Abstract
Objectives
To describe the clinical presentation, management and outcome of cases presenting with intrathoracic wooden skewers originating from the abdominal gastrointestinal tract.
Materials and Methods
Clinical records of dogs presented and treated for an intrathoracic wooden skewer were reviewed from June to August 2020. Data included signalment, clinical presentation, duration of clinical signs, haematological and biochemical abnormalities, diagnostic imaging findings, surgical procedure, postoperative complications and outcome.
Results
Eleven dogs were included in the study. In all cases, the foreign body was identified as a wooden skewer. The most common clinical signs were anorexia/hyporexia (n=7), vomiting/regurgitation (n=7), lethargy (n=6), pyrexia (n=4) and gait abnormalities/lameness (n=3). CT correctly identified a wooden skewer in all cases when performed (n=7). A coeliotomy combined with transdiaphragmatic thoracotomy was performed in six of 11 cases (55%), a coeliotomy combined with median sternotomy in four of 11 cases (36%) and a median sternotomy alone was performed in one case. Foreign bodies penetrated from the stomach (n=10) or the duodenum (n=1). Intrathoracic trauma was most commonly identified to the lungs (n=3) and pericardium (n=3). Complications occurred in three of 11 cases (27%), two minor and one resulting in death. Ten of the 11 cases (91%) survived to discharge. Long‐term outcome was available for seven of 11 cases (66%), all of them excellent.
Clinical Significance
Despite the challenges of managing wooden skewers penetrating the thoracic cavity from the abdominal gastrointestinal tract, the majority of the patients are stable to undergo diagnostic procedures, surgical exploration and management with low morbidity and excellent short‐ and long‐term prognosis.
INTRODUCTION
Migrating foreign bodies from the gastrointestinal or respiratory tracts into the abdomen, organs or body wall have been widely reported throughout the veterinary literature. Migrating plant material has been frequently reported (Brennan & Ihrke 1983, Lamb et al. 1994, Schultz & Zwingenberger 2008) and wooden (Hunt et al. 2004, Stander & Kirberger 2011, Lamb et al. 2017), metallic (Pratt et al. 2014) or quilling (Johnson et al. 2006) foreign bodies have also been described. A high palatability of wooden foreign bodies in dogs has also been suggested (Choi & Han 2017), particularly if they have been in contact with food, increasing the likelihood of ingestion (Choi & Han 2017). Due to their length and sharp ends, migration of wooden skewers from the gastrointestinal tract is possible and has been previously described as part of two case series and several individual case reports (Hunt et al. 2004, Stander & Kirberger 2011, Appleby et al. 2015, Choi & Han 2017, Lamb et al. 2017). Caudal abdominal migration appears to be more common, usually involving viscera or body wall structures (Hunt et al. 2004, Stander & Kirberger 2011), whilst cranial migration into the thorax has only been described sporadically, in three single cases (Hunt et al. 2004, Stander & Kirberger 2011, Choi & Han 2017). When cranial migration occurs, the severity of the clinical presentation will depend on the path of migration of the wooden skewer, its final location, the duration of the migration process and delay to diagnosis. The severity of clinical presentation ranges from asymptomatic to severe; the most severely affected cases can be identified with peritonitis or pyothorax (Hunt et al. 2004, Stander & Kirberger 2011, Choi & Han 2017).
The aim of this study was to describe the clinical presentation, diagnostic investigations, surgical management and outcomes of cases presenting with intrathoracic wooden skewers, which cranially migrated from the intra‐abdominal gastrointestinal tract. For the purpose of the study, a “wooden skewer” refers to any pointed longitudinal wooden structure including both cocktail (shorter) or kebab (longer) sticks. We hypothesised patients presenting with intrathoracic wooden skewers migrating from the cranial intra‐abdominal gastrointestinal tract will have a guarded prognosis due to the severity of the lesions caused by the migration tract.
MATERIALS AND METHODS
Twelve referral hospitals in the UK were invited to participate in the study. Ethical approval was obtained from the veterinary ethical review committee of the University of Edinburgh (VERC 116.20). The surgical database of each institution (Provet Cloud©, Nordhealth; VetSpace's Voyager©, AmerisourceBergen; Microsoft Word©, Microsoft; Microsoft Excel©, Microsoft; RxWorks©, Covetus) was searched by a single operator per practice from June to August 2020. Searched words included “kebab stick” and/or “skewer” combined with “thorax” and/or “thoracotomy” and/or “sternotomy” and/or “abdomen.” All dogs diagnosed with and treated for a migrating wooden foreign body from the abdominal gastrointestinal tract into the thoracic cavity were eligible for study inclusion. Medical records were received from six referral hospitals that met the inclusion criteria. Patients were excluded from the study if the intrathoracic foreign body could not be confirmed to have migrated from the abdominal gastrointestinal organs either on diagnostic imaging or surgical exploration or they were euthanased after further treatment was declined.
Data collected included signalment, bodyweight, clinical presentation, duration of the clinical signs, haematological and biochemical results, diagnostic imaging modalities and findings, surgical procedures and findings, type of foreign body, antibiotic use, complications and outcome.
