Abstract
Since the outbreak of COVID-19 pandemic, maintaining safety in dental operations has challenged health care providers and policy makers. Studies on dental aerosols often focus on bacterial viability or particle size measurements inside dental offices during and after dental procedures, which limits their conclusions to specific cases. Fundamental understanding on atomization mechanism and dynamics of dental aerosols are needed while assessing the risks. Most dental instruments feature a build-in atomizer. Dental aerosols that are produced by ultrasonic or rotary atomization are considered to pose the highest risks. In this work, we aimed to characterize dental aerosols produced by both methods, namely by Mectron PIEZOSURGERY® and KaVo EXPERTtorque™. Droplet size distributions and velocities were measured with a high-speed camera and a rail system. By fitting the data to probability density distributions and using empirical equations to predict droplet sizes, we were able to postulate the main factors that determine droplet sizes. Both dental instruments had wide size distributions including small droplets. Droplet size distribution changed based on operational parameters such as liquid flow rate or air pressure. With a larger fraction of small droplets, rotary atomization poses a higher risk. With the measured velocities reaching up to 5 m s−1, droplets can easily reach the dentist in a few seconds. Small droplets can evaporate completely before reaching the ground and can be suspended in the air for a long time. We suggest that relative humidity in dental offices are adjusted to 50% to prevent fast evaporation while maintaining comfort in the office. This can reduce the risk of disease transmission among patients. We recommend that dentists wear a face shield and N95/FFP2/KN95 masks instead of surgical masks. We believe that this work gives health-care professionals, policy makers and engineers who design dental instruments insights into a safer dental practice.
Keywords: COVID-19, Dental aerosols, Airborne transmission, Droplet size distribution, PIEZOSURGERY, Dental drill
1. Introduction
Airborne diseases such as pneumonic plague, tuberculosis, influenza, Legionnaires’ disease, severe acute respiratory syndrome (SARS) and flu in dental settings have been a topic of concern in dental settings for a while (Harrel & Molinari, 2004). The study of dental aerosols dates back over 30 years (Micik et al., 1969, 1971; Miller et al., 1971). However, the COVID-19 pandemic has brought the importance of dental aerosols as vectors of infection transmission to the forefront. The dental healthcare was reduced to acute needs worldwide during the lock-down periods. With the reopening of dental practices, new safety measures were suggested in dental clinics. Some of these measures include patients wearing face masks in the waiting rooms, treating patients alone in a room, use of rubber dam during the operations or use of high-volume extraction devices (Li et al., 2020; Politis et al., 2020a, 2020b).
There are several classifications for dental instruments based on shape and materials of the tips. In addition, there are several ISO standards based on the general and specific characteristics of dental instruments, on the materials and on the shape of the dental instruments (Ahmed & Jackson, 2019). However, there is no classification on droplet size distributions of aerosols generated by dental instruments. The lack of the fundamental studies on atomization mechanisms, droplet size distributions and droplet velocities makes it difficult to assess the risks associated to specific dental instruments and to develop standards based on dental aerosols.
In the field of dentistry, the term aerosols is defined to contain small particles suspended in air or gas. Depending on the study, aerosols are defined as suspension of particles which have diameters less than 5 μm (Innes et al., 2021), 10 μm (Allison et al., 2021) or 50 μm (Harrel & Molinari, 2004; Micik et al., 1969, 1971; Miller et al., 1971) whereas splatter is used to contain larger particles (Allison et al., 2021; Harrel & Molinari, 2004; Innes et al., 2021; Micik et al., 1969, 1971; Miller et al., 1971). Aerosols which contain droplets smaller than 100 μm were considered risky in terms of disease transmission such as coronavirus instead of commonly used threshold of 5 μm (Prather et al., 2020). Droplet size distribution is a continuum and these distinctions are done somewhat arbitrarily without precise scientific evidence. In addition, large particles can evaporate quickly depending on the relative humidity. In this work, we follow the definitions in the field of aerosol sciences. We use the term, aerosol, to refer to suspension of liquid or solid particles of any size in air. In aerosol science, atomizer is used to refer to any device that produces aerosols by spraying a liquid suspension or solution (Hinds, 1999; Nasr et al., 2002). In this paper, we use the term, atomizer, to refer to the dental instruments which generate aerosols.
Although there is no consensus on the threshold droplet diameter that is considered risky as just discussed, the threshold diameter can be based on particle deposition on the respiratory system and infection route of microorganisms for airborne transmission. Particle deposition on the respiratory system can be predicted accurately by a model proposed by International Commission on Radiological Protection (ICPR 66 model) (ICRP, 1994). Hinds (Hinds, 1999) simplified the ICRP 66 model to some equations which can predict the regional deposition fraction of inhaled particles based on just droplet diameter (Hinds, 1999). Based on this model, droplets with diameters larger than 10 μm are most likely to end up in the head airways whereas droplets with diameters smaller than 10 μm are more likely to deposit on the alveolar region (Hinds, 1999; Rostami, 2009). When bioaerosols containing large droplets are deposited in the head airways, viruses were hypothesized to pass through the mucous membranes, especially nasal and larynx mucosa. Then, they can spread towards the lungs through the respiratory tract (Lin et al., 2020). However, small droplets are considered to be more dangerous since they remain suspended in air for a longer period of time and can cause direct transmission by reaching deep into the lungs (Guzman, 2021). All in all, droplets of any size that contain viruses or bacteria are potentially infectious (Guzman, 2021) although it is relatively easier to mitigate the risks associated to large droplets. Surgical masks can filter droplets larger than 5 μm whereas N95/FFP2/KN95 masks can filter droplets larger than 0.3 μm with 95% efficiency (Tcharkhtchi et al., 2021). In addition, surgical masks are not designed to tightly fit to the face and consequently a fraction of the inhaled and exhaled breath bypasses the filter material. Therefore, it is important to know both droplet size distribution and how far droplets can reach in dental settings to suggest correct personal protective equipment for dentists. Keeping droplets large also decreases the likelihood of infecting the next patient since large droplets settle more quickly.
Many dental instruments have built-in atomizers for cooling purposes. The main sources of dental aerosols in the dental practice are ultrasonic scalers, piezotomes, high-speed air rotors and air-water syringes (Harrel & Molinari, 2004). National services of Scotland consider dental procedures using high-speed devices such as ultrasonic scalers and high-speed drills as posing an increased risk of respiratory infection transmission (National Services Scotland, 2021). Although dental instruments are spraying water, tips of the instruments are directly in touch with the tissues which potentially carry various viruses and bacteria. Indeed, higher microbial activity was observed in the air (Dawson et al., 2016; Grenier, 1995; Ireland et al., 2003) and on the coats of the dentists after the dental procedures (Acharya et al., 2010). Innes et al. reviewed 83 studies on dental procedures which generate aerosols. Most of the studies reviewed used settle plates and air samplers. Although dental procedures were not directly associated with the transmission of pathogenic microorganisms, contamination of persons in the dental surgery and the air was found in all studies. The authors suggested that a hierarchy of contamination risk: high (ultrasonic scaling, high-speed air-rotor, air-water syringe, air polishing and extractions using motorized hand pieces), moderate (slow-speed handpieces, prophylaxis and extractions) and low (air-water syringe with water only and hand scaling) (Innes et al., 2021).
Several studies focused on measurement of particle sizes inside dental offices during and after various dental procedures. A wide range of particle sizes was observed (Din et al., 2020; Dudding et al., 2022; Ireland et al., 2003; Kun-Szabó et al., 2021; Polednik, 2014). Contamination was observed at the maximum distance measured (up to 4 m) with higher contamination levels within 1–1.5 m of the source (Allison et al., 2021). Depending on the measurement setting, particle concentrations or microbial activity reached baseline levels after 5 min (Din et al., 2020), 15 min (Kun-Szabó et al., 2021) or after 2 h (Grenier, 1995).
