Abstract
COVID‐19 disruptions severely impacted access to health services for noncommunicable diseases, including cancer, but few studies have examined patient perspectives of COVID‐19‐induced barriers to care in low/middle‐income countries. Data come from a survey completed online, over the phone or in person of 284 adult people with cancer in Kenya. One‐third (36%) of participants had primary or no education and 34% had some or complete secondary education. Half of the participants (49%) were aged 40 to 59, 21% were 18 to 39 and 23% were 60 or older. Two‐thirds were female (65%) and most visited a national referral hospital in Nairobi to receive care (84%). Mean travel time to Nairobi from the respondent county of residence was 2.47 hours (±2.73). Most participants reported decreased household income (88%) and were worried about their ability to afford cancer treatment due to COVID‐19 (79%). After covariate adjustment, participants who lost access to hospitals due to COVID‐19 travel restrictions were 15 times more likely to experience a cancer care delay (OR = 14.90, 95% CI: 7.44‐29.85) compared to those with continued access to hospitals. Every additional hour of travel time to Nairobi from their county of residence resulted in a 20% increase in the odds of a cancer care delay (OR = 1.20, 95% CI: 1.06‐1.36). Transportation needs and uninterrupted access to cancer care and medicines should be accounted for in COVID‐19 mitigation strategies. These strategies include permits for cancer patients and caregivers to travel past curfew time or through block posts to receive care during lockdowns, cash assistance and involving patient navigators to improve patient communication.
Keywords: access to care, barriers to care, cancer patient, COVID‐19, financial burden, Kenya, low‐/middle‐income countries, pandemic mitigation, patient transportation
What's new?
During the coronavirus disease 2019 (COVID‐19) pandemic, cancer patients were vulnerable to both severe COVID‐19 and, owing to interruptions in health care services, cancer progression. Here, the impact of the COVID‐19 pandemic on cancer care was examined specifically among patients in low‐resource settings in Kenya. Survey data show that patients experienced significant economic and logistical challenges during the pandemic. Patients reported declines in income, worries about affordability of care, interruptions in access to medications and losses in access to specialized care due to travel restrictions. The findings emphasize the importance of incorporating cancer patient needs into national pandemic mitigation plans.

Abbreviations
- CSOs
civil society organizations
- HICs
high‐income countries
- KENCO
Kenyan Network of Cancer Organizations (Nairobi, Kenya)
- KNH
Kenyatta National Hospital (Nairobi, Kenya)
- LMICs
low‐ and middle‐income countries
- MOH
Ministry of Health
1. INTRODUCTION
COVID‐19‐related disruptions around the globe severely impacted access to health services for noncommunicable diseases, including cancer. 1 This is true for both high‐income countries (HICs) and, to an even higher degree, in low‐ and middle‐income countries (LMICs). 1 , 2 , 3 , 4 , 5 , 6 , 7 From the onset of the pandemic, studies (mostly in HICs) have revealed increased COVID‐19 morbidity and higher mortality in people with cancer, 8 , 9 , 10 who have poorer prognosis as a result of COVID‐19 and cancer comorbidity. 5 , 8 , 9 , 10
Cancer is the third leading cause of mortality in Kenya, an LMIC with 42 116 new cases and 27 092 deaths for the estimated population of 53.7 m. 11 The next day after the first case was registered in Kenya on March 12, 2020, 12 the country introduced strict pandemic control measures, including public transport regulations and social distancing measures. On March 27, a nightly curfew was introduced nationwide restricting any movement at night. On April 6, all movement to and from the Nairobi metropolitan area was ceased for an initial period of 21 days. 13 These restrictions have been lifted and re‐introduced throughout 2020 and 2021, 14 , 15 , 16 , 17 , 18 creating logistical challenges to triage patients in need of urgent care; increasing the impact of existing barriers to care such as transportation and access to medicines.
