Abstract
Purpose
The COVID-19 pandemic continues to have major and long-lasting impacts on health care delivery and mental health. As health care shifted to telehealth, legislation was adjusted to expand telehealth allowances, creating a unique opportunity to elucidate outcomes. The aim of this study was to assess long-term patient and clinician satisfaction and outcomes with virtual behavioral health.
Methods
Data were obtained over 16 months from surveys to patients and clinicians receiving/providing virtual treatment. Outcomes data also were collected from medical records of adults receiving in-person and virtual behavioral health treatment. Data were summarized using descriptive statistics. Groups were compared using various chi-squared tests for categorical variables, Likert response trends over time, and conditional independence, with Wilcoxon rank-sum or Jonckheere trend test used to assess continuous variables. P-values of ≤0.05 were considered statistically significant.
Results
Patients gave high ratings to virtual treatment and indicated a preference for virtual formats. Both patient and clinician preference for virtual visits increased significantly with time, and many clinicians perceived virtual services to be equally effective to in-person. Virtual programs had higher completion rates, attendance rates, and number of treatment visits, suggesting that virtual behavioral health had equivalent or better outcomes to in-person treatment and that attitudes toward telehealth changed over time.
Conclusions
If trends found in this study continue, telehealth may emerge as a preferred option long term This is important considering the increase in mental health needs associated with the COVID-19 pandemic and the eventuality that in-person restrictions ease as the pandemic subsides.
Keywords: telehealth, telemedicine, patient and clinician satisfaction, behavioral health, COVID-19, no-shows, hybrid virtual
COVID-19 has significantly impacted the mental health of Americans and prompted major changes in behavioral health utilization.1,2 Psychological illnesses increased3,4 — both as direct and indirect products of COVID-191,5 — and symptoms worsened for patients with preexisting psychiatric illness,4,6,7 significantly increasing the need for behavioral health services. Historically, most behavioral health treatments have been conducted in-person.2 However, COVID-19 pressured health systems to incorporate telehealth options.8,9 Clinics transitioned quickly, clinicians adapted to virtual services while upholding quality of care, and the scope of insurance coverage expanded to encompass telehealth.10,11 Overall, patient and physician satisfaction for telehealth has been positive across medical specialties,11–16 which is critical given established correlations between patient satisfaction and outcomes.17–19
One field uniquely capable of adopting telehealth was behavioral health.20,21 Pre-COVID-19 studies suggested that virtual behavioral health treatment was effective and comparable to in-person care,22–30 although some patients had concerns regarding quality and privacy.31 Given the now-widespread use of telehealth for behavioral health treatment, it is imperative to assess patient and physician satisfaction with telehealth in a clinical setting across time.
The purpose of this quality-of-care study was to elucidate patient and clinician satisfaction with virtual behavioral health care delivered within an integrated health system across an extended duration. The secondary purpose was to compare outcomes between virtual and in-person mental health intensive outpatient treatment programs (IOP). IOP were targeted because they had parallel virtual and in-person options, thereby allowing comparison of virtual and in-person formats within a single program type. In contrast, partial hospitalization programs only briefly offered virtual treatment, thereby limiting the ability to compare virtual versus in-person versions of that program.
METHODS
This study design was retrospective and quantitative. Data were initially collected for internal quality purposes and included responses to surveys by clinicians and patients as well as electronic health record (EHR) characteristics. The study was deemed non-human subject research by the relevant institutional review board. Virtual visits across the behavioral health system utilized HIPAA-compliant telephone or Zoom modalities.
Study Population
The target population for the patient surveys analysis was all adult patients completing at least one virtual behavioral health visit for mental health and/or substance use treatment between May 4, 2020, and July 25, 2021, within a large integrated health system. This included all available levels of behavioral health care acuity that offered a virtual component, meaning virtual partial hospitalization programs, virtual IOP, and virtual outpatient programs. Although clinical care teams were asked to provide all eligible patients with links to the surveys, the anonymity of the survey responses precluded confirming which teams were consistently sending survey links to their patients. Further, patients could enter treatment more than once, thus potentially resulting in more than one survey submission per patient. Therefore, it is unknown which patients received the survey link and also went on to complete the survey.
The target population for the clinician survey analysis was all behavioral health clinicians providing virtual mental health and/or substance use treatment between June 2020 and May 2021. This included psychiatrists, psychologists, therapists, social workers, and other professionals providing direct virtual behavioral health care. Although all clinicians providing virtual treatment were eligible to take the survey, surveys were sent by clinical leadership and responses were anonymous. Therefore, it is unknown whether every leader consistently forwarded the survey to all of their eligible clinicians and whether all clinicians who received the survey also completed it.
