Abstract
Recruitment, retention, and adherence within health intervention research have been understudied in Indigenous communities, where well-known health disparities exist. The purpose of this paper is to describe planned versus actual recruitment, retention, and adherence strategies and the evaluation of retention and adherence strategies for a community-based research study of a Chronic Illness (CI) self-management intervention within an Indigenous community. A Community-Based Participatory Research (CBPR) approach was used to develop and implement Báa nnilah, a culturally consonant educational intervention to improve CI self-management. Reasons for participant adherence and retention were tracked and recorded over time. A post-intervention survey assessed barriers and facilitators to intervention adherence. Overall, recruitment, retention, and adherence methods were successful in enrolling and maintaining participation. Using a CBPR approach and culturally consonant strategies may assist in meeting recruitment goals and improving sustained participation of community members, thus impacting health disparities among Indigenous communities.
Keywords: Recruitment, Retention, Adherence, Indigenous, Chronic Illness, Intervention Evaluation
Background
Effective recruitment and retention of participants in health research provides individuals and communities opportunities to access innovative medical interventions, which are important for reducing health disparities. Unfortunately, Indigenous communities are under-represented in health research despite experiencing health inequities [1]. Previous and current harmful U.S. governmental policies and programs, externally imposed research agendas, and lack of community benefit from prior research can negatively impact recruitment and retention for health research studies within Indigenous populations [2].
Intervention research involves the following: recruitment of community members to participate in research; retention of participants for the duration of the research study; and adherence of participants in intervention activities for the entire intervention period [3, 4]. Each has a range of impacts on the quality and translatability of study findings, such as the ability to make inferences about the data (internal validity), the extent to which findings can be generalized to the greater population (external validity), and statistical power for quantitative studies [5–7]. High levels of recruitment and retention increase confidence in whether an intervention has contributed to improved health, which is valued by communities. Additionally, individuals with greater program adherence often benefit the most from the intervention [4].
Community-Based Participatory Research (CBPR) is an approach for partnership building, intervention development and dissemination, and implementation research. Using a CBPR approach may improve recruitment, retention, and adherence by using local community knowledge about barriers and facilitators of each [7–9]. Principles of CBPR that particularly apply to recruitment and retention include 1) building on strengths and resources within the community and 2) facilitating collaborative, equitable partnerships in all research phases and involving a power-sharing process that attends to social inequalities [10]. U.S. tribal college students responded in a survey that they believe the application of CBPR principles can overcome common research participation obstacles by gaining trust, credibility, and establishing interest and relevancy [11]. CBPR approaches can also successfully guide the development of recruitment, retention, and adherence strategies that result in respectful interaction between the research team and community members [12, 13].
There are few published studies whose topics touch upon effective strategies for recruitment, retention, and adherence for intervention research and even fewer that use a CBPR approach in Indigenous communities. We reviewed 15 articles discussing barriers and facilitators regarding recruitment for research studies in Indigenous communities. Some articles provided information or gave recommendations from work groups, the authors’ experience, or current strategies being implemented rather than providing information from research studies [14–18]. Research studies that addressed recruitment included the following barriers: 1) a lack of participant telephones; 2) participants having conflicting beliefs about health care or research; 3) mistrust in researchers, government, and academic institutions; 4) lack of confidentiality; 5) possible discrimination against one’s family, tribe, or racial group; and 6) fear of possible negative outcomes [2, 12, 14–19].
Research on recruitment has demonstrated that participant engagement was facilitated by the use of CBPR approaches, including early community engagement and collaboration, development of trust, and respect, and inclusion of community members [2, 11–13, 19–22]. Other facilitators include providing information to participants, researchers being flexible with their time, and racial/ethnic matching between research staff and participants [2, 22, 23]. Specifically, tribal college students endorsed having a study conducted by a tribal college or university or by a national organization, bringing money into the community, addressing health problems of concern to the community, having an Indigenous community member leading the study, maintaining anonymity, using information from the research to answer new questions, and providing programs to both intervention and control participants [11].
Various methods have been used to recruit Indigenous community members into studies. These include community activities, such as having booths at community health fairs, providing presentations to community groups, and utilizing community members for recruitment (including home visits) [13, 19, 21, 23, 24]. Other methods included mass mailings, local radio broadcasting and print media, use of diabetes registries and medical databases, and presentations to boards and health providers [13, 19, 21, 23, 24].
We reviewed 11 studies that discussed retention and adherence in Indigenous communities. Barriers to retention include: 1) researcher’s inability to contact participants, 2) distrust of the study, and 3) participants’ disability/disease [25–27]. Facilitators include: 1) community involvement, 2) trust between the researchers and the community, and 3) providing practical incentives [11, 13, 21, 28–31].