Most research on dental aerosols focuses on measuring microbial activity from the samples collected around the dental offices (Acharya et al., 2010; Akin et al., 2021; Dawson et al., 2016; Grenier, 1995; Ireland et al., 2003) or on measuring particle size distributions of the samples collected from the dental offices (Din et al., 2020; Dudding et al., 2022; Ireland et al., 2003; Polednik, 2014). In addition, a few studies focused on measuring fluorescence of the samples collected around the dental office after introducing a fluorescent dye either in the reservoir water of the instruments (Allison et al., 2021) or to the oral cavity of the mannequin (Llandro et al., 2021). The increased levels of particle sizes, bacterial contamination or fluorescence after the use of aerosol-producing dental instruments suggest that these instruments increase the risk of disease transmission. Although these studies point out the potential risks associated to the dental operations, their conclusions are case specific and do not explain the physical mechanisms behind the measured risk factors. Aerosols scattered around a dental office can depend on direction of the spray, size of the room, humidity and air flow inside dental offices and whether the dental operation was performed on a patient or a mannequin. Therefore, there is a need for fundamental understanding on the source of these dental aerosols. To the best of our knowledge, there is only one study which studied the atomization mechanism of rotary dental instruments by measuring droplet sizes of a dental drill positioned on the dental enamel of a mannequin. The authors concluded that elimination of mixing of coolant water and air prior to burr contact reduced the number of small droplets. Droplet sizes were measured from only one position with a camera which can detect droplets with diameters above 100 μm. Therefore, a large fraction of the size distribution were missing. The authors also used an optical particle size counter with a range from 0.3 to 10 μm to compensate for some part of the missing fraction of droplet sizes (Sergis et al., 2021). Due to the limitations of their camera set-up, data collection from only one position and representation of droplet size distribution on heat maps, the overall size distribution is not clear. A more comprehensive work is necessary to understand atomization mechanism, droplet size analysis and dynamics of dental aerosols.
Since dental instruments that produce aerosol through ultrasonic and high-speed rotary atomization are considered to have the highest risks of contamination (Innes et al., 2021), we investigated atomization mechanism and droplet size distribution of both types of dental instruments with measurements right after the tip of the dental instruments at several positions inside the aerosol. Ultrasound is used in many dental operations. Ultrasonic scalers are used in everyday dental operations to remove dental plaque and calculus (George et al., 2014). PIEZOSURGERY® was patented around two decades ago. At the moment, it is the leading bone-cutting technology in oral and maxillofacial surgeries since it reduces the damage to the surrounding soft tissues (Labanca et al., 2008). Although the exact tip length and design vary according to the manufacturer and the application, most tips look similar. The tip of ultrasonic dental instruments bend towards the end of the tip. Water is sprayed on top of the tip to prevent damages due to overheating (George et al., 2014). The choice of the correct parameters and the design of the instruments might have a major effect on the health of the dentists. An ultrasonic frequency of 25–30 kHz is used in dental instruments to cut the mineralized tissue (George et al., 2014; Labanca et al., 2008). Sizes of droplets generated by ultrasonic atomizers are mostly affected by ultrasound frequency along with other parameters such as flow rate, viscosity and surface tension of the liquid (Kooij et al., 2018, 2019; Rajan & Pandit, 2001). High-speed dental drills are also used in daily dental operations. Dental drills utilize a rotary motion to atomize water. In this work, we worked on atomization mechanism and droplet size distribution of Mectron PIEZOSURGERY® and the dental drill, KaVo EXPERTtorque™. We expect that other dental instruments which utilize ultrasound or rotary motion to generate aerosols have similar atomization mechanism. We believe that this work provides insights into safer dental operation by highlighting the importance of designs and operational parameters of dental instruments, relative humidity in dental clinics and use of personal protective equipment.
2. Methods
Droplet size analysis and the velocity measurements were done by a high-speed camera (Pyrooptic, Denmark). One pixel corresponded to 2.5 μm. At least five pixels are needed to be able to detect a droplet. Therefore, in theory, minimum detectable droplet diameter of our lens was 4.0 μm. The depth of field (DOF) of the lens was measured with a calibration ruler (Thorlabs) as 0.64 mm. The field of view (FOV) was 3.2 × 2.4 mm. The counting efficiency of the optical methods decreases towards the minimum detectable droplet diameter. We checked the counting efficiency of our lens by doing the same experiments with another lens which can detect droplets as small as 1.0 μm. The results showed that the counting efficiency of the lens that we used in this work started decreasing when droplets diameter was below 11 μm. However, the lens which can detect smaller droplets could see a volume that was more than ten times smaller compared the volume that the lens used in this work could see. Since the dental instruments are not designed to deliver a proper spray cone, aerosol concentration is quite low in most positions. As a result, most measurements result in empty images, which also decreases the accuracy of the measurements. Therefore, we chose to work with the lens which has a larger DOF and FOV.
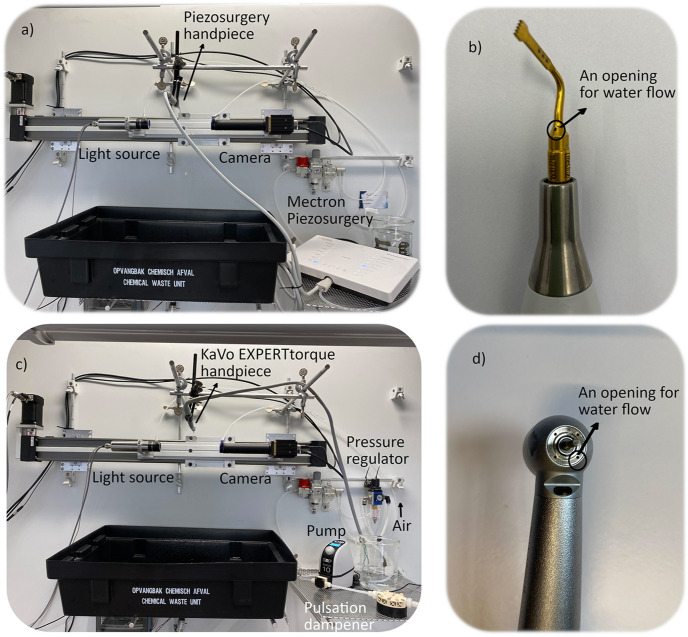
Two consecutive images were taken with a time delay of 1 μs for the velocity measurements. The camera set-up was placed on a linear rail system (Igus, Belgium), which was controlled with a computer. The Mectron PIEZOSURGERY® and the KaVo EXPERTtorque™ Lux E680 were placed as shown in Fig. 1 a and c, respectively. The measurements were done in every 3 mm along 90 mm (from −45 to 45 mm) in the direction of the linear rail system (x-direction) and in every 5 mm along 90 mm (from −45 to 45 mm) in the direction perpendicular to the rail system (y-direction). The tip of the dental equipment was considered as the origin. All measurements were taken 3 cm below the tip of dental equipment. Around a thousand images were taken at each position. The images of the spray break up was taken with a digital camera by shining light on the spray with Mightex high-power LED collimator light source (LCS-6500-xx).
Fig. 1.
Experimental systems. a) The Mectron PIEZOSURGERY® with the camera and the rail system, b) the Mectron PIEZOSURGERY® hand piece, c) the KaVo EXPERTtorque™ Lux E680 with the camera and the rail system, d) the hand piece of the KaVo EXPERTtorque™ Lux E680.
Water goes through an oval opening with dimensions of approximately 0.85 × 0.60 mm close to the tip of Mectron PIEZOSURGERY® (Fig. 1b). There are over 90 different tips (inserts) for Mectron PIEZOSURGERY® for different types of dental operations (Mectron. (n.d.-b)). Here, we worked with tip OT7 which is often used for bone cutting (Mectron Medical Technology. (n.d.-a)). The KaVo EXPERTtorque™ has a circular opening with a diameter of approximately 0.60 mm for water flow (Fig. 1d). The rotating drill has a diameter of 1.6 mm. The Mectron PIEZOSURGERY® has six functions: endo, perio, special, cancellous, cortical and implant and six irrigation levels. The measurements were taken at each function with irrigation levels 1, 3 and 6. The irrigation level was controlled by a peristaltic pump which was attached to the instrument. For the KaVo EXPERTtorque™, air pressure was adjusted to 2.5 and 3.0 bars and water flow rate was 50.0 and 100 ml min−1 (KaVO Dental Technologies, n.d.). KNF Simdos 10 pump and KNF pulsation dampener were used to pump water. The whole set-up was inside a fume hood. Air was supplied to the fume hood from a central air compressor. Air pressure was adjusted with a pressure regulator.