The study population for the retrospective EHR analysis included all patients who started mental health IOP treatment on or after April 1, 2021, and were discharged by July 2, 2021, with data collection starting at the patient’s first completed visit. This relatively brief time period was chosen to control for temporal changes in extraneous factors such as overall treatment program quality and social/environmental variables (eg, changes to community-level COVID-19 restrictions).
Data Collection
Patient Surveys
Two surveys were used to collect patient feedback: a daily survey and a survey at discharge. Each provider could choose their own process for sending survey links, such as sending via email or via the health system’s patient portal. The daily survey asked patients to rate the quality of their treatment that day on a scale of 1 to 10. This survey was delivered to patients each day after treatment (Online Appendix A, Survey 1). The discharge survey was sent to patients after program discharge and used a Likert scale to collect feedback about ratings and preferences comparing virtual and in-person treatment (Online Appendix A, Survey 2).
Anonymous responses were collected in Microsoft Forms. Patients submitted 2479 responses to the daily survey, which could be submitted across multiple visits during treatment, and 414 responses to the discharge surveys, which were only submitted once per patient at treatment discharge for each program admission.
Clinician Surveys
Clinicians were surveyed around every 2 months (Online Appendix A, Survey 3). The clinician survey was sent via a survey link in an email from each team member’s clinical leadership 6 times between August 2020 and May 2021, and 381 responses were collected overall. The quantitative Likert scale survey was anonymous, and therefore the number of unique clinicians represented in this population across time is unknown. Assuming each clinician respondent completed no more than one survey for any individual request, unique clinician participation for each of the 6 survey time points ranged from 37 to 84 responses.
EHR Data
Retrospective patient EHR data were collected manually to assess no-show, length of stay (completed visit count within the episode of care), and program completion rates for patients enrolled in the virtual or in-person versions of equivalent mental health IOP at a single psychiatric hospital. All eligible patient records were assessed, resulting in 116 admissions to in-person mental health IOP treatment and 81 admissions to virtual mental health IOP treatment, for a total of 197 admissions across 194 unique patients (3 patients were admitted twice).
Program completion data were measured as a binary variable determined by whether the patient successfully completed the program based on clinical discharge notes (eg, “Patient completed program,” “Patient lost to follow-up”). Length of stay was measured as the number of completed visits within the episode of care. To calculate no-show rates, data included the total number of scheduled appointments, appointments attended, and appointments that were no-shows or cancelled late (ie, patient did not show up, indicated they were ill, or indicated they did not have transportation). No-show rates were calculated by dividing the total number of no-show/cancelled visits by the total number of scheduled visits.
Statistical Analyses
Descriptive statistics including frequencies, percentages, medians, and quartiles were used to summarize data. Beta regression was used to model proportion data. Chi-squared test of association was used to compare groups of categorical variables. Wilcoxon-Mann-Whitney test was used to compare groups of continuous variables. Cochran-Mantel-Haenszel chi-squared test for linear trend (M2) was used to examine trends in responses to Likert-type questions over time,32 with its accompanying Breslow-Day statistic for homogeneous association used to test conditional independence. Jonckheere-Terpstra test (Z-score) was used to assess trends in nonnormal continuous variables over time. Data were analyzed using Prism version 8.0.0 (GraphPad Sofware) and SAS 9.4 (SAS Institute Inc.) software. P-values of ≤0.05 were considered statistically significant.