The purpose of this article is to describe planned versus actual recruitment, retention, and adherence strategies and the evaluation of retention and adherence strategies for a community-based research study of a Chronic Illness (CI) self-management intervention within an Indigenous community. The intervention was for Apsáalooke (Crow) tribal members who reside in Southeastern Montana. We present the context of our study, our planned versus actual strategies and evaluation, and provide recommendations for boosting recruitment for health intervention research within Indigenous communities using a CBPR approach.
Methods
Intervention approach
Báa nnilah (to give advice) is a CI self-management intervention developed by the CBPR partnership comprised of the Apsáalooke Nation non-profit organization Messengers for Health and faculty and students from Montana State University. Our partnership applies a CBPR approach in all stages of our work, from deciding on topic areas to dissemination, and uses a consensus process with community member input driving decision-making. We are led by our community advisory board (CAB), which is comprised of tribal members including elders, educators, and others invested in the health of the community. They decide on topic areas (e.g., that this intervention would focus on supporting community members with CIs) and make sure that all of our processes and products are consonant with the Apsáalooke culture. Báa nnilah consisted of seven biweekly gatherings led by 10 respected Apsáalooke tribal members who had a CI and served as mentors (Aaakbaabaaniilea, the ones who give advice). Aaakbaabaaniilea were individuals who role-modeled successful living with a CI and who were seen in their communities as strong leaders. Prior to implementing the intervention, we held monthly meetings with them and our CAB to develop the intervention approach and content and to provide training to Aaakbaabaaniilea in participant recruitment, group facilitation, intervention content, and other topics.
A conceptual model of CI self-management was co-developed by the CBPR partnership from 20 qualitative interviews with community members who had CIs [32]. The model supported intervention content, which included the following topics: understanding chronic illnesses, historical and current trauma loss and resilience, healthy food and physical activity, working with the healthcare system, and healthy communication and overcoming challenges. The interviews guided the approach, which included learning through advice given by others along with personal and collective stories, and mutual support between participants and Aaakbaabaaniilea. Foundational to the intervention were Apsáalooke spirituality and the Apsáalooke language. Detailed information about Báa nnilah intervention development, content, and approach has been published [32–34]. Institutional Review Board (IRB) approval was obtained from Montana State University. There is not a registered IRB through the U.S. Office for Human Research Protections on the Apsáalooke Reservation at the time of this study.
Study design
To evaluate the results of the Báa nnilah intervention on its participants, we used a cluster randomized trial (CRT) design with the intervention group participating from January 2018 to May 2018 and the waitlist control group participating from June 2018 to October 2018. Qualitative interviews with intervention participants also provided evaluation information. Eligibility requirements included living on or near the Apsáalooke reservation, being Indigenous, living with a CI, and being 25 years or older. Groups of family members and individuals participating in the trial were randomly assigned to participate in the intervention or waitlist control groups. Each of the 10 Aaakbaabaaniilea led 1 intervention group and 1 waitlist control group, to equal 20 total groups. Data were collected from participants prior to and directly after intervention participation, and approximately 6 and 12 months after participation. Quantitative survey measures and brief physical activity tests were completed at data collection meetings in the community.
Planned recruitment methods
Recruitment methods were determined by the CAB and Apsáalooke intervention staff. The primary recruitment method utilized Apsáalooke close kinship relationships by having Aaakbaabaaniilea recruit from their family and clan. Aaakbaabaaniilea were provided intervention brochures and were encouraged to share information about the intervention including incentives (meals, gas cards, and health-related gifts) to aid in recruiting. Aaakbaabaaniilea were asked to recruit 20 eligible community members and obtain informed consent as they recruited. They recruited using casual conversations when seeing family and clan members in homes, in the community, and at social events.
A secondary recruitment strategy occurred in the community through community meetings and at information tables at community events. Intervention staff and Aaakbaabaaniilea provided information and invited community members to join the intervention during these events. Aaakbaabaaniilea were encouraged to invite potential participants.
Planned retention and adherence methods
We defined retention by how many participants completed the follow-up data collections and adherence was defined by attendance at intervention gatherings. Strategies were selected from literature, past intervention experience, and community staff and CAB knowledge of strengths and support needed to achieve high retention and adherence rates. To encourage retention and adherence, we implemented multiple approaches including: 1) email/phone/text reminders, 2) offering healthy drinks and meals at intervention gatherings, 3) providing gas and gift cards at each data collection and intervention gathering, and 4) offering health-related incentives at intervention gatherings.
