Abstract
Aims
To identify key research questions where answers could improve care for older people living with diabetes (PLWD), and provide detailed recommendations for researchers and research funders on how best to address them.
Methods
A series of online research workshops were conducted, bringing together a range of PLWD and an acknowledged group of academic and clinical experts in their diabetes care to identify areas for future research. Throughout the pre‐workshop phase, during each workshop, and in manuscript preparation and editing, PLWD played an active and dynamic role in discussions as part of both an iterative and narrative process.
Results
The following key questions in this field were identified, and research recommendations for each were developed:
How can we improve our understanding of the characteristics of older people living with diabetes (PLWD) and their outcomes, and can this deliver better person‐centred care?
How are services to care for older PLWD currently delivered, both for their diabetes and other conditions? How can we optimise and streamline the process and ensure everyone gets the best care, tailored to their individual needs?
What tools might be used to evaluate the level of understanding of diabetes in the older population amongst non‐specialist Healthcare Professionals (HCPs)?
How can virtual experts or centres most effectively provide access to specialist multi‐disciplinary team (MDT) expertise for older PLWD and the HCPs caring for them?
Is a combination of exercise and a nutrition‐dense, high protein diet effective in the prevention of the adverse effects of type 2 diabetes and deterioration in frailty, and how might this be delivered in a way which is acceptable to people with type 2 diabetes?
How might we best use continuous glucose monitoring (CGM) in older people and, for those who require support, how should the data be shared?
How can older PLWD be better empowered to manage their diabetes in their own home, particularly when living with additional long‐term conditions?
What are the benefits of models of peer support for older PLWD, both when living independently and when in care?
Conclusions
This paper outlines recommendations supported by PLWD through which new research could improve their diabetes care and calls on the research community and funders to address them in future research programmes and strategies.
Keywords: diabetes; ageing, PLWD, research
What's new.
Research prioritisation exercises identified care for older people with diabetes as an area of need of further research.
Diabetes UK convened a series of online workshops that brought together a range of people living with diabetes as well as a wide group range of experts in the clinical, and academic care of older people with diabetes to clearly understand what research is needed.
Eight priority questions with clear recommendations for the research needed to answer each was developed.
1. INTRODUCTION
Over four and a half million people in the UK have diabetes, 1 and over a third are over the age of 65. 2 This group is more likely to face additional challenges in diabetes self‐management and have additional care needs, due to the likelihood that people in this group will be living with multiple long‐term conditions. 3 , 4 The importance of this demographic is likely to grow: The number of people living with diabetes (PLWD) in the UK is predicted to rise by 0.8 million by 2025 and this will include many older adults 1 ; however, older people's care is often not a focus for investment or research and the impact of ageism on health outcomes has become clear. 5
The diabetes research steering groups (DRSGs) bring together researchers, HCPs and PLWD or at risk of diabetes to collaboratively identify areas where advances in research could improve the lives of those with or at risk of diabetes and establish these as priorities for future research. The groups are facilitated and supported by Diabetes UK. From their foundation in 2017, the need to improve how care for older PLWD is delivered has been one of their top priorities, particularly in relation to long‐term residential care, how new technology can provide innovative support care and how diabetes is managed alongside other long‐term conditions.
Additional insight gathered from PLWD identified several other broad areas of concern. Two of the priority questions from the Type 2 diabetes James Lind Alliance Priority Setting Partnership top 10 6 also refer to issues central to ageing well: priority 3 called for self‐management support tailored to the needs of different groups of people living with type 2 diabetes and priority 6 asked why type 2 diabetes gets progressively worse over time and how to prevent this. Insight gathering carried out by the DRSGs also identified significant anxiety amongst PLWD relating to the fear of loss of control of diabetes self‐management to non‐specialist carers in residential care and concerns over whether they would be deprioritised for new technology or treatments for diabetes due to their age.
The vulnerability of older PLWD and people living with frailty to the recent COVID‐19 pandemic 7 showed the impact of shortfalls in their care and emphasised the existing need for improvement in how diabetes is managed in long‐term care facilities. 8 The limited evidence base on the best way to care for older PLWD has long been cited as a limitation to the way care is delivered, 9 with a particular need for a greater understanding of cognitive decline and how it should affect diabetes care. 10 The lack of evidence is also driven by the fact that clinical trials often exclude older people with diabetes when there is no need to. 11
With clear unmet needs and concerns relating to the care of older people with diabetes recognised, Diabetes UK convened an expert advisory group (EAG) which was well represented by PLWD to determine the scope and format for the workshop reported in this manuscript. It aimed to identify key gaps in knowledge and major shortfalls in diabetes care and how research could best address them. Additional aims were how to foster research collaborations and ensure that older people with diabetes are actively involved in all stages of future research.
2. METHODOLOGY
An EAG was convened to consider the scope of the workshop and recommended that the workshop focus on the contexts in which older people with diabetes receive care or support: both when living independently and when living in care. They also outlined six key issues to consider:
The impact of frailty
The use of technology
The impact of health inequalities
The need for better education and training on diabetes for HCPs who care for older people
Questions around differences in therapies and glycaemic targets, according to morbidity profile
The importance of quality of life (QoL)
For clarity, whilst there were discussions on what age range should define ‘older people with diabetes’, thresholds were not defined in most cases. This was to avoid artificially narrowing the scope, but it was stressed that all individual projects would need to set and justify age ranges. Similarly, for the purpose of this paper living independently is defined as any situation in which older PLWD are able to choose to continue living in their own home, without needing around the clock assistance with the activities of daily living. Living in care is defined as any situation in which older PLWD are provided with more support for these activities and potentially the management of their diabetes, covering a range of circumstances including residential and nursing homes and temporary situations such as acute care in hospital.
On the basis of this scope, Diabetes UK brought together a wide range of experts in the care of older people with diabetes for a digital workshop series, ensuring a mix of clinical, academic and lived expertise in both contexts when inviting participants so that all highlighted key issues could be explored. The series was designed to identify key gaps in the evidence and co‐design a set of priority research questions that should be addressed to improve the care of older people with diabetes. In total, there were 59 attendees, including 12 PLWD of whom six were living with type 1 diabetes and six were living with type 2 diabetes, 38 researchers and HCPs, six members of staff from Diabetes UK and three facilitators from The Collective Facilitation Ltd., the professional facilitation company who facilitated the workshop and supported the planning. Attendees are listed in Appendix I. A broad platform of recruiting PLWD was undertaken based on known active contributors to the work of Diabetes UK in the DRSGs (PLWD were represented in all seven groups), a 50/50 representation on a DUK Lay/HCP Research Forum and an EAG, and suggestions from invited clinicians and academics with an equal emphasis on those with type 1 or type 2 diabetes. It is important to emphasise that PLWD were involved actively at all stages of developing the themes for the workshops with contributions ranging from the early discussions involving the DRSGs, the outputs of the EAG, the development of some pre‐recorded videos (Vox Pops) outlining their lived experiences, as well as the reported online workshop discussions and its recommendations. Additional research ideas and priorities from PLWD arose from outputs of the Diabetes and Healthy Ageing Group where PLWD were well represented. Two members of the PLWD group also had important additional roles in the conceptual design, writing and editing of this manuscript and are represented as named authors. The digital format primarily consisted of online workshops, with an online discussion platform for sharing ideas and outputs from each session provided and facilitated by the organisers (Figure 1).