The images were analyzed in Fiji yielding the raw droplet size distribution data. The rest of the data analysis was done in MATLAB R2020b. Probability density (pd) distributions of droplet diameters (histograms) and droplet velocities were obtained by considering all the measurements along the x and y directions. Aerosol number concentration was calculated at each position in x and y directions. The parameters of the probability density functions (pdfs) were obtained by MATLAB Statistics and Machine Learning Toolbox™ function ‘mle’ by fitting droplet size data to bimodal lognormal pdfs. More details on the data analysis is given in the Appendix. Correlation between droplet diameter and droplet velocities were checked by using Pearson correlation with the MATLAB function ‘corr’. While checking for the correlation between velocities and droplet sizes, the negative and the positive values of velocities in the z-direction were taken into account whereas absolute values for the velocities in the y-direction was considered. That was because droplets going up or down in the z-direction are expected to have an effect on the correlation because of the effect of gravity. On the other hand, droplets moving in positive or negative y-direction are not expected to make any difference in the correlation since the instruments are expected to have quasi symmetrical distributions in the y-direction. Velocities in y and z directions are reported with both positive and negative values. Average velocities are reported based on the sign of the z-direction without taking into account the sign of the y-direction. The algorithms of the overall data acquisition and analysis and of all the codes used to obtain histograms for droplet diameters, pdfs, velocities and aerosol number concentration are given in the Appendix in Fig. A1 – Fig. A7. Details of the calculations of droplet coagulation and evaporation rate are given in the Appendix.
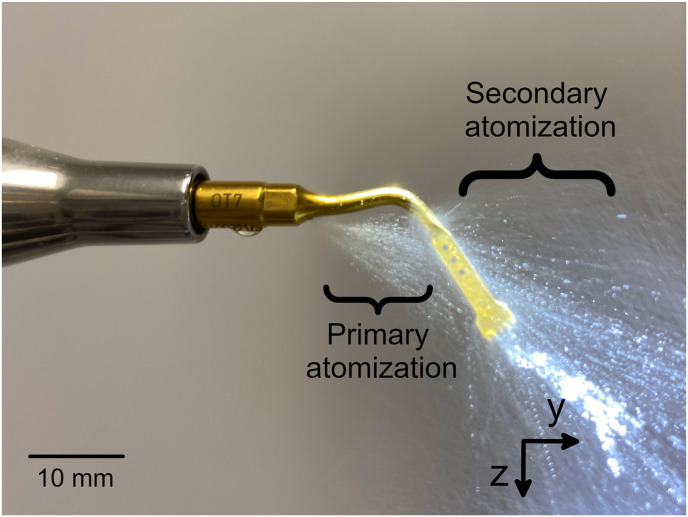
Fig. 7.
The formation of droplets at the tip of the KaVo Expert Torque™. The arrows showing z and y directions point towards the positive directions. The positive values of the x direction are pointing away from the reader. The origin point was at 3 cm below the tip of the dental instrument as illustrated on the figure.
3. Results
3.1. Droplet size distributions and velocities of Mectron PIEZOSURGERY®
The number- and volume-weighted pd distributions of droplet sizes of the Mectron PIEZOSURGERY® were fitted to bimodal lognormal pdfs (Equation (1)). Three irrigation levels and six functions were studied. Water flow rates at different irrigation levels are given in Fig. A8. The functions are used for different kinds of treatments and surgeries such as periodontal treatment (cleaning the pockets around the teeth), osteotomy (bone cutting), osteoplasty (plastic surgeries on the bones), endodontics (root canal treatment), tooth extractions, sinus membrane elevation, etc. Usually a mixture of the functions with different tips (inserts) are used depending on the type of treatment (Mectron Medical Technology. (n.d.-a)).
| (1) |
where D is droplet diameter, D50 is median droplet diameter, σ is standard deviation and p is mixing parameter. Subscripts 1 and 2 denotes the first and the second pdfs.
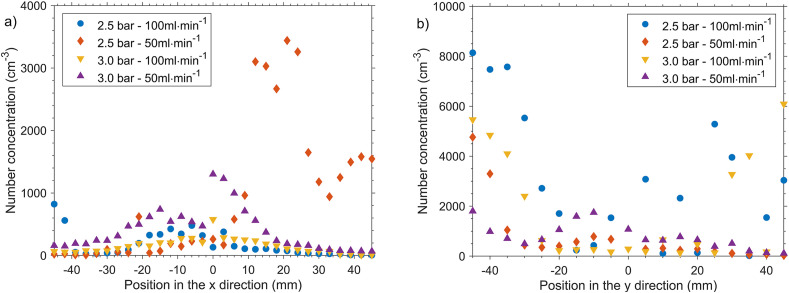
Fig. 8.
Aerosol number concentration of KaVo EXPERTtorque™ a) in the x-direction, and b) in the y-direction.
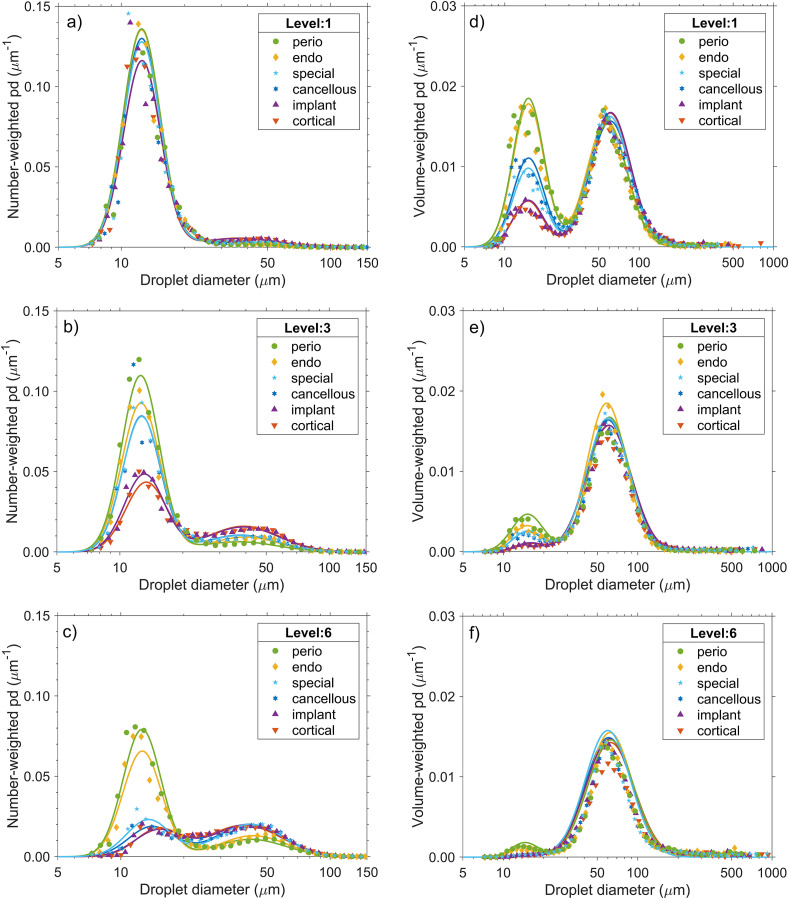
As shown in Fig. 2 , the peak for the small droplet sizes was reduced significantly at high irrigation levels for all the functions of Mectron PIEZOSURGERY®. The parameters of the number- and volume-weighted pdfs are given in Table A.1 and A.2, respectively. For all droplet size distributions, the experimental data fitted the bimodal lognormal pdfs very well with most R2 values over 0.90. The mixing parameter decreased as the irrigation level increased since the weight of the peak for the small droplets was decreased.
Fig. 2.
Number-weighted probability density (pd) distribution of droplet diameters of Mectron PIEZOSURGERY® at irrigation levels (a) 1, (b) 3, and (c) 6. Volume-weighted pd distributions of droplet diameters of Mectron PIEZOSURGERY® at irrigation levels (d) 1, (e) 3, and (f) 6. pd represents probability density. The x axis is on log-scale. The lines show the predictions of the probability density function.
Median diameter (D50 (μm)) of droplets generated by ultrasonic atomizers depend on the excitation frequency of the ultrasound (f (Hz)), the surface tension (σ (mN.m−1)) and the density of the liquid (ρ (g.cm−3)). Lang proposed a correlation (Equation (2)) to predict droplet diameters of the ultrasonic nebulization (Lang, 1962).
| (2) |
The Mectron PIEZOSURGERY® operates at frequencies in the range of 24–36 kHz (Mectron. (n.d.-c)). The median diameters of water droplets which were generated at ultrasonic frequencies of 24 and 36 kHz can be calculated based on Equation (2) as 50 and 38 μm, respectively. The spray break-up of the Mectron PIEZOSURGERY® is shown in Fig. 3 . Droplet formation right after water was coming out of the opening could be associated with the ultrasound (primary atomization). D50 2 can be associated with the primary atomization. D50 2 of the number-weighted bimodal lognormal pd were found in the range of 32–49 μm (Fig. 2 and Appendix Table 1), which were in line with the predictions of the Lang’s correlation. It seems that droplets are broken down into smaller droplets when they hit the vibrating tip of the dental handpiece (secondary atomization). These two different mechanisms for atomization must be the reason of the two peaks observed in droplet size distribution (Fig. 2).
Fig. 3.
