Abstract
Objectives
Hypospadias is a congenital disease characterized by morphological abnormalities of the penis, including abnormal urethral opening and penile flexion, which cause urination disorders and/or sexual intercourse difficulty. Various factors have been suggested to cause this anomaly, but evidence concerning risk factors causing this anomaly is insufficient. We evaluated the etiology of hypospadias in Japan using the Common Database of the National Hospitals' Neonatal study group.
Study design
We retrospectively evaluated 7,865 male neonates registered in the NICU Common Database of the National Hospitals' Neonatal study group. The subjects were divided into two groups by the presence (n = 43) or absence (n = 7,822) of hypospadias. Statistical analyses were performed to compare nominal variables between the groups by Fisher's direct establishment calculation method and logistic regression analyses.
Results
A univariate analysis showed significant between‐group differences in hypertensive disorders in pregnancy (odds ratio [OR]: 4.02, 95% confidence interval [CI]: 1.95–7.90), placental weight <−1.28 standard deviation (SD; OR: 5.06, 95% CI: 2.45–10.32), abnormal placental cord insertion (OR: 4.7, 95% CI: 2.62–9.76), birth length <−2SD (OR: 10.56, 95% CI: 5.00–21.1) and birth weight <−2SD (OR: 8.17, 95% CI: 4.17–15.68). A multivariate analysis showed a significant between‐group difference in hypertensive disorders of pregnancy (adjusted OR [AOR]: 2.30, 95% CI: 1.09–4.85), abnormal placental cord insertion (AOR: 3.69, 95% CI: 1.83–7.44) and birth length <−2SD (AOR: 3.44, 95% CI: 1.26–9.42).
Conclusion
Abnormal placental cord insertion, hypertensive disorders of pregnancy and birth length may be involved in hypospadias development in male neonates in conjunction with placental dysfunction in early pregnancy.
Keywords: abnormal placental cord insertion, birth length, hypertensive disorders of pregnancy, hypospadias, NICU
Abbreviations
- 95% CI
95% confidence interval
- AOR
adjusted odds ratio
- GDM
gestational diabetes mellitus
- NHO
National Hospital Organization
- NICU
neonatal intensive care unit
- SGA
small for gestational age
1. INTRODUCTION
Hypospadias is a congenital disease characterized by an abnormal morphology of the penis, causing urination disorders due to abnormal opening of the urethra and difficulty engaging in sexual intercourse in the future due to penile flexion (van der Horst & de Wall, 2017). The frequency of hypospadias is 5.2–34.2/10,000 males in general (Bergman et al., 2015; Springer, van den Heijkant, & Baumann, 2016; Yu et al., 2019) and 3.9–12.3/10,000 in Japanese boys, showing racial differences (Kurahashi et al., 2004; Michikawa et al., 2019).
The present study evaluated the clinical features of neonates with hypospadias and explored the factors related to hypospadias in males, using the Common NICU Database created for the neonatal study group of the National Hospitals' Organization in Japan.
2. MATERIAL AND METHODS
A total of 17,250 neonates were registered in the NICU Common Database from 2010 to 2014 and from 2016 to February 2019, and 9,345 of them were males. Among the 9,345 male neonates, 1,480 were excluded due to the exclusion criteria (twins, triplets and cases with deficient data). A total of 7,865 male neonates were thus available for the present study.
The subjects were separated into two groups: 7822 neonates without hypospadias were included in Group A, and 43 neonates with hypospadias were in Group B, and the following clinical features were compared and examined between these groups: maternal information, placenta information, and neonatal information (Figure 1). This information was collected from chart review, and they had been previously reported in relation to be related to fetal development and the advancement development of hypospadias. Maternal age ≥35 years old, fertility treatment, alcohol history, smoking status and presence of gestational diabetes mellitus (GDM) or hypertensive disorders in pregnancy were collected as maternal information. Placental weight <−1.28 standard deviation (SD; Ogawa et al., 2016) and abnormal placental cord insertion (velamentous and marginal cord insertions) were collected as placenta information. Birth length <−2SD, birth weight <−2SD, head circumference <−2SD, small for gestational age (SGA; <−2SD for both weight and height) and cryptorchism were collected as neonatal information.
FIGURE 1.