FIGURE 1.
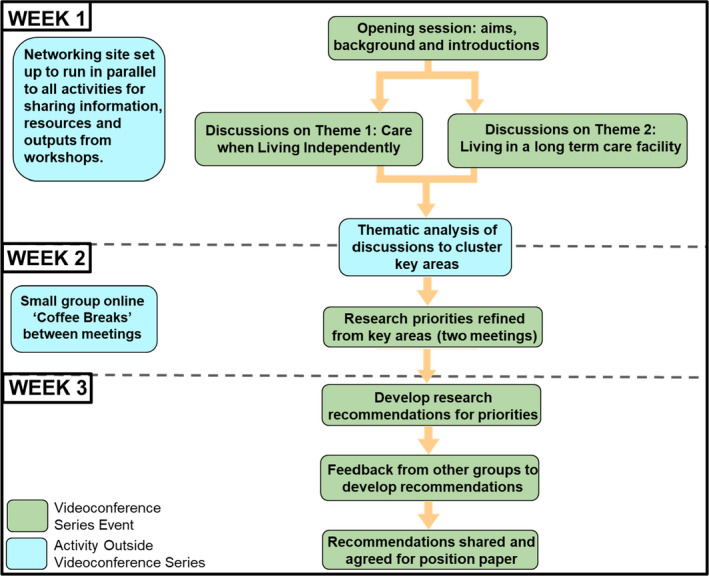
Workshop Structure (Credit to The Collective Facilitation Ltd).
The workshop began with three sessions designed to give attendees the chance to discuss and identify where change is needed. This was delivered through breakout groups which included representation from a variety of clinical and academic specialities and people with diabetes. Groups were asked to answer two questions: ‘What are some of the wicked problems we should be thinking about solving?’ and ‘What do you see as the opportunities for research to make a difference?’. These discussions were prompted by pre‐filmed presentations from clinical academics talking about the challenges and uncertainties from their perspective, and PLWD sharing their experiences of care and what needs to change. This also enabled the representation of views from older people with diabetes whose situation would have made it more challenging to share their expertise in the workshop itself, such as those living in residential care.
This was followed by a thematic analysis of the discussion by the Diabetes UK team to identify the key themes raised. These were phrased as key questions on how care for older people with diabetes is currently delivered and how it could be improved:
How might we build effective long‐term diabetes care plans, which can account for how age or other long‐term conditions may change what is needed?
How might we reconcile the different recommendations for diet and activity for type 2 diabetes and frailty?
How might we ensure diabetes care is not inappropriately deprioritised in older age, particularly when it might need to be managed alongside multiple conditions?
How might we bring the expertise of MDTs from hospitals into care homes?
How might we reduce the psychological impact of shifting away from self‐management, to help people adjust to the change?
How might we make effective use of technology in the ageing population?
How might models of peer support help people manage their diabetes as they age?
How might we ensure HCPs are equipped to manage diabetes in an ageing population?
These were expanded on by asking what questions research would need to answer to achieve this change, to support the development of recommendations for future research. Over the course of the final two events, eight sets of recommendations were developed by working groups, along with additional details on what would be required to effectively address them. This included opportunities for all groups to input into each recommendation. These were developed by asking five questions:
What is the research idea/question?
What difference will it make?
Who needs to be involved? Including the academic and clinical skills and inputs needed, funders and commissioners who might be involved and how to engage people with diabetes to ensure a representative cohort in the research which is carried out.
Beyond funding, what would be needed to ensure this research happens and is successful?
What are the first steps to take?
All discussions were captured to inform this paper, for the attention of both researchers and research funders, and the results (Figure 2) are presented below.
FIGURE 2.
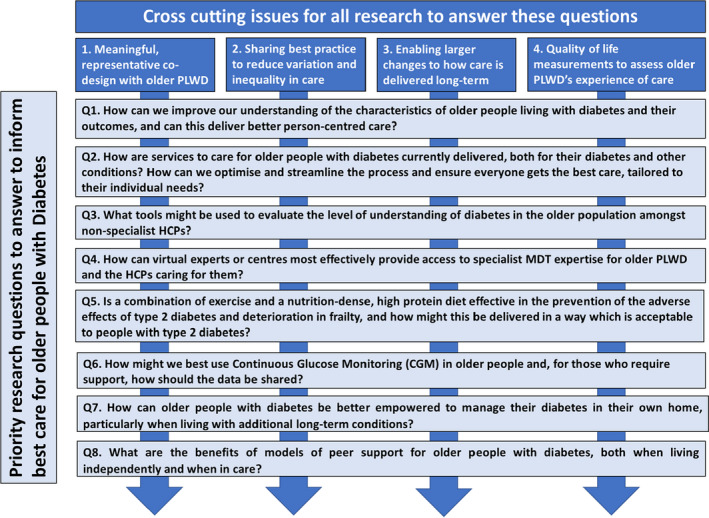
Priority research questions to inform the best care for older people with diabetes developed at this workshop, and cross‐cutting areas of importance.
3. RESULTS
3.1. Research Question 1: How can we improve our understanding of the characteristics of older PLWD and their outcomes, and can this deliver better person‐centred care?
3.1.1. Background and potential impact
Whilst the focus of the workshop was older people with diabetes, it was acknowledged that this describes a very heterogeneous and diverse population. 12 In addition to types of diabetes, this includes a wide range of diabetes treatments, 13 priorities in care, 14 other long‐term conditions being managed alongside diabetes 3 , 4 and what health and QoL benefits they could receive from different interventions. The increasing importance, 15 information on challenges 16 and the number of trials 17 of health and social care working together more, and how they applied in this context, 18 was also emphasised.