One primary method of encouraging retention and adherence was to draw on the close-knit nature of the Apsáalooke. Aaakbaabaaniilea had existing relationships with intervention participants and encouraged them to develop close relationships with each other. The purpose of this strategy was to allow participants to feel loved and supported, create an intimate and safe interventional setting, and create a space for participants to be comfortable sharing and encouraging each other.
An additional strategy to encourage retention and adherence was to match participants into supportive partnerships so they could help facilitate accountability of each other, attend gatherings together, and to stay engaged outside of the gatherings. A final strategy was to have Aaakbaabaaniilea track attendance to be aware of which participants needed additional support to attend intervention gatherings. Support included contacting participants to remind them of the gatherings, transporting them to and from gatherings and data collection meetings, and following up with those who missed gatherings.
Informal one-on-one public contact between community partners and participants allowed for conversation and discussion about the intervention and to casually remind participants of upcoming meetings. Additionally, at preintervention data collection meetings, participants shared attendance obstacles they may encounter during the intervention and past solutions to overcoming these barriers. This allowed participants to voice concerns and create action plans with fellow participants to achieve higher adherence rates.
To understand attendance facilitators and barriers, upon completion of the intervention we administered a survey asking participants to rate the level of impact of 14 facilitators and 13 barriers. The scale ranged from 1 = very much impactful to 5 = not at all impactful. Qualitative data was gathered by asking participants to share additional facilitators or barriers. To understand intervention adherence, we analyzed intervention gathering attendance records.
Results
Participant Characteristics
There were 211 participants with a mean age of 52.1 years (SD = 13.5; range of 24 to 82 years); 72% were females (n = 152). The most commonly reported CIs were diabetes (57%), high blood pressure (55%), and chronic pain (35%). Most (70%) participants reported multiple CIs.
Actual recruitment methods.
Recruitment methods varied from what was planned for several reasons. Some of the recruited participants were not able to attend data collection meetings. New participants joined in multiple ways including those who: 1) saw us collecting data in the community and joined after learning about the intervention, 2) were recruited by participants who attended earlier data collection meetings or while at a data collection meeting, 3) were recruited by mentors during a concurrent event in the same facility as a data collection meeting, and 4) were recruited by mentors who needed additional participants to reach 20 participants.
We planned for Aaakbaabaaniilea to receive informed consent from participants as part of the recruitment process. However, the vast majority of participants were not consented prior to the data collection meetings. This was due to the Aaakbaabaaniilea’s focus on recruiting participants, which left most of the technical consent work to the rest of the team at the data collection meeting. It worked well to complete the informed consent at the collection meetings since Aaakbaabaaniilea understood that the availability of their participants was limited due to busy personal schedules. In the end, we recruited our desired number of participants. However, the actual recruitment varied from our planned recruitment as shared above.
Actual intervention adherence and participant retention.
Regarding intervention adherence, of the 153 who completed the intervention, 135 participants had complete attendance data, 6 had partially recorded data, and 12 had missing attendance data. Table 1 shows the number and percentage of the 135 participants with complete records by number of gatherings attended. Nearly half attended all 7 intervention gatherings; the mean number of gatherings attended was 6 (SD = 1.50). An unplanned adherence strategy that occurred was that Aaakbaabaaniilea shared adherence strategies with each other in order to increase participation in gatherings.
Table 1:
Number and Percent of Participant Attendance at Program Gatherings (n = 135)
| Number of gatherings attended | Number and percent of participants |
|---|---|
|
| |
| 0 | n = 3 (2.2%) |
| 1–4 | n= 26 (19.3%) |
| 5–6 | n= 39 (28.9%) |
| 7 | n = 67 (49.6%) |
Data from the 145 participants (response rate = 92.9%) who completed the Barriers and Facilitators survey showed that the top three barriers to attending intervention gatherings were: 1) a death in the family, 2) personal or family crisis, 3) and weather (see Figure 1). The top three facilitators for attending gatherings were: 1) gas cards received at each gathering, 2) information learned at the gathering, and 3) relationship between the participant and their mentor (see Figure 2).
