Abstract
Background
This study aims to describe associations of obesity and CKD in a Swedish urban population. The impact of fat mass, from bioimpedance analysis, on eGFR based on cystatin C and/or creatinine is studied.
Methods
5049 participants from Malmö Diet and Cancer Study the cardiovascular arm (MDCS‐CV) with available body mass composition (single frequency bioimpedance analysis) and cystatin C measured at baseline were selected. Body mass index (kg/m2) was used to define overweight/obesity. eGFR was calculated using cystatin C (eGFRCYS) and creatinine (eGFRCR) equations: Chronic Kidney Disease Epidemiology Collaboration 2012 (CKD-EPICR, CKD-EPICYS, CKD-EPICR-CYS), eGFRCYS based on Caucasian, Asian, pediatric, and adult cohorts (CAPA), the Lund-Malmö revised equation (LMrev), and Modified Full Age Spectrum creatinine-based equation (EKFCCR). Two different fat mass index (FMI) z-scores were calculated: FMI z-scoreLarsson and FMI z-scoreLee.
Results
Lower eGFRCYS and eGFRCR-CYS following multiple adjustments were prevalent in overweight/obese subjects. Increase in FMI z-scoreLarsson or FMI z-scoreLee was related to decrease in predicted CAPA, CKD-EPICYS, CKD-EPICR-CYS and CAPA-LMrev equation.
Conclusion
eGFRCYS, in contrast to combined eGFRCR-CYS and eGFRCR, demonstrate the strongest association between FMI and kidney function.
Introduction
The growing burden of obesity worldwide and its associations with chronic kidney disease (CKD) is becoming a hot topic for the renal medicine community. Actually, obesity and CKD share the same mechanisms such as renin-aldosterone-angiotensin system alteration [1], hyperinsulinemia, inflammation and oxidative stress [2–4]. The obesity related inflammation [5] enhances athero-/arteriosclerosis and kidney damage3, and on the opposite, CKD leads to an inflammatory state [6] causing cardiovascular dysfunction.
CKD diagnosis using creatinine-based estimated glomerular filtration rate (eGFR) tends to be inaccurate in obese subjects [7]. Cystatin C (≅13.3 kDa), a cysteine protease inhibitor, has been proposed as an alternative biomarker for evaluating kidney function and unlike creatinine is not dependent on muscle mass [8]. Cystatin C is also a stronger predictor of cardiovascular diseases compared to creatinine [9]. An increase of cystatin C in cardiovascular outcomes might be compensatory to increased cathepsin S (19–23 kDa) activity in atherosclerotic plaques [10]. Besides, cathepsin S was discovered in obese subjects [11] pointing out the potential shared pathophysiologic pathways between obesity and cardiovascular disease [12], and/or identifying altered glomerular permeability and consequently leading to serum cystatin C accumulation.
Cystatin C expression in human adipose tissue could in part explain increased serum cystatin C levels in obesity [13, 14]. Besides, fat accumulation per se [15, 16], determined by bioelectrical impedance analysis, has been shown to be associated with CKD estimated by creatinine based eGFR equations and needs further clarification. Based on the current knowledge, we aimed to identify relationship between fat mass and kidney function measured by different cystatin C and creatinine eGFR equations, and to determine certain sex-specific link between body composition and kidney function.
Hereby, we hypothesize that tools for fat mass evaluation acquired by bioimpedance analysis are strongly associated with eGFR based on cystatin C and indicate sex-specific relationship in a Swedish urban population.
Materials and methods
Study design and settings
Subjects who participated in the population-based Malmö Diet and Cancer Study (MDCS) [17] were selected to this observational cohort study. MDCS included 17 035 women and 11 063 men, born 1923–1950 and residing in Malmö. MDCS was initially designed as a prospective case-control study that aimed to explore influence of western diet on the incidence of certain forms of cancer after follow-up.
Participants
During the year 1991–1996 MDCS participants were randomly invited to participate in the cardiovascular arm (MDCS‐CV; n = 6103), see Hedblad B et al. [17]. We selected those participants who had their body mass composition, creatinine, and cystatin C (n = 5049) measured at the baseline. None of them had cancer at the inclusion to the study.
For more detailed participant recruitment and data collection see Lahmann P et al. [18].
Measurements
Body composition and anthropometric measurements
The anthropometric and body composition measurements were performed in a non-fasting state. Weight (kg), height (m), waist circumference (WC) and hip circumference (HC) in cm were measured by a trained nurse as previously described by Lahmann P et al. [19]. Body mass index (BMI) calculated as weight in kilograms divided by height in meters squared (kg/m2). BMI <25 kg/m2 determined as normal, 25 ≤BMI<30 kg/m2 as overweight, and >30 kg/m2 as obesity. Waist to hip ratio calculated as WC in cm divided by HC in cm (cm/cm).
Diabetes was defined as diabetes mellitus type 1 or type 2 or fasting plasma glucose concentration greater or equal 7 mmol/L. Hypertension was considered as the presence of diagnosis or the use of antihypertensive medication.
Body composition analysis was performed by using single frequency (50 kHz) bioimpedance equipment, BIA-103 RJL system analyzer (RJL Systems, Detroit, MI), according to procedures provided by the manufacturer (tetrapolar electrode placement, subjects in a supine position). Fat mass (FM) (kg), body fat percent (%), lean mass (LM) (kg), total body water (TBW; liter, L) were estimated automatically by using algorithms implemented in BIA-103 RJL system analyzer. Fat mass index (FMI) calculated as FM in kilograms divided height in meters squared (kg/m2).
Systolic and diastolic blood pressure (SBP and DBP, mmHg) measured by trained nurses during 1991 to 1996. Mean arterial pressure (MAP) was calculated as follows: SBP+2DBP/3 (mmHg).