A move towards person‐centred care, in which HCPs focus on the needs of an individual patient and work with them so their preferences, needs and values guide clinical decisions, would take these dynamics into account, in a way they are not at the moment. For example, current approaches often do not take sufficient account of how predictive frailty in diabetes is of other adverse outcomes. 19 This was thought to have the potential to make a significant difference to the quality of care, QoL and clinical outcomes of older PLWD. This would also ensure that diabetes care is not inappropriately deprioritised when treatments for multiple long‐term conditions are needed, 20 which was a concern for many. However, a significant cultural change like this will both take time and require substantial evidence of the effectiveness and cost‐effectiveness of the new approach to justify the investment and training required.
3.1.2. Research recommendation
Research to better characterise the population of older PLWD is needed. This could be achieved using existing or new datasets, to examine how different characteristics affect outcomes to ensure care can be effectively targeted and delivered in the long term.
3.1.3. What will be needed?
To characterise this population effectively requires the collection of a wide range of data in a number of contexts. Measurements should include all factors which could impact the care needs and outcomes of older PLWD, including clinical metrics and outcomes, functional assessment and frailty detection, QoL assessments, detailed demographic information and social care metrics, and be collected from older PLWD either independently or in long‐term care.
Regional and national databases for this data could be built in several ways: by linking and expanding existing databases of health and social care, collecting novel data from routine care or supporting its collection in the community through patient input using apps such as the Freestyle View. Feasibility studies or systematic reviews of different methods may be needed to assess which would be most suitable.
Once data have been collected, the characteristics of PWLD which impact outcomes should be mapped to help identify needs and risks, and how this could inform future approaches.
In the long term, this could shape guidance, training or tools to support HCPs in taking a holistic view of a patient's needs, to implement the right strategies to improve outcomes from their care.
Experts in qualitative research into culture change could play a key role in ensuring this can be implemented at scale, and the potential to run a getting it right first time initiative 21 on primary and/or residential care for diabetes once it is better understood was also highlighted.
3.2. Research Question 2: How are services to care for older people with diabetes currently delivered, both for their diabetes and other conditions? How can we optimise and streamline the process and ensure everyone gets the best care, tailored to their individual needs?
3.2.1. Background and potential impact
Care for older people with diabetes, and knowledge held amongst HCPs, is fragmented 9 and currently delivered through several providers. Numerous problems with the way these services connect and communicate with each other have been identified, and this can affect the care that individuals receive when they are living with several conditions. 22 There are established difficulties with various electronic systems not sharing information, but some examples of good practice do exist in diabetes 23 and elsewhere, 24 and could be a foundation towards development and progression.
More integration could help to provide better, joined up and individualised care, and we know this can result in improved patient satisfaction and better access to services. 25 , 26
3.2.2. Research recommendation
Mapping of existing services available to older people with diabetes is needed, to understand their needs and establish how services need to change to meet them.
3.2.3. What will be needed?
A consensus on current shortfalls in care provision for older people with diabetes should be generated through surveys, analysing existing guidelines and qualitative research, to support and inform the development of agreed quality standards relating to joined‐up care. This also needs to account for the diversity of this population and what is provided, as per recommendation 1.
Research is needed to establish models of integrated care for older people covering both diabetes and any co‐morbidities they are living with, involving all stakeholders and specialities. These should be co‐created with older people with diabetes and tested to establish whether they reduce fragmentation, increase patient satisfaction, have a positive impact on outcomes and improve access to services.
The resources needed to accommodate these new models of optimal integrated care for older people should be assessed, along with their cost‐effectiveness. Telemedicine was also proposed, to reduce resourcing barriers to optimal integrated care. 27
In the future, effective auditing of these contexts to the new standards and criteria to strengthen adherence to them will be critical.
3.3. Research Question 3: What tools might be used to evaluate the level of understanding of diabetes in the older population amongst non‐specialist HCPs?
3.3.1. Background and potential impact
The low level of understanding of all forms of diabetes amongst non‐diabetes specific HCPs of any kind involved in care is a major concern for PLWD 28 and an established clinical issue, 29 which can be exacerbated by the low level of understanding in the general population and the availability of incorrect information. 30 In older people who may require more care for multiple long‐term conditions and/or be cared for more regularly by non‐specialists including care home staff or HCPs from other disciplines, this can be even more significant. This has been reported in poor experiences of care and outcomes for older people with diabetes, such as medication errors which can result in hospitalisation and deterioration of health and QoL, 8 , 31 , 32 which can lead to anxiety when they need more support.
A competency framework targeted to these gaps could help to raise the understanding of diabetes in older people amongst non‐specialist HCPs to a level that will prevent harm. In addition to improved outcomes, this will ensure HCPs are confident they are providing best practices and give PLWD more confidence in those caring for them. This includes knowledge relating to the interaction of diabetes treatments with those of other long‐term conditions. 3 , 4
3.3.2. Research recommendation
There is a clear need for research, first to establish exactly where the critical gaps in knowledge and training needs are, and second to address them, potentially using models from HCP education in other conditions. Resolving this issue will likely require investment in the training and education of HCPs.
3.3.3. What will be needed?
Using existing competency frameworks for diabetes specialist HCPs as a basis, 33 carry out qualitative research with both older PLWD and specialist HCPs who care for them to establish a version focussed on non‐specialists. This should also include careful consideration of what is and is not a specialist diabetes role and how social care is covered.
Develop and pilot surveys to compare the current expertise of HCPs with the requirements of this draft framework.
Undertake a health economic assessment of the investment required to implement this framework, and ensure it gets met to make the case for change.
Carry out these surveys at scale in multiple settings to establish exactly where critical gaps in knowledge exist. Refine the competency framework based on the results and work with policymakers to establish it and ensure training to meet it can be delivered.
Training, once developed, will need to be maintained, both in terms of those who receive it and in terms of the need to adapt to changes in care such as new treatments.
3.4. Research Question 4: How can virtual experts or centres most effectively provide access to specialist MDT expertise for older PLWD and the HCPs caring for them?
3.4.1. Background and potential impact
As well as ensuring non‐specialist HCPs have a good level of diabetes knowledge, specialist MDT expertise which could not feasibly be provided outside of specialist care by additional training will also be required. 29 It can be challenging for older PLWD to travel to access this expertise in secondary care, particularly when they are no longer living independently, but ways to provide consultations and expertise to them remotely are becoming more prevalent, effective, and accessible. 34
Making this expertise more widely available and sharing it would be hugely beneficial to how care is delivered for older people with diabetes, primarily by reducing risks of harm 31 and giving older PLWD more confidence in their care. Better communication channels between acute and community care centres would also be developed, which could help to create a more integrated and personalised care system with effective transitions of care outlined in previous recommendations.