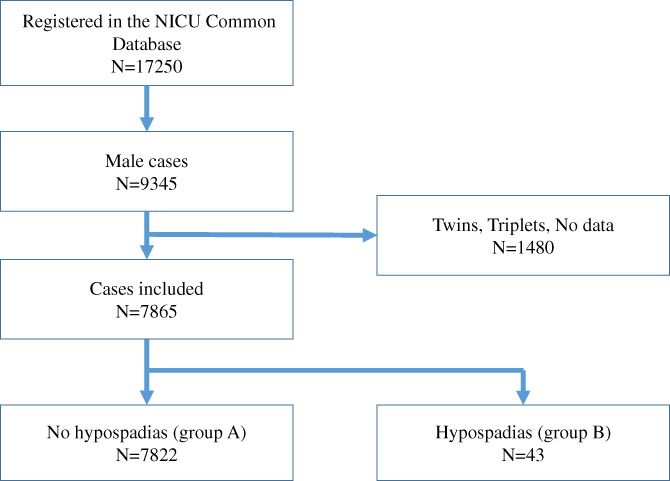
Flowchart of the study
We declared that this study was approved by an ethics committee and/or follows the tenants of the Declaration of Helsinki and was approved by the Ethics Committee of the National Hospital Organization Kokura Medical Center. (Approval number: REC2021‐009). Written informed consent was obtained from the parents.
Statistical analyses were performed to compare nominal variables between the groups by Fisher's direct establishment calculation method and logistic regression analyses. p < .05 were considered to indicate statistical significance. A univariate analysis was performed to identify significant factors. Then, all factors with a p < .05 in the univariate analysis were included in a multivariate analysis. In this way, we protected the study‐wide p value of .05. All statistical analyses were performed using EZR (Kanda, 2013).
3. RESULTS
The average gestation period for all male neonates registered was 36.7 ± 4.1 weeks, and the average weight at birth was 2,564 ± 725.8 g. The median SD of the birth weight was −0.19SD (interquartile range: −0.94 to 0.61), and the median SD of the birth length was −0.19SD (interquartile range: −0.58 to 0.89). In our data, the rate of abnormal cord insertion was 486 (6.2%) in marginal cases and 121 (1.5%) in velamentous cases. Hypospadias was associated with anal atresia (n = 2), hydronephropathy (n = 1), bifid scrotum (n = 1), cryptorchidism (n = 1), and spina bifida (n = 1). A univariate analysis showed a significant difference between the two groups with regard to hypertensive disorders of pregnancy as maternal information. Maternal age ≥35 years old, fertility treatment, alcohol habit, smoking habit and a history of GDM did not show any significant difference between the two groups. However, significant differences were observed between the two groups with regard to placental weight <−1.28SD and abnormal placental cord insertion (Table 1). There was also a significant difference between the two groups with regard to birth length <−2SD and birth weight <–2SD as neonatal information. There was no significant difference in the head circumference, SGA or presence of cryptorchism (Table 2).
TABLE 1.
A univariate analysis of the maternal and placental information in Groups A and B
| N | Group A | % | Group B | % | Odds ratio | 95% CI | p Value | ||
|---|---|---|---|---|---|---|---|---|---|
| Maternal age ≥35 years | 7,678 | 2,306/7,635 | 30.2 | 14/43 | 32.6 | 1.11 | 0.54 | 2.18 | .74 |
| Multipara | 7,636 | 3,851/7,594 | 50.7 | 18/42 | 42.9 | 0.72 | 0.37 | 1.4 | .35 |
| Fertility treatment | 7,450 | 807/7,407 | 10.9 | 3/43 | 7 | 0.61 | 0.12 | 1.93 | .62 |
| Alcohol | 5,834 | 209/5,794 | 3.6 | 3/40 | 7.5 | 2.16 | 0.42 | 6.92 | .17 |
| Smoking | 5,817 | 401/5,777 | 6.9 | 1/40 | 2.5 | 0.34 | 0.01 | 2.04 | .52 |
| GDM | 7,647 | 555/7,604 | 7.3 | 0/43 | 0 | 0 | 0 | 1.14 | .07 |
| Hypertensive disorders of pregnancy | 7,650 | 814/7,607 | 10.7 | 14/43 | 32.6 | 4.02 | 1.95 | 7.9 | <.01 |
| Placental weight <−1.28SD | 5,715 | 853/5,679 | 15 | 17/36 | 47.2 | 5.06 | 2.45 | 10.3 | <.01 |
| Abnormal placental cord insertion | 5,292 | 593/5,255 | 11.3 | 14/37 | 37.8 | 4.7 | 2.62 | 9.76 | <.01 |
Abbreviations: CI, confidence interval; GDM, gestational diabetes mellitus.
TABLE 2.