Fat mass index z-score calculation
Recently Lee MM et al. [20] published sex specific reference values for FMI and skeletal muscle mass index (SMMI) in the white ethnic population older than 40 years. They used single-frequency bioimpedance equipment (Tanita BC-418 MA) and developed reference values based on measurements in 390 565 UK adults. Meanwhile, Larsson I et al. [21] provided reference values on body composition (FM, FMI, body fat percent) based on dual-energy X-ray absorptiometry (DEXA) measurements in adult Swedes. They pooled data from four population-based studies: The young adult, The Mölndal Metabolic study, The Swedish Obese Subjects reference study and The Geriatric and Gerontologic Population Study and the Population Study of Women). In total 623 men and 801 women that underwent the anthropometric and DEXA measurements in between 1990 and 2006 were analyzed.
Based on these reference values we calculated two different FMI z-scores. One z-score FMILee by using FMI reference values for bioimpedance [20] and the other z-score FMILarsson−by using DEXA provided references [21].
The equation for z-score calculation was as follows:
Where x is a raw value, μ –is the population mean (reference value), and σ –is the population standard deviation. For example z-score FMILarsson = (FMI–FMILarsson)/ σLarsson.
Biochemistry
Participants donated fasting blood samples that were drawn and immediately frozen to −80°C and stored in a biobank as reported previously [22]. Plasma creatinine (μmol/L) concentration measured by using Jaffé method [23], a calibrator traceable to the international standardization with isotope dilution mass spectrometry (IDMS) [24]. Plasma cystatin C (mg/L) was analyzed with a particle-enhanced immunonephelometric assay (N Latex Cystatin; Dade Behring, Deerfield, IL, USA). The values for cystatin C were analyzed before the introduction of the world calibrator in 2010 and thus not standardized [25]. The standardization of cystatin C values was performed as described elsewhere [26].
Estimation of kidney function
Estimated glomerular filtration rate (eGFR) was calculated by using seven different equations: Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) 2012 creatinine and cystatin C equations [24] (CKD-EPICR, CKD-EPICYS, CKD-EPICR-CYS)), cystatin C eGFR equation based on Caucasian, Asian, pediatric, and adult cohorts (CAPA) [25], the Lund-Malmö revised creatinine based eGFR equation (LMrev) [27], modified Full Age Spectrum creatinine-based equation (EKFCCR) [28] and combined CAPA-LMrev equation.
Urinary albumin-to-creatinine ratio (mg/mmol) (UACR) was measured in morning urine samples as described previously [29].
Statement of ethics
Each investigator committed to comply with legislation and to conduct the study in line with regulations, in accordance with the 1975 Declaration of Helsinki and its later amendments. The following ethical permissions apply for the cohort: MDCS (LU 51/90, 532/2006). All participants signed the informed consent.
Statistical analysis
Statistical analysis was conducted by using Rcrmdr version R 3.6.2 GUI 1.70 El Capitan build macOS. A p-value less than 0.05 was considered significant.
Continuous variables are expressed as mean and standard deviations (SD), discrete variables as medians with interquartile ratio (IQR) and categorical variables as numbers and percentages in parentheses. F-test was applied to test the equality of two populations for normally distributed continuous data, and only after this a Student’s t-test was performed. Two groups of not normally distributed data were compared by using nonparametric two-sample Wilcoxon test. When applicable, a Chi-square test was conducted. Spearman correlation test was carried out to define the correlations among variables if at least one of variables was not normally distributed. Adjusted P values (Holm-Bonferroni method) were used in order to counteract the problem of multiple comparisons.
Since the difference between men and women in baseline clinical parameters was significant the interaction analysis was performed. We checked if interaction between sex, fat mass index and mean arterial pressure was associated with different equations for eGFR. For this fat mass index z-score and the centralized values for mean arterial pressure were calculated and then put in the multiple linear regression.
To find out which factors that reflect body composition are associated with estimated kidney function following adjustments for age, sex and mean arterial pressure the multivariable linear regression was accomplished.
Results
Participants
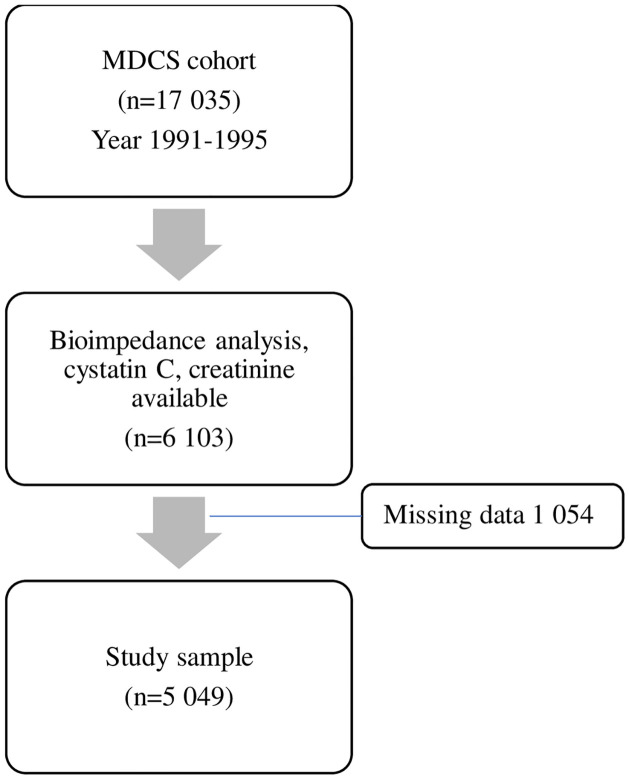
The flow chart of this study is presented in Fig 1.
