Abstract
The aim of this systematic review was to examine the associations between physical activity and sleep in children aged less than 6 years. Articles were included if participants were primarily aged less than 6 years and study designs were observational or experimental. Study characteristics were extracted, and the Grading Recommendations Assessment, Development and Evaluation framework was used to assess study quality. Thirty-six studies (16 sleep, 16 physical activity, and three fitness outcomes) from 18 countries reported in 29 articles were included. The majority of sleep and physical activity outcome studies reported mixed effects with very low to low quality of evidence. Fitness outcome studies were limited, and therefore, evidence was insufficient. The high prevalence of mixed and null results could be related to study limitations. Importantly, this review points to the critical need for higher quality studies of sleep and physical activity in young children, which would support health recommendations and intervention strategies for healthier child development.
Keywords: fitness, infant, movement, overnight, preschool, toddler
Physical activity (i.e., any bodily movement that results in energy expenditure during wake periods) and sleep are important behaviors that contribute significantly to childhood health. Achieving sufficient physical activity and sleep in childhood can positively impact health outcomes, such as improved mental and physical health, attention and behavior, and overall quality of life, as well as reduce the likelihood of developing adverse health outcomes, such as depression, diabetes, and obesity (2018 Physical Activity Guidelines Advisory Committee, 2018; Chaput et al., 2017; Paruthi et al., 2016). Furthermore, early childhood is an important life phase to develop good physical activity and sleep habits given that these behaviors track into later childhood (Jones et al., 2013; Wang et al., 2016). Accordingly, U.S. health organizations have developed age-specific guidelines for these behaviors. The 2018 Physical Activity Guidelines for Americans recommend that preschoolers be physically active throughout the day (Piercy et al., 2018). The American Academy of Sleep Medicine recommends that within a 24-hr period, infants sleep 12–16 hr each day (including naps), toddlers sleep 11–14 hr each day, and preschoolers sleep 10–13 hr (Paruthi et al., 2016).
Our current level of understanding of the relationships between physical activity and sleep comes primarily from reviews reporting on adult studies (Chennaoui et al., 2015; Dolezal et al., 2017; Kredlow et al., 2015; Rubio-Arias et al., 2017). In the 2018 Physical Activity Guidelines for Americans Advisory Report (2018 Physical Activity Guidelines Advisory Committee, 2018), committee members concluded that among adults, there is strong evidence that both acute and chronic physical activity can improve sleep outcomes. The advisory report also found moderate evidence that, independent of exercise intensity, longer durations of single bouts of physical activity or participating in regular physical activity can both improve some measures of sleep health. Adult studies have also suggested that in addition to the level of habitual physical activity, fitness (i.e., the ability to perform physical activity) is positively associated with sleep outcomes (Chennaoui et al., 2015). Due to the lack of review papers about the relationships between physical activity and sleep in youth populations available at the time, an evidence rating was not assigned for children and adolescents in the advisory report. Among the limited review papers that have examined relationships between physical activity and sleep in youth, results have been mixed (Antczak et al., 2020; Chaput et al., 2017; Janssen et al., 2020) and primarily derived from studies in preadolescent children and adolescents (Bartel et al., 2015; Lang et al., 2016).
Given the emerging evidence of the interactive relationships of physical activity and sleep, other nations and the World Health Organization have developed 24-hr movement guidelines that provide recommendations for daily sleep, sedentary behavior, and physical activity (Government of Australia, 2018; Okely et al., 2017; Tremblay et al., 2017; Willumsen & Bull, 2020). Understanding how these health behaviors affect one another in childhood may provide insight into the optimal composition of 24-hr movement patterns (Rosenberger et al., 2019). However, among the few systematic reports that have included younger children, review papers have primarily focused on only one direction of the potential relations between physical activity and sleep (e.g., inclusion of studies with physical activity as the exposure and sleep as the outcome and not also studies with sleep as the exposure and physical activity as the outcome), examined only one sleep variable (e.g., sleep duration), included only older years of early childhood (i.e., 3–5 years), or have not examined the association between fitness and sleep (Antczak et al., 2020; Chaput et al., 2017; Janssen et al., 2020; Krietsch et al., 2019; Kuzik et al., 2017). Therefore, there is not yet a consensus of the influence of sleep on physical activity outcomes or physical activity on sleep outcomes in early childhood. The purpose of this systematic review was to examine the relationships between physical activity (including fitness) and sleep in children 5 years and younger. In addition to exploring the potential bidirectional nature of these relationships (i.e., physical activity influencing sleep and sleep influencing physical activity), studies were examined by method of sleep and physical activity assessment (i.e., subjective and objective measures).
Methods
Protocol and Registration
This systematic review was registered with the International Prospective Register of Systematic Reviews (registration number: CRD42020141743). The protocol followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (Moher et al., 2015).
Eligibility Criteria
Articles were included in this review if they were published in a peer-reviewed journal, they were written in English, and the protocol followed an observational (i.e., cross-sectional, cohort, and case control) or experimental (i.e., acute bout or intervention) study design. Articles that described case studies or case series reports were not included. Additional eligibility criteria were established a priori using Population, Intervention, Comparator, and Outcome study criteria (Schardt et al., 2007).
Population
Articles that reported on nonclinical, youth participants (i.e., samples primarily aged less than 6 years) were included. Articles were excluded if samples consisted of only participants aged 6 years and older or the study was conducted primarily in a clinical population (e.g., diagnosed sleep or cardiometabolic disorders).
Intervention (Exposure) and Outcomes
Articles that examined the interaction of sleep measures (e.g., total sleep duration, overnight sleep duration, nap sleep duration or frequency, sleep efficiency, time in bed, sleep onset latency, wake after sleep onset, daytime sleepiness, sleep disorder symptoms, and sleep architecture components) and physical activity measures (e.g., time or percentage of time spent in physical activity or fitness levels) were included. For observational studies, articles were included if (a) sleep was defined as the exposure (and physical activity or fitness was an outcome) or (b) physical activity or fitness were defined as the exposure (and sleep was an outcome). For experimental studies, articles were included if the authors (a) examined the effects of acute sleep bouts (e.g., shortened or extended sleep, nap or wake promotion) or sleep interventions on physical activity outcomes or (b) examined the effects of acute physical activity bouts (e.g., single exercise session) or physical activity interventions on sleep outcomes.
Comparator
For observational studies, the comparator was defined as the nonexposed group (e.g., less physically active vs. more physically active or short sleep duration vs. long sleep duration). For the experimental studies, the control groups were defined as standard care groups or alternative condition/intervention groups.
Information Sources and Search Strategy
A systematic literature search was conducted using Boolean strategies with a predefined list of keywords in PubMed, PsycINFO, and Web of Science and by manual review of reference lists of eligible studies and review articles. Given that the registered protocol included preadolescent and adolescent participants in the inclusion criteria, the initial searches included youth of all ages and then were reduced to include the present age criteria. Original searches were filtered to include publication dates between 1980 and 2019 on July 15, 2019. Additional searches were conducted on July 28, 2020 to capture articles published in the previous year. All articles retrieved from the database and reference list searches were imported into the Rayyan systematic review web-based application (Ouzzani et al., 2016). Two authors (C.W. St. Laurent and K. Rodheim) independently searched and screened the titles and abstracts of eligible articles to determine inclusion/exclusion status and identify duplicates. If needed, full-text articles were retrieved to determine eligibility. At each stage, the two authors discussed conflicts (i.e., lack of agreement for article inclusion) identified in the search and screening process. If necessary, the third author (R.M.C. Spencer) was consulted for a final inclusion decision.
Data Extraction
Study characteristics were extracted from full-text articles that met inclusion criteria following the Population, Intervention, Comparator, and Outcomes framework by one author (C.W. St. Laurent) and reviewed and cross-referenced for accuracy by a second author (K. Rodheim) in a prepiloted Excel document. Extracted information for observational studies included participants (i.e., age, sex, setting, and location); exposure(s) (i.e., variable, measurement method, measurement timing); outcome(s) (i.e., variable, measurement method, measurement timing); study design; covariates; analysis method; and results. Study designs were categorized as cross-sectional, longitudinal, acute experimental, and chronic experimental. In some cross-sectional studies, authors did not explicitly identify which variable was the exposure (or independent variable) and which variable was the outcome (i.e., when correlations were used in the analysis). In such cases, the authors of this review used their discretion to categorize studies into physical activity or sleep outcomes.
Experimental studies were categorized as acute studies if they looked at effects of single bouts of physical activity (on sleep outcomes) or temporary (i.e., 1 day to 2 weeks) change in normal sleep habits (on physical activity or fitness outcomes). Experimental studies were categorized as chronic if effects were examined after repeated exposure to the intervention. Extracted information for experimental studies included participants (i.e., age, sex, setting, and location); intervention(s) (i.e., description, delivery method, dosage/length, timing, implementation measures); outcome(s) (i.e., variable, measurement method, measurement timing); study design; covariates; analysis method; and results. Results were classified into one of four results categories (i.e., null, positive, mixed, or negative). Effects were designated as null if there was no statistical significance in the examined association or effect. Effects were classified as positive if the association or effect was statistically significant in the predicted direction (i.e., according to the authors’ hypothesis or hypotheses) and negative if the association or effect was statistically significant in the opposite direction than predicted. In cases where hypotheses were not explicitly stated, the reviewers assumed the anticipated direction (i.e., the association that would be deemed beneficial for both sleep and physical activity unless otherwise described). If more than one association or effect was examined but not all of the results were statistically significant, the results were indicated as mixed.