Figure 1:
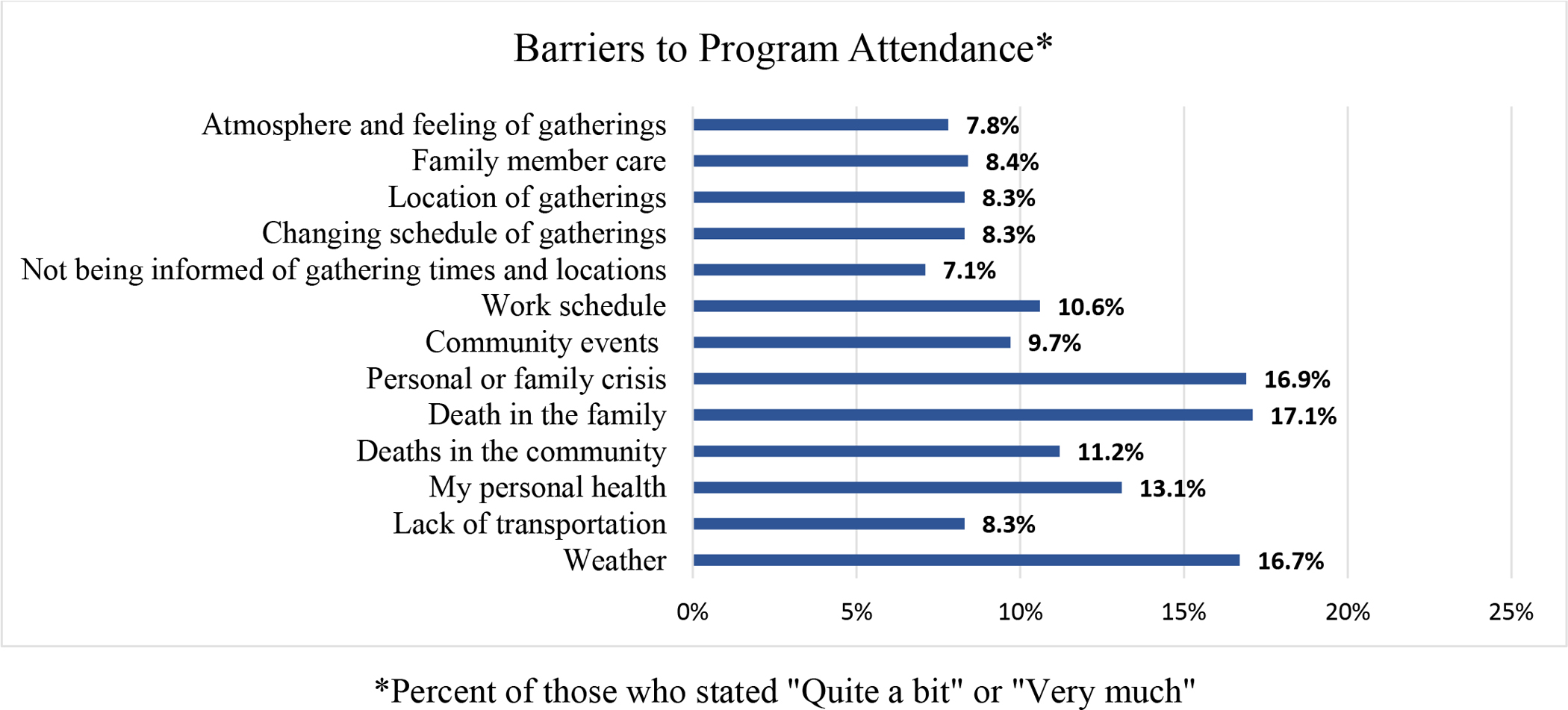
Barriers to Program Attendance
Figure 2:

Facilitators to Program Attendance
Regarding study retention, 146 of the 211 participants completed follow-up data collections, representing a loss of 64 participants. The top three reasons for study attrition were: 1) lack of attendance at intervention gatherings, 2) condition, work and family obligations, incarceration, and death having moved away from the community, and 3) the research team being unable to contact participants (see Figure 3). Other reasons included a worsened health condition, work and family obligations, incarceration, and death.