To date, a number of COVID‐19 and cancer surveys have targeted health care providers and health institutions globally, 1 , 3 , 19 and some have focused on surveying people with cancer that have access and skills to complete online surveys, 4 , 6 , 20 but, to the best of our knowledge, no studies have focused on hard‐to‐reach patients in low‐resource settings with limited access to the internet or familiarity and adeptness with online surveys. To fill these gaps, this article examined the effects of COVID‐19 disruptions on patient's perceived ability to afford care, delays in cancer care and access to pain relief and other prescription medications.
2. MATERIALS AND METHODS
2.1. Study design
This cross‐sectional survey research study was conducted between December 2020 and February 2021 (the survey tool is provided as the Supporting Information). Data were collected using an anonymous survey of adult (18+) cancer patients currently residing in Kenya.
2.2. Measures
The survey questionnaire assessed community‐ and facility‐level barriers to accessing cancer care that emerged or increased due to the COVID‐19 pandemic. The survey questionnaire was designed in English and translated into the Kiswahili language, both official languages of Kenya. Both versions of the survey questionnaire were reviewed by local sector experts and revised in the light of their feedback. Additionally, both versions were also pretested and revised accordingly. Tables 1 and 2 report outcome measures and covariates.
TABLE 1.
Demographic characteristics of the participants and other covariates (n = 284)
| Frequency | Percent | |
|---|---|---|
| Female | 185 | 65 |
| Male | 86 | 30 |
| Blank/missing | 13 | 5 |
| Treatment phase | ||
| Diagnoses/treatment planning | 39 | 14 |
| Receiving treatment | 136 | 48 |
| Completed treatment | 98 | 35 |
| Blank/missing | 11 | 4 |
| Age (in years) | ||
| 18‐39 | 60 | 21 |
| 40‐59 | 140 | 49 |
| 60 and above | 64 | 23 |
| Blank/missing | 20 | 7 |
| Education | ||
| No education/some/completed primary school | 103 | 36 |
| Some/completed secondary school | 97 | 34 |
| Some/completed college/university | 65 | 23 |
| Other | 3 | 1 |
| Blank/missing | 16 | 6 |
| Hospital—health facility a , b | ||
| KNH | 238 | 84 |
| Texas Cancer Center | 21 | 7 |
| Agha Khan Hospital | 8 | 3 |
| Moi Teaching and Referral Hospital | 12 | 4 |
| Logistical challenges of accessing care | ||
| Transportation challenges | ||
| Limited access to hospitals (eg, due to hospitals seeing less patients, changing appointments) c | 98 | 35% |
| Ability to travel for treatment limited by curfews or county lockdowns c | 143 | 50% |
| Respondent's travel time to Nairobi (in hours) | ||
| Mean ± SD | 2.47 ± 2.73 | |
| Median | 2.0 | |
| Range | 0‐11 | |
| Blank/Missing | 16 (6%) cases | |
Percentages do not add up to 100 because this was a multianswer question. Only options included in logistic regression are reported here.
Percentages do not add up to 100 because this was a multianswer question. Only top‐four options selected by respondents are reported.
Other health facilities included AIC Kijabe Hospital, MP Shah Hospital, Afya Bora Hospital, Mama Lucy Kibaki Hospital and Coptic Hospital, Nairobi.
TABLE 2.
Outcome variables distribution (n = 284)
| Survey question | Categories/options | Frequency | Percent |
|---|---|---|---|
| Self‐reported delays based on the patient's stage in the cancer journey (eg, diagnosis, active treatment, survivorship) | I have experienced a delay of less than 1 month a | 51 | 18 |
| I have experienced a delay of 1 month to 2 months a | 29 | 10 | |
| I have experienced a delay of more than 2 months a | 40 | 14 | |
| I have not experienced any delays | 152 | 54 | |
| Blank/missing | 12 | 4 | |
| Access to pain relief medicines since the start of COVID‐19 | Yes | 149 | 52 |
| No | 79 | 28 | |
| Did not need b | 39 | 14 | |
| Blank/missing | 17 | 6 | |
| Access to other prescription medicines (not pain relief) like refills, treatment for other symptoms since the start of COVID‐19 | Yes | 141 | 50 |
| No | 80 | 28 | |
| Did not need b | 40 | 14 | |
| Blank/missing | 23 | 8 |
All these categories denoting a delay were combined to compute binary logistic regression.
