Abstract
Background
Consensus on the treatment of choice for complicated crown fractures of teeth is limited. Recent guidance recommends vital‐pulp‐therapy; however, the preferred type is not specified. Higher success rates for pulpotomy compared to pulp‐capping have been documented, which suggests pulpotomy may be a preferable option for complicated crown‐fractures.
Objectives
The purpose of this systematic review was to determine the success rate of pulpotomy (partial and complete) on teeth that suffered complicated crown fractures. Participants: patients who have suffered a complicated crown fracture to an anterior permanent tooth. Intervention: pulpotomy (partial or complete). Comparator: pulp‐capping or root canal treatment. Outcome: combined clinical and radiographic success at or after 12 months.
Methods
A systematic literature using key search terms was conducted using PubMed, Web of Science and Cochrane‐Central‐Register‐of‐Controlled‐Trials (CENTRAL) as well as a grey literature search from inception to May 2021 and without language restricted to English. Strict inclusion criteria were applied. A standardized tool with defined criteria to assess the risk of bias in each study was used. For non‐randomized comparative trials, the Robins‐I tool was used while the Newcastle‐Ottawa scale was used for non‐comparative non‐randomized studies.
Results
Seven retrospective clinical studies were included. The studies reported high success rates for pulpotomy with overall success ranges for partial or complete pulpotomy ranging from 75% to 96%. One study compared the success rates of pulpotomy to an alternative treatment option pulp capping (90.9% vs. 67%, respectively). Due to the lack of homogeneity in the included studies, a meta‐analysis was not possible.
Discussion
This review highlights the limited evidence based for the current guidance on treatment of complicated crown fractures. The findings of the review indicate high success rates for pulpotomy; however, there is a moderate risk of bias and small sample sizes in the included studies with the result that the overall results should be interpreted with caution.
Conclusion
Within the limitations of this review, the benefits and high success rates reported for partial pulpotomy suggest this procedure, rather than pulp‐capping, should be considered as the treatment of choice for both immature and mature teeth that have suffered complicated crown‐fractures.
Keywords: complicated crown fractures, dental trauma, follow‐up, pulp exposure, pulpotomy, vital pulp therapy
INTRODUCTION
Traumatic dental injuries are frequently encountered in dental practice. The majority of dental trauma to the permanent dentition involves the maxillary central and lateral incisors (Glendor, 2008), most commonly occurring in children with immature or young permanent teeth between the ages of 6 and 12 (Altun et al., 2009; Diaz et al., 2010). Crown fractures which involve pulpal exposure can account for up to a third of all traumatic dental injuries (Altun et al., 2009; Diaz et al., 2010) and the maxillary central incisor is most commonly affected (Maguire et al., 2000).
Treatment of traumatic pulp exposures is challenging for many clinicians as the primary objective should be to select a strategy aimed at maintaining pulp vitality (Fuks et al., 1982). Failure to do so can impose considerable treatment difficulties particularly in immature teeth, when there are thin roots, wide root canals, weak residual dentine and open apices, which can complicate the patient's dental treatment for the rest of their lives (Duggal et al., 2017). It has been reported that root fracture is more likely to occur in immature teeth compared to mature teeth (Andreasen et al., 2002a; Cvek, 1992; Katebzadeh et al., 1998); therefore, even in a young patient with complete root formation, maintenance of pulp vitality should allow the continued deposition of secondary and tertiary dentine in the cervical area, which is likely to reduce the risk of root fracture in later years. In the last decade, due to the advances in knowledge of pulp biology and availability of bioactive materials, pulpotomy has been investigated as a more definitive treatment for mature permanent teeth; however, the bulk of this research focuses on carious mature teeth (Cushley et al., 2019; Li et al., 2019; Zanini et al., 2016). Revitalization and apexification in immature permanent teeth which have pulps that become non‐vital may provide success in the elimination of disease; however, there is evidence to suggest that they do not produce predictable continued root development and the root walls remain thin and prone to fracture (Duggal et al., 2017; Silujjai & Linsuwanont, 2017). There is also limited evidence available to determine whether teeth that have undergone revitalization can be successfully moved orthodontically (Chaniotis, 2018), therefore maintenance of pulp vitality in both immature teeth and mature teeth should be a treatment goal.
The goal of the partial or Cvek pulpotomy (Cvek, 1978) is to remove the coronally inflamed pulp leaving the deeper remaining pulp, which continues to be free from significant inflammatory changes. In animal studies where pulps were mechanically exposed and left untreated, it was found that there was negligible pulpal inflammation in the first few hours after trauma (Cox et al., 1982; Heide & Mjor, 1983) and was confined to the coronal 2–3 mm after 7 days (Cvek et al., 1982). Therefore, in theory, removal of this exposed area of pulp should leave a vital functioning pulp (Fong & Davis, 2002). The advantages of a partial pulpotomy over a complete pulpotomy include the preservation of cell‐rich coronal pulp tissue which provides a better healing potential and continued deposition of dentine in the cervical area, which otherwise could be potentially weak and more prone to fracture (Cvek, 1992).
The severity of the initial injury, extent of pulpal exposure, concomitant luxation injury and time interval between accident and treatment may all play an important role in the healing of the pulp (Andreasen et al., 2002b; Cvek, 1978; Fuks et al., 1982; Oulis & Berdouses, 1996). Root canal treatment is the alternative treatment choice to vital pulp therapy and was the traditional treatment option for mature teeth (ESE, 2006). Guidance published by the European Society of Endodontology (ESE), The International Association of Dental Traumatology (IADT) and the American Academy of Paediatric Dentistry (AAPD) currently indicate that complicated (i.e. exposure of pulp) crown fractures of mature and immature permanent teeth should be treated by a vital pulp therapy, which includes pulp capping or pulpotomy (AAPD, 2014; Bourguignon et al., 2020; ESE, 2021). However, some studies have suggested a higher rate of pulpal necrosis for those teeth treated by pulp capping compared to pulpotomy (Fuks et al., 1982; Hecova et al., 2010; Wang et al., 2017). In a retrospective observational study, it was reported that the rate of pulp necrosis was three‐fold higher with pulp capping (45.5%) compared to partial pulpotomy (13.6%) over a 5‐year period (Hecova et al., 2010). Similarly, in a study by Wang et al. (2017), the rate of pulp necrosis following treatment of 375 teeth with a complicated crown fracture was significantly higher in teeth, which were treated with pulp capping compared to both partial and complete pulpotomy. Over half (57.1%) of the pulps which had been treated by pulp capping became necrotic compared to 10.1% for partial pulpotomy, 9.8% for coronal pulpotomy and 6.1% for retreatment by pulpotomy after a direct pulp cap.
In general, the knowledge on the most appropriate treatment for dental trauma amongst dentists is limited (Kostopoulou & Duggal, 2005). Despite the recommendation that especially in immature teeth, the maintenance of pulp vitality is essential, pulp extirpation is often provided as an emergency treatment. In an observational study (Jackson et al., 2006) that examined the treatment provided to 73 teeth of 68 patients who were referred to Newcastle Dental Hospital, UK, 37 were immature incisors. The authors reported that pulp extirpation was the initial treatment provided in 44% of these cases with the majority of this management occurring outside the hospital setting. Whilst the IADT (Bourguignon et al., 2020) recommend either a pulp cap or a partial pulpotomy as the treatment of choice the ESE (2021) recommend partial pulpotomy for large exposures and when there is a treatment delay and pulp capping for minor exposures within the first hours after trauma. It can be particularly difficult for dental professionals to choose the most appropriate treatment for complicated crown fractures because even when the primary goal for all teeth is maintenance of pulp vitality, the rationale for the choice of one approach (pulp capping) over the other (pulpotomy) in the current guidelines is questionable.
Since the recent literature has suggested a greater incidence of pulpal necrosis following direct pulp capping compared to partial and complete pulpotomy (Wang et al., 2017) and long‐term success of partial pulpotomies has been demonstrated in both mature and immature teeth (Fuks et al., 1993), a question must be raised as to whether pulpotomy should be the preferred treatment option for all pulps of teeth which have undergone complicated crown fractures.
There are no previous systematic reviews examining whether pulpotomy (partial or complete) is an appropriate treatment choice for both mature and immature permanent teeth following complicated crown fractures. The main objective of this review was to determine the success rate of pulpotomy (partial or complete) in the treatment of pulps associated with complicated crown fracture for mature and immature teeth. An additional aim was to evaluate whether pulpotomy is as successful as either pulp capping or root canal treatment for the treatment of pulps associated with complicated crown fractures.
METHOD
This systematic review was registered in PROSPERO (number CRD42021255689) and followed the PRISMA guidelines (Preferred Reporting Items for Systematic reviews and Meta‐Analyses) using the PICOTS (Population, Intervention, Comparison Outcome, Duration of Data collection, Study types included) framework to investigate the following clinical questions: ‘What is the success rate of pulpotomy in permanent teeth which have had a traumatic complicated crown fracture and what is the success rate of pulpotomy compared with pulp capping or root canal treatment in that scenario?’. Where in relation to the PICOTS framework: P = Patients with a complicated crown fracture of an immature or mature permanent anterior tooth as a result of a trauma. I = Pulpotomy (complete or partial), C = Root canal treatment including apexification/apical plug procedures or pulp capping. O = Critical outcomes were the absence of pain, swelling or other clinical symptoms as well as radiographic absence of periapical area or change suggestive of apical periodontitis. Important (secondary) outcomes were tooth discolouration, response to pulp sensibility testing, root‐end closure, cost effectiveness, radiographic evidence of a hard tissue bridge, patient and operator satisfaction, initial restoration and maintenance of coronal restoration. T = a minimum of 12 months and maximum of as long as possible for all outcome measures. S = is human experimental studies (Randomized Control Trials, Non‐randomized Comparative Clinical trials [CCTs] − non‐randomized). The search was supplemented by longitudinal observational studies (retrospective and prospective comparative cohort and case‐control studies as well as single‐arm studies) to ensure that all relevant clinical information that is often not tested in experimental studies was captured (Liberati et al., 2009; Nagendrababu et al., 2019).
Information sources and search strategy
The search strategy is outlined in Figure 1. A systematic literature using key search terms was conducted using PubMed, Web of Science and Cochrane Central Register of Controlled Trials (CENTRAL), from inception to May 2021 and without language restricted to English. Searches were conducted using a variety of MeSH terms or keywords which included: pulpotomy, dental pulp exposure, dental trauma, complicated crown fracture, traumatic pulp exposure, vital pulp therapy. A detailed search strategy carried out using MeSH terms on the PubMed database is outlined in Table S1. To identify conference papers, and other grey literature, additional searches were performed with the same search terms using Google Scholar (first 50 returns) and available repositories (e.g. Networked Digital Library of Theses and Dissertations, Open Access Theses and Dissertations, DART‐Europe E‐theses Portal – DEEP, Opening access to UK theses – EThOS). Reference lists of included trials and observational studies were also analysed to assure the reliability of data collected.
FIGURE 1.
