Abstract
The present study investigated the relationship between anxiety, social support, living arrangements and cognitive performance of university students during the global pandemic. Two hundred and fifteen students participated by completing online questionnaires. Separate moderated multiple regression models were used to test whether social support (Family, Friends, Significant Other subscales of the Multidimensional Scale of Perceived Social Support) moderated the relationship between anxiety (Anxiety subscale of Depression, Anxiety Stress Scale), living arrangements (Living Alone vs Living with Friends and Family) and cognitive performance (Cognitive Failures Questionnaire), after controlling for comorbid depression. The results for each level of perceived social support suggested that anxiety was negatively associated with cognitive performance. Our most significant finding was that for students living alone, social support from a significant other offered a protective factor, whereby buffering the anxiety related cognitive deficits prevalent in those who reported lower social support. These data have important practical implications for supporting the social-emotional and academic needs of university students during the global pandemic.
Keywords: Anxiety, Social support, Cognitive performance
1. Introduction
Attending university is mostly a positive experience yet for some students the associated experiences of separating from family, establishing new social connections, and increasing responsibilities, are stressful (Duffy et al., 2019). As such, university students commonly report elevated anxiety, depression, and social isolation (Auerbach et al., 2016). Given that academic success at university is heavily reliant on good mental health (see Royal College of Psychiatrists, 2021) it is vital to understand the interplay of individual differences contributing to poor performance.
Since the outbreak of COVID-19, rates of anxiety and depression have increased among university students globally, for example, US (Son et al., 2020), UK (Chen & Lucock, 2022), Hong Kong (Sun et al., 2020) and Australia (Liu et al., 2021). Causes of elevated symptomology include fear of illness, social isolation, and exaggerated media coverage (Galea et al., 2020; Huang & Zhao, 2020; Pfefferbaum & North, 2020). In addition, pandemic-related university closures and face-to-face teaching which limits contact with classmates replaced with online or e-learning (Favale et al., 2020), have resulted in many students feeling isolated from significant support networks on campus (Sahu, 2020; Saltzman et al., 2020). Further, students who moved interstate or abroad to study were further isolated by virtue of living in student accommodation and sometimes living alone (Smith & Victor, 2019). Therefore, it is possible that students living alone might be more vulnerable to social-emotional problems due to the addition of pandemic-related social isolation restrictions.
A growing number of studies have explored the sequalae of mental health problems for university students studying during the pandemic. Some studies have reported a link between low perceived social support and elevated anxiety (Ortenburger et al., 2021) and depression (Grey et al., 2020; Guo et al., 2021). In accord, high perceived social support was a protective factor in university students with elevated anxiety (Szkody et al., 2020), depression (Sun et al., 2020) and stress (Cao et al., 2020), during the pandemic. However, less is known about the source of the perceived social support and whether social support from family, friends or a significant other have the same or different influence on psychological wellbeing and furthermore if living arrangements play a role.
The relationship between anxiety, depression and cognitive performance has interested researchers for decades (see Eysenck et al., 2007 for a review). Studies have shown highly anxious (e.g., Edwards et al., 2016) and depressed (e.g., Dillon & Pizzagalli, 2018) individuals performed poorer on memory tasks compared to those with lower symptoms. More specifically, one study with university students measured everyday memory using the Cognitive Failures Questionnaire (Broadbent et al., 1982) and found that elevated anxiety and depression was related to poorer self-reported cognitive performance (Uddin et al., 2021). Although the association between anxiety, depression and social support, and cognitive performance is well-established, to our knowledge, no studies have attempted to untangle the interrelationships between these factors, especially during heightened symptoms during COVID-19. Such is the focus of the present research.
We premised our study on attentional control theory (Eysenck et al., 2007) which provides an explanation for the detrimental effects of anxiety on cognitive performance. The theory posits that highly anxious individuals have poorer attentional control and difficulty moving their focus away from worrisome thoughts which in turn reduces the cognitive or memory resources available to complete the tasks at hand. Memory is involved in most aspects of everyday life and most certainly in the undertaking of demanding tasks like those required for university study. Moreover, due to the well-known overlap of symptoms between anxiety and depression (see Bradley et al., 1995), and the link between depression and perceived social support (Grav et al., 2012) we argued that any assessment of anxiety should be treated with caution unless controlling for the comorbidity of depression and/or considering the moderating effects of social support.