This category was excluded to compute binary logistic regression models.
Treatment delays were assessed through the question: “Based on where you are in your cancer journey (e.g., diagnosis, treatment, etc.), have you experienced any delays since the start of COVID‐19?” Response options included delays of (a) less than 1 month, (b) 1 month to 2 months, (c) more than 2 months and (d) no delays. During the analysis, responses were dichotomized as any delay (options 1‐3) vs no delay (option 4).
Access to pain relief or other prescription medicines was assessed through the questions “Since the start of COVID‐19 pandemic, have you had access to pain relief medicines?” and “since the start of COVID‐19 pandemic, have you had access to other prescription medicines (not pain relief) like refills, treatment for other symptoms (e.g., nausea, vomiting)?” Response options to both items were “Yes,” “No” and “Did not need.” “Did not need” responses were excluded from the analyses.
The covariates used in our study were measured as follows. The survey asked participants: “How, in your opinion, has COVID‐19 impacted your cancer treatment and care journey?” The multi‐answer responses included “I have limited access to hospitals (e.g., hospitals are seeing less patients, changing appointments)” and “my ability to travel for treatment has been limited by curfews or county lockdowns.” If a respondent checked the option, it was coded as 1, otherwise 0 to create dichotomous variables.
Besides demographics such as gender, age, education and treatment phase, the county of patients' residence was also assessed. Google Maps was used to estimate the travel time to Nairobi, the location of the national teaching and referral hospital. These travel time estimates were reviewed by local experts on the team and adjusted for accuracy based on local road conditions.
2.3. Data collection
The survey was administered using the following three methods: (a) a self‐administered online survey for respondents who could read and understand English and technologically felt comfortable completing an online survey with recruitment from communication and social networking platforms targeting cancer patients in Kenya; (b) an enumerator assisted telephonic survey; and (c) an enumerator‐assisted in‐person survey. For the last two methods, participant recruitment materials, distributed by the Kenyatta National Hospital (KNH) and the Kenyan Network of Cancer Organizations (KENCO), gave cancer patients the option to contact trained survey enumerators, who spoke both English and Kiswahili languages, to complete the survey via phone or in person.
2.4. Statistical analyses
Statistical analyses and data management were performed using IBM SPSS Statistics 24. Descriptive statistics were conducted. Stepwise logistic regression with forward selection was used to calculate odds ratios (Nagelkerke R2, P < .05 cutoff) with 95% confidence intervals to determine which variables would go into the final model for the three outcomes. Multicollinearity was also examined (all variance inflation factors were <2) before making the final determination of the variables for the final models.
3. RESULTS AND DISCUSSION
3.1. Participants
Of the 314 survey participants, 30 respondents did not meet inclusion criteria (ie, they did not complete the survey beyond demographic section), leaving 284 valid responses of adult cancer patients from 28 counties (see Figure 1 for the breakdown of responses by county). Sociodemographic characteristics of participants are shown in Table 1. Two‐thirds (65%) of the respondents were female. One‐fifth (21%) of the participants were between 18 and 39 years of age; nearly half were between 40 and 59 years; and 23% were 60 or older. Over a third (36%) of the survey participants had no education to complete primary education, 34% had some or complete secondary education; and 23% had some or complete higher education. Nearly half of the survey participants (48%) were in active cancer treatment; 35% had completed the treatment; and only 14% were in the diagnosis/treatment planning phase at the time of survey completion. A majority (84%) of the participants had visited KNH in the course of their cancer diagnosis and/or treatment. The mean travel time to Nairobi from the survey respondents' county of residence was 2.47 ± 2.73 hours. The median travel time was 2 hours with interquartile range of 4 hours.
FIGURE 1.
