Abstract
Climate change (CC) is expected to negatively impact respiratory health due to air pollution and increased aeroallergen exposure. Children are among the most vulnerable populations due to high ventilation rates, small peripheral airways, and developing respiratory and immunological systems. To assess the current knowledge among Italian pediatric pulmonologists on the potential effects of CC on pediatric respiratory allergic diseases, a national survey was launched online from February 2020 to February 2021. The members of the Italian Pediatric Respiratory Society (SIMRI) were contacted by email and 117 questionnaires were returned (response rate 16.4%). 72.6% of respondents were females, 53.8% were academic pediatricians, 42.7% had been working >10 years. Most of the participants were aware of the potential health effects of CC and stated that they had noticed an increase in the incidence (90.6%) and severity (67.5%) of allergic respiratory diseases among their patients. About 61% and 41% of participants respectively felt that there had been an increase in the number of children sensitized to pollen and molds. When applying latent class analysis to identify the features characterizing participants with greater awareness and knowledge of CC‐related health effects, two classes were identified: almost 60% of the participants were labeled as “poor knowledge” and those with greater awareness were older, had longer work experience, and were those using the Internet to gather information about CC. There is urgent need to increase pediatricians' awareness of the detrimental effects of CC on children's respiratory health and integrate them in the educational programs of healthcare professionals.
Keywords: allergic rhinitis, allergy, asthma, global warming, pollen, thunderstorm asthma
Abbreviations
- AAAAI
American Academy of Asthma, Allergy and Immunology
- ATS
American Thoracic Society
- CC
climate change
- LCA
latent class analysis
- SIMRI
Italian Pediatric Respiratory Society (Società Italiana per le Malattie Respiratorie Infantili)
1. INTRODUCTION
Global warming is an unequivocal event caused by the increasing atmospheric concentrations of pollutants and greenhouse gases, such as carbon dioxide, related to human industrial growth, which is causing huge variations in the biosphere, including long‐lasting climate change (CC) with altered precipitations, recurrent and severe heat waves, extreme weather events, droughts and frequent floods. 1 , 2 As recalled on the occasion of the 2021 United Nations Climate Change Conference, also known as COP26 (the 26th Conference of the Parties to the United Nations Framework Convention on Climate Change), 3 CC will be threatening human health significantly in the near future and is now considered as the biggest global health threat of the 21st century 4 with an estimated future increase in deaths due to cardiovascular, respiratory, and infectious diseases, favored by malnutrition, water shortage, and migrations.
In a milestone position paper, the European Respiratory Society stated that CC will cause significant respiratory morbidity related to an increase in the prevalence and exacerbation of chronic respiratory diseases and a faster decline in respiratory function. 5 Detrimental effects on respiratory health will be caused mainly by worsening air quality due to increased pollutant levels, but also by higher pollen exposure, due to the increased growth of many plants, as well as increased pollen production and earlier and lengthened pollen seasons. 6 , 7 , 8 As a consequence, pollen allergic‐patients are expected to show increased severity and duration of respiratory symptoms and a global increase in sensitization is also expected. 9
Children are disproportionately at risk of the negative impacts on their respiratory health due to the effect of CC, because of higher ventilation rates, developing respiratory and immunological systems and smaller peripheral airways. 1 , 10 A systematic search on studies assessing how health professionals and the public perceive the health issues related to CC showed a higher perception that CC is threating health among health professionals than among the public. 11 However, the evidence available on health professionals' knowledge and perception of the potential health effects of CC is limited and does not focus on pediatricians, whose role should be pivotal in correctly advising and educating their patients and families on CC issues as well as in training them on monitoring air quality in terms of pollen and pollution, to minimize exposure. 10 The health literature supporting the increasing efforts of health professionals to address CC and related health risks is also limited. 12
Notably, recent data from the Italian National Institute of Health shows that CC is already having negative impacts on the health of the Italian population. 13 Therefore, our study was aimed at evaluating the current knowledge and awareness among Italian pediatric pulmonologists on the potential effects of CC on pediatric respiratory allergic diseases, as well as on their awareness of epidemiological changes that are potentially already occurring in our country.