Study Quality Assessment
For studies that met the inclusion criteria, two authors (C.W. St. Laurent and K. Rodheim) independently followed the Grading Recommendations Assessment, Development and Evaluation Working Group’s framework to assess the quality of the evidence (Schünemann et al., 2019). Within the Grading Recommendations Assessment, Development and Evaluation framework, each outcome of a study is assigned a category of study quality (i.e., high, moderate, low, or very low). Experimental studies are initially categorized as high and observational studies are initially categorized as low. Studies can then be downgraded by one or more levels of quality based on a number of study factors, including limitations of study design, risk of bias (i.e., concerns related to the study execution, such as lack of concealment and blinding, quality of measurement, and description of eligibility criteria), inconsistency (i.e., heterogeneity in results), indirectness (i.e., concern with confidence in the effect due to differences in population, intervention, outcome measures, or indirect comparisons), and imprecision (i.e., confidence in the estimates of effect). Any discrepancies in study quality ratings were discussed and resolved between the two authors with consultation of the third author if needed (R.M.C. Spencer).
Analysis
Included studies were summarized in table format, which included study details, results, and quality assessment ratings. Extracted data in summary tables were coded, and descriptive analyses were conducted in Stata (Release 16.0; StataCorp LLC, College Station, TX). As heterogeneity in study methodologies and outcomes measures was expected, conducting meta-analyses for each outcome was not planned. Studies were evaluated overall and then by method of physical activity and sleep assessment (i.e., subjective vs. objective methods).
Results
Description of All Studies
As shown in Figure 1, the initial database search resulted in 7,377 articles. References from review papers and included articles were also reviewed, and 56 additional articles were identified for screening. After duplicates were removed, 7,208 articles were screened (i.e., via title and abstract) and 7,007 did not meet the inclusion criteria mainly due to exposure and/or outcome, study design, or age (i.e., adult participants). Among the remaining 201 articles, full texts were screened for eligibility, and 35 were excluded. Although some studies may have met multiple exclusion reasons, they were assigned the first, most apparent reason. The final article list of youth samples was then reduced to meet the age criteria for this review (i.e., population aged less than 6 years), resulting in the additional exclusion of 137 articles. Overall, 29 articles reporting on 36 studies met the inclusion criteria. It should be noted that in the subsequent sections, studies may not always add up to the associated totals due to multiple articles meeting criteria for more than one category (e.g., multiple study designs presented in one article or multiple outcome measures.)
Figure 1 —
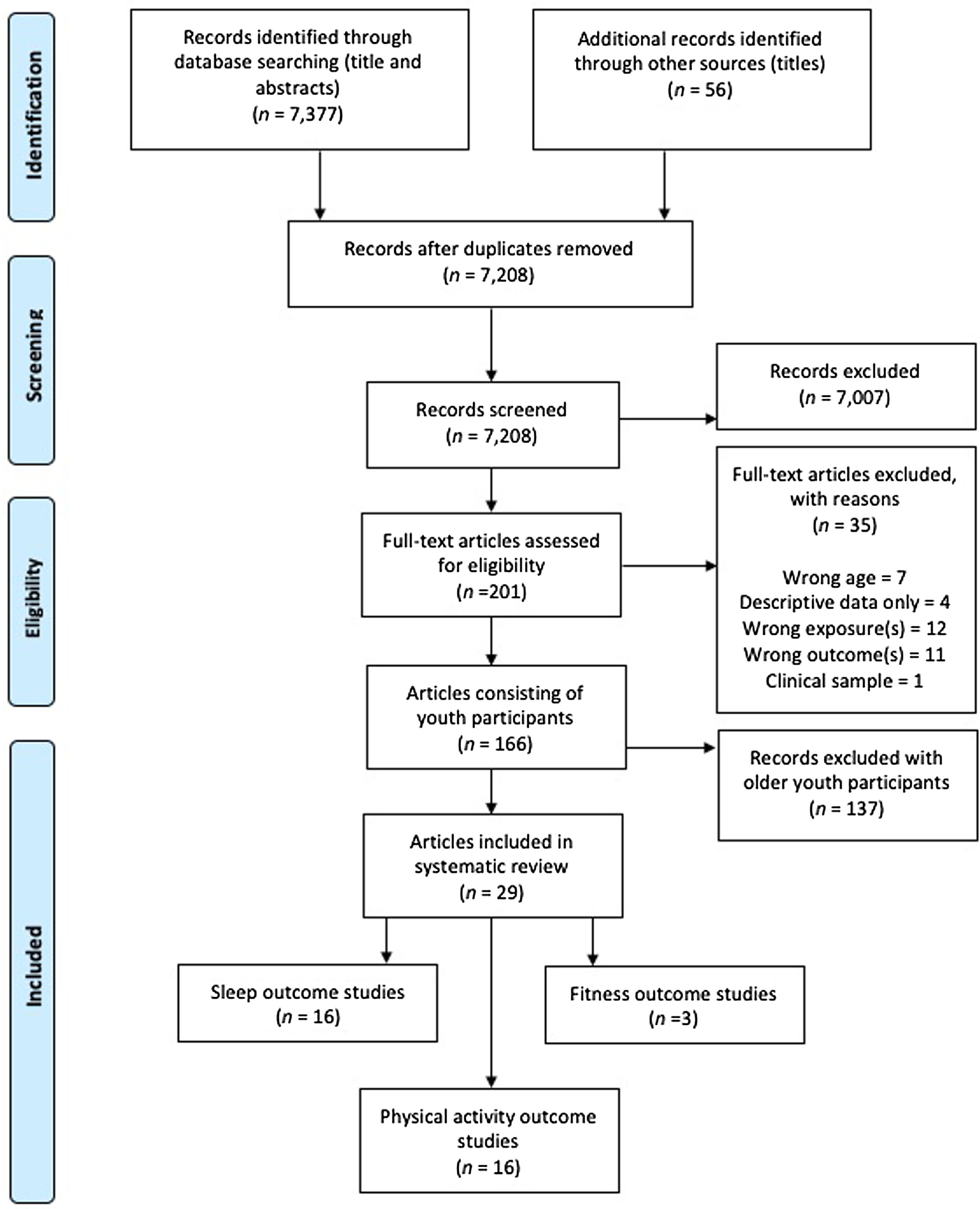
Flow diagram of the search screening and identification process for article inclusion.
Individual study characteristics are presented in Table 1. Studies were conducted in 18 different countries. Four articles included infants, eight included toddlers, and 20 included preschoolers. Study designs were categorized as cross-sectional (n = 17 studies) or chronic experimental (n = 30 studies). There were no studies that used longitudinal or acute experimental designs. Overall, 17 articles (53.1%) reported objective measures of sleep and/or physical activity.
Table 1.
Summary of Findings of Included Articles
| Reference | Study | Participants | Exposure | Outcome | Risk of bias | |
|---|---|---|---|---|---|---|
| First author (year) Country Parent study—if applicable | Design (type or follow-up—if applicable) | Sample size, age (range or mean/SD), % female | Variable(s) (measurement) timing (if applicable) | Variables(s) (measurement) timing (if applicable) | Potential risk(s) (see table note) | Main findings |
| Sleep outcomes: Observational | ||||||
| Chang et al. (2018) Canada Canadian Health Measures Survey | Cross-sectional | n = 4,924, 3–17 years, 47.7–48.9% | PA guidelines adherence (questionnaire) | Sleep duration (questionnaire) | E and M | Null: PA guideline adherence not associated with sleep duration |
| Duraccio and Jensen (2017) United States | Cross-sectional | n = 131, 4–6 years 43.5% | ST, meeting PA guidelines (accelerometry—3 days) | Sleep duration (accelerometry—3 days) | E and C | Mixed: No association between the number of days that children engaged in ≥ 60 min of PA and sufficient sleep and no association between the number of days that children engaged in ≥20 min of VPA and sufficient sleep Children who engaged in minimal ST had greater odds of obtaining sufficient sleep as compared with children who engaged in more ST |
| Eythorsdottir et al. (2020) Denmark Healthy Start Project | Cross-sectional | n = 54, 2–6 years, 35.2% | Total PA counts/min (accelerometry—5 days) | Night sleep latency, duration, and efficiency (accelerometry—5 days) | E | Mixed: Higher PA counts associated with longer sleep latency (β = 33.65, p = .04) No association between PA and sleep duration or efficiency |
| Felzer-Kim and Hauck (2020) United States | Cross-sectional | n = 50, 1–3 years, 42% | MVPA (accelerometry—3 days) | Sleep duration (parent report) | M | POS: MVPA positively association with sleep duration (β = 0.038, p = .019) |
| Iwata et al. (2011) Japan | Cross-sectional | n = 47, 5 years, 42.6% | Regular or no sports participation (questionnaire) | SOL, sleep end time, and sleep efficiency (accelerometry—7 days) | E and M | Mixed: On weekdays, sports lessons related to an earlier sleep end time (21 min, 95% CI [−0.641, −0.062]) and higher sleep efficiency (3.7%, 95% CI [0.093, 7.149]) On weekends, sports lessons associated with higher sleep efficiency (3.6%, 95% CI [0245, 6.921]) |
| Parsons et al. (2018) United States Preschool Eating and Activity Study | Cross-sectional | n = 369, 36–72 months, 51.5% | SB, LPA, MPA, VPA, time outdoors, and in gym (accelerometry—1 day, report) | Sleep duration (questionnaire—1-day diary) | E and M | Mixed: Inside PA time provided associated with increased nighttime sleep duration (β = 0.092 ± 0.04 hr per 30 min PA, p < .03) No association between outdoor time or MVPA and nighttime sleep |
| Wang et al. (2019) Taiwan | Cross-sectional | n = 183, 6 months, 54.6% female | Mean and total activity counts, floor time activity, and screen time or limited activity (accelerometry—7 days, questionnaire) | Total/night/day sleep duration and sleep efficiency (accelerometry—7 days) | N/A | Mixed: More hours of screen time or limited PA per day associated with a decrease in total daily 24-hr sleep duration (p< .01) All other associations were null |
| Williams et al. (2014) New Zealand Family Lifestyle, Activity, Movement, and Eating | Repeated cross-sectional | n = 234, 3, 5, 7 years, 42.7% | SB, LPA, and MVPA (accelerometry—5 days) | Sleep duration (accelerometry—5 days) | CC | Mixed: Time spent asleep related to SB and LPA, but not MVPA The most active (95th percentile) children spent 55–84 fewer minutes asleep and 16–19 more minutes awake at night compared with the least active (fifth percentile) children Children with later bedtimes were more sedentary (10–15 min) but also more light (18–23 min) activity during the day No differences in MVPA by bedtime schedule |
| Zhang et al. (2019) Australia GET UP! Study | Cross-sectional | n = 173, 19.7 (4.1) months, sex unknown | Total PA and MVPA (accelerometry—7 days) | Night sleep duration, variability, and problems (accelerometry—7 days, questionnaire) | E | Mixed: Less PA (OR = 2.38; 95% CI [1.27, 4.45]) associated with higher odds of having longer nocturnal sleep duration PA not associated with nocturnal sleep problems |
| Sleep outcomes: Experimental | ||||||
| De Bock et al. (2013) Germany | Chronic (RCT) | n = 809, 4–6 years, 48% | Home based: 6- to 9-month participatory school and home PA program with PE programs and parent resources | Sleep quality (questionnaire) Baseline, 6 months, and 12 months | C, B, and M | Null: No difference in sleep quality was found between study arms |
| Haines et al. (2018) Canada | Chronic (RCT) | n = 44, 1.5–5 years, 52.8% | Home based: ~6 months of family obesity prevention (health education on PA, sleep, and family meals): Four home visits vs. two home visits vs. general health advice via emails | Sleep quantity (accelerometry—3–7 days) Baseline and postintervention | C, A, and S | Null: No significant intervention effect for sleep |
| Lerner-Geva et al. (2015) Israel | Chronic (RCT) | n = 204, 4–6 years, 49% | School based: 10 weeks of nutrition lessons with daily exercise vs. daily exercise vs. regular curriculum | Night sleep duration (questionnaire) Baseline and “follow-up” | C, B, A, S, and M | Null: No effect of interventions on sleep duration |