3.4.2. Research recommendation
Health services research is needed to establish the best way for this remote expertise to be delivered. This could be through providing remote access to PLWD’s current HCPs, 35 networks of other specialist HCPs who can be consulted remotely when needed, or centres of expertise with teams specialised in consulting remotely on the care needs of older PLWD.
3.4.3. What will be needed?
Existing models for providing remote specialist clinical expertise to people living either in residential care settings or independently, but who face significant barriers to attending clinics, should be reviewed to establish best practices. These could be examples from diabetes care, geriatric care or other conditions.
This information should then be used as a basis to co‐design a proposed virtual MDT approach with PLWD.
Qualitative research should be carried out with all relevant groups of HCPs (any specialists who would be involved remotely, district nurses and staff for long term care facilities), to iterate on the approach and determine how it could be delivered. Where possible, people with significant real‐world expertise in similar models of remote care should be involved to support this process.
Any new model of virtual MDT care should be piloted, against the current standard of care. Any subsequent trial would need to assess cost‐effectiveness, clinical effectiveness and person‐centred measurements including acceptability, QoL and potentially the effect on independence.
3.4.4. Alternative approach
In addition to outlining the research needed to ensure specialist diabetes care is accessible when required, attendees recommended that research should explore the feasibility of a residential care setting in which all residents are PLWD, the staff all have specialist knowledge in diabetes care and the environment is designed to support this. This could draw on experiences in other conditions, such as work on how home environments with integrated technology could support the specific needs of people with Parkinson's disease within the SPHERE project 36 or specialised dementia units within long‐term residential care settings. 37 It is vital that any such feasibility studies are co‐designed with older PLWD and that they ensure needs beyond diabetes care are also met.
3.5. Research Question 5: Is a combination of exercise and a nutrition‐dense, high protein diet effective in the prevention of the adverse effects of type 2 diabetes and deterioration in frailty, and how might this be delivered in a way that is acceptable to people with type 2 diabetes?
3.5.1. Background and potential impact
Research into the prevention and palliation of frailty in older people focuses on the importance of a nutrient‐rich diet 38 to prevent muscle loss, as well as increased moderate physical activity. 39 There are few intervention studies on people living with frailty and fewer still assessing how this interacts with diabetes, despite calls for these. 40
Current dietary advice also conflicts with NICE guidelines for the prevention and treatment of type 2 diabetes, 41 and people living with type 2 diabetes have been found to be at an increased risk of frailty. 42 Equally, developing frailty is associated with poor health outcomes when living with diabetes 43 as well as loss of independence. 44
3.5.2. Research recommendation
Research is needed to determine a balanced combination of diet and exercise which is suitable for preventing frailty and managing diabetes, and crucially which is acceptable to older people living with type 2 diabetes from any background.
3.5.3. What will be needed?
Current approaches to nutrition for people with type 2 diabetes and frailty should be reviewed in a range of settings, from independent living to care homes. Both their effectiveness in clinical terms and their acceptability to people with diabetes need to be assessed in each context, as well as how this can vary by age, level of frailty, personal preference and access to food or information about food.
Any assessment of acceptability with people with diabetes needs to ensure sufficiently broad representation to assess all cultural dietary needs.
As well as being co‐designed with older people with diabetes, work in this area should also heavily involve those who create and manage the environments in which older PLWD and frailty often live: town planners, care home and retirement village providers. This will ensure that the project is designed around the facilities available and with the decision‐makers, as well as how people with diabetes will engage with them. This would also raise awareness of what people with diabetes and frailty need in these contexts beyond these projects.
Once an approach to exercise and nutrition has been developed, clinical trials in different settings will be needed to assess how effective it is alongside implementation research to ensure it is feasible to deliver at scale.
3.6. Research Question 6: How might we best use CGM in older people and, for those who require support, how should the data be shared?
3.6.1. Background and potential impact
Serious concerns were raised around the difficulty experienced by older people with type 1 diabetes when attempting to access technology. There were reports of resistance from HCPs, as well as the concern that technology is not always appropriate for the older person, either because they are experiencing barriers that affect their ability to use it 45 or because it may not have been tested as extensively in the older population, despite positive results when it is. 46 This is despite the fact that they are likely to be eligible for some technology such as Flash glucose monitoring under current criteria, 47 and additional data suggesting it could be an effective tool to support carers for older PLWD with memory problems. 48 Similar results have been seen in older people with type 2 diabetes, who face additional barriers to accessing this kind of technology despite evidence of its effectiveness. 46
We also know that some symptoms of hypoglycaemia may be misinterpreted as neurological symptoms in older people more frequently than in younger people. 49 The impact of severe hypoglycaemia has also been shown to be more significant for older PLWD. 50 In addition to the increased risk of and from falls which people living with both diabetes and frailty have from this,S51 a bidirectional relationship has been found with both cardiovascular eventsS52 and cognitive declineS53. Evidence also suggests that the use of CGM could reduce the risk of severe hypoglycaemia to mitigate these risks. 46
These gaps in understanding and concerns suggest that there may be a missed opportunity for older people with diabetes to be better supported by technology to allow them to continue to live independently.
3.6.2. Research recommendation
Research is needed to establish how CGM is best used in older PLWD and the impact on outcomes and QoL.
3.6.3. What will be needed?
Research is needed to identify older PLWD who would most benefit from CGM in both glycaemic control and QoL outcomes: their characteristics and how care settings can affect this, to support the development of future criteria for access.
Training should be developed to support HCPs who are managing older people who need assistance to benefit from CGM.
Attention should also be paid in this work to working out the best way for CGM data to be shared and with who, to support older PLWD who have access to these devices but need support using them to self‐manage without causing data security or privacy concerns.
Qualitative research should be undertaken to understand HCP attitudes to the provision of technology for older people and any barriers.
New CGM technology should also be developed in a way that ensures that it can be used to support older people with diabetes and considers the barriers for them, with the voice of the patient being integral to this process. This is particularly important as past trials on effectiveness have often not collected enough data from participants older than 65S54, which has meant that dedicated follow‐up trials were required. 46
3.7. Research Question 7: How can older people with diabetes be better empowered to manage their diabetes in their own home, particularly when living with additional long‐term conditions?
