Abstract
The National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) established the Burn Model System (BMS) in 1993 to improve the lives of burn survivors. The BMS program includes 1) a multicenter longitudinal database describing the functional and psychosocial recovery of burn survivors; 2) site-specific burn-related research; and 3) a knowledge dissemination component directed toward patients and providers. Output from each BMS component was analyzed. Database structure, content, and access procedures are described. Publications using the database were identified and categorized to illustrate the content area of the work. Unused areas of the database were identified for future study. Publications related to site-specific projects were cataloged. The most frequently cited articles are summarized to illustrate the scope of these projects. The effectiveness of dissemination activities was measured by quantifying website hits and information downloads. There were 25 NIDILRR-supported publications that utilized the database. These articles covered topics related to psychological outcomes, functional outcomes, community reintegration, and burn demographics. There were 172 site-specific publications; highly cited articles demonstrate a wide scope of study. For information dissemination, visits to the BMS website quadrupled between 2013 and 2014, with 124,063 downloads of educational material in 2014. The NIDILRR BMS program has played a major role in defining the course of burn recovery, and making that information accessible to the general public. The accumulating information in the database serves as a rich resource to the burn community for future study. The BMS is a model for collaborative research that is multidisciplinary and outcome focused.
The National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) established the Burn Model System (BMS) in 1993 to improve the lives of individuals following burn injuries. The BMS aims to define a comprehensive, multidisciplinary model system for the long-term care of burn survivors. BMS centers are funded to lead research into the long-term effects of burn injury and identify the continuing needs of burn survivors in areas such as functional outcome, health and rehabilitation services, and community reintegration. The BMS program includes (1) a multicenter longitudinal database describing the functional and psychosocial recovery of burn survivors; (2) site-specific burn-related research; and (3) the development of knowledge dissemination directed toward patients, providers, and the general public.
The purpose of this study is to examine the output from each BMS component during the past two decades. Now that queries into the multicenter database are open to the general public, we aim to describe the multicenter database structure and content, to describe how to access the data, and to map the database to highlight unexplored areas for future study. Past publications using the database are identified and categorized to illustrate the content area of the study. Publications related to the BMS site-specific projects are collected and cataloged to illustrate the scope of these projects. We aim to measure the effectiveness of the knowledge dissemination activities by quantifying website hits and downloads of patient education materials.
THE BMS PROGRAM
The primary aim of NIDILRR is to generate new knowledge and promote its effective use to improve the lives of individuals with disabilities. The NIDILRR was formerly known as the National Institute on Disability and Rehabilitation Research (NIDRR). The name was recently changed with the move of the entire program from the Department of Education, Office of Special Education and Rehabilitative Services, where it resided for 36 years (1978–2014), to the Department of Health and Human Services in 2014. The name change reflects the increased focus on independent living for those with disabilities. NIDILRR funds the Model System Centers Programs to conduct innovative research and provide high-quality patient care for individuals with three conditions: spinal cord injuries (Spinal Cord Injury Model System Centers Program [SCIMS] developed in the 1970s), traumatic brain injuries (Traumatic Brain Injury Model System Centers Program [TBIMS] originating in 1978), and burn injuries (Burn Model System Centers Program [BMS] starting in 1993). The focus of these programs includes processes aimed at community reintegration and return to a productive, independent life. Model system centers are characterized by multidisciplinary teams that span the complete continuum of care—from preventative, emergency, and acute care services, to rehabilitation, outpatient services, and systems that support community reintegration.
The stated priorities for each of the grant announcements and institutions that received grants at each funding cycle are listed in Table 1. Note that the Model Systems Knowledge Translation Center (MSKTC) was established in 2007 to provide scientific results and information for dissemination to clinical and consumer audiences. The MSKTC summarizes research and collaborates with the Model Systems (BMS, TBIMS, and SCIMS) to produce systematic reviews of the literature; identify health information needs; develop information resources to support the Model Systems programs; and develop other systems for sharing information. NIDILRR’s long range plan for burn injury focuses research funding on projects that address the domains of employment, community living and participation, health, and function.1
Table 1.
NIDILRR grant priorities, centers, and role by year
| Year | Priority | Centers | Role |
|---|---|---|---|
| 1994 | Develop and demonstrate a comprehensive, multidisciplinary model system of rehabilitative services for individuals with severe burns, and evaluate the efficacy of that system through the collection and analysis of uniform data | UW, Seattle | BMS |
| UTSW Medical Center, Dallas | BMS | ||
| UC, Denver | BMS, BMS database coordinating center | ||
| 1997 | Recognized the need for additional research in intervention effectiveness, functional assessment, psychosocial adjustment, rural outreach, and vocational interventions. This cycle also specified the need for a center devoted to pediatric burn care | UW, Seattle | BMS |
| UTSW Medical Center, Dallas | BMS | ||
| JHU, Baltimore | BMS | ||
| Shriners Hospital for Children (UTMB-Shriners), Galveston | Pediatric BMS | ||
| UC, Denver | BMS database coordinating center | ||
| 2002 | Priorities based on NIDRR long range plan and focus was on five major areas that included health and function, technology for access and function, employment, independent living and community integration, and associated areas; required centers to conduct no more than five research studies in burn injury rehabilitation | UW, Seattle | BMS |
| UTSW Medical Center, Dallas | BMS | ||
| JHU, Baltimore | BMS | ||
| Shriners Hospital for Children (UTMB-Shriners), Galveston | Pediatric BMS | ||
| UC, Denver | BMS database coordinating center | ||
| 2007 | Continued assessment of long-term outcomes of burn injury by enrolling at least 30 subjects per year into the national longitudinal database for BMS data; contribute to improved outcomes for individuals with burn injury by proposing two site-specific research studies, one collaborative research module project, and participating in at least one collaborative research module project. Coordination with NIDRR-funded MSKTC (established in 2007) to provide scientific results and information for dissemination to clinical and consumer audiences | UW, Seattle | BMS |
| UTSW Medical Center, Dallas | BMS | ||
| JHU, Baltimore | BMS | ||
| Shriners Hospital for Children (UTMB-Shriners), Galveston | Pediatric BMS | ||
| UC, Denver | BMS database coordinating center | ||
| 2012 | Provision of a multidisciplinary system of rehabilitation care specifically designed to meet the needs of individuals with burn injury; continued assessment of long-term outcomes of individuals with burn injury by enrolling at least 30 subjects per year into the BMS database, and collection of follow-up data on all subjects enrolled in the database at 6 months, and at 1, 2, 5, and 10 years post injury and extend the assessment to every 5 years thereafter; propose and conduct at least one, but no more than two site-specific research projects; and coordination with MSKTC | UW, Seattle | BMS database coordinating center |
| UTSW Medical Center, Dallas | BMS | ||
| Shriners Hospital for Children (UTMB-Shriners), Galveston | Pediatric BMS | ||
| Boston-Harvard Burn Injury Model System (Massachusetts General Hospital, Spaulding Rehabilitation Hospital, Shriners Hospitals for Children-Boston, Brigham and Women’s Hospital, Boston University School of Public Health) | BMS; pediatric BMS |
JHU, Johns Hopkins University; NIDILRR, National Institute on Disability, Independent Living and Rehabilitation Research; NIDRR, National Institute on Disability and Rehabilitation Research; BMS, burn model system; MSKTC, Model System Knowledge Translation Center; UC, University of Colorado; UTMB, University of Texas Medical Branch; UTSW, University of Texas Southwestern; UW, University of Washington.