Figure 3:
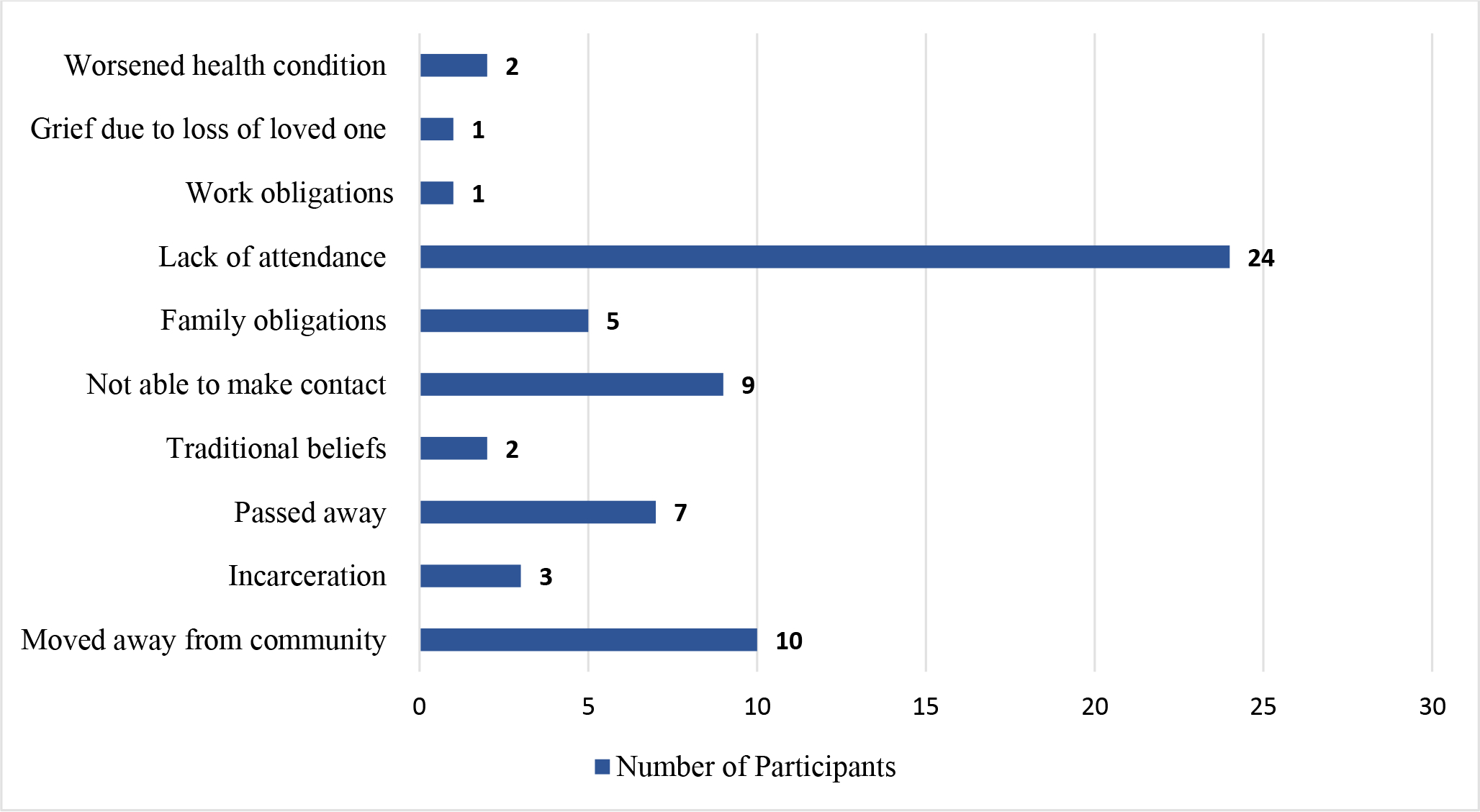
Reasons for Study Attrition
Discussion and Implications
The Báa nnilah intervention used a CBPR approach to implement recruitment, retention, and adherence strategies to facilitate the participation of Apsáalooke community members in our intervention research project. We found that planned versus actual recruitment and retention strategies varied in a number of ways and that certain retention and adherence strategies were more effective than others. Additionally, culturally consonant retention and adherence efforts resulted in the majority of participants attending all intervention gatherings and data collection meetings.
Our findings are similar to what others have found when working in Indigenous communities such that being integrated into the community, being visible in the community, and having community members on the team are important participation facilitators [12, 13, 19, 20, 22]. We agree with Minkler [35], who suggested that by “increasing community trust and ownership, CBPR can improve recruitment and retention efforts” (p.ii7), and the NHLBI [15] panel recommendation that by attending to the needs of participants, caring and trusting relationships can be encouraged. Apsáalooke team members share that the history of past harmful research and imposition by outside forces/agencies in their community impacts community member interest in being involved in research. The partnerships’ 20+ years of trust building and positive research outcomes positively impacted recruitment, retention and adherence in this study. As one community member shared, “if Alma (the Executive Director of the Apsáalooke non-profit partner) is involved, I’m in.”
Specific to recruitment, our findings mirror those of other studies [11, 19, 22] and a review [18] that having Indigenous community members and team members take the lead, using respectful interactions, and having methods determined by a CAB and Indigenous community members of the research team facilitated recruitment. Community members were never coerced into joining the project or pressured to join quickly. It was important for potential participants to feel comfortable and to have autonomy to join or not join the intervention. It was the positive and trusting relationship between Aaakbaabaaniilea and community members that made our recruitment efforts successful. One of the participants expressed what we were trying to convey by sharing, “it’s research, but it doesn’t feel like research.”
