Abstract
Objective
Physical and natural environments might strongly influence mental health and well‐being. Many studies have examined this relationship in urban environments, with fewer focused on rural settings. The aim of this systematic review was to synthesise quantitative evidence for the relationship between environmental factors (drought, climate and extreme weather events, land use/environmental degradation, green space/vegetation, engagement in natural resource management activities) and mental health or well‐being in rural areas.
Design
Following a systematic search of three databases (PsycINFO, MEDLINE and Web of Science), 4368 articles were identified, of which 28 met eligibility criteria for inclusion in the review.
Results
Poorer mental health and well‐being was typically found to have an association with extreme climate or weather events and environmental degradation. The observed relationships were largely assessed at area‐wide or community levels.
Conclusions
Studies examining the relationship between the environmental condition of land and mental health at an individual level, particularly within farms, are lacking. Addressing this gap in research requires interdisciplinary expertise and diverse methodology. Few studies examined the effects of natural resource management practices/principles or biodiversity on mental health. While there is evidence that extreme climate or weather events have a negative impact on mental health in rural areas, there remain considerable gaps in our knowledge of how rural environments influence mental health and well‐being.
Keywords: biodiversity, degradation, drought, environment, farmers, mental health, rural
What is already known on this subject:
Natural and physical environments can have impacts on mental health and well‐being
Many studies have investigated this relationship in urban settings, with fewer in rural settings
Previous reviews have found weak effects between green space and mental health, although clear associations between drought and mental ill health have been reported
What this study adds:
No previous review has examined the relationship between environment and mental health specifically in rural settings
This systematic review identified 28 articles that quantified a relationship between environment and mental health in rural areas
The review identified gaps in the literature related to the effects of individual‐level environmental factors, biodiversity and natural resource management
1. INTRODUCTION
There is a growing body of literature suggesting that the physical and natural environments in which people live and work play important roles in mental health and well‐being. Theoretical frameworks and empirical evidence suggest multiple potential pathways for the environment to influence mental health. A poor physical environment might directly lead to physiological stress responses associated with poor mental health, 1 while exposure to high‐quality natural and physical environments might be associated with cognitive restoration and a greater sense of control. 2 In addition, perceived or objective indicators of poor natural environment are associated with reduced quality of social supports 2 and increased sedentary behaviour, 3 which are both associated with poorer mental health. Previous reviews have examined the effects of physical environment, 4 built environment, 5 climate change 6 , 7 and green space 8 on mental health. There have been mixed findings to date, with weak effects for green space and environmental conditions on mental health with many studies demonstrating poor quality that precludes causal inferences. Clear associations have been established between drought and mental ill health, including suicide. 4 , 9 Similarly, other extreme weather events tend to have well‐document impacts on trauma responses. 6 However, beyond specific climatic events, the broader effects of climate change, natural resource management or degradation, and biodiversity on mental health have not been adequately quantified. 6 , 10 , 11 , 12
The majority of studies described in existing reviews have primarily examined people living in urban areas, with limited evaluation of differences between rural and urban settings in the effects of environmental conditions. There might be differences in how people from rural areas, particularly in farming communities, view and respond to the natural environment. 13 , 14 The potential impact on mental health of the rural environment might be more salient, as it provides the basis of livelihoods and is enmeshed with the lives of the community. 10 Therefore, there is a need to separately examine the evidence for how the environment impacts on mental health and well‐being in rural communities. Identifying clear relationships between aspects of the environment and mental health might provide avenues for strengthening vulnerable rural communities. 15 , 16 Such relationships might also build a stronger rationale for people living in rural areas to engage in environmental stewardship activities, such as a tree planting or riparian restoration, with potential benefits to social capital, 11 land quality, water quality and biodiversity. 17
In this systematic review, we examine quantitative evidence for whether there is a relationship between diverse environmental factors and mental health or well‐being in rural communities. We defined environmental factors as including the impacts of land use, green space/vegetation, engagement in natural resource management activities, biodiversity, and natural or man‐made disasters (including drought, climate change, human‐caused environmental degradation) based on the World Health Organization Disaster taxonomy. 18 While there is extensive literature on the impacts of shorter‐term disasters on trauma response, this literature is largely focused on trauma, loss and grief related to the disaster event rather than its environmental effects. 18 The mental health focus included general psychological distress, symptoms of common mental disorders (anxiety disorders, depression), suicidality, self‐harm and psychological well‐being; however, studies that examined the trauma of specific events were excluded. Given the diversity of definitions used for rurality, we included studies of non‐urban settings (ie remote areas, rural areas, or regional/semi‐urban centres within rural areas), or where separate analyses were reported for urban and non‐urban settings.
2. METHOD
2.1. Search strategy
We searched MEDLINE, PsycINFO and Web of Science databases for relevant articles from inception until the end of March 2021, based on title, abstract and key words. Search terms were used to identify studies with a rural focus that included environmental and mental health key words. The search string used was as follows: (rural or farm*) and (environm* or natur* or drought or land degradation or climate change or land conservation or biodiversity) and (mental health or depress* or anx* or wellbeing or distress or suicid*). We included studies that were conducted in rural or regional (non‐city) areas, or where separate data were reported for rural/regional areas. The studies needed to include one or more quantitative indicators related to environment and an outcome directly relevant to mental health or psychological well‐being. Studies were excluded if they were purely qualitative, not published in English, not published in a peer‐reviewed journal or did not present new data (eg review, editorial, commentary). Studies that focused exclusively on traumatic stress related to a natural disaster were also excluded. We also hand‐searched reference lists and citations of identified studies to identify additional eligible papers missed in the database searches. We follow PRISMA guidelines in reporting the methodology and outcomes of the review. The review was not registered. All data extracted are presented in this paper.