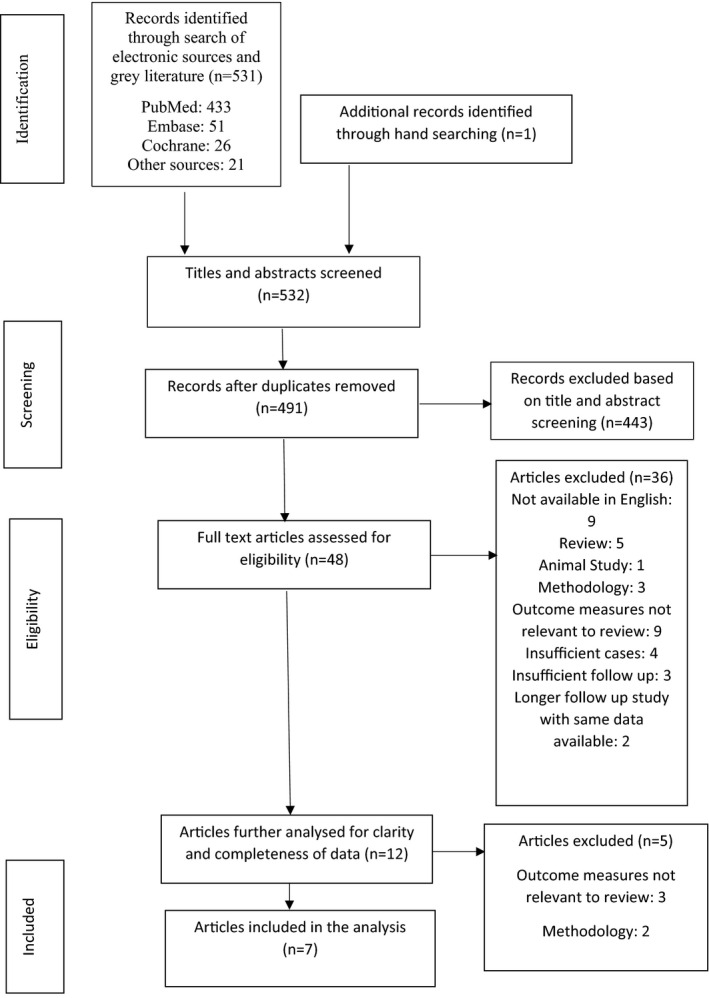
The PRISMA flow diagram details the search and selection process applied during our systematic literature search
Study selection process
The following inclusion criteria were established for studies to be eligible for this systematic review:
Human experimental studies (Randomized Control Trials, Non‐randomized Comparative Clinical trials [CCTs]). The search was supplemented by longitudinal observational studies (retrospective and prospective comparative cohort and case‐control studies as well as single‐arm studies).
Patient's with mature or immature permanent incisors, which had a complicated crown fracture (i.e. exposure of pulp) following a trauma.
Complete or partial coronal pulpotomy carried out on a permanent incisor tooth with a vital pulp no longer than 3 weeks following the initial trauma.
In comparative studies, either pulp capping or root canal treatment as the comparative treatment, which could include apexification or apical plug procedures.
Studies reporting clinical, radiographic or overall success rates with at least 12 months follow‐up.
Radiographic success was established as no abnormality suggestive of apical periodontitis (i.e. apical radiolucency or emerging breakdown of lamina dura) and continued root formation if tooth was immature.
Clinical success was defined as an absence of clinical symptoms (e.g. pain, discomfort, swelling) or the patient was described as remaining asymptomatic after treatment.
Secondary outcomes were also examined such as impact of time interval to treatment, impact of pulpotomy medicament, tooth discolouration, pulp vitality, root‐end closure, economic evaluations, dentine bridge formation, patient and operator satisfaction and success of coronal restoration.
Studies were excluded if they:
Examined primary teeth or involved permanent teeth with pulp exposures due to caries.
Did not specify whether pulp exposure was due to caries or trauma.
Had fewer than 10 cases in their outcome results.
Did not specify whether teeth were anterior or posterior.
Two reviewers independently carried out the literature screening process and a third reviewer resolved any disagreements. Full text assessments were then performed on the screened articles prior to a final decision on eligibility and acceptance for inclusion in this systematic review.
Data collection
The included papers were assessed and the following data were collected from each study and collated into a spreadsheet: study characteristics (country and year of publication), name of journal, type of study, number and demographics of the participants, diagnosis (pulpal, trauma, periapical), root maturity, intervention, time from injury to intervention, pulp medicament material (which refers to any material directly applied to the pulp), type of restoration, follow‐up period, number lost to follow‐up, funding source and final clinical and radiographic outcomes. In studies reporting mixed data (traumatic and carious pulpal exposures), only data that were relevant to the inclusion criteria (traumatic exposure and had follow‐up of at least 12 months) could be extracted were included and if this was not identifiable the study was excluded.
Quality evaluation
A standardized tool with defined criteria to assess the risk of bias in each study was used (Nagendrababu et al., 2020) and each study was assessed by the two independent reviewers who conducted the literature search. For non‐randomized comparative trials, the Robins‐I tool was used (Sterne et al., 2016). Each study in this category was assessed in each of the seven domains. A study was categorized as a low risk of bias if the following occurred:
Confounding: No confounding is expected when the confounding factors are controlled in the design (e.g. concomitant luxation injury).
Selection of the participants into the study: When the patients were recruited from different places or dental clinics.
Classification of intervention: When the treatment provided was well defined for each group.
Deviations from intended intervention: After initial treatment provided, both groups received no further intervention during the follow‐up period.
Missing data: When all the participants of the study were included in the data provided.
Measurement of outcomes: When clinical and radiographic follow‐up examination were carried out by a blinded examiner.
Selection of reported results: When all data involved in assessment of success was provided.
An overall risk of bias was then assigned to each study depending on the results of the seven domains.
For non‐comparative non‐randomized studies, the quality of each study was assessed in accordance with the Newcastle‐Ottawa scale (NOS; Wells et al., 2019). The NOS scale contains eight items within three domains and the total maximum score is 9. A study with a score from 7 to 9 was considered a low risk of bias whilst 4–6 was moderate risk and 0–3 very high risk of bias. Disagreements during the review were discussed and resolved by a third reviewer.
Data synthesis
Considering the discrepancies in standardization and heterogeneity of each of the included studies, a meta‐analysis was not possible. The success rate for pulpotomy or comparative treatment intervention was calculated for each study by dividing the number of successful cases by the total number of cases during a specific time period.
RESULTS
Included studies
In total, 491 articles were screened by two assessors after duplicates were removed. Of these 491, 48 studies were deemed relevant and a full text evaluation of each was carried out by each assessor independently in accordance with the preferred reporting of systematic reviews (PRISMA‐P 2016).
Forty‐one articles were then excluded. The detailed reasons for exclusions are outlined in Table 1. Two studies had different time points using the same primary data from two previous prospective clinical trials so the earlier study in each case was excluded (Cvek, 1978, 1993; Fuks et al., 1987, 1993). A total of seven studies were included in the final review.
TABLE 1.
Reasons for exclusion
| Reason for exclusion | Number of articles | Author(s), year |
|---|---|---|
| Not available in English | 9 | Ortiz 1973, Ravn 1973, Ravn 1974, Wojnar‐Kalina 1979, Sluka et al., 1981, Ravn 1982, Dabrowska et al., 1997, Bai et al., 2011, Wang et al., 2011 |
| Review article | 5 | Gutmann & Heaton 1981, Garcia‐Godoy & Murray 2012, Bimstein & Rotstein 2016, Bjorndal et al., 2019, Chen et al., 2019 |
| Pulp examined histologically only after pulpotomy | 1 | Cvek & Lundberg 1983 |
| Single case description | 1 | Patterson 1967 |
| Animal study | 1 | Chiang et al., 2016 |
| Did not specify if exposure due to caries or trauma | 2 | Ehrmann 1981, Boltacz‐Rzepkowska & Pawlicka 2003 |
| Did not provide overall clinical and radiographic success | 1 | Abuelniel et al., 2020 |
| Not all teeth included in results were examined clinically and radiographically | 1 | de Blanco 1996 |
| Results of pulp capping and pulpotomy not separate | 1 | Robertson et al., 2000 |
| Specific number of successful cases not given | 1 | Blanco & Cohen 2002 |
| Did not satisfy inclusion criteria for clinical success | 5 | Magnusson et al., 1969, Yilmaz et al., 2010, Jackson et al., 2006, Wang et al., 2017, Witherspoon et al., 2017 |
| Did not specify which teeth were included | 1 | Kunert et al., 2015 |
| Study did not include clinical follow‐up | 3 | Winter 1977, Gelbier & Winter 1988, Maguire et al., 2000 |
| Insufficient cases of traumatized teeth (per inclusion criteria) | 4 | El‐Meligy & Avery 2006, Yilmaz et al., 2008, Witherspoon et al., 2006, Kang et al., 2017 |
| Inadequate follow up time of less than 12 months | 3 | Oulis & Berdouses 1996, Viduskalne & Care 2010, Haikal et al., 2020 |
| Subsequent follow‐up study with longer follow up time available | 2 | Cvek 1978, Fuks et al., 1987 |
Included study characteristics
Included study and population characteristics are shown in Tables 2 and 3. All seven included studies were retrospective clinical studies. Five studies had one study group examining pulpotomy only (Caprioglio et al., 2014; Cvek, 1993; Fuks et al., 1993; Klein et al., 1985; Xu, 2016). Two of the studies were comparative and had two clinical groups; Fuks et al. (1982) compared complete pulpotomy to pulp capping and Rao et al. (2020) compared two different materials (iRoot BP Plus and Calcium Hydroxide (CH)) for use in pulpotomy. Six of the studies examined partial pulpotomy (Caprioglio et al., 2014; Cvek, 1993; Fuks et al., 1993; Klein et al., 1985; Rao et al., 2020; Xu, 2016) whilst Fuks et al. (1982) examined complete pulpotomy. All studies combined clinical and radiographic success, whilst Rao et al. (2020) separated the two variables. The follow‐up of the participants ranged from 3 months to 15 years but only results with at least 12 months follow‐up were included in the systematic review.
TABLE 2.
Included study characteristics
| Author | Study design | Location | Follow up | Intervention | Comparator | Outcome | Funding | Level of evidence |
|---|---|---|---|---|---|---|---|---|
| Caprioglio et al., 2014 | Retrospective single arm clinical trial | Italy | 3–42 months | Partial pulpotomy | NA | Clinical and radiographic | NA | 2b |
| Cvek 1993 | Retrospective single arm clinical trial | Sweden | 3–15 years | Partial pulpotomy | NA | Clinical and radiographic | NA | 2b |
| Fuks et al., 1982 | Retrospective double arm clinical trial | Israel | 3–36 months | Complete pulpotomy | Direct pulp cap | Clinical and radiographic | NA | 2b |
| Klein et al., 1985 | Retrospective single arm clinical trial | Israel | 3–36 months | Partial pulpotomy | NA | Clinical and radiographic | NA | 2b |
| Fuks et al., 1993 | Retrospective single arm clinical trial | Israel | 7.5–11 years | Partial pulpotomy | NA | Clinical and radiographic | NA | 2b |
| Xu 2016 | Retrospective single arm clinical trial | USA | 1 year | Partial pulpotomy | NA | Clinical and radiographic | NA | 2b |
| Rao et al., 2020 | Retrospective double arm clinical trial | China | 1–5years | Partial pulpotomy with iRroot BP Plus | Pulpotomy with CH | Clinical and radiographic | Supported by grants from the Natural Science Foundation of China | 2b |
TABLE 3.
