Abstract
Purpose
To assess the clinical, radiographic, and patient‐reported outcome measures, including the success of screw‐retained monolithic zirconia implant‐supported restorations with CAD/CAM titanium abutments in the posterior region during a 1‐year follow‐up.
Methods
In a prospective case series, 50 molar sites in the posterior region of 46 patients with a minimum age of 18 years and sufficient bone volume and anatomical conditions for placing an implant (≥8 mm) and an anatomical restoration were included. Parallel‐walled implants with a conical connection were inserted in a two‐stage surgical procedure. Implant uncovering and healing abutment placement occurred 12 weeks after insertion. Two weeks after mucosa healing, a screw‐retained monolithic zirconia restoration with a CAD/CAM titanium abutment was placed. Clinical, radiographic, and patient‐reported outcome measures were collected at baseline before implant placement and then during the 1 month and 1 year follow‐ups.
Results
At the 1 year follow‐up, 49 restorations could be evaluated. The plaque accumulation, presence of calculus, bleeding tendency and peri‐implant inflammation indices were low, representing healthy peri‐implant conditions. The mean marginal bone level change between the 1 month and the 1 year follow‐up was −0.17 ± 0.46 mm. The mean patient satisfaction was high. The restoration success was, according to the modified USPHS criteria, 95.9%.
Conclusion
Monolithic zirconia implant‐supported restorations with CAD/CAM titanium abutments have very good clinical, radiographic and patient‐reported outcomes after 1 year in function.
Keywords: abutment, CAD/CAM, implant, monolithic, restorations, titanium, zirconia
What is known
Monolithic zirconia implant‐supported restorations with CAD/CAM titanium abutments are presumed to have high survival and success rates but studies assessing their clinical performance are scarce.
What this study adds
The first registered prospective case series study on this topic shows that monolithic zirconia implant‐supported single restorations with CAD/CAM abutments have excellent clinical, radiographic, and patient‐reported outcomes.
1. INTRODUCTION
Single tooth implant‐supported restorations are a reliable and commonly used treatment option to replace a missing tooth in partially edentulous patients. High survival rates for single tooth implants and restorations have been documented, but technical and biological complications can occur. 1 Technical complications include fracturing of the veneering material or abutment and screw loosening, whereas biological complications comprise peri‐implant soft tissue inflammation and a marginal bone loss of >2 mm. 2 , 3 The aim of any improvements in the design and the materials of implant‐supported restorations is to reduce these complications. Using monolithic zirconia instead of bilayered restorations could be a solution for veneering material chipping, especially in the posterior area. 4 , 5 , 6 , 7 The fracture loads of monolithic zirconia restorations are higher compared to bilayered restorations. 8
Regarding the material for abutments in the posterior region, a metal‐to‐metal interface of the implant and abutment is considered essential. The material properties of titanium, such as high fracture strength, are excellent for this purpose from a mechanical point of view. Using titanium abutments, especially in the molar area, leads to more favorable long‐term results compared to zirconia abutments. 9 , 10 The grayish discoloration of the peri‐implant mucosa associated with metal abutments in combination with a thin soft tissue phenotype can be reduced by using gold‐shaded titanium.
On the implant‐abutment connection level, the use of a conical connection appears to minimize screw loosening complications. 11 Furthermore, applying screw‐retained instead of cement‐retained restorations can reduce biological complications as it avoids excess cement. 12 , 13
Other than the restoration and abutment material and connection type, abutment design can influence the hard and soft peri‐implant tissues. Patient‐specific CAD/CAM abutments are increasingly used for implant‐supported restorations. The benefits include a customized emergence profile and a greater distance from the material junction to the peri‐implant bone level compared to stock abutments. Nonetheless, the number of studies on this topic is limited and mainly focused on the anterior region. 14 , 15 Clinical studies evaluating monolithic zirconia implant‐supported single restorations with CAD/CAM abutments are also scarce. A challenge with monolithic zirconia restorations is the esthetic outcome. Material properties, such as lack of translucency and higher opacity, make it difficult to get an optimal shade and color match. 16 , 17 Patient satisfaction with the esthetics and the outcome of the color and translucency should therefore be assessed when evaluating monolithic zirconia restorations.
Implant and implant‐supported restoration survival rates are well‐established. 1 However, the success rates of implant‐supported restorations are not always reported. If they are, the criteria are not applied uniformly. The modified United States Public Health Service (USPHS) criteria 18 could be an effective standardized evaluation method for the clinical performance, including the success of implant‐supported restorations.
