Abstract
Objective
The primary aim was to assess the feasibility of undertaking a study evaluating the novel Motivational and Psycho‐Educational Self‐Help Programme for Athletes with Mild Eating Disorder Symptoms (MOPED‐A). A mixed‐methods approach was adopted to explore the feasibility of recruiting and retaining participants, and to evaluate the acceptability of measures, procedures and the intervention. A secondary aim was to explore the potential efficacy of MOPED‐A in reducing athletes' eating disorder symptoms.
Method
Thirty‐five athletes were recruited. Participation involved completing MOPED‐A over a 6‐week period and completing self‐report measures at baseline (T1), post‐intervention (T2) and 4‐week follow‐up (T3). A subsample (n = 15) completed an interview at T2.
Results
Retention was good throughout the study (n = 28; 80%). Quantitative and qualitative feedback suggested the format, delivery, content and dosage of MOPED‐A were acceptable. Athletes valued that the intervention was tailored to them, and this facilitated both participation and completion. Over a third of participants reported disclosing their eating difficulties and deciding to seek further support. Large reductions in eating disorder symptoms were detected at T2 and sustained at T3.
Conclusions
The MOPED‐A intervention can be feasibly implemented, is acceptable to participants, and demonstrates potential for reducing symptoms in athletes. A larger, controlled trial is warranted.
Keywords: athletes, disordered eating, evaluation, self‐help intervention
Highlights
Participant recruitment to the study was feasible, and an acceptable proportion of participants were retained throughout the study.
This is the first study to show that the format and delivery of a self‐help intervention is acceptable to athletes with mild eating disorder symptoms, and that athletes valued the intervention being tailored to them which facilitated participation and completion.
The intervention demonstrates potential for reducing athletes' eating disorder symptoms.
Abbreviations
- EDE‐Q
Eating Disorder Examination Questionnaire
- IMA
Intervention Mapping for Adaptation
- MCAR test
Missing Completely At Random test
- MOPED‐A
Motivational and Psycho‐Educational Self‐Help Programme for Athletes with Mild Eating Disorder Symptoms
1. INTRODUCTION
Eating disorder symptoms are associated with serious mental and physical health impairment, can become chronic and may result in the development of clinical eating disorders, which are linked with significant morbidity and mortality (Attard et al., 2013; Dooley‐Hash et al., 2019; Fitzsimmons‐Craft, 2011; Neumark‐Sztainer et al., 2011). Early intervention is therefore important to mitigate against symptoms worsening (Royal College of Psychiatrists, 2019). Indeed, self‐help interventions have been recommended as the first line of treatment for mild to moderate eating disorder symptoms (National Institute for Health and Care Excellence, 2017). Mild to moderate eating disorder symptoms refer to subclinical disturbances in eating behaviours and attitudes which are not sufficiently severe or do not occur frequently enough to meet the diagnostic criteria for clinical eating disorders (American Psychiatric Association, 2013). For instance, mild to moderate symptoms may include occasional food restriction/binging/purging behaviours ([1–3 episodes per week]; American Psychiatric Association, 2013).
Eating disorder symptoms are common in athletes (Bratland‐Sanda & Sundgot‐Borgen, 2013; Joy et al., 2016). Prevalence estimates for mild eating disorder symptoms (i.e., disordered eating) have been suggested to range from 20% to 46% in female athletes and from 10% to 19% in male athletes (Anderson & Petrie, 2012; Greenleaf et al., 2009; Krebs et al., 2019; Martinsen et al., 2010). Prevalence rates across different sport types have also been explored, yet the results are conflicting. Some research has found particularly high prevalence rates for female athletes in endurance and aesthetic sports, and for male athletes in weight‐class sports (Schaal et al., 2011). In contrast, others have found no sport‐specific differences in the prevalence of eating disorder symptoms among athletes (Martinsen et al., 2010), or that there is a lack of evidence to support clear differences in prevalence between sport types (Mancine et al., 2020). Importantly, few interventions have been developed to reduce mild eating disorder symptoms in athletes. A recent systematic review of existing interventions targeting eating disorder symptoms in athletes found that most interventions generally achieved small to medium reductions in athletes' symptoms immediately post‐intervention (Sandgren et al., 2020). While some interventions reported sustained effects, others reported no effects or even an increase in symptoms (Sandgren et al., 2020). Participant retention rates in the studies reviewed by Sandgren et al. (2020) also varied considerably (range: 20–100%). This suggests varying degrees of efficacy and acceptability of existing athlete interventions and their study procedures, and evidence of feasibility is further threatened by a notable lack of reported process evaluation data. Notwithstanding, there is some evidence to suggest that healthy‐weight and nutrition‐oriented interventions can be acceptable to student‐athletes (Becker et al., 2012).
Furthermore, many people with eating disorder symptoms are low on motivation/readiness to change (Vandereycken, 2006), hence a key priority for interventions should be around helping to motivate individuals to initiate and maintain changes to their eating behaviour (Price‐Evans & Treasure, 2011). This is important due to the key role that motivation plays in making and maintaining behavioural changes to recover from an eating disorder (Prochaska et al., 1993). Low motivation to change has been found to negatively predict engagement, adherence and outcomes with eating disorder treatments and interventions (Clausen et al., 2013). Accordingly, targeting motivation in early interventions for addressing eating disorder symptoms is likely to be important for initiating change in participants (Brewin et al., 2016). However, this approach has yet to be adopted with interventions that target eating disorder symptoms in athlete populations. Motivation will likely be particularly important given that athletes can be resistant to change due to fear of being excluded from training or competition (Thompson & Sherman, 2014), although it is noteworthy that some athletes might be more motivated to initiate change if they believe doing so will improve their athletic performance. Additionally, considering the potential for scalability of future athlete interventions is another area needing to be addressed so that at‐risk athletes can access appropriate and timely intervention more widely. Due to the training and competition schedules of many athletes which require them to travel frequently, the accessibility of a future intervention is also likely to be an important factor in facilitating adherence and acceptability. Together, this evidence highlights the need for athlete‐specific interventions to address mild levels of eating disorders in this at‐risk group.
To date, all existing athlete eating disorder interventions have been delivered face‐to‐face in group‐based settings and have largely been delivered to collegiate level, female athletes in North America (Sandgren et al., 2020). While face‐to‐face interventions can offer real‐time discussion and support (Kaufman et al., 2018), they are not easily scalable for implementation across a variety of settings, and logistic, resource and fidelity concerns are common challenges for implementation (Milat et al., 2012). There is thus a need for more scalable and accessible interventions that can be rolled out to athletes more widely. Self‐help interventions are structured programmes that individuals work through on their own or with minimal guidance, accompanied by evidence‐ and theory‐based assignments and activities (Aardoom et al., 2016). Such interventions are scalable (Traviss‐Turner et al., 2017), can offer privacy, accessibility and flexibility to users (Yim & Schmidt, 2019), and are recommended for delivering early intervention for mild to moderate eating disorder symptoms (National Institute for Health and Care Excellence, 2017). Indeed, recent evidence points to the potential value of self‐help interventions for reaching a larger number of athletes with mild eating disorder symptoms (Flatt & Taylor, 2018; Sandgren et al., 2020). However, a self‐help intervention to address mild eating disorder symptoms in athletes has yet to be developed, rolled out and evaluated.
Rigorous development and evaluation processes are needed to ensure new interventions to address mild eating disorder symptoms in athletes achieve maximum effectiveness and to ensure they are appropriate and acceptable for the target population. Assessing the feasibility of a new intervention is an essential first step in determining its potential value to participants (Bartholomew et al., 2016), and such studies are an important steppingstone towards larger, controlled and definitive trials (e.g. Can it work? If so, how? Tickle‐Degnen, 2013). If feasibility studies are not conducted prior to larger‐scale trials, there is an increased risk of wasting resources and the efficacy, wider relevance, generalisability and dissemination of interventions is threatened (Bowen et al., 2009; Orsmond & Cohn, 2015).
The primary aim of this study is therefore to assess the feasibility of undertaking a study evaluating a novel motivational and psycho‐educational self‐help intervention for athletes with mild eating disorder symptoms. Key study objectives were informed by existing feasibility guidelines (Bowen et al., 2009; Orsmond & Cohn, 2015) and are to: (1) explore the feasibility of recruiting and retaining participants in the study; (2) determine the acceptability of measures and research procedures; and (3) conduct a mixed methods process evaluation to determine the acceptability of the intervention to participants. A secondary aim is to explore the potential efficacy of the intervention at reducing eating disorder symptoms in athletes, and to use this to inform the required sample size for an intervention arm of a larger, future trial.
2. METHOD
2.1. Study design and reporting
Institutional ethical approval was granted and an intervention‐arm only, mixed methods feasibility design was implemented. The reporting of this study aligns with the guidelines for reporting non‐randomised feasibility studies (Lancaster & Thabane, 2019) and the CONSORT extension checklist and statement for pilot and feasibility trials (Eldridge et al., 2016).