Fig 1. Selection of subjects for a study.
MDCS, Malmo Diet Cancer study.
General characteristics of the study population
The general demographic characteristics and comparison of clinical characteristics between men and women are presented in Tables 1 and 2, respectively.
Table 1. Demographic characteristics of study subjects.
| Variable | Total (n = 5049) | Women (n = 2990) | Men (n = 2059) |
|---|---|---|---|
| Age, at baseline, years | 57 (6) | 57 (6) | 57 (6) |
| Age, at follow-up, years | 73 (6) | 73 (6) | 73 (6) |
| Diabetes, yes | 668 (13.2) | 412 (13.8) | 256 (12.4) |
| Hypertension, yes | 1889 (22.3) | 1028 (34.3) | 861 (41.8) |
| Obesity, yes | 651 (12.9) | 401 (13.4) | 250 (12.1) |
| Lipid-lowering treatment, at follow-up, yes | 120 (2.9) | 55 (1.8) | 65 (3.1) |
| AntiHT treatmenta, at follow-up, yes | 831 (36.7)a | 466 (56.1)a | 365 (43.9)a |
| Smoking, yes | 1085 (21.5) | 628 (21.0) | 457 (22.1) |
Data expressed as number (%).
a data available in total of 2265 subjects: 1513 women and 752 men.
Abbreviations: AntiHT, antihypertensive treatment.
Smoking determined as current active smoking; obesity as BMI ≥30 kg/m2.
Table 2. Clinical characteristics and comparisons between men and women at baseline.
| Variable | Total (n = 5049) | Women (n = 2990) | Men (n = 2059) | P |
|---|---|---|---|---|
| BMI, kg/m2 | 25.7 (3.9) | 25.4 (4.2) | 26.2 (3.5) | <0.001 |
| FM, kg | 20.0 (6.8) | 21.7 (6.7) | 17.5 (6.2) | <0.001 |
| LM, kg | 52.9 (10.9) | 45.8 (5.6) | 63.4 (8.1) | <0.001 |
| Body fat % | 27 (7) | 31 (5) | 21 (5) | <0.001 |
| FMI, kg/m2 | 7.1 (2.6) | 8.1 (2.5) | 5.6 (2.0) | <0.001 |
| z-score FMILarssona | -0.53 (0.85) | -0.47 (0.79) | -0.62 (0.91) | <0.001 |
| z-score FMILeeb | -1.45 (2.51) | -1.32 (2.42) | -1.64 (2.63) | <0.001 |
| TBW, L | 37.9 (7.4) | 32.7 (3.1) | 45.5 (4.8) | <0.001 |
| WC, cm | 84 (13) | 77 (10) | 93 (10) | <0.001 |
| WHR | 0.85 (0.09) | 0.79 (0.05) | 0.94 (0.06) | <0.001 |
| SBP, mmHg | 141 (19) | 141 (19) | 143 (19) | <0.001 |
| DBP, mmHg | 87 (9) | 86 (9) | 89 (10) | <0.001 |
| MAP, mmHg | 105 (12) | 104 (11) | 107 (12) | <0.001 |
| Cystatin C, mg/L | 1.17 (0.29) | 1.18 (0.28) | 1.17 (0.29) | 0.005 |
| Creatinine, µmol/L | 85 (16) | 79 (13) | 93 (18) | <0.001 |
| CAPA, mL/min/1.73m2 | 64 (15) | 64 (15) | 65 (15) | 0.005 |
| CKD-EPICYS, mL/min/1.73m2 | 69 (16) | 63 (17) | 77 (8) | <0.001 |
| LMrev, mL/min/1.73m2 | 77 (13) | 82 (12) | 71 (12) | <0.001 |
| CKD-EPICR, mL/min/1.73m2 | 76 (14) | 74 (13) | 76 (9) | <0.001 |
| EKFCCR, mL/min/1.73m2 | 69 (14) | 80 (14) | 79 (14) | <0.001 |
| CKD-EPICR-CYS, mL/min/1.73m2 | 79 (14) | 67 (14) | 73 (14) | <0.001 |
| CAPA-LMrev, mL/min/1.73m2 | 71 (12) | 73 (12) | 68 (12) | <0.001 |
| UACR, mg/mmol | 2.36 (11.04) | 1.54 (6.04) | 3.45 (15.28) | 0.830 |
Data expressed as Mean (± SD) or Median with interquartile ratio (IQR).
a based on DEXA acquired fat mass.
b based on bioimpedance acquired fat mass.
Abbreviations: BMI, body mass index; F: fasting; FM, fat mass; LM, lean mass; FMI, fat mass index; TBW, total body water; WC, waist circumference; WHR, waist-to-hip ratio; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; eGFR, estimated glomerular filtration rate; CAPA, cystatin C eGFR equation based on Caucasian, Asian, pediatric, and adult cohorts; LMrev, the Lund-Malmö revised creatinine based eGFR equation; CKD-EPICYS, the Chronic Kidney Disease Epidemiology Collaboration cystatin C equation; CKD-EPICR, the Chronic Kidney Disease Epidemiology Collaboration creatinine equation; CKD-EPICR-CYS, the Chronic Kidney Disease Epidemiology Collaboration combined creatinine and cystatin C equation; EKFCCR, a Modified Full Age Spectrum creatinine-based equation; CAPA-LMrev, average eGFR calculated from CAPA and LMrev; UACR, urinary albumin to creatinine ratio.
