Abstract
Background and Objectives
Physician health programs (PHPs) have demonstrated efficacy, but their mechanism of influence is unclear. This study sought to identify essential components of PHP care management for substance use disorder (SUD), and to assess whether positive outcomes are sustained over time.
Methods
Physicians with DSM‐IV diagnoses of Substance Dependence and/or Substance Abuse who had successfully completed a PHP monitoring agreement at least 5 years before the study (N = 343) were identified as eligible. Of the 143 (42%) that could be reached by phone, 93% (n = 133; 86% male) completed the anonymous online survey.
Results
Virtually all PHP program components were rated as being at least “somewhat helpful” in promoting recovery, with the plurality of respondents rating almost all components as “extremely helpful.” The top‐rated components were: signing a PHP monitoring agreement, participation in the PHP, formal SUD treatment, and attending 12‐step meetings, with each receiving a mean rating of at least 6.2 out of 7. Notably, 88% of respondents endorsed continued participation in 12‐step fellowships. Despite the significant financial burden of PHP participation, 85% of respondents reported they believed the total financial cost of PHP participation was “money well spent.”
Discussion and Conclusions
Components of PHP monitoring were viewed as acceptable and helpful to physicians who completed the program, and outcomes were generally sustained over 5 years. More studies are needed to confirm these preliminary findings.
Scientific Significance
This study documents the perceived cost‐benefit of participation in a PHP among a small sample of program completers.
INTRODUCTION
Drug epidemics are measured in part by the prevalence of substance use disorder (SUD) within a population. In 2019, an estimated 20.4 million Americans aged 12 or older (about 7.4% of the population) had a SUD. 1 With increased overdose deaths 2 contributing to 3 years of decline in life expectancy in the United States, 3 there is an urgent need to increase access to SUD treatment and improve patient outcomes. Treatment has changed over many decades, with an improved understanding of SUD as a chronic relapsing brain disease. 4 Like other chronic health conditions, SUD must be managed for many years, with recurrence of symptoms expected during the course of treatment. But unlike those other conditions, treatment “success” for SUD is typically measured in the short‐term (i.e., decreases in substance use) instead of sustained abstinence and recovery. 5 A notable exception to this approach exists for SUD treatment of individuals in safety‐sensitive professions, for whom dedicated profession‐based care programs are available. 6
SUDs and treatment among physicians
Estimated rates of SUDs among physicians are similar to or slightly higher than in the general population. 7 A study of 7209 physicians 8 found 15.3% reported symptoms consistent with alcohol use disorder. Contributing risk factors for SUD among healthcare professionals include access to substances in the work environment, perceived invincibility or immunity to substance‐related impairments, and work role‐related stress. 9 There are also unique challenges associated with treating physicians diagnosed with SUDs. Physicians often exhibit overconfidence in their ability to control their substance use due to their medical knowledge. 10 , 11 Many resist accessing treatment until their ability to continue working is in jeopardy, 12 and most do not seek treatment voluntarily. Instead, they may come to the attention of their colleagues and supervisors due to excessive absences, behavioral changes, impaired work performance, or even overdose. Once identified, physicians are typically connected to a physician health program (PHP), which facilitates referral for a comprehensive assessment of substance use history, psychiatric diagnoses, personality functioning, and neurocognitive functioning to determine fitness‐for‐duty. 13
Physician health programs
PHPs are state programs whose primary dual missions include: (1) supporting physicians diagnosed with a potentially‐impairing condition (i.e., SUD, severe psychiatric disorder, cognitive disorder, or other medical condition) and (2) protecting patient safety by providing monitoring services. Most participants with a moderate‐severe SUD sign a monitoring agreement with a duration of 5 years. Monitoring agreements typically include random drug screening, participation in facilitated group meetings and mutual support groups, and quarterly evaluations completed by healthcare professionals working with the enrolled physician. 14 Participation is typically confidential and voluntary, representing an alternative to discipline by the state medical/licensing board.
