Abstract
Introduction:
Electrical injuries exhibit significant acute and long-term sequelae. Amputation and neurological deficits are common in electrical injury survivors. There is a paucity of information on the long-term outcomes of this population. Therefore, this study examines the long-term outcomes of electrical injuries by comparing them to fire/flame injuries.
Methods:
Data from the Burn Model System National Database collected between 1996 and 2015 was examined. Demographic and clinical characteristics for adult burn survivors with electrical and fire/flame injuries were compared. Satisfaction With Life Scale (SWLS), Short Form-12 Physical Composite Score (SF-12 PCS), Short Form-12 Mental Composite Score (SF-12 MCS), and employment status were examined at 24 months post-injury. Linear and logistic regression models were used to assess differences in outcome measures between groups, controlling for demographic and clinical variables.
Results:
A total of 1147 adult burn survivors (111 with electrical injuries; 1036 with fire/flame injuries) were included in this study. Persons with electrical injuries were more likely to be male and injured at work (p<0.001). SF-12 PCS scores were significantly worse for survivors with electrical injuries at 24 months post-injury than survivors with fire/flame injuries (p<0.01). Those with electrical injuries were nearly half as likely to be employed at 24 months post-injury than those with fire/flame injuries (p=0.002). There were no significant differences in SWLS and SF-12 MCS between groups.
Conclusions:
Adult survivors with electrical injuries reported worse physical health and were less likely to be employed at 24 months post-injury compared to survivors with fire/flame injuries. A more detailed understanding of return to work barriers and work accommodations is merited for the electrical injury population. Furthermore, the results of this study should inform future resource allocation for the physical health and employment needs of this population.
Keywords: Electrical injury, Electrical burns, Satisfaction with life, Patient reported outcomes, Burn rehabilitation, Employment outcomes, Return to work
1. Introduction
Electrical injury results from heat generated by a flash to the external skin, current to the internal tissues, electroporation of cell membranes, or interruption of organized electrical activity in the body such as heart rhythm or respiratory drive. An electrical arc can also cause burns through clothing ignition, trauma through acoustic blast, or other energy-related blast [1,2]. Electrical injuries are complicated by their multiple acute and long-term sequelae, with injuries often disturbing deep tissues and blood vessels due to heating of bone and muscle from the current [2,3]. The high electrical resistance of bone results in necrotic tissue surrounding bone and injured muscle [4].Necrosis of tissue, damage to nutrient arteries, and rhabdomyolysis, can lead to functional loss due to required amputation, compartment syndrome, and renal failure [1,2]. These critical deep-tissue injuries make electrical burn care particularly complex by requiring treatment for both superficial and deep sequelae [35].In addition, damage to deep tissues presents a unique set of physical complications that impact recovery.
Demographic information and short-term complications of the electrical injury population are well-documented. Electrical injuries in the U.S occur mostly in young, white, male populations [6,7]. Amputation (15%–39%) and neuropathy (11%–60%) are common complications resulting from electrical injuries [8–12]. These complications potentially affect the population’s mental and physical functioning, ability to return to work, and satisfaction with life [10]. Mental health outcomes, such as post-traumatic stress disorder and depression, are largely understudied due to small sample sizes [11,12]. Electrical injuries in combination with pre-existing comorbidities, delayed presentation of the full extent of tissue damage, open amputations with delayed wound closure, and high rehabilitation needs contribute to prolonged hospital stays [3,6,13,14]. Often more than one surgery is required for wound closure due to injury depth [5,15].
Following hospitalization, employment status serves as an important indicator of recovery. Employment is an especially relevant outcome due to large proportions of electrical injuries occurring at work [5]. Ability to return to work is a surrogate marker of overall function and is affected by psychological, neurological, and musculoskeletal sequelae following injury [16]. Three years after injury, rates of return to work among all burn etiologies are 72% [17]. However, those with electrical injuries demonstrate particular challenges in returning to work. Electrical injury survivors indicate fear of asking for or utilizing work accommodations, particularly in those seeking cognitive and psychosocial impairment accommodations [17,18]. Persons with electrical injuries, especially those with pre-injury psychological comorbidities, are more likely to exhibit chronic psychiatric complications, neuropsychological symptoms, and a decreased return to work rate [12]. Although there is significant literature on short-term complications of electrical injuries, study of the long-term outcomes beyond return to work is sparse. Significantly more data is available on the long-term complications of fire/flame injuries [19,20]. Longitudinal studies of electrical injuries are limited by single centers, small sample sizes, lack of control groups, and scarcity of outcomes examined [19–22]. A robust, multicenter examination of the electrical injury population’s long-term outcomes is needed to establish long-term outcomes and identify care needs. Therefore, the purpose of this study is to investigate the long-term outcomes associated with electrical injuries and compare them to those with fire/flame injuries.