A univariate analysis of the neonatal information in Groups A and B
| N | Group A | % | Group B | % | Odds ratio | 95% CI | p Value | ||
|---|---|---|---|---|---|---|---|---|---|
| Birth length <−2SD | 7,865 | 308/7,822 | 3.9 | 13/43 | 30.2 | 10.56 | 5 | 21.1 | <.01 |
| Birth weight <−2SD | 7,865 | 633/7,822 | 8.1 | 18/43 | 41.9 | 8.17 | 4.17 | 15.6 | <.01 |
| HC <−2SD | 7,865 | 117/7,822 | 1.5 | 1/43 | 2.3 | 1.56 | 0.03 | 9.39 | .47 |
| SGA | 7,865 | 38/7,822 | 0.5 | 1/43 | 2.3 | 4.87 | 0.11 | 30.3 | .19 |
| With cryptorchidism | 7,865 | 29/7,822 | 0.4 | 1/43 | 2.3 | 6.39 | 0.15 | 40.4 | .15 |
Abbreviations: CI, confidence interval; HC, head circumference; SGA, small for gestational age; SD, standard deviation.
A logistic regression analysis was then performed for hypertensive disorders of pregnancy, placental weight <−1.28SD, abnormal placental cord insertion, birth length <−2SD and birth weight <−2SD, with all of these factors showing significant differences in a univariate analysis between the two groups. We adjusted five factors in the regression analysis, hypertensive disorders of pregnancy, placental weight <−1.28SD, abnormal placental cord insertion, birth length <−2SD, and birth weight <−2SD. A multivariate analysis revealed significant differences in hypertensive disorders of pregnancy, abnormal placental cord insertion and birth length <−2SD between the two groups (Table 3). There was no significant difference in placental weight or birth weight between the two groups according to the multivariate analysis.
TABLE 3.
A multivariate analysis of factors associated with hypospadias
| AOR | 95% CI | p Value | ||
|---|---|---|---|---|
| Hypertensive disorders of pregnancy | 2.30 | 1.09 | 4.85 | .029* |
| Placental weight <−1.28SD | 2.04 | 0.88 | 4.67 | .092 |
| Abnormal placental cord insertion | 3.69 | 1.83 | 7.44 | .000263* |
| Birth length <−2SD | 3.44 | 1.26 | 9.42 | .016* |
| Birth weight <−2SD | 1.58 | 0.55 | 4.51 | .392 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; SD, standard deviation.
p < .05.
4. DISCUSSION
Various factors have been described as causes of hypospadias, including synthetic abnormalities of androgen in fetal testes (Batch, Evans, Hughes, & Patterson, 1993), deficient secretion of hCG due to placental dysfunction (Toufaily, Roberts, Westgate, Hunt, & Holmes, 2018), maternal elderly childbirth (Fisch et al., 2001), low birth weight (Hashimoto et al., 2016; Hussain et al., 2002), oral contraceptives (Nørgaard, Wogelius, Pedersen, Rothman, & Sørensen, 2009) and genetic abnormalities (e.g., FOXO3 [Ross et al., 2011], FGF10 [Haid et al., 2020]).
In the present study, a data‐based analysis using the NICU Common Database of NHO neonatal centers showed that abnormal placental cord insertion, hypertensive disorders of pregnancy, and birth length were significantly correlated with the occurrence of hypospadias. Several author reported that placenta cord insertion is established around 15 week's gestation. (Knofler et al., 2019; Turco & Moffett, 2019), and the onset of penile formation hypospadias occurs at 10–14 weeks' gestation (Blaschko, Cunha, & Baskin, 2012) under stimulation of testosterone. At 10–14 weeks' fetal gestation, the secretion of hCG and fetal testosterone in the placenta are both increased, and placental dysfunction at this time may cause abnormal formation of the urethra (Toufaily et al., 2018). Although small placentas are more prone to placental dysfunction than larger ones (Longtine & Nelson, 2011), there was no significant difference in the placental weight by the presence of hypospadias in this study. A decrease in placental weight at birth does not always indicate placental dysfunction during the critical period of penile formation in the early stage of pregnancy, as placental size is affected by various effects, such as calcification and blood flow abnormalities (Longtine & Nelson, 2011), throughout pregnancy. However, the presence of abnormal placental cord insertion reportedly causes placental dysfunction from early pregnancy and induces nutritional damage to fetuses, easily resulting in SGA or a low‐birth‐weight infant (Ismail, Hannigan, O'Donoghue, & Cotter, 2017). Abnormal placental cord insertion is completed at 9–11 weeks' gestation (Hasegawa et al., 2006), after which the adhesion site of the umbilical cord is not moved. Therefore, male fetuses with abnormal placental cord insertion may develop hypospadias due to placental dysfunction and nutritional disorders from the early stage of pregnancy.