PHP outcomes are remarkably favorable compared to outcomes for individuals with SUD in the general population and have produced the best long‐term outcomes for individuals with SUDs, 13 , 15 including those with opioid use disorders. 16 McLellan and colleagues 13 found that 80.7% of 802 PHP participants successfully completed their 5‐year agreements, with 78.7% continuing working with no license restrictions. Though debate exists over the potentially coercive nature of PHP care, 17 , 18 many PHP components have been integrated into other forms of SUD treatment and care management. 19 For example, sustained post‐treatment monitoring and support have become standard features in efforts to extend acute care into recovery management models nested within larger recovery‐oriented systems of care. 20 , 21 , 22 Yet, the specific reason(s) for the success of the PHP model are not well‐understood, and the stability of favorable outcomes is unknown due to the lack of studies assessing recovery status after PHP monitoring has ended. This study targeted physicians who successfully completed PHP SUD monitoring agreements five or more years earlier. Specific aims were to (1) identify the essential components of PHP care management and (2) determine whether positive outcomes are sustained when monitoring ends.
METHODS
Participants
The sample included 133 physicians with a DSM‐IV diagnosis of Substance Dependence and/or Substance Abuse who had successfully completed a PHP monitoring agreement at least 5 years before the study. Physicians who voluntarily elected to continue some level of PHP participation were eligible for the study, as long as the PHP determined that they qualified for “graduation” from the PHP by January 1, 2009.
Procedures
Study procedures were approved by the Chestnut Health Systems IRB. Eight PHPs assisted with study recruitment. PHP staff were provided with a manual outlining recruitment procedures and participated in multiple training conference calls to ensure adequate competence with the protocol. PHPs were asked to identify at least 30 former PHP participants who were eligible for the study by examining participant records for those who completed a SUD monitoring agreement no later than January 1, 2009 (and moving consecutively backward in time, contacting each eligible physician in order, until reaching the target number).
Eligible individuals were contacted in 2014–2015 by PHP staff via phone, using IRB‐approved scripts. PHP staff provided potential study participants with a brief description of the study, reviewed the time required to participate (about 30 min), and assured anonymity of participation. Potential study participants were provided a link to the online survey hosted on SurveyMonkey.com. Disinterested individuals were asked the reason(s) they did not want to participate. The PHP staff were asked to make at least three attempts to contact each eligible physician; however, due to staff time constraints, some PHPs made only one or two attempts. Given the length of time since their PHP participation, up‐to‐date phone numbers were not available for all eligible physicians, and no attempts were made to contact physicians via email or letters. The PHPs were encouraged to continue identifying/contacting eligible program completers until at least 20 individuals agreed to participate in the study. See Figure 1 for the breakdown of study participation.
Figure 1.
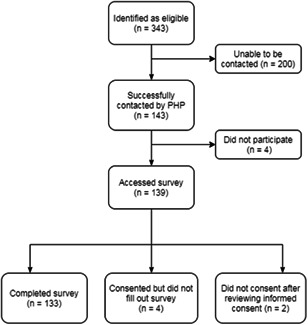
CONSORT Diagram for study participation
Study measure
The questionnaire was developed by members of the study team with significant expertise in the areas of SUD treatment, monitoring of professionals with potentially‐impairing conditions, and PHP care. The first page of the online survey contained informed consent. To maintain anonymity, participants typed “I give my consent” rather than signing their names.
The questionnaire included 100 items assessing the physicians' medical training and certification, experiences with the PHP [i.e., reason(s) for referral and monitoring parameters], and views regarding the helpfulness of PHP program elements (i.e., initial PHP contact, formal assessment/evaluation, formal SUD treatment, treatment for comorbid conditions, signing a monitoring agreement, random drug testing, worksite monitors, 12‐step meetings, Caduceus meetings, monitoring group meetings, and individual counseling/therapy). PHP components were rated on an 8‐point scale, with 0 = “did not participate,” and the remaining response options ranging from 1 = “extremely unhelpful” to 7 = “extremely helpful.” Items assessed experiences related to recurrence of substance use and recovery both during and after the monitoring period, the perceived cost/benefit of PHP participation, and overall satisfaction with PHP care. Participants were invited to respond to open‐ended questions about their experiences. The questionnaire concluded with a series of demographic questions and an assessment of truthfulness in responding.
Data analysis
All available data were included in the analyses. Due to some missing data, the number of responses for each item differs slightly. The n for each item is reported in the results/tables. Descriptive statistics were computed using SPSS v.27. The first and last authors reviewed qualitative responses and selected representative quotes for inclusion.