2. MATERIALS AND METHODS
2.1. Study design and data collection
After having reviewed the available literature on the subject, in January 2020 we created an anonymous questionnaire on the Google Forms platform: the survey comprised 21 questions and was revised and approved by a panel of senior members of the Italian Pediatric Respiratory Society (Società Italiana per le Malattie Respiratorie Infantili, SIMRI, www.simri.it), a national scientific society founded in 1995 that included 712 members during the study period (mainly primary care and academic pediatricians). The link to the survey was spread through the SIMRI newsletter in February 2020 and a reminder was sent every month till February 2021. The survey took approximately 5 min to complete, was available only for SIMRI members and consisted of close‐ended questions or multiple‐choice answers. In particular, the questionnaire was divided into two sections: the first part included questions on personal data such as age, gender, occupation/professional status, work place and experience of the participants, while the second part consisted of specific questions about their knowledge and awareness of the main potential effects of CC on heath, perception about ongoing changes to the epidemiology and severity of respiratory allergic diseases in children, CC effects on aeroallergens, and their interest in further understanding the subject (Table 1). Answering all the questions was mandatory to continue the survey, with the result that whoever completed the questionnaire had to provide all the answers, which were later collected in a database for further analysis.
Table 1.
Items included in the questionnaire
| Item | Question | Answer |
|---|---|---|
| 1 | Gender | ‐ Male |
| ‐ Female | ||
| ‐ Other | ||
| 2 | Age (years) | ‐ 25–29 |
| ‐ 30–39 | ||
| ‐ 40–49 | ||
| ‐ ≥50 | ||
| 3 | In what kind of facility do you work? | ‐ Primary care/Local hospital |
| (General care pediatricians) | ||
| ‐ University Hospital/Research Institute (Academic pediatricians) | ||
| ‐ Pediatric residency program (Students) | ||
| 4 | How long have you been doing your job? | ‐ <5 years |
| ‐ 5–9 years | ||
| ‐ ≥10 years | ||
| 5 | Do you agree with the Lancet commission statement: "Climate change represents the greatest global health threat of the 21st century"? | ‐ Partially |
| ‐ No | ||
| ‐ Yes | ||
| 6 | Are you interested in the issue of the health impacts of climate change? | ‐ Partially |
| ‐ No‐Yes | ||
| 7 | Which are the main health problems involving children as a result of climate change? | ‐ Infectious diseases carried by vectors, food, and water |
| ‐ Malnutrition | ||
| ‐ Allergic diseases | ||
| ‐ Heat stress | ||
| 8 | In your experience, have you noticed an increase in the incidence of allergic respiratory diseases in children living in urban areas compared to those living in rural areas? | ‐ Yes |
| ‐ No | ||
| ‐ I don't know | ||
| 9 | In your experience, what is the status of the incidence of allergic respiratory diseases in children? | ‐ Increased |
| ‐ Unchanged | ||
| ‐ I don't know | ||
| 10 | In your work experience, have you noticed an increase in cases of asthma and/or pollen‐induced rhinitis? | ‐ No |
| ‐ Yes, for both | ||
| ‐ Yes, for asthma only | ||
| ‐ Yes, for allergic rhinitis only | ||
| 11 | In your experience, have you noticed an increase in the severity of asthma and/or pollen‐induced rhinitis? | ‐ No |
| ‐ Yes, for both | ||
| ‐ Yes, for asthma only | ||
| ‐ Yes, for allergic rhinitis only | ||
| 12 | Do you know which pollen species are responsible for allergic respiratory diseases in the area where you work? | ‐ No |
| ‐ Yes, I consult the regional pollen calendars | ||
| ‐ Yes, but I don't consult the regional pollen calendars | ||
| 13 | In your experience have you noticed an increase in the number of children with positive allergy tests for pollen? | ‐ Yes |
| ‐ No | ||
| ‐ I don't know | ||
| 14 | In your experience, does the pollen season start earlier and last longer than in the past? | ‐ Start first |
| ‐ It starts earlier and ends later | ||
| ‐ Unchanged | ||
| ‐ I don't know | ||
| ‐ Finish later | ||
| 15 | Do you know what "thunderstorm asthma" is? | ‐ Yes |
| ‐ No | ||
| ‐ I don't know | ||
| 16 | In your experience, is it useful to warn pollen‐allergic asthmatic patients of the risks of “thunderstorm asthma”? | ‐ Yes |
| ‐ No | ||
| ‐ I don't know | ||
| 17 | In your experience have you noticed an increase in the number of children with positive allergy tests for molds? | ‐ Yes |
| ‐ No | ||
| ‐ I don't know | ||
| 18 | Do your patients' parents know the potential health effects of climate change? | ‐ Yes |