| Puder et al. (2011) Switzerland | Chronic (RCT) | n = 652, 5.2 (0.6) years, 50% | School and home based: Culturally tailored lifestyle intervention (22 lessons on healthy nutrition, media use, and sleep; four 45 min PA sessions/week for school year) vs. regular curriculum | Sleep duration (questionnaire) Baseline and postintervention | C | Null: No significant effect of the intervention on sleep duration. |
| Taylor et al. (2015) New Zealand | Chronic (RCT) | n = 206, 4–8 years, 55.3% | Community based: Tailored lifestyle, healthy promotion intervention for parents (met with mentor each month) vs. usual care | Sleep duration (accelerometry—7 days) Baseline, 12 months, and 24 months | C, A, and S | Null: There was no intervention effect on sleep duration |
| Taylor et al. (2018) New Zealand | Chronic (RCT) | n = 345, 3.5 and 5 years, 51.2% | Community based: Four arms = food, activity, breastfeeding vs. sleep vs. combination vs. standard care (contacts/dosage varied by group) | Sleep-wake timing, sleep duration, and night awakenings (accelerometry—5 days) 3.5 and 5 years after birth | B, A, and S | Null: Sleep duration did not differ between groups. |
| Taylor et al. (2017) New Zealand | Chronic (RCT) | n = 686, pre-birth, 48.8% female | Community-based: Four arms = food, activity, breastfeeding vs. sleep vs. combination vs. standard care (contacts/dosage varied by group) | Sleep duration, night awakenings, and sleep problems (accelerometry—5–7 days, questionnaire) 12 and 24 months | B, A, and S | Null: No difference in sleep duration, frequency of waking at night, or prevalence of sleep problems between arms (all, p ≥ .187) |
| PA outcomes: Observational | ||||||
| Dolinsky et al. (2011) United States KAN-DO RCT Study | Cross-sectional | n = 337, 2–5 years, 42% | Insufficient sleep (questionnaire) | MPVA and ST (accelerometry—7 days) | E and M | Null: Sleeping too little not associated with time spent sedentary or MVPA |
| Hager et al. (2016) United States | Cross-sectional | n = 240, 12–32 months, 45% | Sleep duration and behaviors (questionnaire) | MVPA and activity counts (accelerometry—7 days) | M | POS: Low MVPA and activity counts/minutes associated with shorter sleep duration (MVPA: F = 3.7, p = .028; counts/min: F= 5.4, p = .005) and poor sleep behaviors (MVPA: r= .193, p= .012; counts/min: r = .212, p = .006) |
| Hauck et al. (2018) United States | Cross-sectional | n = 22, 6 months, 59% | Total sleep duration, nap duration, and nap frequency (accelerometry—24 hr) | LPA as proxy for sedentary movement (accelerometry—24 hr) | E | POS: Infants accumulating less total sleep spent more time in LPA (r = −.524, p = .012) |
| Hinkley et al. (2012) Australia Healthy Active Preschool Years Study | Cross-sectional | n = 705, 3–5 years, 45% | Daily sleep (questionnaire) | PA (accelerometry—8 days) | M | Mixed: Among males, daily sleep duration associated with PA (weekly PA OR = 1.04, 95% CI [1.02, 1.07]; weekday PA OR = 1.04, 95% CI [1.01, 1.06]) No association in females |
| Kohyama (2007) Japan | Cross-sectional | n = 204, 12–40 months, 49.5% | Sleep onset, sleep duration, waking time, and nap duration (accelerometry—6 days) | Daily PA (accelerometry—6 days) | E | Mixed: Early waking time positively correlated with PA (p = .008) No association with other measures |
| Raza et al. (2019) United Kingdom The Growing Up in Wales, Environments for Healthy Living | Cross-sectional | n = 141, 12 months, 45.4% | Daytime sleep duration, night sleep duration, number of night wakings, sleepless hours in night, and SOL (unclear—potentially medical records) | PA (accelerometry—7 days) | E and M | Null: Higher PA was associated with fewer night wakings (p < .05), but only in unadjusted model |
| Schmutz et al. (2017) Switzerland Swiss Preschoolers’ Health Study | Cross-sectional | n = 394, 2–6 years, 46% female | Sleep duration (questionnaire) | Total PA, MVPA, and SB (accelerometry) | E and M | Null: Sleep duration not significantly associated with PA and ST |
| Yu et al. (2011) Australia Longitudinal study Australian Children, Wave 1 | Cross-sectional | n = 2,758, 4–5 years, 48.6% | Overnight and nap sleep duration (questionnaire) | Walk for fun/travel, bicycle for fun/travel, and other time in exercise (questionnaire) | M | Null: No association between sleep hours and PA |
| Physical Activity Outcomes: Experimental | ||||||
| Alhassan et al. (2019) United States | Chronic (RCT) | n = 52, 2.9–6 years, 50% | School and home based: PA, diet, and sleep lesson plans on 4 days per week for 12 weeks and weekly parent education and recommended family activities vs. regular curriculum | Full day and preschool day ST, LPA, and MVPA (accelerometry—7 days) Baseline and 12 weeks |
C and B | POS: Compared with the control group, the intervention group had greater full day VPA (p = .004), greater full day MVPA (p = .02), greater preschool day MVPA (p = .009) and VPA (p< .001) and less preschool day ST (p = .03) |
| Händel et al. (2017) Denmark | Chronic (RCT) | n = 307, 2.4–5.7 years, 41–44% | Home and health office based: 4–5 family health consultations on diet, PA, sleep, and stress management over 15 months vs. usual care | Outdoor time and sport activity participation (questionnaire)Baseline and postintervention | C and B | Mixed: Intervention group spent more time in sports and outdoor activities combined per week than the control group (intervention = 400 min/week, 95% CI [341, 459] vs. control = 312 min/week, 95% CI [277, 366]) No intervention effects for subcategories |
| Haines et al. (2018) Canada | Chronic (RCT) | n = 44, 1.5–5 years, 52.8% | Home based: ~6 months of family obesity prevention (health education on PA, sleep, and family meals): Four home visits vs. two home visits vs. general health advice via emails | ST, LPA, and MVPA (accelerometry—3–7 days) Baseline and postintervention |
C and A | Null: No intervention effect for PA or sedentary behavior |
| Puder et al. (2011) Switzerland | Chronic (RCT) | n = 652, 5.2 (0.6) years, 50% | School and home based: Culturally tailored lifestyle intervention (22 lessons on healthy nutrition, media use, and sleep; four 45-min PA sessions/week for school year) vs. regular curriculum | PA (accelerometry = 5 + days and questionnaire) Baseline and postintervention |
C | Mixed: No effects of intervention on objective PA Beneficial effect of the intervention on reported PA (effect estimate = 1.7, p = .01) |
| Taylor et al. (2015) New Zealand | Chronic (RCT) | n = 206, 4–8 years, 55.3% | Community based: Tailored lifestyle, healthy promotion intervention for parents (met with mentor each month) vs. usual care | Counts/min, ST, and MVPA (accelerometry—7 days) Baseline, 12 months, and 24 months |
C, A, and S | Mixed: Intervention children were more physically active (for counts/min, p = .035) |
| Taylor et al. (2018) New Zealand | Chronic (RCT) | n = 345, 3.5, 5 years, 51.2% | Community based: 4 arms = food, activity, breastfeeding vs. sleep vs. combination vs. standard care (contacts/dosage varied by group) | PA (counts/min) and LPA to VPA (accelerometry—5 days) 3.5 and 5 years after birth | B, A, and S | Null: PA did not differ between groups |
| Taylor et al. (2017) New Zealand | Chronic (RCT) | n = 686, pre-birth, 48.8% | Community based: 4 arms = food, activity, breastfeeding vs. sleep vs. combination vs. standard care (contacts/dosage varied by group) | Time in active play outside (questionnaire) 12 and 24 months after birth | B, A, and S | POS: Children in the food, activity, and breastfeeding group and combination group spent more time active outside than the control group |
| Yoong et al. (2019) Australia | Chronic (RCT) | n = 76, parent/child dyads 3–6 years,42.1% | Home based: 3-month theory-informed parental sleep education intervention (online video, telephone call, and 2 text messages) vs. usual care | Total PA and MVPA (accelerometry—7 days) Baseline and 3 months |
C, B, A, and S | POS: Estimated effect size for the intervention relative to control was 10.8 min/day for MVPA and 2.7 min/day for PA |
| Fitness outcomes: Observational | ||||||
| None | ||||||
| Fitness outcomes: Experimental | ||||||
| Bürgi et al. (2012) Switzerland | Chronic (RCT) (effect modification by parent educational level and migrant status) | n = 652, 5.2 (0.6) years, 49–53% | School and home based: culturally tailored lifestyle intervention (22 lessons on healthy nutrition, media use, and sleep; four 45-min PA sessions/week for school year) vs. regular curriculum | CRF (20-m shuttle run) Baseline and postintervention | C | Mixed: Average intervention effect sizes for CRF were 0.55, 0.20, 0.37, and −0.05 stages for children of nonmigrant, migrant, middle/high educational level, and low educational level parents, respectively |
| Niederer et al. (2013) Switzerland | Chronic (RCT) (effect modification by weight and fitness status) | n = 649, 5.1–5.3 (0.6) years, 46.1–53.9% | School and home based: culturally tailored lifestyle intervention (22 lessons on healthy nutrition, media use, and sleep; four 45-min PA sessions/week for school year) vs. regular curriculum | CRF and motor agility C (20-m shuttle run, obstacle course) Baseline and postintervention |
C | Null: Intervention effects on both fitness outcomes were not modified by BMI or fitness group (all p’s for interaction ≥.2) |