RESULTS
Patient Survey Outcomes
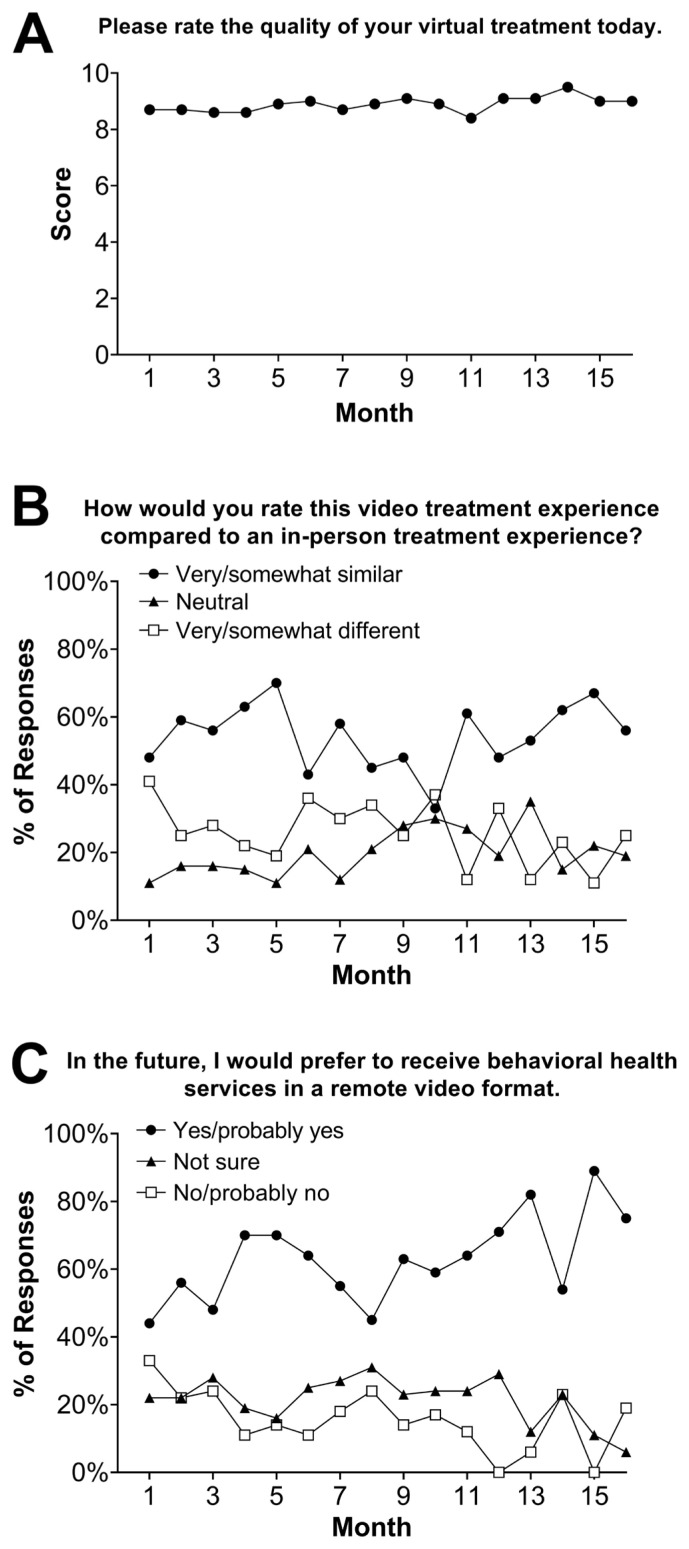
Patient daily surveys demonstrated consistently high satisfaction ratings (on 1–10 scale) across the 16-month survey period (Figure 1A). The mean rating over the study period was 8.9 out of 10. A Jonckheere-Terpstra test indicated that there was a significant upward trend in mean ratings over time (Z=5.37; P<0.0001).
Figure 1.
Patient virtual behavioral health survey responses. Virtual patient daily score submissions (Panel A) and perceptions at program discharge (Panels B and C) across time.
Across the 16-month data collection period, most discharge survey responses (53.6%) indicated that virtual treatment was very or somewhat similar to in-person treatment experiences, and there was no significant trend in the responses over the study period (M2(1)=0.51; P=0.48) (Figure 1B). Most responses (61.3%) indicated a preference for virtual treatment over in-person treatment or indicated no preference (22.4%), and there was a significant increasing trend in the data path of preference for virtual care delivery over time (M2(1)=6.63; P=0.01) (Figure 1C).