In sum, we examined the relationship between anxiety, social support, living arrangements and cognitive performance of university students during the peak of the pandemic and controlled for comorbid depression. We expected that students may be protected from anxiety's adverse effects if they had access to meaningful social support. To provide a sensitive test of this hypotheses we delineated social support using the separate subscales Multidimensional Scale of Perceived Social Support (Zimet et al., 1988). Specifically, we predicted that after controlling for comorbid depression, we would reveal a 3-way (anxiety x social support x living arrangements) interaction such that higher anxiety would be associated with lower cognitive performance but that these effects would be restricted to those living alone who reported lower social support from family, friends, and significant others.
2. Methods
2.1. Participants
University students were recruited using social media (Facebook, Twitter, We-chat) to participate in the online questionnaire administered using the Quatrics platform. The questionaries were attempted by 317 participants; however, 102 respondents abandoned it after less than one minute (M = 50.74 s; SD = 44.17 s) and these cases were removed (32 %). The final sample of university students (N = 215) ranged in age from 18 to 41 years, M age = 24.17 years, SD age = 3.77 years, and 53 % were female. Table 1 shows the demographic characteristics of the sample.
Table 1.
Demographic characteristics of participants (N = 215).
| Characteristic | Domestic Students |
International Students |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | m | f | ns | m | f | ns | ns | ||
| Type of study | Undergraduate | 87 | 29 | 23 | 1 | 22 | 11 | 1 | |
| Post-graduate | 128 | 17 | 21 | 31 | 59 | ||||
| Living arrangement | Living alone | 109 | 26 | 15 | 1 | 34 | 33 | ||
| Living with F&F | 106 | 20 | 29 | 19 | 37 | 1 | |||
NOTE: ns = did not specify; F&F = friends and family.
2.2. Measures
2.2.1. Depression Anxiety Stress Scale (DASS-21; Lovibond & Lovibond, 1995)
The DASS-21 was used to index symptoms of anxiety and depression. The Anxiety and Depression subscales of the DASS-21 include 7 statements related to anxiety e.g., I felt I was close to panic, I felt scared without any good reason, and 7 items for depression e.g. I felt that life was meaningless, I found it difficult to work up the initiative to do things. The items related to Stress were not used. Participants indicate how much the statements applied to them in the past week on a 4-point scale from 0 = Did not apply to me at all to 3 = Applied to me very much, or most of the time. As per the author's standardized scoring instructions, no items are reverse scored, totals are multiplied by 2, and maximum total scores = 42. Higher scores reflected greater symptoms of anxiety and depression. The DASS-21 has satisfactory reliability with Cronbach's α =0.84 for DASS-Anxiety and α = 0.96 for DASS- Depression (Lovibond & Lovibond, 1995), and α = 0.85 and α = 0.87, respectively, in the current sample.
2.2.2. Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al., 1988)
The MSPSS was used to measure perceived social support from Family e.g., My family really tries to help me, from Friends e.g., I have friends with whom I can share my joys and sorrows and from a Significant Other e.g. I have a special person who is a real source of comfort to me. Participants respond to 4-items for each subscale using a 7-point Likert scale from 1 = Very Strongly Disagree to 7 = Very Strongly Agree. No items were reverse scored; maximum total scores for each subscale were 84, with higher scores indicating higher perceived social support. The MSPSS has shown good psychometric properties (Zimet et al., 1988) and in the current sample i.e., α = 0.86 for MSPSS-Family, α = 0.88 for MSPSS-Friends, and α = 0.88 for MSPSS- Significant Other.