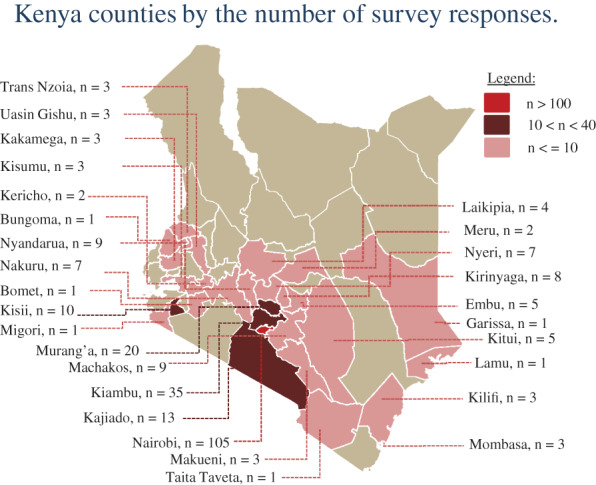
Counties of Kenya by the number and percentage of responses. The base map used is courtesy of yourfreetemplates.com licensed under CC BY‐ND 4.0 [Color figure can be viewed at wileyonlinelibrary.com]
3.2. Economic impact of COVID‐19 on people with cancer
COVID‐19 has had devastating financial effects on people with cancer in Kenya as it significantly reduced household incomes and caused patients to worry that they cannot afford the cancer treatments they need. Specifically, 88% of the survey participants reported a decrease in their household income due to COVID‐19. On top of this, most patients reported the financial burden of treatment outside of the clinical setting, with 87% reporting that transportation to cancer treatment facility options became more expensive since the start of COVID‐19 pandemic.
These results demonstrate the additional negative impact on people with cancer in low‐ and middle‐income countries (LMICs) in comparison to high‐income countries, where survey results were already alarming. For example, in Australia, 26% of respondents reported losing income and 29% indicated a worsening of financial concerns due to COVID‐19. 21 In a US‐based cancer patient survey, 46% of respondents reported experiencing some loss of income and nearly 48% were worried about the potential loss of health insurance. 6
In our study from Kenya, the economic impact of COVID‐19 manifested negatively in participants' mental health. Overall, 79% of participants were worried that the financial impact of COVID‐19 had made it harder for them to afford the cancer care they needed. Of those in the diagnosis or treatment planning phase 87%, and of those in active treatment, 89% reported being worried.
A female in her 50's living with cancer summarized the financial impact of COVID‐19 in her response to an open‐ended question:
We would sell tea for 35 [Kenya] shillings pre‐COVID, but currently we sell at 6 shillings the same quantity. The market has been extremely disrupted by COVID 19. This loss of revenue has made it difficult to afford treatment.
In comparison, a US‐based study of cancer survivors found that only 27% were worried the pandemic would make it harder to afford their cancer care. 6 These data highlight the critical need to include vulnerable people with cancer and their caregivers in subsistence assistance and subsidized insurance programs, especially in LMICs.
3.3. Delays in cancer care
As shown in Table 2, 42% of participants reported experiencing delays in their cancer care journey since the start of COVID‐19. As reported in Table 3, longer travel time from Nairobi was associated with a higher likelihood of experiencing a delay in cancer care (OR = 1.20, 1.06‐1.36). The importance of affordable and convenient transportation for access to care has been well established and reducing public transportation options as pandemic control measures hurts patients' ability to receive timely care.
TABLE 3.
