ABSTRACT
Background
Health professionals’ willingness to accept the COVID-19 vaccine is very important, and evidence suggests that only a limited proportion of health-care workers were ready to accept a COVID-19 vaccine, which is very low when compared with the risk of the disease. This study aimed to assess health professionals’ acceptability and associated factors in Wollega University referral hospital, Western Ethiopia.
Methods
An institution-based cross-sectional study was conducted among health-care workers in Wollega University referral hospital from March 26–28, 2021. The data were collected by using a self-administered questionnaire. Epi-data version 3.2 was used for data entry, and STATA version 14 was used for data analysis. The binary logistic regression model was employed to determine factors associated with the acceptability of the COVID-19 vaccine. Adjusted Odds Ratio (AOR) with 95% confidence intervals was computed and statistical significance was declared at a 5% level (p-value <.05).
Results
A total of 191 health professionals have participated in the study. The study indicates that 65.4% (95% CI: 58.6%, 72.2%) of health professionals had the willingness to receive the COVID-19 vaccine if available. Age of health professionals (AOR = 3.58, 95% CI: 1.38, 8.38), knowledge of the COVID-19 vaccine (AOR = 2.98, 95% CI: 1.22, 7.23), and perception of COVID 19 vaccine (AOR = 5.71, 95% CI: 2.50, 13.00) were significantly associated with vaccine acceptability.
Conclusions and recommendations
Nearly, two-thirds of health professionals were willing to accept the COVID-19 vaccine, which is low. In general, continuous communication and health education have to be provided to enhance overall awareness of the COVID-19 vaccine.
KEYWORDS: COVID-19, willingness, health professionals, vaccine, Ethiopia
Introduction
The COVID-19 pandemic has been resulting in a range of illnesses, from mild symptoms to severe illness and death in recent history. It is still not clear how SARS-CoV-2 will affect each person in which it is mild in some, however, severe and can even cause death in some individuals.1 It is known that vaccination is one of the most crucial strategies in the control of the pandemic. Currently, available COVID-19 vaccines are being held to the same safety standards as all vaccines.1,2 Available evidence is suggesting that AstraZeneca is effective in preventing COVID-19 in people aged 18 years and older.3 Vaccination of health professionals is very crucial as they are on the front lines and at risk of exposure, can potentially transmit the virus that causes COVID-19 to patients, their families, and their communities.1,3,4 Two doses are indicated to provide the best protection against COVID-19 for both mRNA vaccines in which the first dose primes the immune system, helping it recognize the virus, while the second dose boosts the immune response. Like any other vaccine, it is not free from side effects; minor manifestations are visible, especially after the second dose, which include fever, headache, and muscle ache.1
The first batch of COVID-19 vaccines, 2.2 million doses of AstraZeneca, has arrived in Addis Ababa, Ethiopia, on 7 March 2021, through the COVAX facility, a global partnership for equitable and timely access to COVID19 vaccines.5 Ethiopia reported the highest number of COVID-19 confirmed cases in East Africa. As of 7 March 2021, 166,138 confirmed COVID-19 cases, and 2,429 deaths were recorded in the country. This puts Ethiopia in the fifth position by the number of confirmed cases and in the sixth position by the number of deaths due to COVID-19.5 Research revealed greater than 67,569 cases of COVID-19 infected HCWs in Ethiopia.6
Not all vaccines are a hundred percent protective, so every individual has the possibility of getting sick from COVID-19 after vaccination. It is not known how long the protection from the COVID-19 vaccine AstraZeneca will last after completing the two doses.3 In Ethiopia, to maximize the public health benefit of the vaccine, the first doses will be prioritized for health and essential workers, and other at-risk and vulnerable groups.5 The COVID-19 pandemic has brought about an unusual crisis in healthcare as the number of COVID-19 cases has risen unacceptably globally, which include health-care workers (HCWs) infections. The signs and symptoms of the disease were studied in tandem with the rapid development of a vaccine against this fatal disease. Global, sustained efforts have been undertaken by the WHO to limit the spread of infection and improve treatment protocols to decrease morbidity and mortality through available strategies.7
Acceptability of vaccination against COVID-19 among HCWs is very important because health professionals’ willingness toward vaccine acceptance is a crucial factor as they will take it for their own and their probability of recommending the vaccine to their patients will be increased.1,2 Evidence is suggesting that only 27.7% of HCWs were ready to accept a COVID-19 vaccine if it was available which is very low when compared with the risk of the disease.2 Several associated factors were identified so far regarding the willingness of the people to take COVID-19 vaccines; perceived susceptibility, safety (fear of side effects), willingness to pay for the vaccine, history of contracting COVID-19, knowledge regarding COVID-19, sex, occupation, religion, age and marital status.8–10
Disclosing information related to the vaccine is very crucial to increasing the acceptability of the vaccine and reducing factors that contributed to the hesitancy of the vaccine of COVID-19 among health professionals.11,12 It is known that with the risk of COVID-19 reemerges, health professionals can contribute to control it comprehensively, which benefits for better combat COVID-19. However, there is a paucity of research that fully examines the willingness of health professionals toward the COVID-19 vaccine in the study area. Therefore, this study targeted identifying health professionals’ readiness for acceptability of the vaccine in WURH.