Population characteristics
| Author | No. of patients receiving treatment | No. of teeth treated | Gender M:F | Age (years) | Tooth maturity | Pulpotomy material | Restoration | Follow up (months) | Lost to follow up |
|---|---|---|---|---|---|---|---|---|---|
| Caprioglio et al., 2014 | 26 | 27 | Unknown | 8.3 | All immature | MTA | Temporary cement (unspecified) and a composite restoration | 35.1 | 0 at 24 months |
| Cvek 1993 | 162 | 209 | Unknown | 6–17 a | 90 immature 88 mature | CH | ZOE cement and composite later | 36–180 | 31 at 3 years |
| Fuks et al., 1982 | 72 | 76 b | Unknown | 7–14 a | 38 immature 38 mature | CH | ZOE and unspecified restoration usually amalgam | 6–36 | 22 c at 3 years |
| Klein et al., 1985 | 33 | 34 | 21:12 | 7–22 | Unknown distribution | CH | Composite or stainless steel basket crowns | 3–36 | 20 at 13 months |
| Xu 2016 | 70 d | 70 d | Unknown | Unknown | Unknown | CH | Unknown | 12 months | 58 e |
| Fuks et al., 1993 | 62 | 63 f | 35:27 | 7–22 a | Unknown distribution | CH | ZOE and composite or stainless‐steel metal basket crown | 6–132 | 19 at 7.5 years |
| Rao et al., 2020 | 168 | 205 g | Group 1 59:18 | Group 1 9 ± 1.1 | Group 1 62 immature & 43 mature | Group 1root BP, Group 2 | Ketac cement and composite or fragment reattachment | 17.5 ± 4.4 | 50 at 1 year |
| Group 2 65:26 | Group 2 9.1 ± 1.3 | Group 2 66 immature & 34 mature | CH |
Age range as mean age not provided.
Total 76 teeth, 38 immature teeth received pulpotomy and 38 mature teeth received direct pulp cap.
17 in mature group pulp capping group and five in immature group pulpotomy group.
Number of cases treated under 12 h as those over 12 h had unspecified time to treatment so were excluded from the results for this review.
Number of cases treated under 12 h that were lost to follow up.
Figures taken from cross reference to earlier study by Fuks et al. (1987).
Total 205 cases split into two groups after 55 excluded due to failure to attend 12‐month review: group 1 pulpotomy completed with Iroot BP Plus and group 2 pulpotomy completed with CH.
Quality assessment
Five studies were single‐arm cohort studies and assessed using the NOS scale (Table 4; Caprioglio et al., 2014; Cvek, 1993; Fuks et al., 1993; Klein et al., 1985; Xu, 2016). Rao et al. (2020) was also assessed using the NOS scale, as although it was a double‐armed study, only one treatment partial pulpotomy was examined and the comparative groups only applied to the medicament used. Five of these studies were deemed to have a moderate risk of bias whilst the study by Rao et al. (2020) was deemed to have a low risk of bias. One study was a non‐randomized comparative trial and was assessed according to the Robins‐I tool (Table 5) and had a moderate risk of bias (Fuks et al., 1982). The level of evidence provided by each included study (Caprioglio et al., 2014; Cvek, 1993; Fuks et al., 1982, 1993; Klein et al., 1985; Rao et al., 2020; Xu, 2016) was categorized as 2b according to the Oxford Centre for Evidence‐Based Medicine (2009; Table 6).
TABLE 4.
Risk of bias assessment using the Newcastle‐Ottawa Scale for Cohort study
| Study | Selection cohort representative (1 a ) | Selection of non‐exposed cohort (1 a ) | Selection exposure ascertained (1 a ) | Selection outcome of interest not present at start (1 a ) | Comparability (2 a ) | Outcome independent (1 a ) | Outcome follow up (1 a ) | Outcome subjects (1 a ) | Stars (out of 9) | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|
| `Caprioglio et al., 2014 | a | Not described | Surgical records a | a | No controls | Not blinded | a | Complete follow up | 5 | Moderate |
| Cvek 1993 | a | Not described | Surgical records a | a | No controls | Not blinded | a | a Subjects lost no Description | 4 | Moderate |
| Klein et al., 1985 | a | Not described | Surgical records a | a | No controls | Not blinded | a | Subjects lost no description | 4 | Moderate |
| Fuks et al., 1993 | a | Not described | Surgical records a | a | No controls | Not blinded | a | Subjects lost no description | 4 | Moderate |
| Xu 2016 | a | Not described | Surgical records a | a | No controls | Not blinded | a | Subjects lost no description | 4 | Moderate |
| Rao et al., 2020 | a | Not described | Surgical records a | a | Some controlled factors a | a | a | Complete follow up a | 7 | Low |
Newcastle‐Ottawa Scale contains 8 items within 3 domains and the total maximum score is 9. A study with score from 7 to 9, has high quality, 4 to 6, high risk, and 0 to 3 very high risk of bias.
The appraisal was based on the 1 or 2 stars assessed within the selection domain, and 2 stars in comparability and outcome domain.
TABLE 5.
Quality assessment of the non randomized studies according to Robins‐I tool
| Study | Baseline confounding | Selection of participants | Classification of intervention | Deviation from intended intervention | Missing data | Measurement of outcomes | Selection of reported results | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|
| Fuks et al., 1982 | High | Moderate | Low | Low | Moderate | High | Low | Moderate |
TABLE 6.
Oxford centre for evidence‐based medicine‐levels of evidence employed in this study
| Level | Therapy/Prevention, Aetiology/Harm |
|---|---|
| 1a | SR (with homogeneity) of RCTs |
| 1b | Individual RCT (with narrow Confidence Interval) |
| 1c | All or none |
| 2a | SR (with homogeneity) of cohort studies |
| 2b | Individual cohort study (including low quality RCT; e.g. <80% follow‐up) |
| 2c | ‘Outcomes’ Research; Ecological studies |
| 3a | SR (with homogeneity) of case‐control studies |
| 3b | Individual Case‐Control Study |
| 4 | Case‐series (and poor‐quality cohort and case‐control studies) |
| 5 | Expert opinion without explicit critical appraisal, or based on physiology, bench research or ‘first principles’ |
Overall pulpotomy success rate
Table 7 shows the success rates of pulpotomy recorded at the first observation period after 12 months from the included studies. Several studies did not record data at exactly 12 months and some included the participants who were followed up before 12 months in their success rates, so the closest data recorded following 12 months was outlined for each study. All failures recorded up to as well as within the documented observation period were included in these results. Those studies which included successful results recorded before 12 months were not included. This allows the most accurate overall success rate for pulpotomy with at least 12 months follow‐up. The observation periods varied between studies so the average overall success rate across all studies could not be determined at any specific time period. Due to the heterogeneous nature of the data, a meta‐analysis was not possible.
TABLE 7.
Pulpotomy success rates ≥12 months
| Author | Number receiving intervention | Observation period (months) | Number available at follow‐up | Failures % (n) | Calculated % success (n) | Mature success % (n) | Immature success % (n) |
|---|---|---|---|---|---|---|---|
| Caprioglio et al. (2014) | 27 | 24–42 | 27 | 0 | 85.1 (23) a | 0 (0) | 85.1 (23) |
| Cvek (1993) | 209 | 36 | 178 | 5 (9) | 95 (169) | 93.75 (90) | 96.70 (88) |
| Fuks et al. (1982) | 38 | 12–36 | 33 | 7.9 (3) | 90.9 (30) | 0 (0) | 90.9 (30) |
| Klein et al. (1985) | 34 | 13–36 | 14 | 14.29% (2) | 85.7% | Unknown | Unknown |
| Xu (2016) | 70 | 12 | 12 b | 25% (3) | 75% (9) | Unknown | Unknown |
| Fuks et al. (1993) c | 63 | 13–50 | 39 | 10.25 (4) | 89.74 (35) | NA | NA |
| Rao et al. (2020) | 255 | 12–24 | 205 | 4 (8) | 96 (197) | 97.4 (75) | 95.3 (122) |
Combined healed and healing results as criteria for healing falls under successful criteria for this systematic review.
Only cases which were included in specified time to treat time period of <12 h were included.
Data taken from earlier study in series Fuks et al. (1987).
The studies reported high success rate for pulpotomy with overall success ranges for partial pulpotomy ranging from 75% to 96% (Caprioglio et al., 2014; Cvek, 1993; Fuks et al., 1993; Klein et al., 1985; Rao et al., 2020; Xu, 2016). Only one study examined complete pulpotomy on immature teeth only which recorded a success rate of 90.9% at or after 12 months (Fuks et al., 1982). All studies combined radiographic and clinical success except Rao et al. (2020) who separated clinical and radiographic success. Their results were recorded as 100% clinical and 99% radiographic success for the iRoot BP Plus group compared to 94% clinical and 93% radiographic success for the CH group, respectively. This combined to an overall success rate of 99% in the iRoot BP Plus group and 93% in the CH group. This gave an overall success rate for partial pulpotomy of 96% for both groups combined.
Table 8 shows the success rates documented in studies with longer follow‐up periods after those recorded in Table 7. The success rates are high as most failures were recorded prior to these observation periods and were therefore not included. Cvek (1993) recorded all failures (n = 9) within the first 36 months giving a success rate of 95% at this time. This success rate increased to 100% in all subsequent observation periods. Fuks et al. (1982) documented three failures and two of them occurred prior to 6 months so the success rate increased from 90.9% to 93.3%. Fuks et al. (1993) did not recall four failures in their follow‐up study. These failures occurred 6 months after treatment, so are not included in their success/failure rates. However, there were a greater number of patients available for follow‐up overall in the later observation period with 39 available at 13–50 months and 40 available at 90–132 months. The success rate dropped from 89.74 to 87.5%.
TABLE 8.
Success rates in studies with further recorded observation periods
| Author | Number receiving intervention | Observation period (months) | Number available at follow up | Failures % (n) | Calculated % success (n) | Mature success % (n) | Immature success % (n) |
|---|---|---|---|---|---|---|---|
| Fuks et al. (1982) | 38 | ≥36 | 15 a | 6.6 (1) | 93.3 (14) | 0 (0) | 93.3 (14) |
| Fuks et al. (1993) | 63 | 90–132 | 40 b | 12.5 (5) a | 87.5 (35) | NA | NA |
| Cvek (1993) | 178 | 37–72 | 162 c | 0 | 100 (162) | 100 (84) | 100 (78) |
| Cvek (1993) | 178 | 73–108 | 85 c | 0 | 100 (85) | 100 (43) | 100 (42) |
| Cvek (1993) | 178 | 109–114 | 52 c | 0 | 100 (52) | 100 (27) | 100 (25) |
| Cvek (1993) | 178 | 145–180 | 29 c | 0 | 100 (29) | 100 (12) | 100 (17) |
2 patients diagnosed as failure in first 6 months not included.
4 further patients were diagnosed with pulpal necrosis within 6 months of treatment and were not recalled so are not included in data for this study.
6 patients diagnosed as failure in first 36 months not included in data for this study.
Pulpotomy versus comparative treatment option
Only one study compared pulpotomy with an alternative treatment option. Fuks et al. (1982) compared complete pulpotomy to pulp capping. All the participants in the pulp capping group had mature teeth and all the participants in the complete pulpotomy group had immature teeth. There were 38 cases in each group and at the 12–23‐month observation period, there were seven failures in the pulp capping group (33%) and three failures in the pulpotomy group (9.1%). It is specified in the study that two failures in the pulpotomy group occurred within 6 months. The third failure which was classified as pulp canal obliteration (PCO) with no periapical pathosis was not categorized into a specific time period. All failure cases in the pulp capping group occurred before 12 months. There were high numbers lost to follow up in this study with 17 cases not followed up after 11 months in the pulp capping group and five in the pulpotomy group. There were no studies identified which directly compared pulpotomy with root canal treatment.
Success rates with stage of root maturity
There were two studies that examined whether success rates were affected by root maturity (Cvek, 1993; Rao et al., 2020) and the results of these can be seen in Tables 7 and 8. The success rates ranged between 93.75% and 97.4% for mature teeth and 95.3%–96.7% for immature teeth. Both studies found that there was no significant difference between partial pulpotomy success rates for mature and immature teeth. Two studies used immature teeth only for pulpotomy (Caprioglio et al., 2014; Fuks et al., 1982) with Fuks et al. (1982) using mature teeth for the comparison pulp capping group. The remaining three studies examined both mature and immature teeth but the results suitable for the purposes of this systematic review were not categorized according to root maturity (Fuks et al., 1993; Klein et al., 1985; Xu, 2016).