The objective of this 1‐year prospective study was to evaluate clinical, radiographic and patient‐reported outcome measures, including the success of screw‐retained monolithic zirconia restorations with CAD/CAM titanium abutments in the posterior region. The hypothesis was that monolithic zirconia restorations with CAD/CAM titanium abutments have low technical and biological complication rates.
2. MATERIALS AND METHODS
2.1. Study design
This prospective case series included 50 single‐tooth implant‐supported restorations in healed sites in the posterior maxilla or mandible. Recruitment, inclusion, treatment and follow‐up took place in the Department of Oral and Maxillofacial Surgery and in the Department of Implant Dentistry at the University Medical Center Groningen (UMCG), the Netherlands from August 2017 to July 2021. The research protocol was approved by the Medical Ethics Review Board of the UMCG (METc 2017/295) and the study was registered in the Netherlands Trial Register (NL9059). Written informed consent was obtained from all the participants prior to enrollment. This manuscript follows the STROBE guidelines for cohort studies. 19
2.2. Participants
Consecutive patients who met the following criteria were included:
At least 18 years of age when being treated;
In need of a single tooth implant‐supported restoration in a healed site (missing tooth >3 months) in the first or second molar region in the maxilla and mandible;
The implant site had sufficient bone volume for placing an implant ≥8 mm long;
Suitable anatomical conditions (mesial‐distal, buccal‐lingual, and interocclusal space) to place an anatomic restoration;
The participant complies with good oral hygiene practices.
The exclusion criteria were
Medical and general contraindications for the surgical procedures;
Heavy smokers (> 10 cigarettes/day);
Severe bruxism with dysfunctional tendencies;
The presence of acute untreated periodontitis in the implant site or adjacent tissue;
Infections in the planned implant site or adjacent tissue;
History of local radiotherapy to the head and neck region.
2.3. Surgical procedures
One hour prior to surgery the patients took a prophylactic antibiotic (amoxicillin 2 g or clindamycin 600 mg in case of penicillin allergy). The surgical procedure was performed using local anesthesia (Ultracain D‐S forte, Sanofi‐Aventis Deutschland GmbH, Frankfurt am Main, Germany). A small muco‐periosteal flap was raised after a mid‐crestal incision. The implant site was prepared using a surgical template and a straight bone‐level implant with a tapered apex and conical connection (OsseoSpeed EV, Astra Tech Implant System, Dentsply Sirona Implants, Mölndal, Sweden) was inserted according to the manufacturer's instructions. The implant's diameter was 4.2 mm, and it was 8 or 11 mm in length depending on the available bone height at the implant site. The implant was placed at bone level, or subcrestal in thin gingival phenotype cases. A cover screw was placed, and the wound was closed with interrupted sutures. The postoperative care consisted of a 0.12% chlorhexidine oral rinse twice a day, starting 1 day before and ending 7 days after the surgery. One week after implant placement, a follow‐up visit was scheduled to remove the sutures and to review the healing process. Twelve weeks later, the implant was uncovered during the second‐stage surgery and a healing abutment (HealDesign EV, Dentsply Sirona Implants) was placed. Implant stability was checked manually. All the surgical procedures were performed by two experienced implant dentistry clinicians (GMR, CJ).
2.4. Restorative procedures
Two weeks after uncovering the implant, an impression was made at implant level with a polyether precision impression material (Impregum Penta Soft, 3 M, Saint‐Paul, MN, United States) using an individual open tray and impression coping (Implant Pick‐up EV, Dentsply Sirona Implants). A plaster model was poured with a laboratory analog (Implant Replica EV, Dentsply Sirona Implants) and digitized using an extraoral scanner (Ceramill Map 400, Amann Girrbach AG, Koblach, Austria). The digital file was sent to a centralized production facility (Atlantis, Dentsply Sirona Implants, Mölndal, Sweden) where a screw‐retained restoration, consisting of a monolithic zirconia (Zpex Smile, Tosoh Corporation, Tokyo, Japan) crown and a CAD/CAM gold‐shaded titanium abutment with an individualized emergence profile (Atlantis CustomBase Solution, Dentsply Sirona Implants, Mölndal, Sweden) was designed and manufactured. The supragingival part of the restoration was characterized (IPS e.max Ceram Essence, Ivoclar Vivadent AG, Schaan, Liechtenstein) and glazed (IPS e.max Ceram Glaze Paste, Ivoclar Vivadent AG) in a dental laboratory and adhesively cemented onto the abutment with a self‐curing luting composite (Multilink Implant, Ivoclar Vivadent AG). All the laboratory procedures were performed in one dental laboratory and in one centralized production facility. The restoration was tightened on the implant with an insertion torque of 25 Ncm. The screw access hole was sealed with polytetrafluoroethylene tape and composite resin (Figures 1 and 2). All the restorative procedures were performed by one prosthodontist (HJAM). After the restoration placement, oral hygiene instructions were given to the patient.