Body mass index and kidney function
Overweight (n = 2000) and/or obesity (n = 651) were associated with decreased eGFR, irrespective of sex. Obese subjects vs. overweight vs. normal BMI had lower CAPA (66 vs. 63 vs. 60 mL/min/1.73m2 respectively, p<0.001). As for LMrev equation, only overweight subjects had lower LMrev as compared either to obese subjects or to those with normal BMI (76 vs.78 mL/min/1.73m2, p = 0.003 and 76 vs 79 mL/min/1.73m2, p<0.001 respectively). The latter observations were not present in CKD-EPICR equation. CKD-EPICYS but not CAPA equation revealed sex- and BMI interactions, showing significantly lower eGFR among overweight/obese women (61 and 57 mL/min/1.73m2, p<0.001) compared to men (77 and 76 mL/min/1.73m2, p<0.001). These associations–except for the LM rev, CKD-EPICR and EKFCCR equation—between BMI and kidney function were confirmed by performing linear regression analysis with different eGFR equations as dependent variables following adjustments for age, sex and mean arterial pressure (Table 3). BMI as a continuous variable was associated with eGFR equations that take cystatin C concentration into account. The addition of diabetes to linear regression models did not influence the results due to its low prevalence rate (13.2%).
Table 3. Association between body mass index and eGFR equations.
| CAPA | CKD-EPICYS | LMrev | CKD-EPICR | |||||||||
| ß | SE | P | ß | SE | P | ß | SE | P | ß | SE | P | |
| Age, y | -0.838 | 0.035 | <0.001 | -0.893 | 0.032 | <0.001 | -0.742 | 0.027 | <0.001 | -0.829 | 0.031 | <0.001 |
| Sex, male | 1.228 | 0.415 | 0.003 | 14.925 | 0.382 | <0.001 | -11.173 | 0.321 | <0.001 | 6.448 | 0.367 | <0.001 |
| MAP, mmHg | -0.019 | 0.018 | 0.298 | -0.009 | 0.017 | 0.588 | -0.010 | 0.014 | 0.475 | -0.007 | 0.016 | 0.666 |
| Overweight, yes (n = 2000) | -2.181 | 0.441 | <0.001 | -1.956 | 0.406 | <0.001 | -0.409 | 0.341 | 0.231 | -0.451 | 0.391 | 0.248 |
| Obesity, yes (n = 651) | -4.942 | 0.645 | <0.001 | -4.667 | 0.594 | <0.001 | 0.697 | 0.499 | 0.162 | 0.779 | 0.571 | 0.172 |
| Age, y | -0.841 | 0.035 | <0.001 | -0.896 | 0.032 | <0.001 | -0.743 | 0.027 | <0.001 | -0.831 | 0.031 | <0.001 |
| Sex. male | 1.308 | 0.411 | 0.001 | 15.012 | 0.379 | <0.001 | 11.259 | 0.319 | <0.001 | 6.355 | 0.365 | <0.001 |
| MAP, mmHg | -0.013 | 0.018 | 0.494 | -0.002 | 0.017 | 0.862 | -0.010 | 0.014 | 0.490 | -0.007 | 0.016 | 0.689 |
| BMI, kg/m2 | -0.464 | 0.053 | <0.001 | -0.043 | 0.049 | <0.001 | 0.023 | 0.041 | 0.566 | 0.024 | 0.047 | 0.604 |
Multiple linear regression analysis, eGFR equations (dependent variable) following adjustments for age, sex and mean arterial pressure.
Where applicable normal body mass index group used as a reference value.
Abbreviations: BMI, body mass index; eGFR, estimated glomerular filtration rate; CAPA, cystatin C eGFR equation based on Caucasian, Asian, pediatric, and adult cohorts; LMrev, the Lund-Malmö revised creatinine based eGFR equation; CKD-EPICYS, the Chronic Kidney Disease Epidemiology Collaboration cystatin C equation; CKD-EPICR, the Chronic Kidney Disease Epidemiology Collaboration creatinine equation; CKD-EPICR-CYS, the Chronic Kidney Disease Epidemiology Collaboration combined creatinine and cystatin C equation; EKFCCR, a Modified Full Age Spectrum creatinine-based equation; CAPA-LMrev, average eGFR calculated from CAPA and LMrev.
Fat mass and kidney function
Body impedance acquired measurement and anthropometric parameter correlations with different eGFR equations, as well as with cystatin C and creatinine concentrations, in men and women are listed as S1 Table. The strongest significant correlations were as follows: fat mass, FMI, z-score FMILee and WC negatively correlated with both cystatin C equations, and positively with cystatin C concentration in both men and women, whereas combined creatinine and cystatin C equations were negatively correlated to fat mass, FMI and WC only. Lean mass was negatively associated with CKD-EPICR and positively with plasma creatinine concentration in men.
The interaction analysis could not confirm neither interrelationship between sex and FMI, nor between sex, MAP and FMI z-scores that is associated with eGFR equations (S2 Table). Therefore, the differences between sexes were addressed with caution.
In multivariable linear regression models (Table 4) a 1 kg/m2 increase in FMI was associated with a decrease in predicted CAPA by 0.77 mL/min/1.73m2, a decrease in predicted CKD-EPICYS by 0.73 mL/min/1.73m2, as well as in CDK-EPICR-CYS by 0.36 mL/min/1.73m2 and in CAPA-LMrev by 0.26 mL/min/1.73m2. Furthermore, increase in FMI z-scoreLarsson or FMI z-scoreLee was related to a decrease in predicted CAPA by 2.02 and 0.69 mL/min/1.73m2, respectively, a decrease in predicted CKD-EPICYS by 1.81 and 0.62 mL/min/1.73m2, as well as in predicted CDK-EPICR-CYS by 0.90 and 0.32 mL/min/1.73m2 and in CAPA-LMrev by 0.65 and 0.23 mL/min/1.73m2, respectively. The association with eGFR based on creatinine–LM rev, EKFCCR and CKD-EPICR−was much weaker though statistically significant; showing that an increase in FMI and its z-scores was related to an increase in kidney function derived from eGFRCR equations. The addition of diabetes mellitus to the models did not affect the results provided (not listed in a Table 4).