The formation of droplets at the tip of the Mectron PIEZOSURGERY®. The arrows showing z and y directions point towards the positive directions. The positive values of the x direction are pointing away from the reader. The origin point was at 3 cm below the tip of the dental instrument as illustrated on the figure. (The position of the origin point is not to scale.) The instrument tip moves in the y-direction to cut the tissue. The irrigation level was 6.
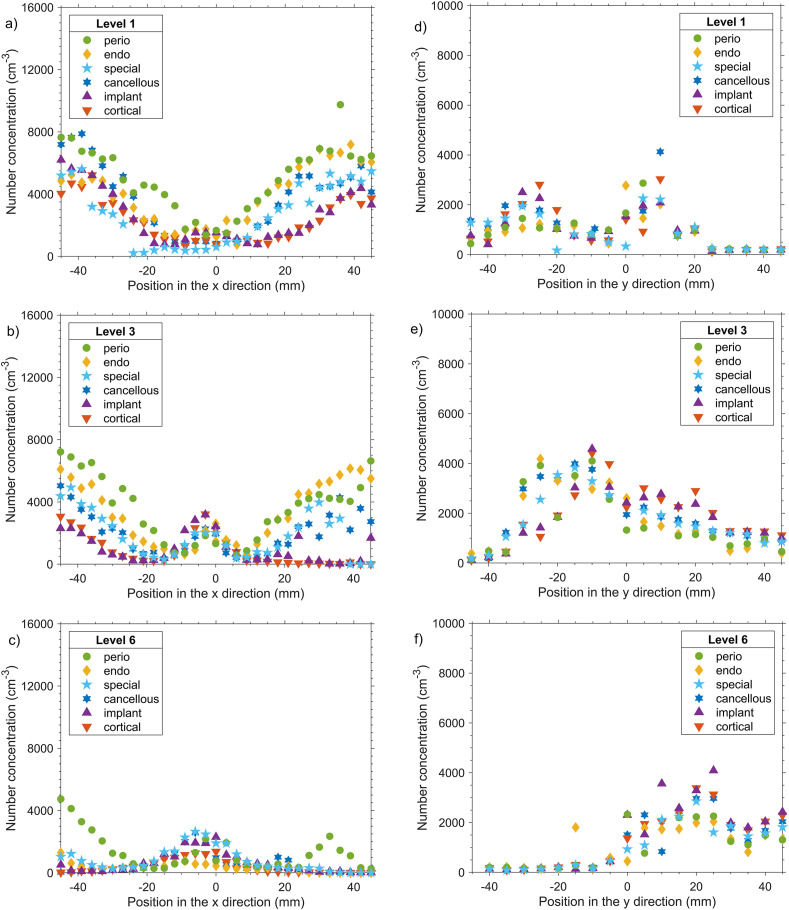
The number of droplets which were generated by the secondary atomization decreased with increasing irrigation level. That seems to be because the spray cone widens at high irrigation levels. As a result, less droplets hit the tip of the nozzle compared to overall generated droplets. When less droplets hit the tip of the nozzle, less droplets with smaller diameters were generated. This can also be seen from the aerosol number concentration at several positions in x and y directions (Fig. 4 ) The direction of the secondary atomization was also different at different irrigation levels. At lower irrigation levels, the droplets generated after the impact of the tip of the nozzle ended up mostly in the negative y-direction while more droplets ended up in the positive y-direction as the irrigation increased. It should also be noted that at high irrigation levels, aerosol number concentration was less since most of the liquid was carried with larger droplets. The amount of droplets that are scattered in x direction were also less. That shows that after the impact with the nozzle tip, droplets are more scattered.
Fig. 4.
Aerosol number concentration of the Mectron Piezosurgery® in the x-direction for irrigation levels a) 1, b) 3, and c) 6. Aerosol number concentration in the y-direction for irrigation levels d) 1, e) 3, and f) 6.
Droplet size distributions with large median droplet sizes and a small standard deviation are desired for a safer dental practice. Droplet size distribution generated by dental equipment can be controlled by the design of the equipment and the physical properties of the liquid such as surface tension and density (Lang, 1962; Mugele, 1960). Based on the Lang’s correlation, physical properties of liquids cannot increase droplet sizes more than 10 μm. The main parameter that affects droplet sizes is the ultrasonic frequency (Fig. A9). Micromovements caused by different ultrasonic frequencies can cut different tissue types. For example, an ultrasonic frequency of 25–30 kHz is used to cut only the mineralized tissue whereas neurovascular tissue is cut by frequencies higher than 50 kHz (Labanca et al., 2008). Therefore, the ultrasonic frequency of the dental instruments cannot be adjusted to generate larger droplets. The same applies for ultrasonic scalers which work with similar ultrasonic frequencies (George et al., 2014). Therefore, the best strategy to increase droplet sizes seems to be to consider droplet size distribution of the aerosols generated by the ultrasonic dental instruments while designing the tips of the instruments. It should be noted that once the tip of the Mectron PIEZOSURGERY® is changed, droplet size distribution at different irrigation levels might be different. However, atomization mechanism is expected to remain the same. As a result, bimodal lognormal pd distribution is also expected with different tips. More research on aerosol generation and droplet size analysis is needed while designing dental instruments. This work shows that aerosol needs to be targeted to more to have similar cooling efficiencies and less small droplets as seems to be the case for the higher irrigation levels of the Mectron PIEZOSURGERY®.
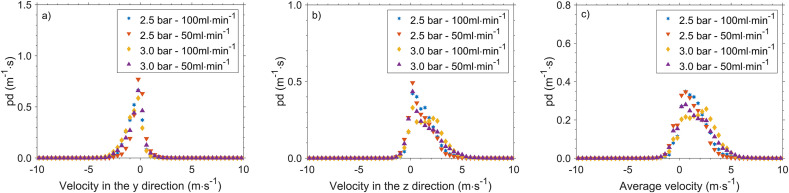
Fig. 9.
Probability density (pd) distributions of velocities of KaVo EXPERTtorque™ a) in the y-direction, b) in the z-direction, c) average velocity. Average velocities are reported based on the sign of the z-direction without taking into account the sign of the y-direction.
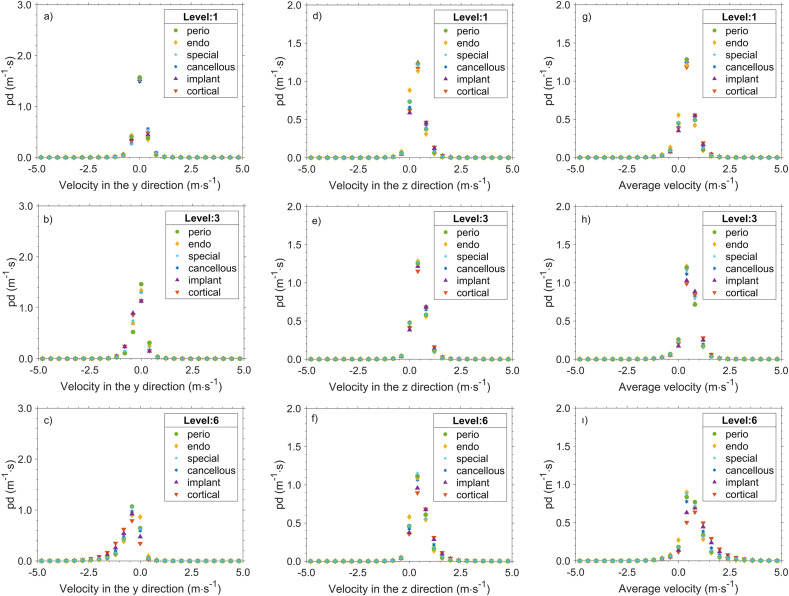
The pd distribution of droplet velocities of Mectron PIEZOSURGERY® at different irrigation levels for velocities in the y-direction (the direction of the rail system), in the z-direction (the direction of the gravitational force) and the average velocity are shown in Fig. 5. Droplet velocities increased as the irrigation level increased, which can be expected. While most of droplets had velocities around 0.4 m s−1, droplet velocities went up to 2.5 m s−1. Droplet diameter versus velocity figures are given Fig. A.10 for the endo function at several irrigation levels. The rest of the functions had similar trends. We checked for a correlation between droplet diameter and velocity with Pearson correlation. The hypothesis of no correlation was checked. When p-values are smaller than the significance value of 0.05, the hypothesis was rejected. In other words, a correlation exists between droplet diameters and velocities when p-values are smaller than 0.05. The positive values of the Pearson correlation coefficient (ρ) values indicates that there is a positive correlation. The p-values were smaller than 0.05 for all the parameters tested. There was a correlation between droplet diameter and velocities in the y-direction (Table A.3), velocities in the z-direction (Table A.4) and the average velocities (Table A.5). The positive correlation between velocities in the z-direction and droplet diameter (Table A.4) indicates that larger droplets land faster, as expected. On the other hand, there was a both positive and negative correlation between velocities in the y-direction and droplet diameter depending on the function. Small values of the Pearson correlation coefficient indicates that the correlation was weak (Table A3). Here, we checked for a correlation considering all droplets from all camera positions. The correlation for velocities in the y-direction and droplet diameter might depend on the camera position. Still, droplets that are escaping the mouth of the patient at these y-velocities can reach the dentist in a few seconds.