| Puder et al. (2011) Switzerland | Chronic (RCT) | n = 642, 5.2 (0.6) years, 50% | School and home based: Culturally tailored lifestyle intervention (22 lessons on healthy nutrition, media use, and sleep; four 45-min PA sessions/week for school year) vs. regular curriculum | CRF, motor agility, and C dynamic and static balance (20-m shuttle run, obstacle course, balance beam steps, and platform) Baseline and postintervention |
C | POS: Compared with controls, children in the intervention group had an increase in CRF at the end of the intervention (adjusted mean difference: 0.32 stages, 95% CI [0.07, 0.57], p = .01) Relative to controls, children in the intervention group had beneficial effects in motor agility (−0.54 s, [−0.90, −0.17], p = .004) |
Note. Self-report or parent-report measures (e.g., recall, semistructured or structured survey) were labeled generally as a “questionnaire.” CI = confidence interval; CRF = cardiorespiratory fitness; LPA = light physical activity; MPA = moderate physical activity; MVPA = moderate to vigorous physical activity; OR = odds ratio; PA = physical activity; PE = physical education; BMI = body mass index; RCT = randomized controlled trial; SB = sedentary behavior; SOL = sleep onset latency; ST = sedentary time; VPA = vigorous physical activity. Risk of Bias Categories: E = eligibility (e.g., lack of information or application of eligibility criteria); M = measurement (e.g., potential for misclassification with the measures in exposure and/or outcome); CC = control for confounding (e.g., inadequately controlled for potential confounding); C = concealment (e.g., lack of randomization concealment); B = blinding (e.g., lack of blinding of research staff and/or participants to study arm or lack of information regarding blinding); A = accounting (e.g., incomplete accounting of participants and/or outcome events); S = selective outcome reporting (e.g., incomplete or absent reporting of some outcomes and not others); POS = positive (beneficial) association/effect.
Sleep Outcomes Data Synthesis
Overall, 16 studies reported on sleep outcomes (Table 2). Sleep outcome variables included sleep duration, bedtime, sleep onset latency time, wake after sleep onset, sleep efficiency, wake time, sleep variability, sleep problems, and overall sleep quality. Most studies reported on nighttime sleep or did not specify the measurement period, but Wang, Chen, Tung, Lee, and Tsai (2019) also reported both daytime and 24-hr sleep measures. Study designs with sleep outcomes included cross-sectional and chronic experimental. Although a study by Williams, Farmer, Taylor, and Taylor (2014) conducted measurements over time, it appeared that each time point consisted of different participant samples, so this study was categorized as cross-sectional rather than longitudinal.
Table 2.
Associations/Effects Between Physical Activity/Fitness and Sleep Outcomes in Early Childhood
| Quality assessment | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other | No. of participantsa | Overall effectb | Quality |
| 9 | Cross-sectional | Some risk of biasc | Some inconsistencyc | No serious indirectness | No serious imprecision | None | 6,155 | 1 null, 1 positive, and 7 mixedd | Very low |
| 0 | Longitudinal | N/A | N/A | N/A | N/A | None | N/A | N/A | Not assignable |
| 0 | Acute experimental | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Not assignable |
| 7 | Chronic experimental | Some risk of biase | No serious inconsistency | Serious indirectnesse | No serious imprecision | None | 2,946 | 7 nullf | Low |
Note. Sleep outcome measures included sleep duration, bedtime, sleep onset latency time, wake after sleep onset, sleep efficiency, wake time, sleep variability, sleep problems, and overall sleep quality. N/A = not applicable.
The number of participants may not represent unique participants.
Overall effect key: Null = no statistically significant association/effect; positive = statistically significant association/effect in hypothesized direction; mixed = at least one statistically significant association/effect if more than one association/effect examined; negative = statistically significant association/effect in opposite of hypothesized direction.
Downgraded one level from low to very low due to some risk of bias (i.e., lack of eligibility information in some studies and potential misclassification of measures) and some inconsistency (most associations were mixed).
Study effects were null (Chang et al., 2018), positive (Felzer-Kim & Hauck, 2020), and mixed (Duraccio & Jensen, 2017; Eythorsdottir et al., 2020; Iwata et al., 2011; Parsons et al., 2018; Wang et al., 2019; Williams et al., 2014; Zhang et al., 2019).
Downgraded two levels from high to low due to serious risk of bias (i.e., some studies lacked information regarding concealment and blinding and concerns for misclassification of the outcome due to self-report or parent report for sleep measures in some studies) and due to serious risk of indirectness (i.e., interventions varied considerably, and most had multicomponents so that the effects of physical activity on sleep could not be determined).
Study effects were all null (De Bock et al., 2013; Haines et al., 2018; Lerner-Geva et al., 2015; Puder et al., 2011; Taylor et al., 2015, 2017, 2018).
Overall, the cross-sectional studies (n = 9 studies and 6,155 participants) examined general associations between physical activity exposure measures and sleep outcomes. Physical activity measures included total daily activity (i.e., accelerometer counts/min), time spent sedentary or in light and moderate to vigorous physical activity, sports participation, meeting physical activity and/or screen time guidelines, outdoor physical activity, and floor time activity (i.e., for infants). No studies examined the associations between fitness measures and sleep outcomes. Most studies reported mixed associations (n = 7; Duraccio & Jensen, 2017; Eythorsdottir et al., 2020; Iwata et al., 2011; Parsons et al., 2018; Wang et al., 2019; Williams et al., 2014; Zhang et al., 2019). Among the mixed results, the majority reported combinations of beneficial and null associations (Duraccio & Jensen, 2017; Iwata et al., 2011; Parsons et al., 2018; Wang et al., 2019; Williams et al., 2014), but some reported combinations of null and nonbeneficial associations (i.e., greater physical activity was associated with longer sleep latency; Eythorsdottir et al., 2020; Zhang et al., 2019). One study reported no significant associations (i.e., no association between physical activity guideline compliance and sleep duration; Chang et al., 2018), and one reported a positive association between moderate to vigorous physical activity and sleep duration (Felzer-Kim & Hauck, 2020). The quality of evidence for cross-sectional studies with sleep outcomes was downgraded from “low” to “very low” due to some risk of bias and some inconsistency of overall effects across studies.
Seven studies (n = 2,946 participants) utilized a chronic experimental design and evaluated interventions in home- (De Bock et al., 2013; Haines et al., 2018), school- (Lerner-Geva et al., 2015), and community-based settings (Taylor et al., 2015, 2017, 2018) or a combination of these (Puder et al., 2011). Interventions consisted of physical activity promotion programs, structured exercise programs, physical education enhancement, and combined or multi-component programs (i.e., interventions targeting health behaviors such as sleep and nutrition in addition to physical activity, which may also have used more than one method or setting). All intervention studies observed null effects, indicating no beneficial effect of the physical activity or health interventions on sleep outcomes. Due to serious risk of bias in some studies and serious indirectness, the quality of evidence was downgraded from “high” to “low.”
Among the sleep outcome studies that used objective methods to assess sleep and physical activity, most were cross-sectional analyses. Five out of the nine cross-sectional studies used objective measures of both physical activity and sleep, and all reported mixed effects (Duraccio & Jensen, 2017; Parsons et al., 2018; Wang et al., 2019; Williams et al., 2014; Zhang et al., 2019). Approximately half of the chronic experimental studies described in the overall section (n = 4) utilized an objective measure of sleep for outcome variables (Puder et al., 2011; Taylor et al., 2015, 2017, 2018). Objective measures for all of these studies were assessed with accelerometry, with measurement protocols varying across studies (i.e., 1–7 days of measurement and with differing body placements, wear time criteria, devices, and processing protocols).
Physical Activity Outcomes Data Synthesis
Overall, 16 studies examined physical activity outcomes (Table 3). Physical activity-related outcomes included sedentary time, light physical activity, moderate to vigorous physical activity, total accelerometry-derived activity counts, active outdoor play, or other indices of physical activity (e.g., meeting physical activity guidelines, outdoor time, participating in walking or biking, or extracurricular physical activity or sports participation). Similar to the sleep outcomes studies, designs included cross-sectional and chronic experimental.