RESULTS
Response rate
Staff at eight PHPs identified 343 eligible physicians and successfully contacted 143 (42%) of them. Given differences among PHPs in maintaining up‐to‐date contact information, the number of eligible individuals in each program, and the amount of time required to re‐contact individuals who did not answer on the first attempt, there was significant variability in rates of successful contact among the PHPs. This ranged from a low of 24% (34 out of 141 eligible physicians contacted) for the largest program to 80% (4 out of 5 eligible physicians contacted) for the smallest program. Of the 143 physicians successfully contacted, 93% submitted survey responses, resulting in a sample of 133 respondents. Reasons given to the PHPs for declining participation included: not being interested, too busy, concerns about privacy/anonymity, and being retired/retiring.
Demographics
To ensure anonymity, respondents were only asked to indicate their age, sex, and marital status. A total of 127 physicians (95% of the study sample) fully answered these demographic questions. This group was 86% male, ranging in age from 35–86 years old (M = 56, SD = 9.2). The majority (80%) were currently married, 13% were divorced or separated, 3% were single, and 4% were in a long‐term committed relationship. Most participants (95%) reported being “completely honest” when completing the questionnaire, with less than 5% reporting being “mostly honest,” and one individual skipping the item. Comparison of the current sample to a large nationally‐representative sample of PHP participants from a previous study 13 demonstrated no meaningful group differences (see Table S1).
Virtually all physicians (96%) reported being currently licensed to practice medicine, with 78% practicing full‐time, 10% practicing part‐time, 7% retired, 2% working in another field, 1% unemployed, and 2% reporting “other.” None of the non‐licensed physicians reported a lack of licensure due to consequences of substance use. In this sample, 38% voluntarily extended their PHP participation at some point, with 20% still undergoing some form of voluntary monitoring.
Participant recovery journeys
Of the 131 respondents who completed items assessing recurrence of substance use, 116 (89%) completed their monitoring agreement without any return‐to‐use during the monitoring period. By contrast, 13 (10%) reported one recurrence, 1 individual (<1%) reported two recurrences, and 1 individual (<1%) reported 3 recurrences of substance use.
Using their own definition, 124 of 128 respondents (97%) reported that they currently considered themselves to be “in recovery.” Additionally, 79% of respondents (n = 101) reported no use of alcohol since the completion of their PHP monitoring agreement. A total of 23 (18%) reported any alcohol use, with 4 (3%) declining to answer. Of those reporting post‐monitoring alcohol use, 5 reported using alcohol in the first year after completing their monitoring agreement, and 14 reported alcohol use at some point in the 12 months prior to completing the survey (n = 3 declined to answer). Of participants who reported past‐year alcohol use (n = 14), 12 (86%) described their use as “benign” and 2 (14%) described their use as “malignant.” One of these individuals commented that completing the survey prompted a plan to self‐report to the PHP to obtain their support in addressing this recent alcohol use.
The vast majority (95%, n = 121) of respondents self‐reported no illicit or nonmedical use of drugs since PHP completion, 6 (5%) reported any use, and 1 (<1%) declined to answer. Among those reporting nonmedical drug use, 2 used in the first year post‐monitoring and 3 used in the past year (1 declined to answer). In addition, 49 respondents (38%) reported any use of prescribed controlled substances for medical reasons in the last year. Of these, 84% (n = 41) reported this use did not interfere with their life or threaten their sobriety, whereas 16% (n = 8) felt that it did.
Evaluation of monitoring agreement components
Two‐thirds (66%) of respondents said that participation in PHP care had been “extremely helpful,” another 17% rated it as “moderately helpful,” and only 5% indicated it was “unhelpful” (see Table 1). Ratings for the various components of care were calculated using only responses from physicians who had experience with them. All components except the worksite monitor were rated as being at least “somewhat helpful.” The plurality of respondents rated virtually all components as being “extremely helpful.” Top‐rated components of monitoring and recovery support were signing a monitoring agreement, formal SUD treatment, and attending 12‐step meetings, with each receiving a mean rating of 6.2 out of 7. Table 2 shows mandated participation in 12‐step meetings and formal SUD treatment were ranked as the most valuable components, followed by random drug and alcohol testing. When ranking the least valuable component, the top choice was “None of the above (all were valuable).” Having a worksite monitor was consistently rated as less valuable than other components and was never selected as the “most valuable” component of care.
Table 1.