Fig. 5.
Probability density (pd) distributions of velocities in the y-direction of the Mectron PIEZOSURGERY® for irrigation levels a) 1, b) 3, and c) 6. Pd distributions of velocities in the z-direction for irrigation levels d) 1, e) 3, and f) 6. Pd distribution of average velocities for the irrigation levels g) 1, h) 3, and i) 6. Average velocities are reported based on the sign of the z-direction without taking into account the sign of the y-direction.
The size and the number of droplets that end up in the proximity of the dentist depend on the aerosols generated by the dental equipment in addition to the other factors such as water suction in the mouth of the patient, the breathing pattern of the patient and temperature and humidity in the dental clinics. Droplet sizes between 5 and 300 μm and velocities between 1.3 and 2.6 m s−1, which were similar to our findings, were recently reported during dental scaling around the patient’s mouth (Mirbod et al., 2021). It seems that some droplets are indeed escaping the mouth of the patient.
3.2. Droplet size distributions and velocities of Kavo EXPERTtorque™
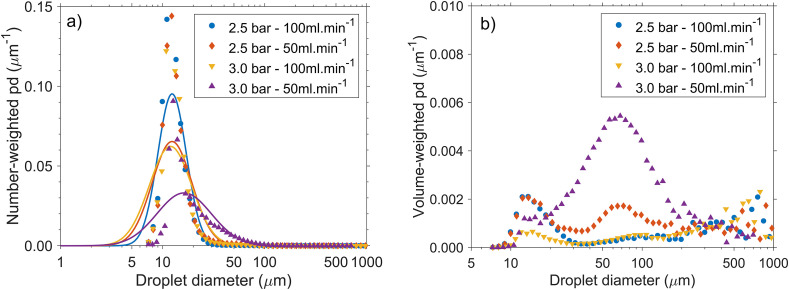
The number-weighted and volume-weighted pd of droplet diameters of KaVo EXPERTtorque™ in Fig. 6 a and b, respectively. The number-weighted distributions were fitted to a lognormal distribution. The parameters of the number-weighted pdfs are shown in Table A.6. The pdf did not fit very well with R2 as low as 0.58. The reasons for the lack of the fit can be due to the small droplets that could not be measured with our camera system along with the atomization mechanism which is explained later. There is a sharp decrease at the lower end of the droplet size distribution which indicates that there were more, smaller droplets than what was measured in this work. It should be noted that the goal of this work was not to provide an exact size distribution but to understand the atomization mechanism and the effect of the parameters such as air pressure and liquid flow rate on the size distribution. The difference in number- and volume-weighted distribution shows that there were only a few large droplets which had large volumes. Therefore, water was poorly atomized (Fig. 6 a and b). The number of small droplets was the highest at 2.5 bar and 100 ml min−1 for KaVo EXPERTtorque™. As the pressure increased to 3.0 bar, larger droplets were generated, which is counter intuitive. This phenomenon can be related to the atomization mechanism as explained below.
Fig. 6.
Probability density (pd) distribution of KaVo EXPERTtorque™ at different air pressures and the liquid flow rates: a) the number-weighted distribution, b) the volume-weighted pd distribution. The x-axis is on log-scale. The lines show the predictions of the probability density function.
KaVo EXPERTtorque™ series is an air-turbine handpiece which operates between 400,000 and 480,000 rpm (KaVO Dental Technologies, n.d.). However, air is not supplied to break-down the liquid into droplets as in the case of air blast nozzles. Air is circulated inside the head of this dental handpiece to propel the drill (Juraeva et al., 2020). Sergis et al. (Sergis et al., 2021) mentioned that water and air was premixed in the head of the dental drills. When the authors blocked the premixing, they manage to get larger droplets. However, we could not find any technical drawings which include premixing of water and air in the head of the dental drill. From the technical drawings in the dental drill patents, it can be seen that water comes out from the holes on the drill head directly without getting mixed inside the head of dental drill (Aymar et al., 1959; Zhang, 2009).
Mechanical atomization is achieved by various ways such as pressure nozzles, air blast nozzles, spinning discs and whirl chambers, etc. The main mechanism of atomization is similar among different nozzles. First, the applied force, either pressure or rotation, creates liquid sheets or ligaments from the bulk of the liquid. Secondly, waves are formed on the liquid sheets or ligaments due to the friction by the surrounding air. These waves grow in amplitude and create thickness modulations in the liquid sheets or ligaments. Then, the thickness modulations cause the liquid sheet to create fragments, which, in turn, break up into droplets (Kooij et al., 2018; Marmottant & Villermaux, 2004; Mugele, 1960). Mugele (Mugele, 1960) suggested correlations to predict droplet sizes of several mechanical atomizers (Equation (3)). We used the constants suggested for the calculation of the maximum droplet sizes for the spinning discs or cups (Mugele, 1960). Based on these values the maximum droplet sizes were calculated around 55 μm for both water flow rates (50 and 100 ml min−1). These predictions were close to the maximum droplet sizes of KaVo EXPERTtorque™ (Fig. 6a). The formation of droplets at the tip of the KaVo EXPERTtorque™ are shown in Fig. 7 . As the pressure increases, the rotational speed is expected to increase. That is expected to cause a decrease in droplet sizes. However, droplet sizes decrease as the pressure increases (Fig. 6 and Table A.6). A possible explanation could be that there were two different atomization mechanisms. Air circulating around the rotating drill can break down the liquid somewhat similar to the case of air-assisted atomization. In addition, the liquid film can be broken down by hitting the rotating drill as in the case of rotary atomization. It seems that the interplay of the air-assisted and rotary atomization is changing with the rotational speed. At high rotational speed, swirling air flow around the drill is expected to increase, which can break down more liquid whereas droplet formation due to rotary atomization might increase at lower rotational speeds. In fact, the lack of fit of droplet size distribution to the pdf (Fig. 6) might also be due to the two atomization mechanisms taking place at the same time. When the liquid flow rate is lower, the amount of liquid that can get into the strong swirling air current and hit the nozzle tip will be less. That might be the reason why the predictions of the correlation provided by Mugele (Mugele, 1960) cannot predict the experimental data properly only at higher air pressures and lower liquid flow rates. Therefore, at these conditions, the dominant atomization mechanism seems to be shifting from rotary atomization to air-assisted atomization.
| (3) |
where D nozzle is the diameter of the opening for the water flow, μ is the viscosity of the liquid, V r is the velocity of liquid droplet relative to the gas phase, and A, B and C are constants which depend on the type of the nebulization. The constants, A, B and C, were given as 1.73, −0.50 and −0.45 for the calculation of the maximum droplet sizes for the spinning discs or cups (Mugele, 1960).
As it can be seen from the aerosol number concentration at several positions in x- and y-direction in Fig. 8 droplets are scattered widely especially in the y-direction. When the air pressure was 2.5 bar and the liquid flow rate was 100 ml min−1, more small droplets were generated as discussed above. That setting also resulted in droplets that are scattered around the most with a high number concentration at several positions as shown in Fig. 8 . When the air pressure was 3.0 bar and the liquid flow rate was 50 ml min−1, the larger droplets were generated and most droplets were in the proximity of the tip. Therefore, for the air turbine hand pieces, we recommend high air pressures and low liquid flow rates.
The probability density distribution of the velocities of KaVo EXPERTtorque™ in the y- and the z-direction and the average velocity are given in Fig. 9. Droplet velocities of KaVo EXPERTtorque™ went up to 5 m s−1, which were larger than droplet velocities of Mectron PIEZOSURGERY®. Using different air pressures and liquid flow rates did not change droplet velocities significantly. Droplet diameters versus velocities are shown in Fig.A.11 at 2.5 bar and 50 ml min−1. The trend in the data was similar for other parameters tested in this work. Parameters of the Pearson correlation between droplet diameter and velocities in the y-direction, in the z-direction and the average velocities were given in Table A.7. Based on the p-values, it can be concluded that there was a correlation between droplet diameters and velocities. As droplet diameter increased, droplets landed faster for most of the parameters studied except when the air pressure was 3.0 bar and the liquid flow was 50 ml min−1. The low Pearson correlation coefficient (ρ) indicated that the correlation was not strong. That was probably because the measurements were taken close to the tip. The negative correlation might be due to the strong air current around the drill at high pressure (3.0 bar). Droplets seem to be moving with the air flow rather than based on the effect of the gravity when they are close to the tip. At these y-velocities (Fig. 9 a), droplets can reach the dentist instantly.