THE BMS NATIONAL DATABASE
The BMS National Database collects and analyzes data on the course of recovery and outcomes of individuals who were admitted to BMS centers for acute burn care. The BMS National Database is the largest national database in the field of burns that tracks long-term outcomes. To date, this database contains information on over 5500 individuals with burn injuries including data on preinjury, injury, acute care, and rehabilitation (Table 2).2
Table 2.
Summary of burn model system longitudinal database demographics 1993–2014, n = 5519
| Adults (3496) |
Children (2023) |
|
|---|---|---|
| Mean age (range) | 43.3 years (18.0–94.4) |
7.3 years (0.1–17.9) |
| Gender | ||
| Males | 2622 (75%) | 1335 (66%) |
| Females | 874 (25%) | 688 (34%) |
| Race/ethnicity | ||
| White/Caucasian | 2377 (68%) | 606 (30%) |
| Black/African American | 524 (15%) | 262 (13%) |
| Hispanic | 385 (11%) | 1085 (54%) |
| Asian | 70 (2%) | 20 (1%) |
| Other | 140 (4%) | 50 (2%) |
| Cause of burn | ||
| Fire/flame | 2133 (61%) | 1176 (58%) |
| Grease | 315 (9%) | 83 (4%) |
| Scald | 315 (9%) | 528 (26%) |
| Electricity | 210 (6%) | 123 (6%) |
| Hot object | 175 (5%) | 63 (3%) |
| Chemical | 70 (2%) | 0 (0%) |
| Other | 278 (8%) | 50 (2%) |
| Mean hospital LOS | 28 days | 30 days |
| Mean TBSA burned | 18.6% | 33.4% |
| Mean TBSA grafted | 9.7% | 23.7% |
| Number of participants who went on to inpatient rehabilitation | 486 (14%) | 39 (2%) |
| Mean inpatient rehabilitation LOS | 24 days | 10 days |
LOS, length of stay.
Since 1994, the BMS National Database itself has gone through several changes in terms of the variables collected over the years to align with NIDILRR’s priorities (Table 1). The ability to access the data has also undergone change. In 1998, the first official policy on data sharing with outside investigators was established; and in 2012, this policy was amended whereby BMS centers, as well as outside investigators, may submit research proposals with requests for data queries to the BMS National Data and Statistical Center to perform independent research. The MSKTC maintains a list of all published articles that are supported by NIDILRR Burn Model System funding (http://www.msktc.org/publications?sys=B).
Data from the BMS National Database can be requested by completing a Data Request and Use Agreement Form, available at http://burndata.washington.edu/procedures (under the link for Standard Operating Procedure #604, External Collaboration). More information on the policies and procedures associated with accessing and using the BMS National Database can be found at: http://www.msktc.org/lib/docs/Data_Sheets_/MSKTC_SOP_Factsheet_Access_BMS_Database_3_25_14_508.pdf.
Database Inclusion/Exclusion Criteria
Enrollment in the BMS National Database requires that patients meet at least one of the following current inclusion criteria:
Burn injury greater than or equal to 10% TBSA which required surgery for at least some portion of wound closure (defined as autografting); ages 65 years and older.
Burn injury greater than or equal to 20% TBSA which required surgery for at least some portion of wound closure; ages 0 to 64 years old.
Electrical high voltage/lightning injury which required surgery for at least some portion of wound closure.
Burn injury of any size to critical area(s) (face and/or hands and/or feet) which required surgery for at least some portion of wound closure.
Eligibility is also contingent on patients meeting each of the following current criteria:
Received treatment for burn at a BMS center.
Surgery for burn wound closure within 30 days of burn injury (effective date of this criterion: August 13, 2013).
Primary burn cause includes fire/flame, scald, contact with hot object, grease, tar, chemical, hydrofluoric acid, electricity, radiation, ultra-violet light, flash burn, and other burn.
Inclusion criteria have been modified over time. Current and previous inclusion criteria can be found at http://burndata.washington.edu/standard-operating-procedures.
Data, Data Collection Points, and Data Utilization
Subjects are enrolled and data are collected from consenting subjects at the time of acute burn care hospital discharge. Preinjury information is collected by recall and demographics/clinical variables are collected by chart review. Data are collected at 6, 12, and 24 months from injury. When available, charts are also accessed for current clinical information for these intervals. Recently, the BMS National Database has been expanded to include participant follow-up every 5 years until death.3 Children require different instruments from adults for the assessment of outcomes. A full and current description of the data collected over time is available on the MSKTC website, http://burndata.washington.edu/about-the-database. All data are entered into REDCap™ (Research Electronic Data Capture) data collection software and processed by the BMS datacenter.
The instruments collected by the BMS have varied over the years. A longitudinal map of the validated instruments and BMS-specific variables collected for the database and the years that these instruments were collected is presented in Figure 1. At this time, the BMS National Database includes the following validated instruments: WeeFIM®,4 Beck Anxiety and Depression Inventories for Youth and Adult,5 Child Health Questionnaire™,6 Satisfaction with Life Scale,7 Satisfaction with Appearance Scale,8 SF369/SF1010/SF1211 (Medical Outcomes Study 36-Item Short-Form Health Survey), Patient Health Questionnaire-9,12 Burn Specific Health Scale,13 World Health Organization Disability Assessment Scale14, Jebsen-Taylor Hand Function Test,15 FIM-Moberg,16 Functional Assessment Screening Questionnaire,17 Community Integration Questionnaire,18 Brief Symptom Inventory,19 and 5-D Itch Scale.20 Furthermore, the BMS have developed additional data variables for some burn outcomes and burn-related demographics such as vocational, scar problems, inpatient and outpatient charges, insomnia, itch, therapy, distress, contractures, burn complications, amputations, as well as demographic and burn injury information (http://burndata.washington.edu/about-the-database).
Figure 1.