2.2. Participants
Participants were recruited on a rolling basis during February and March 2020 by advertising the study through several UK sport organisations, clubs and via social media (further details on the recruitment and retention of participants are presented in the results). Eligible participants had to be based in the United Kingdom, aged 18 years or over, currently be training for, and competing in, any sport at any level, and to self‐identify with mild eating disorder symptoms (e.g. occasional food restriction/binging/purging behaviours [1–3 episodes per week]; American Psychiatric Association, 2013). Participants who reported moderate or severe eating disorder symptoms, or were currently receiving treatment for, and/or had ever been diagnosed with a clinical eating disorder were not eligible to take part. Thirty‐five athletes gave informed consent and started the study (female: n = 27; male: n = 8; M age = 27.1 years, SD = 8.2, range: 18–46 years). Athletes participated and competed in a range of different team and individual sports at club (n = 12), university (n = 6), regional (n = 6), national (n = 7) or international (n = 4) level. They had experienced their concerns about their eating behaviours and attitudes for an average of 5.6 years (SD = 5.1; range: 0.5–20 years).
2.3. Procedure
Following receipt of study information, and an opportunity to ask questions, participants provided informed consent and were involved in the study for 10 weeks (Figure 1). Participants were screened for eligibility at the start of the study. Only those meeting the inclusion criteria were able to proceed with the study. Participants completed an online survey at three timepoints: baseline (T1), immediately after the 6‐week intervention (T2), and 4 weeks after intervention completion (T3). After completing the T1 survey, an intervention manual and instructions were sent via post to participants. A courtesy email was sent to all participants mid‐way through the intervention to answer any questions and to promote continued engagement. At T2, all participants were invited to take part in a one‐to‐one interview on the phone/via video call. This took place within 7 days of completing the intervention. Participants were remunerated with shopping vouchers for their time spent completing measures at each timepoint (£5 voucher at T1 and T2, and a £10 voucher at T3; participants who agreed to complete the interview at T2 received an additional £10 voucher).
FIGURE 1.
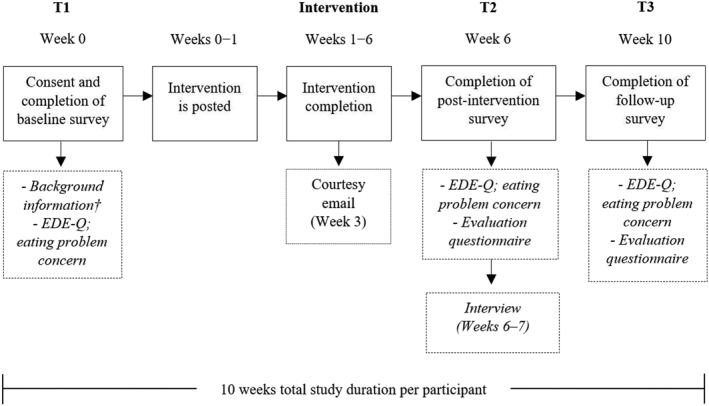
Study timeline and the measures employed at each timepoint. †Sex, age, details of sport and eating disorder history; EDE‐Q, Eating Disorder Examination Questionnaire (Fairburn & Beglin, 2008)
2.4. The intervention
Participants received a paper‐based manual (A4 booklet) of the self‐led ‘Motivational and Psycho‐Educational Self‐Help Programme for Athletes with Mild Eating Disorder Symptoms’ (MOPED‐A; see Table 1 for an outline). MOPED‐A is an athlete adapted version of the ‘Motivation and Psycho‐Educational Package for People with Eating Disorders’ (Brewin et al., 2016; Cashmore et al., 2015). MOPED‐A was comprehensively adapted using Intervention Mapping for Adaptation (IMA), a theory‐driven, evidence‐based and participant‐centred protocol for systematically adapting health interventions (Bartholomew et al., 2016). Adaptations were primarily around enhancing the contextual relevance of the intervention to an athlete/sport setting (e.g., reflection on sport performance pressures and eating disorder symptoms specific to athletes). Athletes were recommended to engage with MOPED‐A for 1–1.5 h per week for six consecutive weeks. This included reading one to two chapters a week, completing the relevant activities in each chapter, writing a summary for each chapter, and allowing some time to recap materials (nine chapters in total; Table 1). Underpinned by Motivational Enhancement Therapy (specifically, Motivational Interviewing) and Cognitive Behavioural Therapy, the goals of MOPED‐A are to motivate and encourage athletes to seek further support for their eating disorder symptoms and to help them to reduce their symptoms by making positive changes to their eating behaviours and attitudes.
TABLE 1.
Outline of the chapters included within the MOPED‐A intervention and the timeframe for completing them (6 weeks in total)
| MOPED‐A chapters | Chapter overview | Week |
|---|---|---|
| Chapter 1 | Eating problems and their symptoms | Week 1 |
| Chapter 2 | Development of eating problems | Week 2 |
| Chapter 3 | Different patterns of eating | Week 3 |
| Chapter 4 | Deciding to change or not to change | Week 3 |
| Chapter 5 | Making changes (‘how to’) | Week 4 |
| Chapter 6 | Getting rid of binges | Week 4 |
| Chapter 7 | Managing purging | Week 5 |
| Chapter 8 | Maintaining progress | Week 6 |
| Chapter 9 | Problems and solutions | Week 6 |
Note: Chapters were based on the original intervention (Cashmore et al., 2015) but the content in each chapter had been tailored to athletes.
2.5. Measures
Figure 1 indicates the timepoints that each of the measures were completed by participants and details of the measures used are provided below.
2.5.1. Recruitment, retention and acceptability of measures and research procedures
Recruitment data were recorded to determine the feasibility of recruiting participants to the study and to determine the recruitment rate (N recruited ÷ recruitment time [weeks]; Walters et al., 2017). Feasible recruitment was determined as the ability to recruit between 24 and 30 participants, which has been suggested to be sufficient for feasibility studies (Julious, 2005; Lancaster et al., 2004; Sim & Lewis, 2012). Retention data were recorded at T2 and T3 to determine the proportion of participants who were still actively participating in the study and retention was considered successful if ≥ 80% of participants were retained at T3 (Thomas et al., 2004). Measures were determined to be acceptable to participants if there was <10% missing data which was missing completely at random (Bennet, 2001), in addition to ≥80% survey completion rates at T2 and T3 (Thomas et al., 2004). Research procedures were determined acceptable if there were no significant burdens or issues raised by participants (Palmcrantz et al., 2015).
2.5.2. Process evaluation: acceptability of the intervention
The outcomes assessed in the process evaluation were informed by existing feasibility guidelines (Bowen et al., 2009; Orsmond & Cohn, 2015), and are shown in Table 2. Data were obtained via (i) an evaluation questionnaire and (ii) one‐to‐one interviews with a subsample of participants (n = 15).
TABLE 2.
Outcomes, criteria and the methods used to assess intervention acceptability (T2)
| Outcomes | Assessment criteria and data collection method used (Q = questionnaire, I = interview) |
|---|---|
|
|
|
|
| |
|
|
| |
|
|
| |
| |
|
|
| |
|
T2 evaluation questionnaire . The post‐intervention evaluation questionnaire was developed after consulting existing feasibility guidelines (Arain et al., 2010; Bowen et al., 2009; Orsmond & Cohn, 2015) and included a series of Likert‐scale, multiple‐choice and free‐text questions to assess the outcomes listed in Table 2. An example Likert‐scale question was ‘‘On a scale of 1 (strongly disagree) to 5 (strongly agree), how satisfied were you with the format of MOPED‐A being a self‐led booklet?’’. An example multiple‐choice question was ‘What time of day did you typically complete the MOPED‐A programme?’, and two example free‐text questions were ‘As a result of completing MOPED‐A, please describe any benefits/concerns to your eating behaviours that you have experienced’ and ‘How long did you typically spend each week engaging with the intervention?’.
T2 one‐to‐one interviews. A semi‐structured interview schedule with open‐ended questions and prompts was developed and finalised following a comprehensive review of the literature. Topics for discussion included participants' experiences of completing MOPED‐A to collect further data on the acceptability of the intervention (Table 2). Example interview questions were ‘What do you think makes MOPED‐A specific to athletes?’ and ‘How did you find completing the MOPED‐A programme?’. The interviews were audio recorded and ranged in duration from 20 to 41 min (M = 30.33, SD = 6.37).
T3 evaluation questionnaire. In line with the recommendations by Bowen et al. (2009), follow‐up data at T3 were obtained in relation to intervention completion rate and use (criteria: what proportion of participants report continuing to use parts of the intervention at follow‐up?) and perceived benefits from the intervention (criteria: do participants describe any sustained benefits/concerns to their eating behaviours at follow‐up?). These data were collected via multiple‐choice and free‐text questions in a refined version of the evaluation questionnaire.
2.5.3. Measures of potential efficacy
Eating Disorder Examination Questionnaire version 6.0 (EDE‐Q; Fairburn & Beglin, 2008). The EDE‐Q includes four subscales that assess eating disorder symptoms in the past 28 days: (a) restraint, (b) eating concern, (c) shape concern and (d) weight concern. The mean of the four subscales creates a global score. Additionally, the EDE‐Q measures the frequency of eating disordered behaviours in the preceding 28 days (binge eating and purging episodes were included in this study). Higher scores indicate higher levels of eating disorder symptoms. The measure has previously been used with athletes, demonstrating evidence of acceptable levels of reliability and internal consistency (Pope et al., 2015; Shanmugam et al., 2013, 2014). Cronbach alphas for the EDE‐Q global score ranged from 0.92 to 0.94 across the current study.