Complications were defined as (1) none reported, (2) mild (requiring no or minor invasive procedures or medical management), (3) moderate (requiring major medical intervention), (4) severe (resulting in failure of an organ or requiring surgical reintervention) or (5) death (postoperative death) as proposed by Follette et al. (2020). When patients survived to discharge, short‐term (≤30 days) and long‐term (>30 days) follow‐up were recorded, when data were available in the clinical records and/or by contacting the referring veterinarian.
Descriptive statistical analysis was performed using Microsoft Excel© (Microsoft, 2021) statistical software. Categorical data were reported as number. Normality was assessed by the Shapiro–Wilk test. Normal data were reported as mean (±sd), and data not normally distributed were reported as median and range. Statistical significance was defined as P < 0.05.
RESULTS
Fourteen cases were assessed and 11 cases met the inclusion criteria. Case signalment, clinical presentation, haematological findings and diagnostic imaging techniques are summarised in Table 1. Breeds included Labrador retriever (n=3), cocker spaniel (n=2), English springer spaniel (n=2) and one of each of the following: Dobermann, pug, small‐sized crossbreed (<10 kg) and medium‐sized crossbreed (10 to 20 kg). Sex and neuter status included nine males (seven neutered and two entire) and two neutered females. A mean age of 57 months (±36) and a mean bodyweight of 21 kg (±12) was reported.
Table 1.
Summary of case signalment, clinical presentation, diagnostic procedures, surgical treatment and findings and follow‐up in 11 cases treated for intrathoracic wooden skewers penetrating from the abdominal cavity
| Case | Breed | Age | Neuter status | Bodyweight (kg) | Clinical presentation | Laboratory findings | Diagnostic imaging | Surgical approach | Surgical findings – summary | Surgical treatment – summary | Drain placement | Follow‐up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Cocker spaniel | 4 years | ME | 13.0 | 14‐day history of lethargy, hyporexia, vomiting; 6‐day history of right thoracic limb lameness and pyrexia | Left‐shift neutrophilia, thrombocytopenia, ↑ALKP, ↓Mg, ↓TS, ↑CRP, 4Dx (−) | APOCUS, TPOCUS, CT | Coeliotomy+diaphragmotomy | Wooden skewer in stomach, passing through pylorus, penetrating through anti‐mesenteric surface of duodenum, penetrating through right lateral liver lobe peripherally and dorsally through diaphragm into right caudal lung lobe | Coeliotomy performed and skewer extracted from duodenal lumen via duodenal fistula site; fistula tract subsequently excised. Circumferential diaphragmotomy with excision of fistula and adhesions. Right lateral liver partial hepatectomy. Right caudal lung lobectomy | Bilateral thoracic drains | Survive to discharge, lost follow‐up after |
| 2 | Dobermann | 8 years | ME | 49.3 | 3‐day history of lethargy, anorexia, reluctance to lay down, kyphosis, generalised ataxia | Lymphopenia, neutrophilia, thrombocytopenia, ↑ALKP, ↑Gly | Thoracic radiographs, MRI, CT | Coeliotomy+diaphragmatomy+median sternotomy | Wooden skewer penetrating from stomach, through left medial liver lobe, diaphragm and pericardium. End of skewer located at level of left atrium | Coeliotomy and identification of migrating skewer, which was broken midway to facilitate safe extraction. Sternotomy and diaphragotomy. Accessory lung lobectomy performed due to profuse haemorrhage. Pericardotomy and half of skewer extraction from pericardium. Gastrotomy and remaining skewer extracted | Unilateral thoracic drain | Survive to discharge, lost follow‐up after |
| 3 | Labrador retriever | 2 years | MN | 32.2 | 14‐day history of malaise and intermittent vomiting; 24‐hour history of panting and vocalisation | Neutrophilia, normocytic hypochromic anaemia, ↓Alb | Thoracic radiographs, thoracic US, CT | Coeliotomy+diaphragmotomy | Wooden skewer penetrating from gastric lesser curvature through diaphragm into thoracic cavity. Severe pleuritis | Coeliotomy and partial gastrectomy to retrieve the skewer and resect gastric fistula and fibrous tract to the liver. Diaphragmotomy to resect remainder of fibrous tract | Jackson–Pratt abdominal drain | Alive |
| 4 | Cocker spaniel | 7 years | FN | 12.4 | 70‐day history of malaise, lethargy; 3‐day history of regurgitation, praying stance, grunting/vocalisation when laying down | Monocytosis, ↑ALKP,↓Alb | Echocardiography, CT | Coeliotomy+diaphragmotomy | Wooden skewer penetrating from the stomach, through the hilus of the spleen and through the dorsal right diaphragm | Coeliotomy and partial gastrectomy to retrieve the skewer and resect gastric fistula. Diaphragmotomy to resect remainder of fibrous tract. Splenectomy performed due to significant scar tissue around the splenic hilus | Unilateral thoracic drain | Alive |