2. Methods
2.1. Database
A retrospective study was conducted using data from the Burn Model System (BMS) National Database, funded by the National Institute on Disability, Independent Living, and Rehabilitation Research. The BMS National Database was created in 1993 as a means of exploring the long-term physical and social outcomes of burn survivors. Six burn centers in the United States have contributed to the database since its creation. [23] Data is collected at time of discharge from the acute care hospital and at 6±2, 12±3, and 24±6 months post-injury. Informed consent is obtained from all participants and each site’s oversees data collection. Participants who were burned between 1993 and 2015; age greater than or equal to 18 years at time of injury; and alive at discharge were included in this study. Using the “Main Cause of Injury — Primary Etiology” variable, participants with electrical burns and fire/flame burns were identified. Fire/flame injuries represent the majority of all burn injury etiologies; therefore, they were chosen as the comparison group. Comparing electrical injuries to fire/flame injuries allows one to consider the relative differences in outcomes between a relatively uncommon etiology (electrical) and the most common etiology (fire/flame). Additionally, many outcome measures have population-based norms, which can be used to examine the data. When applicable, population-based norms are defined in the individual outcome measure descriptions. Current criteria for enrollment in the BMS Database are those who require autografting surgery for wound closure and meet one of the following criteria:
0–64 years of age with a burn injury ≥20% total body surface area (TBSA) OR
≥65 years of age with a burn injury ≥10% TBSA OR
Any age with a burn injury to their face/neck, hands, or feet OR
Any age with a high-voltage electrical burn injury
The BMS National Database inclusion criteria have been modified since the database’s creation. Further details regarding data collection, inclusion criteria, and data sites was previously published and can be found at http://burndata.washington.edu/ [23]. The BMS National Database is a centralized database that utilizes REDCap electronic data capture tools and is housed at the BMS National Data and Statistical Center at the University of Washington [24].
2.2. Demographic and clinical characteristics
Demographic data included age, gender, race/ethnicity, marital status, highest education level, pre-injury employment status, and employment-related injury. Clinical variables included total body surface area (TBSA) burned, acute hospital length of stay, inhalation injury, ventilator days, amputation due to burn, and neuropathy. Demographic and clinical variables were collected through self-report or medical record data abstraction at discharge. A p-value less than 0.05 was considered statistically significant.
2.3. Outcome measures
The following patient reported outcome measures were used to evaluate physical health, mental health, life satisfaction, and employment status at 24 months post-injury:
2.3.1. The Short Form-12 Version 2
The Short Form-12 (SF-12) is a standardized, clinically validated evaluation of general health and capability that is frequently used in research and was created as a shortened version of the Short Form Health Survey, a 36-item health survey. [25] The SF-12 is comprised of two sub-scores: the Physical Health Composite Scale (PCS) and the Mental Health Composite Scale (MCS). PCS and MCS scores are based on the U.S. population and are standardized through t-score transformation with a mean of 50, standard deviation of 10, and a maximum score of 100 [26]. Lower PCS and MCS scores are associated with poorer physical and mental health, respectively.
2.3.2. Satisfaction With Life Scale
The Satisfaction With Life Scale (SWLS) is a validated scale comprised of 5 items regarding life satisfaction and well-being. [27] The SWLS is validated in the spinal cord, traumatic brain, and burn injury populations for use in evaluating trauma outcomes [27]. Each of the 5 items are scored on a 1–7 Likert scale, with a maximum score of 35; higher scores are associated with greater satisfaction with life.
2.3.3. Employment Status
Employment status is collapsed into three categories (working; not working; retired) and is self-reported at 24 months post-injury.
2.4. Data analysis
Descriptive statistics of the two groups were assessed. Differences between groups for demographic and clinical variables were evaluated using Chi-square tests of association and two-sample t-tests for categorical and continuous variables, respectively. In addition, univariate statistics were used to assess for differences between groups for the four outcomes. Linear regression models were used to determine if electrical injury was associated with MCS, PCS, and SWLS after adjusting for potential confounding factors. Similarly, a logistic regression model was used to determine if electrical injury was associated with employment status at 24 months post injury (in regression analyses, retired was coded as not working). Linear regression analyses utilized standardized z-scores for PCS and MCS. Both linear and logistic regression models controlled for age, gender, race/ethnicity, TBSA, inhalation injury, any days on a ventilator, and working at the time of burn injury. Although amputation and neuropathy are important variables related to electrical injury, they were excluded from the regression analyses due to their role as intermediate variables, which could introduce bias into the analyses. Intermediate variables are those that influence the evaluation of the exposure-outcome’s total causal effect, but are not defined as confounders. [28] Variables were included in the models regardless of significance. Regression diagnostics to test model assumptions were completed. In order to account for heteroskedasticity, regression models were fit using robust variance estimators.
2.5. Sensitivity analysis
A sensitivity analysis was performed to assess for selection bias by assessing for differences in follow-up rates by demographic and clinical characteristics.