Clinician Survey Outcomes
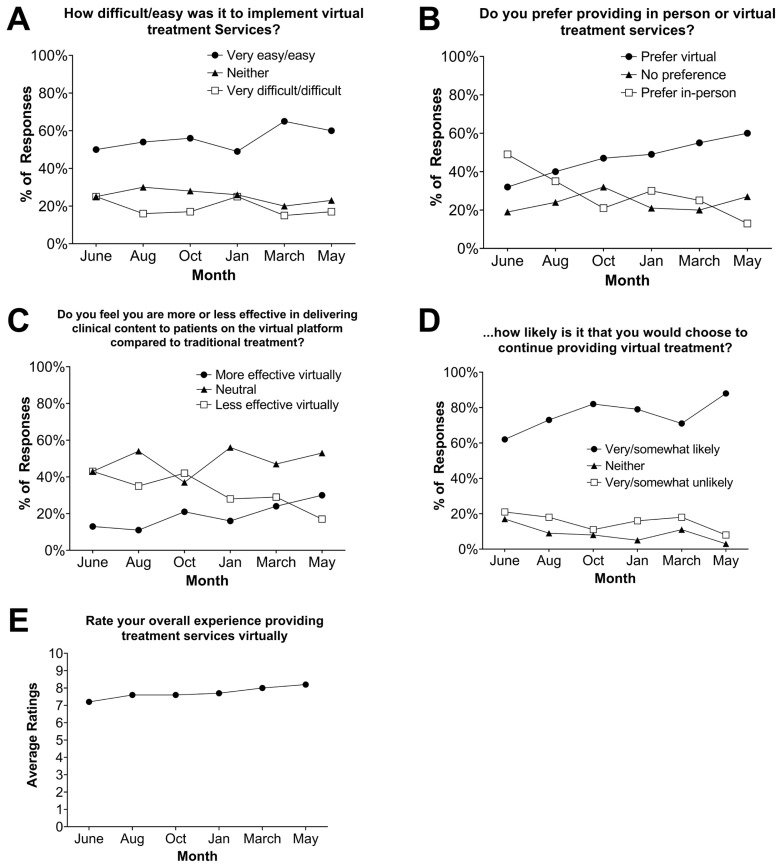
Across the study period, the majority of clinician responses (54.6%) rated virtual treatment as very easy/easy, and an additional 25.7% considered it neither easy nor difficult (Figure 2A). There was no significant trend in perception of ease of implementing virtual treatment across time (M2(1)=1.73; P=0.19). At the inception of virtual treatment in June 2020, more clinicians preferred in-person services (49.4%) compared to virtual (31.8%), yet there was a significant increasing trend of clinician preference for virtual services over time (M2(1)=21.49; P<0.0001) (Figure 2B). By the last survey period in May 2021, the majority preferred virtual services (60.0%) compared to only 13.3% who preferred in-person and 26.7% who had no preference.
Figure 2.
Aggregated clinician perceptions of virtual behavioral health treatment across time per responses to multiple survey questions (Panels A–E).
There was a significant increase in perceptions of virtual treatment effectiveness over time, from 13.1% in June 2020 to 30.0% in May 2021 (M2(1)=15.52; P<0.0001) (Figure 2C). Nearly half of clinicians perceived virtual and in-person treatments as equally effective. On average over the study period, most clinicians (74.3%) indicated they would choose to continue offering virtual treatment, with a significant upward trend from 61.2% at study inception to 88.3% at study end (M2(1)=5.77; P=0.02) (Figure 2D). Clinician ratings of their experience providing virtual treatment services were high, with a mean rating of 7.7 out of 10 and a significant upward trend over time (Z=3.84; P<0.0001) (Figure 2E).
Patient Outcomes and Demographics
Of the 197 mental health IOP patient admissions pulled from the EHR, 59.9% were female, the majority were White, and the median age was 35 years (Table 1). Groups were demographically comparable (race/ethnicity and age) except that women were significantly more likely to be in virtual treatment (69.1%) than in-person treatment (χ2(1)=4.89; P=0.03). Patients in virtual treatment had significantly higher rates of program completion (60.5%) than their in-person counterparts (44.0%) (χ2(1)=5.21; P=0.02).
Table 1.
Patient Demographics and IOP Outcomes (N=197)
| Characteristic | In-person IOP, n=116 | Virtual IOP, n=81 | P |
|---|---|---|---|
| Age in years, mean (IQR) | 35 (25.3–49.0) | 35 (24.0–46.5) | 0.78 |
| Sex, n (%) | 0.03 | ||
| Female | 62 (53.5%) | 56 (69.1%) | |
| Male | 54 (46.5%) | 25 (30.9%) | |
| Race, n (%) | 0.43 | ||
| White, not of Hispanic origin | 83 (74.1%) | 52 (70.3%) | |
| Black, not of Hispanic origin | 19 (17.0%) | 14 (18.9%) | |
| AI/AN, AAPI, multiracial, or unknown | 10 (8.9%) | 8 (10.8%) | |
| White, of Hispanic origin | 4 (3.6%) | 7 (9.5%) | |
| Attendance outcomes | |||
| Completed treatment, n (%) | 51 (44.0%) | 49 (60.5%) | 0.02 |
| Rate of no-shows or late cancellation, median (IQR) | 11.0% (0–33.0) | 6.0% (0–12.0) | 0.02 |
| Length of stay by visit count, median (IQR) | 9.5 (6.0–14.0) | 11.0 (7.0–15.0) | <0.001 |
Note: Categorical data are given as count with percentage and continuous data as median with IQR.