Success rates and time interval to treatment
There were five studies which examined whether success rates corresponded to time interval from injury to time of treatment (Cvek, 1993; Fuks et al., 1982, 1993; Klein et al., 1985; Xu, 2016) and the results are outlined in Table 9. Xu (2016) separated the results according to time interval to treatment; however, only those results available for cases treated within 12 h of trauma were extracted for this systematic review as there was no defined maximum time interval for those treated at an interval greater than 12 h. These cases were excluded as they did not satisfy the inclusion criteria for the review of a time interval to treatment of less than 3 weeks so are not included in Table 9.
TABLE 9.
Time interval to treatment
| Study | Observation period (months) | Number available at follow up period | Medicament | Success rate: time interval to treatment <24 h % (n) | Success rate: time interval to treatment 25–72 h % (n) | Success rate: time interval to treatment >72 h % (n) | Overall success rate % (n) |
|---|---|---|---|---|---|---|---|
| Cvek (1993) | 36 | 178 | CH | 95.65 (132) | 95.83 (23) | 87.5 (14) | 95 (169) |
| Fuks et al. (1982) | 12–36 months | 33 | CH | 100 (21) | 50 (3) a | 100 (8) b | 90.9 (30) |
| Klein et al. (1985) | 12–36 months | 14 | CH | 77.7 (7) | 100 (5) c | ||
| Fuks et al. (1993) | 90–132 | 40 d | CH | 90.9 (30) | 66.6 (4) c | 100 (1) e | 87.5 (35) |
Time interval 2–6 days.
Time interval >6 days.
Time interval to treatment 25–96 h.
4 patients who had pulp necrosis within 6 months of treatment were not recalled for this recall and of these four patients 2 were treated within 24 h, one was treated between 1 and 4 days and one was treated after 4 days.
Time interval greater than 96 h.
Cvek (1993) reported that there was a numerical difference relating to success rates when the time interval to treatment was considered, with the success rate dropping from 95.83% before 72 h to 87.5% over 72 h; however, the difference was not significant. Only five teeth were treated after 24 h in the study by Fuks et al. (1993) and the success rate dropped from 90.9% within 24 h to 66.6% for treatment provided between 25 and 96 h; however, the participant numbers were small and the authors did not investigate if this difference was significant. There was also a numerical decrease in the success rates after a 24‐h treatment interval in the study by Fuks et al. (1982). However, this number was also not statistically significant and the eight teeth that were treated after 6 days were all deemed successful at their reviews, five of which were followed up for at least 36 months. Rao et al. (2020) outlined the time intervals to treatment which ranged between less than 24 h to greater than 72 h, for both the CH and iRoot BP Plus pulpotomy groups and reported there was no significant difference between the groups; however, they did not correlate whether time interval was significant in relation to the overall success rate. Klein et al. (1985) had only five results available of cases treated with an interval from trauma of more than 24 h with at least a 12‐month follow‐up; however, all of these cases were deemed successful.
Studies comparing different medicaments
Five studies used CH as the only pulp medicament (Cvek, 1993; Fuks et al., 1982, 1993) and one study used Mineral Trioxide Aggregate (MTA; Caprioglio et al., 2014). Only one study was identified that compared the success rates of medicaments which were CH and iRoot BP Plus (Rao et al., 2020). The overall success rate of the CH group was 93% compared to 99% in the iRoot BP Plus group, this difference was statistically significant. The overall success rate after 12 months in the study by Caprioglio et al. (2014) which used MTA was 81.5% compared to success rates ranging from 89.74% to 94% in those studies that used CH (Cvek, 1993; Fuks et al., 1982, 1993; Klein et al., 1985; Xu, 2016).
Secondary outcomes
In four studies, a positive electric pulp test (EPT) was necessary criteria for a successful outcome (Cvek, 1993; Fuks et al., 1982, 1993; Klein et al., 1985). Caprioglio et al. (2014) used a physiological response to thermal testing as successful criteria whilst Rao et al. (2020) used EPT as a reference to verify clinical failure when teeth showed other signs or symptoms. No study outlined the exact numbers of positive or negative responses to pulp sensibility tests in their follow‐up.
In five studies, evidence of dentine (or mineralized) bridge formation was also a defined criterion for success (Cvek, 1993; Fuks et al., 1982, 1993; Klein et al., 1985; Xu, 2016) Rao et al. (2020) assessed the presence of a dentine bridge in all cases and reported that dentine bridges were radiographically observed in 92.3% and 90.3% of the successful cases in the iRoot BP Plus and CH groups and in 100% and 85.7% of the failed cases, respectively. PCO was considered a successful outcome in Rao et al. (2020) but considered a failure in the studies by Fuks et al. (1982) and Cvek (1993). The remaining two studies did not specifically mention it in their criteria or results.
No study recorded secondary outcomes of discolouration, success of coronal restoration, patient or operator satisfaction or economic evaluations so these outcomes could not be assessed.
DISCUSSION
There is a growing evidence base available from multiple systematic reviews that demonstrates high success rates for molar teeth that have been treated by pulpotomy due to carious pulp exposures or resulting pulpitis (Cushley et al., 2019; Elmsmari et al., 2019; Li et al., 2019). However, there is a paucity of literature available in relation to the success rates of pulpotomy in teeth which have had traumatic exposures due to complicated crown fractures and, there are no published systematic reviews assessing this outcome. Within this review there were only seven studies which satisfied the inclusion and exclusion criteria and unfortunately none of these were randomized controlled trials. The seven included studies varied in number of the participants, pulp medicament, length of follow‐up, outcome measures and stage of maturity of teeth but all included patients that had undergone either partial or complete pulpotomy after a complicated crown fracture. The overall quality of the included studies was assessed as being moderate with six studies (Caprioglio et al., 2014; Cvek, 1993; Fuks et al., 1982, 1993; Klein et al., 1985; Xu, 2016) recorded as having a moderate risk of bias and one study by Rao et al. (2020) being categorized as low risk in the assessment scale. This highlights that the strength of recommendation is moderate and caution must be exercised in extrapolating the results of the included studies and findings of the review.
One strength of the current systematic review is the strict inclusion and exclusion criteria used. However, many of the original studies included follow‐up results which were recorded less than 12 months after the intervention and although these were excluded from the results of this systematic review, it resulted in two studies having a reduced sample size (14 and 33 cases, respectively; Fuks et al., 1982; Klein et al., 1985). Xu (2016) also had a small sample size of 12 as only cases which were treated within 12 h of the trauma were included. The lack of standardized follow‐up times in the included studies meant direct comparison and pooling of results was impossible. It would be recommended that future studies ensure follow‐up of at least 12 months with larger sample sizes to allow adequate pooling of results and increase the strength of evidence available. The range of included study designs is a limitation of this review as it includes both retrospective and non‐comparative single‐arm studies, which are of a lower quality of evidence and limits comparison. These study designs were included after an initial pilot literature search had highlighted that there was insufficient comparative evidence in this area.
The nature of these procedural interventions (partial or complete pulpotomy or pulp capping) makes it difficult to completely blind the operator or the assessor at treatment or follow‐up, which implicates all studies in both performance and detection bias. Rao et al. (2020) was the only study that attempted to blind the assessors when examining follow‐up radiographs. Caprioglio et al. (2014) used patients in private endodontic practice whilst Xu (2016) examined patients in an emergency clinic as well as a separate dental clinic in a nationwide children's hospital, all other studies used patients who had attended specialist pedodontic departments. The use of a subpopulation means there is a potential selection bias and reduced external validity where subjects are selected from referral only patients and the results may not be reflective of the general population such as those presenting to general dental practice.
The findings of the review found an encouraging outcome for partial and complete pulpotomy in both mature and immature teeth, which had suffered complicated crown fractures with the overall success rate ranging from 75% to 96.7% with a minimum 12 month follow‐up period. Only one study examined complete pulpotomy which had a success rate of 90.9% (Fuks et al., 1982). Fuks et al. (1993) included four failures which were recorded in a preceding study (Fuks et al., 1987) but not in the follow‐up study, which led to a slightly higher success rate being recorded. There are considerable advantages to pulpotomy over pulpectomy for mature teeth as it is less invasive and technically simpler and does not take up as much time for patient or operator (Cushley et al., 2019). A shorter time for appointments has a big advantage in the treatment of children, who are most commonly affected by complicated crown fractures, as this may increase compliance (Alqaderi et al., 2014). Maintenance of pulp vitality also preserves the protective mechanisms of the pulp‐dentinal complex and in partial pulpotomy allows continuous deposition of dentine in the cervical area to reduce the risk of root fracture. The standard of root canal treatment in the general population has also being found to be low with a high incidence of periapical disease amongst root‐treated teeth (Saunders et al., 1997), so a more conservative alternative than root canal treatment which is technically simpler would be a better option. Despite these advantages, until recently, the choice of treatment for complicated crown fractures is most commonly root canal treatment in mature teeth (Hecova et al., 2010; Jackson et al., 2006).
Only one study directly compared pulpotomy (complete) to a treatment alternative, which was pulp capping and the success rate was significantly higher for pulpotomy (90.9% vs. 66.1%; Fuks et al., 1982). However, the pulpotomy cases were performed on immature teeth whilst all pulp capping cases were performed in mature teeth. The treatment allocation is not random in this case and with the added possibility that immature teeth may have a higher chance of maintaining pulp vitality, these results should be interpreted with caution when directly comparing the two treatment groups. The results of this study do correlate with other studies showing high rates of pulpal necrosis (45.5%–57%) following pulp capping after complicated crown fractures (Hecova et al., 2010; Wang et al., 2017). The higher rate of pulp necrosis may be related to the failure to remove the contaminated superficial layer of the exposed pulp, which is removed during a pulpotomy procedure but not during a pulp capping procedure (Fuks et al., 1982) or may be due to the practical difficulties in placing a pulp cap on a smooth fractured surface after crown fracture. The importance of a coronal seal to maintain a good outcome in root canal‐treated teeth (Gillen et al., 2011; Ray & Trope 1995) and following vital pulp treatment has been established (Cox et al., 1987). Wang et al. (2017) demonstrated that the pulp had a lower survival rate after vital pulp treatment of complicated crown fractures if the coronal restoration failed within 6 months. A potential explanation to pulpotomy being more successful than direct pulp cap is that it facilitates a better coronal seal. It has been suggested that pulp capping procedures may occupy parts of dentine and even enamel, thereby reducing the quality of the seal of an adhesive restoration (Hecova et al., 2010). The nature of troughing out an area for the pulpotomy medicament to be placed may reduce the risk of subsequent bacterial penetration (Hecova et al., 2010).
The studies included in this systematic review did not assess whether the restoration was satisfactory on review or whether the choice of restoration impacted the outcome, although Rao et al. (2020) excluded cases from their results, which had partial or complete loss of restoration. There was also no reference in any study to the quantity of remaining tooth structure, which could also impact tooth survival rates (Al‐Nuaimi et al., 2020). In the study by Caprioglio et al. (2014), it was reported that the tooth was initially restored with temporary cement and only when the mineralized bridge was formed was the tooth restored with a composite restoration. The lack of adequate coronal seal in this study may contribute to the slightly lower success rate of 81.5%. It would be beneficial for future pulpotomy studies to clarify the choice of restorative material used and include whether there were any failures observed in the restoration during follow‐up, which may impact the coronal seal and overall success rates. In accordance with the ESE guidelines on outcome assessment for vital pulp treatments, the inclusion criteria specified that both clinical (absence of symptoms) and radiographic (no abnormalities suggestive of periapical periodontitis) success criteria should be included (ESE, 2019). Although all included studies used both clinical and radiographic criteria to assess the outcome, the exact criteria specified for successful outcomes such as documented symptoms, sensibility tests and radiographic findings differed significantly between studies. Failure to satisfy the designated outcome criteria also excluded several studies from this systematic review. This finding is in accordance with another systematic review carried out by Kenny et al. (2018), which concluded that outcome criteria for traumatic dental injuries varied significantly in the literature. They published a recommended standardized set of core outcomes for all traumatic dental injuries and some injury‐specific outcomes to facilitate easier comparison across different studies in the future (Kenny et al., 2018).