| 5 | Labrador retriever | 6 years | MN | 35.0 | 112‐day history of right thoracic limb lameness, marked pain on full extension of the right elbow and on palpation of the medial humerus | Neutrophilia, normocytic hypochromic anaemia, thrombocytopenia | MRI, CT | Median sternotomy | Fibrous tract from dorsal right diaphragm consisting with gastric migration. Wooden skewer lodged within the right cranial, middle and caudal lung lobes | Median sternotomy and right cranial, middle and caudal lung lobectomies. Removal of skewer and debridement of fistulous tract to the diaphragm | Unilateral thoracic drain | Euthanased |
| 6 | English springer spaniel | 6 years | MN | 23.0 | 9‐day history of vomiting, hyporexia, pyrexia and tachypnoea | Neutrophilia, monocytosis, ↑ALKP, ↑Chol | Thoracic US | Coeliotomy+diaphragmotomy | Wooden skewer in gastric fundus and pylorus, penetrating through greater curvature of pyloric antrum and into the right hemithorax. Septic peritonitis evident | Coeliotomy and partial gastrectomy to retrieve the skewer and resect gastric fistula. Diaphragmotomy to resect remainder of fibrous tract | Unilateral thoracic drain. Jackson–Pratt abdominal drain | Alive |
| 7 | Crossbreed | 2 years | MN | 9.6 | 14‐day history of cranial abdominal pain, vomiting | Neutrophilia, normocytic hypochromic anaemia | Echocardiography, CT | Coeliotomy+median sternotomy | Wooden skewer penetrating from stomach, through diaphragm and into pericardium. End of skewer located at the level of the left ventricle | Coeliotomy and partial gastrectomy to retrieve the skewer and resect gastric fistula. Median sternotomy and subtotal pericardectomy for retrieval of wooden skewer | Unilateral thoracic drain | Alive |
| 8 | Pug | 9 months | MN | 10.4 | 5‐day history of reluctance to sit down and hyporexia | Neutrophilia, ↑ALKP, ↑AMYL | CT, oesophagoscopy | Coeliotomy+diaphragmotomy | Wooden skewer in stomach penetrating from cranioventral aspect of the fundus, through dorsal left aspect of the crus of the diaphragm into the pleural space, exiting in the 12th intercostal space | Coeliotomy and partial gastrectomy to retrieve the skewer and resect gastric fistula. Diaphragmotomy to resect remainder of fibrous tract | Unilateral thoracic drain | Survive to discharge, lost follow‐up after |
| 9 | Labrador retriever | 10 years | FN | 25.4 | 7‐day history of vomiting, cranial abdominal pain, pyrexia, tachypnoea | NA | Thoracic radiographs, echocardiography, CT | Coeliotomy+median sternotomy+diaphragmotomy |
Primary care surgical findings: wooden skewer identified in stomach fundus. Gastrotomy revealed wooden skewer perforating through diaphragm craniodorsally Referral surgical findings: abscessation of the previous penetrating tract in the left dorsal paraspinal musculature of the thorax |
Surgery performed by referring vet: coeliotomy and partial gastrectomy to retrieve the skewer and resect gastric fistula. Diaphragmotomy to resect remainder of fibrous tract Revision surgery by specialist surgeon: median sternotomy and caudal thoracic dorsal paraspinal abscess and penetrating tract debrided |
Ventral thoracic drain | 5 years follow‐up; euthanased for reasons unrelated to this study |
| 10 | English springer spaniel | 1 year | MN | 10.0 |
14‐day history of lethargy and vomiting 2‐day history of draining sinus tract over the left parasternal region |
NA | Thoracic radiographs, thoracic US, MRI | Coeliotomy+diaphragmatomy+median sternotomy+sinus tract excision | Wooden skewer in fundus of stomach penetrating from lesser curvature into the left hemi‐diaphragm, the ventrocaudal pericardium and exiting at the level of the fourth sternebra. Extensive adhesions between the gastric lesser curvature, the left medial hepatic lobe and left hemi‐diaphragm present | Coeliotomy and partial gastrectomy to retrieve the skewer and resect gastric fistula. Diaphragmotomy to resect remainder of fibrous tract. Median sternotomy and subtotal pericardectomy for retrieval of wooden skewer. Parasternal sinus tract debrided | Unilateral thoracic drain | Alive |
| 11 | Crossbreed | 4 years | MN | 17.5 | 21‐day history of lethargy, pyrexia and swelling over the left thoracic wall | Neutrophilia | CT | Coeliotomy+diaphragmotomy+sinus tract excision | Wooden skewer identified in stomach lumen, perforating through the lesser omentum, the left diaphragm, left caudal lung lobe and subcutaneous tissues of the 11th intercostal space | Coeliotomy and partial gastrectomy to retrieve the skewer and resect gastric fistula. Left 11th intercostal space swelling and sinus tract debrided | None | Alive |
ME Male entire, ALKP Alkaline phosphatase, Mg Magnesium, TS Total solids, CRP Canine reactive protein, APOCUS Abdominal point of care ultrasound, TPOCUS Thoracic point of care ultrasound, Gly Glycaemia, MN Male neutered, Alb Albumin, US Ultrasound, FN Female neutered, Chol Cholesterol, AMYL Amylase, NA Not available.
All CTs and MRIs assessed both thorax and abdomen.