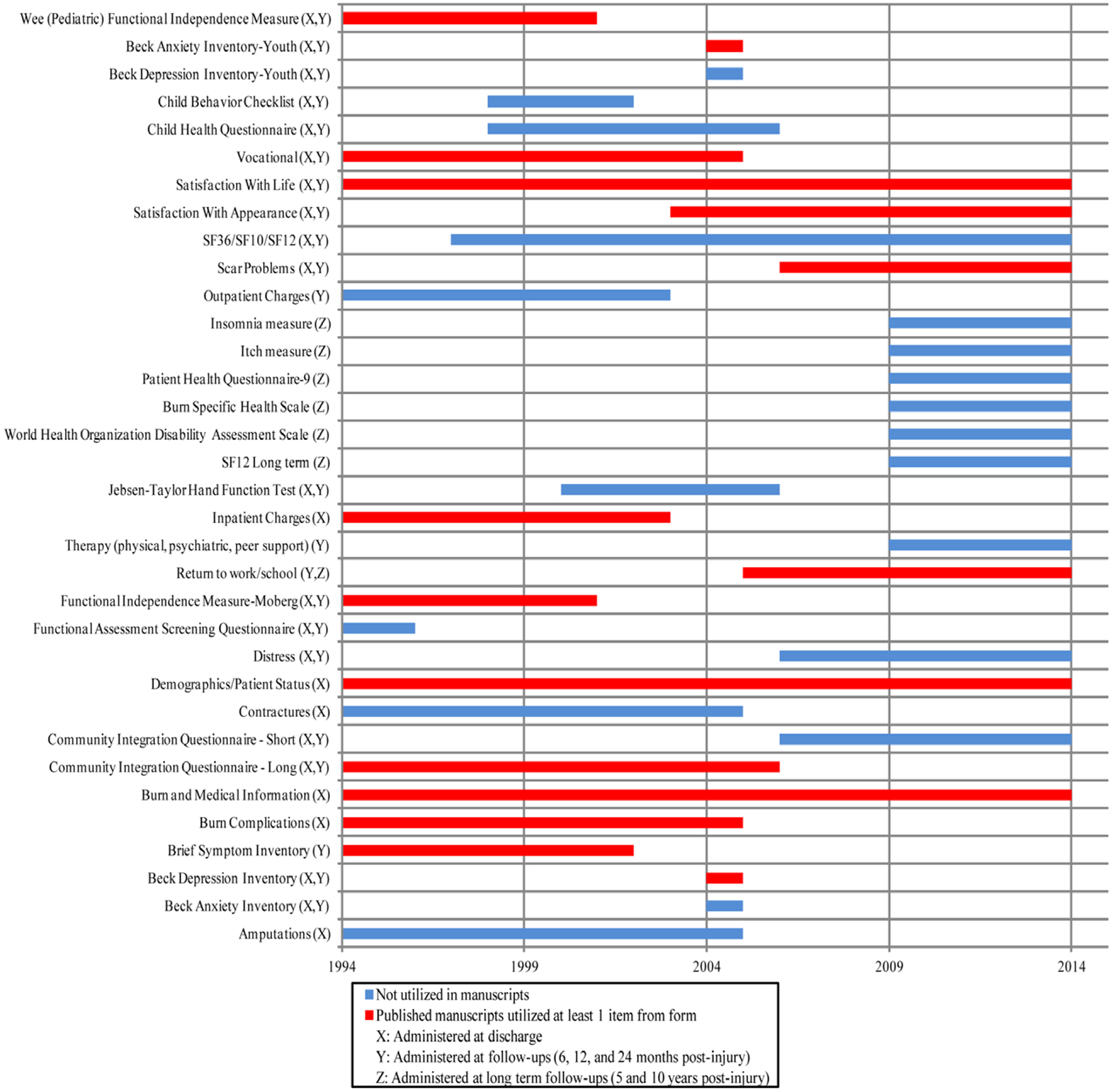
Longitudinal view of database variables.
Utilization of standardized and nonstandardized outcome measures of the BMS National Database is also presented in Figure 1. The bar beside each outcome metric represents the time period in which that metric was collected. For metrics with at least one item that was examined in a published article, the bar is colored red and for metrics that have never been published the bar is colored blue. Three instruments have been collected from the inception of the BMS National Database to present: satisfaction with life, demographics/patient status, and burn and medical information. Overall, 40.6% of outcome metrics maintained within the BMS National Database have been examined in published articles. The most frequent outcome instrument examined in the literature was the Brief Symptom Inventory (12 manuscripts). Burn/medical information and demographic/patient status variables were reported in all articles.
Data Completeness and Quality
The BMS National Data and Statistical Center, located at the University of Washington, maintains standard operating procedures to maximize completeness and quality of data (http://burndata.washington.edu/standard-operating-procedures). For example, all patients meeting the eligibility requirements are required to be approached about the study, so as to guarantee a database representative of the burn population. The NDSC has also established data quality benchmarks that include (as of October 3, 2014): at least 80% of eligible subjects are enrolled; 80% of enrolled participants complete follow-up questionnaires at all follow-up time points (6 months, 12 months, 24 months, etc.); finally, no more than 10% missing data for all variables.
As another measure of data quality, at the end of each quarter data entry for a random sample of at least 10% of questionnaires is verified by a second staff member. If any discrepancies are detected, they are corrected in the database and another 10% of questionnaires are verified. Furthermore, at the end of each quarter, the NDSC completes a missing data report and all BMS centers attempt to complete all missing data or ensure its accuracy.
Data Reporting
The BMS National Data and Statistical Center issues quarterly reports on the National Database. These reports include data on number of subjects enrolled, number of follow-ups completed, and amount of missing data. Reports are also produced that notify data collectors of subjects soon to be due for follow-ups, or follow-up windows that are soon to close. These reports serve as quality checks for the centers. Annual reports are also provided to all centers so they can track their performance in regards to the National Database benchmarks.
Database Research
The BMS National Database serves as a rich source of data and information for researchers. All abstracts listed on the NIDILRR Model System Knowledge Translation Center website for the Burn Injury Model Systems were reviewed on August 15, 2015. All manuscripts meeting inclusion criteria, by definition of using the BMS National Database, were reviewed and sorted by topic. To ensure completeness of this list, all current and former BMS centers (Dallas, TX; Galveston, TX; Seattle, WA; Baltimore, MD; Boston, MA; Denver, CO) and National Data Centers (University of Colorado Health Sciences Center, Denver, CO; University of Washington, Seattle, WA) were contacted by email and asked to compare the Translation Center list of publications to their records of publications. In addition, a PubMed search for keywords “NIDRR,” “NIDILRR,” and “Burn Model System” was performed to ensure capture of all possible BMS National Database articles.
One hundred ninety-one articles were identified through initial search of the NIDILRR Model System Knowledge Translation Center website and confirmed via PUBMED search, with six more added after individual BMS center were directly queried. Twenty-five of 197 (13%) manuscripts utilized more than one center’s data from the BMS National Database. These manuscripts were reviewed and categorized into four broad topic areas. Twelve papers described psychological outcomes,21–32 four papers reported on functional outcomes,21,22,33,34 six papers dealt with community reintegration,35–40 and five papers described burn demographics3,41–44 (Table 3). Two manuscripts were categorized into more than one topic area (psychological outcomes and functional outcomes).21,22 The manuscripts were published in eight different journals (Table 3). More than half of the articles (60%) were published in the Journal of Burn Care and Research (JBCR).