2.2. Procedure and coding strategy
CP and AT conducted searches of the databases and refined search terms in discussion with PB and AC. After removing duplicate records, CP, DK, AT and KB screened 4368 abstracts to determine whether papers met the inclusion criteria. This process resulted in 4095 abstracts being excluded, leaving 273 papers for full coding. The full‐text papers were obtained, and a pro forma coding sheet was developed to systematically collect key information from each paper. The sheet collected information about study eligibility (reasons for inclusion/exclusion), year, country of study, aim, design, mental health outcomes, types of environmental variables, participant characteristics (sample size, specific age/occupation group of population, age, sex), setting of study and summary of outcomes. Dual coding was conducted for all full‐text papers, with CP, DK, PB, AC and KB contributing to this coding process. Discrepancies in coding were resolved by consensus. Risk of bias was assessed using the Joanna Briggs Institute Critical Appraisal Checklist for Analytical Cross‐Sectional Studies. 19 The full‐text coding process identified 245 papers that did not meet eligibility criteria, leaving 28 papers included in the review (Figure 1).
FIGURE 1.
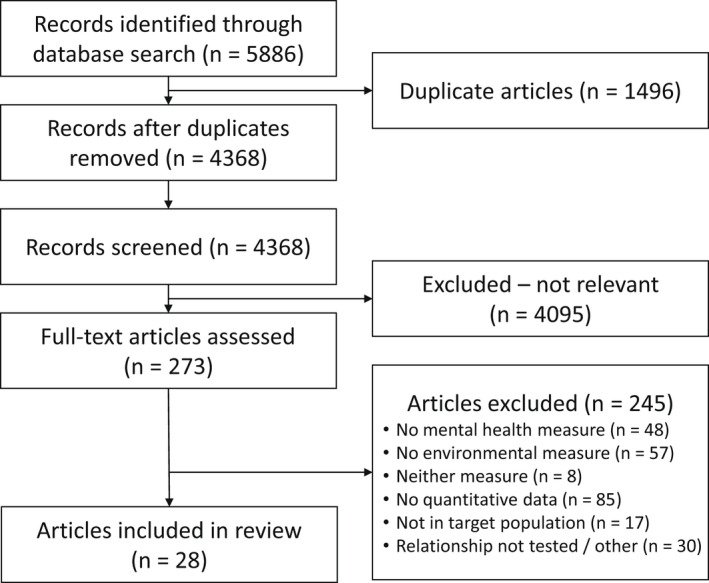
PRISMA diagram of the review procedure
3. RESULTS
The characteristics of the 28 studies are provided in Table 1. Most (n = 17, 61%) of the studies were conducted in Australia, with 4 (14%) conducted in Europe, 3 (11%) in the USA and 3 (11%) in Asia. Notably, all of the studies have been conducted in the past 15 years. Sample sizes varied considerably, as there were 9 studies with n < 400 and 3 whole‐of‐population ecological studies, where the unit of analysis was at the community rather than at the individual level. Excluding population‐scale ecological studies, the mean sample size was n = 3915 (SD = 7037, median = 1284). Among the 11 studies where mean age was reported, the mean age was 49.8 years (SD = 3.6). Among the 16 studies where sex was reported for the full sample, women constituted on average 49.3% of participants.
TABLE 1.
Summary of study characteristics
| Author | Year | Country of study | Setting/ design | Rurality description | Sample size | Participant details | Mean age (SD) | Sex | Mental health measures | Environmental measures |
|---|---|---|---|---|---|---|---|---|---|---|
| Studies of green space | ||||||||||
| Akpinar, Barbosa‐Leiker 38 | 2016 | USA | Explore specific types of green spaces associated with mental and general health using data from Behavioral Risk Factor Surveillance System Survey and National Land Cover Data | State with a variety of eco‐zones (heavily forested, shrubland, grassland and both irrigated and dryland agriculture) | N = 5148 | Residents of Washington State | 52.40 | Male 39.2%; Female 60.8% | Mental health complaints (last 30 d); anxiety‐depression complaints (last 14 d) | Percentage of green space type by ZIP code |
| Alcock, White 41 | 2015 | England | Examine relationships between types of green space and mental health using data from 18‐y longitudinal British Household Panel Survey linked with Land Cover Map (LCM) | Rural residential areas | N = 2020 (12 697obs) | Residents in English rural neighbourhoods | 47.59 | Female 52.4% | GHQ‐12; 2‐item second standard scoring method | 10 aggregate land cover classes in the LCM2007 |
| Losert, Schmauss 39 | 2012 | Germany | Test environmental risk factors for mental illness in rural catchment area | Rural municipalities | N = 4198 | Psychiatric patients living in study region | NA | NA | Hospital admission data for schizophrenia and affective disorders from 2006 to 2009 | Data on proportion of forest and agricultural areas |
| Nishigaki, Hanazato 40 | 2020 | Japan | Examine relationship between green space and depression among older adults living in rural (and urban) areas | Rural municipalities, nationwide | N = 33 823 | Older adults (age 65+) living in the community | NA | NA for rural sample (full sample: female 51.5%) | Geriatric Depression Scale (GDS) | Total green space, grass, tree and field ratios (tertiles) from satellite imagery, at the school district level |
| Studies of drought | ||||||||||
| Austin, Handley 28 | 2018 | Australia | Examine drought‐related stress using data from longitudinal cohort study—Australian Rural Mental Health Study (ARMHS) | Non‐metropolitan New South Wales | N = 664 | Living or working on a farm | 55‐64 27.7% | Male 43.7%; Female 56.3% | K10; personal and community drought‐related stress | Drought conditions by comparing rainfall during prior 12 mo |
| Brew, Inder 26 | 2016 | Australia | Determine whether farming is associated with poorer health using data from ARMHS study | Non‐metropolitan New South Wales | N = 1284 | Farmers and non‐farming workers (other rural workers and farm residents employed elsewhere) | 48.3 (11.9) | Female 57% | K10; PHQ‐9; item on self‐report overall mental health | Remoteness of location of residence (ARIA+); item on drought stress |
| Edwards, Gray 21 | 2015 | Australia | Impact of drought on mental health using data from stratified random Rural and Regional Family Survey | Rural and regional ‐ agricultural | N = 8000 | Adults living in agricultural areas | 46.5 (10.91) | Female 54.2% | 5‐item Mental Health Inventory Form SF‐36 | Area‐based self‐report drought measure |
| Friel, Berry 45 | 2014 | Australia | Association between drought exposure, food insecurity and mental health using data from longitudinal study Household, Income and Labour Dynamics in Australia (HILDA) Survey | Rural and urban | N = 5012 | Wave 7 survey participants aged 15+ | NA | NA | K10 | Monthly rainfall data from Australian Bureau of Meteorology |
| Guiney 29 | 2012 | Australia | Examination of farming suicides during prolonged drought based on reports to State Coroner | NA | N = 110 | Farmers and primary producers in Victoria | 40‐49 22% | Male nearly 95% | Intentional self‐harm fatalities data obtained from National Coroners Information System for 7‐y period | NA |
| Gunn, Kettler 22 | 2012 | Australia | Examination of psychological distress and coping in drought‐affected area | Rural farming | N = 309 | Farmers or spouses of farmers in South Australia | 51.81 (11.69) | Male 63.4%; Female 34.6% | K10 | NA |
| Hanigan, Butler 30 | 2012 | Australia | Investigation of suicide in rural populations with a previously established climatic drought index | Rural and urban regions of New South Wales (NSW) | NA | Residents of 11 regions in NSW | NA | NA | Data on suicides 1970‐2007 | Hutchinson Drought Index |