The most common clinical signs were anorexia/hyporexia (n=7), vomiting/regurgitation (n=7), lethargy (n=6), pyrexia (n=4) and gait abnormalities/lameness (n=3). Gait abnormalities included thoracic limb lameness (2/3), kyphosis and thoracic proprioceptive ataxia with no case having any other orthopaedic or neurological abnormality detected on examination. Two dogs were presented with tachypnoea, two with abdominal pain and two with body wall involvement (sinus tract/soft tissue swelling). Median time from the development of clinical signs to presentation at the referral centre was 14 (2 to 112) days.
Haematological results were available in nine of 11 cases (82%) with the most commonly identified haematological findings including left‐shifted neutrophilia (n=8) and thrombocytopenia (n=3). The most commonly identified biochemical findings included mild elevation in alkaline phosphatase (n=5) and mild hypoalbuminaemia (n=2).
Diagnostic imaging reports were available for all 11 cases, allowing comparison with intraoperative findings. Thoracic radiography was performed in four of 11 cases (36%), three of which failed to identify the foreign body. In one single case where thoracic radiography was performed, the foreign object could be identified as a linear radiolucent structure measuring approximately 10 cm, penetrating from the craniodorsal abdomen into the caudodorsal thoracic cavity, at the level of the caudoventral edge of the caudal lung lobes. Abdominal and thoracic ultrasound identified the penetrating foreign body in two of four cases. Echocardiography identified the foreign body in one of two cases (Fig 1A). MRI was used to identify the foreign body in two of three cases and confirmed with thoracic and abdominal CT in eight of nine cases (Fig 1B, C). In case 9, abdominal and thoracic CT revealed a linear gas tract from the caudodorsal aspect of the thoracic cavity into the paraspinal tissues, consistent with the former location of the penetrating foreign body.
FIG 1.
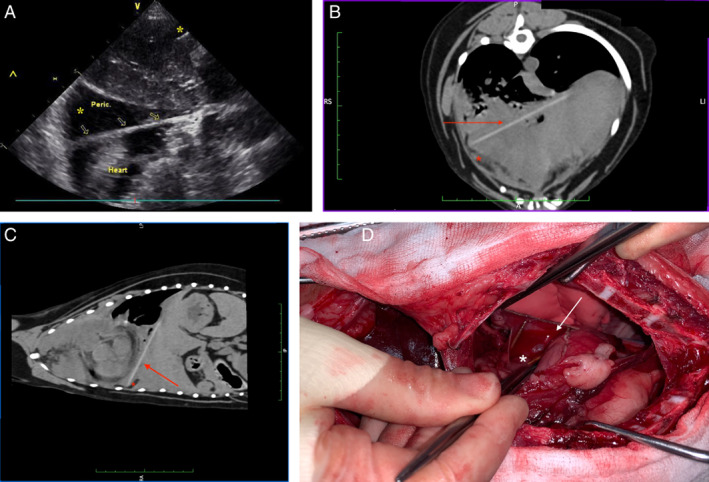
(A) Sagittal echocardiographic view of the heart and pericardium of case 7. There is a hyperechoic (soft tissue‐like) linear structure located in the pericardial sac, penetrating from caudoventral to craniodorsal and in close proximity with the ventral aspect of the heart, consistent with a wooden skewer (arrows). Pericardial effusion and small areas of pleural effusion are also present (*). V (ventral), ^ (cranial). Transverse (B) and sagittal (C) CT views of the thorax and abdomen of case 7 displayed in a soft tissue window. A 77‐mm hyperattenuating linear structure is evident extending from the left diaphragmatic outline to the right, in a dorsoventral direction from the caudoventral aspect of the left caudal lung lobe until the fourth sternebrae. The structure is caudal to the cardiac silhouette. There is an accumulation of small quantities of free fluid on its ventral aspect. The soft tissue structures surrounding it present mild hyperattenuation. The image is consistent with a wooden skewer (arrows) causing mild to moderate pleural effusion (*). RS (right), LI (left), P (dorsal), A (ventral). (D) Intraoperative view (case 7). A median sternotomy and cranial coeliotomy have been performed. The wooden skewer had penetrated the thoracic cavity from the stomach, through the left crus of the diaphragm and through the pericardium. A pericardiectomy has been performed (arrow) to allow removal of the entire skewer (*) from the pericardium
Surgical exploration was performed in all 11 cases; the surgical findings and management are summarised in Table 1. In 10 of 11 cases (91%), the surgery was performed at a referral centre. In one of 11 cases (9%) (case 9), the initial surgery was performed at the primary clinic, identifying a wooden skewer penetrating from the stomach into the pleural cavity. Surgical removal of the skewer, debridement of the gastric and diaphragmatic points of perforation and primary closure was performed at that time. The dog was presented to the referral practice following acute postoperative deterioration, where it underwent a second exploratory surgery, including thoracotomy.
The median anaesthetic time was 240 minutes (165 to 570) and mean surgical time 123 minutes (±50). A coeliotomy was performed in 10 of 11 cases (91%). In these cases, six of 10 had a concurrent diaphragmotomy and four of 10 had a median sternotomy. Case 5 underwent median sternotomy alone.