Methods
Study area and period
This study was conducted at Wollega University referral hospital (WURH). The hospital is found in Nekemte town, Oromia regional state, western Ethiopia. The town was found 331 km to the west of the capital city, Addis Ababa. The study was conducted from March 26–28, 2021 before the distribution of the vaccine. The hospital has around 232 health workers, of which around 20 health professionals were on duty during the study period. Since the occurrence of the pandemic in Ethiopia, this hospital is serving as a treatment center for COVID-19 cases.
Study design
An institutional-based cross-sectional study design was employed.
Population, sample size, and sampling techniques
All health professionals working in WURH were a source population. Health professionals who were not on duty due to different reasons were excluded from the study. All health professionals who were on duty during data collection, and have willing to participate in the study were included in the study. WURH was selected purposely because this hospital has been serving as the only treatment center for COVID-19 among all health institutions found in Nekemte city.
Variables
Willingness to accept the COVID-19 vaccine was the dependent variable of this study. Acceptance of the COVID-19 vaccine is defined as a willingness to the vaccine if it is available.13 It was assessed by asking the question” Are you willing to accept the approved COVID-19 vaccine if it is available?” If they have a willingness to accept the answer is recorded as “Yes”, and if they have no interest to accept, it is recorded as “No”. Socio-demographic variables such (as age, sex, marital status, educational level, educational background, religion), medical history (chronic medical disease and previously infected with COVID-19), knowledge toward COVID-19 vaccine, attitude toward covid-19 vaccine, and perception toward COVID-19 vaccine were independent variables of this study. The knowledge of health professionals about COVID-19 vaccine was assessed by five items. Each item contained the category of “Yes” and “No”. A correct answer was assigned a “1” point and an incorrect answer was assigned “0” points. The total score ranged from 0 to 5. “Good knowledge” was when the scoring was ≥ mean score and a score below the mean value indicated “poor knowledge” of COVID-19 vaccine.
Ten items were used to assess the attitude of health professionals toward COVID-19 cases. Each item was measured on Likert-scale with a five-point scale (strongly agree, agree, neutral, disagree, strongly disagree) to allow the study participants to express how much they agree or disagree with a particular question. “Favorable attitude” was when the scoring was ≥ mean score and less than mean value was rated as an “unfavorable attitude” toward COVID-19 vaccine. Finally, the perception of participants toward the COVID-19 vaccine was assessed by using five items with the “Yes”/No” category. Respondents who scored greater than or equal to the mean score were grouped to have “good perception” and participants who scored less than mean score were grouped to have “poor perception” toward COVID-19 vaccine.
Data collection techniques and data quality assurance
A questionnaire was developed by reviewing previously published papers. The questionnaires comprised socio-demographic data, medical history, knowledge, attitude, and perception toward the COVID-19 vaccine. The data was collected by using self-administered questionnaires. The questionnaire was given to all health professionals who were present on duty and returned to data collectors after they filled it. The questionnaire was prepared in English, and the content of the questionnaire was explained to them prior to distributing it.
The questionnaire was pre-tested on 5% of participants among health professionals working in Nekemte Specialized hospital. Possible amendments were then made based on the findings. A discussion was held between investigators and data collectors, based on the result of the pretest and accordingly, some amendments were made. One-day training was given to the data collectors about the tool and data collection procedure. Data were checked for completeness, accuracy, clarity, and consistency by the supervisors and principal investigator on a daily basis. Any error or ambiguity and incompleteness were corrected accordingly.