| Hanigan, Schirmer 23 | 2018 | Australia | Association between drought and distress using survey questionnaire | Rural area | N = 5312 | Residents of Victoria—farmers and non‐farmers | NA | Male 41.5%; female 57.7% | K10 | Hutchinson Drought Severity Index |
| Kelly, Lewin 27 | 2011 | Australia | Individual and contextual factors influencing mental health within rural communities using data baseline sample from ARMHS | Non‐metropolitan regions of New South Wales | N = 2462 | Residents aged 18‐65 | 55.6 (14.5) | Female 59% | K10 | Data on drought severity and remoteness (ARIA+and ASGC) |
| Mann, Freyens 43 | 2016 | Australia | Impact of natural and economic crises on structural change in farming sector using data from Australian Regional Well‐being Survey | Rural and regional | N = 2492 | Dryland farmers and irrigators | NA | NA | 1 item on happiness (in the last 4 weeks) | 1 item each on drought and other natural disaster (over the last 5 y) |
| O'Brien, Berry 24 | 2014 | Australia | Quantitatively identify association between patterns of drought and mental health using HILDA Survey and rainfall data from Australian Bureau of Meteorology | Rural and urban | N = 5012 | People aged 15+ | 40‐55—rural 33.04 (0.02), urban 31.38 (0.01) | Male—rural 51.62 (0.01), urban 47.28 (0.01) | K10 | Drought patterns for 2001‐2008 |
| Parida, Dash 31 | 2018 | India | Examine the effects of drought and flood on farmer suicides using state‐level panel data for 1995‐2011 | Agricultural | NA | Residents of 17 Indian states | NA | NA | Suicide data from annual report from National Crime Record Bureau | Flood data from Dartmouth Flood Observatory; Drought data from Department of Land Resources |
| Stain, Kelly 44 | 2011 | Australia | Examine factors associated with drought impact | Rural and remote | N = 302 | Randomly selected residents of NSW aged 18+ | 53 | Female 57% | K10; Worry about Drought Scale | Drought status |
| Wheeler, Zuo 25 | 2018 | Australia | Large‐scale assessment of Murray‐Darling Basin irrigators’ mental health | Irrigation districts | N = 1000 | irrigators | NA | NA | K10 | Items on drought, water availability |
| Studies of land degradation | ||||||||||
| Canu, Jameson 36 | 2017 | USA | Examine relative risk for mental health diagnoses in areas with mountaintop removal (MTR) using data from State Emergency Department Database | Residential area | N = 1 380 394 | Kentucky State ED outpatients in a calendar year aged 18+ | 42.2 (18.19) | Female 58.1% | Rates of emergency department diagnosis for depressive disorders, substance use disorders and anxiety disorders in 2008 | ZIP code to determine active MTR area and rural status |
| Kallioniemi, Simola 46 | 2016 | Finland | Stress among Finnish dairy farmers using cross‐sectional survey | Dairy farms | N = 265 | Finnish dairy farmers | 47.8 (10.35) | Men 56%; female 44% | MBI‐GS | Items on work and living environment resources |
| Morgan, Hine 47 | 2016 | Australia | Examine contribution of coal seam gas (CSG) extraction to global stress burden and mental health of farmers | NA | N = 378 | Farmers or their partners | 53.08 (10.28) | Male 50.5%; female 49%; other 0.5% | DASS‐21 | Items on farm stress, that is weather, CSG concerns; engagement with CSG industry |
| Speldewinde, Cook 37 | 2009 | Australia | Examine the effects of environmental degradation (dryland salinity) on mental health | Dryland agricultural areas | N = 2669 | Residents of southwest Western Australia | 20‐39 42% | Male 38%; Female 62% | Hospital cases (1st admission) for depression | Soil and landscape mapping as a measure of dryland salinity |
| Studies of climate conditions and extreme weather | ||||||||||
| Daghagh Yazd, Wheeler 32 | 2020 | Australia | Longitudinal examination of whether area‐level climatic conditions and water scarcity were associated with poorer mental health for farmers | Rural areas | N = 235 | Active farmers living in the Murray–Darling Basin region of Australia | 49.7 (16.2) | Female 35%; Male 65% | MHI‐5 subscale | Water scarcity (measured through decreased rainy days; drought period; increased summer temperatures; reduced water allocations; lower soil moisture) |
| Howard, Ahmed 33 | 2020 | USA | Impact of perception of climate change on mental health among rural agricultural populations using cross‐sectional survey | Rural agricultural | N = 125 | Farmers and ranchers aged 18+ from Montana | 35‐54 49.2% | Mostly male | Modified GAD‐7; PHQ‐9 | 3 items from Climate Change in the American Mind; 4 items from Climate Harm Scale |
| Pailler and Tsaneva 34 | 2018 | India | Test effects of extreme weather and precipitation on psychological well‐being using data from World Health Survey (WHS) and Study on Global AGEing and Adult Health (SAGE) | Rural and urban | N = 16 227 | Adults aged 18‐60 | NA | Female—WHS 52%, SAGE 68% | Items on depression symptoms | Climate data using GPS coordinates—average monthly temperature and total monthly precipitation |
| Wind, Joshi 35 | 2013 | India | Examine immediate impact of recurrent flood on mental health | Rural district | N = 615 | Affected population in Bahraich, Uttar Pradesh, compared with non‐affected group in the same region | Affected 46.03 (15.74); non‐affected 47.23 (13.92) | Affected—male 61%, female 39%; non‐affected male 54.9%, female 44.1% | HSCL‐25; SF‐12 | NA |
| Studies of engagement in natural resource management activities | ||||||||||
| Hounsome, Edwards 42 | 2006 | Wales | Exploration of farmer health as a variable in adoption of agri‐environment schemes | Farm households | N = 111 | Farmers | NA | NA | SF‐36 | Involvement in agri‐environment schemes |
| Moore, Kesten 5 | 2018 | Australia | Explore benefits gained by involvement in management of land for conservation using mixed methods | Rural regions in Victoria | N = 102 | Members of community‐based land management group and controls matched by age and sex | 45‐64 nearly 50% | Male 63%; female 37% | 1 item feel anxious; 1 item feel depressed | NA |
Abbreviations: ARMHS, Australian Rural Mental Health Study; DASS‐21, 21‐item Depression Anxiety and Stress Scale; ED, emergency department; GAD‐7, 7‐item Generalized Anxiety Disorder; GDS, Geriatric Depression Scale; GHQ‐12, 12‐item General Health Questionnaire; HILDA, Household; HSCL‐25, 25‐item Hopkins Symptom Checklist; Income and Labour Dynamics in Australia; K10, Kessler‐10 Distress Scale; MBI‐GS, Maslach Burnout Inventory—General Survey; MHI‐5, 5‐item Mental Health Inventory; NA, not applicable; PHQ‐9, 9‐item Patient Health Questionnaire; SF‐12, 12‐item Short‐Form Health Survey; SF‐36, 36‐item Short‐Form Health Survey.
