajale N, Khadilkar A. Predictive value of WHO vs. IAP BMI charts for identification of metabolic risk in Indian children and adolescents. J Pediatr Endocrinol Metab. 2021;34:1605–10. doi: 10.1515/jpem-2021-0411. [DOI] [PubMed] [Google Scholar]
- 23.Gillman MW. Early infancy as a critical period for development of obesity and related conditions. Nestle Nutr Workshop Ser Pediatr Program. 2010;65:13–20. doi: 10.1159/000281141. discussion 20-14. [DOI] [PMC free article] [PubMed] [Google Scholar]