Multiple logistic regression models
| Experienced delay (Yes = 1, No = 0) | Access to pain relief medicine since the start of COVID‐19 (Yes = 1, No = 0) | Access to other prescription medicine since the start of COVID‐19 (Yes = 1, No = 0) | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender (ref. Male) | 1.06 | 0.52‐2.17 | 0.76 | 0.38‐1.52 | 0.76 | 0.38‐1.51 |
| Age (ref. 60 years and above) | P < .05 | |||||
| 18‐39 | 2.31 | 0.90‐5.94 | 0.42 | 0.16‐1.09 | 0.81 | 0.32‐2.04 |
| 40‐59 | 1.98 | 0.85‐4.61 | 0.35 | 0.15‐0.83 | 0.42 | 0.18‐0.94 |
| College (ref. Some college or higher) | 0.22 | 0.10‐0.46 | 0.88 | 0.43‐1.8 | 1.13 | 0.57‐2.26 |
| Ability to travel limited by curfews or county lockdowns (ref. Yes) | 2.01 | 1.09‐3.69 | 2.19 | 1.19‐4.02 | ||
| Ability to access hospital (ref. Yes) | 14.90 | 7.44‐29.85 | ||||
| Treatment Phase (ref. Completed treatment) | P < .05 | |||||
| Diagnosis or treatment planning | 2.65 | 1.003‐7.01 | 0.92 | 0.37‐2.31 | 1.01 | 0.41‐2.52 |
| Receiving treatment | 1.05 | 0.51‐2.15 | 2.14 | 1.11‐4.13 | 1.91 | 0.99‐3.69 |
| Travel time to Nairobi (in hours) | 1.20 | 1.06‐1.36 | 0.91 | 0.82‐1.01 | 0.99 | 0.89‐1.10 |
| χ2 test (Model Significance) | X 2 (df 8) = 113.48, P < .001 | X 2 (df 8) = 24.15, P < .005 | X 2 (df 8) = 21.77, P < .005 | |||
| Classification without IVs (percent correct) | 55.6% | 64.4% | 62.1% | |||
| Classification with all IVs (percent correct) | 80.3% | 67.1% | 64.9% | |||
| Nagelkerke R 2 | .48 | .15 | .13 | |||
| Cox and Snell R 2 | .36 | .11 | .10 | |||
| Hosmer and Lemeshow Test | X2 (df 8) = 3.45, P = .90 | X2 (df 8) = 4.24, P = .84 | X2 (df 8) = 5.22, P = .73 | |||
Note: Ability to access hospitals and ability to travel are highly correlated variables and therefore both were not included in all multiple regression models.
All values in bold are significant at p < .05.
Lack of access to hospitals due to lockdowns had a dramatic effect on the receipt of cancer treatment. Compared to those with continued access to hospitals, participants with limited access to hospitals had markedly higher odds of experiencing a delay in their cancer care (OR 14.90, 7.44‐29.85). It is ever more important that the development of clear criteria for scheduling in‐person cancer care and the increased use of innovative tools such as telemedicine 22 during lockdowns, along with the critical infrastructure, should be prioritized in national pandemic response strategies.
Compared to those who had completed treatment, the participants who were currently in the diagnosis or treatment planning phase had higher odds of experiencing delays in their cancer care (OR 2.65, 1.003‐7.01). This is likely because patients in the diagnosis and treatment planning phase needed to visit health facilities more frequently, but due to access challenges and lockdowns, they might have been prohibited from doing so. Likewise, those who had completed treatment require fewer visits to the hospital than those in active treatment; thus, the impact of the delays may be less clinically significant. Age and gender were not associated with experiencing delays in cancer care in our participant population.
Compared to those who had a college degree or better, participants without college degree or lower had lower odds of experiencing delays in their cancer care (OR 0.22, 0.10‐0.46). While this finding seems counter intuitive, discussions with in‐country partners revealed that patients with college or higher education were likely more empowered, knowledgeable about infection risk, and may have chosen to delay cancer care due to fear of being infected with COVID‐19.
This perspective is supported by a recent study in Ethiopia that found a significant association between education level and COVID‐19 risk perception. 23
3.4. Challenges in accessing pain relief and prescription medicines
As shown in Table 2, 52% of respondents reported not having access to pain relief medicine, and 50% reported not having access to other prescription medicines, such as refills and treatment for other symptoms (eg, nausea, vomiting) since the start of the COVID‐19 pandemic. Compared to older participants (aged 60 years and above), younger participants (aged between 40 and 59) had lower odds of having access to pain relief medicine (OR 0.35, 0.15‐0.83), and access to other prescription medicines (OR 0.42, 0.18‐0.94). More research is needed to identify the associations between age and access to medicines among people with cancer in Kenya.