| ‐ No | ||
| 19 | Do your patients' parents want to increase their knowledge of the effects of climate change on health? | ‐ Yes |
| ‐ No | ||
| 20 | What are the update sources you consult on these issues? | ‐ Scientific papers |
| ‐ Internet | ||
| ‐ Meetings | ||
| ‐ Training courses | ||
| 21 | Would you be interested in receiving more education on health problems for children as an effect of climate change? | ‐ Yes |
| ‐ No |
2.2. Statistical analysis
The data are presented as absolute and percentage frequencies; differences of categorical variables were compared using the χ2 test. A latent class analysis (LCA) was used to discover underlying response patterns, thus allowing the identification of respondent groups with similar knowledge. The method assumes that all associations between the included variables are entirely due to the existence of distinct subpopulations called latent classes (LCs), and all variables within the LCs are assumed to be independent. The LCA was computed using the R poLCA package. 14 The variables included in the LCA concerned the pediatricians' knowledge of the subject on the basis of the answers to item n. 7 in the questionnaire: participants were asked to choose one or more between four main health problems involving children as a result of CC, including infectious diseases (Y vs. N), malnutrition (Y vs. N), allergic diseases (Y vs. N), and heat stress (Y vs. N), considering that all have been already reported as possibly related to CC in the literature. Akaike Information Criterion (AIC) 15 , 16 was computed to select the best number of classes.
A logistic regression model was used to investigate which independent variables influenced latent class membership (dependent variable). A full model was estimated including the following independent variables: gender (M vs. F), age (>50 vs. ≤50 years), type of physician (primary care pediatricians, academics, or students), increase in cases of asthma and/or rhinitis (Y vs. N), increase in the number of children with positive allergy tests for pollen (Y vs. N), work experience (<5 vs. ≥5 years), use of scientific papers for CC update (Y vs. N), use of the Internet for CC update (Y vs. N), participation in meetings for CC update (Y vs. N), participation in training courses for CC update (Y vs. N). Using a stepwise procedure based on the AIC, a reduced model was obtained. The odds ratios (ORs) and their relative 95% confidence intervals (CIs) were used to describe the strength of the associations. Class 2 was used as the reference group. The analyses were performed using R Statistical Software (version 4.0; R Foundation for Statistical Computing). A p < 0.05 was considered statistically significant.
3. RESULTS
3.1. Main results from the study cohort
At the end of the study period, 117 questionnaires were returned (response rate: 16.4%): 72.6% of the total of participants were females, and most of the participants were between 30 and 39 years of age (47%) (Table 2). 21.4% were primary care pediatricians, 53.8% were academic pediatricians, and 24.8% were students. 42.7% of the participants had been working for more than 10 years, 36.8% for less than 5 years, and 20.5% between 5 and 10 years. The majority of the participants were interested in the health impact of CC (95.7%) and 76.1% totally agreed with the recent Lancet commission definition of CC as the greatest global health threat of the 21st century. 4 About 91% of the participants said they had noticed an increase in the incidence of allergic respiratory diseases among their patients, mainly for both allergic asthma and rhinitis (70.1%), and most of them reported a higher increase in children living in urban areas compared to those living in rural areas (70.9%). Regarding symptom severity, 45.3% of the participants perceived an increase in both asthma and allergic rhinitis (12.8% for rhinitis only and 9.4% for asthma only). About 61% and 41% of participants respectively felt that there had been an increase in the number of children with positive allergy tests for pollens and molds. While 88.9% of the participants stated that they knew which pollen species are responsible for allergic respiratory diseases in their area, only 61.5% regularly consult local pollen calendars. Only 56.4% of the participants knew what “thunderstorm asthma” is, and only 25.6% stated that their patients' parents were aware of the health effects of CC. Notably, almost all the participants declared that they were interested in receiving more education on the potential health effects of CC in childhood.
Table 2.