AI/AN, American Indian or Alaskan Native; AAPI, Asian American Pacific Islander; IQR, interquartile range; IOP, intensive outpatient treatment program.
Given that women were more likely to receive virtual treatment and the virtual treatment group was more likely to complete treatment, the degree of association was assessed between program type and treatment completion while controlling for sex. Program completion was associated with treatment type, independent of patient sex, and patients in the virtual group had almost twice the odds of completing treatment compared to their in-person counterparts regardless of sex (odds ratio: 1.98, 95% CI: 1.10–3.56).
Median visit no-shows and late cancellation rates were 6.0% for virtual admissions and 11.0% for in-person admissions (P=0.024). Again, sex had no effect on the no-show and late cancellation rates, and the virtual group was less likely to miss a scheduled visit compared to in-person (odds ratio: 0.68, 95% CI: 0.49–0.95; P=0.025). Patients who did not complete the program had significantly higher median no-shows and late cancellation rates (23%) compared to those who completed (6%) (Z=6.14; P<0.0001). Each unique patient admission in the virtual group averaged more visits (14) compared to in-person admissions (9.5) (Z=2.90; P=0.004).
DISCUSSION
Results of study data captured early in the pandemic through mid-2021 suggest patients were consistently satisfied with telehealth, which aligns with recent research.26–28,31,33,34 However, exposure to virtual treatment resulted in increased preferences for telehealth across time. These preferences likely stemmed from improved treatment access and barrier removal.26,31,35–37 In addition to patients who preferred virtual treatment, many patients had no preference between virtual and in-person options. This finding concurs with a previous study in which 83% of virtual behavioral health patients had a preference for a hybrid treatment program38 and suggests opportunities to further improve treatment using hybrid formats.36
EHR data analyses comparing virtual versus in-person mental health IOP indicated that virtual patients had significantly higher rates of attendance, number of visits, and completion of treatment, which was similar to literature correlating telehealth programs with similar or improved attendance rates39,40 and treatment outcomes.26–30,39,41 This is critical given the correlation of appropriate and planned transitions between treatment programs and lower readmission rates.42–44
Women were significantly more likely to be admitted to virtual treatment than in-person treatment, a finding similar to other studies45,46 and consistent with women’s tendency to prefer virtual care as compared to men.47 This skewing may be due to personal provider preferences, as clinicians determined program type (virtual or in-person) based on each patient’s clinical needs, as well as patient preferences. Although no data were available to assess why women were more likely to enroll in virtual treatment, previous studies suggest women may experience more barriers to travel than men. Specifically, women tend to have more family/caregiving responsibilities,48 which have increased during the pandemic,49,50 and women may be more likely than men to avoid COVID-19 exposure.51
Many clinicians were satisfied with telehealth and perceived it as effective, with that trend increasing over time. The percentage of clinicians perceiving virtual treatment as less effective early in the transition to virtual was similar to previous reports52 and consistent with data on clinicians new to virtual care reporting a desire to return to in-person.36 However, clinician satisfaction with virtual treatment increased with exposure,9,13,36 as did the desire to continue telehealth after the pandemic.9,13 Further research is needed to better understand clinicians’ experiences and preferences, as providers are an integral part of implementing telehealth services.
Limitations
Given the rapid transition to virtual care, survey questions were not validated using evidence-based questionnaire methodology. Another limitation is that surveys were anonymous. This limited the ability to differentiate responses based on acuity level, reason for treatment, or patient/provider demographics and prevented the ability to track who received the surveys or capture changes within an individual responder over time. Approximate sample sizes for the patient and clinician surveys were not able to be ascertained given the paucity of relevant population sizes, thus potentially limiting the internal validity of the results due to potential selection bias by a nonrepresentative sample of these populations. In addition, EHR data were retrospective, and therefore patient assignment to virtual/in-person programs was not randomized, as evidenced by the higher frequency of women in virtual treatment. Although analyses controlled for sex, other variables could similarly be skewed across groups, and future studies should control for this using prospective, randomized designs. Future studies also could include qualitative data to assess reasons for patient preferences and/or concerns related to virtual treatment, especially targeting previously identified concerns related to quality and privacy.31
CONCLUSIONS
The COVID-19 pandemic forced the establishment of virtual behavioral health as a treatment mechanism. This long-term study found that both behavioral health patients and clinicians perceived virtual treatment as appealing and effective. Importantly, virtual care had better attendance outcomes compared to in-person care, suggesting that virtual behavioral health treatments may be superior for some patients.