Similar to the delays in care, reduced ability to travel due to lockdowns and curfews also had a negative effect on access to pain relief medicine. Compared to those with the reduced ability to travel, participants without such restrictions had twice the odds of having access to pain relief medicine (OR 2.01, 1.09‐3.69) and access to other prescription medicines (OR 2.19, 1.19‐4.02). The importance of transportation has been well documented as an important determinant of access to care. 1 , 24 Lockdowns, curfews or other movement restrictions should account for the needs of people with cancer in active treatment to adhere to their treatment plan in a timely manner, and to access medicines and pain relief, both often necessary during the active cancer treatment phase.
Compared to those who had already completed treatment, participants who were currently in the active treatment had higher odds of having access to pain relief medicine (OR 2.14, 1.11‐4.13). Gender and travel time to Nairobi were not associated with access to pain relief and other prescription medicine, which may suggest more local availability of medicines without the need to travel to the cancer treatment center.
3.5. Limitations
Despite the strengths of our study, such as reaching patients who may be less likely to respond to an electronic‐only survey and utilizing bilingual survey deployment, our study had notable limitations, including a cross‐sectional design, self‐reported information, and survey items not previously validated. The use of multiple modalities likely introduced biases, such as social desirability of responses, especially for the in‐person channel.
Without having access to exact participant addresses, travel times based on the county center provided estimates that may be too conservative since not all patients live in county centers and are likely to require even more time to get to the center before embarking on travel to Nairobi.
Given these limitations, our results are not generalizable to other populations, but they provide a better understanding of the challenges faced by hard to reach and not well‐understood cancer patients.
Our results highlight that people with cancer in Kenya, an LMIC in East Africa, are facing disproportionately strong downward pressure of the economic burden and logistical challenges accessing vital cancer care. The pandemic mitigation policies, such as cash assistance, inter‐county travel permits and so forth will be very helpful for patients with cancer in these times.
More research is needed to examine the financial impact of COVID‐19 on people with cancer and health care delivery institutions and the importance of creative approaches to facilitating transportation for cancer patients.
CONFLICT OF INTEREST
The authors have declared no conflicts of interest for this article.
ETHICS STATEMENT
Our study was exempt from review in the U.S. by the Morehouse School of Medicine IRB (title 1637695‐1) and approved by the Ethics and Research Committee of KNH and University of Nairobi (full review, protocol P428/08/2020). The survey did not collect any information that could be linked to an individual. In all modes of data collection, all participants went through an informed consent process.
Supporting information
Appendix S1 Supporting Information
ACKNOWLEDGEMENTS
Tom Ochieng’, Gladys Mukosi, and Ronniey Obulemire, Kenyatta National Hospital, provided inputs to the survey tool and served as a data collector. Caroline Ntinyari, Kenyan Network of Cancer Organizations, coordinated telephonic data collection. Forrest Brady, MPH, Rollins School of Public Health, Emory University, Atlanta, GA, researched the timeline of the public health response to the COVID‐19 pandemic in Kenya and Uganda, parts of which have been used for writing the introduction. The base map used for Figure 1 is courtesy of yourfreetemplates.com licensed under CC BY‐ND 4.0.
Umar S, Chybisov A, McComb K, et al. COVID‐19 and access to cancer care in Kenya: patient perspective. Int. J. Cancer. 2022;150(9):1497-1503. doi: 10.1002/ijc.33910
No external funding was used for this project. The American Cancer Society has sponsored the establishment of a comprehensive patient navigation program within KNH’s Cancer Treatment Centre and organizational capacity strengthening of KENCO. Both KNH and KENCO have provided data collectors for interviewing and data entry, and all three parties participated collaboratively in the design, ethics review and are co‐authors on this article, per the collaboration agreement signed prior to the project.