FIGURE 1.

Clinical view of a screw‐retained monolithic zirconia restoration of the lower left first molar after 1 year in function
FIGURE 2.
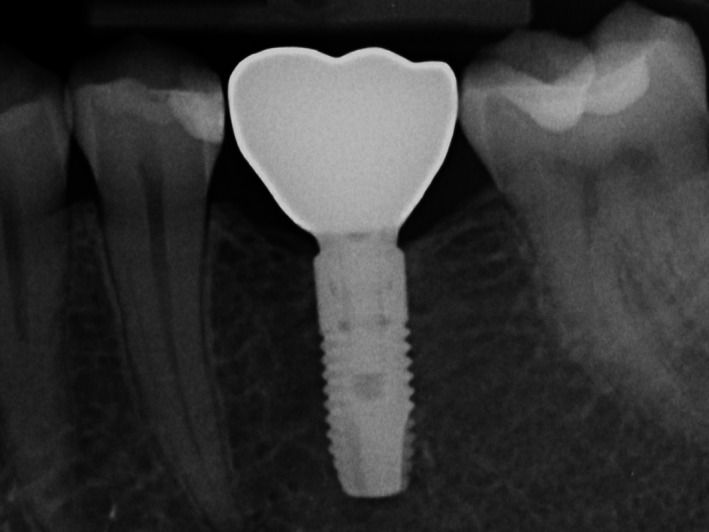
Intraoral radiograph of a straight bone‐level implant with a screw‐retained monolithic zirconia restoration and a CAD/CAM titanium abutment with an individualized emergence profile after 1 year in function
2.5. Outcome measures
Clinical, radiographic and patient‐reported outcome measures were collected prior to placing the implant (baseline, Tpre), and then 1 month (T1) and 1 year (T12) after placing the restoration. All the data were collected by one observer (VJJD).
The following outcome measures were collected:
Implant and restoration survival rate up to the 1 year follow‐up. Survival was defined as the percentage of implants and restorations that were in situ and functional at the time of follow‐up;
Soft tissue outcomes at the 1 month and 1 year follow‐ups assessed with the modified Plaque Index, 20 the presence of calculus, the modified Sulcus Bleeding Index, 20 the Gingival Index, 21 keratinized mucosa width (KMW) measured to the nearest 1 mm with a periodontal probe, 22 and pocket probing depth at four sites (mesial, distal, buccal, lingual/palatal) measured to the nearest mm;
Marginal bone level change (MBLC) from 1 month to 1 year after the procedure, assessed from calibrated intraoral radiographs with a long cone paralleling technique by a dedicated software (DicomWorks, Biomedical Engineering, UMCG, The Netherlands), and defined as change in the vertical distance in mm measured from the implant shoulder to the first bone to implant contact on the mesial and distal site of the implant. The MBLC's value was considered to be zero if the implant shoulder was below the crestal bone 23 ;
Patient‐reported outcome measures (PROMs) from baseline to the 1 year follow‐up, assessed with a questionnaire on overall satisfaction based on a 10‐point rating scale, and statements regarding feelings, function and esthetics based on a 5‐point Likert scale ranging from “disagree” to “agree” (see Telleman et al. 24 for the non‐validated questionnaire);
Restoration success rate up to the 1 year follow‐up, assessed with the modified USPHS criteria. 18 The modified USPHS criteria involve the following outcomes: restoration fracture, abutment fracture, loosening of the restoration (screw loosening or de‐cementation from the abutment), screw‐access hole restoration, occlusal wear, anatomical shape, restoration color and translucency, cementation gap and patient satisfaction. Success encompassed the percentage of restorations with no technical or biological complications.
2.6. Statistical methods
Each implant's highest MBLC and pocket probing depth values were used for the statistical analysis. Any loss to follow‐up was addressed by excluding the case from the analysis. The data were checked for normality with the Shapiro–Wilk test. Mean values, standard deviations (SD), range and frequency distributions were calculated using descriptive statistics. The mean difference in the PROMs from baseline to the 1 year follow‐up was analyzed with the Wilcoxon Signed‐rank Test. A cutoff point of ɑ = 0.05 was considered to indicate statistical significance. There were no significant differences between the maxilla and mandible. Therefore, the data were presented collectively. All the statistical analyses were performed with a statistical software (IBM SPSS Statistics, Version 23.0. Armonk, NY, United States).