Helpfulness of PHP monitoring agreement components
| Monitoring agreement component (# of physicians endorsing participation) | n | Mean rating (SD)a | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|
| PHP Participation Overall | 129 | 6.3 (1.4) | 3% | 2% | 0% | 4% | 8% | 17% | 66% |
| Signing PHP Monitoring Agreement | 130 | 6.2 (1.4) | 4% | 1% | 0% | 3% | 15% | 19% | 59% |
| Formal Substance Use Disorder Treatment | 124 | 6.2 (1.5) | 4% | 2% | 0% | 1% | 11% | 15% | 66% |
| Attending 12‐step Meetings | 127 | 6.2 (1.5) | 3% | 4% | 1% | 3% | 7% | 15% | 67% |
| Random Drug & Alcohol Testing | 130 | 5.9 (1.6) | 4% | 2% | 1% | 9% | 11% | 21% | 52% |
| Initial contact/intervention w/PHP | 128 | 5.8 (1.8) | 8% | 3% | 2% | 5% | 11% | 19% | 53% |
| Individual Counseling/therapy (not for Comorbid Psychiatric Condition) | 71 | 5.7 (1.4) | 1% | 3% | 3% | 9% | 28% | 18% | 38% |
| Formal Professional Assessment | 125 | 5.6 (1.8) | 7% | 4% | 4% | 4% | 10% | 26% | 44% |
| Other Elements of PHP Participation (e.g., retreats/reunions, meeting with PHP director, fellowship/support) | 96 | 5.6 (1.7) | 5% | 3% | 2% | 12% | 13% | 25% | 41% |
| Facilitated PHP Monitoring Group Meetings | 90 | 5.6 (1.5) | 4% | 1% | 3% | 9% | 20% | 27% | 36% |
| Treatment for Comorbid Psychiatric Condition(s) | 56 | 5.5 (1.7) | 5% | 4% | 0% | 16% | 21% | 9% | 45% |
| Attending Caduceus (Doctor “self‐help”) meetings | 117 | 5.4 (1.7) | 4% | 4% | 5% | 7% | 25% | 21% | 33% |
| Worksite Monitor | 70 | 4.8 (1.4) | 3% | 4% | 3% | 37% | 20% | 19% | 14% |
Note: 1, Extremely Unhelpful; 2, Moderately Unhelpful; 3, Somewhat Unhelpful; 4, Neither Helpful nor Unhelpful; 5, Somewhat Helpful; 6, Moderately Helpful; 7, Extremely Helpful.
Abbreviation: PHP, Physician health programs.
Mean rating calculated only among responses for individuals who reported participation in the monitoring agreement component.
Table 2.
Most and least valuable components of monitoring agreement
| Most valuable PHP monitoring agreement component (n = 131) | Rank | % Selecting as MOST valuable |
|---|---|---|
| 12‐Step Meeting Attendance | 1 | 35% |
| Formal Substance Use Disorder Treatment | 2 | 26% |
| Random Drug & Alcohol Testing | 3 | 16% |
| Treatment for Comorbid Psychiatric Condition | 4 | 8% |
| Caduceus (Doctor “self‐help”) Group Meetings | 5 | 7% |
| None of the Above (None were valuable) | 6 | 5% |
| Other (i.e., “Counseling,” “12 step program,” and “Being accountable to PHP Director”) | 7 | 2% |
| Least valuable PHP monitoring agreement component (n = 130) | Rank | % Selecting as LEAST Valuable |
|---|---|---|
| None of the Above (All were valuable) | 1 | 33% |
| Worksite Monitor | 2 | 23% |
| Caduceus/Doctor “self‐help” Group Meetings | 3 | 16% |
| Random Drug & Alcohol Testing | 4 | 10% |
| Treatment for Comorbid Psychiatric Condition | 5 | 9% |
| 12‐Step Meeting Attendance | 6 | 5% |
| Formal Substance Use Disorder Treatment | 7 | 2% |
| Other (i.e.“Drug testing 3 times a week,” and “Weekly monitoring sessions”,) | 8 | 2% |
Post‐monitoring recovery supports
Most respondents reported continued participation in 12‐step fellowships. Among 128 physicians, 112 (88%) reported attending meetings in the first year post‐monitoring and 88 (69%) reported at least some attendance at meetings in the 12 months prior to study participation (i.e., more than 4 years after monitoring agreement completion). Additionally, 47% of respondents reported that participation in religious gatherings helped them to maintain sobriety, with 57% of respondents (n = 73) currently participating in religious gatherings. Finally, 25% of respondents reported participating in other community/support meetings (e.g., Caduceus meetings) to help maintain sobriety.