Data management and analysis
Epidata version 3.0 was used for data entry and exported to STATA version 14.0 for further analysis. Descriptive statistics, like frequencies, percentages, mean and standard deviation were computed. Before analysis, data were cleaned and edited by using simple frequencies and cross-tabulation. Re-categorization of categorical variables and categorization of continuous variables was done. The assumption of the logistic regression model was checked before fitting it to the model. The binary logistic regression model was fitted to determine factors associated with COVID-19 vaccine acceptability. Factors that were associated with the outcome variable at a 20% (P-value ≤.20) significant level in the bivariable logistic regression analysis were included in the multivariable logistic regression analysis. Then, crude and adjusted odds ratios together with their corresponding 95% confidence intervals were presented in the final multivariable logistic regression table. AOR with 95% confidence intervals was computed and statistical significance was declared when it was significant at a 5% level (p-value <.05). Multicollinearity (association between explanatory variables) was checked by correlation matrices, and the model goodness-of-fit test was checked by Hosmer and Lemeshow test.
Results
Socio-demographic characteristics of the health care workers
Of the total participants, 191 health professionals responded to the question yielding a response rate of 90.1%. In this study, more than three-fourth of health professionals were relatively younger, and the proportion of the male participants in this study is more than half of the total participants 142 (59.2%). Half of the health professionals were married and 60% of them were protestant religion followers. One hundred sixty-one (84.3%) of the health professionals were first degree holders and close to half of the participants were Nurses in the profession (Table 1).
Table 1.
Socio demographic characteristics of the health professionals in WURH, Nekemte town, Western Ethiopia, 2021.
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Age | <30 years old | 142 | 74.4 |
| ≥30 years old | 49 | 26.6 | |
| Sex | Male | 113 | 59.2 |
| Female | 78 | 40.8 | |
| Never married | Never married | 87 | 45.5 |
| Married | 94 | 49.2 | |
| Separated | 7 | 3.7 | |
| Others | 3 | 1.6 | |
| Religion | Muslim | 31 | 16.2 |
| Protestant | 115 | 60.2 | |
| Catholic | 2 | 1.0 | |
| Orthodox | 35 | 18.3 | |
| Others | 8 | 4.2 | |
| Education level | Diploma | 23 | 12.0 |
| Degree | 161 | 84.3 | |
| Above | 7 | 3.6 | |
| Background | Nurses | 92 | 48.2 |
| Midwifery | 24 | 12.6 | |
| Pharmacy | 15 | 7.8 | |
| Medical Practitioner | 17 | 8.9 | |
| Medical specialty | 21 | 10.9 | |
| MLS | 16 | 8.4 | |
| Others | 6 | 3.3 | |
| Previously infected with COVID-19 | No | 168 | 88.0 |
| Yes | 23 | 12.0 | |
| Chronic medical illness | No | 188 | 98.4 |
| Yes | 3 | 1.6 |
Others** Psychiatry, Anesthesia, Biomedical engineering, Environmental health.
Knowledge of COVID-19 vaccine and its acceptability
In this study, 99 (51.8%) of the respondents know the availability of the COVID-19 vaccine, and 147 (76.9%) did not know the effectiveness of the COVID-19 vaccine. Thirty (15.7%) of the respondent’s belief COVID-19 vaccine increase allergic reaction and only 13.6% of the health professionals assume the COVID-19 vaccine protect against a variant of COVID-19 strains. Overall the mean knowledge level of the COVID-19 vaccine was 2.76 and 126 (66.0%) of health professionals had good knowledge of COVID-19 vaccine (Figure 1).
Figure 1.