3. RESULTS
All the consecutively recruited patients meeting the inclusion criteria agreed to participate in the study. None of the participants met the exclusion criteria. Fifty implants were placed in a total of 46 participants (Table 1). The 1‐year follow‐up was attended by 45 participants. One participant had moved without leaving an address after the restoration was placed and so was lost to follow‐up. Therefore, 49 implants and restorations were evaluated after 1 month and 1 year.
TABLE 1.
Participant baseline characteristics
| Number of participants (patients/implants) | 46/50 |
| Sex distribution (male/female) | 20/26 |
| Mean age in years (SD, minimum–maximum) | 53 (±11.9, 26–74) |
| Implant location (maxilla/mandible) | 15/35 |
| Implant position (in between teeth/distal free‐end) | 41/9 |
| Implant length (8 mm/11 mm) | 9/41 |
All were in situ and functional at the 1‐year evaluation resulting in a survival rate of 100% for both implants and restorations.
The soft tissue outcomes from the 1‐month (T1) and 1‐year (T12) evaluations are shown in Table 2. The plaque accumulation, presence of calculus, bleeding tendency and peri‐implant inflammation indices were low. The keratinized mucosa width was <2 mm around 26, and ≥ 2 mm around 23 restorations at the 1‐year evaluation. The mean pocket probing depth was 2.2 ± 0.5 mm at the 1‐year follow‐up evaluation.
TABLE 2.
Frequencies and percentages of the modified Plaque Index (possible scores 0–3), presence of calculus (possible scores 0–1), modified Sulcus Bleeding Index (possible scores 0–3), Gingival Index (possible scores 0–3), keratinized mucosa width and the mean (SD) pocket probing depth value in mm 1 month (T1) and 1 year (T12) after restoration placement
| T1 | T12 | |
|---|---|---|
| Modified Plaque Index | Score 0: 49 (100%) | Score 0: 49 (100%) |
| Calculus | Score 0: 49 (100%) | Score 0: 49 (100%) |
| Modified Sulcus Bleeding Index | Score 0: 46 (93.9%) | Score 0: 40 (81,6%) |
| Score 1: 3 (6.1%) | Score 1: 8 (16.3%) | |
| Score 2: 1 (2%) | ||
| Gingival Index | Score 0: 49 (100%) | Score 0: 49 (100%) |
| Keratinized mucosa width | <2 mm: 25 (51.0%) | <2 mm: 26 (53.1%) |
| ≥2 mm: 24 (49.0%) | ≥2 mm: 23 (46.9%) | |
| Pocket probing depth | 2.1 ± 0.9 | 2.2 ± 0.5 |
The mean MBLC between 1 month (T1) and 1 year (T12) after restoration placement was −0.17 ± 0.46 mm. The frequency distribution is shown in Table 3.
TABLE 3.
Mean (SD) value, frequency distribution and percentages of the marginal bone level changes in mm between 1 month (T1) and 1 year (T12) after final restoration placement
| Marginal bone level change | n = 49 |
|---|---|
| Mean (SD) | −0.17 ± 0.46 |
| > −2.5 to −2.0 | 1 (2.0%) |
| > −2.0 to −1.5 | 0 (0.0%) |
| > −1.5 to −1.0 | 0 (0.0%) |
| > −1.0 to −0.5 | 5 (12.2%) |
| > −0.5 to 0.0 | 43 (87.8%) |
Note: A negative value indicates bone loss.
The baseline patient‐reported outcomes (Tpre) and 1 year after restoration placement (T12) are shown in Table 4. The mean overall satisfaction score (scale 0–10) was 5.8 ± 1.3 at baseline (Tpre) and 9.2 ± 0.7 at the 1‐year evaluation (p < 0.001). The patient‐reported‐outcomes on feelings and function improved from baseline to the 1‐year follow‐up appointment (p < 0.001). All the patients were satisfied with the shape and color of the restoration.
TABLE 4.
Patient‐reported outcome measures and mean (SD) overall satisfaction (possible scores 0–10) at baseline (Tpre) and 1‐year after placing the final restoration (T12) and the significant differences between the times
| Tpre % in agreement (n = 49) | T12% in agreement (n = 49) | Significance | |
|---|---|---|---|
| Feelings | |||
| Ashamed of edentulous zone/implant | 22.4 | 0.0 | p < 0.001 |
| Self‐confidence has decreased | 12.2 | 0.0 | p = 0.007 |
| Edentulous zone/implant is visible to others | 18.4 | 0.0 | p < 0.001 |
| Function | |||
| Avoid eating with the edentulous zone/implant | 61.2 | 0.0 | p < 0.001 |
| Ability to chew is decreased | 61.2 | 0.0 | p < 0.001 |
| Implant does influence speech | – | 0.0 | |
| Implant does influence taste | – | 0.0 | |
| Esthetics | |||
| Not satisfied with the restoration's color | – | 0.0 | |
| Not satisfied with the restoration's shape | – | 0.0 | |
| Not satisfied with the color of the mucosa around the restoration | – | 0.0 | |
| Not satisfied with the shape of the mucosa around the restoration | – | 0.0 | |
| Overall satisfaction | 5.8 ± 1.3 | 9.2 ± 0.7 | p < 0.001 |
Restoration success, assessed with the modified USPHS criteria, is shown in Table 5. Two technical complications (loosening of the restoration, n = 2) were noted at the 1‐year evaluation, resulting in a restoration success rate of 95.9%.