Level of concern about eating disorder symptoms . Participants also reported their perceived level of concern for their eating disorder symptoms on a 1–5 Likert scale (1 = not at all concerned, 5 = extremely concerned) at each timepoint (Linardon et al., 2020).
2.6. Data analyses
2.6.1. Quantitative analysis
Data from the evaluation questionnaires were analysed using descriptive analytic techniques (e.g. means, frequencies; Sebire et al., 2019). To investigate whether any missing data was completely at random, Little's MCAR test was performed and missing data were replaced using the Expectation‐Maximisation algorithm where appropriate (Schafer & Olsen, 1998). A Shapiro–Wilk test revealed all EDE‐Q data were non‐normally distributed (p < 0.05). Therefore, to investigate the potential efficacy of the intervention with study completers (n = 28), two Friedman tests were conducted and post hoc analysis with Wilcoxon signed‐ranks tests was subsequently run and effect sizes (r) computed. Mann–Whitney U analysis was conducted to examine any differences in scores on the outcome variables at T2 between interviewees and non‐interviewees. The level of statistical significance was set to p < 0.05 for all analysis. The p value was not adjusted (e.g. Bonferroni corrected) where multiple tests were conducted as statistical significance was instead interpreted alongside the magnitude of effect and study quality; consistent with evidenced recommendations (Armstrong, 2014; Feise, 2002). A sample size estimation for an intervention arm to power a future trial was manually calculated (Sullivan, 2020). The estimation was based on the EDE‐Q global score and on a 95% CI (standard normal distribution: Z = 1.96) and achieving 90% power (Z 0.90 = 1.282; Whitehead et al., 2016) with a specified 0.50 effect size to detect a large difference. Because no standardised effect sizes are available for the EDE‐Q with athletes with current eating disorder symptoms completing a self‐help intervention, the specified effect size was based on the mean effects detected for the change in EDE‐Q global score in this study, and the large effect sizes previously detected in non‐self‐help eating disorder interventions delivered to non‐clinical community athletes (Abood & Black, 2000; Becker et al., 2012; Brown et al., 2016).
2.6.2. Qualitative analysis
Free‐text response data from the evaluation questionnaires were grouped into similar categories based on content, and frequencies and descriptive summaries were produced (Sebire et al., 2019). Interviews were transcribed and analysed using framework analysis (Beard et al., 2012; Ritchie & Lewis, 2003), which is suitable for evaluating interventions, using pre‐defined themes based on pre‐determined feasibility outcomes (as per Table 2). The analysis involved four steps: (1) manual transcription and familiarisation with the data, (2) identifying and collating data around pre‐defined themes, (3) identifying a thematic framework (i.e. mapping the results to each theme), and (4) presenting descriptive accounts and illustrative quotations. Frequent discussions within the research team were held regarding the most accurate representation of the data (Graneheim & Lundman, 2004). Triangulation of the interview and questionnaire data was conducted to enhance the integrity and trustworthiness of the analyses (Williams & Morrow, 2009).
3. RESULTS
3.1. Feasibility of MOPED‐A
3.1.1. Recruitment and retention
The recruitment strategy included contacting key personnel (e.g. the presidents, management and/or administrators) from 143 sport organisations and clubs across the United Kingdom to invite them to share the study information with their athletes and sport professionals via email, social media or through team/staff meetings. Sixty‐one organisations and clubs (43%) responded to the request and agreed to share the study information. Additionally, social media was used, which included a total of 40 posts advertising the study (e.g. via Twitter and Facebook) and four Twitter posts tagged key UK sporting organisations. Advertisements were posted in specific groups or on specific pages (e.g. special interest groups and pages that focussed on sport and/or eating disorders), with approval from the administrators.
Over a 5‐week period, 60 athletes expressed an interest in the study via email. Of these, 35 (58%) were eligible and successfully entered the study (Figure 2). Of the remaining 25 athletes, 12 did not meet one or more of the inclusion criteria (e.g. currently not participating in sport, did not self‐identify with mild eating disorder symptoms, and/or had previously been diagnosed with an eating disorder) and 13 individuals subsequently decided not to participate in the study (these individuals met the inclusion criteria, were sent information about the study and the intervention, but subsequently did not give their consent). Most of the enrolled athletes reported that they came across the study on social media (74%). An average recruitment rate of seven participants per week was achieved. Twenty‐eight participants (80%; female: n = 23, male: n = 5) completed the study, while seven participants (female: n = 4, male: n = 3) dropped out (see Figure 2). One participant dropped out 3 weeks into the intervention (they made the decision to seek other, more intense treatment for their eating disorder symptoms), five participants did not complete the T2 survey, and one did not complete the T3 survey despite email reminders. Reasons why these six participants dropped out are unknown.
FIGURE 2.
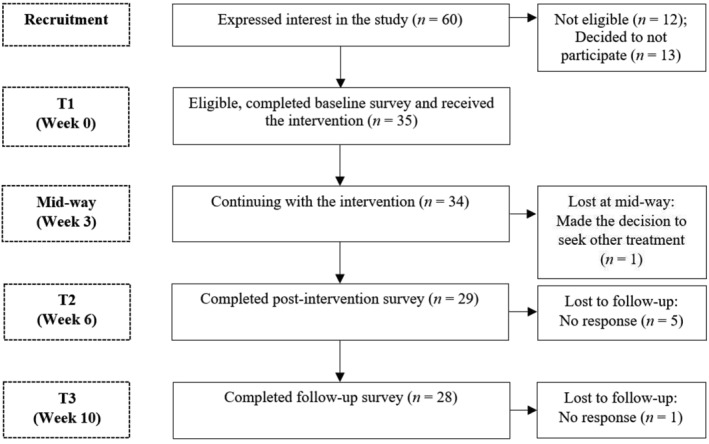
Participant progress through the study
3.1.2. Acceptability of measures and research procedures
Participant response data indicated a high acceptability of measures; missing data were minimal (5.2%) and Little's MCAR test demonstrated that this was completely at random (p > 0.05) and therefore replaced. A high proportion of participants completed the online surveys at T2 (n = 29; 83%) and T3 (n = 28; 96%). None of the participants reported any issues or perceived burdens with any of the study procedures.
3.1.3. Process evaluation: acceptability of the intervention
The results from the process evaluation are presented according to the outcomes listed in Table 2. Twenty‐nine participants completed the evaluation questionnaire at T2; 15 of these participants (52%; female: n = 14; male: n = 1; M age = 25.8 years, SD = 8.06, range: 18–46 years) also completed an interview and chose to do this over the phone. Twenty‐eight participants completed the follow‐up survey at T3. Quantitative and qualitative data from the evaluation questionnaires and interviews are presented concurrently for clarity and to demonstrate consistency and/or contrasting results from these two sources.
-
(a)
Satisfaction and enjoyment . Participant responses on the T2 evaluation questionnaire (n = 29) indicated a high level of satisfaction with the intervention format (1–5 Likert scale [5 = strongly agree]; M = 4.48, SD = 0.87) and that they enjoyed engaging with the intervention (1–5 Likert scale [5 = strongly agree]; M = 4.24, SD = 0.63). Satisfaction with the format and delivery of the intervention as a hard copy manual was further underpinned by feedback from 11 of the 15 interviewees, for example,: ‘I liked having a booklet, it felt like the programme was personal to me, like it's mine now and I can refer back to it whenever I feel the need to’ (female, 20‐year‐old). Furthermore, all 15 interviewees discussed how engaging with the intervention was a positive experience overall, for example: ‘I enjoyed reading through and doing the activities. I really liked how the programme put you in control of making your own decisions, I felt that was quite motivating’ (Female, 23‐year‐old).
-
(b)
Intervention completion rate and use . The T2 evaluation questionnaire data showed that 22 of 29 participants (76%) fully completed all nine MOPED‐A chapters and associated activities. Completion of individual chapters was generally high with ≥79% of participants completing chapters 1–5, 8 and 9, while 72% and 69% of participants completed chapters 6 and 7, respectively. Twenty‐eight participants (96%) reported engaging with the intervention for the recommended duration (6 weeks) and completed the programme in that timeframe. On average, participants reported spending a total of 1.7 h (SD = 0.46) each week engaging with MOPED‐A, which is consistent with the guidance provided. The acceptability of the intervention dosage was further highlighted by most interviewees (n = 13), for example: ‘Engaging for around two hours a week is very feasible for most athletes, and the six weeks allows you to revisit certain bits and to actually see the effects and progress as a result of your efforts’ (Female, 27‐year‐old).
At T3 (n = 28), most participants (n = 25; 89%) reported continuing to use the principles and/or activities of MOPED‐A. Additionally, three‐quarters of participants (n = 21; 75%) also reported that they continued to refer back to the content of MOPED‐A for ongoing support or guidance, ranging between one and eight times over the past month (M = 3.5, SD = 2.1 times/month).