Table 4. Association between fat mass index z-scores and eGFR equations.
| CAPA | CKD-EPICYS | LMrev | CKD-EPICR | |||||||||
| ß | SE | P | ß | SE | P | ß | SE | P | ß | SE | P | |
| Age, y | -0.831 | 0.035 | <0.001 | -0.886 | 0.032 | <0.001 | -0.749 | 0.027 | <0.001 | -0.84 | 0.03 | <0.001 |
| Sex, male | -0.972 | 0.475 | 0.041 | 12.846 | 0.437 | <0.001 | -10.597 | 0.367 | <0.001 | 7.12 | 0.42 | <0.001 |
| MAP, mmHg | -0.014 | 0.018 | 0.449 | -0.004 | 0.017 | 0.828 | -0.020 | 0.014 | 0.166 | -0.02 | 0.02 | 0.26 |
| FMI, kg/m2 | -0.768 | 0.089 | <0.001 | -0.731 | 0.082 | <0.001 | 0.243 | 0.069 | <0.001 | 0.28 | 0.08 | <0.001 |
| Age, y | -0.899 | 0.035 | <0.001 | -0.948 | 0.032 | <0.001 | -0.726 | 0.027 | <0.001 | -0.811 | 0.031 | <0.001 |
| Sex, male | 0.652 | 0.414 | 0.116 | 14.416 | 0.382 | <0.001 | -11.195 | 0.320 | <0.001 | 6.543 | 0.366 | <0.001 |
| MAP, mmHg | -0.015 | 0.018 | 0.408 | -0.007 | 0.017 | 0.678 | -0.021 | 0.014 | 0.147 | -0.019 | 0.016 | 0.236 |
| z-score FMILarsson | -2.023 | 0.245 | <0.001 | -1.806 | 0.226 | <0.001 | 0.716 | 0.189 | 0.001 | 0.834 | 0.217 | 0.0001 |
| Age, y | -0.868 | 0.035 | <0.001 | -0.920 | 0.032 | <0.001 | -0.737 | 0.027 | <0.001 | -0.824 | 0.031 | <0.001 |
| Sex, male | 0.745 | 0.412 | <0.001 | 14.500 | 0.380 | <0.001 | -11.138 | 0.319 | <0.001 | 6.491 | 0.365 | <0.001 |
| MAP, mmHg | -0.014 | 0.018 | 0.448 | -0.006 | 0.017 | 0.721 | -0.020 | 0.014 | 0.161 | -0.018 | 0.016 | 0.263 |
| z-score FMILee | -0.694 | 0.082 | <0.001 | -0.616 | 0.076 | <0.001 | 0.225 | 0.064 | <0.001 | 0.256 | 0.073 | <0.001 |
Multiple linear regression analysis, eGFR equations (dependent variable) following adjustments for age, sex and mean arterial pressure.
Abbreviations: FMI, fat mass index; eGFR, estimated glomerular filtration rate; CAPA, cystatin C eGFR equation based on Caucasian, Asian, pediatric, and adult cohorts; LMrev, the Lund-Malmö revised creatinine based eGFR equation; CKD-EPICYS, the Chronic Kidney Disease Epidemiology Collaboration cystatin C equation; CKD-EPICR, the Chronic Kidney Disease Epidemiology Collaboration creatinine equation; CKD-EPICR-CYS, the Chronic Kidney Disease Epidemiology Collaboration combined creatinine and cystatin C equation; EKFCCR, a Modified Full Age Spectrum creatinine-based equation, CAPA-LMrev, average eGFR calculated from CAPA and LMrev.
Discussion and conclusions
The introduction of cystatin C, as a marker of kidney function, has simplified early detection of CKD. Though, the use of eGFR in obese population is less well studied. Here we show that fat mass index and its z-scores are strongly associated with lower cystatin C based eGFR equations possibly indicating either early kidney damage with altered glomerular permeability or cystatin C production by adipose tissue. The association between fat mass index and creatinine-based eGFR formulas was much weaker.
The interaction between adipose and renal tissue, the so called adipo-renal axis, is critical for kidney health [4]. This bi-directional crosstalk complicates the diagnosis of kidney lesion in obesity since it raises doubts as to whether altered immunologic and endocrine function of adipose tissue has led to kidney damage, or the underlying kidney disease has exacerbated obesity. The identifications of body composition and fat distribution has become a game changer in adiposity evaluation in relation to CKD, and helps to address the “obesity paradox” based on BMI calculation in end stage renal disease (ESRD) [3]. The “obesity paradox” defines beneficial effect of increasing BMI on survival in end-stage kidney disease [30].
In this observational cohort study, we show that both increased BMI and fat mass index were associated with significantly lower cystatin C derived eGFR, irrespective of sex. Moreover, decreased cystatin C based kidney function and increased cystatin C concentration per se correlated with increased fat mass and abdominal obesity. Obesity induced glomerular damage is one of possible explanations [31], since 2651 from 5049 subjects in our study were either overweight or obese. Indeed, kidney biopsies in obese subjects [31] report glomerular basement membrane thickening in addition to glomerulosclerosis. These histological changes are like those observed in Shrunken Pore Syndrome (SPS) [32]. Increased thickness of glomerular basement membrane alters glomerular permeability and might cause reduced clearance of middle-sized weight proteins (10–30 kDa) [33], including cystatin C and atherosclerosis-promoting proteins [34]. This possible link between increased cystatin C and atherosclerosis needs further exploration.