Cost‐benefit of PHP participation
Reported costs of participating in PHP care and SUD treatment varied significantly (Table 3). Out‐of‐pocket personal costs ranged from $250 to $321,000 (M = $31,528, SD = $39,570, Median = $23,750). Despite the significant financial burden, 85% of respondents (n = 108) reported they believed the cost of the PHP participation was “money well spent.” Representative quotes offered in an open‐ended question included:
“The loss of income was devastating. But the costs of actual recovery are well worth the money.”
“I am able to continue in my profession and maintain/improve my family life. That is priceless.”
“Without complete 3‐month treatment I would have rationalized a way back to using, or at least wouldn't have gained openness needed in other facets of my life.”
Table 3.
Financial cost of SUD treatment and PHP participation
| Costs | Mean (SD) | Median | Range |
|---|---|---|---|
| Loss of earnings due to time away from practice | $127,128 ($379,362) | $37,500 | $0–$2,500,000 |
| Cost of initial evaluation(s) | $3682 ($6202) | $1000 | $0–$40,000 |
| Cost of treatment | $21,928 ($31,794) | $19,000 | $0–$300,000 |
| Cost of alcohol & drug testing | $4779 ($5929) | $3000 | $0–$42,120 |
| Cost of monitoring | $4503 ($8025) | $3000 | $0–$60,000 |
| Other Costs? | $6470 ($15,542) | $1000 | $0–$80,000 |
| Total Personal Cost | $31,528 ($39,570) | $23,750 | $250–$321,000 |
| Total Estimated Cost to Insurance Companya | $22,667 ($23,002) | $19,000 | $1000–$121,000 |
Abbreviations: PHP, Physician health programs; SUD, substance use disorder.
n = 38 respondents reported that their insurance provider(s) covered at least some of the cost of their clinical care.
Concerns noted by the 15% of respondents who did not feel the benefits outweighed the financial costs included:
“I found the involuntary (if you want to continue in medicine) costs somewhat high and non‐negotiable for the testing and monitoring, especially right out of residency, but it did contribute to my sobriety. If the state could handle the fees (through the general medical license fee) that would be preferable.”
“The treatment and monitoring phases could have been done far more quickly and cheaply.”
“Mostly money well spent. The malpractice insurance increase was unnecessary in my opinion (it has since returned to normal), but generally the program has allowed me to return to a normal, productive life/career. It's therefore hard to view it in a negative light.”
Satisfaction with PHP requirements and participation
When asked whether they would have been able to maintain sobriety under a “monitoring only” agreement, 76% of physicians (n = 94) reported they would have been unsuccessful without formal SUD treatment. Further, 17 of the 32 (53%) who believed they could have maintained sobriety indicated that they would not have experienced the same quality of recovery or degree of personal growth/maturity without treatment. When asked their views about allowing physicians with SUD to participate in a “monitoring only” option, 66% (n = 82) reported they would not recommend offering that option, even with the caveat that failure to maintain sobriety would result in required treatment plus the full menu of PHP services. Responses to an open‐ended follow‐up question included:
“Put simply: fear of being caught was not enough to keep me sober before participation in PHP, so I doubt it would have helped after. Without treating the underlying addiction, I would have tried to cheat the monitoring or take my chances of not being called for testing. The addiction itself must be treated.”
“I needed to be removed from my environment for an extended period of time before I was capable of choosing abstinence.”
“I think because of treatment I could truly understand the idea that I had an illness and that it had distorted my thinking process. It was helpful to be amongst peers and to not feel so full of shame or alone. I think to have just a random testing program would have made the whole undertaking feel more punitive than therapeutic.”
By contrast, those in favor of the “monitoring only” option offered the following perspectives:
“I got clean through 12‐step programs only. Treatment did not help. Professional meetings were not helpful. UDS screening, I must admit, was helpful early on.”
“I had already quit using drugs on my own and had been sober/clean for months before I was turned in to the PHP, which in turn forced me to go to treatment. Treatment was useless. An expensive and lengthy joke, administered by some very mediocre people.”