2.2.3. Cognitive Failures Questionnaire (CFQ; Broadbent et al., 1982)
The CFQ was used to assess self-reported cognitive performance. The CFQ includes 25 items to measure everyday failures in attention, memory and motor function in the last six months e.g., Do you find you forget whether you've turned off a light or a fire or locked the door? Do you bump into people? and Do you find you confuse right and left when giving directions? Participants respond on a 5-point Likert scale from 0 = Never to 4 = Very often. No items were reverse scored with total scores ranged 0–100. Higher scores represented greater cognitive failures (Wallace et al., 2002). The CFQ has shown good ecological validity and reliability (Broadbent et al., 1982; Wallace, 2004). To aid interpretation in the current study, cognitive performance was operationalized as an inverse of the total CFQ score using the equation: Cognitive Performance = 100 – Total Score on the CFQ.
2.3. Procedure
Approval was obtained from the university's human research ethics committee. Data was collected using an online questionnaire administered using the Qualtrics platform, between 15 August 2020 and 14 September 2020. The sampling region was experiencing strict social distancing restrictions at this time a maximum of 10 people allowed per household; fines applied for noncompliance. On the first page of the questionnaire, participants were provided with the information about the research and provided implied consent. The survey contained questions on demographic characteristics (e.g., age, sex, university student status, living arrangements), followed by DASS-21, MSPSS, and CFQ, and took approximately 15–20 min to complete.
3. Results
3.1. Data cleaning and assumption checking
Standardized scores and box plots were used to detect univariate outliers, however, no out-of-range values were identified (i.e., z-scores >3.50). Computation of Mahalanobis and Cook's distance, and Leverage values revealed two cases meeting criterion for multivariate outliers on two of these detection methods, thus these cases were removed. The retained data set (N = 213) met the assumptions of normality, linearity, and homoscedasticity (Tabachnick et al., 2007). Data analyses were performed on complete cases and Little's test determined items were ‘missing completely at random’ (MCAR); χ2 (476) = 499.42, p = .221.
3.2. Descriptive statistics
Table 2 shows the zero-order correlations between the predictors and criterion variables, and the inter-correlations among the predictors. As shown, there were significant zero-order correlations between all predictors and cognitive performance, such that higher depression and anxiety was related to poorer cognitive performance and higher social support (family, friends and significant other) was associated with higher cognitive performance. There were significant inter-correlations between depression and anxiety, with higher depression associated with higher anxiety. There were also negative inter-correlations between depression and anxiety and social support, such that higher depression and anxiety was related to lower perceived social support (family, friends and significant other).
Table 2.
Means, standard deviations, zero-order and inter-correlations between depression, anxiety, social support (SS), cognitive performance.
| M | SD | Depression | Anxiety | SS Family | SS Friends | SS Sig Other | |
|---|---|---|---|---|---|---|---|
| Depression | 16.20 | 9.61 | |||||
| Anxiety | 15.74 | 9.9 | 0.83⁎⁎ | ||||
| SS Family | 15.35 | 5.68 | −0.28⁎⁎ | −0.30⁎⁎ | |||
| SS Friends | 16.38 | 5.62 | −0.17⁎ | −0.17⁎ | 0.73⁎⁎ | ||
| SS Significant Other | 15.94 | 5.54 | −0.27⁎⁎ | −0.24⁎⁎ | 0.84⁎⁎ | 0.66⁎⁎ | |
| Cognitive Performance | 53.01 | 14.04 | −0.42⁎⁎ | −0.50⁎⁎ | 0.30⁎⁎ | 0.30⁎⁎ | 0.32⁎⁎ |
p < .01.
p < .05.