TABLE 5.
Modified USPHS criteria for evaluating implant‐supported restorations at the 1‐year follow‐up
| Alfa (A) | Bravo (B) | Charlie (C) | Delta (D) | |
|---|---|---|---|---|
| Restoration fracture |
Restoration not fractured 49 (100%) |
Chipping, but polishing possible 0 (0%) |
Chipping down to the abutment 0 (0%) |
Restoration fractured, new restoration needed 0 (0%) |
| Abutment fracture |
Abutment not fractured 49 (100%) |
– | – |
Abutment fractured, new restoration needed 0 (0%) |
| Loosening of the restoration (screw loosening or de‐cementation from abutment) |
No loosening 47 (95.9%) |
– |
Repositioning possible 2 (4.1%) |
Repositioning not possible, new restoration needed 0 (0%) |
| Screw‐access hole restoration |
Restoration not lost 49 (100%) |
– |
Restoration lost (repairable) 0 (0%) |
– |
| Wear |
No wear facets on the restoration and opposing teeth 49 (100%) |
Small wear facets (diameter < 2 mm) on restoration and/or opposing teeth 0 (0%) |
Wear facets (diameter > 2 mm) on restoration and/or opposing teeth 0 (0%) |
– |
| Anatomical shape |
Ideal anatomical shape, tight proximal contacts and balanced occlusal contact 49 (100%) |
Slightly over‐ or undercontoured, weak proximal contacts, occlusal contact only on restoration 0 (0%) |
Highly over‐ or undercontoured, open proximal contacts, no occlusal contact on restoration 0 (0%) |
– |
| Restoration color and translucency |
No mismatch between restoration and adjacent teeth 0 (0%) |
Slight mismatch between restoration and adjacent teeth 49 (100%) |
Major mismatch between restoration and adjacent teeth 0 (0%) |
– |
| Cementation gap |
No cementation gap visible on radiograph 49 (100%) |
Minor gap visible 0 (0%) |
Major gap visible, new restoration not needed 0 (0%) |
Major gap visible, new restoration needed 0 (0%) |
| Patient satisfaction |
Very satisfied 49 (100%) |
Moderately satisfied 0 (0%) |
Not satisfied, new restoration not needed 0 (0%) |
Not satisfied, new restoration needed 0 (0%) |
|
Survival and success 0 (0%) |
Survival and success 47 (95.9%) |
Survival, no success 2 (4.1%) |
Failure 0 (0%) |
4. DISCUSSION
The screw‐retained monolithic zirconia restorations with CAD/CAM titanium abutments in the posterior maxilla and mandible performed very well after 1 year in function in the present case series, with high implant and restoration survival and success rates. Thus, the hypothesis that monolithic zirconia restorations with CAD/CAM titanium abutments have low technical and biological complication rates was accepted.
To date, no other studies have documented anything on screw‐retained monolithic zirconia restorations with CAD/CAM titanium abutments in the posterior region, thus precluding a direct comparison. However, some studies reported their 1‐year evaluations of screw‐retained monolithic zirconia restorations in the posterior area with other abutment types and they had similar implant and restoration survival rates as the present study. The survival of Pol et al.’s 7 implants and monolithic zirconia screw‐retained restorations with titanium angulated screw channel abutments was 100%. Mühlemann et al. 25 and Derksen et al. 26 reported their implant and restoration survival rates for screw‐retained monolithic zirconia restorations on stock Ti‐base abutments as 97.4% and 97.8%, respectively.
The supposed benefit of CAD/CAM abutments with a customized emergence profile that places the material junction further away from the peri‐implant bone level was affirmed by the low bleeding tendency and absence of peri‐implant inflammation at the 1‐year evaluation. As the restorations were screw‐retained, excess cement on the abutment was avoided. The good patient compliance to the oral hygiene instructions given after the restoration placement may have also contributed to the healthy peri‐implant soft tissues.