3. Results
3.1. Demographics analyses
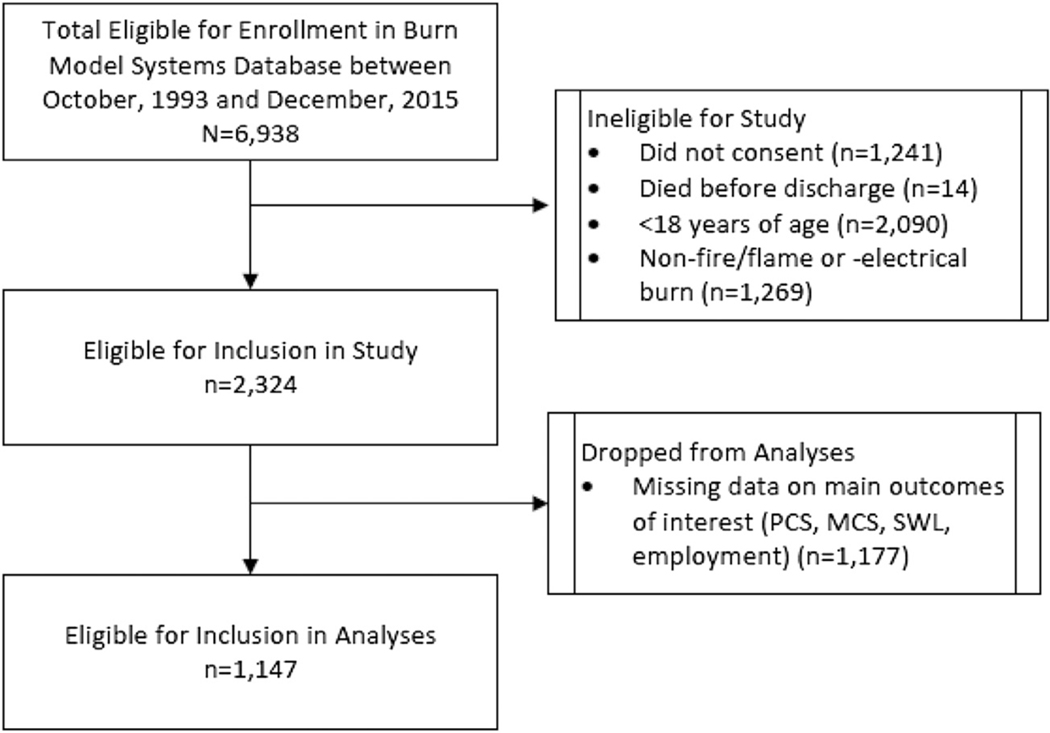
A total of 1147 subjects were included in this study; 111 with an electrical injury and 1036 with a fire/flame injury. Individuals with electrical injuries were significantly younger (electrical: 39.9±11.6 years vs. fire/flame: 43.8±16.0 years; p=0.01), more male (97.3% vs. 75.2%; p<0.001), and fewer were single compared to those with fire/flame injuries (36.3% vs. 51.8%; p=0.004). Although individuals with electrical injuries had significantly smaller burns (12.7±12.4 vs. 24.1±18.0 TBSA burned; p<0.001) and shorter acute lengths of stay (25.0±21.7 vs. 37.0±42.5 days; p=0.004) than subjects with fire/flame injuries, they were more likely to have neuropathy (16.2% vs. 7.9%; p≤0.002) and an amputation (29.4% vs. 5.7%; p<0.001). The majority of electrical injuries were sustained at work, and this was significantly different than the fire/flame injury group (88.3% vs. 17.9%; p<0.001). All demographic and clinical variables can be found in Table 1. A summary of inclusion and exclusion criteria are detailed in Fig. 1.
Table 1 -.
Demographic and clinical characteristics of the study population at discharge.
| Variable | Fire/flame injury | Electrical injury | p-value* |
|---|---|---|---|
| Number of Participants | 1036 | 111 | |
| Age, mean (SD) | 43.8 (16.0) | 39.9 (11.6) | 0.01 |
| Male, % (N) | 75.2 (779) | 97.3 (108) | <0.001 |
| Race/Ethnicity, % (N) | 0.53 | ||
| White, non-Hispanic | 76.6 (790) | 77.5 (86) | |
| Black, non-Hispanic | 10.1 (104) | 6.3 (7) | |
| Hispanic | 9.1 (94) | 11.7 (13) | |
| Other | 4.3 (44) | 4.5 (5) | |
| Single, % (N) | 51.8 (341) | 36.3 (29) | 0.004 |
| TBSA burned, mean (SD) | 24.1 (18.0) | 12.7 (12.4) | <0.0001 |
| Length of acute hospital stay in days, mean (SD) | 37.0 (42.5) | 25.0 (21.7) | 0.004 |
| Amputation, % (N) | 5.7 (56) | 29.4 (32) | <0.001 |
| Inhalation Injury, % (N) | 15.9 (162) | 0(0) | <0.001 |
| Ventilator Days, mean (SD) | 5.5 (14.4) | 3.3 (9.8) | 0.13 |
| Neuropathy, % (N) | 7.9 (49) | 16.2 (12) | 0.02 |
| Working Pre-injury, % (N) | 62.1 (641) | 94.6 (105) | <0.001 |
| Work-related burn, % (N) | 17.9 (184) | 88.3 (98) | <0.001 |
| Highest education level, % (N) | 0.10 | ||
| Less than high school | 20.0 (124) | 11.1 (8) | |
| High school diploma or GED | 58.5 (363) | 69.4 (50) | |
| Associate’s degree | 9.2 (57) | 12.5 (9) | |
| Bachelor’s degree or higher | 12.4 (77) | 6.9 (5) |
TBSA= Total body surface area.