On the other side, cystatin C expression in adipose tissue, confirmed by both animal [35] and human studies [13], might also affect a possible underestimation of kidney function in studied populations. Human adipose tissue biopsy data showed 3-fold higher cystatin C expression in adipose stromal cells in obese subjects as compared to non-obese [13, 14]. Though these findings need further elucidation.
The mGFR (based on iohexol or inulin clearance) might underestimate kidney function if adjusted to body surface area using real body weight instead of ideal body weight [36]. CKD-EPICR as compared to mGFR has been reported to be valid in obesity, especially for CKD stage 3 to 5 [36]. However, both MDRD (The Modification of Diet in Renal Disease) and CKD-EPICR underestimates kidney function if mGFR is lower than 30 ml/min/1,73m2 [37]. Our finding that increased FMI is related to an increase in predicted kidney function derived from creatinine-based eGFR equations might be explained by the previous observations: (i) increased creatinine excretion and generation in obesity [38]; (ii) obesity related renal hyperfiltration–an early sign of chronic kidney damage [39].
In terms of drug prescription, the underestimation of kidney function in obesity prevents overdosing, though, underdosing can result in therapy failure [40]. Interestingly, CKD-EPICR-CYS has better performance in evaluating kidney function as compared to either CKD-EPICR or CKD-EPICYS in patients undergoing bariatric surgery [41].
The strength of this study is that we used a population-based cohort and that it includes different eGFR equations, currently widely used in clinical practice, with body composition measurements. We calculated FMI z-scores based on reference values for bioimpedance and for DEXA and therefore limiting the chance of imprecise result interpretation.
Limitations of the study is the use of bioimpedance performed by single-frequency equipment in 1991–1996. Multifrequency bioimpedance measurements or DEXA are more accurate techniques for evaluating the proposed three-compartment body composition model [42]. We did not have data on measured GFR (iohexol clearance) to clarify whether the cystatin C and creatinine based eGFR was under-/overestimated in our population [43], whilst this method is not suitable for large cohort studies.
In summary, here we show that cystatin C based eGFR equations could better reveal relationship between fat mass index and its z-scores and kidney function. The association between fat mass index and combined cystatin C and creatinine based eGFR equations and creatinine-based eGFR formulas was much weaker.
Future perspectives
The association between cystatin C and fat mass may be due to several reasons. Obesity induced kidney damage is one. Increased cystatin C concentration against the background of different permeability of middle-sized molecules in kidney is the second and can be coupled to cardiorenal diseases. Finally, further human studies are warranted to elucidate whether cystatin C originates from adipose tissue.
Supporting information
(DOCX)
eGFR equations (dependent variable) following adjustments for age. sex and centralized mean arterial pressure.
(DOCX)
Acknowledgments
On behalf of the European Kidney Function Consortium authors acknowledge the support of European Renal Association (ERA) in publishing study results.
Data Availability
Data contain potentially identifying or sensitive patient information. The datasets generated and analysed during the current study could be extracted by sending application to the steering committee for Malmö Diet and Cancer, contact persons: the head of the committee, Olle Melander, olle.melander@med.lu.se; data manager, Anders Dahlin, anders.dahlin@med.lu.se.
Funding Statement
Financial support for Malmö Diet and Cancer Study (MDCS) has been given by the Swedish Cancer Foundation, The Swedish Medical Research Council, The European Commission, the City of Malmö, the Swedish Dairy Association, and the Albert Påhlsson Foundation. MDCS was supported by Lund University Infrastructure grant ”Malmö population-based cohorts” (STYR 2019/2046). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Rüster C,Wolf G. The Role of the Renin-Angiotensin-Aldosterone System in Obesity-Related Renal Diseases. Semin. Nephrol. 2013;33:44–53. doi: 10.1016/j.semnephrol.2012.12.002 [DOI] [PubMed] [Google Scholar]
- 2.Kazancioǧlu R. Risk factors for chronic kidney disease: An update. Kidney International Supplements. 2013;3:368–371. doi: 10.1038/kisup.2013.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lakkis JI, Weir MR. Obesity and Kidney Disease. Progress in Cardiovascular Diseases. 2018,61:157–167. doi: 10.1016/j.pcad.2018.07.005 [DOI] [PubMed] [Google Scholar]
- 4.Zhu Q, Scherer PE. Immunologic and endocrine functions of adipose tissue: implications for kidney disease. Nature Reviews Nephrology. 2018;14:105–120. doi: 10.1038/nrneph.2017.157 [DOI] [PubMed] [Google Scholar]
- 5.Gregor MF, Hotamisligil GS. Inflammatory mechanisms in obesity. Annu Rev Immunol. 2011;29:415–45. doi: 10.1146/annurev-immunol-031210-101322 [DOI] [PubMed] [Google Scholar]
- 6.Brunet P, Gondouin B, Duval-Sabatier A, Dou L, Cerini C, Dignat-George F et al. Does uremia cause vascular dysfunction? Kidney Blood Press Res. 2011;34(4):284–90. doi: 10.1159/000327131 [DOI] [PubMed] [Google Scholar]