In all cases, a wooden foreign body was identified, penetrating the thoracic cavity from the stomach (n=10) or duodenum (n=1). In all cases, the wooden foreign body was identified as a wooden skewer (Figs 1D and 2). Extraction of the foreign body and debridement of the penetrating tract and concurrent adhesions was performed in all cases with the exception of case 9, in which the foreign body had already been removed by the referring clinician. Lung lobectomy (n=3), pericardiectomy (n=2), partial liver lobectomy (n=1) and splenectomy (n=1) were required. The wooden skewer in case 2 was penetrating both the accessory lung lobe and the pericardium, causing profuse haemorrhage. Intraoperative transfusion of one unit of packed red blood cells (canine packed red blood cells, Pet Blood Bank UK) and half unit of fresh frozen plasma (canine fresh frozen plasma, Pet Blood Bank UK) was required for stabilisation. A lung lobectomy of the accessory lung lobe was performed, and the pericardial defect was primarily closed and augmented with a mediastinal patch. In case 5, the wooden skewer was penetrating through the right caudal, middle and cranial lung lobes. A partial lung lobectomy of these three lobes was performed, preserving the accessory lung lobe. Transfusion of one unit of packed red blood cells was also required in this case. A thoracic drain was placed in nine of 11 cases (82%). In cases 3 and 6, a Jackson–Pratt abdominal drain was placed. Peri‐ and postoperative broad‐spectrum antibiotics were administered in all cases for 84 hours (n=1), 7 days (n=1), 10 days (n=6), 14 days (n=2) and 21 days (n=1).
FIG 2.
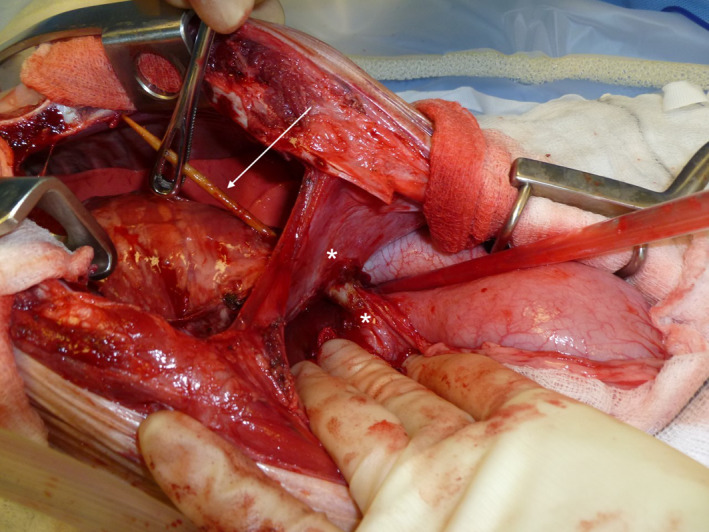
Intraoperative view (case 11). A median sternotomy and cranial coeliotomy have been performed. The wooden skewer (arrow) can be seen penetrating the thoracic cavity from the gastric lesser curvature, through the left crus of the diaphragm and the ventral aspect of the pericardium. The adhesions present between the gastric lesser curvature, the left medial hepatic lobe and left hemi‐diaphragm had been partially debrided at the time of the photograph (*)
Short‐term postoperative complications occurred in three of 11 cases (27%): two mild and one resulting in death. Case 5 developed transient azotaemia during the first 24 hours postoperatively, which resolved uneventfully with intravenous fluid stabilisation. However, 72 hours postoperatively, the patient's clinical status deteriorated, meeting the systemic inflammatory response syndrome (SIRS) criteria. Thoracic ultrasonography identified a pleural effusion, which was confirmed cytologically as a pyothorax. The owner declined further treatment and the dog was euthanased. Case 6 developed a pneumothorax immediately after surgery, which was successfully managed with intermittent drainage of the thoracic cavity via thoracic drain. Case 9 developed mild hypoalbuminaemia and peripheral oedema 48 hours postoperatively. This dog had resumed voluntary food intake and no further intervention was deemed necessary. No long‐term postoperative complications were recorded in the clinical records of the cases.
Ten of the 11 (91%) dogs survived to discharge. Of these 10 dogs, six were still alive at the time of writing, one was euthanased 5 years later for reasons unrelated to this study and three were lost to follow‐up.
DISCUSSION
The reported data suggest that cranially migrating intra‐abdominal wooden foreign bodies penetrating the thoracic cavity can result in clinically challenging scenarios affecting multiple organs and body systems. The results of this study highlight their variable clinical presentations, diagnosis, management and overall successful outcomes, with a 91% (10/11) survival to discharge.