Table 3.
Publications utilizing NIDRR burn model system database organized by topic area with manuscript conclusions
| Topic | Title (Author) | Journal (Year) | Conclusion of Study |
|---|---|---|---|
| Psychological outcomes | Acute pain at discharge from hospitalization is a prospective predictor of long-term suicidal ideation after burn injury (Edwards et al.) | Archives of Physical Medicine and Rehabilitation (2007) | First findings to suggest an association between acute pain severity and the development and maintenance of suicidal ideation in burn patients23 |
| Symptoms of depression and anxiety as unique predictors of pain-related outcomes following burn injury (Edwards et al.) | Annals of Behavioral Medicine (2007) | Suggest potentially distinct effects of depression and anxiety and imply that assessment and early treatment of both depressive and anxiety symptoms may help improve a broad range of long-term pain-related outcomes following burn injury24 | |
| Psychological distress after major burn injury (Fauerbach et al.) | Psychosomatic Medicine (2007) | Clinically significant psychological distress during hospitalization for major burn injury is common and usually persistent. Thus, it is important that acute distress be understood as a marker for poor overall functional outcome post burn injuries25 | |
| Growth curve trajectories of distress in burn patients (Mason et al.) | Journal of Burn Care & Research (2010) | Psychological distress symptoms remain largely stable over time and highlight the psychological vulnerability of this patient population26 | |
| Quality-of-life loss of people admitted to burn centers, United States (Miller et al.) | Quality of Life Research (2012) | Burns cause substantial losses in quality of life, with long-term losses comparable to traumatic brain injury27 | |
| The 2000 Clinical Research Award. Describing and predicting distress and satisfaction with life for burn survivors (Patterson et al.) | Journal of Burn Care & Research (2000) | Results show the utility of biosocial models in which psychological and physical variables interact to influence adjustment and quality of life28 | |
| Rates, trends, and severity of depression after burn injuries (Wiechman et al.) | Journal of Burn Care & Research (2001) | Routine outpatient screening for depression is warranted29 | |
| Pruritus in adult burn survivors: postburn prevalence and risk factors associated with increased intensity (Carrougher et al.) | Journal of Burn Care & Research (2013) | Prevalence of burn pruritus is high, initially affecting >90% and persisting for >40% of long-term burn survivors. New predictors for postburn itch were identified to include younger age, dry skin, and raised/thick scars30 | |
| Sleep onset insomnia symptoms during hospitalization for major burn injury predict chronic pain (Smith et al.) | Pain (2008) | Highlight several risk factors for chronic pain and insomnia beyond acute injury severity, ie, sleep onset insomnia, pain severity, anxiety and depressive symptoms, which are all highly modifiable31 | |
| Pruritus in pediatric burn survivors: defining the clinical course (Schneider et al.) | Journal of Burn Care & Research (2015) | Pruritus is a frequent complication that lasts for at least 2 years after injury in a majority of pediatric burn survivors. Demonstrated a correlation between itch intensity and pain32 | |
| Burn demographics | The NIDRR burn model system database: a tool for the multicenter study of the outcome of burn injury (Klein et al.) | Journal of Burn Care & Research (2007) | The database was designed to focus on patient outcome and, therefore, provides a core of data that can be utilized in the analysis of the functional and psychosocial impact of burn injury and for the design of interventions to enhance the quality of life of burn survivors3 |
| Profile of patients lost to follow-up in the burn injury rehabilitation model systems’ longitudinal database (Holavanahalli et al.) | Journal of Burn Care & Research (2006) | Individuals who were younger, not employed at time of burn, with less than a high school level education, a history of drug abuse, circumstances of injury involving suspected assault, and having no insurance for care were lost to follow-up41 | |
| Burns as a result of assault: associated risk factors, injury characteristics, and outcomes (Kaufman et al.) | Journal of Burn Care & Research (2007) | Women and members of certain economic groups are at greater risk of being burned as a result of assault than to have nonintentional burn injuries. In addition, patients with intentional injuries have worse psychological outcomes than patients with burn injuries related to unintentional causes42 | |
| Assets and liabilities of the burn model system data model: a comparison with the National Burn Registry (Lezotte et al.) | Archives of Physical Medicine and Rehabilitation (2007) | Cohort studies examining long-term outcomes have the potential flaw of using a nonrepresentative study population. The BMS population was found to be sufficiently representative, but future analyses will require cautious and purposeful application of statistical adjustment strategies43 | |
| Assault and substance abuse characterize burn injuries in homeless patients (Kramer et al.) | Journal of Burn Care & Research (2008) | Homeless patients admitted to our burn center had a higher rate of substance abuse, mental illness, incidence of assault by burning, and longer lengths of hospital stay44 | |
| Functional outcomes | Impairment after burns: a two-center, prospective report (Costa et al.) | Burns (2003) | Recommend using the skin categories described in the fifth edition (or the most recently published version of the AMA Guide for Permanent Impairment) and including healed burn and graft sensory impairment in the skin rating32 |
| The WeeFIM Instrument - a pediatric measure of functional independence to predict longitudinal recovery of pediatric burn patients (Serghiou et al.) | Developmental Neurorehabilitation (2008) | WeeFIM can be utilized by burn centers to describe diminished functional capacity at discharge from acute care for severely burnt children. The tool can be used to track return to baseline independence after a major burn injury in a pediatric population34 | |
| Community reintegration | Time off work and return to work rates after burns: systematic review of the literature and a large two-center series (Brych et al.) | Journal of Burn Care & Research (2001) | Employment disruption after burns is significant35 |
| Community integration after burn injuries (Esselman et al.) | Journal of Burn Care & Research (2001) | Individuals with burn injuries have significant difficulties with community integration due to burn and nonburn-related factors36 | |
| Barriers to return to work after burn injuries (Esselman et al.) | Archives of Physical Medicine and Rehabilitation (2007) | Majority of patients return to work after a burn injury. Although physical and work conditions are important barriers, psychosocial issues need to be evaluated and treated to optimize return to work37 | |
| Barriers to employment among working-aged patients with major burn injury (Fauerbach et al.) | Journal of Burn Care & Research (2001) | Greater prevalence of preexisting impairments among survivors who were unemployed before the injury helps explain why preburn employment status is such a powerful determinant of postburn work outcomes, and suggests the need to include psychosocial services in a program of comprehensive rehabilitation38 | |
| Validation of the community integration questionnaire in the adult burn injury population (Gerrard et al.) | Quality of Life Research (2015) | Psychometric properties of the community integration questionnaire were examined and demonstrated validity and reliability in the adult burn survivor population39 | |
| Time to school re-entry after burn injury is quite short (Christiansen et al.) | Journal of Burn Care & Research (2007) | The time to school re-entry after discharge from the burn center is quite short. Length of hospital stay, age, and sex appear to be the most significant factors associated with time to return to school40 | |
| Multiple categories: psychological outcomes; functional outcomes | Functional and psychosocial outcomes of older adults after burn injury: results from a multicenter database of severe burn injury (Klein et al.) | Journal of Burn Care & Research (2011) | Severe burn injury significantly impacts both functional outcome and psychosocial quality of life in older adults. However, the impact seems to be age related as are recovery trajectories21 |
| The 2004 clinical research award. Burden of burn: a norm-based inquiry into the influence of burn size and distress on recovery of physical and psychosocial function (Fauerbach et al.) | Journal of Burn Care & Research (2005) | Complementing wound closure and resuscitation efforts with early interventions designed to reduce initial psychological distress may accelerate both physical and psychosocial recovery22 |
NIDRR, National Institute on Disability and Rehabilitation Research.