3.3. Main analyses
Three separate regression models were constructed to test the hypothesis whether social support (family, friends or significant other) moderated the relationship between anxiety, living arrangements and cognitive performance. For each analysis, the model treated depression as a covariate. Anxiety and living arrangements (living alone, living with family and friends) were predictor variables, and social support was the moderator variable. Each model included the 2-way interaction terms (anxiety x living, anxiety x social support, social support x living), and the 3-way interaction term (anxiety x living x social support) which were formed using mean-centred scores for continuous predictors. All analyses were conducted using SPSS version 25 and the PROCESS macro, Model #3 (Hayes, 2012). Interactions were detected with 5000 bootstrap resamples whereby the bias-corrected bootstrap 95 % confidence intervals were interpreted as significant at the p < .05 level if they did not cross zero (Hayes, 2012). Effect sizes are reported using Cohen's f 2 and calculated using the R 2 Change statistic at the final step of the model. Following conventions 0.02 indicated a small effect, 0.15 a medium effect, and 0.35 a large effect. PROCESS in SPSS decomposes interactions using the Johnson-Neyman technique and performs tests of simple slopes at high and low values on the social support and anxiety scales (calculated at ±1 SD from the mean score on each).
3.3.1. Social support family
Table 3 shows the unstandardised coefficients, t-tests, probabilities and 95 % confidence intervals for cognitive performance. After controlling for depression, the model using the domain for social support from family accounted for 34 % of the variance in cognitive performance, yet failed to reach significance, R = 0.58, R 2Δ = 0.01, FΔ (1, 194) = 1.91, p = .169, despite the significance of the full model, F (8, 194) = 12.22, MSE = 135.85, p < .001, Cohen's f 2 = 0.01. Anxiety was a significant negative predictor of cognitive performance such that higher anxiety was associated with lower performance, b = −0.53, t (194) = 2.90, p = .004. The main effect of social support and the anxiety x social support interaction approached significance, ps = 0.054, and 0.059, respectively. All other tests were non-significant, all t < 1.23, p > .221.
Table 3.
Unstandardised coefficients, t-tests, probabilities and 95 % confidence intervals for cognitive performance.
| Unstandardised Coefficients |
95 % Confidence Intervals |
|||||
|---|---|---|---|---|---|---|
| b | SE | t | p | Lower Bound | Upper Bound | |
| SS Family | ||||||
| Constant | 54.84 | 3.34 | 14.27 | 0.000 | 48.25 | 61.42 |
| Depression | −0.09 | 0.19 | 0.46 | 0.643 | −0.45 | 0.28 |
| Anxiety | −0.53 | 0.18 | 2.90 | 0.004 | −0.90 | −0.71 |
| Social Support (SS) | 0.56 | 0.29 | 1.94 | 0.054 | −0.11 | 1.14 |
| Living | −0.12 | 1.20 | 0.01 | 0.989 | −2.38 | 2.34 |