-
(c)
Practicality of the intervention. Most participants (n = 26; 90%) reported completing the intervention from home in the afternoons or evenings. Furthermore, most interviewees (n = 13) reported that having flexibility around engaging with the intervention helped facilitate engagement and their continuation with the programme. For example, one 21‐year‐old female said: ‘I think MOPED‐A is unique in that you can work on it when it best suits you and at your own pace, which helps when you have training, coach meetings and other stuff to do most days. It was a feasible way of engaging with support which definitely helped me stick to the programme’.
Eight interviewees incorporated completing the intervention into their routine (e.g. to fit with other weekly/daily commitments), whereas the other seven reported engaging with the intervention when they had the time (i.e. no specific routine). Most participants (90%) did not request further guidance or instruction whilst completing the intervention, suggesting that the instructions were largely clear and sufficient. Three participants (10%) sent an email to the lead researcher within the first 2 weeks of having started the intervention and requested additional guidance around completing it. 12 interviewees emphasised the clarity of the instructions and guidance provided to them, for example: ‘All the instructions around when and how to use MOPED‐A were very clear. I wasn't at any point unclear on what to do’ (Female, 21‐year‐old).
-
(d)Intervention relevance, preferences and refinements . All 15 interviewees endorsed the relevance of MOPED‐A, suggesting this was largely due to its focus on sports and training. 12 interviewees highlighted this to be an important facilitating factor for them in following through with the programme. One 25‐year‐old female reflected:The content was very focussed on the physical and mental effects of eating problems on general life but also sports and training. So, to have something that was athlete‐specific was quite useful. The content was very much related to my experiences, and it made me more engaged.Most interviewees (n = 13) found chapters 1–5 of MOPED‐A to be very helpful because the content allowed them to understand their problem(s) with eating and subsequently come to realise why making changes was important, for example: ‘The first few chapters made me think about my eating problems, especially the consequences of restriction, RED‐S [Relative Energy Deficiency in sport] and binging. I already knew my behaviours weren't healthy, and MOPED‐A kind of gave me that push to start doing something about it’ (male, 29‐year‐old). Half of the interviewees (n = 8) perceived chapter 7 (purging) of MOPED‐A as less helpful because they did not currently identify with purging behaviours (particularly vomiting and use of laxatives). However, for those that did experience purging (and binging), chapter 7 and other intervention elements were perceived as helpful for addressing their symptoms. For example, one 19‐year‐old female reflected:I found the purging and binging chapters and the diary asking you to record 'food and drink consumed' [and asking] 'did you binge, purge?' to be very useful. I kept this diary as part of my daily routine as I found it a healthy way to track negative behaviours and thoughts. The restrict and binge purge cycle allowed me to have a better understanding and to recognise my eating patterns.
Interviewees also suggested some refinements to consider should the study proceed to a larger trial. Six interviewees believed more frequent email (or phone/text message) reminders or check‐ups (e.g. once a week) would be a useful reminder to engage with MOPED‐A. Eight interviewees suggested incorporating signposting towards supplemental online resources (e.g. articles, video clips) to gain a deeper understanding of areas of interest (e.g. relative energy deficiency in sport). Six interviewees suggested that supplying an electronic version of the intervention along with the hard‐copy manual could make the programme more accessible (e.g. when travelling for competition).
-
(e)
Perceived benefits from the intervention . In response to the statement ‘MOPED‐A has helped me understand my eating problem(s)’ at T2, participants reported a generally high level of agreement (1 = strongly disagree, 5 = strongly agree; M = 4.31, SD = 0.66). They also reported concordance at T2 with the statement ‘I now feel more able to change my eating problem(s)’ (M = 3.72, SD = 0.99) and with the statement ‘MOPED‐A has helped me reduce symptoms of my eating problem(s)’ (M = 3.55, SD = 0.91). 11 of 29 participants (38%) indicated at T2 that they had made the decision to disclose their eating disorder symptoms and to seek further support from a friend or family member (n = 6), their sport club (n = 2), and/or a professional (n = 9) as a result of completing the intervention. A further 12 participants (41%) reported already having adequate support and that they felt more in control of their eating disorder symptoms since completing the intervention, while the remaining six participants gave no answer.
Most participants at T2 (n = 27; 93%) and T3 (n = 26; 93%) described experiencing a small number of perceived benefit(s) to their eating and/or exercise behaviours at T2 and/or T3. These benefits were classified into seven different categories: (a) feeling more in control over their eating behaviours (T2: n = 13, T3: n = 11); (b) eating more regularly throughout the day (T2: n = 4, T3: n = 7); (c) feeling a reduced urge to binge (T2: n = 4, T3: n = 5); (d) fuelling better for exercise (T2: n = 4, T3: n = 5); (e) improved meal and snack planning (T2: n = 5, T3: n = 4); (f) engaging less in excessive exercise behaviours (T2: n = 3, T3: n = 4); and (g) feeling a reduced urge to purge (T2: n = 1, T3: n = 3). None of the participants reported a worsening of their symptoms over the course of the study. However, two participants at T2 and two at T3 reported experiencing no perceived benefits at all; reasons were not provided. Additionally, five participants who did experience benefits also reported still thinking a lot about their eating disorder symptoms and finding it difficult to change their eating habits at T2. Finally, 11 interviewees highlighted the overall benefit on their lives of completing the intervention, for example:I am now much happier in myself. I enjoy eating for the first time in a long time. I no longer wake up at night to eat or eat large amounts in the evening or very little in the day. My health and my running have improved, and I am much stronger and more capable to address my [eating] problem now (Female, 23‐year‐old).
3.2. Potential efficacy of MOPED‐A
3.2.1. Changes in eating disorder symptoms across the study
Participants' EDE‐Q global, restraint, eating and shape concern scores significantly reduced from T1 to T2, in addition to weight concern scores decreasing from T1 to T3 (large effect sizes; Table 3). There were no significant changes in EDE‐Q scores from T2 to T3. In addition, on diagnostic items of the EDE‐Q, there was a significant reduction in reported binge eating episode frequency from T1 to T3 and from T2 to T3 (large effect sizes). No significant reduction in participants' purging frequency was detected across the study. Furthermore, participants' perceived level of concern for their eating disorder symptoms significantly reduced from T1 to T2, T1 to T3 and from T2 to T3 (large effect sizes; see Table 3). When comparing the scores on all outcome variables between interviewees (n = 15) and non‐interviewees (n = 14) at T2, Mann–Whitney U analysis revealed there were no significant differences (p > 0.05) between the two groups on any of the outcome variables.
TABLE 3.
Mean scores and standard deviations for all outcome variables and differences in these across all three timepoints (n = 28)
| Outcome variables | Timepoints | Differences | |||||
|---|---|---|---|---|---|---|---|
| Baseline (T1) | Post (T2) | Follow‐up (T3) | Overall | T1−T2 | T1−T3 | T2−T3 | |
| M (SD) | M (SD) | M (SD) | χ 2 | Z [r] | Z [r] | Z [r] | |
| EDE‐Q global | 3.17 (1.21) | 2.34 (1.25) | 1.91 (1.22) | 9.92** | 2.41* [0.45] | 2.93** [0.55] | 1.27 [0.24] |
| Restraint | 2.89 (1.48) | 1.73 (1.05) | 1.60 (1.19) | 9.23** | 2.60** [0.49] | 2.63** [0.50] | 0.35 [0.06] |
| Eating concern | 2.69 (1.27) | 1.97 (1.35) | 1.42 (1.18) | 12.51** | 2.18* [0.41] | 2.94** [0.55] | 1.63 [0.30] |
| Shape concern | 3.75 (1.55) | 2.91 (1.68) | 2.37 (1.61) | 6.50* | 2.22* [0.41] | 2.57** [0.48] | 1.05 [0.19] |
| Weight concern | 3.37 (1.36) | 2.75 (1.58) | 2.27 (1.47) | 3.35 | 1.82 [0.34] | 2.70** [0.51] | 1.15 [0.21] |
| Binge eating episodes (days) a | 5.26 (5.90) | 4.07 (4.64) | 2.04 (2.53) | 6.02* | 0.88 [0.16] | 2.51* [0.48] | 2.07* [0.39] |
| Purging behaviours (times) a | 3.29 (3.80) | 2.74 (2.92) | 1.81 (2.58) | 1.98 | 0.09 [0.01] | 1.64 [0.31] | 1.34 [0.25] |
| Level of concern about eating disorder symptoms b | 3.34 (0.68) | 2.93 (0.99) | 2.39 (0.83) | 18.70*** | 2.14* [0.40] | 4.04*** [0.76] | 2.11* [0.39] |
Frequency at which participants experienced a binge eating episode (days) or purged (times) in the past 28 days.
Participants' self‐reported level of concern for their eating disorder symptoms on a 1–5 Likert scale (1 = not at all concerned, 5 = extremely concerned); EDE‐Q, Eating Disorder Examination Questionnaire.
*p < 0.05; **p < 0.01; ***p < 0.001.