Table 3.
Associations/Effects Between Sleep and Physical Activity Outcomes in Early Childhood
| Quality assessment | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other | No. of participantsa | Overall effectb | Quality |
| 8 | Cross-sectional | Serious risk of biasc | Serious inconsistencyc | No serious indirectness | No serious imprecision | None | 4,801 | 4 null, 2 positive, and 2 mixedd | Very low |
| 0 | Longitudinal | N/A | N/A | NA | N/A | N/A | N/A | N/A | Not assignable |
| 0 | Acute experimental | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Not assignable |
| 8 | Chronic experimental | Serious risk of biase | No serious inconsistency | Serious indirectnesse | No serious imprecision | None | 2,368 | 2 null, 3 positive, and 3 mixedf | Low |
Note. PA outcome measures included sedentary time, LPA, MVPA, total accelerometry-derived activity counts, active outdoor play, or other indices of PA (e.g., meeting PA guidelines, outdoor time, participating in walking or biking, or extracurricular PA or sports participation). LPA = light physical activity; MVPA = moderate to vigorous physical activity; PA = physical activity; N/A = not applicable.
The number of participants may not represent unique participants.
Overall effect key: Null = no statistically significant association/effect; positive = statistically significant association/effect in hypothesized direction; mixed = at least one statistically significant association/effect if more than one association/effect examined; negative = statistically significant association/effect in opposite of hypothesized direction.
Downgraded to low quality of evidence due to serious risk of bias (primarily from missing eligibility criteria and potential misclassification risk from measurement methods in some studies) and inconsistency of effect.
Study effects were null (Dolinsky et al., 2011; Raza et al., 2019; Schmutz et al., 2017; Yu et al., 2011), positive (Hager et al., 2016; Hauck et al., 2018), and mixed (Hinkley et al., 2012; Kohyama, 2007).
Downgraded two levels from high to low due to serious risk of bias (i.e., lack of information regarding concealment and blinding and concerns for misclassification of the outcome due to self-report or parent report for sleep measures in some studies) and serious risk of indirectness (i.e., interventions varied considerably, and most had multicomponents so that the effects of sleep on PA could not be determined).
Study effects were null (Haines et al., 2018; Taylor et al., 2018), positive (Alhassan et al., 2019; Taylor et al., 2017; Yoong et al., 2019), and mixed (Händel et al., 2017; Puder et al., 2011; Taylor et al., 2015).
Findings among the eight cross-sectional studies (n = 4,801 participants) varied. Four studies did not report significant associations between sleep measures and physical activity outcomes (Dolinsky et al., 2011; Raza et al., 2019; Schmutz et al., 2017; Yu et al., 2011). Hager et al. (2016) was categorized as observing a positive effect given that less time spent in moderate to vigorous physical activity or achieving fewer activity counts/minute was associated with shorter sleep duration and poor sleep problems. A study in 6-month-old infants by Hauck et al. (2018) was also classified as positive. Infants with less sleep spent more time in sedentary movement. In preschool children, Hinkley et al. (2012) observed that males with greater sleep duration were more likely to participate in greater physical activity, but this association was not replicated in females. Among a sample of mostly toddlers, Kohyama (2007) reported that an earlier waking time was associated with greater physical activity but other sleep measures (i.e., sleep onset, sleep duration, and nap duration) were not. Due to serious concerns of bias and serious inconsistency in the overall effects across studies, the quality of evidence for cross-sectional studies was downgraded from “low” to “very low.”
Eight chronic experimental studies (n = 2,368 participants) examined the effects of chronic sleep interventions or conditions on physical activity outcomes. All of the examined interventions were programs that targeted more than one health behavior (e.g., physical activity and nutrition/diet in addition to sleep; Alhassan et al., 2019; Haines et al., 2018; Händel et al., 2017; Puder et al., 2011; Taylor et al., 2015, 2017, 2018) with the exception of one intervention that focused primarily on parent education for childhood sleep health practices (Yoong et al., 2019). Results were varied and included null (n = 2; Haines et al., 2018; Taylor et al., 2018), positive (n = 3; Alhassan et al., 2019; Taylor et al., 2017; Yoong et al., 2019), and mixed effects (n = 3; Händel et al., 2017; Puder et al., 2011; Taylor et al., 2015). Results from the intervention study that focused solely on sleep indicated that total physical activity and moderate to vigorous physical activity of preschoolers increased following the parent sleep education intervention (Yoong et al., 2019). Similar to the intervention studies examining sleep outcomes, the intervention studies with physical activity outcomes had serious risk of bias in some studies, serious indirectness (i.e., high variability in types of interventions examined with many integrating multiple health components in addition to sleep education or behavior), and inconsistency in the effects. Therefore, the quality of evidence was downgraded from “high” to “low.”
Similar to sleep outcome studies, physical activity outcome studies with objective measures used accelerometry with varying protocols. Only two cross-sectional studies utilized objective measures of sleep and physical activity, and although they varied in reported associations, findings were generally positive (Hauck et al., 2018; Kohyama, 2007). Among the experimental studies that examined chronic sleep interventions, most used objectively measured physical activity (n = 6) with mainly mixed or positive effects. Thus, overall studies with objective measures indicated generally positive findings for physical activity outcomes, but as with sleep outcome studies, the heterogeneity in accelerometry methods should be considered.
Fitness Outcomes Data Synthesis
Only three studies that met review criteria reported on fitness outcomes (Table 4). Types of fitness measures included aerobic/cardiorespiratory fitness, muscular/motor fitness, skill-related fitness (e.g., speed), or combinations of fitness components. No cross-sectional studies examined the associations between sleep variables and fitness outcomes.
Table 4.
Associations/Effects Between Sleep and Fitness Outcomes in Early Childhood
| Quality assessment | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other | No. of participantsa | Overall effectb | Quality |
| 0 | Cross-sectional | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Not assignable |
| 0 | Longitudinal | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Not assignable |
| 0 | Acute experimental | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Not assignable |
| 3 | Chronic experimental | No serious risk of bias | No serious inconsistency | Serious indirectnessc | Serious imprecisionc | None | 1,953 | 1 null, 1 positive, and 1 mixedd | Low |
Note. Fitness outcome measures included cardiorespiratory fitness, muscular/motor fitness, and combinations of fitness components. N/A = not applicable.
The number of participants may not represent unique participants.
Overall effect key: Null = no statistically significant association/effect; positive = statistically significant association/effect in hypothesized direction; mixed = at least one statistically significant association/effect if more than one association/effect examined; negative = statistically significant association/effect in opposite of hypothesized direction.
Downgraded two levels to low due to imprecision (only three published studies) and some concern of indirectness (all three studies examined the same intervention that involved multicomponents/health behaviors).
Study effects were null (Bürgi et al., 2012), positive (Puder et al., 2011), and mixed (Niederer et al., 2013).
Three chronic experimental studies examined the effects of a multicomponent intervention (i.e., one that included sleep education as one of many components) on fitness outcomes in the same cohort of participants with reports of positive (Puder et al., 2011), mixed (Niederer et al., 2013), and null results (Bürgi et al., 2012). One study reported fitness effects for the whole sample (Puder et al., 2011), whereas the other two examined effect modification of various factors (Bürgi et al., 2012; Niederer et al., 2013). Although all of the chronic experimental studies were randomized, there were serious concerns of indirectness (i.e., the specific effect of sleep could not be teased out given that the program integrated multiple health behaviors) and imprecision (i.e., due to the low number of published studies and the examination of only one intervention). Therefore, the quality of evidence for chronic experimental studies was downgraded from “high” to “low.”
Discussion
The aim of this systematic review was to examine both the influence of physical activity and fitness on sleep and the role of sleep on physical activity and fitness in early childhood. This review synthesized 36 studies from 29 articles in young children that examined relationships between sleep, physical activity, and fitness. Overall, the quality of evidence was very low to low across study designs and outcomes. Although both sleep and physical activity outcome studies were generally mixed in reported overall associations or effects, there were limited studies examining fitness (i.e., as either an exposure or outcome measure), and therefore, we posit that the level of evidence is insufficient. Collectively, observational studies consisted of only cross-sectional designs and demonstrated inconsistent associations. Although experimental studies included in this review did not demonstrate a beneficial effect of improved sleep outcomes from physical activity or fitness interventions, sleep interventions appeared to benefit some physical activity measures. However, it should be noted that these interventions were multicomponent and did not examine the isolated effects of sleep-specific interventions (i.e., sleep education or sleep extension) on physical activity and fitness outcomes. No experimental studies examined acute bout interventions for either sleep or physical activity outcomes.
The associations and effects of physical activity on sleep outcomes in the current review were not as evident as has been demonstrated in adults. In a meta-analytic systematic review of acute and chronic exercise interventions targeting sleep outcomes in adults, it was concluded that (a) acute exercise may benefit sleep duration, Stage 1 sleep, sleep onset latency, wake time after sleep onset, sleep efficiency, and rapid-eye-movement sleep with small to moderate effect sizes and (b) chronic exercise training may benefit sleep duration, sleep efficiency, sleep onset latency, and sleep quality with moderate effect sizes (Kredlow et al., 2015). More recently, a similar review examined the effect of exercise interventions on sleep outcomes across age groups, although most studies were in adults (Dolezal et al., 2017). Dolezal et al. (2017) noted that among adults, the positive effects of exercise interventions on sleep measures (including changes in sleep stages and sleep duration) appear more consistent and defined. It was also noted that timing of structured exercise appeared to play an influential role on the results, particularly for cardiorespiratory activities. The reports from experimental studies in the current review were not as resolute.