Intrathoracic cranial migration of wooden skewer‐like foreign bodies has been sporadically reported in the veterinary literature (Matteuci et al. 1999, Hunt et al. 2004, Sereda et al. 2009, Stander & Kirberger 2011, Choi & Han 2017). The most common clinical signs noticed in these reports were pyrexia (Sereda et al. 2009, Stander & Kirberger 2011, Choi & Han 2017) and draining sinus tracts (Matteuci et al. 1999, Hunt et al. 2004), which differ from the cases presented in this study. This finding is not unexpected due to the pleomorphic characteristics of these types of injuries depending on the location of the foreign body. In our study, which assessed cases that only were presented with migration of the wooden skewer cranially into the thoracic cavity, thoracic or abdominal wall involvement was identified in only two of 11 cases (18%), causing an abdominal sinus tract in one case and thoracic wall swelling in another. This is likely explained by the short duration of clinical signs [<14 days in 8/11 cases (73%)]; a later presentation or diagnosis could lead to further migration of the foreign body into the body wall as was seen in cases 10 and 11, which presented at 14 and 21 days, respectively.
Although the remaining clinical signs identified here were non‐specific, gait abnormalities were identified in three of 11 cases, emphasising the multi‐disciplinary approach required in some dogs. In two cases presenting with right thoracic limb lameness, the wooden skewer was localised within the right hemithorax. In the third patient, presenting with kyphosis and ataxia, the wooden skewer was perforating through the mediastinum, into the pericardium. All gait abnormalities were resolved immediately postoperatively. Gait abnormalities were also reported by Stander & Kirberger (2011) where two cases displayed a thoracic limb lameness and one presented with generalised ataxia. Interestingly, this gait abnormality is also widely recognised in bovine species where a traumatic reticuloperitonitis or reticulopericarditis is commonly identified secondary to a migrating foreign body from the stomach (Braun et al. 2018). It is possible that in all these species, these patients are utilising an antalgic manoeuvre, in order to alleviate the discomfort associated with movement of the foreign body and surrounding inflamed tissues, when ambulating.
Several diagnostic imaging techniques were used to detect the wooden foreign body in this study. Due to their radiolucency, thoracic radiographs failed to identify the wooden skewer in three of four cases (75%), which is in agreement with previously reported studies (Stander & Kirberger 2011). However, despite its poor sensitivity in directly identifying a wooden foreign body, radiography can assist in the diagnosis of secondary changes and electing the subsequent diagnostic and therapeutic techniques (Stander & Kirberger 2011). Ultrasonography (cases 6 and 10) and echocardiography (case 7) were successful in identification of the foreign body. Ultrasound has been shown to facilitate foreign body diagnosis in the abdominal cavity, body walls and other soft tissues (Penninck & Mitchell 2003); however, the presence of air within the lung lobes limits the ultrasonographic evaluation to structures in or near the thoracic wall (Reichle & Wisner 2000). Furthermore, it can be difficult to establish the exact location, number and length of a wooden skewer, particularly if fragmentation is present or occurs intraoperatively (Scalf 2006). When compared with MRI, CT has been reported to be the more sensitive technique for detecting wooden foreign material (Nicholson et al. 2008, Ober et al. 2008) and has been recommended for global screening of impalement injuries in canine patients (Matiasovic et al. 2018). In the data presented in this study, CT proved to be the most sensitive technique; eight of eight scanned cases achieved a final diagnosis preoperatively. Although MRI has high sensitivity in the evaluation of pharyngeal foreign bodies and wooden stick injuries (Dobromylskyj et al. 2008) and was useful to identify the wooden skewer in cases 2 and 10, our results suggested that the inflammatory reaction and secondary changes can mask the underlying intrathoracic wooden skewer, as occurred in case 5, which required concurrent CT to achieve a definitive diagnosis. Respiratory and cardiac motion artefact present in MRI studies may also play a role in obscuring the foreign body and secondary lesions (Kraft et al. 2007). Furthermore, if a diagnostic MRI is pursued, a preliminary radiographic study should be taken to rule out the presence of metallic parts within the wooden skewer or concurrent metallic foreign bodies. CT is, therefore, advantageous in eliminating the requirement for this.
Intrathoracic cranial migration of the wooden skewer from the gastrointestinal tract resulted in pulmonary (cases 1, 2 and 5) and pericardial (cases 2, 7 and 10) injuries. Thoracic approaches were attempted via diaphragmotomy in eight of 11 cases, of which only one required conversion to a median sternotomy due to active haemothorax (case 2). Transdiaphragmatic thoracotomy provides enough exposure to inspect the caudal hemithoraces, the mediastinum and the caudal pericardial surface (Hunt 2018) without the morbidity and mortality intrinsically related to median sternotomy (Pelsue et al. 2002, Dean et al. 2020). Furthermore, the upper gastrointestinal tract is known to have lower bacterial concentrations (Cornell 2018). Therefore, foreign bodies perforating from this location into the thorax may cause mild septic and/or different degrees of chemical peritonitis and pleuritis without causing severe pyothorax requiring intense debridement (Kirby 2018). As no gross pyothorax was seen in any of these cases, the authors advocate for a conservative approach to these injuries when bicavitary, by approaching the foreign body via coeliotomy and diaphragmotomy in the first instance and using median sternotomy or lateral thoracotomies to improve the visualisation only if required. For cases presenting with tricavitary perforation (including in the pericardium) where the foreign body is located more cranially or, where the location of the foreign body is limited only to the thorax in the preoperative imaging, median sternotomy or a lateral intercostal approach may be the approach of choice.