Answers to the questionnaire among LCA classes
| All | Class 1 | Class 2 | p value | |
|---|---|---|---|---|
| 117 | 47 | 70 | ||
| Gender: Male | 32 (27.35) | 16 (34.04) | 16 (22.86) | 0.263 |
| Age | 0.022 | |||
| 25–29 | 10 (8.55) | 2 (4.26) | 8 (11.43) | |
| 30–39 | 55 (47.01) | 26 (55.32) | 29 (41.43) | |
| 40–49 | 17 (14.53) | 2 (4.26) | 15 (21.43) | |
| ≥50 | 35 (29.91) | 17 (36.17) | 18 (25.71) | |
| Work experience (years) | 0.048 | |||
| ≥10 | 50 (42.74) | 21 (44.68) | 29 (41.43) | |
| 5–9 | 24 (20.51) | 14 (29.79) | 10 (14.29) | |
| <5 | 43 (36.75) | 12 (25.53) | 31 (44.29) | |
| Type of physician | 0.102 | |||
| Primary Care pediatricians | 25 (21.37) | 10 (21.28) | 15 (21.43) | |
| Academics | 63 (53.85) | 30 (63.83) | 33 (47.14) | |
| Students | 29 (24.79) | 7 (14.89) | 22 (31.43) | |
| Do you agree with the Lancet statement "Climate change represents the greatest global health threat of the 21st century"? | 0.384 | |||
| Partially | 26 (22.22) | 9 (19.15) | 17 (24.29) | |
| No | 2 (1.71) | 0 (0.00) | 2 (2.86) | |
| Yes | 89 (76.07) | 38 (80.85) | 51 (72.86) | |
| Are you interested in the issue of the health impact of climate change? Yes | 112 (95.73) | 47 (100.00) | 65 (92.86) | 0.160 |
| In your experience, have you noticed an increase in the incidence of allergic respiratory diseases in children living in urban areas compared to those living in rural areas? | 83 (70.94) | 36 (76.60) | 47 (67.14) | 0.370 |
| In your experience, what is the status of the incidence of allergic respiratory diseases in children? | 0.247 | |||
| Increased | 106 (90.60) | 40 (85.11) | 66 (94.29) | |
| Unchanged | 8 (6.84) | 5 (10.64) | 3 (4.29) | |
| I don't know | 3 (2.56) | 2 (4.26) | 1 (1.43) | |
| In your experience, have you noticed an increase in cases of asthma and/or pollen‐induced rhinitis? | 0.883 | |||
| No | 20 (17.09) | 9 (19.15) | 11 (15.71) | |
| Yes, for both of them | 82 (70.09) | 31 (65.96) | 51 (72.86) | |
| Yes, allergic bronchial asthma only | 2 (1.71) | 1 (2.13) | 1 (1.43) | |
| Yes, allergic rhinitis only | 13 (11.11) | 6 (12.77) | 7 (10.00) | |
| In your experience, have you noticed an increase in the severity of asthma and/or pollen‐induced rhinitis? | 0.438 | |||
| No | 38 (32.48) | 15 (31.91) | 23 (32.86) | |
| Yes, for both of them | 53 (45.30) | 23 (48.94) | 30 (42.86) | |
| Yes, allergic bronchial asthma only | 11 (9.40) | 2 (4.26) | 9 (12.86) | |
| Yes, allergic rhinitis only | 15 (12.82) | 7 (14.89) | 8 (11.43) | |
| Do you know which pollen species are responsible for allergic respiratory diseases in the area where you work? | 0.482 | |||
| No | 13 (11.11) | 7 (14.89) | 6 (8.57) | |
| Yes, I consult the regional pollen calendars | 72 (61.54) | 29 (61.70) | 43 (61.43) | |
| Yes, but I don't consult the regional pollen calendars | 32 (27.35) | 11 (23.40) | 21 (30.00) | |
| In your experience have you noticed an increase in the number of children with positive allergy tests for pollen? | 71 (60.68) | 34 (72.34) | 37 (52.86) | 0.05 |
| In your experience, does the pollen season start earlier and last longer than in the past? | 0.666 | |||
| Start first | 25 (21.37) | 11 (23.40) | 14 (20.00) | |
| It starts earlier and ends later | 66 (56.41) | 27 (57.45) | 39 (55.71) | |
| Unchanged | 1 (0.85) | 0 (0.00) | 1 (1.43) | |
| I do not know | 10 (8.55) | 5 (10.64) | 5 (7.14) | |
| Finish later | 15 (12.82) | 4 (8.51) | 11 (15.71) | |
| Do you know what "thunderstorm asthma" is? | 66 (56.41) | 30 (63.83) | 36 (51.43) | 0.256 |
| In your experience, is it useful to warn pollen‐allergic asthmatic patients of the risk of “thunderstorm asthma”? | 60 (51.28) | 26 (55.32) | 34 (48.57) | 0.598 |
| In your experience have you noticed an increase in the number of children with positive allergy tests for mold? | 48 (41.03) | 23 (48.94) | 25 (35.71) | 0.217 |
| Do your patients' parents know about the potential health effects of climate change? | 30 (25.64) | 14 (29.79) | 16 (22.86) | 0.532 |
| Do your patients' parents want to increase their knowledge of the effects of climate change on health? | 86 (73.50) | 38 (80.85) | 48 (68.57) | 0.207 |
| Would you be interested in receiving more education on health problems for children as an effect of climate change? | 114 (97.44) | 47 (100.00) | 67 (95.71) | 0.400 |