3.2.2. Sample size estimation for a future controlled trial
The estimated sample size was calculated where n (1.96 + 1.282 ÷ 0.50)2 = 43, which will ensure that a two‐tailed repeated measures test with a p < 0.05 has 90% power to detect a large (r = 0.50) difference in EDE‐Q global score. However, to account for a 20% dropout rate over time, as detected in this study, a minimum sample size of n = 50 should be recruited for the intervention arm at baseline to ensure 43 participants can be retained for analysis.
4. DISCUSSION
The primary aim of this study was to assess the feasibility of undertaking a study evaluating the MOPED‐A intervention. Key objectives were to explore the feasibility of recruiting and retaining participants in the study, and to evaluate the acceptability of measures, research procedures and the intervention. A secondary aim was to explore the potential efficacy of MOPED‐A in reducing eating disorder symptoms in athletes. Findings suggest that recruitment was successful and that an acceptable proportion of participants (80%) could be retained and completed all measures. Participants reported satisfaction with completing MOPED‐A and further highlighted that the format, delivery, content, and dosage of the intervention were acceptable. Large reductions in eating disorder symptoms were detected in participants immediately after the intervention and were sustained at follow‐up.
This is the first known study to recruit athletes with mild eating disorder symptoms to take part in a newly developed self‐help intervention and it has demonstrated success in doing so. The recruitment target was met and slightly surpassed with an average recruitment rate of seven participants per week; recruitment was therefore determined to be feasible over a relatively short period of time. The current study also demonstrated an ability to retain participants over a 10‐week period with an acceptable retention rate of 80% (Thomas et al., 2004). This is comparable with other eating disorder self‐help intervention studies (e.g. 75%; Beintner et al., 2014) but higher than many face‐to‐face disordered eating intervention studies with athletes (mean 72%; Sandgren et al., 2020). Many factors can impact retention, however, the current study provided flexibility around the time of day for engaging with the intervention and completing measures, used one electronic reminder mid‐way through the intervention, and compensated participants for their time to complete measures; all of which are suggested to facilitate retention (Duncan et al., 2020; Zweben et al., 2009). Additionally, participants demonstrated good compliance with completing study measures at each timepoint (≥83%) which was above the required threshold of 80% (Thomas et al., 2004). No concerns or burdens with the study requirements were identified, suggesting acceptability of the chosen measures and research procedures (Palmcrantz et al., 2015) and that these can be feasibly used in future.
The process evaluation highlighted that all participants were satisfied with the format and mode of delivery of the MOPED‐A intervention. These results are encouraging given the evidence of variable acceptability of the face‐to‐face group‐based approach of existing athlete disordered eating interventions (Becker et al., 2012; Brown et al., 2016; Gorrell et al., 2021). However, evidence for the acceptability of existing athlete interventions, as well as details around how the development of these informed the final format and mode of delivery, was previously lacking. In contrast, MOPED‐A was extensively developed in collaboration with the target group and key stakeholders (using IMA; Bartholomew et al., 2016); a likely key factor behind finding evidence of its acceptability. Additionally, the intervention completion rate of 76% met the requirement for acceptable intervention completion (i.e. ≥75%; Beintner et al., 2014; Burnette & Mazzeo, 2020) and is also much higher than that found with other eating disorder self‐help interventions delivered to the general population (e.g. 50%; Beintner et al., 2014). This may be because athletes in the current study emphasised the content of MOPED‐A to be highly relevant and tailored to them, which has been recommended to enhance the relevance of interventions for this population (Arthur‐Cameselle & Quatromoni, 2014; Biggin et al., 2017; Hines et al., 2019; Plateau et al., 2017). This reinforces that by adopting a participatory approach to the intervention development process, as was taken here, researchers and practitioners can effectively tailor their interventions to the target populations' social context (Bartholomew et al., 2011).
Furthermore, flexibility around engaging with MOPED‐A was highlighted by participants to be a key facilitating factor in them continuing with the programme (i.e. they could plan engagement around their schedules). This is consistent with other, non‐athletes’ experiences of completing self‐help interventions for disordered eating (Yim & Schmidt, 2019), and is an important finding given that fixed participation days/times in face‐to‐face group‐based disordered eating interventions can negatively affect athletes' engagement (Abood & Black, 2000). It is therefore important that researchers and practitioners gather and consider the views of the target population to ensure interventions are in line with their preferences around intervention delivery and structure (Merlin et al., 2017) so that interventions can be more acceptable and successful for participants (Janols & Lindgren, 2017). The acceptability of MOPED‐A was further reinforced in the current study by the finding that a large proportion of participants continued to use the manual 1 month after completing the intervention. This is promising and may suggest ongoing relevance and value of MOPED‐A to athletes with mild eating disorder symptoms (Fleming et al., 2018). However, longer‐term follow‐up assessments will be useful to include in future to explore any sustained or reduced rates of continued intervention use and how this may influence longer‐term efficacy.
Some minor intervention refinements were highlighted (e.g. signposting towards supplemental resources, supplying an electronic copy of the manual and receiving more frequent reminders). These suggestions are relatively simple to implement, yet they may pose some challenges for researchers in relation to future implementation and testing (e.g. linking to reputable, valid and previously tested resources; delivering the intervention in a dual format; additional resource demands). Participants were satisfied with the provision of a hard copy manual, although this may present an issue around sustainability if rolled out on a large scale in future. Researchers may therefore need to explore the feasibility and acceptability of an electronic copy of MOPED‐A before it can be offered to, and tested with, participants as part of a larger trial. The current findings highlight the value in rigorously evaluating the feasibility (using mixed methods) of new interventions to detect any potential refinements needed to the intervention prior to larger scale testing or implementation (Tickle‐Degnen, 2013).
The process evaluation further revealed that almost all participants who completed the intervention reported experiencing at least one positive, sustained benefit to their eating behaviours and attitudes (e.g. feeling more in control of their eating problem), and no participants reported any negative consequences on their eating behaviours. This points to the perceived usefulness of the intervention to participants (Bowen et al., 2009), which likely facilitated their motivation to continue with the programme. Of significant importance is that just over a third of participants who completed MOPED‐A reported having disclosed their eating difficulties and made the decision to seek further support as a result. This is a positive finding and confirms that the MOPED‐A intervention targets its primary goal (i.e. to encourage symptom disclosure and motivate further treatment seeking in participants). However, this finding could also suggest that some athletes still lacked the courage or motivation to take further action, and the reasons why athletes do or do not decide to disclose their symptoms to relevant people and seek further support should be explored in more detail in future. This is important given that symptom disclosure has been identified as a key first step in accessing subsequent support for an eating disorder, irrespective of symptom severity (Gilbert et al., 2012).
Regarding the potential efficacy of MOPED‐A, large reductions in eating disorder symptoms were detected in participants immediately after the intervention and these were sustained at follow‐up. Although controlled, most existing intervention studies with athletes where the interventions are similar in duration to MOPED‐A (i.e., 4–8 weeks) typically report small to moderate reductions (Sandgren et al., 2020). The current study further found large reductions in participants' binge eating frequency at follow‐up (but not immediately post intervention), suggesting that this behaviour may take longer to change as previously suggested with non‐athlete populations (Murphy et al., 2012). Additionally, large reductions in athletes' perceived concern about their eating disorder symptoms were detected across the study. This is consistent with other eating disorder self‐help intervention studies which report reduced levels of psychological distress in participants at follow‐up (Carter et al., 2020). Consistent with previous non‐athlete eating disorder intervention development research (Shaw & Stice, 2016; Stice et al., 2013), the promising efficacy results in the current study are likely a product of the participatory approach adopted for the development of MOPED‐A. However, and importantly, future controlled studies are needed to determine the true efficacy of MOPED‐A in reducing eating disorder symptoms, but also to explore any potential cross‐over effects (e.g. compulsive exercise).
Additionally, because athletes in the current study were likely highly motivated to initiate change because they self‐referred themselves to the study and the intervention, future research should explore ways to reach those that lack the motivation to initiate change. It will also be important for future research to explore the characteristics/traits of those who self‐refer to the intervention and to identify for whom the intervention may be most effective (e.g. athletes with restriction vs. bulimic‐like symptoms; longer vs. shorter duration of symptoms; motivated vs. less motivated athletes; younger vs. older). Comparably, the current study estimated that 50 participants should be recruited at baseline to an intervention arm to power a future trial, and recruitment of a control group will also be required. Exploring whether magnitude of changes is consistent across sex may also be relevant for sample size estimations and useful for determining whether a sex stratified analytic approach will be necessary in future.
Furthermore, the mean baseline EDE‐Q score was 3.17 in the current study. This is lower than what is typically seen in clinical samples (e.g. global scores of 3.92–3.98; Jennings & Phillips, 2017; Lichtenstein et al., 2021) but higher than what is typically observed in non‐clinical, community athlete samples (e.g. global scores of 0.89–2.50; Gorrell et al., 2021; Lichtenstein et al., 2021). This confirms that participants in our study reported experiencing mild eating disorder symptoms. While the MOPED‐A intervention seems to be successful at reducing eating disorder symptoms, it is noteworthy that the mean follow‐up EDE‐Q global score in the present study was still relatively high (M = 1.91), albeit this may be typical with athlete samples (Gorrell et al., 2021).