Similar to our findings and in contrast to adult reports, other reviews in youth participants have also reported variable associations or effects of physical activity on sleep outcomes. One meta-analytic review on factors associated with adolescent sleep described physical activity as a protective factor of bedtime (i.e., more physical activity was associated with an earlier bedtime), but physical activity was not associated with sleep latency or total sleep time (Bartel et al., 2015). Among the youth experimental studies synthesized by Dolezal et al. (2017), greater moderate to vigorous physical activity was associated with less sleep duration, better sleep quality and efficiency, or there was no association at all. Although none of the studies in our review observed negative effects of exercise or physical activity on sleep, many reported null results (e.g., all of the experimental studies). Another recent systematic review examined the relationships between movement behaviors (i.e., sedentary time and physical activity) and sleep in children aged less than 5 years (Janssen et al., 2020). Although the age criterion was more limited than in the present review and, therefore, fewer articles were included, Janssen et al. developed similar conclusions given the overall mixed effects between movement behaviors and sleep and overall very low quality of evidence across studies included in their review. Most recently, Antczak et al. (2020) conducted a meta-analysis that reported inconsistent associations between physical activity and sleep in healthy children (mean age range of 3.9–13.4 years). Although, statistically, there was not significant evidence of a relation between these behaviors in children, Antczak and colleagues did note that some associations were weaker in younger children compared with older children. This finding appears to quantify the trend observed in the current and previous reviews.
Differences between sleep outcome studies in early childhood samples compared with those conducted in adult participants may partially be attributed to variability in methodology. For example, some sleep outcome categories have not been examined in younger participants, such as sleep architecture from polysomnography and sleep timing (e.g., chronotype and timing of activity bouts). This review highlights the need for studies that examine sleep physiology (i.e., sleep stages or microstructure such as sleep spindles) and physical activity timing in relation to sleep outcomes. Furthermore, experimental studies included in adult reviews were more likely to examine exercise-specific interventions. However, most of the intervention studies included in the present review were targeting multiple health behaviors. Although this is pragmatic for school-and community-based health intervention studies, it strongly limits the ability to isolate the role of physical activity on the sleep effects.
In addition to the aforementioned recommendations for future research, it may be important that early childhood studies include information regarding 24-hr or nap sleep quantity and quality. Indeed, napping is typically a component of 24-hr sleep in young children. Early childhood is a period that includes transitions from polyphasic to biphasic sleep (i.e., the shift from multiple daily daytime and overnight sleep bouts to one daytime and one overnight sleep bout during infancy into toddlerhood) and from biphasic to monophasic sleep (i.e., the shift from a daily nap and an overnight sleep bout to one consolidated overnight sleep bout in the preschool years; Weissbluth, 1995). However, most of the studies included in this review either focused on overnight sleep or did not distinguish whether sleep measures included nap sleep. Given that early childhood sleep recommendations focus on 24-hr sleep and that the majority of the reviewed studies reported associations or effects with only overnight sleep, this could partially contribute to the mixed effects observed in young children relative to adult studies. Moreover, a review by Thorpe et al. (2015) noted that napping in children up to 5 years of age is associated with some behavior and cognitive outcomes, particularly in younger children that still depend on daytime sleep, but indicated that more studies examining health outcomes are needed. Thorpe et al. future directions are in alignment with the need highlighted in the present review to explore relations of physical activity, fitness, and nap sleep metrics.
Although some bidirectional relationships between physical activity and sleep have been observed in adults, the evidence of the influence of sleep on physical activity-related outcomes (including fitness) is less conclusive than physical activity’s effect on sleep (Chennaoui et al., 2015). Although there is some support that sleep restriction or poor sleep quality may reduce exercise performance or increase the risk of exercise-related injuries in adults, less is known about the impact on physical activity behaviors. Other review analyses in early childhood populations have primarily focused on sleep outcome studies (Chaput et al., 2017; Janssen et al., 2020). Although Chaput et al. (2017) reported mixed results when exploring the association between sleep duration and physical activity in young children (i.e., 0–4 years), only four studies were included in their review, and all were observational (one longitudinal and three cross-sectional). In concordance, the evidence from the current review was not conclusive regarding physical activity and fitness outcomes, although no studies indicated an adverse association or effect of sleep on physical activity-related outcomes. Similar to sleep outcome studies, inconsistency of findings may partially be related to differences in methodologies and measurements and, among the experimental studies, intervention design and components (i.e., most interventions targeted multiple health behaviors rather than sleep-specific interventions, such as sleep extension or sleep health education only).
Temporal studies (e.g., microlongitudinal or daily repeated measures designs) have been used by some research groups to examine both within- and between-individual associations between physical activity and sleep by exploring the predictive nature of daytime physical activity levels on subsequent nighttime sleep and/or the role that nighttime sleep plays on the physical activity levels of the subsequent day. Among adults, although these types of studies have generally reported bidirectional and beneficial relationships (Irish et al., 2014; Lambiase et al., 2013; Mead et al., 2019), a recent meta-analysis of such studies concluded that there is not strong evidence of bidirectional daily relations between physical activity and sleep and, in fact, even the unidirectional associations lack consistency (Atoui et al., 2021). Interestingly, although the temporal studies included in the review by Atoui et al. (2021) followed different methodologies than those included in this present review, there were similarities in the evidence regarding a relation between sleep as an exposure and physical activity as an outcome. Specifically, Atoui et al. noted that in adults, there is some support that sufficient or higher quality sleep at night is linked to greater physical activity the following day. Fewer studies have examined these temporal relationships in youth samples and have, overall, reported less consistent findings (Ekstedt et al., 2013; Krietsch et al., 2016; Lin et al., 2018; Pesonen et al., 2011). Interestingly, no studies included in this review examined temporal relationships between physical activity and sleep in children aged less than 6 years.
The data synthesis of studies that used objective measurements of sleep or physical activity indicated that findings somewhat paralleled the overall effects of all studies. This is comparable with what was described by Lang et al. (2016) in a 2016 systematic review and meta-analysis on relationships between physical activity and sleep in mid-adolescence and early adulthood. In their review, Lang et al. examined the influential effects of different approaches (i.e., combinations of subjective vs. objective physical activity and sleep measures). Although their results were somewhat more consistent than in the current review, they noted that favorable associations between sleep and physical activity were observed regardless of measurement approaches and that these positive effects were somewhat larger in studies that used objective methods. As only one study had used accelerometry to assess both sleep and physical activity in their included studies, and given that objective methods may be more robust and less prone to recall bias (Smith et al., 2018; Sylvia et al., 2014), the authors described a need for future research that assesses both health behaviors objectively. Though it appears that this call to action has received some attention from the number of studies included in the current review that have used measurements such as accelerometry to measure both sleep and physical activity, continued use of objective measures is warranted.
Studies that used subjective measures of sleep and physical activity did not appear to differ in overall effects from studies that used objective measures or from overall studies. Given the young ages of these early childhood participants, it is unsurprising that studies with subjective measures primarily used parent-reported assessments. However, given that young children may spend time in childcare or early education programs or in the care of other adult caregivers, researchers may consider collecting information on sleep and wake behaviors from sources outside of the traditional parent record or questionnaire. In addition, sleep diaries and physical activity tracking forms can provide important information sometimes missed with objective devices (e.g., actual bedtime to better estimate sleep latency, type of physical activities, context relating to behaviors, and information regarding behaviors when devices are not worn; Ancoli-Israel et al., 2003; Galland et al., 2014; Littner et al., 2003), and therefore, subjective reports may be a useful supplement to objective measures, particularly in early childhood samples.
Strengths of this article include the rigorous and transparent methods used to conduct the systematic review. However, there are some limitations that should be noted. First, among the cross-sectional studies, it was occasionally difficult to determine exposure variables versus outcome variables, so variables were categorized using the authors’ discretion and consensus. Second, there is also the potential of misclassification of absolute effects for some studies, particularly among those that were exploratory, articles that did not clearly indicate the hypothesis(es) or the expected effect/direction of association, or studies that reported on numerous associations or effects. Third, despite the broad net that was used to search for articles, the search filters may have excluded some titles. However, a manual review of review papers and reference lists was conducted and did identify some articles that were missed in the initial search. Finally, publication bias could be a concern for null studies that did not get reported.
Conclusions
In this study, we provided a systematic review of the potential bidirectional associations and effects of physical activity and fitness with sleep throughout early childhood. Although the evidence is less conclusive than in adults, the studies reported here suggest that physical activity and fitness may beneficially influence some aspects of sleep in children aged less than 6 years. However, the impact that sleep has on fitness and physical activity is even more inconclusive in young children. This review highlights the need for future research to further explore these relationships, including: (a) high-quality longitudinal studies with objective measurements (in conjunction with subjective measures) to examine the predictive nature of either sleep or physical activity on each other throughout childhood; (b) inclusion of fitness measures as independent variables to examine associations between fitness factors and sleep; (c) studies to determine temporal or within-subject associations between physical activity and sleep (to examine the association between physical activity levels of a day on that subsequent night’s sleep and vice versa); (d) experimental designs including acute bout studies to examine immediate effects of sleep or physical activity, chronic studies with fitness outcomes, and more sleep-specific interventions; and (e) continued and increased use of objective measurement methods of physical activity and sleep (i.e., actigraphy and polysomnography). Future subgroup meta-analyses may be warranted as well to assess for different effects across age groups or methodological approaches. Findings from higher quality studies of sleep and physical activity in young children may support health recommendations and intervention strategies for healthier child development.
Acknowledgments
The authors would like to thank Ellen Lutz from the University of Massachusetts Amherst Libraries for her assistance in the development and review of the study’s methodology. This work was funded in part by the National Heart, Lung, and Blood Institute (R01 HL11169; PI: Spencer).