| What are the update sources you consult on these issues? | ||||
| Scientific paper | 96 (82.05) | 38 (80.85) | 58 (82.86) | 0.975 |
| Internet | 73 (62.39) | 35 (74.47) | 38 (54.29) | 0.044 |
| Meeting | 74 (63.25) | 30 (63.83) | 44 (62.86) | 1.000 |
| Training course | 21 (17.95) | 9 (19.15) | 12 (17.14) | 0.975 |
Note: Bold values refer to significance for differences between the two classes (p < 0.05 was considered statistically significant).
Abbreviation: LCA, latent class analysis.
3.1.1. LCA
Figure 1 illustrates the two identified classes using the LCA. Class 1 (n = 47, 40%) was labeled as “good knowledge” and was mainly composed of subjects who recognize the potential impact of CC on infectious diseases (100%), allergic diseases (76.7), malnutrition (61.7), heat stress (55.3%). Class 2 (n = 70, 60%) was labeled as “poor knowledge” and only 4.3% and 2.9% of subjects in this group stated to be aware of the potential impact of CC on malnutrition and heat stress in children.
Figure 1.
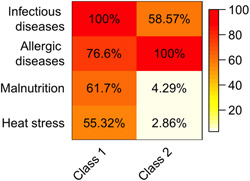
Response probabilities among the two latent classes. The figure illustrates the two classes identified by means of LCA. The proportion of each variable in each class is represented with a color scale spanning from white (0%) to red (100%). LCA, latent class analysis [Color figure can be viewed at wileyonlinelibrary.com]
3.1.2. Comparisons between LCA classes
Figure 2 reports the number of correct answers regarding the potential impact of CC on infectious and allergic diseases, malnutrition and heat stress. The subjects in Class 2 reported at most only two correct answers (p < 0.001). The subjects in Class 1 were older than those in Class 2. In addition, they had more years of work experience, noted an increase in the number of children with positive allergy tests for pollen and more frequently used the Internet to gather information about CC.
Figure 2.
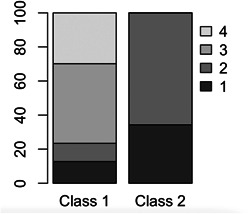
Number of correct answers to the potential impact of climate change on infectious diseases, allergic diseases, malnutrition, and heat stress
3.1.3. Multivariable analyses
The results from the logistic regression model are shown in Figure 3. Risk factors associated with membership to Class 1 when compared to Class 2 were: work experience (odds ratio [OR]: 2.528 [95% confidence interval [CI]: 1.085–6.193], reporting an increase in the number of children with positive allergy tests for pollen (OR: 2.862 [1.145–7.756]) and using the Internet to obtain information about CC (OR: 2.787 [1.207–6.782]).
Figure 3.
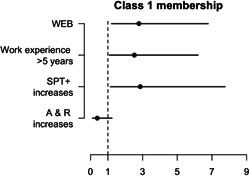
OR and 95% confidence intervals from the logistic regression for Class 1 membership. OR, odds ratio
4. DISCUSSION
To our knowledge, our study is the first to investigate the awareness of pediatricians involved in respiratory care regarding the effects of CC on allergic respiratory diseases through the application of LCA to identify features characterizing those with a higher level of awareness and knowledge of health effect of CC. A recent survey by Kotcher et al. involving the members of 12 health professional organizations around the world confirmed that health professionals have at least a basic understanding of CC, and most of the participants reported that CC had already adversely affected the health of people in their nation in various ways, to either a moderate or a great extent. 17 When compared to a previous similar survey performed on 66 academic pediatricians with a known interest in environmental health, who were members of the Academic Pediatric Association, 18 our study shows similar rates of respondents who were aware of CC, its potential health effects and were keen to learn more on the topic. However, our study adds data from pediatricians with a special interest in childhood respiratory health, reporting changes in the epidemiology of allergies already occurring in our country, such as an increase in incidence and severity of allergic asthma and rhinitis (especially for those living in urban areas), as well as an increase in the number of children sensitized to pollen or molds. In other words, our survey provides evidence that pediatricians with a special interest in childhood respiratory health are starting to recognize the effects of CC on their patients in their clinical practice.