3.3. Discussions on the effect of droplet coagulation and evaporation
After being generated, droplets start to both coagulate and evaporate. Droplet coagulation depends on droplet diameter and aerosol number concentration which is the number of droplets per unit volume. For both dental instruments, aerosol number concentrations were less than 10,000 cm−3 at any position inside the spray. At these low aerosol number concentrations, droplet sizes are not expected to change significantly due to droplet coagulation.
When the relative humidity is below 100%, droplets evaporate. Evaporation rate depends on many parameters such as droplet diameter, relative humidity, temperature and physicochemical properties of the liquid and airflow around the droplets. If droplets do not hit a surface before drying out, they can remain suspended in air for a long time and are transported and distributed in the room by any air flow such as breathing of room occupants or buoyancy caused by thermal gradients (e.g. away from the warm body surface of the occupants). Therefore, it is important to keep droplets as large as possible to prevent airborne diseases transmission.
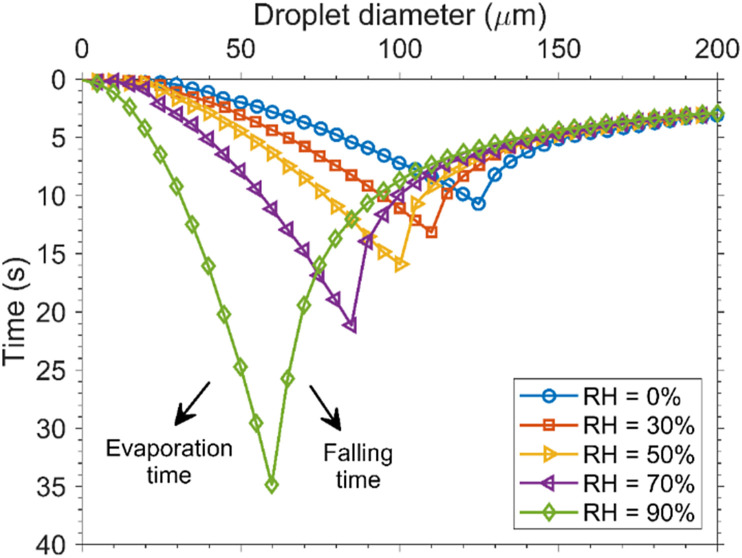
Xie et al. (Xie et al., 2007) investigated how far droplets can move in indoor environments theoretically. The authors validated their model with literature data. Evaporation of pure water droplets were studied for freely falling droplets. The authors depicted their results at several relative humidities (Fig. 10) by using Wells evaporation-falling curve of droplets after the seminal work of Wells (Wells, 1934). Wells evaporation-falling curve of droplets reports the relationship between droplet size, evaporation and falling rate from 2 m, which is the maximum human height. The dental chairs can go up to around 1.5 m depending on the treatment (ASI Dental Specialties, n.d.). Therefore, it is safe to assume a distance of 2 m for the dental chairs, as well. The lowest point of the Wells evaporation-falling curve is the critical droplet diameter. Above this diameter, droplets reach the ground before drying out completely due to evaporation. Larger droplets evaporate slowly and settle more rapidly to the ground. On the other hand, smaller droplets can evaporate completely before reaching to the ground. As the relative humidity increases, the evaporation rate slows downs and critical droplet diameters decreases. As it can be seen from Fig. 10, the critical droplet diameters are 125, 110, 100, 85 and 60 μm when relative humidities are 0%, 30%, 50%, 70% and 90%, respectively. It is recommended to have the relative humidity between 30% and 50% indoors (Environmental Protection Agency, n.d.) for comfort and to prevent mold. Therefore, keeping the relative humidity at 50% is a good strategy to keep the droplets large in dental offices.
Fig. 10.
Wells evaporation-falling curve of droplets for freely falling pure water droplets under different relative humidities (RH). Initial droplet temperature is 33 °C and room temperature is 18 °C. Falling times were calculated based on 2 m distance. The figure is redrawn based on (Xie et al., 2007). Copyright (2007) Wiley. Used with permission from X. Xie, Y. Li, A.T.Y. Chwang, P. L. Ho and W.H. Seto. How far droplets can move in indoor environments – revisiting the Wells evaporation-falling curve. Indoor Air 17: 211–225. (2007).
It should be added that Fig. 10 gives an optimistic result for the evaporation rate of droplets generated by dental instruments. Depending on the dental instruments, droplets had initial velocities going up to 2.5 and 5.0 m s−1. Higher droplet velocities increases evaporation rate and likelihood of droplets being scattered all around the room. In addition, if there are airflows around the droplets, evaporation rate increases due to convection. Evaporation rate is expected to be more for the dental drill due to the air flow created around the drill. The dental instruments are operated inside the mouth of the patient. Even though Mectron PIEZOSURGERY® does not create an airflow around the instrument, breathing pattern of the patient is expected to affect the evaporation rate of droplets. Breathing has an air velocity of around 1 m s−1. Xie et al. also modelled the evaporation of physiological saline solutions (0.9% sodium chloride w/v) to mimic saliva by considering the airflow models of exhalation flows. The critical droplet diameter at 50% relative humidity was found as 95, 85, 80, 75 μm for air velocities of 1, 5, 20 and 50 m s−1, respectively (Xie et al., 2007). Physiological saline solution has a lower vapor pressure than pure water droplets, which causes droplets to evaporate more quickly. As a result, actual evaporation rate for the dental instruments is expected to be between evaporation rate of freely falling pure water droplets and evaporation rate of droplets of physiological solution moving with an air jet.
Keeping the relative humidity high might be the easiest way to reduce the risk of disease transmission to the next patient entering the dental office. When the relative humidity is 50%, the critical droplet diameter is around 75–100 μm depending on the airflow around the droplets. If the dental chair is kept at a lower level than 2 m, the critical droplet diameter will be even smaller. That can reduce the likelihood of disease transmission to the next patient entering the dental office. However, only keeping the droplets large enough won’t protect the dentists since dentists work very closely to the patients. The dentists need to use face shields and mouth masks to protect themselves. A fraction of the droplet size distribution of both dental instruments contained droplets smaller than 50 μm. As a result, we suggest that dentists use N95/FFP2/KN95 masks instead of surgical masks while working with high-speed air rotor dental instruments and ultrasonic dental instruments. Use of additional high-volume extraction devices might help to prevent aerosols being spread around the room.
4. Conclusions
Dental aerosols have been a topic of concern for more than three decades. However, COVID-19 pandemic has brought dental aerosols to the forefront. With the awareness brought by the pandemic, safety instructions in dental offices are being revised. Most of the dental instruments have a build-in atomizer for cooling purposes. Dental aerosols which are produced by ultrasonic or rotary atomization are considered to have the highest risks of disease transmission. The lack of the fundamental studies on atomization mechanisms, droplet size distributions and droplet velocities makes it difficult to assess the risks associated to specific dental instruments and to develop standards based on dental aerosols. In this work, droplet size analysis and droplet velocities of the aerosols generated by both methods were measured with a high-speed camera and a rail system. In addition, atomization mechanisms of two of the most popular instruments were explained. It seems that for both dental instruments, there were two different mechanisms for atomization. The number- and volume-weighted probability density distributions were fitted to bimodal lognormal or lognormal distributions where possible. Droplet sizes were larger and the aerosol was less scattered around at high irrigation levels of Mectron PIEZOSURGERY® and at higher pressures (3.0 bar) and lower liquid flow rates (50 ml min−1) of KaVo EXPERTtorque™. Median droplet sizes were predicted using known correlations. The velocity measurements suggested that droplets can reach the dentist in a few seconds. This work highlights the importance of the design of dental instruments and selection of correct operational parameters to generate larger droplets and indicates the mechanisms controlling the aerosol quality. Droplet coagulation did not change droplet diameter significantly. Evaporation rate is largely determined by the initial droplet diameter, relative humidity and the airflow around the droplets. It was concluded that relative humidity inside dental clinics should be adjusted to 50% for both keeping droplets larger and maintaining comfort. Larger droplets have a higher chance on landing near the patient’s mouth. The use of a face shield can prevent the droplets settling on the dentists’ face. Since both instruments generated droplets smaller than 50 μm, we recommend dentists use N95/FFP2/KN95 masks instead of surgical masks while working with high-speed dental drills and ultrasonic dental instruments.