Patient-Friendly Recap
As the COVID-19 pandemic shifted more care delivery to “telehealth,” those receiving or providing treatment for mental health conditions increased their use of virtual visits.
Authors assessed changes in patient and clinician satisfaction with virtual behavioral health visits over time and also compared program attendance and completion rates for virtual versus in-person treatment.
They found that patients and clinicians both perceived virtual behavioral health treatment as appealing and effective. Moreover, the superior outcomes seen from virtual care suggest such visits should continue to be offered after the pandemic.
Supplementary Information
Footnotes
Author Contributions
Study design: Waite. Data acquisition or analysis: Waite, Adefisoye. Manuscript drafting: all authors. Critical revision: all authors.
Conflicts of Interest
None.
References
- 1.Mazza MG, De Lorenzo R, Conte C, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pierce BS, Perrin PB, Tyler CM, McKee GB, Watson JD. The COVID-19 telepsychology revolution: a national study of pandemic-based changes in U.S. mental health care delivery. Am Psychol. 2021;76:14–25. doi: 10.1037/amp0000722. [DOI] [PubMed] [Google Scholar]
- 3.MÉ Czeisler, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic – United States, June 24–30 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–57. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–42. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8:416–27. doi: 10.1016/s2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raihan MMH. Mental health consequences of COVID-19 pandemic on adult population: a systematic review. Ment Health Rev J. 2021;26:42–54. doi: 10.1108/MHRJ-07-2020-0044. [DOI] [Google Scholar]
- 7.Sher L. Post-COVID syndrome and suicide risk. QJM Mon J Assoc Physicians. 2021;114:95–8. doi: 10.1093/qjmed/hcab007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crain K, Hunt S, Schmidt RN. Adaptive telemedicine care: pre/post COVID-19 pandemic. J Bus Educ Leadersh. 2020;10:58–70. [Google Scholar]
- 9.Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett ML, Huskamp HA. Suddenly becoming a “virtual doctor”: experiences of psychiatrists transitioning to telemedicine during the COVID-19 pandemic. Psychiatr Serv. 2020;71:1143–50. doi: 10.1176/appi.ps.202000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Busch AB, Sugarman DE, Horvitz LE, Greenfield SF. Telemedicine for treating mental health and substance use disorders: reflections since the pandemic. Neuropsychopharmacology. 2021;46:1068–70. doi: 10.1038/s41386-021-00960-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prasad A, Carey RM, Rajasekaran K. Head and neck virtual medicine in a pandemic era: lessons from COVID-19. Head Neck. 2020;42:1308–9. doi: 10.1002/hed.26174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolf J, Rubin J, Bossie A, Lizcano J. Acceptance of telemedicine by kidney transplant recipients during the COVID-19 pandemic: a survey study of patient experiences. Trends Transplant. 2021;14(2):1–4. [Google Scholar]
- 13.Miner H, Fatehi A, Ring D, Reichenberg JS. Clinician telemedicine perceptions during the COVID-19 pandemic. Telemed J E Health. 2021;27:508–12. doi: 10.1089/tmj.2020.0295. [DOI] [PubMed] [Google Scholar]
- 14.Darr A, Senior A, Argyriou K, et al. The impact of the coronavirus (COVID-19) pandemic on elective paediatric otolaryngology outpatient services – an analysis of virtual outpatient clinics in a tertiary referral centre using the modified Paediatric Otolaryngology Telemedicine Satisfaction Survey (POTSS) Int J Pediatr Otorhinolaryngol. 2020;138:110383. doi: 10.1016/j.ijporl.2020.110383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morrow K. Providing quality patient care during uncertain times. Telemedicine adaption may be a silver lining in the pandemic. Podiatry Management. 2020;39(5):97–8. [Google Scholar]