SITE-SPECIFIC AND OTHER COLLABORATIVE RESEARCH
In addition to contributing to the National Database, each BMS center is required to design and conduct site-specific projects. These projects do not use the database, but rather investigate a particular area of interest within the field of burns. Of the 197 total manuscripts reviewed from the NIDILRR MSKTC BMS website, 172 were based on site-specific and other collaborative projects. To ensure completeness of this list, all current and former BMS (Dallas, TX; Galveston, TX; Seattle, WA; Baltimore, MD; Boston, MA; Denver, CO) and national data centers (University of Colorado Health Sciences Center, Denver, CO; University of Washington, Seattle, WA) were contacted by email and asked to compare the Translation Center list of publications to their own records of publications.
Tables 4, 5, and 6 summarize the site-specific manuscripts. Manuscripts were reviewed and categorized into nine broad topic areas as listed in Table 4. (A complete list of site-specific articles is available in Supplemental Digital Content 1 at http://links.lww.com/BCR/A37). Fourteen manuscripts were categorized into more than one topic area. The majority of manuscripts, 70.2%, were observational studies, 21.1% were treatment studies, and 8.8% were literature reviews. A total of 66.7% of treatment studies were classified as randomized controlled trials (Table 5). Manuscripts were published in a total of 56 journals, with 31.6% of the publications in the JBCR, followed by 14.6% in Burns.
Table 4.
General topic areas of site-specific publications
| Manuscript Topics | Number of Publications |
|---|---|
| Psychology | 49 |
| Pain | 11 |
| Burn pathophysiology | 19 |
| Rehab/functional outcomes/scar | 38 |
| Hypermetabolism | 25 |
| Community integration | 4 |
| Demographics/outcome predictors | 21 |
| Translational medicine* | 18 |
| Healthcare costs | 1 |
BMS, burn model system; MSKTC, Model System Knowledge Translation Center.
A list of n = 209 publications through MSKTC’s website and other BMS centers were identified for burn database publications. Repeat articles, and the 25 publications utilizing the BMS database were excluded, resulting in n = 172 individual articles which were evaluated. Fourteen manuscripts were categorized into more than one topic area.
Basic research that can be translated into clinical utility.
Table 5.
Site-specific study types
| Type of Study | Number of Studies |
|---|---|
| Observational study | |
| Retrospective cohort | 35 |
| Prospective cohort | 29 |
| Cohort study | 28 |
| Case-control study | 20 |
| Cross-sectional study | 7 |
| Community survey | 1 |
| Time series study | 0 |
| Nested case-control study | 0 |
| Ecological study | 0 |
| Treatment study | |
| Randomized controlled trial | 24 |
| Nonrandomized trial | 6 |
| Nonblind trial | 4 |
| Double-blind randomized trial | 2 |
| Single-blind randomized trial | 0 |
| Adaptive clinical trial | 0 |
| Review study | |
| Literature review | 15 |
A complete list of the site-specific manuscripts can be found in the Supplemental Digital Content (http://links.lww.com/BCR/A37).
Table 6.
Findings and significance of the top 10 most cited site-specific papers (web of science, accessed August 24, 2015
| Topic | Title (Author/Journal) | Finding/Significance (#Citations) |
|---|---|---|
| Pain | Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study (Hoffman et al./The Clinical Journal of Pain)45 | Demonstrates the efficacy of virtual reality as a nonpharmacologic pain reduction technique during physical therapy as well as the potential for other methods of distraction in burn recovery (214 citations) |
| Burn Physiology | Pathophysiologic response to severe burn injury (Jeschke et al./Annals of Surgery)46 | Examines the pathophysiologic response to burn injury in a large prospective clinical trial which included 242 pediatric burn patients (TBSA >30%). Serum hormones and cytokine expression profile, organ function, hypermetabolism, muscle protein synthesis, incidence of wound infection sepsis, and body composition were obtained throughout acute hospital course. Hypermetabolism, muscle protein loss, lean body mass loss, bone mineral content loss, abnormal cardiac function, insulin resistance, and hyperinflammation were all clearly demonstrated to be profound post burn responses (230 citations) |
| Pain | Effectiveness of virtual reality-based pain control with multiple treatments (Hoffman et al./The Clinical Journal of Pain)47 | Provides additional evidence of the analgesic effects of virtual reality and suggests that virtual reality does not diminish in effectiveness with repeated use. These findings extend our understanding of how best to utilize virtual reality in clinical practice with acute procedure-related burn pain (202 citations) |
| Rehab/functional outcomes/scar | Burn rehabilitation: state of the science (Esselman et al./American Journal of Physical Medicine and Rehabilitation)48 | A comprehensive systematic review of 352 studies in the burn rehabilitation literature with level of evidence grading and recommendations, identifying areas of strengths and weaknesses in the burn rehabilitation literature and areas for future research (205 citations) |
| Psychology | Personality predictors of injury-related PTSD (Fauerbach et al./The Journal of Nervous and Mental Disease)49 | Demonstrates that variation in personality structure is associated with a relative susceptibility to the development of PTSD and therefore has implications as to a possible modulatory relationship between personality traits and PTSD onset (183 citations) |
| Rehab/functional outcomes/scar therapy | What is the prevalence of hypertrophic scarring following burns (Bombaro et al./Burns)50 | An investigation which revealed the lack of quality data regarding the prevalence of hypertrophic scarring after burn injuries, frequently referenced in studies looking at best practices for both treatment and prevention of hypertrophic scars (153 citations) |
| Burn pathophysiology, hypermetabolism | Burn size determines the inflammatory and hypermetabolic response (Jeschke et al./Critical Care)51 | Demonstrates that morbidity and mortality in pediatric burn patients is burn size dependent starting at 60% TBSA, and is due to increased hypermetabolic reactions, hyperinflammatory reactions, and impaired cardiac function (137 citations) |
| Burn pathophysiology | Respiratory management of inhalation injury (Mlcak et al./Burns)52 | A general review of the diagnosis and management of inhalation injury (132 citations) |
| Rehab/functional outcomes/scar | Effect of a 12-week resistance exercise program on skeletal muscle strength in children with burn injuries (Suman et al./Journal of Applied Physiology)53 | Demonstrates that participation in a resistance exercise program significantly improves muscle strength, power, and lean body mass (120 citations) |
| Psychology | The 2003 clinical research award: Visible vs. hidden scars and their relation to body esteem (Lawrence et al./Journal of Burn Care & Research)54 | Reports the results of a burn survivor questionnaire. Demonstrates a correlation between visible scarring and different aspects of body esteem. Burn scar visibility and severity did not have a strong correlation with social and emotional adjustment variables (112 citations) |
PTSD, Post traumatic stress disorder.