GED= General education development.
Differences between groups were examined using chi-square tests for categorical and two-sample t-tests for continuous variables.
Fig. 1 -.
Flowchart of inclusion and exclusion criteria.
PCS=Physical Component Summary of the SF-12.
MCS=Mental Component Summary of the SF-12.
SWLS=Satisfaction With Life Scale.
3.2. Univariate analyses
Univariate analyses demonstrate a significant association between injury type and employment status, with those who sustained an electrical injury more likely to be employed at 24 months post-injury compared to those with a fire/flame injury (63% vs 49%; p≤0.002). PCS, MCS, and SWLS were not significantly different between the two groups, although PCS approached statistical significance (p=0.057) (Table 2).
Table 2 -.
Univariate analyses for PCS, MCS, and SWLS at 24 months.
| Outcome | Fire/flame injury | Electrical injury | p-value* |
|---|---|---|---|
| Employment status, % (N) | 0.001 | ||
| Employed | 49 (491) | 63 (69) | |
| Not employed | 37 (373) | 35 (38) | |
| Retired | 14 (137) | 3(3) | |
| PCS (n=617 and 62), mean (SD) | 46.13 (10.76) | 43.41 (10.42) | 0.057 |
| MCS (n=617 and 62), mean (SD) | 47.78 (12.04) | 47.88 (12.20) | 0.948 |
| SWLS (n=548 and 54), mean (SD) | 21.34 (8.56) | 21.35 (8.20) | 0.990 |
MCS=Mental component summary of the SF-12.
PCS =Physical component summary of the SF-12.
SWLS= Satisfaction With Life Scale.
Differences between groups were examined using chi-squared tests for categorical and two-sample t-tests for continuous variables.
3.3. Regression analyses
In adjusted linear regression analysis, PCS scores for electrical injuries were significantly lower for those with electrical injury at 24 months post-injury than those with fire/flame injuries (p<0.001) (Table 3). Average t-score differences for individuals with electrical injuries were 5.75 points lower on the PCS than those with fire/flame injuries. In logistic regression analysis, survivors with electrical injury had less than one half the odds of being employed at 24 months post-injury (OR=0.45) compared to those with fire/flame injuries when controlling for demographic and clinical variables (Table 4). Adjusted linear regression analysis did not exhibit significant differences in MCS by burn etiology (p=0.333) (Supplementary Table 1). Due to the poor fit of the SWLS model (F(8562)=1.41; p=0.19), the relationship between SWLS and the set of predictors was ruled statistically unreliable and the model 2 did not explain significant variance in SWLS (R2: 1.9%).
Table 3 -.
Linear regression analysis examining the association between standardized PCS score and electrical injury at 24 months, controlling for demographic and clinical variables.
| Variable | Coef. | Robust SE | t | p-value | 95% CI | |
|---|---|---|---|---|---|---|
| Electrical injury | −0.534 | 0.139 | −3.850 | <0.001 | −0.807 | −0.261 |
| Age (at time of injury) | −0.014 | 0.003 | −5.350 | <0.001 | −0.019 | −0.009 |
| Female gender | −0.083 | 0.091 | −0.920 | 0.358 | −0.262 | 0.095 |
| Not White, not Hispanic | −0.075 | 0.084 | −0.900 | 0.368 | −0.240 | 0.089 |
| TBSA burned | −0.010 | 0.003 | −3.780 | <0.001 | −0.016 | −0.005 |
| Inhalation injury | −0.079 | 0.131 | −0.600 | 0.548 | −0.337 | 0.179 |
| Any days on ventilator | −0.228 | 0.095 | −2.390 | 0.017 | −0.416 | −0.041 |
| Employed at time of burn | 0.219 | 0.091 | 2.410 | 0.016 | 0.040 | 0.397 |
| Regression constant | 1.593 | 0.303 | 5.260 | 0.000 | 0.998 | 2.188 |
PCS =Physical Component Summary of the SF-12.
TBSA=Total body surface area burned.
Table 4 -.