This is the first study to have delivered and tested a novel, athlete‐specific self‐help intervention with a wide range of male and female athletes with mild eating disorder symptoms. The current study is also the first to report on an eating disorder intervention delivered to athletes in the United Kingdom. A key strength is the array of feasibility outcomes that have been evaluated quantitatively and qualitatively. This study also adheres to published guidelines for study reporting (Eldridge et al., 2016; Lancaster & Thabane, 2019) to ensure research processes and findings are accurately described, thereby addressing a limitation with previous work in this area (Sandgren et al., 2020). However, one potential confounding variable in the current study is the lockdown restrictions placed in the United Kingdom in late March 2020 due to the coronavirus pandemic (COVID‐19; World Health Organisation, 2020). This meant that for much of the study period (March–May 2020), participants were instructed by the UK government to self‐isolate (i.e. stay at home and away from others; Iacobucci, 2020). Exercising in groups where it was not possible to adhere to social distancing rules was not allowed during this period. It is plausible that the lockdown restrictions, to some degree, impacted participants' engagement with the intervention. However, despite the limitations and challenges with conducting research at the start of a pandemic, the evidence presented here suggests that MOPED‐A could be a practical tool for delivering support to at‐risk athletes remotely, both now and in the future. Indeed, self‐help interventions are increasingly being recommended as a valuable source of support (Murphy et al., 2020) and may hold more value than ever in the face of continuing needs for physical distancing.
Additionally, this study only measured whether participants had disclosed their eating disorder symptoms and decided to seek further support immediately after completing the intervention. Given the high rate of continued intervention use detected in this study, participants' symptom disclosure and support seeking behaviours and attitudes should also be assessed at subsequent follow‐up assessments to ascertain if some athletes make these important decisions later. Furthermore, most participants were recruited via social media which could mean that the sample was already motivated to address their eating disorder symptoms. Future research should therefore measure participants' level of motivation and assess this against the recruitment methods used to ascertain which groups of athletes are ‘easier’ and ‘harder’ to recruit and retain. Finally, the high variability in behavioural eating disorder symptoms in the current sample suggests value in future research with larger samples to test the efficacy of the intervention for a wide range of athletes.
In conclusion, carefully assessing the feasibility of new eating disorder interventions should be the norm for all future intervention development (for athletes and non‐athletes alike). Grounding interventions in evidence and participant perspectives will be particularly important for those seeking to develop targeted and impactful interventions. The findings presented here demonstrate that the MOPED‐A intervention can be feasibly implemented, is acceptable to athletes with mild eating disorder symptoms, and shows good potential for motivating further treatment seeking and helping to reduce symptoms. Collectively, these findings suggest additional testing of MOPED‐A is worthwhile and provide the foundation for conducting a larger controlled trial, which is now warranted (i.e. will the intervention work and to what extent?). In doing so, this will build on the current study's findings and provide further evidence for the efficacy of MOPED‐A as a useful, scalable early intervention alternative in supporting athletes with mild eating disorder symptoms.
CONFLICT OF INTEREST
The authors have no financial or non‐financial competing interests to declare.
PARTICIPANT CONSENT STATEMENT
Every participant in this study provided informed written consent prior to taking part in the research.
ACKNOWLEDGEMENTS
We would like to acknowledge Dr Rebecca Cashmore and Tara Cousins from the Leicester Adult Eating Disorders Service and the Leicestershire Partnership NHS Trust as the original developers of MOPED. We would also like to thank Rhona Pearce and Andrew Shepherd from the Sports Development Centre, Loughborough University, for their support in facilitating participant recruitment. Dr Sebastian S. Sandgren was supported by a PhD studentship from the School of Sport, Exercise and Health Sciences, Loughborough University. This research was also supported by the NIHR Leicester Biomedical Research Centre.
Sandgren, S. S. , Haycraft, E. , Arcelus, J. , & Plateau, C. R. (2022). Evaluating a motivational and psycho‐educational self‐help intervention for athletes with mild eating disorder symptoms: A mixed methods feasibility study. European Eating Disorders Review, 30(3), 250–266. 10.1002/erv.2891
DATA AVAILABILITY STATEMENT
Due to the nature of this research, participants in this study did not agree for their data to be shared publicly, so supporting data are not available.
REFERENCES
- Aardoom, J. J. , Dingemans, A. E. , & Van Furth, E. F. (2016). E‐health interventions for eating disorders: Emerging findings, issues, and opportunities. Current Psychiatry Reports, 18(4), 1–8. 10.1007/s11920-016-0673-6 [DOI] [PubMed] [Google Scholar]
- Abood, D. A. , & Black, D. R. (2000). Health education prevention for eating disorders among college female athletes. American Journal of Health Behavior, 24(3), 209–219. 10.5993/AJHB.24.3.6 [DOI] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Anderson, C. , & Petrie, T. A. (2012). Prevalence of disordered eating and pathogenic weight control behaviors among NCAA division I female collegiate gymnasts and swimmers. Research Quarterly for Exercise & Sport, 83(1), 120–124. 10.1080/02701367.2012.10599833 [DOI] [PubMed] [Google Scholar]
- Arain, M. , Campbell, M. J. , Cooper, C. L. , & Lancaster, G. A. (2010). What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Medical Research Methodology, 10(1), 1–7. 10.1186/1471-2288-10-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong, R. A. (2014). When to use the Bonferroni correction. Ophthalmic and Physiological Optics, 34(5), 502–508. 10.1111/opo.12131 [DOI] [PubMed] [Google Scholar]
- Arthur‐Cameselle, J. N. , & Quatromoni, P. A. (2014). A qualitative analysis of female collegiate athletes’ eating disorder recovery experiences. The Sport Psychologist, 28(4), 334–346. 10.1123/tsp.2013-0079 [DOI] [Google Scholar]
- Attard, S. M. , Herring, A. H. , Howard, A. G. , & Gordon‐Larsen, P. (2013). Longitudinal trajectories of BMI and cardiovascular disease risk: The national longitudinal study of adolescent health. Obesity, 21(11), 2180–2188. 10.1002/oby.20569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholomew Eldrigde, L. K. , Markham, C. M. , Ruiter, R. A. C. , Fernàndez, M. E. , Kok, G. , & Parcel, G. S. (2016). Planning health promotion programs: An Intervention Mapping approach (4th ed.). Wiley. [Google Scholar]
- Bartholomew, L. K. , Parcel, G. S. , Kok, G. , Gottleib, N. H. , & Fernandez, M. E. (2011). Planning health promotion programs: An intervention mapping approach. Jossey‐Bass. [Google Scholar]
- Beard, E. , Vangeli, E. , Michie, S. , & West, R. (2012). The use of nicotine replacement therapy for smoking reduction and temporary abstinence: An interview study. Nicotine & Tobacco Research, 14(7), 849–856. 10.1093/ntr/ntr297 [DOI] [PubMed] [Google Scholar]
- Becker, C. B. , McDaniel, L. , Bull, S. , Powell, M. , & McIntyre, K. (2012). Can we reduce eating disorder risk factors in female college athletes? A randomized exploratory investigation of two peer‐led interventions. Body Image, 9(1), 31–42. 10.1016/j.bodyim.2011.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beintner, I. , Jacobi, C. , & Schmidt, U. H. (2014). Participation and outcome in manualized self‐help for bulimia nervosa and binge eating disorder—A systematic review and metaregression analysis. Clinical Psychology Review, 34(2), 158–176. 10.1016/j.cpr.2014.01.003 [DOI] [PubMed] [Google Scholar]
- Bennett, D. A. (2001). How can I deal with missing data in my study? Australian & New Zealand Journal of Public Health, 25(5), 464–469. 10.1111/j.1467-842X.2001.tb00294.x [DOI] [PubMed] [Google Scholar]
- Biggin, I. J. , Burns, J. H. , & Uphill, M. (2017). An investigation of athletes’ and coaches’ perceptions of mental ill‐health in elite athletes. Journal of Clinical Sport Psychology, 11(2), 126–147. 10.1123/jcsp.2016-0017 [DOI] [Google Scholar]
- Bowen, D. J. , Kreuter, M. , Spring, B. , Cofta‐Woerpel, L. , Linnan, L. , Weiner, D. , Kaplan, C. P. , Squiers, L. , Fabrizio, C. , & Fernandez, M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. 10.1016/j.amepre.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bratland‐Sanda, S. , & Sundgot‐Borgen, J. (2013). Eating disorders in athletes: Overview of prevalence, risk factors and recommendations for prevention and treatment. European Journal of Sport Science, 13(5), 499–508. 10.1080/17461391.2012.740504 [DOI] [PubMed] [Google Scholar]