References
- 2018 Physical Activity Guidelines Advisory Committee. (2018). 2018 Physical Activity Guidelines Advisory Committee Scientific Report. To the Secretary of Health and Human Service. https://health.gov/paguidelines/second-edition/report/pdf/PAG_Advisory_Committee_Report.pdf
- Alhassan S, St. Laurent CW, Burkart S, Greever CJ, & Ahmadi MN (2019). Feasibility of integrating physical activity into early education learning standards on preschooler’s physical activity levels. Journal of Physical Activity and Health, 16(2), 101–107. 10.1123/jpah.2017-0628 [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, & Pollak CP (2003). The role of actigraphy in the study of sleep and circadian rhythms. Sleep, 26(3), 342–392. 10.1093/sleep/26.3.342 [DOI] [PubMed] [Google Scholar]
- Antczak D, Lonsdale C, Lee J, Hilland T, Duncan MJ, del Pozo Cruz B, … Sanders T (2020). Physical activity and sleep are inconsistently related in healthy children: A systematic review and meta-analysis. Sleep Medicine Reviews, 51, 101278. 10.1016/j.smrv.2020.101278 [DOI] [PubMed] [Google Scholar]
- Atoui S, Chevance G, Romain AJ, Kingsbury C, Lachance JP, & Bernard P (2021). Daily associations between sleep and physical activity: A systematic review and meta-analysis. Sleep Medicine Reviews, 57, 101426. 10.1016/j.smrv.2021.101426 [DOI] [PubMed] [Google Scholar]
- Bartel KA, Gradisar M, & Williamson P (2015). Protective and risk factors for adolescent sleep: A meta-analytic review. Sleep Medicine Reviews, 21, 72–85. 10.1016/j.smrv.2014.08.002 [DOI] [PubMed] [Google Scholar]
- Bürgi F, Niederer I, Schindler C, Bodenmann P, Marques-Vidal P, Kriemler S, & Puder JJ (2012). Effect of a lifestyle intervention on adiposity and fitness in socially disadvantaged subgroups of preschoolers: A cluster-randomized trial (Ballabeina). Preventive Medicine, 54(5), 335–340. 10.1016/j.ypmed.2012.02.007 [DOI] [PubMed] [Google Scholar]
- Chang VC, Chaput J-P, Roberts KC, Jayaraman G, & Do MT (2018). Factors associated with sleep duration across life stages: Results from the Canadian Health Measures Survey. Health Promotion and Chronic Disease Prevention in Canada, 38(11), 404–418. 10.24095/hpcdp.38.11.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Birken CS, … Tremblay MS (2017). Systematic review of the relationships between sleep duration and health indicators in the early years (0–4 years). BMC Public Health, 17(Suppl.), 855. 10.1186/s12889-017-4850-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chennaoui M, Arnal PJ, Sauvet F, & Léger D (2015). Sleep and exercise: A reciprocal issue? Sleep Medicine Reviews, 20, 59–72. 10.1016/j.smrv.2014.06.008 [DOI] [PubMed] [Google Scholar]
- De Bock F, Genser B, Raat H, Fischer JE, & Renz-Polster H (2013). A participatory physical activity intervention in preschools: A cluster randomized controlled trial. American Journal of Preventive Medicine, 45(1), 64–74. 10.1016/j.amepre.2013.01.032 [DOI] [PubMed] [Google Scholar]
- Dolezal BA, Neufeld EV, Boland DM, Martin JL, & Cooper CB (2017). Interrelationship between sleep and exercise: A systematic review. Advances in Preventive Medicine, 2017, 1–14. 10.1155/2017/1364387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolinsky DH, Brouwer RJN, Evenson KR, Siega-Riz AM, & Østbye T (2011). Correlates of sedentary time and physical activity among preschool-aged children. Preventing Chronic Disease, 8(6), A131. [PMC free article] [PubMed] [Google Scholar]
- Duraccio KM, & Jensen CD (2017). Associations between physical and sedentary activity regularity and sleep in preschoolers and kindergartners. Sleep Health, 3(4), 263–268. 10.1016/j.sleh.2017.04.001 [DOI] [PubMed] [Google Scholar]
- Ekstedt M, Nyberg G, Ingre M, Ekblom O, & Marcus C (2013). Sleep, physical activity and BMI in six to ten-year-old children measured by accelerometry: A cross-sectional study. International Journal of Behavioral Nutrition and Physical Activity, 10(1), 82. 10.1186/1479-5868-10-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eythorsdottir DY, Frederiksen P, Larsen SC, Olsen NJ, & Heitmann BL (2020). Associations between objective measures of physical activity, sleep and stress levels among preschool children. BMC Pediatrics, 20(1), 258. 10.1186/s12887-020-02108-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felzer-Kim IT, & Hauck JL (2020). Sleep duration associates with moderate-to-vigorous intensity physical activity and body fat in 1- to 3-year-old children. Infant Behavior and Development, 58, 101392. 10.1016/j.infbeh.2019.101392 [DOI] [PubMed] [Google Scholar]
- Galland B, Meredith-Jones K, Terrill P, & Taylor R (2014). Challenges and emerging technologies within the field of pediatric actigraphy. Frontiers in Psychiatry, 5, 99. 10.3389/fpsyt.2014.00099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Australia. (2018). Australian 24-hour movement guidelines for children and young people (5–17 years)—An integration of physical activity, sedentary behaviour and sleep. http://www.health.gov.au/internet/main/publishing.nsf/Content/health-24-hours-physact-guidelines [DOI] [PMC free article] [PubMed]
- Hager ER, Calamaro CJ, Bentley LM, Hurley KM, Wang Y, & Black MM (2016). Nighttime sleep duration and sleep behaviors among toddlers from low-income families: Associations with obesogenic behaviors and obesity and the role of parenting. Childhood Obesity, 12(5), 392–400. 10.10.1089/chi.2015.0252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines J, Douglas S, Mirotta JA, O’Kane C, Breau R, Walton K, … Ma DWL (2018). Guelph Family Health Study: Pilot study of a home-based obesity prevention intervention. Canadian Journal of Public Health, 109(4), 549–560. 10.17269/s41997-018-0072-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Händel MN, Larsen SC, Rohde JF, Stougaard M, Olsen NJ, & Heitmann BL (2017). Effects of the Healthy Start randomized intervention trial on physical activity among normal weight preschool children predisposed to overweight and obesity. PLoS One, 12(10), e0185266. 10.1371/journal.pone.0185266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauck JL, Zott GR, Felzer-Kim IT, & Adkins CM (2018). A comparison of low-intensity physical activity, growth, and sleep behavior in 6-month old infants. Infant Behavior and Development, 53, 18–24. 10.1016/j.infbeh.2018.09.013 [DOI] [PubMed] [Google Scholar]
- Hinkley T, Salmon J, Okely AD, Hesketh K, & Crawford D (2012). Correlates of preschool children’s physical activity. American Journal of Preventive Medicine, 43(2), 159–167. 10.1016/j.amepre.2012.04.020 [DOI] [PubMed] [Google Scholar]
- Irish LA, Kline CE, Rothenberger SD, Krafty RT, Buysse DJ, Kravitz HM, … Hall MH (2014). A 24-hour approach to the study of health behaviors: Temporal relationships between waking health behaviors and sleep. Annals of Behavioral Medicine, 47(2), 189–197. 10.1007/s12160-013-9533-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata S, Iwata O, Iemura A, Iwasaki M, & Matsuishi T (2011). Determinants of sleep patterns in healthy Japanese 5-year-old children. International Journal of Developmental Neuroscience, 29(1), 57–62. 10.1016/j.ijdevneu.2010.09.004 [DOI] [PubMed] [Google Scholar]
- Janssen X, Martin A, Hughes AR, Hill CM, Kotronoulas G, & Hesketh KR (2020). Associations of screen time, sedentary time and physical activity with sleep in under 5s: A systematic review and meta-analysis. Sleep Medicine Reviews, 49, 101226. 10.1016/j.smrv.2019.101226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones RA, Hinkley T, Okely AD, & Salmon J (2013). Tracking physical activity and sedentary behavior in childhood: A systematic review. American Journal of Preventive Medicine, 44(6), 651–658. 10.1016/j.amepre.2013.03.001 [DOI] [PubMed] [Google Scholar]
- Kohyama J (2007). Early rising children are more active than late risers. Neuropsychiatric Disease and Treatment, 3(6), 959–963. 10.2147/ndt.s2087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, & Otto MW (2015). The effects of physical activity on sleep: A meta-analytic review. Journal of Behavioral Medicine, 38(3), 427–449. 10.1007/s10865-015-9617-6 [DOI] [PubMed] [Google Scholar]
- Krietsch KN, Armstrong B, McCrae CS, & Janicke DM (2016). Temporal associations between sleep and physical activity among overweight/obese youth. Journal of Pediatric Psychology, 41(6), 680–691. 10.1093/jpepsy/jsv167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krietsch KN, Chardon ML, Beebe DW, & Janicke DM (2019). Sleep and weight-related factors in youth: A systematic review of recent studies. Sleep Medicine Reviews, 46, 87–96. 10.1016/j.smrv.2019.04.010 [DOI] [PubMed] [Google Scholar]
- Kuzik N, Poitras VJ, Tremblay MS, Lee EY, Hunter S, & Carson V (2017). Systematic review of the relationships between combinations of movement behaviours and health indicators in the early years (0–4 years). BMC Public Health, 17(Suppl.), 849. 10.1186/s12889-017-4851-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambiase MJ, Gabriel KP, Kuller LH, & Mattews KA (2013). Temporal relationships between physical activity and sleep in older women. Medicine & Science in Sports & Exercise, 45(12), 2362–2368. 10.1249/MSS.0b013e31829e4cea [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang C, Kalak N, Brand S, Holsboer-Trachsler E, Pühse U, & Gerber M (2016). The relationship between physical activity and sleep from mid adolescence to early adulthood. A systematic review of methodological approaches and meta-analysis. Sleep Medicine Reviews, 28, 32–45. 10.1016/j.smrv.2015.07.004 [DOI] [PubMed] [Google Scholar]