Andreasen et al. (2018) stated that only histological criteria can definitively verify pulp healing so to establish whether there is pulp vitality the use of sensibility tests and evidence of radiographic bridge formation have been used as indicators. Although assessment of the blood supply within the dental pulp with laser Doppler flowmetry may be the best indicator of true pulp vitality (Alghaithy & Qualtrough 2017; Mainkar & Kim 2018), none of the included studies in this review used this method to aid assessment of pulp vitality. Pulp sensibility tests (thermal and EPT) can indirectly test pulp vitality by assessing the response of the nerve fibres in the pulp (Alghaithy & Qualtrough 2017); however, false positive and false negative results are common, especially in immature teeth (Gopikrishna et al., 2009), and in the first few months after trauma (Bastos et al., 2014). It has been suggested in a systematic review on the outcome criteria for pulpotomy in mature teeth that it would be unreliable to use such tests due to the inaccurate readings (Zanini et al., 2016); however, this recommendation is based on outcome results of coronal pulpotomy on molar teeth and sensibility tests may be more reliable in pulpotomy in anterior teeth due to the remaining vital pulp, particularly if a partial pulpotomy has been performed. Some studies included in this review did have outcome success measures such as a positive response to thermal testing (Caprioglio et al., 2014) and EPT tests (Cvek 1993; Fuks et al., 1982, 1993; Klein et al., 1985). Considering these studies included both mature and immature teeth, it is possible due to unreliable sensibility tests readings, some cases were documented as failures based solely on an inaccurate test result. Unfortunately, the exact reasoning for classifying the case as a failure was not always specified within the studies so it is unknown if this is the case. It would be advisable that in future studies of the success rates of pulpotomy that sensibility tests would be used as one of a number of core indicators rather than specific criteria for an outcome to be successful.
Considering the difficulties and reliability of clinically identifying vital pulp tissue, similarly to other reviews assessing the outcomes of pulpotomy, assessment of periapical health was deemed to be a clinically relevant outcome (Cushley et al., 2019; Zanini et al., 2016). High quality radiographs are essential for determining periapical health and limitations in the use of periapical radiographs for this are well documented which include the compression of 3‐dimensional anatomy (Velvart et al., 2001), anatomical noise (Bender & Seltzer 1961) and geometrical distortion (Forsberg & Halse 1994) all of which can obscure the area of interest. Periapical periodontitis is usually diagnosed with a periapical radiolucency (Ørstavik et al., 1986); however, this can be difficult to determine on a periapical radiographic particularly in the early stages of bone destruction (Patel et al., 2009; Tsai et al., 2012). It has been well documented that cone beam computed tomography (CBCT) is superior to conventional radiographs for detection of periapical periodontitis (Davies et al., 2015; Estrela et al., 2008; Lofthag‐Hansen et al., 2007; Low et al., 2008; Patel et al., 2012) and resorption (Lima et al., 2016). No study included in this review used CBCT to detect these changes. This may be partly due to most included studies being conducted prior to the CBCT‐era use and the drawbacks due to radiation dose (Patel et al., 2019) and cost.
Two studies also identified PCO as a failure, despite there being no other periradicular changes evident (Cvek 1993; Fuks et al., 1982). PCO was not included as a reason for failure in the review criteria due to the low incidence of these teeth developing periapical infection (McCabe & Dummer 2012), and it being more likely to be related to damage to the neurovascular supply to the pulp from a luxation injury (Robertson et al., 2000). Three of the nine failures in the study by Cvek (1993) were attributable to PCO so the overall success rate would be higher if this was deemed an acceptable outcome as it was in the study by Rao et al. (2020).
In part, the reported success rates for pulpotomy may be higher than that for the general population as although not all studies focused on immature teeth, many used young adults or children with the mean age being reported between 8 and 9.1 years in two studies (Caprioglio et al., 2014; Rao et al., 2020) with the remainder studies having age ranges between 6 and 22 years (Cvek 1993; Fuks et al., 1982, 1993; Klein et al., 1985; Xu 2016). The results may be representative of this age group, but it is possible that as people get older the decreased blood supply or reduced pulpal cellularity may decrease success rates. However, considering dental trauma mainly occurs in younger age groups (Glendor 2008), it is important to find the most appropriate treatment option at this age.
As young permanent teeth have open apices and abundant apical blood supply, it is thought that these factors may prevent bacterial invasion and the spread of inflammation (Andreasen & Kahler 2015), which could provide a better outcome for healing (Camp 2008). Two studies in this systematic review compared the success rates for pulpotomy in mature and immature teeth (Cvek 1993; Rao et al., 2020). The authors from both studies determined that root maturity had no significance on the success rates. Caprioglio et al. (2014) examined partial pulpotomy on immature teeth only and this study had a slightly lower success rate of 85.1%. This could suggest that root maturity should not be a significant indicator of treatment and instead the maintenance of pulp vitality should be the aim for all teeth with complicated crown fracture.
It has been proposed that the primary factor related to pulp healing after a complicated crown fracture appears to be compromised pulpal circulation due to concomitant luxation injuries (Robertson et al., 2000). Robertson et al. (2000) looked at 103 teeth with complicated crown fractures, 69 of which had associated luxation injury and it was found that an associated damage to the PDL increased the likelihood of pulp necrosis from 0% to 14%. It has been documented that a quarter of teeth which suffer complicated crown fractures can have associated ligament injuries (Maguire et al., 2000). Caprioglio et al. (2014) outlined that they only included teeth which had an assumed healthy radicular pulp; however, at initial preoperative examination 22 of the 27 teeth were tender to percussion and all had increased mobility except one. This may suggest that some teeth had concomitant periodontal injuries which again may account for the slightly lower success rate of 81.5% compared to other studies. Only two studies included in this review excluded teeth that had undergone luxation injuries and this may account for the highest success rates in those studies of between 95% and 96% (Cvek 1993; Rao et al., 2020). Since the remaining studies did not control for luxation injuries and still maintained high success rates, this could indicate that although the risk of necrosis may be increased, an associated luxation injury does not contraindicate vital pulp treatment.
In many cases there is a delay between the time of injury and attendance for treatment, with two studies reporting that only 43%–54% of patients who suffer a complicated crown fracture were treated on the day of their accident (Jackson et al., 2006; Maguire et al., 2000). It is important to determine whether this delay could impact treatment outcome; however, there are few studies available examining this (Andreasen et al., 2002b). Four of the seven studies included in this review examined whether time from injury to treatment impacted the overall success rates and there was no significant impact found in any study (Cvek 1993; Fuks et al., 1982, 1993; Klein et al., 1985). Rao et al. (2020) did not assess whether the time interval impacted on treatment outcome, but out of a total number of 168 cases in both the iRoot BP Plus and CH, 72 cases were treated between 24 and 72 h and 36 cases were treated at an interval longer than 72 h. The high overall success rates in each group of 99% in the iRoot BP plus group and 93% in the CH group, would suggest that treating teeth several days after trauma should still achieve high success rates. In comparison, in animal studies it has been found that the success of pulp capping mechanical exposures in primates reduced from 93% to 56%, when microbial exposure increased from 1 h to 7 days (Cox et al., 1982). This would suggest that time‐dependent treatment for pulp capping is more essential than for pulpotomy.
It has historically been suggested that the size of pulpal exposure may be a determining factor in deciding whether a pulp cap or pulpotomy is the most appropriate treatment choice (Cvek 1978). Xu (2016) outlined that 81% of the exposures in their study were under 2 mm in diameter. However, in the study by Xu (2016), only certain cases were suitable for inclusion, therefore, in this review it is unclear what size the exposures were in the included results. No other study included in the review outlined the size of exposures or the location. Fuks et al. (1982) only carried out the pulp capping procedure on pinpoint exposures, they performed pulpotomy on all teeth with immature roots regardless of exposure size. The rationale for the size of exposure after trauma having no influence on success rates for vital pulp treatment is if it is not infected; however, it may be important for carious exposures where a larger exposure is likely to be accompanied by increased pulpal infection and severity of pulpitis.
Whilst CH has traditionally been used as a pulp capping agent due to its antimicrobial activity and stimulation of hard tissue formation, it has drawbacks such as high solubility, lack of adhesion, poor sealing ability (Mohammadi & Dummer 2011) and tunnel defects in the mineralized tissue formed (Cox et al., 1985). The development of MTA with superior physical properties has substituted the use of CH in many situations of vital pulp therapy; however, it remains to have limitations of its own such as discolouration (Kahler & Rossi‐Fedele 2016) and long setting time (Parirokh & Torabinejad 2010). This has led to the development of many more hydraulic cements, which appear to have the same characteristics but overcome the limitations of MTA (Parirokh et al., 2018). The use of MTA and these hydraulic cements for coronal pulpotomy of carious molars has increased overtime due to high success rates (Cushley et al., 2019; Li et al., 2019), and more predictable mineralized bridge formation (Asgary et al., 2008). There are multiple case reports in the literature outlining the success of these materials in complicated crown fractures (Abarajithan et al., 2010; Asgary & Fazlyab 2014; Martens et al., 2015; Tuloglu & Bayrak 2016); however, only two studies in this review used materials other than CH for pulpotomy, which were iRoot BP Plus and MTA (Caprioglio et al., 2014; Rao et al., 2020). iRoot BP Plus is a calcium silicate bioactive ceramic (Rao et al., 2020) composed of tricalcium silicate, zirconium oxide, tantalum pentoxide, dicalcium silicate, calcium sulphate, calcium phosphate monobasic and filler agents (Mahgoub et al., 2019). The iRoot BP Plus group had the highest success rate in this systematic review whilst MTA had a lower success rate at 81.5%. Interestingly, Rao et al. (2020) advised they selected iRoot BP Plus to assess its success in pulpotomy over MTA due to MTA’s side effect of discolouration. However, in their study they did not examine whether the alternative of iRoot BP Plus caused discolouration itself. No study in the review identified specifically if discolouration was evident in their outcome and there is limited available research on this topic in the literature. Abuelniel et al. (2020) compared MTA with Biodentine as medicaments for pulpotomy in traumatized anterior permanent teeth. They separated clinical and radiographic success independently without pooling an overall success rate so were not included in this review; however, they found that discolouration was significantly more prevalent in the MTA group compared to the Biodentine group. It would be beneficial for future studies in this topic to examine whether discolouration was evident at follow‐up as this can have a significant impact on patient satisfaction levels.