In the limited number of previously described cases of intrathoracic penetrating wooden foreign bodies (Hunt et al. 2004, Stander & Kirberger 2011, Choi & Han 2017), an excellent short‐term prognosis was reported when surgical management was undertaken. The majority of dogs (4/5) presenting with this clinical entity in the previous reports recovered uneventfully and survived to discharge if surgery had been performed (Hunt et al. 2004, Stander & Kirberger 2011, Choi & Han 2017), including when cardiac or pericardiac injuries were present (Sereda et al. 2009). However, the previously reported non‐survival case was euthanased at presentation due to the age of the patient, severity of thoracic changes and surgical risk (Stander & Kirberger 2011).
When assessing the previously described outcomes of cases presenting with intra‐abdominal migration of the wooden skewer (Hunt et al. 2004, Stander & Kirberger 2011), all nine cases survived when surgical treatment was pursued. From the obtained data in these studies, the migration had presumably originated from the upper gastrointestinal tract (stomach or duodenum) (Hunt et al. 2004, Stander & Kirberger 2011). In the data presented from the current study, 10 of 11 cases (91%) survived to discharge and only one developed a major complication, prompting elective euthanasia. In the eight cases in our study with long‐term follow‐up, prognosis for those recovering uneventfully from surgery was excellent with no cases reported to develop any complications beyond 3 months postoperatively. The null hypothesis previously stated was therefore rejected. However, considering the morbidity presented by all these cases, the authors recommend investigations and safe retrieval of wooden skewers via endoscopy or gastrotomy as soon as possible, ideally after ingestion has been noticed, to prevent latter penetration and need for major surgery.
The limitations of this study include those inherent to retrospective studies. Firstly, the small number of cases precluded statistical analysis, and secondly, the retrospective and multi‐centric nature of the study may have introduced historical data recording inaccuracies, as well as variability from the multiple attending surgeons and referral institutions.
In conclusion, despite the challenges of managing wooden skewers penetrating the thoracic cavity from the gastrointestinal tract, the majority of the patients are stable to undergo diagnostic tests, surgical exploration and management with a low morbidity and excellent short‐ and long‐term prognosis. The recommendation to refer such cases to a multi‐disciplinary specialist setting may be prudent due to the complex diagnostic and surgical requirements of these cases.
Conflict of interest
None of the authors of this article has a financial or personal relationship with other people or organisations that could inappropriately influence or bias the content of the paper.
Acknowledgements
The authors would like to thank Nicolas Israeliantz Gunz for his contribution in the diagnostic imaging figure descriptions.
References
- Appleby, R. , Zur Linden, A. , Singh, A. , et al. (2015) Computed tomography diagnosis of a thoracic and abdominal penetrating foreign body in a dog. Canadian Veterinary Journal 56, 1149‐1152 [PMC free article] [PubMed] [Google Scholar]
- Braun, U. , Warislohner, S. , Torgerson, P. , et al. (2018) Clinical and laboratory findings in 503 cattle with traumatic reticuloperitonitis. BMC Veterinary Research 14, 66. 10.1186/s12917-018-1394-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan, K. E. & Ihrke, P. J. (1983) Grass awn migration in dogs and cats: a retrospective study of 182 cases. Journal of the American Veterinary Medical Association 182, 1201 [PubMed] [Google Scholar]
- Choi, Y. D. & Han, H. J. (2017) Pyothorax induced by an intrathoracic foreign body in a miniature dachshund: migration of a popsicle stick from the stomach. The Journal of Veterinary Medical Science 79, 1398‐1403. 10.1292/jvms.17-0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornell, K. (2018) Stomach. In: Veterinary Surgery Small Animal. 2nd edn. Eds Johnston S. A. and Tobias K. M.. Elsevier, St. Louis, MO, USA. pp 1700‐1732 [Google Scholar]
- Dean, B. , Anderson, T. , Garcia‐Pertierra, S. , et al. (2020) Diaphragmotomy to aid exposure during hepatobiliary surgery: a multi‐centre retrospective review of 31 dogs. Journal of Small Animal Practice 61, 278‐284. 10.1111/jsap.13121 [DOI] [PubMed] [Google Scholar]
- Dobromylskyj, M. J. , Dennis, R. , Ladlow, J. F. , et al. (2008) The use of magnetic resonance imaging in the management of pharyngeal penetration injuries in dogs. Journal of Small Animal Practice 49, 74‐79. 10.1111/j.1748-5827.2007.00436.x [DOI] [PubMed] [Google Scholar]