Assessment of mental health used a range of measures and approaches. The Kessler‐10 20 measure of general psychological distress was most commonly used, in 9 (33%) studies. Including the 9 studies that used the K10, there were 18 (64%) that used a validated self‐report scale assessing mental health (eg PHQ‐9, DASS‐21, GDS). Six studies (21%) used administrative data on hospital admissions or suicide deaths. The remaining 4 studies used non‐validated items to assess depression, anxiety or well‐being (eg single items assessing current depression or happiness). Study characteristics associated with risk of bias are summarised in Table 2. Overall, study quality was good, with most (n = 24, 86%) studies receiving a score of 6 or higher and a mean quality rating of 6.6 (SD = 1.4).
TABLE 2.
Risk‐of‐bias assessment
| Inclusion criteria | Participants/settings detailed | Valid reliable measure of exposure | Objective criteria to measure MH | Confounding factors identified | Strategies to handle confounding | Valid reliable outcome measures | Appropriate stat analysis | Total criteria met | |
|---|---|---|---|---|---|---|---|---|---|
| Akpinar et al (2016) | Y | Y | Y | Y | Y | Y | U | Y | 7 |
| Alcock et al (2015) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Austin et al (2018) | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Brew et al (2016) | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Canu et al (2017) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Daghagh Yazd et al (2020) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Edwards & Hunter (2015) | Y | Y | U | Y | Y | U | Y | Y | 6 |
| Friel et al (2014) | Y | U | U | Y | Y | Y | Y | Y | 6 |
| Guiney et al (2012) | Y | Y | U | Y | N | N | Y | U | 4 |
| Gunn et al (2012) | Y | Y | U | Y | Y | U | Y | Y | 6 |
| Hanigan et al (2012) | Y | Y | Y | Y | U | U | Y | Y | 6 |
| Hanigan et al (2018) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Hounsome et al (2006) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Howard et al (2020) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Kallioniemi et al (2016) | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Kelly et al (2011) | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Losert et al (2012) | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Mann et al (2017) | U | U | U | U | Y | Y | U | Y | 3 |
| Moore et al (2006) | Y | Y | Y | U | Y | U | U | U | 4 |
| Morgan et al (2016) | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Nishigaki et al (2020) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| OBrien et al (2014) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Pailler (2018) | Y | Y | Y | U | Y | Y | U | Y | 6 |
| Parida et al (2018) | Y | U | Y | Y | U | Y | Y | Y | 6 |
| Speldewinde et al (2009) | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Stain et al (2011) | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Wheeler et al (2018) | U | Y | U | Y | Y | U | Y | U | 4 |
| Wind et al (2013) | Y | Y | Y | Y | Y | U | Y | U | 6 |
Abbreviations: MH, mental health; stat, statistical; U, unclear; Y, yes.
Outcomes for each study are described in Table 3. The primary environmental characteristic assessed was drought in 14 (50%) studies, typically assessed at the area level based on drought indices. Most of these studies found significant impacts of drought on mental health, with many 21 , 22 , 23 , 24 , 25 but not all 26 , 27 studies reporting increased psychological distress in drought‐affected areas, which might persist beyond the drought period. 28 For example, drought was associated with a decrease of 0.4 standard deviations on the SF‐36 mental health index for Australian farmers and farm workers (P < .01), and a doubling in the odds of mental health problems for farm workers (P < .01). However, the effects of drought on suicides were mixed and largely non‐significant. 29 , 30 , 31 Four studies (14%) primarily examined indicators of climate change (typically self‐reported) or extreme weather events (recurrent flooding, high temperatures). In each of these studies, climate change or extreme weather all had significant negative effects on mental health, well‐being or functioning. 32 , 33 , 34 , 35 For example, Howard et al 33 found moderate correlations between perceived climate harms with anxiety (r = .61, P < .001) and distress (r = .43, P < .001) among farmers in the USA.
TABLE 3.