- 7.Wuerzner G, Bochud M, Giusti V, Burnier M. Measurement of glomerular filtration rate in obese patients: pitfalls and potential consequences on drug therapy. Obes Facts. 2011;4(3):238–43. doi: 10.1159/000329547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osaka T, Hamaguchi M, Hashimoto Y, Ushigome E, Tanaka M, Yamazaki M et al. Decreased the creatinine to cystatin C ratio is a surrogate marker of sarcopenia in patients with type 2 diabetes. Diabetes Res Clin Pract. 2018;139:52–58. doi: 10.1016/j.diabres.2018.02.025 [DOI] [PubMed] [Google Scholar]
- 9.Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB, et al. Cystatin C and the risk of death and cardiovascular events among elderly persons. N Engl J Med. 2005;352(20):2049–60. doi: 10.1056/NEJMoa043161 [DOI] [PubMed] [Google Scholar]
- 10.Liu J, Sukhova GK, Sun JS, Xu WH, Libby P, Shi GP. Lysosomal cysteine proteases in atherosclerosis. Arterioscler Thromb Vasc Biol. 2004;24(8):1359–66. doi: 10.1161/01.ATV.0000134530.27208.41 [DOI] [PubMed] [Google Scholar]
- 11.Taleb S, Clément K. Emerging role of cathepsin S in obesity and its associated diseases. Clin Chem Lab Med. 2007;45(3):328–32. doi: 10.1515/CCLM.2007.083 [DOI] [PubMed] [Google Scholar]
- 12.Pei YF, Zhang L, Liu Y, Li J, Shen H, Liu YZ, et al. Meta-analysis of genome-wide association data identifies novel susceptibility loci for obesity. Hum Mol Genet. 2014;23(3):820–30. doi: 10.1093/hmg/ddt464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naour N, Fellahi S, Renucci JF, Poitou C, Rouault C, Basdevant A, et al. Potential contribution of adipose tissue to elevated serum cystatin C in human obesity. Obesity (Silver Spring). 2009;17(12):2121–6. doi: 10.1038/oby.2009.96 [DOI] [PubMed] [Google Scholar]
- 14.Lafarge JC, Naour N, Clément K, Guerre-Millo M. Cathepsins and cystatin C in atherosclerosis and obesity. Biochimie. 2010;92(11):1580–6. doi: 10.1016/j.biochi.2010.04.011 [DOI] [PubMed] [Google Scholar]
- 15.Kang SH, Cho KH, Park JW, Yoon KW, Do JY. Association of visceral fat area with chronic kidney disease and metabolic syndrome risk in the general population: analysis using multi-frequency bioimpedance. Kidney Blood Press Res. 2015;40(3):223–30. doi: 10.1159/000368498 [DOI] [PubMed] [Google Scholar]
- 16.Chen YY, Fang WH, Wang CC, Kao TW, Chang YW, Yang HF, et al. Changes of Percent Body Fat as a Useful Surrogate for Risk of Declined Renal Function. Sci Rep. 2018;8(1):17289. doi: 10.1038/s41598-018-35601-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hedblad B, Nilsson P, Engström G, Berglund G, Janzon L. Insulin resistance in non-diabetic subjects is associated with increased incidence of myocardial infarction and death. Diabet Med. 2002;19(6):470–5. doi: 10.1046/j.1464-5491.2002.00719.x [DOI] [PubMed] [Google Scholar]
- 18.Lahmann PH, Gullberg B, Olsson H, Boeing H, Berglund G, Lissner L. Birth weight is associated with postmenopausal breast cancer risk in Swedish women. Br J Cancer. 2004;91(9):1666–8. doi: 10.1038/sj.bjc.6602203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lahmann PH, Lissner L, Gullberg B, Berglund G. Differences in body fat and central adiposity between Swedes and European immigrants: the Malmö Diet and Cancer Study. Obes Res. 2000. Dec;8(9):620–31. doi: 10.1038/oby.2000.80 [DOI] [PubMed] [Google Scholar]
- 20.Lee MM, Jebb SA, Oke J, Piernas C. Reference values for skeletal muscle mass and fat mass measured by bioelectrical impedance in 390 565 UK adults. J Cachexia Sarcopenia Muscle. 2020;11(2):487–496. doi: 10.1002/jcsm.12523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larsson I, Lissner L, Samuelson G, Fors H, Lantz H, Näslund I, et al. Body composition through adult life: Swedish reference data on body composition. Eur J Clin Nutr. 2015;69(7):837–42. doi: 10.1038/ejcn.2014.268 [DOI] [PubMed] [Google Scholar]
- 22.Pero RW, Olsson A, Berglund G, Janzon L, Larsson SA, Elmståhl S. The Malmö biological bank. J Intern Med. 1993;233(1):63–7. doi: 10.1111/j.1365-2796.1993.tb00650.x [DOI] [PubMed] [Google Scholar]
- 23.Delanghe JR, Speeckaert MM. Creatinine determination according to Jaffe-what does it stand for? NDT Plus. 2011;4(2):83–6. doi: 10.1093/ndtplus/sfq211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Björk J, Grubb A, Larsson A, Hansson LO, Flodin M, Sterner G, et al. Accuracy of GFR estimating equations combining standardized cystatin C and creatinine assays: a cross-sectional study in Sweden. Clin Chem Lab Med. 2015;53(3):403–14. doi: 10.1515/cclm-2014-0578 [DOI] [PubMed] [Google Scholar]
- 25.Grubb A, Horio M, Hansson LO, Björk J, Nyman U, Flodin M, et al. Generation of a new cystatin C-based estimating equation for glomerular filtration rate by use of 7 assays standardized to the international calibrator. Clin Chem. 2014;60(7):974–86. doi: 10.1373/clinchem.2013.220707 [DOI] [PubMed] [Google Scholar]
- 26.Laucyte-Cibulskiene A, Sharma S, Christensson A, Nilsson PM. Early life factors in relation to albuminuria and estimated glomerular filtration rate based on cystatin C and creatinine in adults from a Swedish population-based cohort study. J Nephrol. 2021; 8. Epub ahead of print. doi: 10.1007/s40620-021-01159-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Björk J, Grubb A, Sterner G, Nyman U. Revised equations for estimating glomerular filtration rate based on the Lund-Malmö Study cohort. Scand J Clin Lab Invest. 2011;71(3):232–9. doi: 10.3109/00365513.2011.557086 [DOI] [PubMed] [Google Scholar]