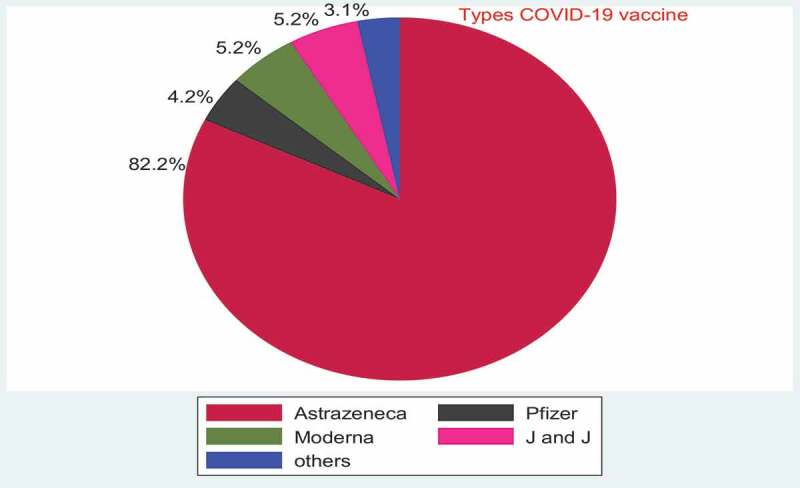
Types of COVID-19 vaccine known by health professionals in WURH, Nekemte town, Western Ethiopia, 2021.
Furthermore, nearly two-third 65.0% (95%CI: 58.6, 72.2) of the health professionals had willing to accept the COVID-19 vaccine as opposed to 35% of health professionals has no intention to accept the COVID-19 vaccine (Table 2).
Table 2.
Knowledge toward COVID-19 vaccine among health professionals in WURH, Nekemte town, Western Ethiopia, 2021.
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Do you know about the COVID-19 vaccine availability? | No | 99 | 51.8 |
| Yes | 92 | 48.1 | |
| Do you know about the effectiveness of COVID-19 vaccine? | No | 44 | 23.1 |
| Yes | 147 | 76.9 | |
| Does vaccination increase allergic reactions? | No | 30 | 15.7 |
| Yes | 161 | 84.3 | |
| Do developed vaccine protect against variant strains? | No | 26 | 13.6 |
| Yes | 165 | 86.4 | |
| Will COVID-19 vaccine provide long term protection? | No | 24 | 12.6 |
| Yes | 167 | 87.4 | |
| Knowledge toward COVID-19 vaccine | Good knowledge | 126 | 66.0 |
| Poor knowledge | 65 | 34.0 | |
| Are you willing to accept COVID-19 vaccine? | Yes | 125 | 65.5 |
| No | 66 | 34.5 |
Attitude and perception toward COVID-19 vaccine
All respondents were asked about their attitudes toward COVID 19 vaccine. Only 20.9% of health professionals agree that the COVID-19 vaccine that is currently used in Ethiopia is also used in the country where the vaccine was discovered. Around 9% of the participants accept the vaccine without any hesitation and only 3.7% agree that the vaccine is safe. Overall, nearly half of the health professionals had a favorable attitude toward COVID-19 vaccine (Table 3).
Table 3.
Attitude of health professionals toward COVID-19 vaccine in WURH, Nekemte town, Western Ethiopia, 2021.
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Newly discovered COVID-19 vaccine that is given for Ethiopia is the actual one that the discovered country is using yet. | Strongly disagree | 57 | 29.8 |
| Disagree | 61 | 31.9 | |
| Neutral | 29 | 15.2 | |
| Agree | 40 | 20.9 | |
| Strongly agree | 4 | 2.0 | |
| If one individual is vaccinated it will have great contribution for the other person (society) | Strongly disagree | 38 | 19.9 |
| Disagree | 31 | 16.2 | |
| Neutral | 29 | 15.2 | |
| Agree | 73 | 38.2 | |
| Strongly agree | 20 | 10.5 | |
| The newly discovered COVID-19 vaccine is safe. | Strongly disagree | 44 | 23.0 |
| Disagree | 65 | 34.0 | |
| Neutral | 40 | 20.9 | |
| Agree | 35 | 18.3 | |
| Strongly agree | 7 | 3.7 | |
| I will take the COVID-19 vaccine without any hesitation | Strongly disagree | 42 | 22.0 |
| Disagree | 89 | 46.6 | |
| Neutral | 24 | 12.6 | |
| Agree | 19 | 9.9 | |
| Strongly agree | 17 | 8.9 | |
| I will encourage my family/friends/relatives to get vaccinated | Strongly disagree | 39 | 20.4 |
| Disagree | 56 | 29.3 | |
| Neutral | 35 | 18.3 | |
| Agree | 47 | 24.6 | |
| Strongly agree | 14 | 7.3 | |
| It is not possible to reduce the incidence of COVID-19 without vaccination | Strongly disagree | 40 | 20.9 |
| Disagree | 63 | 33.0 | |
| Neutral | 26 | 13.6 | |
| Agree | 49 | 25.6 | |
| Strongly agree | 13 | 6.8 | |
| “Even though I am a religious man I have probability to be infected and for that I have to take the vaccine” | Strongly disagree | 31 | 16.2 |
| Disagree | 115 | 60.2 | |