A short length at birth and hypertensive disorders of pregnancy were also significantly and independently correlated with the onset of hypospadias in our study. While previous reports have shown that SGA is related to the development of hypospadias, our study showed that a short birth length was more closely associated with the occurrence of hypospadias than a low birth weight in male neonates. A short birth length is associated with placental and umbilical cord abnormalities in early pregnancy (Burton & Jauniaux, 2018; Ismail et al., 2017). In addition to the placental function, the birth weight is greatly affected by maternal factors, such as GDM and the fetus's condition, such as subcutaneous edema in the late stage of pregnancy; however, the birth length is less markedly affected by those factors and may instead be strongly influenced by placental dysfunction in the early stage of pregnancy. Therefore, the birth length may be significantly related to hypospadias. Hypertensive disorders of pregnancy is also thought to cause placental dysfunction. In hypertensive disorders of pregnancy, remodeling failure of the spiral arterioles of the placenta reduces the oxygen supply from the mother and causes hypoxic chorionic mesothemble and placental dysfunction (Roberts & Hubel, 2009). Hypertensive disorders of pregnancy might thus be significantly associated with the occurrence of hypoplasia. Consequently, both abnormal placental cord insertion and hypertensive disorders of pregnancy may induce placental dysfunction, which can cause deficient secretion of hCG and testosterone in the early stage of pregnancy and lead to hypospadias in male fetuses. A short length at birth may be induced by placental dysfunction in the early stage of pregnancy and is independently associated with the formation of hypospadias. On the other hand, in female babies, abnormal placental cord insertion was also significantly associated with short birth length in females (p < .05 data not shown). While there have been many reports that hypospadias is strongly associated with cryptorchism (Arendt et al., 2016), no significant correlation was noted in the present study. The occurrence of cryptorchism is also thought to be related to the lack of testosterone activity. Penile formation occurs under the action of testosterone in early pregnancy, while testosterone affects testicular descent in the latter half of pregnancy (Hutson, Li, Southwell, Newgreen, & Cousinery, 2015). Therefore, we only noted a low association of hypospadias and cryptorchidism in our study.
4.1. Limitations
Several limitations associated with the present study warrant mention. First, the NICU Common Database was established based on patients who were transferred to the intensive care unit of NHO hospitals. Second, a pathological examination of the placenta was not performed. Third, the degree of hypospadias was not determined. Therefore, further studies will be necessary to verify the etiologically related factors of hypospadias.
5. CONCLUSION
Abnormal placental cord insertion, hypertensive disorders of pregnancy and birth length are significantly related to the occurrence of hypospadias in neonates hospitalized in the NICU. These factors are strongly correlated with placental dysfunction in the early stage of pregnancy and may induce hypospadias in male fetuses.
MEMBERS OF COLLABORATIVE RESEARCH IN NATIONAL HOSPITAL ORGANIZATION NETWORK: PEDIATRIC AND PERINATAL GROUP OF 2021
Principal Investigators: Noriko Sugino, Motoki Bonno (Mie Chuo Medical Center, Mie, Japan), Toshinori Nakashima (Kokura Medical Center, Fukuoka, Japan), Toru Kuboi (Shikoku Medical Center for Children and Adults, Kagawa, Japan), Kou Kawada (Kyoto Medical Center, Kyoto, Japan), Kazuhiro Takahashi (Nagara Medical Center, GIfu, Japan), Kazuo Sato (Kyushu Medical Center, Fukuoka, Japan), Hiroshi Koga (Beppu Medical Center, Oita, Japan), Tsuneo Igarashi (Takasaki General Medical Center, Gunma, Japan), Toshimitu Takayanagi (Saga National Hospital, Saga, Japan), Motohiro Inotani (Fukuyama Medical Center, Hiroshima, Japan), Makoto Nakamura (Okayama Medical Center, Okayama, Japan), Yasuhiko Sera (Kure Medical Center, Hiroshima, Japan), Masashi Miharu (Tokyo Medical Center, Tokyo, Japan), Isamu Kamimaki (Saitama Hospital, Saitama, Japan).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Yoshihiro Sakemi and Takeshi Shono designed the study protocol and drafted the initial manuscript. Noriko Sugino and Motoki Bonno statistical support and designed the analysis. Toshinori Nakashima and Hironori Yamashita coordinate data collection; conceptualized and designed the study, reviewed the analysis. Yoshihiro Sakemi and Takeshi Shono reviewed and revised the manuscript. All authors approved the final manuscript as submitted.