| Anxiety x SS | 0.05 | 0.03 | 1.90 | 0.059 | −0.01 | 0.11 |
| Anxiety x Living | −0.17 | 0.14 | 1.22 | 0.223 | −0.43 | −0.10 |
| SS x Living | −0.28 | 0.28 | 0.98 | 0.330 | −0.83 | 0.28 |
| Anxiety x SS x Living | −0.03 | 0.29 | 1.23 | 0.221 | −0.09 | 0.02 |
| SS Friends | ||||||
| Constant | 56.64 | 3.35 | 16.02 | 0.000 | 47.03 | 60.24 |
| Depression | −0.03 | 0.18 | 0.17 | 0.864 | −0.39 | 0.39 |
| Anxiety | −0.59 | 0.18 | 3.34 | 0.001 | −0.93 | −0.24 |
| Social Support (SS) | 0.68 | 0.25 | 2.72 | 0.007 | 0.19 | 1.17 |
| Living | −0.32 | 1.10 | 0.30 | 0.773 | −2.48 | 1.84 |
| Anxiety x SS | 0.05 | 0.03 | 2.02 | 0.045 | 0.01 | 0.10 |
| Anxiety x Living | −0.19 | 0.13 | 1.51 | 0.134 | −0.49 | 0.06 |
| SS x Living | −0.28 | 0.24 | 1.16 | 0.247 | −0.76 | 0.20 |
| Anxiety x SS x Living | −0.04 | 0.03 | 1.46 | 0.147 | −0.09 | 0.01 |
| SS Significant Other | ||||||
| Constant | 52.49 | 3.21 | 16.36 | 0.000 | 47.16 | 58.81 |
| Depression | 0.06 | 0.18 | 0.31 | 0.757 | −0.29 | 0.40 |
| Anxiety | −0.59 | 0.17 | 3.45 | 0.001 | −0.93 | −0.25 |
| Social Support (SS) | 0.56 | 0.26 | 2.11 | 0.036 | 0.04 | 1.08 |
| Living | −0.42 | 1.13 | 0.37 | 0.710 | −2.64 | 1.80 |
| Anxiety x SS | 0.04 | 0.03 | 1.53 | 0.127 | −0.01 | 0.93 |
| Anxiety x Living | −0.20 | 0.13 | 1.51 | 0.134 | −0.46 | 0.06 |
| SS x Living | −0.49 | 0.27 | 1.85 | 0.066 | −1.01 | 0.03 |
| Anxiety x SS x Living | −0.07 | 0.03 | 2.57 | 0.011 | −0.12 | −0.02 |
3.3.2. Social support friends
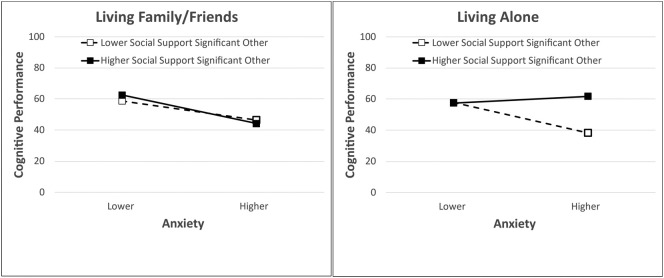
The model using the domain for social support from friends accounted for 36 % of the variance in cognitive performance yet was nonsignificant, R = 0.60, R 2Δ = 0.02, FΔ (1, 194) = 2.48, p = .117, although the full model reached significance F (8, 194) = 14.18, MSE = 131.19, p < .001, Cohen's f 2 = 0.02, after controlling for depression (see Table 3). There was an inverse relationship between anxiety and cognitive performance, b = −0.59, t (194) = 3.34, p = .001, such that higher anxiety was associated with lower performance. There was a positive relationship between social support and performance, b = 0.68, t (194) = 2.72, p = .007; higher social support was related to higher performance. The only other significant effect was the anxiety x social support interaction, b = 0.05, t (194) = 2.02, p = .045, which can be seen in Fig. 1 . Simple slopes tests indicated that there was no relationship between anxiety and cognitive performance at higher social support, b = −0.33, 95 % CI [−0.81, 0.16], t (194) = 1.33, p = .186, whereas at lower social support, higher anxiety was related to lower cognitive performance, b = −0.88, 95 % CI [−1.25, −0.52], t(194) = 4.80, p < .001.
Fig. 1.
Relationship between anxiety, social support friends, and cognitive performance. Simple slopes are calculated at ±1 SD from the mean score on each of high and low values on the predictor variables.