The MBLC at the 1‐year evaluation was limited (−0.17 mm) and similar to the previously mentioned Pol et al. 7 (−0.16 mm) and Mühlemann et al. 25 (−0.19 mm) studies. In the present study, the case with a high MBLC (−2.47 mm) showed no clinical signs of peri‐implantitis (bleeding, peri‐implant inflammation, exudate). The case involved a distal free‐end restoration on an 8 mm implant in the mandible with a crown‐to‐implant ratio of 2:1. Thus, the MBLC might not have been a biological complication but the result of mechanical overload. However, this factor is debated in the literature. 27 , 28 , 29
The PROMs in relation to feelings, function and esthetics were assessed using an established questionnaire at baseline prior to implant placement and at the 1‐year follow‐up after restoration placement. The outcome measures related to feelings and function improved significantly after the missing molar had been rehabilitated. This is similar to the Pol et al., 7 Guljé et al. 23 and Telleman et al. 24 studies which evaluated single tooth implant‐supported restorations in the posterior area with the same questionnaire. Thus, the present study's results affirm the patient acceptance of monolithic zirconia implant‐supported single molar restorations. Guljé et al. 23 and Telleman et al. 24 used bilayered zirconia and porcelain restorations whereas Pol et al. 7 used monolithic zirconia restorations like the present study. The material properties related to lack of translucency and higher opacity, and the limited possibilities to characterize monolithic zirconia, make it more difficult to get an optimal shade and color match compared to bilayered porcelain‐fused restorations. The observers' findings of a slight mismatch between the restoration and adjacent teeth in all the present study's cases did not affect the patient‐reported outcome measures in the esthetics domain. All the patients were satisfied with the color of the monolithic zirconia restoration. This is consistent with the Pol et al. 7 1‐year results. Possibly, the observer is more critical than the patient when it comes to the color of the restoration.
According to the modified USPHS criteria, the restoration success rate was 95.9%, which is similar to those reported by Pol et al. 7 (100%) and Mühlemann et al. 25 (97.4%) who also used the modified USPHS criteria to define restoration success. In the present study, no ceramic or abutment fracture was noted which is in line with the Pol et al., 7 Mühlemann et al., 25 and Derksen et al. 26 studies. Loosening of the restoration occurred in 4.1% of the cases which is similar to Derksen et al. who reported that loosening of the restoration occurred in 4.6% of the cases (screw loosening, n = 1; de‐cementation from the abutment, n = 1). A recent in vitro study showed that the stability of CAD/CAM titanium abutment screws tightened on implants with a conical connection is very high when inserted with a torque of 25 Ncm. 30 In the present study, both screw loosening cases had a relatively high anatomical restoration, making it hard to tighten the restoration to the implant as the screwdriver was only just long enough. The 25 Ncm insertion torque value might have not been reached in those cases which could have contributed to the loosening of the restorations.
The clinical results of the present study show that using screw‐retained monolithic zirconia restorations with CAD/CAM titanium abutments in the posterior maxilla and mandible leads to low technical and biological complications. However, long‐term evaluations are needed of the clinical, radiographic and patient‐reported outcomes of monolithic zirconia restorations with CAD/CAM titanium abutments. In addition, the small number of participants in the present study is a limitation. Another factor to be considered is the inherent lack of a control group in the present case series study.
5. CONCLUSION
The results of the present prospective case series study demonstrate very good clinical, radiographic and patient‐reported outcomes for screw‐retained monolithic zirconia restorations with CAD/CAM titanium abutments in the posterior maxilla and mandible after 1 year in function.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
AUTHOR CONTRIBUTIONS
Vincent J.J. Donker: Conceptualization, Data Curation, Formal Analysis, Investigation, Methodology, Project Administration, Writing—Original Draft. Gerry M. Raghoebar: Conceptualization, Investigation, Methodology, Supervision, Project Administration, Writing—Review and Editing. Charlotte Jensen‐Louwerse: Conceptualization, Investigation, Methodology, Project Administration, Writing—Review and Editing. Arjan Vissink: Conceptualization, Methodology, Supervision, Project Administration, Writing—Review and Editing. Henny J.A. Meijer: Conceptualization, Data Curation, Investigation, Methodology, Supervision, Project Administration, Writing—Review and Editing.