Similar surveys have been carried out within other scientific societies such as the American Thoracic Society (ATS), whose membership is offered also to pediatricians, starting from US ATS members: the Authors collected responses from 915 members, 6.5% of whom were practicing pediatrics, showing similar rates of awareness of CC (89%) and its impact on patient care (“a great deal”–“a moderate amount”) (65%). 19 The majority of the respondents indicated that they were already observing health impacts of CC among their patients, most commonly in terms of increases in chronic disease severity related to air pollution (77%), increased allergic symptoms from exposure to plants or mold (58%), and severe weather injuries (57%). Moreover, 66% of the participants reported that children aged 0 to 4 years are one of the groups that will be disproportionately affected by CC. 19 Unfortunately, it is not possible to extrapolate data relating to pediatricians from the study results. The same questionnaire was later sent also to international ATS members: responses were received from 489 members in 68 countries, 5% of whom were practicing pediatrics, 96% were aware of CC and 81% indicated that CC has direct relevance to patient care. 20 In agreement with the survey on US members, the majority of international respondents indicated that they were already observing health impacts of CC among their patients such as increases in chronic disease severity from air pollution (88%), allergic symptoms from exposure to plants or mold (72%), and severe weather injuries (69%). Similar to the previous study, data relating to answers from pediatricians cannot be extrapolated from the study results. The same research group administered the questionnaire to members of the American Academy of Allergy, Asthma & Immunology (AAAAI), from which 1184 responses were retrieved, but with no clarification as to how many were from pediatricians or physicians practicing in pediatrics: the results were comparable to the ATS studies, with 81% of respondents aware of CC, 63% indicating that CC was relevant to patient care (“a great deal”–“a moderate amount”), 73% expecting a worsening in severity in chronic diseases including asthma and COPD, and 63% expecting increased care for allergic sensitization and symptoms related to exposure to plants or mold. 21
Even though our study reported that CC is felt to be an important health issue among SIMRI members, it should be noted that their knowledge of the main effects of CC on childhood health (in terms of malnutrition, infectious diseases, allergic diseases, and heat stress) was lower than expected, with 60% of respondents labeled as the “poor knowledge” group in the LCA. Only about 57% of the participants knew the term “thunderstorm asthma,” which is particularly surprising when considering that the survey includes experts in pediatric respiratory disorders.
To identify features characterizing participants with a greater awareness and knowledge of CC‐related health effects we chose to apply LCA, which represents an advanced statistical method useful to identify unmeasured class membership among subjects using categorical and/or continuous observed variables. The results obtained from the LCA allowed us to identify two latent classes related to pediatricians' knowledge of the topic. Pediatricians with a higher level of awareness were older and had longer work experience than those with poor knowledge and were those using the Internet to gather information on CC. Notably, contrary to our data, in the AAAAI survey, older physicians perceived that CC affected their patients to a lesser extent when compared with physicians younger than 50 years, even when controlling data for strength of belief in CC. 21 However, in that study no data is reported on the number of pediatricians who took the survey, therefore the results may not be comparable to our data, which could also reflect geographical differences in terms of medical education and health care system. Noticing an increased number of children with positive allergy tests for aeroallergens was also associated with a higher level of awareness of the topic: such data may be explained considering that pediatricians who are more aware of CC effects on aeroallergens may be keener to perform and extend allergy testing.