3.7.1. Background and potential impact
The importance of being able to live independently was critical to workshop attendees living with diabetes and this was also reflected in previous insight. There are many factors key to enabling this, with three highlighted as particularly critical and recommendations for how research could optimise the role each plays developed:
Technology
The role of technology in diabetes care is establishedS55 and likely to grow in importance, and extends beyond the blood glucose monitoring and remote care devices from previous recommendations to other forms of wearable technologyS56 and data analysis.S57 These could be important tools for older people living independently, however current devices are extremely limited in how they can adapt to the accessibility barriers which affect whether PLWD can use them in older age, such as a reduction in manual dexterityS58 or visual impairment.S59 It is also important to learn from cases where technology has not been widely implementable for reasons which could have been avoided by considering end‐stage implementation, to ensure that outputs are feasibly deliverable at scale.
Education
Structured education is one of the key ways in which PLWD are given information around self‐management when diagnosed, with DAFNES60 and DESMONDS61 representing the main courses for people with type 1 and type 2 diabetes respectively. Additional factors which could impact diabetes self‐management in older people have been highlighted throughout this paper, and include frailty, how to manage diabetes alongside additional long‐term conditions, cognitive decline and anxiety around needing to relinquish control of care. These factors and their potential consequences were not thought to be sufficiently covered in these courses at present.
In addition to this, older PLWD people who are diagnosed early in life may benefit from a refreshed version of the core course when updated information is provided and older people who are newly diagnosed with diabetes would benefit from tailored information appropriate for their situation.
Consistency of Care
The relationship PLWD have with their HCPs can be critical to their experience of care and its outcomes throughout life, and the benefits of continuity of careS62 both in terms of maintaining these relationships and the management decisions made with trusted HCPs wherever possible have been established.S63 When the need for care becomes more frequent in any context, particularly when living in long‐term care settings which report high staff turnover, this can become more difficult to maintain and this may affect the consistency of care and increase the anxiety reported by older PLWD around allowing HCPs to control more of their diabetes management.S65.
Long‐term care plans addressing all eventualities and detailing how a person living with diabetes would want to be cared for in different situations, co‐created between the person in question and their HCPs before they need to be implemented were proposed. These could provide consistency in care and also empower PLWD, by giving some certainty on the next steps. These could be maintained across social and health care providers and would cover any issues which could affect an older person's ability to live independently with diabetes.
3.7.2. Research recommendations
Technology
Research to establish adaptations to existing technology and pathways for trialling and incorporating emerging technology into care could transform how PLWD are supported to live independently.
Education
Research to establish how to adapt current structured education so it can cover additional issues older PLWD face could support and empower them to continue to live independently for longer, despite additional challenges.
Consistency of Care
Whilst this would be a significant shift in how to care for older people with diabetes is delivered which would require more than research to implement, research to determine how this could be done and establish what it needs to do is a critical step towards changing practice.
3.7.3. What will be needed?
Technology
Carry out a mapping exercise of the options currently available within supportive technology for older people, including those not focusing on diabetes care. This should include emerging options that have not yet been widely implemented such as personal care robotics.S66
Alongside this, qualitative research should be carried out with older people with diabetes living independently from a range of backgrounds and clinical needs to assess how technology could meet these needs.
-
Subsequent research to map the needs to the options for supportive technology would be able to identify three types of future research to help meet them:
Technology that could meet identified needs for implementation research.
Examples where existing devices need to be appropriately adapted to meet a need.
Gaps in technology where a specific device needs to be developed.
Any output from this work would need to involve significant co‐design which was representative of the target audience for the new technology.
Education
Map the content of current structured education programmes and any work to look at how diabetes care and education needs to adapt to changes in older age, to determine the gaps which need to be addressed.S67
Carry out qualitative research with older people who experienced structured education in the past and older people newly diagnosed with diabetes to determine how to deliver the information required, followed by co‐design of educational interventions.
This would need to include recruitment of representative groups of PLWD, to ensure that the ways of delivering the information are suitable for people from different backgrounds and address any barriers which may exist.
Consistency of care
Qualitative research is needed to explore whether consistent long‐term diabetes care plans which can address future care needs are something older PLWD want and whether they would provide reassurance.
If this work showed that such a model could be effective, a format for care plan documentation should be co‐designed by PLWD who would be likely to need one soon (50–60 years old) and HCPs specialists in diabetes care and geriatrics.
These would need to be holistic plans to cover all potential clinical concerns, but also be delivered with consideration to the factors identified in qualitative research to make them most beneficial to their recipients.
3.8. Research Question 8: What are the benefits of models of peer support for older people with diabetes, both when living independently and when in care?
3.8.1. Background and potential impact
There is evidence that peer support can be a tool that can support people living with long term conditions such as diabetes with self‐management in several ways and contexts,S68 but this is often under‐appreciated. This is partly because whilst the improvements in clinical measures can be statistically significant,S69 benefits are most clearly seen in behavioural or psychosocial outcomesS70,S71,S72 and how empowered PLWD are to self‐manage their condition,S73 with positive changes also observed in participants' family members. Additionally, there is evidence from studies on older people not living with diabetes that some of the additional challenges older PLWD may be more likely to face, such as loneliness and social isolation, can be helped by peer support interventions.S74
Models captured within the term peer support also vary significantly, including support groups set up and managed independent of care, clinically linked support groups and dedicated peer support roles either in community care or the MDT for someone with experience of living with diabetes.S75 The increasing prevalence of remote care which technology has enabled also applies to this approach, with evidence that peer support through social media and online communities can be effective as well.S76
As a result, the best way for this to be delivered is often unclear, as is how it can and should be adapted to support older PLWD who may face different challenges and have different needs. Research to establish how best to provide or enable peer support for older people with diabetes is needed, and how it could be delivered.
3.8.2. Research recommendation
Research to understand which models of peer support have been used previously in this population, what is effective about them and how to maximise the benefit from this service could have an enormous impact on the QoL of PLWD.
3.8.3. What will be needed?
Existing models through which PLWD provide advice and support to each other should be scoped to understand what works and what could be improved in a model framework specific to older PLWD. This should cover both official programmes and unofficial networks through which peer support is provided.
This information should be taken to focus groups of older PLWD to define a peer support intervention that is specific to their needs, both in terms of format and content. Multiple groups would need to be convened, to cover the way that needs and therefore peer support interventions' effectiveness can vary by the culture and socioeconomic status of the audience it would be delivered to [S77].
Careful consideration needs to be paid to all participants. Peer support interventions do require that those receiving them want to engage with other people with the condition for advice and support, which may not be universal. Equally, the peers delivering the intervention will need training, clear boundaries, and support from HCPs outside of the intervention and will need to be carefully selected to criteria identified in the scoping and focus group stage of development.
When a potential model for peer support has been prepared, they should undergo feasibility studies to look at their effectiveness and cost‐effectiveness and inform a future wider trial to compare different models.