The NIDILRR-funded site-specific research has resulted in a significant clinical impact. To illustrate this, a brief overview of 10 of the 172 site-specific papers is presented in Table 645–54. These articles were chosen because they were the top 10 most cited manuscripts (Web of Science, August 24, 2015) in the group.
INFORMATION DISSEMINATION
All model system centers help to disseminate evidence-based information to patients, family members, educators, health-care providers, policymakers, and the general public through a variety of avenues. The centers all maintain informative websites that detail their current research as well as general information on burn injuries, support groups, and recovery. In addition, all past and present BMS centers collaborated to produce eight consumer tested fact sheets, geared toward burn patients, covering the following topics: sleep problems, psychological distress, body image, managing pain, social interactions, employment, wound care and scars, and itchy skin after burn injury. In addition, three new fact sheets have been recently developed and can be downloaded from the website (Table 7). These fact sheets are available in English and Spanish, online, and on the model system hospital floors and outpatient centers (http://www.msktc.org/burn/factsheets). Furthermore, centers produce newsletters that update patients on BMS research and center events. BMS centers regularly show a strong presence at national professional meetings, such as the American Burn Association’s Annual Meeting; for example, at the 2014 American Burn Association annual meeting in Boston, MA, 22 (7.4%) of 297 abstracts referenced their funding source as NIDILRR. Websites and social media tags are listed below.
Table 7.
Download numbers for burn injury fact sheets
| Fact Sheet | 2013 Downloads |
2014 Downloads |
|---|---|---|
| Sleep problems after burn injury | 644 | 803 |
| Psychological distress after burn injury | 2048 | 2913 |
| Understanding and improving body image after burn injury | 6024 | 8393 |
| Managing pain after burn injury | 17,240 | 25,937 |
| Social interaction after burn injury | 460 | 443 |
| Employment after burn injury | 616 | 571 |
| Wound care and scar management after burn injury | 25,588 | 38,930 |
| Itchy skin after burn injury | 39,628 | 44,721 |
| Return to school after burn injury (available 2015) | ||
| Build your child’s resilience after burn injury (available 2015) | ||
| Exercise after burn injury(available 2015) | ||
| Total | 92,248 | 122,711 |
The NIDILRR sponsored MSKTC website consists of three areas: the Burn, Spinal Cord Injury, and Traumatic Brain Injury Model Systems. The BMS section contains general information on the BMS centers, the fact sheets, and recent research. In 2013, a total of 185,170 visits were made to the MSKTC website, with 34,435 going to the Burn Injury section. In 2014, 737,855 visits were made to the MSKTC website, with 121,307 visits to the Burn Injury section. In addition, the MSKTC tracks the number of downloads of the eight fact sheets from the BMS website section. Table 7 lists the number of downloads of each fact sheet for both 2013 and 2014.
DISCUSSION
The NIDILRR BMS Program has made progress toward its goal to improve the quality of life and the course of recovery for individuals with burn injury. A large body of work has been published as a result of this program. Emerging from this data is the definition of the burn survivor as a population with specific longitudinal health care needs. This study identifies challenges that burn survivors face including, from a functional standpoint, a risk for chronic pain, pruritus, insomnia, burn/graft sensory impairment, as well as range of motion deficits. They are also at risk for psychosocial effects, such as distress, depression, anxiety, and suicidality. These functional and psychosocial effects can impair societal reintegration, and more specifically employment, education, social activities, and quality of life. Addition of the MSKTC and the dissemination components of the program have brought the research findings directly to the consumer via the Internet.
The BMS National Database is the largest of the very few multicenter datasets in the field that measures long-term multidisciplinary outcomes following burns. Opening access to the dataset (2012) and clarifying content and procedures for queries as noted in this manuscript will hopefully increase the utilization of this comprehensive dataset. Examining trajectories of recovery over time, linking to datasets such as the National Burn Registry, the Uniform Data System for Medical Rehabilitation, and the Shriners Hospitals for Children/American Burn Association Burn Outcome Data to expand the scope of the study are potential directions of research. Testing the generalizability of these results obtained from these seriously injured patients treated at a few highly specialized model system burn centers to other programs nationally and internationally is an important path for further study. Testing the generalizability of these results to smaller burns or to other disability conditions are also potential directions for future work. In addition, as the BMS National Database continues to grow, statistical models can be applied to develop population benchmark standards that could help improve patient and family-centered care. The benchmarks for recovery could be used to validate condition-specific rehabilitation methods that enhance recovery trajectories and improve outcomes. Population benchmarks could be employed not only to test the utility of new interventions or act as a performance metric but also be used on the individual level to screen a patient for deficits in their recovery during an office visit and provide them feedback on the course of their expected recovery.55 Finally, another important current and future goal is to improve the long-term follow-up of the study subjects.
Given the success of the program and the fact that the other NIDILRR-sponsored Model System programs (SCIMS and TBIMS) are much larger (ie, more centers), there is opportunity for the burn community to advocate for increased funding for the BMS to increase the number of centers. This could increase the scope of its impact commensurate with the growing need to further understand the long-term sequelae of burn injury. Deploying these research findings and patient information via the Internet to the general public has important national and international implications for the long-term care of the burn-injured patient.
The BMS will continue periodic assessment of the instruments used to collect data as part of the database in order to ensure that relevant and accurate information is obtained. In the future, the BMS is also looking to improve data collection techniques, including digitizing the process, making the questionnaires available online, and developing new instruments using computer adaptive technology such as being developed in the Life Impact Burn Recovery Evaluation project56 (http://sites.bu.edu/libre/) to measure community reintegration following burns. Such technological updates could simplify future data collection and improve data quality. Technology can also be utilized to optimize information dissemination activities, as many forms of multimedia allow information to be directly conveyed to the consumers, as well as care providers, at the national and international level. Furthermore, as BMS centers renew their funding every 5 years or as new centers are added, new and innovative site-specific projects are funded. These new projects promote progressive research in focused areas of acute burn care and rehabilitation. As new technology and techniques develop, BMS researchers launch new projects to further advance the field.