Logistic regression analysis examining the association between employment status and electrical injury at 24 months, controlling for demographic and clinical variables.
| Variable | OR | Std. Err. | z | p | 95% CI | |
|---|---|---|---|---|---|---|
| Electrical injury | 0.45 | 0.11 | −3.13 | 0.002 | 0.27 | 0.74 |
| Age (at time of injury) | 0.97 | 0.01 | −6.34 | <0.001 | 0.95 | 0.98 |
| Female gender | 0.66 | 0.12 | −2.21 | 0.027 | 0.46 | 0.95 |
| Not White not Hispanic | 0.73 | 0.13 | −1.83 | 0.067 | 0.51 | 1.02 |
| TBSA | 0.97 | 0.01 | −4.90 | <0.001 | 0.96 | 0.98 |
| Inhalation injury | 0.53 | 0.13 | −2.51 | 0.012 | 0.32 | 0.87 |
| Any days on ventilator | 0.60 | 0.11 | −2.71 | 0.007 | 0.42 | 0.87 |
| Employed at time of burn | 12.18 | 2.27 | 13.39 | <0.001 | 8.44 | 17.56 |
| Regression constant | 11.74 | 7.21 | 4.01 | <0.001 | 3.52 | 39.14 |
TBSA= Total body surface area.
3.4. Sensitivity analysis
At 24 months post-injury, participants that were older, (p=0.008) were white, (p=0.010) and had a larger TBSA (p=0.004) were more likely to have follow-up data. Also, those that had longer stays in the hospital (p<0.001),were working at time of injury, were married (p=0.038), and those with higher levelsof education completed were more likely to have follow-up data (p<0.001). There was no significant difference in follow-up rates by gender. This study had a loss to follow-up rate of 51%.
4. Discussion
A multi-center database of patient reported outcomes was used to compare the long-term outcomes of electrical injuries to fire/flame injuries. Results suggest that persons with electrical injuries exhibit worse physical functioning and were less likely to be employed at 24 months post-injury compared to those with fire/flame injuries. Burn survivors with electrical injuries and fire/flame injuries reported similar satisfaction with life and mental functioning scores at 24 months post-injury. This is the first study to compare the physical, mental, life satisfaction, and employment outcomes between electrical injuries and fire/flame injuries in the post-acute period.
The significant difference in PCS scores at 24 months post-injury between groups can be better contextualized through examination of a clinically significant difference in scores. Minimally clinically significant difference is defined as the smallest change of significance to a population or the smallest amount that patients distinguish as beneficial [29,30]. In populations with lower back pain, a minimally clinically significant difference in improvement for PCS scores was reported to be >3.29 points [31]. Similarly, pseudarthrosis populations described differences of 3.2–6.1 points to be clinically significant [30]. Although minimally clinically significant differences for the SF-12 PCS have not been examined in the burn population, this study’s findings are within minimally clinically significant difference ranges of other populations. This suggests that the differences in physical functioning between groups in this study, as measured by the SF-12 PCS, are statistically and clinically significant. As previously described, PCS outcomes are scored based on the U.S. population, with a mean score of 50 and a standard deviation of 10 points. In this study both fire/flame and electrical injury populations PCS scores fell below the mean score based on the U.S. population, though neither group fell outside of one standard deviation. Based on these results, both populations are at risk for physical limitations at 24-months post injury, though electrical injuries are significantly more likely to report worse functioning compared to fire/flame injuries.
Inability to return to work has a well-documented negative effect on quality of life [32]. Previous literature has described that financial difficulties and unemployment are associated with worse physical and mental functioning [32,33]. Although this study did not find differences in mental functioning between groups, failure to return to work has been associated with depression symptoms in the burn population [33]. A limitation of the BMS National Database, as well as the majority of literature examining burn employment outcomes, is the treatment of employment as a binary variable [34–36]. This variable is unable to ascertain granular details of employment outcomes that include full-time versus part-time work and need for accommodations at work. A prior systematic review of return to work outcomes found 37% of burn patients experienced no job disruption and returned to the same employer with no accommodations, displaying a more substantial level of job disruption not captured by the binary employment outcome [35]. Those with electrical injuries often exhibit difficulty in asking for and receiving accommodations upon return to work [18,22,37]. Radulovic et al. reported high rates of neuropsychological and social complications and high rates of inability to return to work in electrical injury populations regardless of voltage [38]. Given the high frequency of work related injuries in the electrical population, it is important to note that workers compensation insurance is associated with a lower rate of return to work in other injury populations [39,40]. The difference in rates of retirement between groups can be attributed to the difference in mean age of the two groups, as electrical injury survivors were significantly younger than fire/flame survivors. Additionally, significantly more electrical injury survivors were working pre-injury compared to fire/flame injuries (94.6% and 62.1%, respectively) (Table 1).
Analysis found no difference between groups regarding mental health and life satisfaction. These findings are in spite of more frequent complications in the electrical injury population that include amputation, neuropathy, and contractures [3,41,42]. It is noteworthy that both groups exhibited below average mean MCS scores, which suggests a need for long-term psychosocial support services and interventions for both groups (electrical injury, 47.88; fire/flame injury, 47.78). Burn survivors with depression symptoms had higher rates of neuropsychological complaints and psychological distress and were less likely to return to work [12]. There are limited tools available to collect data on quality of life following amputation, thus the impacts of amputations on the lives of burn survivors is not well documented [41]. Previous studies of burn survivors have suggested that physical trauma was the main factor contributing to depression, post-traumatic stress disorder, and mental functioning following a traumatic event [33,42]. A contrasting finding was observed in the examination of survivors of the Station Nightclub fire. Investigators found no significant difference in quality of life, depression, and post-traumatic stress symptoms between survivors with and without physical injury [43]. Overall, the relationship between physical impairments and mental functioning is not clearly delineated in the burn literature [43,44].