| Neutral | 2 | 1.05 | |
| Agree | 35 | 18.3 | |
| Strongly agree | 8 | 4.2 | |
| The way to overcome the COVID‐19 Pandemic is mass vaccination | Strongly disagree | 29 | 15.2 |
| Disagree | 42 | 22.0 | |
| Neutral | 35 | 18.3 | |
| Agree | 59 | 30.9 | |
| Strongly agree | 26 | 13.6 | |
| Vaccine was not tested for enough time | Strongly disagree | 15 | 7.8 |
| Disagree | 33 | 17.3 | |
| Neutral | 27 | 14.1 | |
| Agree | 53 | 27.7 | |
| Strongly agree | 63 | 33.0 | |
| We can stop precaution after being vaccinated | Strongly disagree | 35 | 18.3 |
| Disagree | 65 | 34.0 | |
| Neutral | 29 | 15.2 | |
| Agree | 29 | 15.2 | |
| Strongly agree | 33 | 17.3 | |
| Attitude toward COVID-19 vaccine | Favorable attitude | 93 | 48.7 |
| Unfavorable attitude | 98 | 51.3 |
The perception of health professionals toward COVID-19 was also assessed. Accordingly, 37% of the participants have perceived the COVID-19 vaccine as it is effective, and half of them perceived that the COVID-19 vaccine is compulsory for all health-care workers. Eighty-eight (46.1%) of health professionals perceive the post-vaccine side effect, and only one-fourth of them perceive the presence of more than one type of COVID-19 vaccine. To sum up, the around 60% of the health professionals had a good perception of COVID 19 vaccines (Table 4).
Table 4.
Health professional’s perception toward Covid-19 vaccine in Nekemte town, 2021.
| Perception questions on Covid-19 vaccine | Yes |
No |
|
|---|---|---|---|
| N (%) | N (%) | ||
| Do you think that the COVID-19 vaccine is effective? | 37 (19.4) | 154 (80.6) | |
| Do you think that COVID-19 vaccination is mandatory for health care workers | 98 (51.3) | 93 (48.7) | |
| Do you think the newly discovered COVID-19 vaccine may have side effects? | 88 (46.1) | 103 (53.9) | |
| Do you think that if everyone in the society maintains the preventive measures, the COVID-19 pandemic can be eradicated without vaccination? | 32 (16.7) | 159 (83.2) | |
| Are you perceive that there are several candidate COVID-19 vaccines being developed? | 50 (26.2) | 141 (73.8) | |
| Do you think the COVID-19 vaccine will be affordable and accessible by the common man? | 30 (15.7) | 161 (84.3) | |
| Perception toward COVID-19 vaccine | Good perception | 114 (59.6) | |
| Poor perception | 77 (40.4) | ||
Factors associated with health professional’s acceptability of the COVID-19 vaccine
In multivariable logistic regression, a variable such as the age of health professionals, knowledge, attitude, and perception toward COVID 19 vaccine was significantly associated with vaccine acceptability in Nekemte town.
Health professionals who are aged greater than 30 years were 3.58 more likely to accept the COVID-19 vaccine when compared to health professionals aged less than 30 years old (AOR = 3.58, 95% CI: 1.38, 8.38). The odds of accepting the COVID-19 vaccine were 2.98 times higher among health professionals who had good knowledge regarding the COVID-19 vaccine than their counterparts (AOR = 2.98, 95% CI: 1.22, 7.23). The perception of health professionals toward COVID-19 vaccine was one of factors that strongly associated with vaccine acceptability. The odds of accepting the vaccine COVID-19 were 5.71 times higher among health professionals who had a good perception of COVID-19 vaccine as compared to their counterparts (AOR = 5.71, 95% CI: 2.50, 13.00) (Table 5).
Table 5.