- Brewin, N. , Wales, J. , Cashmore, R. , Plateau, C. R. , Dean, B. , Cousins, T. , & Arcelus, J. (2016). Evaluation of a motivation and psycho‐educational guided self‐help intervention for people with eating disorders (MOPED). European Eating Disorders Review, 24(3), 241–246. 10.1002/erv.2431 [DOI] [PubMed] [Google Scholar]
- Brown, K. N. , Wengreen, H. J. , Beals, K. A. , & Heath, E. M. (2016). Effects of peer‐education on knowledge of the female athlete triad among high school track and field athletes: A pilot study. Women in Sport & Physical Activity Journal, 24(1), 1–6. 10.1123/wspaj.2014-0058 [DOI] [Google Scholar]
- Burnette, C. B. , & Mazzeo, S. E. (2020). An uncontrolled pilot feasibility trial of an intuitive eating intervention for college women with disordered eating delivered through group and guided self‐help modalities. International Journal of Eating Disorders, 53, 1–1417. 10.1002/eat.23319 [DOI] [PubMed] [Google Scholar]
- Carter, J. C. , Kenny, T. E. , Singleton, C. , Van Wijk, M. , & Heath, O. (2020). Dialectical behavior therapy self‐help for binge‐eating disorder: A randomized controlled study. International Journal of Eating Disorders, 53(3), 451–460. 10.1002/eat.23208 [DOI] [PubMed] [Google Scholar]
- Cashmore, R. , Cousins, T. , & Arcelus, J. (2015). Motivation and psychoeducational package for people with eating disorders. Leicestershire Partnerships NHS Trust. https://www.leicestereatingdisorders.co.uk/uploads/uploads/175_patient_info_‐_moped_phtocopy_friendly_august_2019_‐_august_2019.pdf (leicestereatingdisorders.co.uk) [Google Scholar]
- Clausen, L. , Lübeck, M. , & Jones, A. (2013). Motivation to change in the eating disorders: A systematic review. International Journal of Eating Disorders, 46(8), 755–763. 10.1002/eat.22156 [DOI] [PubMed] [Google Scholar]
- Dooley‐Hash, S. , Adams, M. , Walton, M. A. , Blow, F. C. , & Cunningham, R. M. (2019). The prevalence and correlates of eating disorders in adult emergency department patients. International Journal of Eating Disorders, 52(11), 1281–1290. 10.1002/eat.23140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan, E. M. , Bennett, T. , & Gillies, K. (2020). Assessing effective interventions to improve trial retention: Do they contain behaviour change techniques? Trials, 21(1), 1–9. 10.1186/s13063-020-4151-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldridge, S. M. , Chan, C. L. , Campbell, M. J. , Bond, C. M. , Hopewell, S. , Thabane, L. , & Lancaster, G. A. (2016). CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ, 355, i5239. 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G. , & Beglin, S. (2008). Eating disorder examination questionnaire (EDE‐Q 6.0). In Fairburn C. G. (Ed.), Cognitive behavior therapy and eating disorders (pp. 309–314). Guildford Press. [Google Scholar]
- Feise, R. J. (2002). Do multiple outcome measures require p‐value adjustment? BMC Medical Research Methodology, 2, 8 10.1186/1471-2288-2-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons‐Craft, E. E. (2011). Social psychological theories of disordered eating in college women: Review and integration. Clinical Psychology Review, 31(7), 1224–1237. 10.1016/j.cpr.2011.07.011 [DOI] [PubMed] [Google Scholar]
- Flatt, R. E. , & Taylor, C. B. (2018). Adapting a technology‐based eating disorder model for athletes. Journal of Clinical Sport Psychology, 12(4), 699–717. 10.1123/jcsp.2018-0015 [DOI] [Google Scholar]
- Fleming, T. , Bavin, L. , Lucassen, M. , Stasiak, K. , Hopkins, S. , & Merry, S. (2018). Beyond the trial: Systematic review of real‐world uptake and engagement with digital self‐help interventions for depression, low mood, or anxiety. Journal of Medical Internet Research, 20(6), e199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert, N. , Arcelus, J. , Cashmore, R. , Thompson, B. , Langham, C. , & Meyer, C. (2012). Should I ask about eating? Patients' disclosure of eating disorder symptoms and help‐seeking behaviour. European Eating Disorders Review, 20(1), 80–85. 10.1002/erv.1143 [DOI] [PubMed] [Google Scholar]
- Gorrell, S. , Schaumberg, K. , Boswell, J. F. , Hormes, J. M. , & Anderson, D. A. (2021). Female athlete body project intervention with professional dancers: A pilot trial. Eating Disorders, 29(1), 56–73. 10.1080/10640266.2019.1632592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim, U. H. , & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112. 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- Greenleaf, C. , Petrie, T. A. , Carter, J. , & Reel, J. J. (2009). Female collegiate athletes: Prevalence of eating disorders and disordered eating behaviors. Journal of American College Health, 57(5), 489–496. 10.3200/JACH.57.5.489-496 [DOI] [PubMed] [Google Scholar]
- Hines, J. C. , Wendorf, W. L. , Hennen, A. N. , Hauser, K. L. , Mitchell, M. M. , & Homa, J. M. (2019). How do lean and non‐lean female collegiate athletes view the eating disorder education they receive from their coaches. International Journal of Sports Science & Coaching, 14(2), 169–178. 10.1177/1747954118825060 [DOI] [Google Scholar]
- Iacobucci, G. (2020). Covid‐19: UK lockdown is “crucial” to saving lives, say doctors and scientists. BMJ, 368, m1204. 10.1136/bmj.m1204 [DOI] [PubMed] [Google Scholar]
- Janols, R. , & Lindgren, H. (2017). A method for co‐designing theory‐based behaviour change systems for health promotion. Student Health Technology Informatics, 235, 368–372. [PubMed] [Google Scholar]
- Jennings, K. M. , & Phillips, K. E. (2017). Eating disorder examination–questionnaire (EDE–Q): Norms for clinical sample of female adolescents with anorexia nervosa. Archives of Psychiatric Nursing, 31(6), 578–581. 10.1016/j.apnu.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joy, E. , Kussman, A. , & Nattiv, A. (2016). 2016 update on eating disorders in athletes: A comprehensive narrative review with a focus on clinical assessment and management. British Journal of Sports Medicine, 50(3), 154–162. 10.1136/bjsports-2015-095735 [DOI] [PubMed] [Google Scholar]
- Julious, S. A. (2005). Sample size of 12 per group rule of thumb for a pilot study. Pharmaceutical Statistics: The Journal of Applied Statistics in the Pharmaceutical Industry, 4(4), 287–291. 10.1002/pst.185 [DOI] [Google Scholar]
- Kaufman, J. , Ryan, R. , Walsh, L. , Horey, D. , Leask, J. , Robinson, P. , & Hill, S. (2018). Face‐to‐face interventions for informing or educating parents about early childhood vaccination. Cochrane Database of Systematic Reviews, 5, 1–115. 10.1002/14651858.CD010038.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs, P. A. , Dennison, C. R. , Kellar, L. , & Lucas, J. (2019). Gender differences in eating disorder risk among NCAA division I cross country and track student‐athletes. The Journal of Sports Medicine, 2019, 5035871. 10.1155/2019/5035871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster, G. A. , Dodd, S. , & Williamson, P. R. (2004). Design and analysis of pilot studies: Recommendations for good practice. Journal of Evaluation in Clinical Practice, 10(2), 307–312. 10.1111/j.2002.384.doc.x [DOI] [PubMed] [Google Scholar]
- Lancaster, G. A. , & Thabane, L. (2019). Guidelines for reporting non‐randomised pilot and feasibility studies. Pilot and Feasibility Studies, 5, 114. 10.1186/s40814-019-0499-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein, M. B. , Haastrup, L. , Johansen, K. K. , Bindzus, J. B. , Larsen, P. V. , Støving, R. K. , & Linnet, J. (2021). Validation of the eating disorder examination questionnaire in Danish eating disorder patients and athletes. Journal of Clinical Medicine, 10(17), 3976. 10.3390/jcm10173976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon, J. , Rosato, J. , & Messer, M. (2020). Break Binge Eating: Reach, engagement, and user profile of an internet‐based psychoeducational and self‐help platform for eating disorders. International Journal of Eating Disorders, 53(10), 1719–1728. 10.1002/eat.23356 [DOI] [PubMed] [Google Scholar]
- Mancine, R. P. , Gusfa, D. W. , Moshrefi, A. , & Kennedy, S. F. (2020). Prevalence of disordered eating in athletes categorized by emphasis on leanness and activity type–a systematic review. Journal of Eating Disorders, 8, 47. 10.1186/s40337-020-00323-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinsen, M. , Bratland‐Sanda, S. , Eriksson, A. K. , & Sundgot‐Borgen, J. (2010). Dieting to win or to be thin? A study of dieting and disordered eating among adolescent elite athletes and non‐athlete controls. British Journal of Sports Medicine, 44(1), 70–76. 10.1136/bjsm.2009.068668 [DOI] [PubMed] [Google Scholar]