“I hate to say so, but I feel that the results would not have been terribly different. I am good at obeying rules and don't think that I would have tried to cheat.”
When asked about referring colleagues with SUD to the state PHP, 59 of 77 respondents (77%) said they would do so without reservation, 18% (n = 14) would do so but with reservation, and 5% (n = 4) would not. Notably, 41% of 128 respondents (n = 52) reported they had already referred a colleague to PHP care.
CONCLUSIONS
Results suggest that the components of PHP monitoring agreements for SUD are overwhelmingly viewed as acceptable and helpful to physicians who successfully complete the program. Participants generally described PHP care as worth the cost and crucial to their recovery, with participation in mutual support groups and completion of high‐quality intensive treatment rated as most critical to early and sustained recovery efforts. Most participants reported continued participation in mutual support groups 5 or more years after completing their monitoring agreements. In addition, self‐reported recurrence of substance use and recovery rates were extremely encouraging: 89% self‐reported that they completed their agreement without any recurrence of use during the monitoring period, with nearly 10% reporting only one recurrence. This is comparable to outcomes reported in a previous national PHP study 13 and slightly better than reported outcomes in a large single‐state study. 23 Notably, 97% of respondents reported that they currently considered themselves to be “in recovery.” This recovery rate and those in other PHP studies (consistently near 80%) far exceed the SUD remission rates in studies of other clinical populations (typically 35%–50%), most of which relied on far shorter follow‐up periods and/or a less rigorous definition of recovery. 24 , 25 , 26 Further dissemination of these results may assist physicians at initial PHP referral who are hesitant to accept services and may even dispel some of the myths about the “coercive” nature of PHPs.
Although critics of PHPs underscore the desire for an absolutely voluntary model of care, PHPs grant a safe harbor from the consequences of SUDs that would likely be delivered by others. Of note, physicians endorse being more likely to report a hypothetical colleague impaired by a SUD than one impaired by a psychiatric or cognitive disorder. 27 Furthermore, the fact that 95% of individuals with a SUD do not think they have a problem and do not want treatment 1 helps explain why many physicians appear resentful or critical of the process when first enrolling in PHP care management. Denial and impaired judgment, known consequences of SUD, present significant obstacles to timely treatment entry. 28 As a result, the “compassionate interference” 29 often administered by healthcare providers, family members, friends, employers, and colleagues, remains a vital tool in connecting individuals with SUD to appropriate treatment. PHPs can provide valuable support to this process. As this study suggests, and consistent with previous research, 30 it is often only after participants have achieved recovery that they recognize/report that the PHP saved their medical careers and even their lives.
Another criticism 31 of PHP care is that it does not typically include medication for opioid use disorder (MOUD). Although MOUD is the dominant method of OUD treatment, all treatment programs—those that use MOUD and those that do not—suffer from low rates of patient retention and high rates of recurrence of substance use. 32 No published studies of MOUD report success rates equivalent to what is observed for PHP participants, including those recovering from OUD. 16 Further, this critique represents a misconception regarding PHP care, as all PHPs encourage the use of opioid antagonist medications, and agonist medications are approved on an individual case basis when deemed appropriate. 33 This mirrors an encouraging recent development in OUD treatment for the general population, which includes the integration of MOUD into 12‐step abstinence‐based treatment programs. 34
Limitations and strengths
Some important limitations must be acknowledged. First, the relatively small sample size, consisting of PHP completers, may reflect selection bias resulting from the omission of eligible individuals who could not be reached. Though the high participation rate among those successfully contacted may help to mitigate this concern, more studies are needed to confirm these preliminary findings. Next, the study relied exclusively on self‐report data (with no verification of abstinence via drug testing), which may have introduced social desirability bias and/or recall bias from the respondents. They overwhelmingly reported being honest, with 95% indicating that they were “completely honest,” but responses were not independently verified. Another limitation is the length of time that has elapsed since the monitoring period under study. Personal costs may have changed since the participants underwent monitoring (e.g., increased cost for more expansive drug test panels), which may impact the generalizability of the findings to current PHP participants.
One strength is that this study was among the first to evaluate long‐term post‐monitoring outcomes and perspectives from a multi‐state sample of physicians who completed PHP agreements. It provides preliminary data to answer crucial questions about what happens after the formal monitoring period ends. It also provided respondents an opportunity to reflect on their experiences and to offer an assessment of the cost‐benefit of PHP participation with the benefit of hindsight. Finally, the inclusion of participants from eight different PHPs may increase the generalizability of the study findings to the broader population of physicians in recovery.