Summary of study findings
| Study—author (year) | Summary of outcomes |
|---|---|
| Studies of green space | |
| Akpinar et al (2016) | No significant associations between aggregated green space and mental and general health. Greater percentages of forest and more urban green space were associated with fewer days of mental health complaints, but not for agricultural lands |
| Alcock et al (2015) | Natural space in rural areas was positively related to good mental health when estimated from within‐individual differences. There is some evidence that different types of green and other natural space offer different degrees of benefit to well‐being |
| Losert et al (2012) | Hospital admission rates due to affective disorders decreased with an increase in percentage of total space covered by forest |
| Nishigaki et al (2020) | The middle tertile of grassland area ratio was associated with significantly lower levels of depression in older adults. The highest tertile of grassland ratio had no significant benefit. In addition, area ratios of total green space, trees and fields had no association with depression |
| Studies of drought | |
| Austin et al (2018) | Moderately dry, mild dry and moderately wet conditions were related to higher incidence of community drought‐related stress (CDS). Mild wet conditions were associated with greater incidence of psychological distress, personal drought‐related stress and CDS, suggesting drought‐related stress persists beyond the end of the drought |
| Brew et al (2016) | Farmers who lived more remotely had poorer self‐reported mental health than non‐farm workers living remotely and that this was not mediated by rural specific factors or vulnerabilities. Drought stress did not impact directly on mental health outcomes |
| Edwards & Hunter (2015) | Farmers had a higher rate of mental health problems and a lower level of mental health well‐being than those in non‐agricultural employment. Living in a drought‐affected area was estimated to significantly reduce mental health for farmers and farm workers |
| Friel et al (2014) | Drought mediated the association between food intake and mental health in rural areas |
| Guiney et al (2012) | No trend of increasing numbers of suicides coinciding with prolonged drought conditions |
| Gunn et al (2012) | Farmers or spouses of farmers in drought‐affected areas displayed significantly higher levels of distress than the broader national and rural populations |
| Hanigan et al (2012) | Drought increased the suicide rates for men aged 30‐49 (likely farmers or farmworkers) in rural communities. However, the risk for rural women aged >30 fell |
| Hanigan et al (2018) | All subgroups that were in drought had slightly higher average distress levels compared with those not in drought. Drought was estimated to have a negative impact on mental health in younger women but not in older women or men, and this pattern did not differ by farming status |
| Kelly et al (2011) | District‐level impacts, including severity of drought, on mental health were not evident in a rural sample |
| Mann et al (2017) | Crises, such as drought, reduced both profitability of farms and happiness of farmers, and both these factors reduced the likelihood of continuing the farming business |
| OBrien et al (2014) | Extreme dryness occurring within a drought itself affects mental health: drought was associated with increased distress in rural areas, while no consistent effects for drought were found in urban areas |
| Parida et al (2018) | Frequent occurrence of drought significantly increased farmer suicide due to crop failure. However, flood had almost no direct impact on the occurrence of farmer suicides. Incidence of farmer suicides was higher in cotton‐producing states as they experienced frequent drought conditions |
| Stain et al (2011) | Levels of psychological distress and drought worry were associated with factors reflecting the pragmatic impact of drought and environmental adversity on livelihood. Greatest psychological distress was associated with individual vulnerability factors and attenuation of community and social connectedness |
| Wheeler et al (2018) | Land–water use and drought were associated with psychological distress: some irrigators had higher levels of distress than dryland farmers or the Australian population, while horticulturists reported the highest levels of distress. Financial worry was the most important day‐to‐day stress for irrigators, but the results emphasise the integral nature of drought and water availability pressures |
| Studies of land degradation | |
| Canu et al (2017) | Emergency department visits by residents of areas with active mountaintop removal sites would be more likely to involve a psychological disorder, that is depressive disorder and substance use disorder |
| Kallioniemi et al (2016) | All dairy farmers were classified as having slight burnout symptoms. Work and living environment (including resource variables such as ‘work near nature’ ‘living environment’ and ‘farming lifestyle’) as a summary factor reduced the probability of burnout |
| Morgan et al (2016) | Potential coal seam gas (CSG) extraction impacted on health, community and the environment was a source of concern for farmers, and was significantly associated with increased symptoms of depression and stress reactivity |
| Speldewinde et al (2009) | An elevated risk of hospitalisations for depression was associated with residence in areas more affected by dryland salinity |
| Studies of climate conditions and extreme weather | |
| Daghagh Yadz et al (2020) | Farmer mental health was poorer if they were located in an area that had experienced reduced rainfall, markedly reduced water allocations and high mean daily maximum summer temperatures. These effects appeared to be moderated by reduced income, with lower income during drought having a considerable impact on worse mental health |
| Howard et al (2020) | Perceptions of climate risk and harm correlate positively with increased levels of both anxiety and distress. Organic farmers reported higher levels of anxiety than conventional farmers, and fruit/vegetable farmers reported higher levels of anxiety than grain/legume farmers |
| Pailler (2018) | Higher temperatures had a significant negative effect on psychological well‐being in rural, but not urban, areas. Controlling for precipitation, hot weather had a significant effect on increased depression symptoms. The adverse effects of extreme temperatures are partly due to reductions in agricultural output, which in turn reduce income and consumption |
| Wind et al (2013) | Recurrent flood‐affected group scored significantly higher on scales of anxiety and depression. They also scored significantly lower on the mental health component as an indicator of functioning |
| Studies of engagement in natural resource management activities | |
| Hounsome et al (2006) | Adoption of agri‐environment schemes by farmers was likely to be affected by their age, the size (effective area) of the farm and their health. Better mental health appears to improve the odds of farmers’ adoption |
| Moore et al (2006) | Members of land management groups reported that they experienced higher levels of anxiety and the same degree of depression as controls. However, members (especially men and those in older age groups) reported experiencing higher levels of health and well‐being |
Four studies (14%) examined effects of various forms of land degradation (mountaintop removal, salinity, environmental resources, local coal seam gas activity). All 4 of these studies reported significant associations with mental health outcomes, including 2 studies 36 , 37 that reported increases in emergency department visits and hospitalisations for depression and substance use disorders. Finally, 4 studies (14%) examined green space or vegetation cover and 2 (7%) measured engagement in natural resource management activities. The findings for these studies were mixed, with evidence that areas with greater green space might have higher well‐being, marginally less depression and reduced hospitalisations 38 , 39 , 40 but indications that the effects of green space on mental health might be modest for agricultural areas. 41 Engagement in natural resource management appeared to have little impact on mental health, with those engaging in activities more likely to experience anxiety, 5 while in contrast, those with better mental health were more likely to adopt change in agricultural practice. 42
Mediators of the relationship between environment and mental health were also examined in some of the studies. Several of these noted that impacts of environment (drought or degradation) on mental health were moderated by finances such as farm income, with financial strain or worry in combination with environmental factors leading to poorer mental health outcomes. 25 , 32 , 43 , 44 Studies also suggested that effects might be partially explained by changes in social capital that arise from land management activities or disasters including drought. 43 , 44
4. DISCUSSION
This systematic review identified 28 articles, mostly of high methodological quality, testing quantitative relationships between environmental factors and mental health or well‐being in rural areas. Studies typically found high levels of mental ill health among people living in rural areas. Poorer mental health typically had a relationship with extreme climate or weather events. However, the effects appeared to be more pronounced when using area‐level indicators of mental health and environment, such as hospital admissions related to mental health problems and whether the region was declared as drought‐affected. At the individual level, such relationships were not always observed, which suggests that individual responses to drought might vary and be mediated by factors such as impact on finances and social connections. Environmental degradation such as mountaintop removal, local coal seam gas extraction activity and salinity also appeared to have a negative impact on mental health at the community level.