Author contributions
E. Kayahan contributed to the design of the study, acquisition, analysis and interpretation of the data and drafted the manuscript. M. Wu contributed to acquisition and analysis of the data and critically revised the manuscript. T. Van Gerven and L. Braeken contributed to the design of the study, interpretation of the data and critically revised the manuscript. L. Stijven contributed to the conception of the study, acquisition of the data and critically revised the manuscript. C. Politis contributed to the conception and design of the study, acquisition of the data and critically revised the manuscript. M.E. Leblebici contributed to the conception and design of the study, analysis and interpretation of the data and critically revised the manuscript. All authors gave their final approval and agreed to be accountable for all aspects of the work.
Data availability
The data are presented in the manuscript in the form of graphs. More detailed data are given in Tables in the Appendix. The image files of droplets and the raw data are kept in KU Leuven repository for 5 years after the publication and are going to be shared upon request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work is funded by KU Leuven internal funds, Starting Grant STG/18/025 (Belgium). M. E. Leblebici acknowledges Research foundation Flanders (FWO, Belgium) postdoctoral fellowship (39715). The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Biographies

Emine KayahanEmine Kayahan earned her BSc and MSc degrees at the Department of Chemical Engineering at Middle East Technical University in Turkey. During her MSc, she worked on photobioreactor design and pilot scale operations for photofermentative H2 production. Currenly, she is a PhD student at the Department of Chemical Engineering at KU Leuven in Belgium. Her PhD focuses on droplet size analysis of aerosols and mass and photon transfer in aerosol (photo)reactors. She has worked on droplet-light interactions, design and operation of aerosol photoreactors and CO2 capture in aerosol reactors.

Min WuMin Wu graduated from Technical University of Dortmund (Germany) with a Master's degree at the Department of Chemical Engineering, and from China University of Mining and Technology with a Bachelor’s degree in Mineral Processing Engineering. During the studies, she also performed an internship at R&D department in Tata Steel (the Netherlands) and an exchange study in University of British Columbia (Canada). Currently, Min Wu is a PhD student in Center for Industrial Process Technology at KU Leuven (Belgium) with the specialization in the joint research of chemical engineering and artificial intelligence.

Tom van GervenTom Van Gerven is a professor in Process Intensification and head of the Process Engineering for Sustainable Systems (ProcESS) at the Department of Chemical Engineering at KU Leuven. His research interests evolve around the use of alternative energies to intensify mass transfer and mixing in chemical processes. Tom is coordinating several European and national projects. He is chairman of the EFCE Working Party on Process Intensification and member of the board of the European Sonochemistry Society. His h-index is currently 44.

Leen Braeken Leen Braeken works as an associated professor at the Centre of Industrial Process Technology (CIPT) at the Department of Chemical Engineering of KU Leuven on Campus Diepenbeek. Her research interests include separation processes, inline image analysis and process intensification, more specifically acoustic processing and flow technology. The focus lays on reactor characterization, fouling mitigation, image analysis techniques, process development, scale up and industrial valorization. Current research projects are situated in the field of sonocrystallization, continuous crystallization, advanced oxidation processes and membrane technology.

Lambert StijvenLambert Stijven graduated in 1983 as a dentist from the KU Leuven in Belgium. In the same year, he started working as a general dentist in his solo practice in Opglabbeek. His brother Walter joined him in 1993, first as a general practitioner, later as an orthodontist. Lambert soon became involved in the implant-supported prosthesis work as well as the multidisciplinary treatment planning in the ZOL in Genk. After his son Joris joined the practice as a dentist, the practice was renamed Dental Group Stijven in 2014. Lambert is still working in this multidisciplinary practice.

Constantinus PolitisConstantinus Politis is Oral and Maxillo-Facial Surgeon. He is currently Full Professor and Chairperson of the Department of Oral and Maxillofacial Surgery at Leuven University Hospitals, KU Leuven, Belgium. He also holds a master degree in management (MM) from the Applied Economic Sciences at the University of Hasselt and a master degree in Hospital Management (MHM) from the Catholic University of Leuven. He became a recognition as medical specialist in management of health care data. He has been elected as member of the Belgian Royal Academy of Medicine.

M. Enis LeblebiciProf. Enis Leblebici has performed his PhD on the intensification of photo-flow processes. He has then received a Flemish research grant for aerosol photoreactors. Since 2017 his team is developing intensified aerosol chemical process units for various applications from organic synthesis of API precursors to CO2 capture and reutilization units funded by national and international grants of more than 1M€. Prof. Leblebici is also leading a laboratory with advanced aerosol generation and analytics hardware including high-speed microscopic cameras and droplet-light interaction setups.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaerosci.2022.106049.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- Acharya S., Priya H., Purohit B., Bhat M. Aerosol contamination in a rural university dental clinic in south India. International Journal of Integrated Care. 2010;6(1):1–7. doi: 10.3396/ijic.v6i1.003.10. [DOI] [Google Scholar]
- Ahmed W., Jackson M.J., editors. Surgical tools and medical devices. 2nd ed. Springer; 2019. [Google Scholar]
- Akin H., Karabay O., Toptan H., Furuncuoglu H., Kaya G., Akin E.G., Koroglu M. Investigation of the presence of SARS-CoV-2 in aerosol after dental treatment. International Dental Journal. 2021 doi: 10.1016/j.identj.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison J.R., Currie C.C., Edwards D.C., Bowes C., Coulter J., Pickering K., Kozhevnikova E., Durham J., Nile C.J., Jakubovics N., Rostami N., Holliday R. Evaluating aerosol and splatter following dental procedures: Addressing new challenges for oral health care and rehabilitation. Journal of Oral Rehabilitation. 2021;48(1):61–72. doi: 10.1111/joor.13098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASI Dental Specialties Dental chairs. https://asidental.com/asi-elevate-multi-specialty-dental-chair/ from.
- Aymar R.H., Spring S., Weiner E.R. United States Patent Office; 1959. Dental handpiece (patent No. 3,014,278) [Google Scholar]
- Dawson M., Soro V., Dymock D., Price R., Griffiths H., Dudding T., Sandy J.R., Ireland A.J. Microbiological assessment of aerosol generated during debond of fixed orthodontic appliances. American Journal of Orthodontics and Dentofacial Orthopedics. 2016;150(5):831–838. doi: 10.1016/j.ajodo.2016.04.022. [DOI] [PubMed] [Google Scholar]
- Din A.R., Hindocha A., Patel T., Sudarshan S., Cagney N., Koched A., Mueller J.D., Seoudi N., Morgan C., Shahdad S., Fleming P.S. Quantitative analysis of particulate matter release during orthodontic procedures: A pilot study. British Dental Journal. 2020 doi: 10.1038/s41415-020-2280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudding T., Sheikh S., Gregson F., Haworth J., Haworth S., Main B.G., Shrimpton A.J., Hamilton F.W., Ireland A.J., Maskell N.A., Reid J.P., Bzdek B.R., Gormley M. A clinical observational analysis of aerosol emissions from dental procedures. PLoS One. 2022;17(3 March) doi: 10.1371/journal.pone.0265076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Environmental Protection Agency, U. S Indoor air quality. https://www.epa.gov/mold/mold-course-chapter-2 from.
- George M.D., Donley T.G., Pershaw P.M. John Wiley & Sons, Inc; 2014. Ultrasonic periodontal debridement: Theory and technique. [Google Scholar]
- Grenier D. Quantitative analysis of bacterial aerosols in two different dental clinic environments. Applied and Environmental Microbiology. 1995;61(8):3165–3168. doi: 10.1128/aem.61.8.3165-3168.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzman M.I. An overview of the effect of bioaerosol size in coronavirus disease 2019 transmission. The International Journal of Health Planning and Management. 2021;36(2):257–266. doi: 10.1002/hpm.3095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrel K.S., Molinari J. Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. Journal of The American Dental Association. 2004;135(4):429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds W.C. 2nd ed. John Wiley & Sons, Inc; 1999. Aerosol technology: Properties, behavior, and measurements of airborne particles. [Google Scholar]
- Icrp . Annals of the ICPR. Vol. 24. Pergamon; 1994. Human respiratory tract model for radiological protection. Issues 1–3) [PubMed] [Google Scholar]
- Innes N., Johnson I.G., Al-Yaseen W., Harris R., Jones R., KC S., McGregor S., Robertson M., Wade W.G., Gallagher J.E. A systematic review of droplet and aerosol generation in dentistry. Journal of Dentistry. 2021;105 doi: 10.1016/j.jdent.2020.103556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ireland A.J., Moreno T., Price R. Airborne particles produced during enamel cleanup after removal of orthodontic appliances. American Journal of Orthodontics and Dentofacial Orthopedics. 2003;124(6):683–686. doi: 10.1016/S0889-5406(03)00623-1. [DOI] [PubMed] [Google Scholar]
- Juraeva M., Song D.J., Kang D.J. Optimum design of the dental air-turbine handpiece system using the design of experiment method. International Journal of Precision Engineering and Manufacturing. 2020;21(2):265–272. doi: 10.1007/s12541-019-00294-8. [DOI] [Google Scholar]
- KaVO Dental Technologies. (n.d.). User manual Expert torque E680 and Expert torque mini E677.