- Follette, C. M. , Giuffrida, M. A. , Balsa, I. M. , et al. (2020) A systematic review of criteria used to report complications in soft tissue and oncologic surgical clinical research studies in dogs and cats. Veterinary Surgery 49, 61‐69. 10.1111/vsu.13279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt, G. B. (2018) Thoracic wall. In: Veterinary Surgery Small Animal. 2nd edn. Eds Johnston S. A. and Tobias K. M.. Elsevier, St. Louis, MO, USA. pp 2002‐2018 [Google Scholar]
- Hunt, G. B. , Worth, A. & Marchevsky, A. (2004) Migration of wooden skewer foreign bodies from the gastrointestinal tract in eight dogs. Journal of Small Animal Practice 45, 362‐367. 10.1111/j.1748-5827.2004.tb00249.x [DOI] [PubMed] [Google Scholar]
- Johnson, M. D. , Magnusson, K. D. , Shmon, C. L. , et al. (2006) Porcupine quill injuries in dogs: a retrospective of 296 cases (1998‐2002). The Canadian Veterinary Journal 47, 677‐682 [PMC free article] [PubMed] [Google Scholar]
- Kirby, B. M. (2018) Peritoneum and retroperitoneum. In: Veterinary Surgery Small Animal. 2nd edn. Eds Johnston S. A. and Tobias K. M.. Elsevier, St. Louis, MO, USA. pp 1603‐1636 [Google Scholar]
- Kraft, S. , Randall, E. , Wilhem, M. , et al. (2007) Development of a whole body magnetic resonance imaging protocol in normal dogs and canine cancer patients. Veterinary Radiology & Ultrasound 48, 212‐220. 10.1111/j.1740-8261.2007.00231.x [DOI] [PubMed] [Google Scholar]
- Lamb, C. R. , White, R. N. & McEvoy, F. J. (1994) Sinography in the investigation of draining tracts in small animals: retrospective review of 25 cases. Veterinary Surgery 23, 129‐134 [DOI] [PubMed] [Google Scholar]
- Lamb, C. R. , Pope, E. H. & Lee, K. C. (2017) Results of computed tomography in dogs with suspected wooden foreign bodies. Veterinary Radiology & Ultrasound 58, 144‐150. 10.1111/vru.12457 [DOI] [PubMed] [Google Scholar]
- Matiasovic, M. , Halfacree, Z. J. , Moores, A. , et al. (2018) Surgical management of impalement injuries to the trunk of dogs: a multicentre retrospective study. Journal of Small Animal Practice 59, 139‐146. 10.1111/jsap.12767 [DOI] [PubMed] [Google Scholar]
- Matteuci, M. L. , Spaulding, K. , Dassler, C. , et al. (1999) Ultrasound diagnosis: intra‐abdominal wood foreign body. Veterinary Radiology & Ultrasound 40, 513‐516. 10.1111/j.1740-8261.1999.tb00384.x [DOI] [PubMed] [Google Scholar]
- Nicholson, I. , Halfacree, Z. , Whatmough, C. , et al. (2008) Computed tomography as an aid to management of chronic oropharyngeal stick injury in the dog. Journal of Small Animal Practice 49, 451‐457. 10.1111/j.1748-5827.2008.00591.x [DOI] [PubMed] [Google Scholar]
- Ober, C. P. , Jones, J. C. , Larson, M. M. , et al. (2008) Comparison of ultrasound, computed tomography, and magnetic resonance imaging in detection of acute wooden foreign bodies in the canine manus. Veterinary Radiology & Ultrasound 49, 411‐418. 10.1111/j.1740-8261.2008.00399.x [DOI] [PubMed] [Google Scholar]
- Pelsue, D. H. , Monnet, E. , Gaynor, J. S. , et al. (2002) Closure of median sternotomy in dogs: suture versus wire. Journal of the American Animal Hospital Association 38, 569‐576. 10.5326/0380569 [DOI] [PubMed] [Google Scholar]
- Penninck, D. & Mitchell, S. L. (2003) Ultrasonographic detection of ingested and perforated foreign bodies in four dogs. Journal of the American Veterinary Medical Association 233, 206‐209. 10.2460/javma.2003.223.206 [DOI] [PubMed] [Google Scholar]
- Pratt, C. L. , Reineke, E. L. & Drobatz, K. J. (2014) Sewing needle foreign body ingestion in dogs and cats: 65 cases (2000‐2012). Journal of the American Veterinary Medical Association 245, 302‐308 [DOI] [PubMed] [Google Scholar]
- Reichle, J. K. & Wisner, E. R. (2000) Non‐cardiac thoracic ultrasound in 75 feline and canine patients. Veterinary Radiology & Ultrasound 41, 154‐162. 10.1111/j.1740-8261.2000.tb01470.x [DOI] [PubMed] [Google Scholar]
- Scalf, R. (2006) Canine traumatic injury: sticks, bullets and arrows. Proceedings of the Western Veterinary Conference, February 19 to 23. W.B. Saunders, Las Vegas, NV, USA.
- Schultz, R. M. & Zwingenberger, A. (2008) Radiographic, computed tomographic, and ultrasonographic findings with migrating intrathoracic grass awns in dogs and cats. Veterinary Radiology & Ultrasound 49, 249‐255 [DOI] [PubMed] [Google Scholar]
- Sereda, N. C. , Towl, S. , Maisenbacher, H. W. 3rd , et al. (2009) Intracardiac foreign body in a dog. Journal of Veterinary Cardiology 11, 53‐58. 10.1016/j.jvc.2009.03.002 [DOI] [PubMed] [Google Scholar]
- Stander, N. & Kirberger, R. M. (2011) Diagnostic imaging of migrating kebab (sosatie) sticks – a review of 8 cases. Journal of the South African Veterinary Association 82, 160‐165 [DOI] [PubMed] [Google Scholar]