Multivariable analysis of factors associated with acceptance of COVID-19 vaccine among health professionals in WURH, Nekemte town, Western Ethiopia, 2021.
| Variables | Category | Acceptance |
COR | AOR | P-value | |
|---|---|---|---|---|---|---|
| Accepted | Not accepted | |||||
| Age | ≤30 years | 58 | 84 | Ref | Ref | |
| >30 years | 41 | 8 | 3.58 (1.54, 8.10) | 3.40 (1.38, 8.38) | .008* | |
| Sex | Male | 75 | 38 | Ref | Ref | |
| Female | 50 | 28 | 0.90 (0.49, 1.65) | 0.76 (0.37, 1.58) | .476 | |
| Educational level | Diploma | 14 | 9 | Ref | Ref | |
| ≥1st degree | 111 | 57 | 1.25 (0.51, 3.06) | 1.34 (0.45, 3.95) | .595 | |
| Infected with COVID-19 | No | 111 | 57 | Ref | Ref | |
| Yes | 14 | 9 | 1.25 (0.51, 3.06) | 1.12 (0.39, 3.14) | .828 | |
| Knowledge | Good | 80 | 46 | 1.91 (0.96, 3.78) | 2.98 (1.22, 7.23) | .016* |
| Poor | 45 | 19 | Ref | Ref | ||
| Attitude | Favorable | 71 | 22 | 2.62 (1.41, 4.89) | 3.36 (0.97, 7.11) | .076 |
| Unfavorable | 54 | 44 | Ref | Ref | ||
| Perception | Good perception | 84 | 30 | 2.45 (1.33, 4.53) | 5.71 (2.50, 13.00) | |
| Poor perception | 41 | 36 | Ref | Ref | <.001* | |
*Statistical significant association at a p value <.05.
Discussion
HCW are first in line for the COVID-19 vaccine as they are the front lines, and have a high risk of exposure and potential to transmit to others.14 This study was conducted to assess vaccine acceptability and associated factors among health professionals as it is crucial to reduce vaccine hesitancy and improve vaccine coverage which in turn reduces the burden of COVID-19. The study demonstrated that 65% of the health professionals had a willingness to accept the vaccine. This finding shows a lower level of COVID-19 vaccine acceptance, and it might be due to only 1.6% of health professionals having medical comorbidity during the study period. In addition, this finding is comparable with a study conducted in Hong Kong among nurses 63%.15 The finding of this study is higher than a study in the Democratic Republic of the Congo which reported 27.7%.16 On the other hand, the finding of the current study is lower than other studies conducted among HCW in France (76.9%)17 and dental professionals (85%).7 This discrepancy could be because of the professional variation of the studies as they included different health professionals. The study participants of this study were majorly nurses who are less likely to accept the vaccine than other HCW as evidenced by a previous study.18 The other possible justification for this variation might be due to the difference in study settings and study period as studies were conducted before the availability of vaccines.
One-quarter of health professionals (20.9%) agreed on the currently used COVID-19 vaccine which is similar to a study conducted on the general population in Addis Ababa.12 However, this finding is lower than studies conducted in France (72.4%),19 Greek (78.5%),20 and seven European countries; Germany (70%), United Kingdom (79%), Denmark (80%), Netherlands (73%) and Portugal (75%).21 A survey in 19 countries determined the potential acceptance rates of a COVID-19 vaccine reported 71.5% ranging from 90% in China to less than 55% in Russia.22 This difference may be due to the probability that the studies were conducted before the availability of vaccines. In addition, socioeconomic differences across the study settings may be the other possible reason.
Nearly half of HCW had a favorable attitude toward the COVID-19 vaccine which is supported by a study in France.19 Health professionals who had a favorable attitude toward the COVID-19 vaccine had a higher acceptance rate of the COVID-19 vaccine. It is supported by a study conducted in the Democratic Republic of the Congo.16 This finding is in line with a study conducted on the acceptance of the influenza vaccine among Greek HCW.23 This is because as people perceive vaccines positively, the probability to accept vaccines increases. A study on the acceptability of COVID-19 vaccination among Greek health professionals revealed that the absence of fear over vaccine safety increases vaccine acceptability significantly.20
The study revealed that 60% of health professionals had a good perception of the COVID 19 vaccine. Thus, having a good perception regarding the COVID-19 vaccine improves vaccine uptake.24
In this study, the age of HCW was an important socio-demographic factor that has a significant effect on COVID-19 vaccine acceptance. An increase in age was associated with an increase in vaccination acceptance. This finding is supported by other studies in the Democratic Republic of the Congo,16 Greek,20 and France.25 In addition, a survey in 19 countries22 and a meta-analysis26 also suggested that age is significantly associated with acceptance of the COVID-19 vaccine. This is because; an increasing age is associated with a high risk of comorbidities, an increase in risk perception, and a higher probability of the disease being severe.24
HCW with good knowledge regarding the COVID-19 vaccine had a higher degree of acceptance of the vaccine. This finding is supported by previous studies; health professionals who received information from trusted sources were more likely to accept the vaccine.19,20,22 HCW recommendations play an influential role in their patients’ vaccination behavior. They provide information to the general public and their patients about the benefit of vaccination. Therefore, addressing knowledge gaps regarding the COVID-19 vaccine is the top priority.