The remaining studies used CH and their success rates ranged from 75% to 95% (Cvek 1993; Fuks et al., 1982, 1993; Klein et al., 1985; Xu 2016). Previous studies have found a high rate of pulpal necrosis using CH for pulp capping complicated crown fractures, with rates of pulpal necrosis ranging between 45.5% and 57% (Hecova et al., 2010; Wang et al., 2017). In this systematic review, CH has shown to have predictable outcomes for use in pulpotomy. Xu (2016) demonstrated the lowest success rates for partial pulpotomy of 75%; however, due to the strict inclusion criteria used in the systematic review, only limited data could be extracted from this study so only 12 cases were included. This study examined two treatment centres and the authors found that there were higher failure rates for pulpotomy when treatment as carried out in an emergency department. The authors attributed this higher failure rate to absence of dental assistants being present, late night treatments and increased risk of severe luxation injuries concomitantly occurring. As previously mentioned, the low success rates of CH for pulp capping may be due to the fact that inflamed superficial layer is not removed (Fuks et al., 1982) along with difficulties in providing a good coronal seal over a traditional CH pulp cap, making the material more suitable for a pulpotomy procedure. Since some hydraulic calcium silicate cement materials may not be available for use due to economic limitations in general practice (Zanini et al., 2019), CH could remain a suitable alternative if required. Further well‐designed randomized controlled studies examining the difference success rates of pulp medicament materials would be beneficial.
It has been established that bleeding time coincides with prognosis of vital pulp treatment for carious exposures (Matsuo et al., 1996). Recent guidance published on the management of endodontic injuries suggests that the level of pulp amputation be determined by whether the bleeding can be stopped by applying pressure with saline or sodium hypochlorite‐soaked gauze after ‘five minutes’ (Krastl et al., 2021). In this systematic review, only Rao et al. (2020) advised of the exact bleeding time, which was up to 5 min. It would be a recommendation that in future research the bleeding times be recorded, and these can then be assessed against success/failure rates so as to confirm whether 5 min is an appropriate time clinically for a clinician to progress from a partial pulpotomy to a complete pulpotomy.
Strengths and limitations
A strength of this systematic review is that multiple key databases were searched systematically, which covers all the relevant literature in this area and to the authors’ knowledge this is the first systematic review on this topic. Another advantage of this review is the robust inclusion and exclusion criteria that were used to maintain focus within the review and minimise potential bias arising from study selection.
However, there were also several limitations of this review which include the risk of bias in included studies as well as small sample sizes. The lack of standardization in follow‐up times and the range of included study designs is a further limitation of this review as it includes both retrospective and non‐comparative single‐arm studies, which are of a lower quality of evidence and limits comparison. Although a meta‐analysis was not possible due to lack of standardization in the included studies, this review will give guidance for further research particularly in relation to follow‐up and outcome data. Standardization in the future will allow pooling of data from future studies which will increase the strength of evidence in this area which is greatly needed.
CONCLUSIONS
Within the limitations of this review, the high success rates reported for pulpotomy suggests that this procedure, rather than pulp capping, should be considered as the treatment of choice for both immature and mature teeth that have undergone complicated crown fractures. Furthermore, there are high success rates for both complete and partial pulpotomy but due to the advantages (procedure, outcome sensibility testing) of partial pulpotomy, this should be the chosen treatment option where possible.
Well designed and appropriately powered randomized controlled trials with adequately long follow‐up are required to prove long term success of pulpotomy. The use of standardized and core outcome assessment criteria would be greatly beneficial for comparison of future results.
The continued use of CH can be justified, but future studies using newer hydraulic calcium silicate cements would be beneficial to determine if higher success rates can be achieved.
Correction added on 11 th May 2022, after first online publication: IReL funding statement has been added.
CONFLICT OF INTEREST
The authors deny any conflict of interest related to this study.
AUTHOR CONTRIBUTION
Study conception and design – AD, FF, PM, HD; Material Preparation, data collection and analysis – AD, FF; First draft of manuscript – AD; Revision drafting and final approval of manuscript – AD. FF, PM, HD.
ETHICAL APPROVAL
The study did not require ethical approval.
Supporting information
Table S1
ACKNOWLEDGMENTS
Open access funding enabled and organized by IRel WOA Institution: The University of Dublin Trinity CollegeBlended DEAL: IReL hybrid OA 2022.
Donnelly, A. , Foschi, F. , McCabe, P. & Duncan, H.F. (2022) Pulpotomy for treatment of complicated crown fractures in permanent teeth: A systematic review. International Endodontic Journal, 55, 290–311. Available from: 10.1111/iej.13690
Registration: Number‐CRD42021255689‐Prospero
Contributor Information
Aisling Donnelly, Email: aidonnel@tcd.ie.
Henry F. Duncan, Email: hduncan@tcd.ie.
REFERENCES
- Abarajithan, M. , Velmurugan, N. & Kandaswamy, D. (2010) Management of recently traumatized maxillary central incisors by partial pulpotomy using MTA: case reports with two‐year follow‐up. Journal of Conservative Dentistry, 13, 110–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abuelniel, G.M. , Duggal, M.S. & Kabel, N. (2020) A comparison of MTA and Biodentine as medicaments for pulpotomy in traumatized anterior immature permanent teeth: a randomized clinical trial. Dental Traumatology, 36, 400–410. [DOI] [PubMed] [Google Scholar]
- Alghaithy, R.A. & Qualtrough, A.J. (2017) Pulp sensibility and vitality tests for diagnosing pulpal health in permanent teeth: a critical review. International Endodontic Journal, 50, 135–142. [DOI] [PubMed] [Google Scholar]
- Al‐Nuaimi, N. , Ciapryna, S. , Chia, M. , Patel, S. & Mannocci, F. (2020) A prospective study on the effect of coronal tooth structure loss on the 4‐year clinical survival of root canal retreated teeth and retrospective validation of the Dental Practicality Index. International Endodontic Journal, 53, 1040–1049. [DOI] [PubMed] [Google Scholar]
- Alqaderi, H.E. , Al‐Mutawa, S.A. & Qudeimat, M.A. (2014) MTA pulpotomy as an alternative to root canal treatment in children's permanent teeth in a dental public health setting. Journal of Dentistry, 42, 1390–1395. [DOI] [PubMed] [Google Scholar]
- Altun, C. , Ozen, B. , Esenlik, E. , Guven, G. , Gürbüz, T. , Acikel, C. et al. (2009) Traumatic injuries to permanent teeth in Turkish children, Ankara. Dental Traumatology, 25, 309–313. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatric Dentistry . (2014) Guideline on pulp therapy for primary and immature permanent teeth [Accessed 2020 February 12]. Available from: https://www.aapd.org/research/oral‐health‐policies–recommendations/pulp‐therapy‐for‐primary‐and‐immature‐permanent‐teeth/ [Google Scholar]
- Andreasen, F.M. & Kahler, B. (2015) Pulpal response after acute dental injury in the permanent dentition: clinical implications—a review. Journal of Endodontics, 41, 299–308. [DOI] [PubMed] [Google Scholar]
- Andreasen, J.O. , Andreasen, F.M. , Skeie, A. , Hjorting‐Hansen, E. & Schwartz, O. (2002b) Effect of treatment delay upon pulp and periodontal healing of traumatic dental injuries—a review article. Dental Traumatology, 18, 116–128. [DOI] [PubMed] [Google Scholar]
- Andreasen, J.O. , Farik, B. & Munksgaard, E.C. (2002a) Long‐term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dental Traumatology, 18, 134–137. [DOI] [PubMed] [Google Scholar]
- Andreasen, J.O. , Andreasen, F.M. & Andersson, L. (2018) Textbook and color atlas of traumatic injuries to the teeth, 5th edition. UK: Wiley. [Google Scholar]
- Asgary, S. , Eghbal, M.J. , Parirokh, M. , Ghanavati, F. & Rahimi, H. (2008) A comparative study of histologic response to different pulp capping materials and a novel endodontic cement. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics, 106, 609–614. [DOI] [PubMed] [Google Scholar]
- Asgary, S. & Fazlyab, M. (2014) Management of complicated crown fracture with miniature pulpotomy: a case report. Iranian Endodontic Journal, 9, 233–234. [PMC free article] [PubMed] [Google Scholar]
- Bai, J. , Qin, M. & Ji, A.P. (2011) Clinical investigation of pulpotomy with pulpdent multi‐cal in young permanent anterior teeth. Beijing Da Xue Xue Bao Yi Xue Ban, 43, 882–885. [PubMed] [Google Scholar]
- Bastos, J.V. , Goulart, E.M. & de Souza Côrtes, M.I. (2014) Pulpal response to sensibility tests after traumatic dental injuries in permanent teeth. Dental Traumatology, 30, 188–192. [DOI] [PubMed] [Google Scholar]
- Bender, I.B. & Seltzer, S. (1961) Roentgenographic and direct observation of experimental lesions in bone: I. Journal of Endodontics, 29, 702–706. [DOI] [PubMed] [Google Scholar]
- Bimstein, E. & Rotstein, I. (2016) Cvek pulpotomy—revisited. Dental Traumatology, 32, 438–442. [DOI] [PubMed] [Google Scholar]
- Bjorndal, L. , Simon, S. , Tomson, P.L. & Duncan, H.F. (2019) Management of deep caries and the exposed pulp. International Endodontic Journal, 52, 949–973. [DOI] [PubMed] [Google Scholar]
- de Blanco, L.P. (1996) Treatment of crown fractures with pulp exposure. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 82, 564–568. [DOI] [PubMed] [Google Scholar]
- Blanco, L. & Cohen, S. (2002) Treatment of crown fractures with exposed pulps. Journal of the California Dental Association, 30, 419–425. [PubMed] [Google Scholar]
- Boltacz‐Rzepkowska, E. & Pawlicka, H. (2003) Radiographic features and outcome of root canal treatment carried out in the Lodz region of Poland. International Endodontic Journal, 36, 27–32. [DOI] [PubMed] [Google Scholar]
- Bourguignon, C. , Cohenca, N. , Lauridsen, E. , Flores, M.T. , O'Connell, A.C. , Day, P.F. et al. (2020) International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dental Traumatology, 36, 314–330. [DOI] [PubMed] [Google Scholar]
- Camp, J.H. (2008) Diagnosis dilemmas in vital pulp therapy: treatment for the toothache is changing, especially in young, immature teeth. Pediatric Dentistry, 30, 197–205. [PubMed] [Google Scholar]
- Caprioglio, A. , Conti, V. , Caprioglio, C. & Caprioglio, D. (2014) A long‐term retrospective clinical study on MTA pulpotomies in immature permanent incisors with complicated crown fractures. European Journal of Paediatric Dentistry, 15, 29–34. [PubMed] [Google Scholar]