Research must continue to assess long‐term outcomes for individuals with SUDs and the best ways to achieve long‐term recovery. This study offers valuable insight by documenting what happens to physicians who successfully complete PHP SUD monitoring agreements, and demonstrating that PHP care is an integral part of achieving long‐lasting recovery for this population.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Lisa J. Merlo: Conceptualization, Methodology, Data Curation, Formal Analysis, Writing‐ Original Draft, Writing‐ Review & Editing, Visualization. Michael D. Campbell: Software, Conceptualization, Methodology, Writing‐ Review & Editing. Corinne Shea: Software, Resources, Investigation, Data Curation, Writing‐ Original Draft, Project Administration. William White: Conceptualization, Methodology, Writing‐ Review & Editing. Gregory E. Skipper: Conceptualization, Methodology. Jill A. Sutton: Writing‐ Original Draft. Robert L. DuPont: Conceptualization, Methodology, Resources, Writing‐ Review & Editing, Visualization, Supervision.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
The authors would like to thank all the physicians who participated in this study as well as the PHP staff from Idaho, Indiana, Florida, Mississippi, Missouri, Montana, New Hampshire, and Washington physician health programs who assisted with study recruitment. We also wish to acknowledge Jack Croughan, MD who provided guidance to the Research Team throughout the study period.
Merlo LJ, Campbell MD, Shea C, et al. Essential components of physician health program monitoring for substance use disorder: A survey of participants 5 years post successful program completion. Am J Addict. 2022;31:115‐122. 10.1111/ajad.13257
REFERENCES
- 1. Center for Behavioral Health Statistics and Quality . Results from the 2019 National Survey on Drug Use and Health: Detailed tables. In: Administration SAaMHS, ed. Rockville, MD2020.
- 2. Wilson N, Kariisa M, Seth P, Smith Ht, Davis NL. Drug and opioid‐involved overdose deaths—United States, 2017‐2018. MMWR Morb Mortal Wkly Rep. 2020;69:290‐297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959‐2017. JAMA. 2019;322:1996‐2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45‐47. [DOI] [PubMed] [Google Scholar]
- 5. Merlo LJ, Arana J, Stone AM. Pharmacological trials for the treatment of substance use disorders. In: Hertzman M, ed. Clinical Trials in Psychopharmacology. Wiley; 2010:207‐232. [Google Scholar]
- 6. Dupont RL, Skipper GE. Six lessons from state physician health programs to promote long‐term recovery. J Psychoactive Drugs. 2012;44:72‐78. [DOI] [PubMed] [Google Scholar]
- 7. Hughes PH, Brandenburg N, Baldwin DC Jr, et al. Prevalence of substance use among US physicians. JAMA. 1992;267:2333‐2339. [PubMed] [Google Scholar]
- 8. Oreskovich MR, Shanafelt T, Dyrbye LN, et al. The prevalence of substance use disorders in American physicians. Am J Addict. 2015;24:30‐38. [DOI] [PubMed] [Google Scholar]
- 9. Kenna G, Baldwin JN, Trinkoff AM, Lewis DC. Substance use disorders in health care professionals. In: Johnson BA, ed. Addiction Medicine: Science and Practice. Vol 1. Springer; 2011:1375‐1398. [Google Scholar]
- 10. Boisaubin EV, Levine RE. Identifying and assisting the impaired physician. Am J Med Sci. 2001;322:31‐36. [DOI] [PubMed] [Google Scholar]
- 11. Merlo LJ, Cummings SM, Cottler LB. Prescription drug diversion among substance‐impaired pharmacists. Am J Addict. 2014;23:123‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gallegos KV, Norton M. Characterization of Georgia's Impaired Physicians Program treatment population: data and statistics. J Med Assoc Ga. 1984;73:755‐758. [PubMed] [Google Scholar]
- 13. McLellan AT, Skipper GS, Campbell M, DuPont RL. Five year outcomes in a cohort study of physicians treated for substance use disorders in the United States. BMJ. 2008;337:a2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. DuPont RL, McLellan AT, Carr G, Gendel M, Skipper GE. How are addicted physicians treated? A national survey of Physician Health Programs. J Subst Abuse Treat. 2009;37:1‐7. [DOI] [PubMed] [Google Scholar]