Only 2 studies were identified that examined the effects of natural resource management on agricultural land with a focus on environmental impacts. 5 , 42 These studies collectively suggest that having greater well‐being improves the likelihood of engaging in such activity, with limited evidence that engaging in environmental activities has a direct effect on mental health. Indeed, those who engaged in such activities tended to have greater anxiety than those who did not, which might suggest that anxiety about environmental change might be a motivating factor for engaging in environmental stewardship. Despite having greater anxiety symptoms, those farmers who did engage also reported greater well‐being. Relationships between natural resource management, farm resilience, financial productivity and farmer well‐being are likely to be highly complex and warrant further investigation.
There were no quantitative studies that assessed associations between the environmental condition of small geospatial areas (eg individual farms) and mental health, and no studies that investigated the impact of biodiversity on mental health within farms or local regions. While area‐level factors might be informative, considerable variability in natural resource management is likely to influence the resilience of specific land holdings to threats such as drought, climate change and biodiversity loss. For example, farms that are managed to be more resilient to these threats might be more productive during harsh periods, leading to less impact on the well‐being of farmers. The lack of studies examining local indicators might reflect the challenges of collecting both objective ecological data and mental health data, which require interdisciplinary expertise and diverse methodologies. Furthermore, there was a strong focus in the literature on farms, with less focus on rural residents employed in mining, transport, finance and other sectors represented in the rural economy. Data at multiple levels of measurement are needed to disentangle community‐level effects from individual‐level effects of the physical environment on mental health. While there have been several studies examining the relationship between biodiversity and well‐being, 12 none of these has focused on rural areas specifically, and obtaining local and objective markers of species richness and contact with nature remain distinct challenges. 12 The lack of studies on the effects of green space on rural mental health in Australia is also a conspicuous absence.
Furthermore, all but one of the papers 32 reported on observational cross‐sectional research, which limits understanding of causal pathways and directionality of effects. These relationships are likely to be complex and dynamic, as the mental health of people living in rural areas will influence their ability to engage in practices aimed at addressing environmental degradation and climate change. Conversely, climate change‐related weather events and degraded land are likely to influence mental health. Longitudinal data might be better suited to understanding the mechanisms by which mental health is influenced by the environment in rural areas. In addition, understanding what aspects of mental health and well‐being are most influenced by the environment is an important empirical question. Although some studies found differential relationships between environmental factors with depression vs anxiety symptoms, 5 , 36 most studies used measures of general psychological distress that preclude investigation of specific mental health conditions. Future studies would benefit from greater consistency in the use of validated measures of mental health, well‐being, and environmental exposures. While we did not review studies that were exclusively qualitative, it is likely that the use of qualitative and mixed‐methods research would enhance our understanding of the mechanisms underlying the observed associations. The lack of studies with longitudinal designs is a critical gap in the literature, and explorations of the joint impacts of individual‐ and community‐level exposures are limited. Another gap is the lack of studies with a focus on specific population groups, such as Indigenous people or young people.
There were several limitations of this review. We restricted articles to English language and limited our search to databases where mental health and well‐being were most likely to be reported as outcomes. The choice of search terms might have influenced the outcomes, with many studies specifically examining drought and often in the Australian context, which might reflect a particular interest of Australian researchers. While our search strategy was inclusive of many terms related to mental health and environment, and included searching reference lists of included articles, we might have missed some relevant studies. Terms used to describe mental health might be diverse. While we aimed to capture the most common terms used in previous research, broader challenges related to factors such as functioning might have been excluded from the review. We also excluded qualitative studies, of which there were several that might provide insights into the mechanisms by which the environment influences mental health for some individuals. It is likely that effects are not consistent at the population level—that is, for some people in rural areas, the environment is pivotal to their mental health and well‐being, while for other people in rural areas, it has minimal relevance. Quantitative studies might be somewhat limited in their ability to capture this variability, although methods that investigate subgroups are to be encouraged.
Although the quality of studies was generally high, as noted above nearly all of the studies reported on cross‐sectional or retrospective associations, so causation or direction of effects cannot be assumed. Further prospective research would enhance the understanding of the causal pathways into mental ill health in rural areas. Finally, the diversity of studies was not conducive to formal data aggregation methods such as meta‐analysis, so our review resulted in a narrative synthesis. The diversity of study designs, exposures, settings and outcome measures incorporated in the review also precluded standardised indicators of effect. Although some clear themes emerged from the review, it remains possible that findings from high‐income nations might not be comparable with findings from low‐ and middle‐income countries, and environmental impacts in remote settings might differ to those in semi‐urban, regional settings. Comparators also varied, with a mixture of studies comparing rural areas in drought to those not in drought (or other environmental exposure), studies comparing rural to urban or national data, studies examining environmental exposures as a continuum, and studies conducting multiple comparisons. Finally, it should be noted that some data sets might have been used in multiple studies as noted in Table 1, suggesting that the volume of research on this topic might be less than it appears.