ACKNOWLEDGMENTS
The thank the doctors of NHO Child Health and Development Research Meeting for helping us collect data. The author also thank Brian Quinn, the Editor‐in‐chief of Japan Medical Communication (https://www.japan-mc.co.jp), for the English language editing.
Sakemi, Y. , Shono, T. , Nakashima, T. , Yamashita, H. , Sugino, N. , & Bonno, M. (2022). Abnormal placental cord insertion, hypertensive disorders of pregnancy and birth length may be involved in development of hypospadias in male fetuses. Birth Defects Research, 114(8), 271–276. 10.1002/bdr2.1995
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Arendt, L. H. , Ramlau‐Hansen, C. H. , Wilcox, A. J. , Henriksen, T. B. , Olsen, J. , & Lindhard, M. S. (2016). Placental weight and male genital anomalies: A Nationwide Danish cohort study. American Journal of Epidemiology, 183(12), 1122–1128. 10.1093/aje/kwv336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batch, J. A. , Evans, B. A. , Hughes, I. A. , & Patterson, M. N. (1993). Mutations of the androgen receptor gene identified in perineal hypospadias. Journal of Medical Genetics, 30(3), 198–201. 10.1136/jmg.30.3.198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman, J. E. , Loane, M. , Vrijheid, M. , Pierini, A. , Nijman, R. J. , Addor, M. C. , … de Walle, H. E. (2015). Epidemiology of hypospadias in Europe: A registry‐based study. World Journal of Urology, 33(12), 2159–2167. 10.1007/s00345-015-1507-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaschko, S. D. , Cunha, G. R. , & Baskin, L. S. (2012). Molecular mechanisms of external genitalia development. Differentiation, 84(3), 261–268. 10.1016/j.diff.2012.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton, G. J. , & Jauniaux, E. (2018). Pathophysiology of placental‐derived fetal growth restriction. American Journal of Obstetrics and Gynecology, 218(2s), S745–s761. 10.1016/j.ajog.2017.11.577 [DOI] [PubMed] [Google Scholar]
- Fisch, H. , Golden, R. J. , Libersen, G. L. , Hyun, G. S. , Madsen, P. , New, M. I. , & Hensle, T. W. (2001). Maternal age as a risk factor for hypospadias. The Journal of Urology, 165(3), 934–936. [PubMed] [Google Scholar]
- Haid, B. , Pechriggl, E. , Nägele, F. , Dudas, J. , Webersinke, G. , Rammer, M. , … Oswald, J. (2020). FGF8, FGF10 and FGF receptor 2 in foreskin of children with hypospadias: An analysis of immunohistochemical expression patterns and gene transcription. Journal of Pediatric Urology, 16(1), 41.e41–41.e10. 10.1016/j.jpurol.2019.10.007 [DOI] [PubMed] [Google Scholar]
- Hasegawa, J. , Matsuoka, R. , Ichizuka, K. , Otsuki, K. , Sekizawa, A. , Farina, A. , & Okai, T. (2006). Cord insertion into the lower third of the uterus in the first trimester is associated with placental and umbilical cord abnormalities. Ultrasound in Obstetrics & Gynecology, 28(2), 183–186. 10.1002/uog.2839 [DOI] [PubMed] [Google Scholar]
- Hashimoto, Y. , Kawai, M. , Nagai, S. , Matsukura, T. , Niwa, F. , Hasegawa, T. , & Heike, T. (2016). Fetal growth restriction but not preterm birth is a risk factor for severe hypospadias. Pediatrics International, 58(7), 573–577. 10.1111/ped.12864 [DOI] [PubMed] [Google Scholar]
- Hussain, N. , Chaghtai, A. , Herndon, C. D. , Herson, V. C. , Rosenkrantz, T. S. , & McKenna, P. H. (2002). Hypospadias and early gestation growth restriction in infants. Pediatrics, 109(3), 473–478. 10.1542/peds.109.3.473 [DOI] [PubMed] [Google Scholar]
- Hutson, J. M. , Li, R. , Southwell, B. R. , Newgreen, D. , & Cousinery, M. (2015). Regulation of testicular descent. Pediatric Surgery International, 31(4), 317–325. 10.1007/s00383-015-3673-4 [DOI] [PubMed] [Google Scholar]