SUMMARY
Overall, the BMS has been a productive federally funded burn clinical and research program that includes one of the only longitudinal databases of burn recovery and almost 200 research projects that have impacted the field. It has served as an invaluable source of knowledge dissemination to the clinical, scientific, and burn survivor communities. The NIDILRR BMS program has played a major role in defining the course of burn recovery, and making that information accessible to the general public. The accumulating information in the database serves as a rich resource to the burn community for future study. The BMS is a model for collaborative research that is multidisciplinary and outcome focused.
Supplementary Material
Acknowledgments
The contents of this article were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR Grant Number 90DP0035). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site.
REFERENCES
- 1.National Institute on Disability and Rehabilitation Research. Long-Range Plan for Fiscal Years 2013–2017. Federal Register, Volume 78 Issue 65. Department of Education; available from http://www.gpo.gov/fdsys/pkg/FR-2013-04-04/html/2013-07879.htm; accessed 4 April 2013. [Google Scholar]
- 2.BMS National Data and Statistical Center. Burn Model System Summary Report. Burn Model Systems. 2015; available from http://burndata.washington.edu/sites/burn-data/files/files/15-1999_2014_BMS_Annual_Report_April2015.pdf; accessed 26 March 2015. [Google Scholar]
- 3.Klein MB, Lezotte DL, Fauerbach JA, et al. The National Institute on Disability and Rehabilitation Research burn model system database: a tool for the multicenter study of the outcome of burn injury. J Burn Care Res 2007;28:84–96. [DOI] [PubMed] [Google Scholar]
- 4.“UDSMR: Uniform Data System for Medical Rehabilitation.” UDSMR. UB Foundation Activities, Inc. Web. 2015; available from http://www.udsmr.org/; accessed 4 March 2015. [Google Scholar]
- 5.Professional Tools and Resources. Beck Institute for Cognitive Behavior Therapy. Beck Institute. Web; available from http://www.beckinstitute.org/beck-inventory-and-scales/; accessed 12 March 2015. [Google Scholar]
- 6.“CHQ: Child Health Questionnaire™.”. Healthactchq, Inc. Web. 2015; available from https://www.healthactchq.com/chq.php; accessed 4 March 2015. [Google Scholar]
- 7.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess 1985;49:71–5. [DOI] [PubMed] [Google Scholar]
- 8.Lawrence JW, Heinberg LJ, Roca R, et al. Development and validation of the satisfaction with appearance scale: assessing body image among burn-injured patients. Psychol Assess 1998;10:64–70. [Google Scholar]
- 9.“SF36.org.” SF36. Medical Outcomes Trust. Web; available from http://www.sf-36.org/; accessed 9 March 2015. [Google Scholar]
- 10.“SF-10 Health Survey for Children.” Optum, Inc. Web. 2015; available from https://www.optum.com/optum-outcomes/what-we-do/pediatric-health-surveys/children.html; accessed 9 March 2015. [Google Scholar]
- 11.“The SF-12®: An Even Shorter Health Survey.” SF36. Medical Outcomes Trust. Web; available from http://www.sf-36.org/tools/sf12.shtml; accessed 9 March 2015. [Google Scholar]
- 12.“Patient Health Questionnaire (PHQ) Screeners.” Pfizer, Inc. Web; available from http://www.phqscreeners.com/; accessed 11 March 2015. [Google Scholar]
- 13.Blades B, Mellis N, Munster AM. A burn specific health scale. J Trauma 1982;22:872–5. [DOI] [PubMed] [Google Scholar]
- 14.Disability Assessment Schedule WHODAS II. World Health Organization. The WHO/NIH Joint Project on Assessment and Classification of Disablements. Web. 2000; available from http://www.who.int/classifications/icf/12int.pdf; accessed 11 March 2015.
- 15.Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil 1969;50:311–9. [PubMed] [Google Scholar]
- 16.Moberg E Objective methods for determining the functional value of sensibility in the hand. J Bone Joint Surg Br 1958;40:454–76. [DOI] [PubMed] [Google Scholar]
- 17.Millard RW. The functional assessment screening questionnaire: application for evaluating pain-related disability. Arch Phys Med Rehab 1989;70:303–7. [PubMed] [Google Scholar]
- 18.Willer B, Ottenbacher KJ, Coad ML. The community integration questionnaire. A comparative examination. Am J Phys Med Rehabil 1994;73:103–11. [DOI] [PubMed] [Google Scholar]
- 19.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med 1983;13:595–605. [PubMed] [Google Scholar]
- 20.Elman S, Hynan LS, Gabriel V, Mayo MJ. The 5-D itch scale: a new measure of pruritus. Br J Dermatol 2010;162:587–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klein MB, Lezotte DC, Heltshe S, et al. Functional and psychosocial outcomes of older adults after burn injury: results from a multicenter database of severe burn injury. J Burn Care Res 2011;32:66–78. [DOI] [PubMed] [Google Scholar]
- 22.Fauerbach JA, Lezotte D, Hills RA, et al. The 2004 clinical research award. Burden of burn: a norm-based inquiry into the influence of burn size and distress on recovery of physical and psychosocial function. J Burn Care Res 2005;26:21–32. [DOI] [PubMed] [Google Scholar]
- 23.Edwards RR, Magyar-Russell G, Thombs B, et al. Acute pain at discharge from hospitalization is a prospective predictor of long-term suicidal ideation after burn injury. Arch Phys Med Rehabil 2007;88(12 suppl 2):S36–42. [DOI] [PubMed] [Google Scholar]
- 24.Edwards RR, Smith MT, Klick B, et al. Symptoms of depression and anxiety as unique predictors of pain-related outcomes following burn injury. Ann Behav Med 2007;34:313–22. [DOI] [PubMed] [Google Scholar]
- 25.Fauerbach JA, McKibben J, Bienvenu OJ, et al. Psychological distress after major burn injury. Psychosom Med 2007;69:473–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mason ST, Corry N, Gould NF, et al. Growth curve trajectories of distress in burn patients. J Burn Care Res 2010;31:64–72. [DOI] [PubMed] [Google Scholar]
- 27.Miller T, Bhattacharya S, Zamula W, et al. Quality-of-life loss of people admitted to burn centers, United States. Qual Life Res 2012:1–13. [DOI] [PubMed] [Google Scholar]
- 28.Patterson DR, Ptacek JT, Cromes F, Fauerbach JA, Engrav L. The 2000 Clinical Research Award. Describing and predicting distress and satisfaction with life for burn survivors. J Burn Care Rehabil 2000;21:490–8. [PubMed] [Google Scholar]