A wide range of outcomes should be tested whenever a potential model of peer support is assessed, as the benefits can be wide‐ranging, and risk being overlooked. In addition to metabolic measures and QoL, this should include measures of loneliness, frequency of hospitalisation, mental health measures such as PHQ4/2 and the impact on PLWD’s ability to remain living independently rather than in care.
3.8.4. Cross‐cutting themes
In addition to these eight sets of research recommendations for defined research questions, four cross‐cutting themes within them were identified as relevant to research in the area. It is also worth noting that whilst these recommendations are for all types of diabetes, it was stressed that due to the differences in treatment and care required, research projects should consider the needs of different types of diabetes separately.
Co‐design
The first was the importance of meaningful and truly representative co‐design. PLWD with relevant experience should have roles as co‐designers in all research that sets out to address how their care is designed and delivered. Methods to do this effectively have been established and assessed,S78 where chronological age per se was not found to be a barrier, but it needs to be planned, resourced and evaluated. Funders and researchers should consider how this can be made standard practice.
Long‐term perspective
The second highlighted that in several cases significant changes to how care is delivered may be required, such as more integrated person‐centred care and changes to the education of non‐diabetes specialist HCPs. What is needed to achieve this extends beyond the remit of research. Work to change culture, buy‐in from those who organise and provide care, among other stakeholders, and evidence of acceptability, clinical effectiveness and cost‐effectiveness will all be vital, and these will be long term projects. However, the research recommended in this paper is a critical step towards driving this change and should be prioritised as such.
Sharing best practice
Thirdly, and related to the need for system‐wide change, whenever research or improvement work improves care, the importance of sharing this and ensuring it is propagated to other centres was emphasised. Not doing so will result in inconsistency in care and health inequalities, and better sharing of best practice and knowledge is needed.
Quality of life
Finally, and crucially, the importance of QoL measurements were raised in every working group's recommendations. The experience older people with diabetes have of care is often not a central tenet of research, and the consensus from the workshop was that this must change.
3.8.5. Strengths and limitations to this work
As far as we know, this initiative was the first in the UK and wider Europe that has comprehensively examined the knowledge and research horizon for diabetes in older people with an emphasis on PLWD involvement at all stages of the workshops. A similar two‐day workshop was conducted in 2019 in Boston, USA, where research priorities in this area were discussed (79) but patient and public involvement was less pronounced and the format was primarily based on expert lectures with discussion. Nevertheless, similar to our workshops, topics such as long‐term nursing care of residents with diabetes, use of medical technology, and management of frailty were commonly raised points for discussion.
A limitation of our work related to our lack of employing a more detailed and objective method for documenting the roles and input of PLWD such as guidance for reporting involvement of patients and the public (GRIPP) 2 methodology (80) in this series of workshops that would have added greater transparency as well as perhaps more obvious credibility to our conclusions. However, we can confirm a significant and crucial involvement of PLWD at all stages of the workshops and accompanying narrative. Another limitation relates to the lack of an analysis of how we approach the next steps in the co‐design research process in the priorities identified. However, we already had clear objectives specified for the workshops and greater discussion of ‘next steps’ was considered to be beyond the remit of this current work because it would also have required other stakeholder involvement. In addition, our primary focus was on crystallising what PLWD and their carers considered to be the key areas where there were shortfalls in knowledge and care processes, and where research would be beneficial to clinical outcomes.
4. CONCLUSIONS
This workshop emphasised that there are stark gaps, both in the care that older people with diabetes receive and our understanding of the best way to deliver this. Addressing this effectively will require further investment in research, and informing how best to deliver care to ensure PLWD can stay independent as long as possible with an appreciable QoL. Undertaking this innovative work and its accompanying narrative has been a significant learning curve for Diabetes UK and all those involved in the workshops. Further work of this nature by Diabetes UK will include better methodology to document more objectively the individual contributions of all participants and, in particular, this will ensure greater transparency of how those individuals with lived experiences of diabetes we involved. The next steps will be a collaborative initiative that involves additional stakeholders and funders as well as PLWD who will play a crucial role in agreeing with priorities for enhancing care leading to improved and worthwhile clinical outcomes. Diabetes UK calls on the research community, partner organizations and funders to establish how we can work together to deliver this.
CONFLICT OF INTEREST
SCB: Honoraria received from Astra‐Zeneka, Boehringer Ingelheim, Eli Lilly, Merck Sharp and Dohme, Novo Nordisk, Roche, Sanofi‐Aventis. Owns a share of Glycosmedia which carries sponsorship declared on site. Provided expert advice to the All‐Wales Medicines Strategy Group and the National Institute for Health and Care Excellence.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
Financial support for the workshop was provided by Diabetes UK. The design of and facilitation for the workshop was provided by the CollectiveTM Facilitation Ltd. Our thanks go to all attendees (Appendix I) and pre‐filmed speakers who were unable to attend for providing their time and expertise, and to the expert advisory group for supporting the development of the workshop.
APPENDIX I.
WORKSHOP ATTENDEES
All attendees will be contacted for consent to include their name on submission and a complete list will be supplied prior to acceptance/publication.