- Centre for Evidence‐based Medicine . (2009) Oxford centre for evidence‐based medicine‐ levels of evidence. Available from: https://www.cebm.net/2009/06/oxford‐centre‐evidence‐based‐medicine‐levels‐evidence‐march‐2009/ [Accessed 17th January 2020] [Google Scholar]
- Chaniotis . (2018) Orthodontic movement after regenerative endodontic procedure: case report and long term complications. Journal of Endodontics, 44, 432–437. [DOI] [PubMed] [Google Scholar]
- Chen, Y. , Chen, X. , Zhang, Y. , Zhou, F. , Deng, J. , Zou, J. et al. (2019) Materials for pulpotomy in immature permanent teeth: a systematic review and meta‐analysis. BMC Oral Health, 19, 227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang, Y.C. , Chang, H.H. , Wong, C.C. , Wang, Y.P. , Wang, Y.L. , Huang, W.H. et al. (2016) Nanocrystalline calcium sulfate/hydroxyapatite biphasic compound as a TGF‐beta1/VEGF reservoir for vital pulp therapy. Dental Materials, 32, 1197–1208. [DOI] [PubMed] [Google Scholar]
- Cox, C.F. , Bergenholtz, G. , Fitzgerald, M. , Heys, D.R. , Heys, R.J. , Avery, J.K. et al. (1982) Capping of the dental pulp mechanically exposed to the oral microflora—a 5 week observation of wound healing in the monkey. Journal of Oral Pathology, 11, 327–339. [DOI] [PubMed] [Google Scholar]
- Cox, C.F. , Bergenholtz, G. , Heys, D.R. , Syed, S.A. , Fitzgerald, M. & Heys, R.J. (1985) Pulp capping of dental pulp mechanically exposed to oral microflora: a 1–2 year observation of wound healing in the monkey. Journal of Oral Pathology, 14, 156–168. [DOI] [PubMed] [Google Scholar]
- Cox, C.F. , Keall, C.L. , Keall, H.J. , Ostro, E. & Bergenholtz, G. (1987) Biocompatibility of surface‐sealed dental materials against exposed pulps. Journal of Prosthetic Dentistry, 57, 1–8. [DOI] [PubMed] [Google Scholar]
- Cushley, S. , Duncan, H.F. , Lappin, M.J. , Tomson, P.L. , Lundy, F.T. , Cooper, P. et al. (2019) Pulpotomy for mature carious teeth with symptoms of irreversible pulpitis: a systematic review. Journal of Dentistry, 88, 103158. [DOI] [PubMed] [Google Scholar]
- Cvek, M. (1978) A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. Journal of Endodontics, 4, 232–237. [DOI] [PubMed] [Google Scholar]
- Cvek, M. (1992) Prognosis of luxated non‐vital maxillary incisors treated with calcium hydroxide and filled with gutta‐percha. A retrospective clinical study. Endodontics & Dental Traumatology, 8, 45–55. [DOI] [PubMed] [Google Scholar]
- Cvek, M. (1993) Partial pulpotomy in crown—fractured incisors—results 3 to 15 years after treatment. Acta Stomatologica Croatica, 27, 168–173. [Google Scholar]
- Cvek, M. , Cleaton‐Jones, P.E. , Austin, J.C. & Andreasen, J.O. (1982) Pulp reactions to exposure after experimental crown fractures or grinding in adult monkeys. Journal of Endodontics, 8, 391–397. [DOI] [PubMed] [Google Scholar]
- Cvek, M. & Lundberg, M. (1983) Histological appearance of pulps after exposure by a crown fracture, partial pulpotomy, and clinical diagnosis of healing. Journal of Endodontics, 9, 8–11. [DOI] [PubMed] [Google Scholar]
- Dabrowska, E. , Zdanowicz‐Wiloch, J. , Pawinska‐Magnuszewska, M. & Stokowska, W. (1997) Intravital treatment of the pulp with simultaneous laser biostimulation. Roczniki Akademii Medycznej W Bialymstoku, 42, 168–176. [PubMed] [Google Scholar]
- Davies, A. , Mannocci, F. , Mitchell, P. , Andiappan, M. & Patel, S. (2015) The detection of periapical pathoses in root filled teeth using single and parallax periapical radiographs versus cone beam computed tomography—a clinical study. International Endodontic Journal, 48, 582–592. [DOI] [PubMed] [Google Scholar]
- Diaz, J.A. , Bustos, L. , Brandt, A.C. & Fernandez, B.E. (2010) Dental injuries among children and adolescents aged 1–15 years attending to public hospital in Temuco, Chile. Dental Traumatology, 26, 254–261. [DOI] [PubMed] [Google Scholar]
- Duggal, M. , Tong, H.J. , Al‐Ansary, M. , Twati, W. , Day, P.F. & Nazzal, H. (2017) Interventions for the endodontic management of non‐vital traumatised immature permanent anterior teeth in children and adolescents: a systematic review of the evidence and guidelines of the European Academy of Paediatric Dentistry. European Archives of Paediatric Dentistry, 18, 139–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrmann, E.H. (1981) Pulpotomies in traumatized and carious permanent teeth using a corticosteroid antibiotic preparation. International Endodontic Journal, 14, 149–156. [DOI] [PubMed] [Google Scholar]
- El‐Meligy, O.A. & Avery, D.R. (2006) Comparison of mineral trioxide aggregate and calcium hydroxide as pulpotomy agents in young permanent teeth (apexogenesis). Pediatric Dentistry, 28, 399–404. [PubMed] [Google Scholar]
- Elmsmari, F. , Ruiz, X.F. , Miró, Q. , Feijoo‐Pato, N. , Durán‐Sindreu, F. & Olivieri, J.G. (2019) Outcome of partial pulpotomy in cariously exposed posterior permanent teeth: a systematic review and meta‐analysis. Journal of Endodontics, 45, 1296–1306.e3. [DOI] [PubMed] [Google Scholar]
- Estrela, C. , Bueno, M.R. , Leles, C.R. , Azevedo, B. & Azevedo, J.R. (2008) Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. Journal of Endodontics, 34, 273–279. [DOI] [PubMed] [Google Scholar]
- European Society of Endodontology . (2006) Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. International Endodontic Journal, 39, 921–930. [DOI] [PubMed] [Google Scholar]
- European Society of Endodontology . (2019) European Society of Endodontology position statement: management of deep caries and the exposed pulp. International Endodontic Journal, 52, 923–934. [DOI] [PubMed] [Google Scholar]
- European Society of Endodontology . (2021) European Society of Endodontology position statement: endodontic management of traumatized permanent teeth. International Endodontic Journal, 54, 1473–1481. [DOI] [PubMed] [Google Scholar]
- Fong, C.D. & Davis, M.J. (2002) Partial pulpotomy for immature permanent teeth, its present and future. Pediatric Dentistry, 24, 29–32. [PubMed] [Google Scholar]
- Forsberg, J. & Halse, A. (1994) Radiographic simulation of a periapical lesion comparing the paralleling and the bisecting‐angle techniques. International Endodontic Journal, 27, 133–138. [DOI] [PubMed] [Google Scholar]
- Fuks, A.B. , Bielak, S. & Chosak, A. (1982) Clinical and radiographic assessment of direct pulp capping and pulpotomy in young permanent teeth. Pediatric Dentistry, 4, 240–244. [PubMed] [Google Scholar]
- Fuks, A.B. , Cosack, A. , Klein, H. & Eidelman, E. (1987) Partial pulpotomy as a treatment alternative for exposed pulps in crown‐fractured permanent incisors. Endodontics & Dental Traumatology, 3, 100–102. [DOI] [PubMed] [Google Scholar]
- Fuks, A.B. , Gavra, S. & Chosack, A. (1993) Long‐term follow‐up of traumatized incisors treated by partial pulpotomy. Pediatric Dentistry, 15, 334–336. [PubMed] [Google Scholar]
- Garcia‐Godoy, F. & Murray, P.E. (2012) Recommendations for using regenerative endodontic procedures in permanent immature traumatized teeth. Dental Traumatology, 28, 33–41. [DOI] [PubMed] [Google Scholar]
- Gelbier, M.J. & Winter, G.B. (1988) Traumatised incisors treated by vital pulpotomy: a retrospective study. British Dental Journal, 164, 319–323. [DOI] [PubMed] [Google Scholar]
- Gillen, B.M. , Looney, S.W. , Gu, L.‐S. , Loushine, B.A. , Weller, R.N. , Loushine, R.J. et al. (2011) Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta‐analysis. Journal of Endodontics, 37, 895–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glendor, U. (2008) Epidemiology of traumatic dental injuries—a 12 year review of the literature. Dental Traumatology, 24, 603–611. [DOI] [PubMed] [Google Scholar]
- Gopikrishna, V. , Pradeep, G. & Venkateshbabu, N. (2009) Assessment of pulp vitality: a review. International Journal of Paediatric Dentistry, 19, 3–15. [DOI] [PubMed] [Google Scholar]
- Gutmann, J.L. & Heaton, J.F. (1981) Management of the open (immature) apex. 1. Vital teeth. International Endodontic Journal, 14, 166–172. [DOI] [PubMed] [Google Scholar]
- Haikal, L. , Ferraz Dos Santos, B. , Vu, D.D. , Braniste, M. & Dabbagh, B. (2020) Biodentine pulpotomies on permanent traumatized teeth with complicated crown fractures. Journal of Endodontics, 46, 1204–1209. [DOI] [PubMed] [Google Scholar]
- Hecova, H. , Tzigkounakis, V. , Merglova, V. & Netolicky, J. (2010) A retrospective study of 889 injured permanent teeth. Dental Traumatology, 26, 466–475. [DOI] [PubMed] [Google Scholar]
- Heide, S. & Mjor, I.A. (1983) Pulp reactions to experimental exposures in young permanent monkey teeth. International Endodontic Journal, 16, 11–19. [DOI] [PubMed] [Google Scholar]
- Jackson, N.G. , Waterhouse, P.J. & Maguire, A. (2006) Factors affecting treatment outcomes following complicated crown fractures managed in primary and secondary care. Dental Traumatology, 22, 179–185. [DOI] [PubMed] [Google Scholar]
- Kahler, B. & Rossi‐Fedele, G. (2016) A review of tooth discoloration after regenerative Endodontic Therapy. Journal of Endodontics, 42, 563–569. [DOI] [PubMed] [Google Scholar]
- Kang, C.‐M. , Sun, Y. , Song, J.S. , Pang, N.‐S. , Roh, B.‐D. , Lee, C.‐Y. et al. (2017) A randomized controlled trial of various MTA materials for partial pulpotomy in permanent teeth. Journal of Dentistry, 60, 8–13. [DOI] [PubMed] [Google Scholar]
- Katebzadeh, N. , Dalton, B.C. & Trope, M. (1998) Strengthening immature teeth during and after apexification. Journal of Endodontics, 24, 256–259. [DOI] [PubMed] [Google Scholar]
- Kenny, K.P. , Day, P.F. , Sharif, M.O. , Parashos, P. , Lauridsen, E. , Feldens, C.A. et al. (2018) What are the important outcomes in traumatic dental injuries? An international approach to the development of a core outcome set. Dental Traumatology, 34, 4–11. [DOI] [PubMed] [Google Scholar]
- Klein, H. , Fuks, A. , Eidelman, E. & Chosack, A. (1985) Partial pulpotomy following complicated crown fracture in permanent incisors: a clinical and radiographical study. Journal of Pedodontics, 9, 142–147. [PubMed] [Google Scholar]
- Kostopoulou, M.N. & Duggal, M.S. (2005) A study into dentists’ knowledge of the treatment of traumatic injuries to young permanent incisors. International Journal of Paediatric Dentistry, 15, 10–19. [DOI] [PubMed] [Google Scholar]
- Krastl, G. , Weiger, R. , Filippi, A. , Van Waes, H. , Ebeleseder, K. , Ree, M. et al. (2021) Endodontic management of traumatized permanent teeth: a comprehensive review. International Endodontic Journal, 54, 1221–1245. [DOI] [PubMed] [Google Scholar]
- Kunert, G.G. , Kunert, I.R. , da Costa Filho, L.C. & de Figueiredo, J.A.P. (2015) Permanent teeth pulpotomy survival analysis: retrospective follow‐up. Journal of Dentistry, 43, 1125–1131. [DOI] [PubMed] [Google Scholar]
- Li, Y. , Sui, B. , Dahl, C. , Bergeron, B. , Shipman, P. , Niu, L. et al. (2019) Pulpotomy for carious pulp exposures in permanent teeth: a systematic review and meta‐analysis. Journal of Dentistry, 84, 1–8. [DOI] [PubMed] [Google Scholar]