- 29.Wiechman SA, Ptacek JT, Patterson DR, Gibran NS, Engrav LE, Heimbach DM. Rates, trends, and severity of depression after burn injuries. J Burn Care Rehabil 2001;22:417–24. [DOI] [PubMed] [Google Scholar]
- 30.Carrougher GJ, Martinez EM, McMullen KS, et al. Pruritus in adult burn survivors: postburn prevalence and risk factors associated with increased intensity. J Burn Care Res 2013;34:94–101. [DOI] [PubMed] [Google Scholar]
- 31.Smith MT, Klick B, Kozachik S, et al. Sleep onset insomnia symptoms during hospitalization for major burn injury predict chronic pain. Pain 2008;138:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schneider JC, Nadler DL, Herndon DN, et al. Pruritus in pediatric burn survivors: defining the clinical course. J Burn Care Res 2015;36:151–8. [DOI] [PubMed] [Google Scholar]
- 33.Costa BA, Engrav LH, Holavanahalli R, et al. Impairment after burns: a two-center, prospective report. Burns 2003;29:671–5. [DOI] [PubMed] [Google Scholar]
- 34.Serghiou MH, Rose MW, Pidcock FS, et al. The WeeFIM [R] instrument–a paediatric measure of functional independence to predict longitudinal recovery of paediatric burn patients. Dev Neurorehabil 2008;11:39–50. [DOI] [PubMed] [Google Scholar]
- 35.Brych SB, Engrav LH, Rivara FP, et al. Time off work and return to work rates after burns: systematic review of the literature and a large two-center series. J Burn Care Rehabil 2001;22:401–5. [DOI] [PubMed] [Google Scholar]
- 36.Esselman PC, Ptacek JT, Kowalske K, Cromes GF, deLateur BJ, Engrav LH. Community integration after burn injuries. J Burn Care Rehabil 2001;22:221–7. [DOI] [PubMed] [Google Scholar]
- 37.Esselman PC, Askay SW, Carrougher GJ, et al. Barriers to return to work after burn injuries. Arch Phys Med Rehabil 2007;88(12 suppl 2):S50–6. [DOI] [PubMed] [Google Scholar]
- 38.Fauerbach JA, Engrav L, Kowalske K, et al. Barriers to employment among working-aged patients with major burn injury. J Burn Care Rehabil 2001;22:26–34. [DOI] [PubMed] [Google Scholar]
- 39.Gerrard P, Kazis LE, Ryan CM, et al. Validation of the community integration questionnaire in the adult burn injury population. Qual Life Res 2015;24: 1–5. [DOI] [PubMed] [Google Scholar]
- 40.Christiansen M, Carrougher GJ, Engrav LH, et al. Time to school re-entry after burn injury is quite short. J Burn Care Res 2007;28:478–81; discussion 482–3. [DOI] [PubMed] [Google Scholar]
- 41.Holavanahalli RK, Lezotte DC, Hayes MP, et al. Profile of patients lost to follow-up in the burn injury rehabilitation model systems’ longitudinal database. J Burn Care Res 2006;27:703–12. [DOI] [PubMed] [Google Scholar]
- 42.Kaufman MS, Graham CC, Lezotte D, et al. Burns as a result of assault: associated risk factors, injury characteristics, and outcomes. J Burn Care Res 2007;28:21–8; discussion 29. [DOI] [PubMed] [Google Scholar]
- 43.Lezotte DC, Hills RA, Heltshe SL, et al. Assets and liabilities of the Burn Model System data model: a comparison with the National Burn Registry. Arch Phys Med Rehabil 2007;88(12 suppl 2):S7–17. [DOI] [PubMed] [Google Scholar]
- 44.Kramer CB, Gibran NS, Heimbach DM, Rivara FP, Klein MB. Assault and substance abuse characterize burn injuries in homeless patients. J Burn Care Res 2008;29:461–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. Clin J Pain 2000;16:244–50. [DOI] [PubMed] [Google Scholar]
- 46.Jeschke MG, Chinkes DL, Finnerty CC, et al. Pathophysiologic response to severe burn injury. Ann Surg 2008;248:387–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoffman HG, Patterson DR, Carrougher GJ, Sharar SR. Effectiveness of virtual reality-based pain control with multiple treatments. Clin J Pain 2001;17:229–35. [DOI] [PubMed] [Google Scholar]
- 48.Esselman PC, Thombs BD, Magyar-Russell G, Fauerbach JA. Burn rehabilitation: state of the science. Am J Phys Med Rehabil 2006;85:383–413. [DOI] [PubMed] [Google Scholar]
- 49.Fauerbach JA, Lawrence JW, Schmidt CW Jr, Munster AM, Costa PT Jr. Personality predictors of injury-related post-traumatic stress disorder. J Nerv Ment Dis 2000;188:510–7. [DOI] [PubMed] [Google Scholar]
- 50.Bombaro KM, Engrav LH, Carrougher GJ, et al. What is the prevalence of hypertrophic scarring following burns? Burns 2003;29:299–302. [DOI] [PubMed] [Google Scholar]
- 51.Jeschke MG, Mlcak RP, Finnerty CC, et al. Burn size determines the inflammatory and hypermetabolic response. Crit Care 2007;11:R90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mlcak RP, Suman OE, Herndon DN. Respiratory management of inhalation injury. Burns 2007;33:2–13. [DOI] [PubMed] [Google Scholar]
- 53.Suman OE, Spies RJ, Celis MM, Mlcak RP, Herndon DN. Effects of a 12-wk resistance exercise program on skeletal muscle strength in children with burn injuries. J Appl Physiol (1985) 2001;91:1168–75. [DOI] [PubMed] [Google Scholar]
- 54.Lawrence JW, Fauerbach JA, Heinberg L, et al. The 2003 clinical research award: visible vs hidden scars and their relation to body esteem. J Burn Care Res 2004;25.1: 25–32. [DOI] [PubMed] [Google Scholar]
- 55.Ryan CM, Lee AF, Kazis LE, et al. Is real-time feedback of burn-specific patient-reported outcome measures (PROMs) in clinical settings practical and useful? A pilot study implementing the Young Adult Burn Outcome Questionnaire (YABOQ). J Burn Care Res 2015. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 56.Marino M, Soley Bori M, Jette A, et al. The development of a conceptual framework and item pool to measure the social impact of burns. J Burn Care Res 2015. [DOI] [PubMed] [Google Scholar]
WEBSITES AND SOCIAL MEDIA
- 1. http://www.msktc.org/publications?sys=B .
- 2. http://burndata.washington.edu/procedures .
- 3. http://www.msktc.org/lib/docs/Data_Sheets_/MSKTC_SOP_Factsheet_Access_BMS_Database_3_25_14_508.pdf .
- 4. http://burndata.washington.edu/standard-operating-procedures .
- 5.http://burndata.washington.edu/about-the-database).
- 6. http://sites.bu.edu/libre/
- 7. http://www.bh-bims.org/
- 8. http://www.utsouthwestern.edu/education/medical-school/departments/physical-medicine/ntbrms/index.html .
- 9. http://www.utmb.edu/sbhnidrr/
- 10. http://burnrehab.washington.edu/
- 11.Twitter: ; a. @BostonBurn_MS; b. @NWRBMS
- 12.Facebook: Northwest Regional Burn Model System (NWRBMS)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