Wylie TAF, Morris A, Robertson E, et al. Ageing well with diabetes: A workshop to co‐design research recommendations for improving the diabetes care of older people. Diabet Med. 2022;39:e14795. doi: 10.1111/dme.14795
REFERENCES
- 1. Diabetes UK . Number of people with diabetes. Online. Available at: https://www.diabetes.org.uk/about_us/news/diabetes‐prevalence‐2019 [Accessed 13 August 2021]
- 2. NHS Digital . National Diabetes Audit, 2018‐19. Full Report 1: Characteristics of People with Diabetes. 2020. Available at: https://digital.nhs.uk/data‐and‐information/publications/statistical/national‐diabetes‐audit
- 3. Sinclair A, Dunning T, Rodriguez‐Mañas L. Diabetes in older people: new insights and remaining challenges. Lancet Diabetes Endocrinol. 2015;3(4):275‐285. [DOI] [PubMed] [Google Scholar]
- 4. Sinclair A, Saeedi P, Kaundal A, Karuranga S, Malanda B, Williams R. Diabetes and global ageing among 65–99‐year‐old adults: Findings from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2020;14:65‐99. [DOI] [PubMed] [Google Scholar]
- 5. Mikton C, de la Fuente‐Núñez V, Officer A, Krug E. Ageism: a social determinant of health that has come of age. Lancet. 2021;397(10282):1333‐1334. doi: 10.1016/S0140-6736(21)00524-9 [DOI] [PubMed] [Google Scholar]
- 6. Finer S, Robb P, Cowan K, Daly A, Shah K, Farmer A. Setting the top 10 research priorities to improve the health of people with Type 2 diabetes: a Diabetes UK‐James Lind Alliance. Lancet Diabetes Endocrinol. 2017;5(12):935‐936. [DOI] [PubMed] [Google Scholar]
- 7. Sinclair AJ, Abdelhafiz AH. Age, frailty and diabetes—triple jeopardy for vulnerability to COVID‐19 infection. EClinicalMedicine. 2020;22:100343. doi: 10.1016/j.eclinm.2020.100343. Published 2020 Apr 23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sinclair AJ, Gadsby R, Abdelhafiz AH, Kennedy M. Failing to meet the needs of generations of care home residents with diabetes: a review of the literature and a call for action. Diabet Med. 2018;35(9):1144‐1156. doi: 10.1111/dme.13702 [DOI] [PubMed] [Google Scholar]
- 9. Sinclair AJ, Abdelhafiz AH, Forbes A, Munshi M. Evidence‐based diabetes care for older people with Type 2 diabetes: a critical review. Diabet Med. 2019;36(4):399‐413. doi: 10.1111/dme.13859 [DOI] [PubMed] [Google Scholar]
- 10. Srikanth V, Sinclair AJ, Hill‐Briggs F, Moran C, Biessels GJ. Type 2 diabetes and cognitive dysfunction‐towards effective management of both comorbidities. Lancet Diabetes Endocrinol. 2020;8(6):535‐545. doi: 10.1016/S2213-8587(20)30118-2. PMID: 32445740. [DOI] [PubMed] [Google Scholar]
- 11. Cruz‐Jentoft AJ, Carpena‐Ruiz M, Montero‐Errasquín B, Sánchez‐Castellano C, Sánchez‐García E. Exclusion of older adults from ongoing clinical trials about type 2 diabetes mellitus. J Am Geriatr Soc. 2013;61(5):734‐738. doi: 10.1111/jgs.12215 [DOI] [PubMed] [Google Scholar]
- 12. Schernthaner G, Schernthaner‐Reiter MH. Diabetes in the older patient: heterogeneity requires individualisation of therapeutic strategies. Diabetologia. 2018;61(7):1503‐1516. doi: 10.1007/s00125-018-4547-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yakaryılmaz FD, Öztürk ZA. Treatment of type 2 diabetes mellitus in the elderly. World J Diabetes. 2017;8(6):278‐285. doi: 10.4239/wjd.v8.i6.278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Beverly EA, Wray LA, LaCoe CL, Gabbay RA. Listening to older adults’ values and preferences for type 2 diabetes care: a qualitative study. Diabetes Spectr. 2014;27(1):44‐49. doi: 10.2337/diaspect.27.1.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shortell SM, Addicott R, Walsh N, Ham C. The NHS five year forward view: lessons from the United States in developing new care models. BMJ. 2015;21(350): doi: 10.1136/bmj.h2005. PMID: 25899794. [DOI] [PubMed] [Google Scholar]
- 16. Harlock J, Caiels J, Marczak J, et al. Challenges in integrating health and social care: the Better Care Fund in England. J Health Serv Res Policy. 2020;25(2):86‐93. doi: 10.1177/1355819619869745. Epub 2019 Sep 4 PMID: 31483684. [DOI] [PubMed] [Google Scholar]
- 17. Rocks S, Berntson D, Gil‐Salmerón A, et al. Cost and effects of integrated care: a systematic literature review and meta‐analysis. Eur J Health Econ. 2020;21(8):1211‐1221. doi: 10.1007/s10198-020-01217-5. Epub 2020 Jul 6. PMID: 32632820; PMCID: PMC7561551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bunn F, Goodman C, Russell B, et al. Supporting shared decision making for older people with multiple health and social care needs: a realist synthesis. BMC Geriatr. 2018;18(1):165. doi: 10.1186/s12877-018-0853-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sinclair A, Bellary S, Dhatariya KK. Diabetes in older adults—time to include frailty as a care indicator. Diabet Med. 2021;38:e14560. doi: 10.1111/dme.14560 [DOI] [PubMed] [Google Scholar]
- 20. Laiteerapong N, Huang ES, Chin MH. Prioritization of care in adults with diabetes and comorbidity. Ann N Y Acad Sci. 2011;1243:69‐87. doi: 10.1111/j.1749-6632.2011.06316.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rayman G, Kar P. Diabetes: GIRFT Programme National Specialty Report. 2020. Online. Available at: https://www.gettingitrightfirsttime.co.uk/wp‐content/uploads/2020/11/GIRFT‐diabetes‐report.pdf Accessed 13 August 2021
- 22. Shepherd S. Coordinated care: a patient perspective on the impact of a fragmented system of care on experiences and outcomes, drawing on practical examples. Future Hosp J. 2016;3(2):136‐138. doi: 10.7861/futurehosp.3-2-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McKnight JA, Morris AD, Cline D, et al. Implementing a national quality assurance system for diabetes care: the Scottish Diabetes Survey 2001–2006. Diabet Med. 2008;25(6):743‐746. doi: 10.1111/j.1464-5491.2008.02453.x [DOI] [PubMed] [Google Scholar]
- 24. Department of Health and Social Care . The future of healthcare: our vision for digital, data and technology in health and care. 2018. Online. Available at: https://www.gov.uk/government/publications/the‐future‐of‐healthcare‐our‐vision‐for‐digital‐data‐and‐technology‐in‐health‐and‐care/the‐future‐of‐healthcare‐our‐vision‐for‐digital‐data‐and‐technology‐in‐health‐and‐care Accessed 13 August 2021
- 25. Baxter S, Johnson M, Chambers D, et al. Understanding new models of integrated care in developed countries: a systematic review. Health Serv Deliv Res. 2018;6(29):1‐132. [PubMed] [Google Scholar]