- Liberati, A. , Altman, D.G. , Tetzlaff, J. , Mulrow, C. , Gøtzsche, P.C. , Ioannidis, J.P.A. et al. (2009) The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med, 6, e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima, T.F. , Gamba, T.O. , Zaia, A.A. & Soares, A.J. (2016) Evaluation of cone beam computed tomography and periapical radiography in the diagnosis of root resorption. Australian Dental Journal, 61, 425–431. [DOI] [PubMed] [Google Scholar]
- Lofthag‐Hansen, S. , Huumonen, S. , Grondahl, K. & Grondahl, H.G. (2007) Limited cone‐beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics, 103, 114–119. [DOI] [PubMed] [Google Scholar]
- Low, K.M. , Dula, K. , Burgin, W. & von Arx, T. (2008) Comparison of periapical radiography and limited cone‐beam tomography in posterior maxillary teeth referred for apical surgery. Journal of Endodontics, 34, 557–562. [DOI] [PubMed] [Google Scholar]
- Magnusson, B. , Holm, A.K. & Berg, H. (1969) Traumatised permanent teeth in children—a follow‐up. II. The crown fractures. Svensk Tandlakare Tidskrift, 62, 71–77. [PubMed] [Google Scholar]
- Maguire, A. , Murray, J.J. & Al‐Majed, I. (2000) A retrospective study of treatment provided in the primary and secondary care services for children attending a dental hospital following complicated crown fracture in the permanent dentition. International Journal of Paediatric Dentistry, 10, 182–190. [DOI] [PubMed] [Google Scholar]
- Mahgoub, N. , Alqadasi, B. , Aldhorae, K. , Assiry, A. , Altawili, Z.M. & Hong, T. (2019) Comparison between iRoot BP Plus (EndoSequence Root Repair Material) and mineral trioxide aggregate as pulp‐capping agents: a systematic review. Journal of International Society of Preventive & Community Dentistry, 9, 542–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mainkar, A. & Kim, S.G. (2018) Diagnostic accuracy of 5 dental pulp tests: a systematic review and meta‐analysis. Journal of Endodontics, 44, 694–702. [DOI] [PubMed] [Google Scholar]
- Martens, L. , Rajasekharan, S. & Cauwels, R. (2015) Pulp management after traumatic injuries with a tricalcium silicate‐based cement (Biodentine™): a report of two cases, up to 48 months follow‐up. European Archives of Paediatric Dentistry, 16, 491–496. [DOI] [PubMed] [Google Scholar]
- Matsuo, T. , Nakanishi, T. , Shimizu, H. & Ebisu, S. (1996) A clinical study of direct pulp capping applied to carious‐exposed pulps. Journal of Endodontics, 22, 551–556. [DOI] [PubMed] [Google Scholar]
- McCabe, P.S. & Dummer, P.M. (2012) Pulp canal obliteration: an endodontic diagnosis and treatment challenge. International Endodontic Journal, 45, 177–197. [DOI] [PubMed] [Google Scholar]
- Mohammadi, Z. & Dummer, P.M. (2011) Properties and applications of calcium hydroxide in endodontics and dental traumatology. International Endodontic Journal, 44, 697–730. [DOI] [PubMed] [Google Scholar]
- Nagendrababu, V. , Duncan, H.F. , Tsesis, I. , Sathorn, C. , Pulikkotil, S.J. , Dharmarajan, L. et al. (2019) PRISMA for abstracts: best practice for reporting abstracts of systematic reviews in Endodontology. International Endodontic Journal, 52, 1096–1107. [DOI] [PubMed] [Google Scholar]
- Nagendrababu, V. , Duncan, H.F. & Dummer, P.M.H. (2020) Research that matters: systematic reviews and meta‐analyses. International Endodontic Journal, 53, 437–439. [DOI] [PubMed] [Google Scholar]
- Ørstavik, D. , Kerekes, K. & Eriksen, H.M. (1986) The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endodontics & Dental Traumatology, 2, 20–34. [DOI] [PubMed] [Google Scholar]
- Ortiz, G.E. (1973) Failures in the treatment of pulp injuries and pulpotomies–their causes and prevention. Adm, 30, 13–18. [PubMed] [Google Scholar]
- Oulis, C.J. & Berdouses, E.D. (1996) Dental injuries of permanent teeth treated in private practice in Athens. Endodontics & Dental Traumatology, 12, 60–65. [DOI] [PubMed] [Google Scholar]
- Parirokh, M. & Torabinejad, M. (2010) Mineral trioxide aggregate, a comprehensive literature review—part III, clinical applications, drawbacks, and mechanism of action. Journal of Endodontics, 36, 400–413. [DOI] [PubMed] [Google Scholar]
- Parirokh, M. , Torabinejad, M. & Dummer, P.M.H. (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview—part I: vital pulp therapy. International Endodontic Journal, 51, 177–205. [DOI] [PubMed] [Google Scholar]
- Patel, S. , Brown, J. , Pimental, T. , Kelly, R. , Abella, F. & Durack, C. (2019) Cone beam computed tomography in endodontics—a review of the literature. International Endodontic Journal, 52, 1138–1152. [DOI] [PubMed] [Google Scholar]
- Patel, S. , Dawood, A. , Mannocci, F. , Wilson, R. & Pitt Ford, T. (2009) Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. International Endodontic Journal, 42, 507–515. [DOI] [PubMed] [Google Scholar]
- Patel, S. , Wilson, R. , Dawood, A. & Mannocci, F. (2012) The detection of periapical pathosis using periapical radiography and cone beam computed tomography—part 1: pre‐operative status. International Endodontic Journal, 45, 702–710. [DOI] [PubMed] [Google Scholar]
- Patterson, S.S. (1967) Pulp calcification due to operative procedures–pulpotomy. International Dental Journal, 17, 490–505. [PubMed] [Google Scholar]
- PRIMSA‐P . (2016) Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015: elaboration and explanation. BMJ, 350, i4086. [DOI] [PubMed] [Google Scholar]
- Rao, Q. , Kuang, J. , Mao, C. , Dai, J. , Hu, L. , Lei, Z. et al. (2020) Comparison of iRoot BP Plus and calcium hydroxide as pulpotomy materials in permanent incisors with complicated crown fractures: a retrospective study. Journal of Endodontics, 46, 352–357. [DOI] [PubMed] [Google Scholar]
- Ravn, J.J. (1973) Prognosis of pulp capping and pulpotomy by complicated crown fractures of permanent incisors in the injury. Preliminary report. Tandlaegebladet, 77, 31–38. [PubMed] [Google Scholar]
- Ravn, J.J. (1974) Complicated crown fractures of permanent incisors. Review of treatment in the Copenhagen municipal child dental clinics 1967‐72. Tandlaegebladet, 78, 1017–1020. [PubMed] [Google Scholar]
- Ravn, J.J. (1982) Follow‐up study of permanent incisors with complicated crown fractures after acute trauma. Scandinavian Journal of Dental Research, 90, 363–372. [DOI] [PubMed] [Google Scholar]
- Ray, H.A. & Trope, M. (1995) Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. International Endodontic Journal, 28, 12–18. [DOI] [PubMed] [Google Scholar]
- Robertson, A. , Andreasen, F.M. , Andreasen, J.O. & Noren, J.G. (2000) Long‐term prognosis of crown‐fractured permanent incisors. The effect of stage of root development and associated luxation injury. International Journal of Paediatric Dentistry, 10, 191–199. [DOI] [PubMed] [Google Scholar]
- Saunders, W.P. , Saunders, E.M. , Sadiq, J. & Cruickshank, E. (1997) Technical standard of root canal treatment in an adult Scottish sub‐population. British Dental Journal, 182, 382–386. [DOI] [PubMed] [Google Scholar]
- Silujjai, J. & Linsuwanont, P. (2017) Treatment outcomes of apexification or revascularization in nonvital immature permanent teeth: a retrospective study. Journal of Endodontics, 43, 238–245. [DOI] [PubMed] [Google Scholar]
- Sluka, H. , Lehmann, H. & Elgün, Z. (1981) Comparative experiments on treatment technics in vital amputation in view of the preservation of the remaining pulp. Die Quintessenz, 32, 1571–1577. [PubMed] [Google Scholar]
- Sterne, J.A.C. , Hernan, M.A. , Reeves, B.C. , Savović, J. , Berkman, N.D. , Viswanathan, M. et al. (2016) ROBINS‐1: a tool for assessing risk of bias in non‐randomised studies of interventions. BMJ, 355, 4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai, P. , Torabinejad, M. , Rice, D. & Azevedo, B. (2012) Accuracy of cone‐beam computed tomography and periapical radiography in detecting small periapical lesions. Journal of Endodontics, 38, 965–970. [DOI] [PubMed] [Google Scholar]
- Tuloglu, N. & Bayrak, S. (2016) Partial pulpotomy with BioAggregate in complicated crown fractures: three case reports. The Journal of Clinical Pediatric Dentistry, 40, 31–35. [DOI] [PubMed] [Google Scholar]
- Velvart, P. , Hecker, H. & Tillinger, G. (2001) Detection of the apical lesion and the mandibular canal in conventional radiography and computed tomography. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontology, 92, 682–688. [DOI] [PubMed] [Google Scholar]
- Viduskalne, I. & Care, R. (2010) Analysis of the crown fractures and factors affecting pulp survival due to dental trauma. Stomatologija, 12, 109–115. [PubMed] [Google Scholar]
- Wang, G. , Wang, C. & Qin, M. (2017) Pulp prognosis following conservative pulp treatment in teeth with complicated crown fractures—a retrospective study. Dental Traumatology, 33, 255–260. [DOI] [PubMed] [Google Scholar]
- Wang, Q. , Huang, S. , Chen, J. , Ge, L. & Liu, H. (2011) Retrospective study of the prognosis and influence factors of crown‐fractured young maxillary incisors with pulp exposure. Hua Xi Kou Qiang Yi Xue Za Zhi, 29, 622–625. [PubMed] [Google Scholar]
- Wells, G.A. , Shea, B. , O’Connell, D. , Peterson, J. , Welch, V. , Losos, M. et al. (2019) The Newcastle‐Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxfo [Accessed 8th June 2021]
- Winter, G.B. (1977) Endodontic therapy of traumatised teeth in children. International Dental Journal, 27, 252–262. [PubMed] [Google Scholar]
- Witherspoon, D.E. , Regan, J.D. & Small, J.C. (2017) MTA Pulpotomies: along‐term case series outcomes assessment of complicated crown fractures. Texas Dental Journal, 134, 166–175. [PubMed] [Google Scholar]
- Witherspoon, D.E. , Small, J.C. & Harris, G.Z. (2006) Mineral trioxide aggregate pulpotomies: a case series outcomes assessment. Journal of the American Dental Association, 137, 610–618. [DOI] [PubMed] [Google Scholar]
- Wojnar‐Kalina, A. (1979) Results of treatment of post‐traumatic lesions of the dental pulp by means of intravital amputation in teeth unformed root]. Czasopismo Stomatologiczne, 32, 1037–1042. [PubMed] [Google Scholar]
- Xu, H. (2016) Success Rate of Cvek Pulpotomies in permanent teeth with complicated crown fractures (Masters Thesis). Ohio, USA: The Ohio State University. [Google Scholar]
- Yilmaz, Y. , Guler, C. , Sahin, H. & Eyuboglu, O. (2010) Evaluation of tooth‐fragment reattachment: a clinical and laboratory study. Dental Traumatology, 26, 308–314. [DOI] [PubMed] [Google Scholar]
- Yilmaz, Y. , Zehir, C. , Eyuboglu, O. & Belduz, N. (2008) Evaluation of success in the reattachment of coronal fractures. Dental Traumatology, 24, 151–158. [DOI] [PubMed] [Google Scholar]
- Zanini, M. , Hennequin, M. & Cousson, P.Y. (2016) A Review of criteria for the evaluation of pulpotomy outcomes in mature permanent teeth. Journal of Endodontics, 42, 1167–1174. [DOI] [PubMed] [Google Scholar]
- Zanini, M. , Hennequin, M. & Cousson, P.Y. (2019) Which procedures and materials could be applied for full pulpotomy in permanent mature teeth? A systematic review. Acta Odontologica Scandinavica, 77, 541–551. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