- Kooij S., Astefanei A., Corthals G.L., Bonn D. Size distributions of droplets produced by ultrasonic nebulizers. Scientific Reports. 2019;9(1):1–8. doi: 10.1038/s41598-019-42599-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kooij S., Sijs R., Denn M.M., Villermaux E., Bonn D. What determines the drop size in sprays? Physical Review X. 2018;8(3) doi: 10.1103/PhysRevX.8.031019. [DOI] [Google Scholar]
- Kun-Szabó F., Gheorghita D., Ajtai T., Hodovány S., Bozóki Z., Braunitzer G., Antal M.Á. Aerosol generation and control in the dental operatory: An in vitro spectrometric study of typical clinical setups. PLoS One. 2021;16(2 February) doi: 10.1371/journal.pone.0246543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labanca M., Azzola F., Vinci R., Rodella L.F. Piezoelectric surgery: Twenty years of use. British Journal of Oral and Maxillofacial Surgery. 2008;46(4):265–269. doi: 10.1016/j.bjoms.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Lang R.J. Ultrasonic atomization of liquids. The Journal of Acustric Society of America. 1962;34(1):6–8. doi: 10.1121/1.1909020. [DOI] [Google Scholar]
- Li G., Chang B., Li H., Wang R., Li G. Precautions in dentistry against the outbreak of corona virus disease 2019. Journal of Infection and Public Health. 2020;13(Issue 12):1805–1810. doi: 10.1016/j.jiph.2020.09.013. Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L., Lu L., Cao W., Li T. Hypothesis for potential pathogenesis of SARS-CoV-2 infection–a review of immune changes in patients with viral pneumonia. Emerging Microbes & Infections. 2020;9(Issue 1):727–732. doi: 10.1080/22221751.2020.1746199. Taylor and Francis Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llandro H., Allison J.R., Currie C.C., Edwards D.C., Bowes C., Durham J., Jakubovics N., Rostami N., Holliday R. Evaluating splatter and settled aerosol during orthodontic debonding: Implications for the COVID-19 pandemic. British Dental Journal. 2021 doi: 10.1038/s41415-020-2503-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmottant P.H., Villermaux E. On spray formation. Journal of Fluid Mechanics. 2004;498:73–111. doi: 10.1017/S0022112003006529. [DOI] [Google Scholar]
- Mectron Medical Technology. (n.d.-a) PIEZOSURGERY insert settings. https://dental.mectron.com/fileadmin/user_upload/dental/general/pdf/manuals/ml_fly_PS_insert_setting.pdf from.
- Mectron. (n.d.-b) PIEZOSURGERY products. https://dental.mectron.com/products/piezosurgery/ from.
- Mectron. (n.d.-c) Piezzosurgery technical specifications. https://dental.mectron.com/products/piezosurgeryr/units/piezosurgeryr-white/ from.
- Micik R.E., Miller R.L., Leong A.C. Studies on dental aerobiology: III. Efficacy of surgical masks in protecting dental personnel from airborne bacterial particles. Journal of Dental Research. 1971;50(3):626–630. doi: 10.1177/00220345710500031801. [DOI] [PubMed] [Google Scholar]
- Micik R.E., Miller R.L., Mazzarella M.A., Ryge G. Studies on dental aerobiology: I. Bacterial aerosols generated during dental procedures. Journal of Dental Research. 1969;48(1):49–56. doi: 10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- Miller R.L., Micik R.E., Abel C., Ryge G. Studies on dental aerobiology: II. Microbial splatter discharged from the oral cavity of dental patients. Journal of Dental Research. 1971;50(3):621–625. doi: 10.1177/00220345710500031701. [DOI] [PubMed] [Google Scholar]
- Mirbod P., Haffner E.A., Bagheri M., Higham J.E. Aerosol formation due to a dental procedure: Insights leading to the transmission of diseases to the environment. Journal of The Royal Society Interface. 2021;18(176) doi: 10.1098/rsif.2020.0967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugele R.A. Maximum stable droplets in dispersoids. AIChE Journal. 1960;6(1):3–8. doi: 10.1002/aic.690060103. [DOI] [Google Scholar]
- Nasr G.G., Yule A.J., Bendig L. Springer-Verlag; 2002. Industrial sprays and atomization: Design, analysis and applications. [Google Scholar]
- Polednik B. Aerosol and bioaerosol particles in a dental office. Environmental Research. 2014;134:405–409. doi: 10.1016/j.envres.2014.06.027. [DOI] [PubMed] [Google Scholar]
- Politis C., Schuermans A., Lagrou K., Putte M.V., Kruth J.-P. Influence of the COVID-19 on dental practive: Why measures to be taken - the experience of an european university hospital (Part 1) Stomatology Eduation Journal. 2020;7(3):163–174. [Google Scholar]
- Politis C., Schuermans A., Lagrou K., Putte M.V., Kruth J.-P. Influence of the COVID-19 on dental practive: Why measures to be taken - the experience of an european university hospital (Part 2) Stomatology Eduation Journal. 2020;7(4):275–285. [Google Scholar]
- Prather K.A., Marr L.C., Schooley R.T., McDiarmid M.A., Wilson M.E., Milton D.K. Airborne transmission of SARS-CoV-2. Science. 2020;370(6514):303–304. doi: 10.1126/science.abe7828. [DOI] [PubMed] [Google Scholar]
- Rajan R., Pandit A.B. Correlations to predict droplet size in ultrasonic atomisation. Ultrasonics. 2001;39(4):235–255. doi: 10.1016/S0041-624X(01)00054-3. [DOI] [PubMed] [Google Scholar]
- Rostami A.A. Computational modeling of aerosol deposition in respiratory tract: A review. Inhalation Toxicology. 2009;21(4):262–290. doi: 10.1080/08958370802448987. [DOI] [PubMed] [Google Scholar]
- Sergis A., Wade W.G., Gallagher J.E., Morrell A.P., Patel S., Dickinson C.M., Nizarali N., Whaites E., Johnson J., Addison O., Hardalupas Y. Mechanisms of atomization from rotary dental instruments and its mitigation. Journal of Dental Research. 2021;100(3):261–267. doi: 10.1177/0022034520979644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Services Scotland N. Assessing the evidence base for medical procedures which create a higher than usual risk of respiratory infection transmission from patient to healthcare worker. 2021. https://www.nipcm.hps.scot.nhs.uk/media/1740/2021-05-14-sbar-medical-procedures-higher-risk-v12.pdf
- Tcharkhtchi A., Abbasnezhad N., Zarbini Seydani M., Zirak N., Farzaneh S., Shirinbayan M. Bioactive materials. Vol. 6. KeAi Communications Co; 2021. An overview of filtration efficiency through the masks: Mechanisms of the aerosols penetration; pp. 106–122. Issue 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells W.F. On air-borne infection: Study II. Droplets and droplet nuclei. American Journal of Epidemiology. 1934;20(3):611–618. doi: 10.1093/oxfordjournals.aje.a118097. [DOI] [Google Scholar]
- Xie X., Li Y., Chawang A.T.Y., Ho P.L., Seto W.H. How far droplets can move in indoor environments-revisiting the Wells evaporation-falling curve. Indoor Air. 2007:211–225. doi: 10.1111/j.1600-0668.2006.00469.x. 2007. [DOI] [PubMed] [Google Scholar]
- Zhang F. United States Patent Office; 2009. Single-use high-speed turbine dental drill handpiece (Patent No. US 2009/0075233 A1) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are presented in the manuscript in the form of graphs. More detailed data are given in Tables in the Appendix. The image files of droplets and the raw data are kept in KU Leuven repository for 5 years after the publication and are going to be shared upon request.