HCW having a good perception of the COVID-19 vaccine was strongly positively associated with vaccine acceptability. A study in India on predictors of acceptance of the COVID-19 vaccine in the general public reported that respondents with high perceived benefits showed higher intention to receive the vaccine and respondents with a high perception of the side effects and barriers to vaccination showed a lower intention to receive the vaccine.24
This study is not without some limitations. First, the number of sample size was not optimal as the study was conducted on health professionals. Second, healthy worker survivor bias might be happening due to the number of health professionals were on duty leave when the study was conducted, and this finding could not be truly representative of all health professionals found in this hospital and the general population.
Conclusions and recommendations
Nearly, two-third of health professionals had the willingness to accept the COVID-19 vaccine in WURH, which is low as they are at the highest risk of exposure to the disease and the potential to transmit it to others. Age <30 years, poor knowledge, and poor perception of COVID-19 vaccine negatively affect vaccine acceptability. In general, continuous communication and health education have to be provided to enhance overall awareness and perception of the COVID-19 vaccine.
Acknowledgments
We would like to thank WURH for their invaluable cooperation during data collection and our deep acknowledgment also goes to the data collectors for their interest and commitment in carrying out the study.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Abbreviations
- AOR
Adjusted Odds Ratio
- COR
Crude Odds Ratio
- HCW
Health Care Worker
- MLS
Medical Laboratory Science
- J and J
Johnson and Johnson
- WURH
Wollega University Referral Hospital
Authors’ contribution
TT, GF, BW, and DA were involved in the initial development of the proposal. TT is involved in statistical analysis. TT, and BW were involved in developing the initial drafts of the manuscript. All authors participated in the final preparation of the manuscript and they approved the final draft of the manuscript for submission.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data analyzed during this study are included in the manuscript.
Ethical approval and consent to participate
The study was approved and ethical clearance letters were obtained from Wollega University, Institute of Health Science Research Ethics review board. After approval, a permission letter was obtained from the administrative body of the hospital to the respective clinics. Verbal consent was obtained from study participants and the purpose of this study was stated to all participants. Everybody participated voluntarily in this study.
References
- 1.Force, CC-RVT . COVID-19 vaccine basics: what healthcare personnel need to know. 2021.
- 2.Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, Banza Ndala DB, Mbidi Miema J, Luhata Lungoyo C, Lora Mwimba B, Cikomola Mwana Bene A, Mukamba Musenga E.. Acceptability of vaccination against COVID-19 among healthcare workers in the democratic Republic of the Congo. Pragmat Obs Res. 2020;11:103–7. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australian, G . Information on COVID-19 Vaccine AstraZeneca. 2021.
- 4.Force, CC-RVT . Building confidence in COVID-19 vaccines among your patients. 2021.