- 15. DuPont RL, McLellan AT, White WL, Merlo LJ, Gold MS. Setting the standard for recovery: Physicians' Health Programs. J Subst Abuse Treat. 2009;36:159‐171. [DOI] [PubMed] [Google Scholar]
- 16. Merlo LJ, Campbell MD, Skipper GE, Shea CL, DuPont RL. Outcomes for physicians with opioid dependence treated without agonist pharmacotherapy in physician health programs. J Subst Abuse Treat. 2016;64:47‐54. [DOI] [PubMed] [Google Scholar]
- 17. Carr GD, Hall B, Finlayson AJR, DuPont RL. Physician health programs: the US model. In: Brower KJ, Riba MB, eds. Physician Mental Health and Well‐Being: Integrating and Primary Care. Springer International Publishing; 2017:265‐294. [Google Scholar]
- 18. Lenzer J. Physician health programs under fire. BMJ. 2016;353:i3568. [DOI] [PubMed] [Google Scholar]
- 19. Institute for Behavior and Health . The new paradigm for recovery: Making recovery—and not relapse—the expected outcome of addiction treatment. Institute for Behavior and Health; 2014. [Google Scholar]
- 20. White WL. Recovery management and recovery‐oriented systems of care: Scientific rationale and promising practices. Northeast Addiction Technology Transfer Center; 2008. [Google Scholar]
- 21. Kelly J, White WL, eds., Addiction recovery management: Theory, science and practice. Springer Science; 2011. [Google Scholar]
- 22. Dennis ML, Scott CK, Laudet A. Beyond bricks and mortar: recent research on substance use disorder recovery management. Curr Psychiatry Rep. 2014;16:442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Domino KB, Hornbein TF, Polissar NL, et al. Risk factors for relapse in health care professionals with substance use disorders. JAMA. 2005;293:1453‐1460. [DOI] [PubMed] [Google Scholar]
- 24. White WL. Recovery/remission from substance use disorders: An analysis of reported outcomes in 415 scientific studies. 1868‐2011. Great Lakes Addiction Technology Transfer Center; 2012. [Google Scholar]
- 25. Grella CE, Stein JA. Remission from substance dependence: differences between individuals in a general population longitudinal survey who do and do not seek help. Drug Alcohol Depend. 2013;133:146‐153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fleury MJ, Djouini A, Huỳnh C, et al. Remission from substance use disorders: a systematic review and meta‐analysis. Drug Alcohol Depend. 2016;168:293‐306. [DOI] [PubMed] [Google Scholar]
- 27. Farber NJ, Gilibert SG, Aboff BM, Collier VU, Weiner J, Boyer EG. Physicians' willingness to report impaired colleagues. Soc Sci Med. 2005;61:1772‐1775. [DOI] [PubMed] [Google Scholar]
- 28. Vayr F, Herin F, Jullian B, Soulat JM, Franchitto N. Barriers to seeking help for physicians with substance use disorder: a review. Drug Alcohol Depend. 2019;199:116‐121. [DOI] [PubMed] [Google Scholar]
- 29. Verkerk M. A care perspective on coercion and autonomy. Bioethics. 1999;13:358‐368. [DOI] [PubMed] [Google Scholar]
- 30. Merlo LJ, Greene WM. Physician views regarding substance use‐related participation in a state physician health program. Am J Addict. 2010;19:529‐533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Beletsky L, Wakeman SE, Fiscella K. Practicing what we preach—ending physician health program bans on opioid‐agonist therapy. N Engl J Med. 2019;381:796‐798. [DOI] [PubMed] [Google Scholar]
- 32. Fiellin DA, Weiss L, Botsko M, et al. Drug treatment outcomes among HIV‐infected opioid‐dependent patients receiving buprenorphine/naloxone. J Acquir Immune Defic Syndr. 2011;56:S33‐S38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bundy C. Opioid use disorder in physicians. N Engl J Med. 2019;381:2280‐2281. [DOI] [PubMed] [Google Scholar]
- 34. Klein AA, Seppala MD. Medication‐assisted treatment for opioid use disorder within a 12‐step based treatment center: feasibility and initial results. J Subst Abuse Treat. 2019;104:51‐63. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.