Another similarity between our study and another with Indigenous community participants [19] is that participants shared positive comments about the study with other community members, leading to an increased interest in others to join. A final similarity with another study in an Indigenous community [12] is that allowing husbands and wives to be recruited and randomized together increased enrollment, specifically for men.
We found that incentives (such as pedometers, intervention t-shirts, and a book on living with and managing chronic illnesses) suggested by Apsáalooke team members helped to reduce dropout rates, similar to findings from other studies [29, 30]. Team members believed that our use of CBPR approaches, including using participants’ ideas, partnering with local community health clinics, building trusting relationships with participants, and reminding participants of the study impacted intervention adherence and study retention, a finding corroborated by other Indigenous studies [15, 36]. Finally, similar to Redwood and colleagues [31], we found that phone reminders to participants and community networking were the most effective ways to increase adherence and retention.
One finding from our research that we did not see in other publications was that as word of Báa nnilah spread, some community members came to data collection meetings intent on joining the intervention without having had a conversation with a mentor or staff member. This was a challenging and uncomfortable interaction for both staff and potential participants due to Apsáalooke values of openness, inclusiveness, and generosity. Community members were excited to join the intervention to better their health and project staff needed to navigate a difficult situation as only community members who were eligible could join. We welcomed individuals who came to data collection meetings who were not eligible, provided them with health information and a meal, and invited them to stay and visit. However, they could not join the intervention, and stating this directly to a community member is considered an offensive and embarrassing action in the Apsáalooke culture. This is an example of a Western research approach coming into conflict with Indigenous community values [37]. Our partnership has been effective because we understand and act on the importance of building and maintaining relationships in the community. We recommend that other researchers understand the broader implications of determining and acting on eligibility criteria, which is something we did not see discussed in publications. As we work to sustain the program in the community and no longer have the constraints associated with our research protocol, all interested community members will be welcome to participate.
Based on our study, we recommend CBPR approaches that partner community and university researchers in the development and implementation of recruitment, retention, and adherence strategies. Additionally, the inclusion of the community’s culture and language will strengthen relationships and increase participant satisfaction with the intervention. Also, we agree with the recommendations of other researchers working with Indigenous communities to be transparent, for project documents to be clear about the project’s goals, to use accessible language, and to strive for clarity in recruitment materials and consent forms [13, 17, 27].
Our study has a few limitations. First, regarding the Barriers and Facilitators survey, participants were asked to answer these questions in addition to outcome surveys, which may have resulted in survey fatigue. Second, the survey was produced ad hoc and tailored to address strategies employed in this study versus using an existing survey, which limits our ability to compare with other studies. Although our findings are similar to some other studies in Indigenous communities, we note that it is not acceptable to generalize our findings across all communities as there are over 500 federally recognized tribal nations in the U.S. with rich diversity in cultures.
Few studies have examined recruitment, retention, and adherence in health intervention studies in Indigenous communities. It is vital that Indigenous community members and university researchers partner to increase participation in culturally consonant health programming [38]. These activities are best led by Indigenous community members who know the most appropriate and effective manner to facilitate community well-being. We hope that our experiences and lessons learned with recruiting, retaining, and adhering community members in this community-based intervention research project will help to improve future health intervention research in Indigenous and other minority communities, which will lead to improved community health.