Donker VJJ, Raghoebar GM, Jensen‐Louwerse C, Vissink A, Meijer HJA. Monolithic zirconia single tooth implant‐supported restorations with CAD/CAM titanium abutments in the posterior region: A 1‐year prospective case series study. Clin Implant Dent Relat Res. 2022;24(1):125‐132. doi: 10.1111/cid.13069
Funding InformationImplant materials for the clinical study were provided by Dentsply Sirona Implants, Mölndal, Sweden (study code: I‐AA‐17‐001).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
REFERENCES
- 1. Jung RE, Zembic A, Pjetursson BE, Zwahlen M, Thoma DS. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow‐up of 5 years. Clin Oral Implants Res. 2012;23(Suppl. 6):2‐21. doi: 10.1111/j.1600-0501.2012.02547.x [DOI] [PubMed] [Google Scholar]
- 2. Pjetursson BE, Valente NA, Strasding M, Zwahlen M, Liu S, Sailer I. A systematic review of the survival and complication rates of zirconia‐ceramic and metal‐ceramic single crowns. Clin Oral Implants Res. 2018;29:199‐214. doi: 10.1111/clr.13306 [DOI] [PubMed] [Google Scholar]
- 3. Alqutaibi AY, Alnazzawi AA, Algabri R, Aboalrejal AN, AbdElaziz MH. Clinical performance of single implant‐supported ceramic and metal‐ceramic crowns: A systematic review and meta‐analysis of randomized clinical trials. The Journal of Prosthetic Dentistry, 2021;126(3):369‐376. doi: 10.1016/j.prosdent.2020.06.011 [DOI] [PubMed] [Google Scholar]
- 4. de Kok P, Kleverlaan CJ, De Jager N, Kuijs R, Feilzer AJ. Mechanical performance of implant‐supported posterior crowns. J Prosthet Dent. 2015;114(1):59‐66. doi: 10.1016/j.prosdent.2014.10.015 [DOI] [PubMed] [Google Scholar]
- 5. Sadowsky SJ. Has zirconia made a material difference in implant prosthodontics? A review. Dent Mater. 2020;36(1):1‐8. doi: 10.1016/j.dental.2019.08.100 [DOI] [PubMed] [Google Scholar]
- 6. Spitznagel FA, Horvath SD, Gierthmuehlen PC. Prosthetic protocols in implant‐based oral rehabilitations: a systematic review on the clinical outcome of monolithic all‐ceramic single‐ and multi‐unit prostheses. Eur J Oral Implantol. 2017;10:89‐99. [PubMed] [Google Scholar]
- 7. Pol CWP, Raghoebar GM, Maragkou Z, Cune MS, Meijer HJA. Full‐zirconia single‐tooth molar implant‐supported restorations with angulated screw channel abutments: a 1‐year prospective case series study. Clin Implant Dent Relat Res. 2020;22(1):138‐144. doi: 10.1111/cid.12872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Honda J, Komine F, Kamio S, Taguchi K, Blatz MB, Matsumura H. Fracture resistance of implant‐supported screw‐retained zirconia‐based molar restorations. Clin Oral Implants Res. 2017;28(9):1119‐1126. doi: 10.1111/clr.12926 [DOI] [PubMed] [Google Scholar]
- 9. Sailer I, Philipp A, Zembic A, Pjetursson BE, Hämmerle CHF, Zwahlen M. A systematic review of the performance of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin Oral Implants Res. 2009;20(Suppl. 4):4‐31. doi: 10.1111/j.1600-0501.2009.01787.x [DOI] [PubMed] [Google Scholar]
- 10. Vechiato‐Filho A, Pesqueira A, De Souza G, dos Santos D, Pellizzer E, Goiato M. Are zirconia implant abutments safe and predictable in posterior regions? A systematic review and meta‐analysis. Int J Prosthodont. 2016;29(3):233‐244. doi: 10.11607/ijp.4349 [DOI] [PubMed] [Google Scholar]
- 11. Vinhas AS, Aroso C, Salazar F, López‐Jarana P, Ríos‐Santos JV, Herrero‐Climent M. Review of the mechanical behavior of different implant‐abutment connections. Int J Environ Res Public Health. 2020;17(22):1‐20. doi: 10.3390/ijerph17228685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pesce P, Canullo L, Grusovin MG, De Bruyn H, Cosyn J, Pera P. Systematic review of some prosthetic risk factors for periimplantitis. J Prosthet Dent. 2015;114(3):346‐350. doi: 10.1016/j.prosdent.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 13. Staubli N, Walter C, Schmidt JC, Weiger R, Zitzmann NU. Excess cement and the risk of peri‐implant disease – a systematic review. Clin Oral Implants Res. 2017;28(10):1278‐1290. doi: 10.1111/clr.12954 [DOI] [PubMed] [Google Scholar]
- 14. Long L, Alqarni H, Masri R. Influence of implant abutment fabrication method on clinical outcomes: a systematic review. Eur J Oral Implantol. 2017;10:67‐77. [PubMed] [Google Scholar]