Regarding medical education on CC, it should also be noted that it is overall limited worldwide and the current climate health educational offerings appear to vary considerably among health profession institutions, as shown by a recent international survey. 22 Unsurprisingly, in our study, almost every participant stated that they are interested in receiving more education on health problems for children as an effect of CC. Surveys on CC are feasible among physicians and are useful to gather information to plan and organize educational programs; in the meantime, completing a survey may represent an educational intervention in itself, increasing the awareness and knowledge of the respondents. In the near future, CC should be included more and more in professional health education, including national conferences, continuing medical education, and residency training. 23 Considering that children are uniquely vulnerable to the health effects of CC, 24 , 25 pediatricians should be adequately educated on the subject, and we also agree with the Authors who state that physicians, and pediatricians in particular, must become engaged in strategies to address CC, the environmental sustainability of health systems and the resilience of population health to environmental change. 26 , 27
As the main limitation of the current study, we recognize that the number of respondents is quite low and included mainly academic pediatricians, therefore our results may not be suitable for generalization to other pediatric practitioners. While we can only speculate on the reasons behind such low response rates, it should be considered that physicians are among the hardest professionals to reach through surveys in general, 28 and we do believe that those who were already aware of the topic may have been more likely to respond to our survey. Moreover, this survey was conducted during the COVID‐19 pandemic, which may have contributed to the low response rate in many ways: not only were health care professionals more focused on the pandemic itself, but they likely received many different calls to participate in online surveys in the same period and may have felt annoyed (the so‐called “over‐surveying” effect). Nevertheless, our data are in line with those from other similar studies. The two aforementioned surveys distributed to the members of the ATS reported response rates of 17% 19 and 9.8%, 20 respectively. Similarly, in the multinational survey by Kotcher et al. the average participation rate across scientific societies was 10%. 17 Therefore, larger surveys on practicing pediatricians could be useful to address their gap of knowledge as well as to plan tailored educational interventions.
Another limitation of the current study includes that, even though some of the questions in our survey had been already used in other similar studies, the questionnaire did not undergo a process of validation. Furthermore, since our survey was completely anonymous, we couldn't compare the demographic characteristics of non‐respondents and respondents.
5. CONCLUSIONS
Our study, including a sample of Italian pediatricians involved and/or interested in the field of pediatric respiratory diseases and applying an advanced statistical analysis, shows a high level of awareness of CC with poor knowledge of CC‐related health effects in children. Notably, awareness was higher in those with longer work experience. Most of the participants reported having already encountered the health impacts of CC in their practice, in terms of increased incidence and severity of asthma and/or allergic rhinitis, as well as increased number of children sensitized to molds and pollen. There is urgent need to increase awareness and promote a better understanding of the impact of CC on children's respiratory health among pediatricians. CC should be integrated in the educational programs of healthcare professionals to allow them to face its serious threats on human health.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Maria Di Cicco, Marcella Lauletta, Erika Moisè conceptualized and designed the study, drafted the initial manuscript, contributed to data collection, and reviewed and critically revised the final manuscript. Giovanna Cilluffo performed the statistical analysis. Giovanna Cilluffo and Stefania La Grutta, helped with the interpretation of the results and actively participated in manuscript drafting. Diego G. Peroni, Giorgio Piacentini, and Giuliana Ferrante contributed to the review of the literature, actively participated in manuscript drafting, and reviewed and critically revised the final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
ACKNOWLEDGMENTS
We would like to thank the SIMRI executive committee and SIMRI website editorial committee for approving and supporting the survey and spreading it among SIMRI members, as well as for showing interest in the subject of potential health effects of climate change in childhood. We also would like to thank all the SIMRI members who took the survey. Open access funding provided by Universita degli Studi di Pisa within the CRUI‐CARE Agreement.