5. Limitations
This study has several limitations to consider. This study uses patient reported outcome measures and does not contain objective measures of physical functioning or more detailed aspects of employment status previously described. However, patient reported outcome measures have shown validity in both burn and non-burn populations, and are an effective method for tracking longitudinal outcomes [25,45]. Additionally, the database has selection bias, only including patients with more severe injuries. Additionally, the BMS sites that have contributed to the database are not necessarily representative of the greater burn population. However, the BMS National Database has been shown to be representative of the U.S. burn population [46]. TBSA is not necessarily the best estimate of injury severity in the electrical injury population. Additional regression analyses were examined without TBSA as a covariate and demonstrated that electrical injury was still significantly correlated with PCS and employment status outcomes, but with slightly weaker associations (PCS: p=0.003, coef=−0.41; employment status: p=0.050, OR=0.62). Although electrical injuries often require serial surgical procedures, this data has not historically been collected as part of the BMS National Database and therefore is not able to be controlled for in this analysis. Of note, loss to follow-up rates in this study were 51%. A recent study has expressed similar dropout rates in a randomized control trial of burn survivors [47]. This highlights a common issue in long-term studies of burn survivors and warrants further inquiry. While this study examined return to work, long-term changes in rates of return to work are of interest but were out of the scope of this study. Future work is planned to assess these changes over time. Lastly, variables included in the analyses were limited to variables collected in the BMS Database and therefore may not include all relevant confounding variables.
6. Conclusions
Electrical injury survivors exhibited worse physical functioning and were half as likely to be employed at 24 months post-injury when compared to fire/flame injury survivors. These results indicate that electrical injuries warrant different levels of support and rehabilitation for physical and employment outcomes over time than fire/flame injuries. In the future, more detailed examination of barriers to return to work, performance at work, and work accommodations for electrical injury survivors is needed to better inform resource allocation.
Supplementary Material
Funding source
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research, NIDILRR grant numbers 90DP0035,90DP0055, 90DPBU0001. NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS).
Footnotes
Conflict of interest
No authors have any conflicts of interest to disclose.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.burns.2019.07.030.
REFERENCES
- [1].Gille J, Schmidt T, Dragu A, Emich D, Hilbert-Carius P, Kremer T, et al. Electrical injury — a dual center analysis of patient characteristics, therapeutic specifics and outcome predictors. Scand J Trauma Resusc Emerg Med 2018; 26 (1) :1 doi: 10.1186/s13049-018-0513-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Friedstat J, Brown DA, Levi B. Chemical, electrical, and radiation injuries. Clin Plast Surg 2017;44:657–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Baldridge RR. Electric burns. N Engl J Med 1954;250:46–9 doi: 10.1056/NEJM195401142500202. [DOI] [PubMed] [Google Scholar]
- [4].Chen H, Chen Z, Wang J, Tian P, Shen Y, Huang L, et al. A successful limb salvage of an electrical burned patient with extensive soft tissue and femoral bone necrosis. J Burn Care Res 2019;40:128–32, doi: 10.1093/jbcr/irx013. [DOI] [PubMed] [Google Scholar]
- [5].Spies C RG T. Narrative review: electrocution and life-threatening electrical injuries. Ann Intern Med 2006;145:531–7 doi: 10.7326/0003-4819-145-7-200610030-00011. [DOI] [PubMed] [Google Scholar]
- [6].Maghsoudi H, Adyani Y, Ahmadian N, Maghsoudi H, Adyani Y, Ahmadian N. Electrical and lightning injuries. J Burn Care Res 2007;28:255–61, doi: 10.1097/BCR.0B013E318031A11C. [DOI] [PubMed] [Google Scholar]
- [7].Dokov W. Assessment of risk factors for death in electrical injury. Burns 2009;35:114–7, doi: 10.1016/j.burns.2008.05.005. [DOI] [PubMed] [Google Scholar]
- [8].Hussmann J, Kucan JO, Russell RC, Bradley T, Zamboni WA. Electrical injuries — morbidity, outcome and treatment rationale. Burn 1995;21:5305, doi: 10.1016/0305-4179(95)00037-C. [DOI] [PubMed] [Google Scholar]