Acknowledgments
We are grateful to our Community Advisory Board and these funders: Improving Chronic Illness Management with the Apsáalooke Nation: The Báa nnilah Project, NIH, U01MD010619; Montana Healthcare Foundation; The Mountain West Clinical Translational Research Program, NIH U54GM104944; Montana INBRE, National Institute of General Medical Sciences, NIH, P20GM103474 U.S. Department of Education – TRIO McNair Program, P217A130148. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
References
- [1].Umaefulam V, Kleissen T, Barnabe C (2022). The representation of Indigenous peoples in chronic disease clinical trials in Australia, Canada, New Zealand, and the United States. Clin Trials, 19(1), 22–32. doi: 10.1177/17407745211069153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Yancey AK, Ortega AN, Kumanyika SK (2006). Effective recruitment and retention of minority research participants. Annu Rev Public Health, 27, 1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- [3].Blanton S, Morris DM, Prettyman MG, McCulloch K, Redmond S, Light KE, et al. (2006). Lessons learned in participant recruitment and retention: the EXCITE trial. Phys Ther, 86(11), 1520–33. doi: 10.2522/ptj.20060091. [DOI] [PubMed] [Google Scholar]
- [4].Hawley-Hague H, Horne M, Skelton D, Todd C (2016). Review of how we should define (and measure) adherence in studies examining older adults’ participation in exercise classes. BMJ open, 6(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Shadish WR, Cook TD, Campbell DT Experimental and quasi-experimental designs for generalized causal inference. Belmont, CA: Wadsworth Cengage Learning; 2002. [Google Scholar]
- [6].Xiao L, Lv N, Rosas LG, Karve S, Luna V, Jameiro E, et al. (2016). Use of a motivational interviewing-informed strategy in group orientations to improve retention and intervention attendance in a randomized controlled trial. Health Educ Res, 31(6), 729–37. doi: 10.1093/her/cyw048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Israel B, Schulz A, Parker E, and Becker A (1998). Review of community-based research: Assessing partnership approaches to improve public health. Annu Rev Public Health, 19, 173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- [8].Estreet A, Apata J, Kamangar F, Schutzman C, Buccheri J, O’Keefe A-M, et al. (2017). Improving participants’ retention in a smoking cessation intervention using a community-based participatory research approach. Int J Prev Med, 8. doi: 10.4103/ijpvm.IJPVM_303_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Tiwari T, Sharma T, Harper M, Zacher T, Roan R, George C, et al. (2015). Community based participatory research to reduce oral health disparities in American Indian children. J Fam Med, 2(3). [PMC free article] [PubMed] [Google Scholar]
- [10].Minkler M, Wallerstein N Community-based participatory research for health: From process to outcomes: John Wiley & Sons; 2011. [Google Scholar]
- [11].Noe TD, Manson SM, Croy C, McGough H, Henderson JA, Buchwald DS (2007). The influence of community-based participatory research principles on the likelihood of participation in health research in American Indian communities. Ethn Dis, 17(1 Suppl 1), S6–14. [PubMed] [Google Scholar]
- [12].Daley CM, James AS, Ulrey E, Joseph S, Talawyma A, Choi WS, et al. (2010). Using focus groups in community-based participatory research: Challenges and resolutions. Qual Health Res, 20(5), 697–706. doi: 10.1177/1049732310361468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Redwood D, Lanier A, Kemberling M, Klejka J, Sylvester I, Lundgren K (2010). Community-based participatory research in a large cohort study of chronic diseases among Alaska native adults. Prog Community Health Partnersh, 4(4), 325–30. doi: 10.1353/cpr.2010.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Blue Bird Jernigan V, D’Amico EJ, Duran B, Buchwald D (2020). Multilevel and community-level interventions with Native Americans: Challenges and opportunities. Prev Sci, 21(1), 65–73. doi: 10.1007/s11121-018-0916-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].NIH. Multi-level intervention research methods: Recommendations for targeting hard-to-reach, high-risk or vulnerable populations and communities [Internet]. National Heart, Lung, and Blood Institue. 2015. [cited 2022 April 26]. Available from: https://www.nhlbi.nih.gov/events/2015/multilevel-intervention-research-methods-recommendations-targeting-hard-reach-high. [Google Scholar]
- [16].Claw KG, Anderson MZ, Begay RL, Tsosie KS, Fox K, Nanibaa’A G (2018). A framework for enhancing ethical genomic research with Indigenous communities. Nat Commun, 9(1), 1–7. doi: 10.1038/s41467-018-05188-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Trimble JE (2020). “Being grounded in the ancestors and looking forward...”—Blending culturally competent research with Indigenous leadership styles1. Prev Sci, 21(1), 98–104. [DOI] [PubMed] [Google Scholar]
- [18].Woodbury RB, Ketchum S, Hiratsuka VY, Spicer P (2019). Health-related participatory research in American Indian and Alaska native communities: a scoping review. Int J Envrion Res Public Health, 16(16), 2969. doi: 10.3390/ijerph16162969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Stoddart ML, Jarvis B, Blake B, Fabsitz RR, Howard BV, Lee ET, & Welty TK (2000). Recruitment of American Indians in epidemiologic research: the Strong Heart Study. Am Indian Alsk Native Ment Health Res, 9(3), 20–37. doi: 10.5820/aian.0903.2000.20. [DOI] [PubMed] [Google Scholar]