- 15. Raee A, Alikhasi M, Nowzari H, Djalalinia S, Khoshkam V, Moslemi N. Comparison of peri‐implant clinical outcomes of digitally customized and prefabricated abutments: a systematic review and meta‐analysis. Clin Implant Dent Relat Res. 2021;23(2):216‐227. doi: 10.1111/cid.12982 [DOI] [PubMed] [Google Scholar]
- 16. Tabatabaian F. Color aspect of monolithic zirconia restorations: a review of the literature. J Prosthodont. 2019;28(3):276‐287. doi: 10.1111/jopr.12906 [DOI] [PubMed] [Google Scholar]
- 17. De Angelis P, Gasparini G, Rella E, De Angelis S, Grippaudo C, D'Addona A, Manicone PF. Patient Satisfaction with Implant‐Supported Monolithic and Partially Veneered Zirconia Restorations. BioMed Res. Int. 2021;2021:1‐8. doi: 10.1155/2021/6692939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bayne SC, Schmalz G. Reprinting the classic article on USPHS evaluation methods for measuring the clinical research performance of restorative materials. Clin Oral Investig. 2005;9(4):209‐214. doi: 10.1007/s00784-005-0017-0 [DOI] [PubMed] [Google Scholar]
- 19. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806‐808. doi: 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mombelli A, van Oosten MAC, Schürch E, Lang NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2(4):145‐151. doi: 10.1111/j.1399-302X.1987.tb00298.x [DOI] [PubMed] [Google Scholar]
- 21. Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(6):610‐616. doi: 10.1902/jop.1967.38.6.610 [DOI] [PubMed] [Google Scholar]
- 22. Avila‐Ortiz G, Gonzalez‐Martin O, Couso‐Queiruga E, Wang HL. The peri‐implant phenotype. J Periodontol. 2020;91(3):283‐288. doi: 10.1002/JPER.19-0566 [DOI] [PubMed] [Google Scholar]
- 23. Guljé FL, Raghoebar GM, Vissink A, Meijer HJ. Single restorations in the resorbed posterior mandible supported by 6‐mm implants: a 1‐year prospective case series study. Clin Implant Dent Relat Res. 2015;17:e465‐e471. doi: 10.1111/cid.12272 [DOI] [PubMed] [Google Scholar]
- 24. Telleman G, Meijer HJA, Vissink A, Raghoebar GM. Short implants with a nanometer‐sized CaP surface provided with either a platform‐switched or platform‐matched abutment connection in the posterior region: a randomized clinical trial. Clin Oral Implants Res. 2013;24(12):1316‐1324. doi: 10.1111/clr.12000 [DOI] [PubMed] [Google Scholar]
- 25. Mühlemann S, Lakha T, Jung RE, Hämmerle CHF, Benic GI. Prosthetic outcomes and clinical performance of CAD‐CAM monolithic zirconia versus porcelain‐fused‐to‐metal implant crowns in the molar region: 1‐year results of a RCT. Clin Oral Implants Res. 2020;31(9):856‐864. doi: 10.1111/clr.13631 [DOI] [PubMed] [Google Scholar]
- 26. Derksen W, Tahmaseb A, Wismeijer D. Randomized clinical trial comparing clinical adjustment times of CAD/CAM screw‐retained posterior crowns on ti‐base abutments created with digital or conventional impressions. One‐year follow‐up. Clin Oral Implants Res. 2020;2021:1‐9. doi: 10.1111/clr.13790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bertolini MM, Del Bel Cury AA, Pizzoloto L, Acapa IRH, Shibli JA, Bordin D. Does traumatic occlusal forces lead to peri‐implant bone loss? A systematic review. Braz Oral Res. 2019;33:1‐11. doi: 10.1590/1807-3107BOR-2019.VOL33.0069 [DOI] [PubMed] [Google Scholar]
- 28. Klinge B, Meyle J, Claffey N, et al. Peri‐implant tissue destruction. The third EAO consensus conference 2012. Clin Oral Implants Res. 2012;23(SUPPL.6):108‐110. doi: 10.1111/j.1600-0501.2012.02555.x [DOI] [PubMed] [Google Scholar]
- 29. Meijer HJA, Boven C, Delli K, Raghoebar GM. Is there an effect of crown‐to‐implant ratio on implant treatment outcomes? A systematic review. Clin Oral Implants Res. 2018;29:243‐252. doi: 10.1111/clr.13338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yilmaz B, Çakmak G, Batak B, Johnston WM. Screw stability of CAD‐CAM titanium and zirconia abutments on different implants: an in vitro study. Clin Implant Dent Relat Res. 2021;23(3):373‐379. doi: 10.1111/cid.13001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.