- [9].Bailey B, Gaudreault P, Thivierge RL. Neurologic and neuropsychological symptoms during the first year after an electric shock: results of a prospective multicenter study. Am J Emerg Med 2008;26:413–8, doi: 10.1016/j.ajem.2007.06.021. [DOI] [PubMed] [Google Scholar]
- [10].Carrougher GJ, McMullen K, Mandell SP, Amtmann D, Kowalske KJ, Schneider JC, et al. Impact of burn-related amputations on return to work: findings from the burn injury model system national database. J Burn Care Res 2019;40:21–8, doi: 10.1093/jbcr/iry057. [DOI] [PubMed] [Google Scholar]
- [11].Piotrowski A, Fillet A-M, Perez P, Walkowiak P, Simon D, Corniere M-J, et al. Outcome of occupational electrical injuries among French electric company workers: a retrospective report of 311 cases, 1996–2005. Burns 2014;40:480–8 doi: 10.3248/j.burns.2013.08.008. [DOI] [PubMed] [Google Scholar]
- [12].Hahn-Ketter A, Aase DM, Paxton J, Fink JW, Kelley KM, Lee RC, et al. Psychiatric outcome over a decade after electrical injury: depression as a predictor of long-term adjustment. J Burn Care Res 2015;36:509–12, doi: 10.1097/BCR.0000000000000183. [DOI] [PubMed] [Google Scholar]
- [13].Thombs BD, Singh VA, Halonen J, Diallo A, Milner SM. The effects of preexisting medical comorbidities on mortality and length of hospital stay in acute burn injury: evidence from a national sample of 31,338 adult patients. Ann Surg 2007;245:629–34, doi: 10.1097/01.sla.0000250422.36168.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Brandão C, Vaz M, Brito IM, Ferreira B, Meireles R, Ramos S, et al. Electrical burns: a retrospective analysis over a 10-year period. Ann Burns Fire Disasters 2017;30:268–71. [PMC free article] [PubMed] [Google Scholar]
- [15].Bernal E, Arnoldo BD. Electrical injuries. In: Herndon DN, editor. Total burn care. 5th ed. . p. 396–402. [Google Scholar]
- [16].Theman K, Singerman J, Gomez M, JS F, Theman K, Singerman J, et al. Return to work after low voltage electrical injury. J Burn Care Res 2008;29:959–64, doi: 10.1097/BCR.0b013e31818b9eb6. [DOI] [PubMed] [Google Scholar]
- [17].Mason S, Esselman P, Fraser R, Schomer K, Truitt A, Johnson K, et al. Return to work after burn injury: a systematic review. J Burn Care Res 2012;33:101–9, doi: 10.1097/BCR.0b013e3182374439. [DOI] [PubMed] [Google Scholar]
- [18].Stergiou-Kita M, Mansfield E, Colantonio A. Injured workers’ perspectives on how workplace accommodations are conceptualized and delivered following electrical injuries. J Occup Rehabil 2014;24:173–88, doi: 10.1007/s10926-013-9463-8. [DOI] [PubMed] [Google Scholar]
- [19].Mazzetto-Betti KC, Amâncio ACG, Farina JA, MEPM Barros, Fonseca MCR. High-voltage electrical burn injuries: functional upper extremity assessment. Burns 2009;35:707–13, doi: 10.1016/J.BURNS.2008.10.002. [DOI] [PubMed] [Google Scholar]
- [20].Sokhal AK, Lodha KG, Kumari M, Paliwal R, Gothwal S. Clinical spectrum of electrical burns — a prospective study from the developing world. Burns 2017;43:182–9, doi: 10.1016/J.BURNS.2016.07.019. [DOI] [PubMed] [Google Scholar]
- [21].Wesner ML, Hickie J. Long-term sequelae of electrical injury.Can Fam Physician 2013;59:935–9. [PMC free article] [PubMed] [Google Scholar]
- [22].Capelli-Schellpfeffer M. Roadblocks to return to work after electrical trauma. NeuroRehabilitation 2005;20:49–52. [PubMed] [Google Scholar]
- [23].Goverman J, Mathews K, Holavanahalli RK, Vardanian A, Herndon DN, Meyer WJ, et al. The national institute on disability, independent living, and rehabilitation research Burn Model System: twenty years of contributions to clinical service and research. J Burn Care Res 2017;38:e240–53, doi: 10.1097/BCR.0000000000000361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) — a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81, doi: 10.1016/J.JBI.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Ware JE, Kosinski M, Keller SD. A 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 199634:, doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- [26].Ware J, Kosinski M, Dewey J. How to score Version 2 of the SF361 health survey. Lincoln 2000. [Google Scholar]
- [27].Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess 1985;49:71–5, doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- [28].Ananth CV, Schisterman EF. Confounding, causality, and confusion: the role of intermediate variables in interpreting observational studies in obstetrics. Am J Obstet Gynecol 2017;217:167–75, doi: 10.1016/j.ajog.2017.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Jaeschke R, Singer J, Guyatt G. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials 199010:, doi: 10.1016/01972456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- [30].Parker SL, Adogwa O, Mendenhall SK, Shau DN, Anderson WN, Cheng JS, et al. Clinical Study: determination of minimum clinically important difference (MCID) in pain, disability, and quality of life after revision fusion for symptomatic pseudoarthrosis. Spine J 2012;12:1122–8, doi: 10.3248/j.spinee.2012.10.006. [DOI] [PubMed] [Google Scholar]