DATA AVAILABILITY STATEMENT
The data that support the findings of our study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Bullen C, McCormack J, Calder A, et al. The impact of COVID‐19 on the care of people living with noncommunicable diseases in low‐ and middle‐income countries: an online survey of physicians and pharmacists in nine countries. Prim Health Care Res Dev. 2021;22:e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chiang J, Yang VS, Han S, et al. Minimizing transmission of COVID‐19 while delivering optimal cancer care in a National Cancer Centre. J Cancer Policy. 2020;25:100241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jazieh AR, Akbulut H, Curigliano G, et al. Impact of the COVID‐19 pandemic on cancer care: a global collaborative study. JCO Glob Oncol. 2020;6:1428‐1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Juanjuan L, Santa‐Maria CA, Hongfang F, et al. Patient‐reported outcomes of patients with breast cancer during the COVID‐19 outbreak in the epicenter of China: a cross‐sectional survey study. Clin Breast Cancer. 2020;20:e651‐e662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI. A war on two fronts: cancer Care in the Time of COVID‐19. Ann Intern Med. 2020;172:756‐758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leach CR, Kirkland EG, Masters M, et al. Cancer survivor worries about treatment disruption and detrimental health outcomes due to the COVID‐19 pandemic. J Psychosoc Oncol. 2021;39:347‐365. [DOI] [PubMed] [Google Scholar]
- 7. Ueda M, Martins R, Hendrie PC, et al. Managing cancer care during the COVID‐19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw. 2020;18:1‐4. [DOI] [PubMed] [Google Scholar]
- 8. Liang W, Guan W, Chen R, et al. Cancer patients in SARS‐CoV‐2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335‐337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Miyashita H, Mikami T, Chopra N, et al. Do patients with cancer have a poorer prognosis of COVID‐19? An experience in New York City. Ann Oncol. 2020;31:1088‐1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Xia Y, Jin R, Zhao J, Li W, Shen H. Risk of COVID‐19 for patients with cancer. Lancet Oncol. 2020;21:e180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. International Agency for Research on Cancer . The Global Cancer Observatory (Globocan), Kenya. Paris, France: IARC; 2020. [Google Scholar]
- 12. Ministry of Health Kenya . First Case of Coronavirus Disease Confirmed in Kenya; 2020.
- 13. Dentos . COVID‐19—“new” criminal offences in Kenya. Marshall, CA: JD Supra; 2020. [Google Scholar]
- 14. Mersie A, Mohammed O. Kenya announces phased reopening from coronavirus lockdown. London, UK: Reuters; 2020. [Google Scholar]
- 15. Obulutsa G. Kenya Extends Night Curfew to March to Curb COVID‐19 Spread. London, UK: Reuters; 2021. [Google Scholar]
- 16. UNOCHA . Kenya Situation Report, 10 September 2020, Kenya. ReliefWeb; 2020.
- 17. Oketch A. Covid‐19: night curfew times changed to 9 pm‐4 am Kenya; 2020.
- 18. Yusuf M. Kenya Reimposes COVID‐19 Measures Amid Surging Cases|Voice of America—English; 2020.
- 19. Union for International Cancer Consortium . UICC joins COVID‐19 and Cancer Task Force. UICC; 2020.
- 20. Nindrea RD, Sari NP, Harahap WA, et al. Survey data of COVID‐19 awareness, knowledge, preparedness and related behaviors among breast cancer patients in Indonesia. Data Brief. 2020;32:106145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zomerdijk N, Jongenelis M, Short CE, Smith A, Turner J, Huntley K. Prevalence and correlates of psychological distress, unmet supportive care needs, and fear of cancer recurrence among haematological cancer patients during the COVID‐19 pandemic. Support Care Cancer. 2021;29:7755‐7764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alhalabi O, Subbiah V. Managing cancer care during the COVID‐19 pandemic and beyond. Trends Cancer. 2020;6:533‐535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Eyeberu A, Mengistu DA, Negash B, et al. Community risk perception and health‐seeking behavior in the era of COVID‐19 among adult residents of Harari regional state, eastern Ethiopia. SAGE Open Med. 2021;9:20503121211036132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208‐220. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Supporting Information
Data Availability Statement
The data that support the findings of our study are available from the corresponding author upon reasonable request.