In conclusion, extreme climate or weather events and environmental degradation appear to have a negative effect on mental health and well‐being of people living in affected rural communities. However, whether these effects are observed after accounting for local area‐level differences remains to be investigated. Findings are largely consistent with previous reviews that have not focused specifically on rural areas, particularly with regard to mixed findings around green space 8 and negative effects of climate change and extreme weather on mental health. 6 , 7 However, many of the identified studies in the present review examine environmental exposures that are most salient in rural areas. People living in rural areas who are impacted by drought, extreme weather events or man‐made degradation are likely to be at increased risk of experiencing mental ill health. Social and health services might need to consider these impacts in the assessment, prevention and treatment of mental health problems in rural areas and in the promotion of mental well‐being. Services might be targeted to those in the most impacted areas during periods of extended environmental crisis, with providers being aware of the possible impacts of environmental change on their rural clients. The impacts of reduced biodiversity and exposure to high‐quality natural areas on mental health have received little attention in rural areas, and few studies have quantified the impacts of specific indicators of natural resource management. Such investigations would benefit from longitudinal data using objective indicators of both environmental factors and mental health outcomes, which requires well‐resourced large‐scale research with strong interdisciplinary expertise. As climate change and associated natural degradation have increasing impacts on the rural landscape, it is important to rigorously evaluate how these changes might influence human health.
AUTHOR CONTRIBUTIONS
PB: conceptualization; data curation; funding acquisition; investigation; methodology; project administration; resources; supervision; writing – original draft; writing – review & editing. KB: conceptualization; data curation; investigation; writing – review & editing. AT: data curation; writing – review & editing. CP: data curation; investigation; writing – review & editing. DK: data curation; investigation; writing – review & editing. ALC: conceptualization; data curation; investigation; methodology; supervision; writing – review & editing.
ACKNOWLEDGEMENTS
This research was supported by funding from the Ian Potter Foundation. PJB and ALC are supported by NHMRC Fellowships 1158707 and 1173146, respectively. Open access publishing facilitated by Australian National University, as part of the Wiley ‐ Australian National University agreement via the Council of Australian University Librarians.
Batterham PJ, Brown K, Trias A, Poyser C, Kazan D, Calear AL. Systematic review of quantitative studies assessing the relationship between environment and mental health in rural areas. Aust J Rural Health. 2022;30:306‐320. doi: 10.1111/ajr.12851
REFERENCES
- 1. Persiani SGL, Kobas B, Koth SC, Auer T. Biometric data as real‐time measure of physiological reactions to environmental stimuli in the built environment. Energies. 2021;14(1):232. [Google Scholar]
- 2. Evans GW. The built environment and mental health. J Urban Health. 2003;80(4):536‐555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hinckson E, Cerin E, Mavoa S, et al. Associations of the perceived and objective neighborhood environment with physical activity and sedentary time in New Zealand adolescents. Int J Behav Nutr Phys Act. 2017;14(1):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clark C, Myron R, Stansfeld S, Candy B. A systematic review of the evidence on the effect of the built and physical environment on mental health. J Public Ment Health. 2007;6(2):14‐27. [Google Scholar]
- 5. Moore THM, Kesten JM, López‐López JA, et al. The effects of changes to the built environment on the mental health and well‐being of adults: systematic review. Health Place. 2018;53:237‐257. [DOI] [PubMed] [Google Scholar]
- 6. Cianconi P, Betrò S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Front Psychiatry. 2020;11:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smith KR, Woodward A, Campbell‐Lendrum D, et al., et al. Human health: impacts, adaptation, and co‐benefits. In: Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, eds. Climate Change 2014: Impacts, Adaptation, and Vulnerability Part A: Global and Sectoral Aspects Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press; 2014:709‐754. [Google Scholar]
- 8. Gascon M, Triguero‐Mas M, Martínez D, et al. Mental health benefits of long‐term exposure to residential green and blue spaces: a systematic review. Int J Environ Res Public Health. 2015;12(4):4354‐4379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vins H, Bell J, Saha S, Hess JJ. The mental health outcomes of drought: a systematic review and causal process diagram. Int J Environ Res Public Health. 2015;12(10):13251‐13275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Daghagh Yazd S, Wheeler SA, Zuo A. Key risk factors affecting farmers’ mental health: a systematic review. Int J Environ Res Public Health. 2019;16(23):4849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schirmer J, Berry HL, O’Brien LV. Healthier land, healthier farmers: considering the potential of natural resource management as a place‐focused farmer health intervention. Health Place. 2013;24:97‐109. [DOI] [PubMed] [Google Scholar]
- 12. Marselle M, Martens D, Dallimer M, Irvine K. Review of the mental health and well‐being benefits of biodiversity. In: Marselle M, Stadler J, Korn H, Irvine K, Bonn A, eds. Biodiversity and Health in the Face of Climate Change. Springer Open; 2019:175‐211. [Google Scholar]
- 13. Berenguer J, Corraliza JA, Martín R. Rural‐urban differences in environmental concern, attitudes, and actions. Eur J Psychol Assess. 2005;21(2):128‐138. [Google Scholar]
- 14. Ahnström J, Höckert J, Bergeå HL, Francis CA, Skelton P, Hallgren L. Farmers and nature conservation: what is known about attitudes, context factors and actions affecting conservation? Renewable Agric Food Syst. 2009;24(1):38‐47. [Google Scholar]