- 5.Epi-Week W. National Public Health Emergency Operation Center (PHEOC). In: EPHI, editor. Ethiopia, COVID-19 pandemic preparedness and response in Ethiopia. Addis Ababa; 2021. [Google Scholar]
- 6.Papoutsi E, Giannakoulis VG, Ntella V, Pappa S, Katsaounou P. Global burden of COVID-19 pandemic on healthcare workers. ERJ Open Res. 2020;6(2):00195–2020. doi: 10.1183/23120541.00195-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zigron A, Dror AA, Morozov NG, Shani T, Haj Khalil T, Eisenbach N, Rayan D, Daoud A, Kablan F, Marei H, et al. COVID-19 vaccine acceptance among dental professionals based on employment status during the pandemic. Front Med. 2021;8:13. doi: 10.3389/fmed.2021.618403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belsti Y, Gela YY, Akalu Y, Dagnew B, Getnet M, Abdu Seid M, Diress M, Yeshaw Y, Fekadu SA. Willingness of Ethiopian population to receive COVID-19 vaccine. J Multidiscip Healthcare. 2021;14:1233. doi: 10.2147/JMDH.S312637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banik R, Islam MS, Pranta MUR, Rahman QM, Rahman M, Pardhan S, Driscoll R, Hossain S, Sikder MT. Understanding the determinants of COVID-19 vaccination intention and willingness to pay: findings from a population-based survey in Bangladesh. BMC Infect Dis. 2021;21(1):1–15. doi: 10.1186/s12879-021-06406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, Dasch H, Rubin GJ, Sevdalis N. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVaccs), a nationally representative cross-sectional survey. Hum Vaccines Immunother. 2021;17(6):1612–21. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papagiannis D, Rachiotis G, Malli F, Papathanasiou IV, Kotsiou O, Fradelos EC, Giannakopoulos K, Gourgoulianis KI. Acceptability of COVID-19 vaccination among Greek health professionals. Vaccines (Basel). 2021. Feb 28;9(3):200. doi: 10.3390/vaccines9030200. PMID: 33670913; PMCID: PMC7997202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dereje N, Tesfaye A, Tamene B, Alemeshet D, Abe H, Tesfa N, Gedion S, Biruk T, Lakew Y. COVID-19 vaccine hesitancy in Addis Ababa, Ethiopia: a mixed-methods study. medRxiv. 2021. [DOI] [PMC free article] [PubMed]
- 13.Agyekum MW, Afrifa-Anane GF, Kyei-Arthur F, Addo B. Acceptability of COVID-19 vaccination among health care workers in Ghana. Adv Public Health. 2021;2021:1–8. doi: 10.1155/2021/9998176. [DOI] [Google Scholar]
- 14.COVID, C and RVT Force . COVID-19 vaccine basics: what healthcare personnel need to know. 2020.
- 15.Kwok KO, Li K-K, Wei WI, Tang A, Wong SYS, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021;114:103854. doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nzaji MK, Kabamba Ngombe L, Ngoie Mwamba G, Banza Ndala DB, Mbidi Miema J, Luhata Lungoyo C, Lora Mwimba B, Cikomola Mwana Bene A, Mukamba Musenga E. Acceptability of vaccination against COVID-19 among healthcare workers in the democratic Republic of the Congo. Pragmatic Observational Res. 2020;11:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gagneux-Brunon A, Detoc M, Bruel S, Tardy B, Rozaire O, Frappe P, Botelho-Nevers E. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021;108:168–73. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–79. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verger P, Scronias D, Dauby N, Adedzi KA, Gobert C, Bergeat M, Gagneur A, Dubé E. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Eurosurveillance. 2021;26(3):2002047. doi: 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papagiannis D, Rachiotis G, Malli F, Papathanasiou IV, Kotsiou O, Fradelos EC, Giannakopoulos K, Gourgoulianis KI. Acceptability of COVID-19 vaccination among Greek health professionals. Vaccines. 2021;9(3):200. doi: 10.3390/vaccines9030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020. Sep;21(7):977–982. doi: 10.1007/s10198-020-01208-6. PMID: 32591957; PMCID: PMC7317261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rachiotis G, Mouchtouri VA, Kremastinou J, Gourgoulianis K, Hadjichristodoulou C. Low acceptance of vaccination against the 2009 pandemic influenza a (H1N1) among healthcare workers in Greece. Eurosurveillance. 2010;15(6):19486. doi: 10.2807/ese.15.06.19486-en. [DOI] [PubMed] [Google Scholar]
- 24.Sharun K, Rahman CKF, Haritha CV, Jose B, Tiwari R, Dhama K. Covid-19 vaccine acceptance: beliefs and barriers associated with vaccination among the general population in India. J Exp Biol Agric Sci. 2020;8:S210–S218. doi: 10.18006/2020.8(Spl-1-SARS-CoV-2).S210.S218. [DOI] [Google Scholar]
- 25.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–06. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin C, Tu P, Beitsch L. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines 2021. 2020;9:16. s Note: MDPI stays neu-tral with regard to jurisdictional clai-ms in. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data analyzed during this study are included in the manuscript.