Lauletta M, Moisé E, La Grutta S, et al. Climate advocacy among Italian pediatric pulmonologists: a national survey on the effects of climate change on respiratory allergies. Pediatric Pulmonology. 2022;57:862‐870. 10.1002/ppul.25842
Marcella Lauletta and Erika Moisé contributed equally to this study.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Bunyavanich S, Landrigan CP, McMichael AJ, Epstein PR. The impact of climate change on child health. Ambul Pediatr. 2003;3:44‐52. [DOI] [PubMed] [Google Scholar]
- 2. McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367:859‐869. [DOI] [PubMed] [Google Scholar]
- 3. https://www.who.int/publications/i/item/cop26-special-report
- 4. Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change: lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693‐1733. [DOI] [PubMed] [Google Scholar]
- 5. Ayres JG, Forsberg B, Annesi‐Maesano I, et al. Environment and Health Committee of the European Respiratory Society. Climate change and respiratory disease: European Respiratory Society position statement. Eur Respir J. 2009;34:295‐302. [DOI] [PubMed] [Google Scholar]
- 6. Katelaris CH, Beggs PJ. Climate change: allergens and allergic diseases. Intern Med J. 2018;48:129‐134. [DOI] [PubMed] [Google Scholar]
- 7. D'Amato G, Cecchi L, Bonini S, et al. Allergenic pollen and pollen allergy in Europe. Allergy. 2007;62:976‐990. [DOI] [PubMed] [Google Scholar]
- 8. D'Amato G, Vitale C, De Martino A, et al. Effects on asthma and respiratory allergy of climate change and air pollution. Multidiscip Respir Med. 2015;10:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cecchi L, D'Amato G, Ayres JG, et al. Projections of the effects of climate change on allergic asthma: the contribution of aerobiology. Allergy. 2010;65:1073‐1081. [DOI] [PubMed] [Google Scholar]
- 10. Di Cicco M, Ferrante G, Doriana A, et al. Climate change and childhood respiratory health: a call to action for paediatricians. Int J Environ Res Public Health. 2020;17:5344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hathaway J, Maibach EW. Health implications of climate change: a review of the literature about the perception of the public and health professionals. Curr Environ Health Rep. 2018;5:197‐204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dupraz J, Burnand B. Role of health professionals regarding the impact of climate change on health‐an exploratory review. Int J Environ Res Public Health. 2021;18:3222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vineis P, Alfano R, Ancona C, et al. Mitigation of climate change and health prevention in Italy the co‐benefits policy. Rapporti ISTISAN 21/20; 2021. https://www.iss.it/rapporti-istisan
- 14. Linzer DA, Lewis JB. PoLCA: An R package for polytomous variable latent class analysis. J Stat Softw. 2011;42:1‐29. [Google Scholar]
- 15. Collins LM, Lanza ST. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences. John Wiley & Sons; 2010. [Google Scholar]
- 16. Anderson D, Burnham K, White G. Comparison of Akaike information criterion and consistent Akaike information criterion for model selection and statistical inference from capture‐recapture studies. J Appl Stat. 1998;25:263‐282. [Google Scholar]
- 17. Kotcher J, Maibach E, Miller J, et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet Health. 2021;5:e316‐e323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kemper KJ, Etzel RA. Research about climate advocacy Directions from a pilot survey of academic pediatricians. Complement Ther Med. 2020;49:102335. [DOI] [PubMed] [Google Scholar]
- 19. Sarfaty M, Bloodhart B, Ewart G, et al. American Thoracic Society member survey on climate change and health. Ann Am Thorac Soc. 2015;12:274‐278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sarfaty M, Kreslake J, Ewart G, et al. Survey of international members of the american thoracic society on climate change and health. Ann Am Thorac Soc. 2016;13:1808‐1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sarfaty M, Kreslake JM, Casale TB, Maibach EW. Views of AAAAI members on climate change and health. J Allergy Clin Immunol Pract. 2016;4:333‐335. [DOI] [PubMed] [Google Scholar]
- 22. Shea B, Knowlton K, Shaman J. Assessment of climate‐health curricula at international health professions school. JAMA Netw Open. 2020;3:e206609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Maxwell J, Blashki G. Teaching about climate change in medical education: an opportunity. J Public Health Res. 2016;5:673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. COUNCIL ON ENVIRONMENTAL HEALTH . Global climate change and child health. Pediatrics. 2015;136:992‐997. [DOI] [PubMed] [Google Scholar]
- 25. Philipsborn RP, Chan K. Climate change and global child health. Pediatrics. 2018;141:e20173774. [DOI] [PubMed] [Google Scholar]
- 26. Bhutta ZA, Aimone A, Akhtar S. Climate change and global child health: what can paediatricians do? Arch Dis Child. 2019;104:417‐418. [DOI] [PubMed] [Google Scholar]
- 27. Sainsbury P, Charlesworth K, Madden L, Capon A, Stewart G, Pencheon D. Climate change is a health issue: what can doctors do? Intern Med J. 2019;49:1044‐1048. [DOI] [PubMed] [Google Scholar]
- 28. Taylor T, Scott A. Do physicians prefer to complete online or mail surveys? Findings from a national longitudinal survey. Eval Health Prof. 2019;42:41‐70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