- 28.Pottel H, Björk J, Courbebaisse M, Couzi L, Ebert N, Eriksen BO, et al. Development and Validation of a Modified Full Age Spectrum Creatinine-Based Equation to Estimate Glomerular Filtration Rate: A Cross-sectional Analysis of Pooled Data. Ann Intern Med. 2021;174(2):183–91. doi: 10.7326/M20-4366 [DOI] [PubMed] [Google Scholar]
- 29.Das SK, Mannan M, Faruque AS, Ahmed T, McIntyre HD, Al Mamun A. Effect of birth weight on adulthood renal function: A bias-adjusted meta-analytic approach. Nephrology (Carlton). 2016;21(7):547–65. doi: 10.1111/nep.12732 [DOI] [PubMed] [Google Scholar]
- 30.Naderi N, Kleine CE, Park C, Hsiung JT, Soohoo M, Tantisattamo E, et al. Obesity Paradox in Advanced Kidney Disease: From Bedside to the Bench. Prog Cardiovasc Dis. 2018;61(2):168–181. doi: 10.1016/j.pcad.2018.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kato S, Nazneen A, Nakashima Y, Razzaque MS, Nishino T, Furusu A, et al. Pathological influence of obesity on renal structural changes in chronic kidney disease. Clin Exp Nephrol. 2009;13(4):332–340. doi: 10.1007/s10157-009-0169-3 [DOI] [PubMed] [Google Scholar]
- 32.Öberg CM, Lindström M, Grubb A, Christensson A. Potential relationship between eGFRcystatin C /eGFRcreatinine -ratio and glomerular basement membrane thickness in diabetic kidney disease. Physiol Rep. 2021;9(13):e14939. doi: 10.14814/phy2.14939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grubb A. Shrunken pore syndrome—a common kidney disorder with high mortality. Diagnosis, prevalence, pathophysiology and treatment options. Clin Biochem. 2020;83:12–20. doi: 10.1016/j.clinbiochem.2020.06.002 [DOI] [PubMed] [Google Scholar]
- 34.Almén MS, Björk J, Nyman U, Lindström V, Jonsson M, Abrahamson M, et al. Shrunken Pore Syndrome Is Associated With Increased Levels of Atherosclerosis-Promoting Proteins. Kidney Int Rep. 2018;4(1):67–79. doi: 10.1016/j.ekir.2018.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmid C, Ghirlanda C, Zwimpfer C, Tschopp O, Zuellig RA, Niessen M. Cystatin C in adipose tissue and stimulation of its production by growth hormone and triiodothyronine in 3T3-L1 cells. Mol Cell Endocrinol. 2019;482:28–36. doi: 10.1016/j.mce.2018.12.004 [DOI] [PubMed] [Google Scholar]
- 36.Lemoine S, Egziabher FG, Sens F, Sophie Nguyen-Tu M, Juillard L, Dubourg L, et al. Accuracy of GFR Estimation in Obese Patients. Clinical Journal of the American Society of Nephrology. 2014;9(4):720–7. doi: 10.2215/CJN.03610413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bouquegneau A, Vidal-Petiot E, Moranne O, Mariat C, Boffa JJ, Vrtovsnik F, et al. Creatinine-based equations for the adjustment of drug dosage in an obese population. British Journal of Clinical Pharmacology. 2016;81(2):349–61. doi: 10.1111/bcp.12817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fotheringham J, Weatherley N, Kawar B, Fogarty DG, Ellam T. The body composition and excretory burden of lean, obese, and severely obese individuals has implications for the assessment of chronic kidney disease. Kidney Int. 2014;86(6):1221–8. doi: 10.1038/ki.2014.112 [DOI] [PubMed] [Google Scholar]
- 39.Stefansson VT, Schei J, Jenssen TG, Melsom T, Eriksen BO. Central obesity associates with renal hyperfiltration in the non-diabetic general population: a cross-sectional study. BMC Nephrol. 2016;17(1):172. doi: 10.1186/s12882-016-0386-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ebert N, Bevc S, Bökenkamp A, Gaillard F, Hornum M, Jager KJ, et al. Assessment of kidney function: clinical indications for measured GFR. Clinical Kidney Journal [Internet]. 2021;14(8):1861. doi: 10.1093/ckj/sfab042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang AR, George J, Levey AS, Coresh J, Grams ME, Inker LA. Performance of Glomerular Filtration Rate Estimating Equations Before and After Bariatric Surgery. Kidney Medicine [Internet]. 2020;2(6):699. doi: 10.1016/j.xkme.2020.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marra M, Sammarco R, De Lorenzo A, Iellamo F, Siervo M, Pietrobelli A, et al. Assessment of Body Composition in Health and Disease Using Bioelectrical Impedance Analysis (BIA) and Dual Energy X-Ray Absorptiometry (DXA): A Critical Overview. Contrast Media Mol Imaging. 2019;2019:3548284. doi: 10.1155/2019/3548284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Delanaye P, Melsom T, Ebert N, Bäck SE, Mariat C, Cavalier E, et al. Iohexol plasma clearance for measuring glomerular filtration rate in clinical practice and research: a review. Part 2: Why to measure glomerular filtration rate with iohexol? Clin Kidney J. 2016;9(5):700–4. doi: 10.1093/ckj/sfw071 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
eGFR equations (dependent variable) following adjustments for age. sex and centralized mean arterial pressure.
(DOCX)
Data Availability Statement
Data contain potentially identifying or sensitive patient information. The datasets generated and analysed during the current study could be extracted by sending application to the steering committee for Malmö Diet and Cancer, contact persons: the head of the committee, Olle Melander, olle.melander@med.lu.se; data manager, Anders Dahlin, anders.dahlin@med.lu.se.