- 16.Connolly SL, Miller CJ, Lindsay JA, Bauer MS. A systematic review of providers’ attitudes toward telemental health via videoconferencing. Clin Psychol Sci Pract. 2020;27(2):e12311. doi: 10.1111/cpsp.12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hser YI, Evans E, Huang D, Anglin DM. Relationship between drug treatment services, retention, and outcomes. Psychiatr Serv. 2004;55:767–74. doi: 10.1176/appi.ps.55.7.767. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs M, Briley PM, Fang X, Ellis C. Telepractice treatment for aphasia: association between clinical outcomes and client satisfaction. Telemed Rep. 2021;2:118–24. doi: 10.1089/tmr.2020.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelly SM, O’Grady KE, Brown BS, Mitchell SG, Schwartz RP. The role of patient satisfaction in methadone treatment. Am J Drug Alcohol Abuse. 2010;36:150–4. doi: 10.3109/00952991003736371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Margolis BA. Mental health care for individuals with intellectual or developmental disability (I/DD) during the time of COVID-19. [accessed November 18, 2021];Exceptional Parent. Published January 2021. https://www.epmagazine.com/blog/mental-health-care-for-individuals-with-intellectual-or-developmental-disability-idd-during-the-time-of-covid-19 . [Google Scholar]
- 21.Knopf A. Telepsychiatry coming into its own with COVID-19. The Brown University Child and Adolescent Psychopharmacology Update. 2020;22(5):1–3. doi: 10.1002/cpu.30487. [DOI] [Google Scholar]
- 22.McCrae CS, Chan WS, Curtis AF, et al. Telehealth cognitive behavioral therapy for insomnia in children with autism spectrum disorder: a pilot examining feasibility, satisfaction, and preliminary findings. Autism Int J Res Pract. 2021;25:667–80. doi: 10.1177/1362361320949078. [DOI] [PubMed] [Google Scholar]
- 23.Slightam C, Gregory AJ, Hu J, et al. Patient perceptions of video visits using Veterans Affairs telehealth tablets: survey study. J Med Internet Res. 2020;22(4):e15682. doi: 10.2196/15682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013;19:444–54. doi: 10.1089/tmj.2013.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turgoose D, Ashwick R, Murphy D. Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. J Telemed Telecare. 2018;24:575–85. doi: 10.1177/1357633x17730443. [DOI] [PubMed] [Google Scholar]
- 26.Weintraub E, Greenblatt AD, Chang J, Himelhoch S, Welsh C. Expanding access to buprenorphine treatment in rural areas with the use of telemedicine. Am J Addict. 2018;27:612–7. doi: 10.1111/ajad.12805. [DOI] [PubMed] [Google Scholar]
- 27.Weintraub E, Greenblatt AD, Chang J, et al. Outcomes for patients receiving telemedicine-delivered medication-based treatment for opioid use disorder: a retrospective chart review. Heroin Addict Relat Clin Probl. 2021;23(2):5–12. [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng W, Nickasch M, Lander L, et al. Treatment outcome comparison between telepsychiatry and face-to-face buprenorphine medication-assisted treatment for opioid use disorder: a 2-year retrospective data analysis. J Addict Med. 2017;11:138–44. doi: 10.1097/adm.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Godleski L, Darkins A, Peters J. Outcomes of 98,609 U.S. Department of Veterans Affairs patients enrolled in telemental health services, 2006–2010. Psychiatr Serv. 2012;63:383–5. doi: 10.1176/appi.ps.201100206. [DOI] [PubMed] [Google Scholar]
- 30.Varker T, Brand RM, Ward J, Terhaag S, Phelps A. Efficacy of synchronous telepsychology interventions for people with anxiety, depression, posttraumatic stress disorder, and adjustment disorder: a rapid evidence assessment. Psychol Serv. 2019;16:621–35. doi: 10.1037/ser0000239. [DOI] [PubMed] [Google Scholar]
- 31.Talal AH, McLeod A, Andrews P, et al. Patient reaction to telemedicine for clinical management of hepatitis C virus integrated into an opioid treatment program. Telemed J E Health. 2019;25:791–801. doi: 10.1089/tmj.2018.0161. [DOI] [PubMed] [Google Scholar]
- 32.Park C, Hsiung JT, Soohoo M, Streja E. [accessed August 31, 2021];Choosing wisely: Using the appropriate statistical test for trend in SAS. Published in September 2019. https://www.lexjansen.com/wuss/2019/175_Final_Paper_PDF.pdf . [Google Scholar]
- 33.Cole TO, Robinson D, Kelley-Freeman A, et al. Patient satisfaction with medications for opioid use disorder treatment via telemedicine: brief literature review and development of a new assessment. Front Public Health. 2021;8:557275. doi: 10.3389/fpubh.2020.557275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hom MA, Weiss RB, Millman ZB, et al. Development of a virtual partial hospital program for an acute psychiatric population: lessons learned and future directions for telepsychotherapy. J Psychother Integr. 2020;30:366–82. https://psycnet.apa.org/doi/10.1037/int0000212 . [Google Scholar]
- 35.Krider AE, Parker TW. COVID-19 tele-mental health: innovative use in rural behavioral health and criminal justice settings. Journal of Rural Mental Health. 2021;45:86–94. https://psycnet.apa.org/doi/10.1037/rmh0000153 . [Google Scholar]