- 26. Gordon AL, Goodman C, Davies SL, et al. Optimal healthcare delivery to care homes in the UK: a realist evaluation of what supports effective working to improve healthcare outcomes. Age Ageing. 2018;47(4):595‐603. doi: 10.1093/ageing/afx195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sy SL, Munshi MN. Caring for older adults with diabetes during the COVID‐19 pandemic. JAMA Intern Med. 2020;180(9):1147‐1148. doi: 10.1001/jamainternmed.2020.2492 [DOI] [PubMed] [Google Scholar]
- 28. Diabetes UK . Future of Diabetes Report. 2017. Available at https://www.diabetes.org.uk/resources‐s3/2017‐11/1111B%20The%20future%20of%20diabetes%20report_FINAL_.pdf Accessed 13 August 2021
- 29. British Geriatrics Society . British Geriatrics Society Diabetes. Online. 2018. Available at: https://www.bgs.org.uk/resources/diabetes Accessed 13 August 2021
- 30. Kayyali R, Slater N, Sahi A, Mepani D, Lalji K, Abdallah A. Type 2 Diabetes: how informed are the general public? A cross‐sectional study investigating disease awareness and barriers to communicating knowledge in high‐risk populations in London. BMC Public Health. 2019;19(1):138. Published 2019 Jan 31. doi: 10.1186/s12889-019-6460-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Barber ND, Alldred DP, Raynor DK, et al. Care homes’ use of medicines study: prevalence, causes and potential harm of medication errors in care homes for older people. Qual Saf Health Care. 2009;18(5):341‐346. doi: 10.1136/qshc.2009.034231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Montiel‐Luque A, Núñez‐Montenegro AJ, Martín‐Aurioles E, et al. Medication‐related factors associated with health‐related quality of life in patients older than 65 years with polypharmacy. PLoS One. 2017;12(2):e0171320;. doi: 10.1371/journal.pone.0171320. Published 2017 Feb 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Trend‐UK . An Integrated Career and Competency Framework for Diabetes Nursing. 2015. Online. Available at https://trenddiabetes.online/wp‐content/uploads/2017/02/TREND_4th‐edn‐V10.pdf Accessed 13 August 2021
- 34. Williams OE, Elghenzai S, Subbe C, Wyatt JC, Williams J. The use of telemedicine to enhance secondary care: some lessons from the front line. Future Hosp J. 2017;4(2):109‐114. doi: 10.7861/futurehosp.4-2-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stack E, King R, Janko B, et al. Could in‐home sensors surpass human observation of people with Parkinson's at high risk of falling? An ethnographic study. Biomed Res Int. 2016;2016:3703745. doi: 10.1155/2016/3703745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Joyce NR, McGuire TG, Bartels SJ, Mitchell SL, Grabowski DC. The impact of dementia special care units on quality of care: an instrumental variables analysis. Health Serv Res. 2018;53(5):3657‐3679. doi: 10.1111/1475-6773.12867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hernández Morante JJ, Gómez Martínez C, Morillas‐Ruiz JM. Dietary factors associated with frailty in old adults: a review of nutritional interventions to prevent frailty development. Nutrients. 2019;11(1):102. Published 2019 Jan 5. doi: 10.3390/nu11010102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Travers J, Romero‐Ortuno R, Bailey J, Cooney MT. Delaying and reversing frailty: a systematic review of primary care interventions. Br J Gen Pract. 2019;69(678):e61‐e69. doi: 10.3399/bjgp18X700241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yanase T, Yanagita I, Muta K, Nawata H. Frailty in elderly diabetes patients. Endocr J. 2018;65(1):1‐11. doi: 10.1507/endocrj.EJ17-0390. Epub 2017 Dec 14 PMID: 29238004. [DOI] [PubMed] [Google Scholar]
- 40. National Institute for Health and Care Excellence . Type 2 diabetes in adults: management NICE guideline [NG28]. Online. Available at https://www.nice.org.uk/guidance/ng28/chapter/Recommendations#dietary‐advice‐and‐bariatric‐surgery Accessed 13 August 2021
- 41. Castrejón‐Pérez RC, Gutiérrez‐Robledo LM, Cesari M, Pérez‐Zepeda MU. Diabetes mellitus, hypertension and frailty: a population‐based, cross‐sectional study of Mexican older adults. Geriatr Gerontol Int. 2017;17(6):925‐930. doi: 10.1111/ggi.12805 [DOI] [PubMed] [Google Scholar]
- 42. Chen LK, Chen YM, Lin MH, Peng LN, Hwang SJ. Care of elderly patients with diabetes mellitus: a focus on frailty. Ageing Res Rev. 2010;9(Suppl 1):S18‐S22. doi: 10.1016/j.arr.2010.08.008 [DOI] [PubMed] [Google Scholar]
- 43. Kitamura A, Seino S, Taniguchi Y, et al. Impact of lifestyle‐related diseases and frailty on the incidence of loss of independence in Japanese community‐dwelling older adults: a longitudinal study on aging and health in Kusatsu. Nihon Koshu Eisei Zasshi. 2020;67(2):134‐145. doi: 10.11236/jph.67.2_134 [DOI] [PubMed] [Google Scholar]
- 44. Toschi E, Munshi MN. Benefits and challenges of diabetes technology use in older adults. Endocrinol Metab Clin North Am. 2020;49(1):57‐67. doi: 10.1016/j.ecl.2019.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ruedy KJ, Parkin CG, Riddlesworth TD, Graham C; DIAMOND Study Group . Continuous glucose monitoring in older adults with type 1 and type 2 diabetes using multiple daily injections of insulin: results from the DIAMOND trial. J Diabetes Sci Technol. 2017;11(6):1138‐1146. doi: 10.1177/1932296817704445. Epub 2017 Apr 28. PMID: 28449590; PMCID: PMC5951040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. NHS . Flash Glucose Monitoring: National Arrangements for Funding of Relevant Diabetes Patients. 2019. Online. Available at https://www.nhs.uk/conditions/type‐1‐diabetes/flash‐monitoring‐freestyle‐libre/
- 47. Mattishent K, Lane K, Salter C, et al. Continuous glucose monitoring in older people with diabetes and memory problems: a mixed‐methods feasibility study in the UK. BMJ Open. 2019;9(11):e032037. Published 2019 Nov 18. doi: 10.1136/bmjopen-2019-032037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hope SV, Taylor PJ, Shields BM, Hattersley AT, Hamilton W. Are we missing hypoglycaemia? Elderly patients with insulin‐treated diabetes present to primary care frequently with non‐specific symptoms associated with hypoglycaemia. Prim Care Diabetes. 2018;12(2):139‐146. doi: 10.1016/j.pcd.2017.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chow L, Seaquist ER. How significant is severe hypoglycemia in older adults with diabetes? Diabetes Care. 2020;43(3):512‐514. doi: 10.2337/dci19-0069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Abdelhafiz AH, McNicholas E, Sinclair AJ. Hypoglycemia, frailty and dementia in older people with diabetes: reciprocal relations and clinical implications. J Diabetes Complications. 2016;30(8):1548‐1554. doi: 10.1016/j.jdiacomp.2016.07.027 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