- Lerner-Geva L, Bar-Zvi E, Levitan G, Boyko V, Reichman B, & Pinhas-Hamiel O (2015). An intervention for improving the lifestyle habits of kindergarten children in Israel: A cluster-randomised controlled trial investigation. Public Health Nutrition, 18(9), 1537–1544. 10.1017/S136898001400024X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y, Tremblay MS, Katzmarzyk PT, Fogelholm M, Hu G, Lambert EV, … Chaput JP (2018). Temporal and bi-directional associations between sleep duration and physical activity/sedentary time in children: An international comparison. Preventive Medicine, 111, 436–441. 10.1016/j.ypmed.2017.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littner M, Kushida CA, Anderson WM, Bailey D, Berry RB, Davila DG, … Johnson SF, & Standards of Practice Committee of the American Academy of Sleep Medicine. (2003). Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: An update for 2002. Sleep, 26(3), 337–341. 10.1093/sleep/26.3.337 [DOI] [PubMed] [Google Scholar]
- Mead MP, Baron K, Sorby M, & Irish LA (2019). Daily associations between sleep and physical activity. International Journal of Behavioral Medicine, 26(5), 562–568. 10.1007/s12529-019-09810-6 [DOI] [PubMed] [Google Scholar]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, … Stewart L, & PRISMA-P Group. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement David. Systematic Reviews, 207, 1–9. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederer I, Bürgi F, Ebenegger V, Marques-Vidal P, Schindler C, Nydegger A, … Puder JJ (2013). Effects of a lifestyle intervention on adiposity and fitness in overweight or low fit preschoolers (Ballabeina). Obesity, 21(3), E287–E293. 10.1002/oby.20119 [DOI] [PubMed] [Google Scholar]
- Okely AD, Ghersi D, Hesketh KD, Santos R, Loughran SP, Cliff DP, … Tremblay MS (2017). A collaborative approach to adopting/adapting guidelines—The Australian 24-Hour Movement Guidelines for the early years (Birth to 5 years): An integration of physical activity, sedentary behavior, and sleep. BMC Public Health, 17(Suppl.), 869. 10.1186/s12889-017-4867-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouzzani M, Hammady H, Fedorowicz Z, & Elmagarmid A (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 1–10. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons AA, Ollberding NJ, Smith L, & Copeland KA (2018). Sleep matters: The association of race, bedtime, outdoor time, and physical activity with preschoolers’ sleep. Preventive Medicine Reports, 12, 54–59. 10.1016/j.pmedr.2018.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, Lloyd RM, … Wise MS (2016). Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. Journal of Clinical Sleep Medicine, 12(6), 785–786. 10.5664/jcsm.5866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesonen AK, Sjöstén NM, Matthews KA, Heinonen K, Martikainen S, Kajantie E, … Räikkönen K (2011). Temporal associations between daytime physical activity and sleep in children. PLoS One, 6(8), e22958. 10.1371/journal.pone.0022958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, … Olson RD (2018). The physical activity guidelines for Americans. Journal of the American Medical Association, 320(19), 2020–2028. 10.1001/jama.2018.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puder JJ, Marques-Vidal P, Schindler C, Zahner L, Niederer I, Bürgi F, … Kriemler S (2011). Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): Cluster randomised controlled trial. BMJ, 343(7830), 1–11. 10.1136/bmj.d6195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raza H, Zhou SM, Todd C, Christian D, Marchant E, Morgan K, … Brophy S (2019). Predictors of objectively measured physical activity in 12-month-old infants: A study of linked birth cohort data with electronic health records. Pediatric Obesity, 14(7), e12512. 10.1111/ijpo.12512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberger ME, Fulton JE, Buman MP, Troiano RP, Grandner MA, Buchner DM, & Haskell WL (2019). The 24-hour activity cycle: A new paradigm for physical activity. Medicine & Science in Sports & Exercise, 51(3), 454–464. 10.1249/MSS.0000000000001811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio-Arias J, Marín-Cascales E, Ramos-Campo DJ, Hernandez AV, & Pérez-López FR (2017). Effect of exercise on sleep quality and insomnia in middle-aged women: A systematic review and meta-analysis of randomized controlled trials. Maturitas, 100, 49–56. 10.1016/j.maturitas.2017.04.003 [DOI] [PubMed] [Google Scholar]
- Schardt C, Adams MB, Owens T, Keitz S, & Fontelo P (2007). Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Medical Informatics and Decision Making, 7(1), 1–7. 10.1186/1472-6947-7-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmutz EA, Leeger-Aschmann CS, Radtke T, Muff S, Kakebeeke TH, Zysset AE, … Kriemler S (2017). Correlates of preschool children’s objectively measured physical activity and sedentary behavior: A cross-sectional analysis of the SPLASHY study. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 1–13. 10.1186/s12966-016-0456-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schünemann HJ, Mustafa RA, Brozek J, Santesso N, Bossuyt PM, Steingart KR, … Guyatt GH (2019). GRADE guidelines: 22. The GRADE approach for tests and strategies—from test accuracy to patient-important outcomes and recommendations. Journal of Clinical Epidemiology, 111, 69–82. 10.1016/j.jclinepi.2019.02.003 [DOI] [PubMed] [Google Scholar]
- Smith MT, McCrae CS, Heald JL, Harrod CG, Cheung J, Martin JL, & Carden KA (2018). Use of actigraphy for the evaluation of sleep disorders and circadian rhythm sleep-wake disorders: An American Academy of Sleep Medicine Clinical Practice Guideline. Journal of Clinical Sleep Medicine, 14(07), 1231–1237. 10.5664/jcsm.7230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylvia LG, Bernstein EE, Hubbard JL, Keating L, & Anderson EJ (2014). Practical guide to measuring physical activity. Journal of the Academy of Nutrition and Dietetics, 114(2), 199–208. 10.1016/j.jand.2013.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RW, Cox A, Knight L, Brown DA, Meredith-Jones K, Haszard JJ, … Williams SM (2015). A tailored family-based obesity intervention: A randomized trial. Pediatrics, 136(2), 281–289. 10.1542/peds.2015-0595 [DOI] [PubMed] [Google Scholar]
- Taylor BJ, Gray AR, Galland BC, Heath ALM, Lawrence J, Sayers RM, … Taylor RW (2017). Targeting sleep, food, and activity in infants for obesity prevention: An RCT. Pediatrics, 139(3), e20162037. 10.1542/peds.2016-2037 [DOI] [PubMed] [Google Scholar]
- Taylor RW, Gray AR, Heath ALM, Galland BC, Lawrence J, Sayers R, … Taylor BJ (2018). Sleep, nutrition, and physical activity interventions to prevent obesity in infancy: Follow-up of the Prevention of Overweight in Infancy (POI) randomized controlled trial at ages 3.5 and 5 y. American Journal of Clinical Nutrition, 108(2), 228–236. 10.1093/ajcn/nqy090 [DOI] [PubMed] [Google Scholar]
- Thorpe K, Staton S, Sawyer E, Pattinson C, Haden C, & Smith S (2015). Napping, development and health from 0 to 5 years: A systematic review. Archives of Disease in Childhood, 100(7), 615–622. 10.1136/archdischild-2014-307241 [DOI] [PubMed] [Google Scholar]
- Tremblay MS, Chaput JP, Adamo KB, Aubert S, Barnes JD, Choquette L, … Carson V (2017). Canadian 24-Hour movement guidelines for the early years (0–4 years): An integration of physical activity, sedentary behaviour, and sleep. BMC Public Health, 17-(Suppl.), 874. 10.1186/s12889-017-4859-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YC, Chen LC, Tung YC, Lee CC, & Tsai SY (2019). Physical activity and objectively assessed sleep in 6-month-old infants in Taiwan. Research in Nursing and Health, 42(2), 128–135. 10.1002/nur.21929 [DOI] [PubMed] [Google Scholar]
- Wang B, Isensee C, Becker A, Wong J, Eastwood PR, Huang R-C, … Brüni LG (2016). Developmental trajectories of sleep problems from childhood to adolescence both predict and are predicted by emotional and behavioral problems. Frontiers in Psychology, 7, 1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissbluth M (1995). Naps in children: 6 months-7 years. Sleep, 18(2), 82–87. 10.1093/sleep/18.2.82 [DOI] [PubMed] [Google Scholar]
- Williams SM, Farmer VL, Taylor BJ, & Taylor RW (2014). Do more active children sleep more? A repeated cross-sectional analysis using accelerometry. PLoS One, 9(4), e93117. 10.1371/journal.pone.0093117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willumsen J, & Bull F (2020). Development of WHO guidelines on physical activity, sedentary behavior, and sleep for children less than 5 years of age. Journal of Physical Activity and Health, 17(1), 96–100. 10.1123/jpah.2019-0457 [DOI] [PubMed] [Google Scholar]
- Yoong SL, Grady A, Stacey F, Polimeni M, Clayton O, Jones J, … Wolfenden L (2019). A pilot randomized controlled trial examining the impact of a sleep intervention targeting home routines on young children’s (3–6 years) physical activity. Pediatric Obesity, 14(4), e12481. 10.1111/ijpo.12481 [DOI] [PubMed] [Google Scholar]
- Yu M-L, Ziviani JM, & Haynes M (2011). Sleep, structured and social time use and young Australian children’s physical activity. Health Promotion Journal of Australia, 22(3), 203–209. 10.1071/HE11203 [DOI] [PubMed] [Google Scholar]
- Zhang Z, Sousa-Sá E, Pereira J, Chaput JP, Okely A, Feng X, & Santos R (2019). Correlates of nocturnal sleep duration, nocturnal sleep variability, and nocturnal sleep problems in toddlers: Results from the GET UP! Study. Sleep Medicine, 53, 124–132. 10.1016/j.sleep.2018.08.035 [DOI] [PubMed] [Google Scholar]