- 15. Thompson S, Kent J. Connecting and strengthening communities in places for health and well‐being. Aust Plan. 2014;51(3):260‐271. [Google Scholar]
- 16. Winterton R, Hulme Chambers A, Farmer J, Munoz S‐A. Considering the implications of place‐based approaches for improving rural community wellbeing: the value of a relational lens. Rural Soc. 2014;23(3):283‐295. [Google Scholar]
- 17. Lindenmayer D, Crane M, Florance D. Restoring Farm Woodlands for Wildlife. CSIRO Publishing; 2018:122. [Google Scholar]
- 18. de Girolamo G, McFarlane AC. The epidemiology of PTSD: A comprehensive review of the international literature. Ethnocultural aspects of posttraumatic stress disorder: Issues, research, and clinical applications. American Psychological Association; 1996:33‐85. [Google Scholar]
- 19. Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. Joanna Briggs Institute; 2020. https://synthesismanual.jbi.global [Google Scholar]
- 20. Andrews G, Slade T. Interpreting scores on the Kessler psychological distress scale (K10). Aust N Z J Public Health. 2001;25(6):494‐497. [DOI] [PubMed] [Google Scholar]
- 21. Edwards B, Gray M, Hunter B. The impact of drought on mental health in rural and regional Australia. Soc Indic Res. 2015;121(1):177‐194. [Google Scholar]
- 22. Gunn K, Kettler L, Skaczkowski G, Turnbull D. Farmers’ stress and coping in a time of drought. Rural Remote Health. 2012;12:2071. [PubMed] [Google Scholar]
- 23. Hanigan IC, Schirmer J, Niyonsenga T. Drought and distress in Southeastern Australia. EcoHealth. 2018;15(3):642‐655. [DOI] [PubMed] [Google Scholar]
- 24. O'Brien LV, Berry HL, Coleman C, Hanigan IC. Drought as a mental health exposure. Environ Res. 2014;131:181‐187. [DOI] [PubMed] [Google Scholar]
- 25. Wheeler SA, Zuo A, Loch A. Water torture: unravelling the psychological distress of irrigators in Australia. J Rural Stud. 2018;62:183‐194. [Google Scholar]
- 26. Brew B, Inder K, Allen J, Thomas M, Kelly B. The health and wellbeing of Australian farmers: a longitudinal cohort study. BMC Public Health. 2016;16:988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kelly BJ, Lewin TJ, Stain HJ, et al. Determinants of mental health and well‐being within rural and remote communities. Soc Psychiatry Psychiatr Epidemiol. 2011;46(12):1331‐1342. [DOI] [PubMed] [Google Scholar]
- 28. Austin EK, Handley T, Kiem AS, et al. Drought‐related stress among farmers: findings from the Australian Rural Mental Health Study. Med J Aust. 2018;209(4):159‐165. [DOI] [PubMed] [Google Scholar]
- 29. Guiney R. Farming suicides during the Victorian drought: 2001–2007. Aust J Rural Health. 2012;20(1):11‐15. [DOI] [PubMed] [Google Scholar]
- 30. Hanigan IC, Butler CD, Kokic PN, Hutchinson MF. Suicide and drought in New South Wales, Australia, 1970–2007. Proc Natl Acad Sci USA. 2012;109(35):13950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Parida Y, Dash DP, Bhardwaj P, Chowdhury JR. Effects of drought and flood on farmer suicides in Indian states: an empirical analysis. Econ Disasters Clim Chang. 2018;2(2):159‐180. [Google Scholar]
- 32. Daghagh Yazd S, Wheeler SA, Zuo A. Understanding the impacts of water scarcity and socio‐economic demographics on farmer mental health in the Murray‐Darling Basin. Ecol Econ. 2020;169:106564. [Google Scholar]
- 33. Howard M, Ahmed S, Lachapelle P, Schure MB. Farmer and rancher perceptions of climate change and their relationships with mental health. J Rural Ment Health. 2020;44(2):87‐95. [Google Scholar]
- 34. Pailler S, Tsaneva M. The effects of climate variability on psychological well‐being in India. World Dev. 2018;106:15‐26. [Google Scholar]
- 35. Wind TR, Joshi PC, Kleber RJ, Komproe IH. The impact of recurrent disasters on mental health: a study on seasonal floods in northern India. Prehosp Disaster Med. 2013;28(3):279‐285. [DOI] [PubMed] [Google Scholar]
- 36. Canu WH, Jameson JP, Steele EH, Denslow M. Mountaintop removal coal mining and emergent cases of psychological disorder in Kentucky. Community Ment Health J. 2017;53(7):802‐810. [DOI] [PubMed] [Google Scholar]
- 37. Speldewinde PC, Cook A, Davies P, Weinstein P. A relationship between environmental degradation and mental health in rural Western Australia. Health Place. 2009;15(3):880‐887. [DOI] [PubMed] [Google Scholar]
- 38. Akpinar A, Barbosa‐Leiker C, Brooks KR. Does green space matter? Exploring relationships between green space type and health indicators. Urban For Urban Green. 2016;20:407‐418. [Google Scholar]
- 39. Losert C, Schmauss M, Becker T, Kilian R. Area characteristics and admission rates of people with schizophrenia and affective disorders in a German rural catchment area. Epidemiol Psychiatr Sci. 2012;21(4):371‐379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nishigaki M, Hanazato M, Koga C, Kondo K. What types of greenspaces are associated with depression in urban and rural older adults? A multilevel cross‐sectional study from JAGES. Int J Environ Res Public Health. 2020;17(24):9276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Alcock I, White MP, Lovell R, et al. What accounts for ‘England's green and pleasant land’? A panel data analysis of mental health and land cover types in rural England. Landsc Urban Plan. 2015;142:38‐46. [Google Scholar]
- 42. Hounsome B, Edwards RT, Edwards‐Jones G. A note on the effect of farmer mental health on adoption: the case of agri‐environment schemes. Agric Syst. 2006;91(3):229‐241. [Google Scholar]
- 43. Mann S, Freyens B, Dinh H. Crises and structural change in Australian agriculture. Rev Soc Econ. 2016;75(1):76‐87. [Google Scholar]
- 44. Stain HJ, Kelly B, Carr VJ, Lewin TJ, Fitzgerald M, Fragar L. The psychological impact of chronic environmental adversity: responding to prolonged drought. Soc Sci Med. 2011;73(11):1593‐1599. [DOI] [PubMed] [Google Scholar]
- 45. Friel S, Berry H, Dinh H, O’Brien L, Walls HL. The impact of drought on the association between food security and mental health in a nationally representative Australian sample. BMC Public Health. 2014;14(1):1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kallioniemi MK, Simola A, Kaseva J, Kymalainen HR. Stress and burnout among Finnish dairy farmers. J Agromedicine. 2016;21(3):259‐268. [DOI] [PubMed] [Google Scholar]
- 47. Morgan MI, Hine DW, Bhullar N, Dunstan DA, Bartik W. Fracked: coal seam gas extraction and farmers’ mental health. J Environ Psychol. 2016;47:22‐32. [Google Scholar]