- [31].Díaz-Arribas MJ, Fernández-Serrano M, Royuela A, Kovacs FM, Gallego-Izquierdo T, Ramos-Sánchez M, et al. Minimal clinically important difference in quality of life for patients with low back pain. Spine (Phila Pa 1976) 201742:, doi: 10.1097/BRS.0000000000002298. [DOI] [PubMed] [Google Scholar]
- [32].Johan Dyster-Aas, Morten Kildal, Willebrand M. Return to work and health-related quality of life after burn injury. J Rehabil Med 2007;39(7):49–55, doi: 10.2340/16501977-0005. [DOI] [PubMed] [Google Scholar]
- [33].Wiechman SA, Ptacek JT, Patterson DR, Gibran NS, Engrav LE, Heimbach DM. Rates, trends, and severity of depression after burn injuries. J Burn Care Rehabil 2001;22:417–24, doi: 10.1097/00004630-200111000-00012. [DOI] [PubMed] [Google Scholar]
- [34].Schneider JC, Bassi S, Ryan CM. Employment outcomes after burn injury: a comparison of those burned at work and those burned outside of work. J Burn Care Res 2011;32:294–301, doi: 10.1097/BCR.0b013e31820aaf56. [DOI] [PubMed] [Google Scholar]
- [35].Brych S, Engrav L, Rivara F, Ptacek J, Lezotte D, Esselman P, et al. Time off work and return to work rates after Burns: systematic review of the literature and a large two-center series. J Burn Care Rehabil 200122:, doi: 10.1097/00004630-200111000-00010. [DOI] [PubMed] [Google Scholar]
- [36].Li H, Tan J, Zhou J, Yuan Z, Zhang J, Peng Y, et al. Wound management and outcome of 595 electrical burns in a major burn center. J Surg Res 2017;214:182, doi: 10.1016/j.jss.2017.02.032. [DOI] [PubMed] [Google Scholar]
- [37].Schneider JC, Shie VL, Espinoza LF, Shapiro GD, Lee A, Acton A, et al. Original research: impact of work-related burn injury on social reintegration outcomes: a life impact burn recovery evaluation (LIBRE) study. Arch Phys Med Rehabil 2017, doi: 10.3248/j.apmr.2017.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Radulovic N, Mason SA, Rehou S, Godleski M, Jeschke MG. Acute and long-term clinical, neuropsychological and return-to-work sequelae following electrical injury: a retrospective cohort study. BMJ Open 2019;9:e025990, doi: 10.1136/bmjopen-2018-025990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].MacKenzie EJ, Morris JA Jr, Jurkovich GJ, Yasui Y, Cushing BM, Burgess AR, et al. Return to work following injury: the role of economic, social, and job-related factors. Am J Public Health 1998;88:1630–7, doi: 10.2105/AJPH.88.11.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Selvaggi G, Monstrey S, Van Landuyt K, Hamdi M, Blondeel P. Rehabilitation of burn injured patients following lightning and electrical trauma. NeuroRehabilitation 2005;20:35–42. [PubMed] [Google Scholar]
- [41].Levy N, Gillibrand W, Kola-Palmer S. Minor amputation and quality of life: is it time to give the patient a voice? Diabet Foot J 2017;20:228–34. [Google Scholar]
- [42].Idrees S, Faize FA, Akhtar M. Psychological reactions, social support, and coping styles in pakistani female burn survivors. J Burn Care Res 2017;38:e934–943, doi: 10.1097/BCR.0000000000000525. [DOI] [PubMed] [Google Scholar]
- [43].Schneider JC, Trinh N-HT, Selleck E, Fregni F, Salles SS, Ryan CM, et al. The long-term impact of physical and emotional trauma: the station nightclub fire. PLoS One 2012;7:e47339, doi: 10.1371/journal.pone.0047339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Phillips CJ, LeardMann CA, Gumbs GR, Smith B. Risk factors for posttraumatic stress disorder among deployed US male marines. BMC Psychiatry 2010;10:52, doi: 10.1186/1471-244X-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Meirte J, Van Daele U, Maertens K, Moortgat P, Deleus R, Van Loey NE. Convergent and discriminant validity of quality of life measures used in burn populations. Burns 2017;43:84–92, doi: 10.3248/j.burns.2016.07.001. [DOI] [PubMed] [Google Scholar]
- [46].Lezotte DC, Hills RA, Heltshe SL, Holavanahalli RK, Fauerbach JA, Blakeney P, et al. Original article: assets and liabilities of the Burn Model System data model: a comparison with the national burn registry. Arch Phys Med Rehabil 2007;88:S7–S17, doi: 10.3248/j.apmr.2007.09.011. [DOI] [PubMed] [Google Scholar]
- [47].Ohrtman EA, Zaninotto AL, Carvalho S, Shie VL, Leite J, Ianni CR, et al. Longitudinal clinical trial recruitment and retention challenges in the burn population: lessons learned from a trial examining a novel intervention for chronic neuropathic symptoms. J Burn Care Res 2019, doi: 10.1093/jbcr/irz084. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.