- 36.Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett M, Huskamp HA. Treatment of opioid use disorder during COVID-19: experiences of clinicians transitioning to telemedicine. J Subst Abuse Treat. 2020;118:108124. doi: 10.1016/j.jsat.2020.108124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buchheit BM, Wheelock H, Lee A, Brandt K, Gregg J. Low-barrier buprenorphine during the COVID-19 pandemic: a rapid transition to on-demand telemedicine with wide-ranging effects. J Subst Abuse Treat. 2021;131:108444. doi: 10.1016/j.jsat.2021.108444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tse J, LaStella D, Chow E, et al. Telehealth acceptability and feasibility among people served in a community behavioral health system during the COVID-19 pandemic. Psychiatr Serv. 2021;72:654–60. doi: 10.1176/appi.ps.202000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frank HE, Grumbach NM, Conrad SM, Wheeler J, Wolff J. Mental health services in primary care: evidence for the feasibility of telehealth during the COVID-19 pandemic. J Affect Disord Rep. 2021;5:100146. doi: 10.1016/j.jadr.2021.100146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Childs AW, Klingensmith K, Bacon SM, Li L. Emergency conversion to telehealth in hospital-based psychiatric outpatient services: strategy and early observations. Psychiatry Res. 2020;293:113425. doi: 10.1016/j.psychres.2020.113425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kruse CS, Lee K, Watson JB, Lobo LG, Stoppelmoor AG, Oyibo SE. Measures of effectiveness, efficiency, and quality of telemedicine in the management of alcohol abuse, addiction, and rehabilitation: systematic review. J Med Internet Res. 2020;22(1):e13252. doi: 10.2196/13252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tan SY, Feng JY, Joyce C, Fisher J, Mostaghimi A. Association of hospital discharge against medical advice with readmission and in-hospital mortality. JAMA Netw Open. 2020;3(6):e206009. doi: 10.1001/jamanetworkopen.2020.6009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yong TY, Fok JS, Hakendorf P, Ben-Tovim D, Thompson CH, Li JY. Characteristics and outcomes of discharges against medical advice among hospitalised patients. Intern Med J. 2013;43:798–802. doi: 10.1111/imj.12109. [DOI] [PubMed] [Google Scholar]
- 44.Pages KP, Russo JE, Wingerson DK, Ries RK, Roy-Byrne PP, Cowley DS. Predictors and outcome of discharge against medical advice from the psychiatric units of a general hospital. Psychiatr Serv. 1998;49:1187–92. doi: 10.1176/ps.49.9.1187. [DOI] [PubMed] [Google Scholar]
- 45.Drake C, Lian T, Cameron B, Medynskaya K, Bosworth HB, Shah K. Understanding telemedicine’s “new normal”: variations in telemedicine use by specialty line and patient demographics. Telemed J E Health. 2022;28:51–9. doi: 10.1089/tmj.2021.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nguyen OT, Watson AK, Motwani K, et al. Patient-level factors associated with utilization of telemedicine services from a free clinic during COVID-19. Telemed J E Health. 2022;28:526–34. doi: 10.1089/tmj.2021.0102. [DOI] [PubMed] [Google Scholar]
- 47.Parker RF, Figures EL, Paddison CA, Matheson JI, Blane DN, Ford JA. Inequalities in general practice remote consultations: a systematic review. BJGP Open. 2021;5(3) doi: 10.3399/bjgpo.2021.0040. BJGPO 2021-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moreau JL, Cordasco KM, Young AS, et al. The use of telemental health to meet the mental health needs of women using Department of Veterans Affairs services. Womens Health Issues. 2018;28:181–7. doi: 10.1016/j.whi.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 49.Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice and Policy. 2020;16(1):67–73. doi: 10.1080/15487733.2020.1776561. [DOI] [Google Scholar]
- 50.Organisation for Economic Co-operation and Development (OECD) [accessed November 18, 2021];Women at the core of the fight against COVID-19 crisis. Published April 2020. https://www.oecd.org/coronavirus/policy-responses/women-at-the-core-of-the-fight-against-covid-19-crisis-553a8269/ [Google Scholar]
- 51.Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID-19 attitudes and behavior: panel evidence from eight countries. Proc Natl Acad Sci U S A. 2020;117:27285–91. doi: 10.1073/pnas.2012520117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Perle JG, Burt J, Higgins WJ. Psychologist and physician interest in telehealth training and referral for mental health services: an exploratory study. J Technol Hum Serv. 2014;32:158–85. doi: 10.1080/15228835.2014.894488. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.