- [20].Greiner KA, Friedman DB, Adams SA, Gwede CK, Cupertino P, Engelman KK, et al. (2014). Effective recruitment strategies and community-based participatory research: community networks program centers’ recruitment in cancer prevention studies. Cancer Epidemiol Biomarkers Prev, 23(3), 416–23. doi: 10.1158/1055-9965.EPI-13-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Beans JA, Hiratsuka VY, Shane AL, Day GE, Redwood DG, Flanagan CA, et al. (2019). Follow-up study methods for a longitudinal cohort of Alaska Native and American Indian people living within urban south central Alaska: the EARTH study. J Community Health, 44(5), 903–11. doi: 10.1007/s10900-019-00630-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Geana MV, Greiner KA, Cully A, Talawyma M, Daley CM (2012). Improving health promotion to American Indians in the Midwest United States: Preferred sources of health information and its use for the medical encounter. J Community Health, 37(6), 1253–63. doi: 10.1007/s10900-012-9564-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hodge C, Hodge F, Palacios J (2015). Tribal-Based Participatory Research: The Wellness Circles Project. Health promotion in multicultural populations: A handbook for practitioners and students; Huff RM, Kline MV, Peterson DV, Eds. [Google Scholar]
- [24].Pratte KA, Beals J, Johnson A, Bullock A, Manson SM, Jiang L, et al. (2019). Recruitment and effectiveness by cohort in a case management intervention among American Indians and Alaska Natives with diabetes. Transl Behav Med, 9(4), 749–58. doi: 10.1093/tbm/iby068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Jiang L, Manson SM, Dill EJ, Beals J, Johnson A, Huang H, et al. (2015). Participant and site characteristics related to participant retention in a diabetes prevention translational project. Prev Sci, 16(1), 41–52. doi: 10.1007/s11121-013-0451-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Moore K, Jiang L, Manson SM, Beals J, Henderson W, Pratte K, et al. (2014). Case management to reduce cardiovascular disease risk in American Indians and Alaska Natives with diabetes: results from the Special Diabetes Program for Indians Healthy Heart Demonstration Project. Am J Public Health, 104(11), 158–64. doi: 10.2105/AJPH.2014.302108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ratner NL, Davis EB, Lhotka LL, Wille SM, Walls ML (2017). Patient-centered care, diabetes empowerment, and type 2 diabetes medication adherence among American Indian patients. Clin Diabetes, 35(5), 281–5. doi: 10.2337/cd17-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Brockie T, Azar K, Wallen G, Solis MOH, Adams K, Kub J (2019). A conceptual model for establishing collaborative partnerships between universities and Native American communities. Nurse Res, 27(1). doi: 10.7748/nr.2019.e1613. [DOI] [PubMed] [Google Scholar]
- [29].Dickerson DL, Venner KL, Duran B (2014). Clinical trials and American Indians/Alaska Natives with substance use disorders: identifying potential strategies for a new cultural-based intervention. J Public Ment Health. doi: 10.1108/JPMH-01-2014-0003. [DOI] [Google Scholar]
- [30].Jiang L, Yang J, Huang H, Johnson A, Dill EJ, Beals J, et al. (2016). Derivation and evaluation of a risk-scoring tool to predict participant attrition in a lifestyle intervention project. Prev Sci, 17(4), 461–71. doi: 10.1007/s11121-015-0628-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Redwood D, Leston J, Asay E, Ferucci E, Etzel R, Lanier AP (2011). Strategies for successful retention of Alaska Native and American Indian study participants. J Prim Prev, 32(1), 43–52. doi: 10.1007/s10935-010-0209-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Hallett J, Held S, McCormick AKHG., et al. (2017). What touched your heart? Collaborative story analysis emerging from an Apsáalooke cultural context. Qual Health Res. 27(9):1267–1277. doi: 10.1177/1049732316669340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Held S, Hallett J, Schure M, et al. (2019). Improving chronic illness self-management with the Apsáalooke Nation: Development of the Báa nnilah program. Soc Sci Med. 242:112583. doi: 10.1016/j.socscimed.2019.112583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Schure M, Allen S, Trottier C, McCormick A, Castille D, Held S (2020). Daasachchuchik: A trauma-informed approach to developing a chronic illness self-management program for the Apsáalooke people. JHCPU. 31(2):992–1006. doi: 10.1353/hpu.2020.0073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Minkler M (2005). Community-based research partnerships: challenges and opportunities. J Urban Health, 82(2), ii3–ii12. doi: 10.1093/jurban/jti034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Flores G, Portillo A, Lin H, Walker C, Fierro M, Henry M, et al. (2017). A successful approach to minimizing attrition in racial/ethnic minority, low-income populations. Contemp Clin Trials Commun, 5, 168–74. doi: 10.1016/j.conctc.2017.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Wilson S Research is ceremony: Indigenous research methods. 2008.
- [38].Ziabakhsh S, Pederson A, Prodan-Bhalla N, Middagh D, Jinkerson-Brass S (2016). Women-centered and culturally responsive heart health promotion among Indigenous women in Canada. Health Promot Pract, 17(6), 814–26. doi: 10.1177/1524839916633238. [DOI] [PubMed] [Google Scholar]