- Merlin, J. S. , Young, S. R. , Johnson, M. O. , Saag, M. , Demonte, W. , Modi, R. , Anderson, W. A. , Kerns, R. , Bair, M. J. , Kertesz, S. , Davies, S. , & Turan, J. M. (2017). Using patient perspectives to inform the development of a behavioral intervention for chronic pain in patients with HIV: A qualitative study. Pain Medicine, 18(5), 879–888. 10.1093/pm/pnw150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milat, A. J. , King, L. , Bauman, A. E. , & Redman, S. (2012). The concept of scalability: Increasing the scale and potential adoption of health promotion interventions into policy and practice. Health Promotion International, 28(3), 285–298. 10.1093/heapro/dar097 [DOI] [PubMed] [Google Scholar]
- Murphy, R. , Calugi, S. , Cooper, Z. , & Dalle Grave, R. (2020). Challenges and opportunities for enhanced cognitive behaviour therapy (CBT‐E) in light of COVID‐19. The Cognitive Behaviour Therapist, 13. e14. 10.1017/S1754470X20000161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, R. , Straebler, S. , Basden, S. , Cooper, Z. , & Fairburn, C. G. (2012). Interpersonal psychotherapy for eating disorders. Clinical Psychology & Psychotherapy, 19(2), 150–158. 10.1002/cpp.1780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence . (2017). Eating disorders: Recognition and treatment, No. 69. NICE. [PubMed] [Google Scholar]
- Neumark‐Sztainer, D. R. , Wall, M. , Larson, N. I. , Eisenberg, M. E. , & Loth, K. (2011). Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10‐year longitudinal study. Journal of the American Dietetic Association, 111(7), 1004–1011. 10.1016/j.jada.2011.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsmond, G. I. , & Cohn, E. S. (2015). The distinctive features of a feasibility study: Objectives and guiding questions. OTJR: Occupation, Participation and Health, 35(3), 169–177. 10.1177/1539449215578649 [DOI] [PubMed] [Google Scholar]
- Palmcrantz, S. , Tistad, M. , Eldh, A. C. , Holmqvist, L. W. , Ehrenberg, A. , Tomson, G. , & Wallin, L. (2015). Assessing feasibility and acceptability of study procedures: Getting ready for implementation of national stroke guidelines in out‐patient health care. BMC Health Services Research, 15(1). 517. 10.1186/s12913-015-1177-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plateau, C. R. , Arcelus, J. , Leung, N. , & Meyer, C. (2017). Female athlete experiences of seeking and receiving treatment for an eating disorder. Eating Disorders, 25(3), 273–277. 10.1080/10640266.2016.1269551 [DOI] [PubMed] [Google Scholar]
- Pope, Z. , Gao, Y. , Bolter, N. , & Pritchard, M. (2015). Validity and reliability of eating disorder assessments used with athletes: A review. Journal of Sport and Health Science, 4(3), 211–221. 10.1016/j.jshs.2014.05.001 [DOI] [Google Scholar]
- Price‐Evans, K. , & Treasure, J. (2011). The use of motivational interviewing in anorexia nervosa. Child and Adolescent Mental Health, 16(2), 65–70. 10.1111/j.1475-3588.2011.00595.x [DOI] [PubMed] [Google Scholar]
- Prochaska, J. O. , DiClemente, C. C. , & Norcross, J. C. (1993). In search of how people change: Applications to addictive behaviors. Addictions Nursing Network, 5(1), 2–16. 10.3109/10884609309149692 [DOI] [PubMed] [Google Scholar]
- Ritchie, J. , & Lewis, J. (2003). Qualitative research practice: A guide for social science students and researchers. Sage Publications. [Google Scholar]
- Royal College of Psychiatrists . (2019). Position statement on early intervention for eating disorders (PS03, position statement). https://www.rcpsych.ac.uk/docs/default‐source/improving‐care/better‐mh‐policy/position.statements/ps03_19.pdf?sfvrsn=b1283556_2 [Google Scholar]
- Sandgren, S. S. , Haycraft, E. , & Plateau, C. R. (2020). Nature and efficacy of interventions addressing eating psychopathology in athletes: A systematic review of randomised and nonrandomised trials. European Eating Disorders Review, 28(2), 105–121. 10.1002/erv.2704 [DOI] [PubMed] [Google Scholar]
- Schaal, K. , Tafflet, M. , Nassif, H. , Thibault, V. , Pichard, C. , Alcotte, M. , El Helou, N. , Berthelot, G. , Simon, S. , & Toussaint, J.‐F. (2011). Psychological balance in high level athletes: Gender‐based differences and sport‐specific patterns. PLoS One, 6(5), e19007. 10.1371/journal.pone.0019007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer, J. L. , & Olsen, M. K. (1998). Multiple imputation for multivariate missing‐data problems: A data analyst's perspective. Multivariate Behavioral Research, 33(4), 545–571. 10.1207/s15327906mbr3304_5 [DOI] [PubMed] [Google Scholar]
- Sebire, S. J. , Banfield, K. , Jago, R. , Edwards, M. J. , Campbell, R. , Kipping, R. , Kadir, B. , Garfield, K. , Matthews, J. , Lyons, R. A. , & Hollingworth, W. (2019). A process evaluation of the PLAN‐A intervention (Peer‐Led physical Activity iNtervention for Adolescent girls). BMC Public Health, 19(1), 1203. 10.1186/s12889-019-7545-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanmugam, V. , Jowett, S. , & Meyer, C. (2013). Eating psychopathology amongst athletes: The importance of relationships with parents, coaches and teammates. International Journal of Sport and Exercise Psychology, 11(1), 24–38. 10.1080/1612197X.2012.724197 [DOI] [Google Scholar]
- Shanmugam, V. , Jowett, S. , & Meyer, C. (2014). Interpersonal difficulties as a risk factor for athlete’s eating psychopathology. Scandinavian Journal of Medicine and Science in Sport, 24(2), 469–476. 10.1111/sms.12109 [DOI] [PubMed] [Google Scholar]
- Shaw, H. , & Stice, E. (2016). The implementation of evidence‐based eating disorder prevention programs. Eating Disorders, 24(1), 71–78. 10.1080/10640266.2015.1113832 [DOI] [PubMed] [Google Scholar]
- Sim, J. , & Lewis, M. (2012). The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. Journal of Clinical Epidemiology, 65(3), 301–308. 10.1016/j.jclinepi.2011.07.011 [DOI] [PubMed] [Google Scholar]
- Stice, E. , Becker, C. B. , & Yokum, S. (2013). Eating disorder prevention: Current evidence‐base and future directions. International Journal of Eating Disorders, 46(5), 478–485. 10.1002/eat.22105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan, L. (2020). Power and sample size determination. Boston University, School of Public Health. https://sphweb.bumc.bu.edu/otlt/MPH‐Modules/BS/BS704_Power/BS704_Power_print.html [Google Scholar]
- Thomas, B. H. , Ciliska, D. , Dobbins, M. , & Micucci, S. (2004). A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews on Evidence‐Based Nursing, 1(3), 176–184. 10.1111/j.1524-475X.2004.04006.x [DOI] [PubMed] [Google Scholar]
- Thompson, R. A. , & Sherman, R. (2014). Reflections on athletes and eating disorders. Psychology of Sport and Exercise, 15(6), 729–734. 10.1016/j.psychsport.2014.06.005 [DOI] [Google Scholar]
- Tickle‐Degnen, L. (2013). Nuts and bolts of conducting feasibility studies. American Journal of Occupational Therapy, 67(2), 171–176. 10.5014/ajot.2013.006270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traviss‐Turner, G. D. , West, R. M. , & Hill, A. J. (2017). Guided self‐help for eating disorders: A systematic review and metaregression. European Eating Disorders Review, 25(3), 148–164. 10.1002/erv.2507 [DOI] [PubMed] [Google Scholar]
- Vandereycken, W. (2006). Denial of illness in anorexia nervosa – a conceptual review: Part 1 diagnostic significance and assessment. European Eating Disorders Review, 14(5), 341–351. [Google Scholar]
- Walters, S. J. , dos Anjos Henriques‐Cadby, I. B. , Bortolami, O. , Flight, L. , Hind, D. , Jacques, R. M. , Nadin, B. , Rothwell, J. , Surtees, M. , & Julious, S. A. (2017). Recruitment and retention of participants in randomised controlled trials: A review of trials funded and published by the United Kingdom health technology assessment programme. BMJ Open, 7(3), e015276. 10.1136/bmjopen-2016-015276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead, A. L. , Julious, S. A. , Cooper, C. L. , & Campbell, M. J. (2016). Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Statistical Methods in Medical Research, 25(3), 1057–1073. 10.1177/0962280215588241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, E. N. , & Morrow, S. L. (2009). Achieving trustworthiness in qualitative research: A pan‐paradigmatic perspective. Psychotherapy Research, 19(4–5), 576–582. 10.1080/10503300802702113 [DOI] [PubMed] [Google Scholar]
- World Health Organisation . (2020). Coronavirus disease (COVID‐19) situation report – 84. World Health Organisation. https://www.who.int/emergencies/diseases/novelcoronavirus‐2019 [Google Scholar]
- Yim, S. H. , & Schmidt, U. (2019). Experiences of computer‐based and conventional self‐help interventions for eating disorders: A systematic review and meta‐synthesis of qualitative research. International Journal of Eating Disorders, 52(10), 1108–1124. 10.1002/eat.23142 [DOI] [PubMed] [Google Scholar]
- Zweben, A. , Fucito, L. M. , & O’Malley, S. S. (2009). Effective strategies for maintaining research participation in clinical trials. Drug Information Journal: DIJ/Drug Information Association, 43(4), 459–467. 10.1177/009286150904300411 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the nature of this research, participants in this study did not agree for their data to be shared publicly, so supporting data are not available.