- Ismail, K. I. , Hannigan, A. , O'Donoghue, K. , & Cotter, A. (2017). Abnormal placental cord insertion and adverse pregnancy outcomes: A systematic review and meta‐analysis. Systematic Reviews, 6(1), 242. 10.1186/s13643-017-0641-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanda, Y. (2013). Investigation of the freely available easy‐to‐use software 'EZR' for medical statistics. Bone Marrow Transplantation, 48(3), 452–458. 10.1038/bmt.2012.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knofler, M. , Haider, S. , Saleh, L. , Pollheimer, J. , Gamage, T. , & James, J. (2019). Human placenta and trophoblast development: Key molecular mechanisms and model systems. Cellular and Molecular Life Sciences, 76(18), 3479–3496. 10.1007/s00018-019-03104-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurahashi, N. , Murakumo, M. , Kakizaki, H. , Nonomura, K. , Koyanagi, T. , Kasai, S. , … Kishi, R. (2004). The estimated prevalence of hypospadias in Hokkaido, Japan. Journal of Epidemiology, 14(3), 73–77. 10.2188/jea.14.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longtine, M. S. , & Nelson, D. M. (2011). Placental dysfunction and fetal programming: The importance of placental size, shape, histopathology, and molecular composition. Seminars in Reproductive Medicine, 29(3), 187–196. 10.1055/s-0031-1275515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michikawa, T. , Yamazaki, S. , Ono, M. , Kuroda, T. , Nakayama, S. F. , Suda, E. , … Japan Environment and Children's Study Group . (2019). Isoflavone intake in early pregnancy and hypospadias in the Japan environment and children's study. Urology, 124, 229–236. 10.1016/j.urology.2018.11.008 [DOI] [PubMed] [Google Scholar]
- Nørgaard, M. , Wogelius, P. , Pedersen, L. , Rothman, K. J. , & Sørensen, H. T. (2009). Maternal use of oral contraceptives during early pregnancy and risk of hypospadias in male offspring. Urology, 74(3), 583–587. 10.1016/j.urology.2009.04.034 [DOI] [PubMed] [Google Scholar]
- Ogawa, M. , Matsuda, Y. , Nakai, A. , Hayashi, M. , Sato, S. , & Matsubara, S. (2016). Standard curves of placental weight and fetal/placental weight ratio in Japanese population: Difference according to the delivery mode, fetal sex, or maternal parity. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 206, 225–231. 10.1016/j.ejogrb.2016.09.004 [DOI] [PubMed] [Google Scholar]
- Roberts, J. M. , & Hubel, C. A. (2009). The two stage model of preeclampsia: Variations on the theme. Placenta, 30 Suppl A, S32–S37. 10.1016/j.placenta.2008.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross, A. E. , Marchionni, L. , Phillips, T. M. , Miller, R. M. , Hurley, P. J. , Simons, B. W. , … Schaeffer, E. M. (2011). Molecular effects of genistein on male urethral development. The Journal of Urology, 185(5), 1894–1898. 10.1016/j.juro.2010.12.095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer, A. , van den Heijkant, M. , & Baumann, S. (2016). Worldwide prevalence of hypospadias. Journal of Pediatric Urology, 12(3), 152.e1–152.e7. 10.1016/j.jpurol.2015.12.002 [DOI] [PubMed] [Google Scholar]
- Toufaily, M. H. , Roberts, D. J. , Westgate, M. N. , Hunt, A. T. , & Holmes, L. B. (2018). Hypospadias, intrauterine growth restriction, and abnormalities of the placenta. Birth Defects Research, 110(2), 122–127. 10.1002/bdr2.1087 [DOI] [PubMed] [Google Scholar]
- Turco, M. Y. , & Moffett, A. (2019). Development of the human placenta. Development, 146(22), dev163428. 10.1242/dev.163428 [DOI] [PubMed] [Google Scholar]
- van der Horst, H. J. , & de Wall, L. L. (2017). Hypospadias, all there is to know. European Journal of Pediatrics, 176(4), 435–441. 10.1007/s00431-017-2864-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, X. , Nassar, N. , Mastroiacovo, P. , Canfield, M. , Groisman, B. , Bermejo‐Sanchez, E. , … Agopian, A. J. (2019). Hypospadias prevalence and trends in international birth defect surveillance systems, 1980‐2010. European Urology, 76(4), 482–490. 10.1016/j.eururo.2019.06.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