3.3.3. Social support significant other
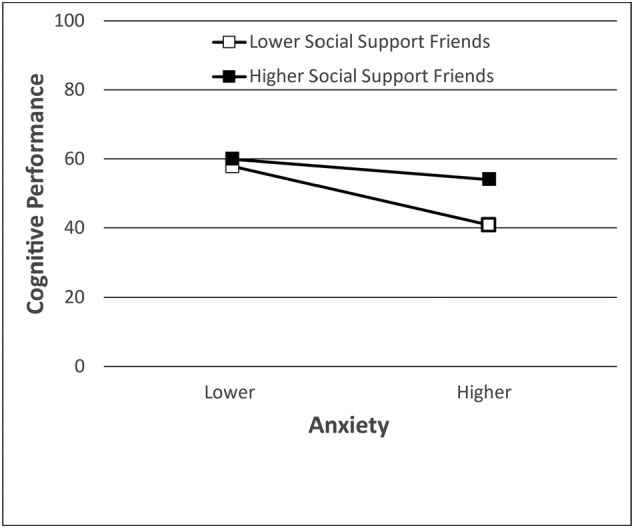
The model using the domain for social support from significant others accounted for 37 % of the variance in cognitive performance and was significant, R = 0.60, R 2Δ = 0.05, FΔ (1, 194) = 7.86, p = .006 and the full model was also significant F (8, 194) = 13.99, MSE = 130.38, p < .001, Cohen's f 2 = 0.05, after controlling for depression (see Table 3). There were significant main effects of anxiety, b = −0.59, t(194) = 3.45, p = .001, and social support, b = 0.56, t(194) = 2.11, p = .036; higher anxiety was associated with lower cognitive performance, whereas higher social support was associated with higher cognitive performance. These main effects were further qualified by the significant 3-way interaction involving anxiety x living x social support, b = −0.07, t (194) = 2.58, p = .011. The pattern of the interaction can be seen in Fig. 2 . As shown in the left panel, for those living with family/friends the anxiety x social support interaction was not significant, F < 1. Tests of simple effects revealed that higher anxiety was associated with lower cognitive performance at both lower, b = −0.64, 95 % CI [−1.18, −0.09], t(194) = 2.32, p = .022 and higher social support, b = −9.42, 95 % CI [−1.51, −0.38], t(194) = 3.29, p = .001. As shown in the right panel, for those living alone the interaction between anxiety and social support was significant, F (1,194) = 6.63, p = .011. The interaction reflected the fact that higher anxiety was associated with lower cognitive performance at lower social support, b = −0.99, 95 % CI [−1.58, −0.41], t(194) = 3.36, p = .001, but not at higher social support, b = 0.22, 95 % CI [−0.46, 0.90], t < 1, n.s.
Fig. 2.
Relationship between anxiety, social support from significant other, living arrangements and cognitive performance. Simple slopes are calculated at ±1 SD from the mean score on each of high and low values on the predictor variables.
4. Discussion
The present study examined the moderating potential of social support on the detrimental effects of elevated anxiety on cognitive performance, in university students. We predicted that higher anxiety would be related to poorer cognitive performance but that these effects would be restricted to those living alone who reported lower social support from family, friends, and significant others. Our hypotheses were partially supported.
For social support from family our hypothesis was not supported, however, consistent with attentional control theory elevated anxiety was related to poor cognitive performance. Although, this relationship was unrelated to living arrangements or social support. For social support from friends, our findings were partly consistent with our hypothesis. We found at lower social support from friends, higher anxiety was associated with poorer cognitive performance, however these effects were unrelated to living arrangements. Nonetheless, for social support from a significant other, our predictions were fully supported. Our data revealed that for students living alone, higher social support from a significant other afforded a protective factor whereby buffering the anxiety related cognitive deficits prevalent in those who reported lower social support.
The present study revealed four important findings. First, we found significant interrelationships between depression, anxiety, and social support. This result validates our treatment of depression as a covariate, the inclusion of social support in our statistical models and aligns with previous literature (Grey et al., 2020; Guo et al., 2021; Ortenburger et al., 2021; Szkody et al., 2020). Second, our findings suggest broadly that higher anxiety is associated with poorer cognitive performance consistent with attentional control theory (Eysenck et al., 2007) and empirical literature (Edwards et al., 2016). Thus, it is possible that for university students exposed to the multiple stressors related to COVID-19, their elevated anxiety may have interfered with their everyday cognitive performance. Third, through our fine grain analysis we identified that social support of a significant other was crucial for those students living alone as a protective factor for the detrimental influence of anxiety of their cognitive performance. This study is the first to show this relationship. Finally, and incidentally, we identified that perceived social support from family was highly correlated with that from a significant other, despite each having differential moderating effects on anxiety and living arrangements in predicting cognitive performance. The precise reason for this discrepancy is unclear, but what seems plausible is that having a self-determined significant other plays a more important role than a familial special person in buffering the negative implications for cognitive performance. Future research to clarify why this is the case is warranted.
Several limitations need mention. The data comprised a small sample taken from students at a single Australian university, and as such may not be generalisable to other tertiary students. Second, the use of self-reported cognitive performance may not concur with students' academic performance. Our data was collected during the peak of pandemic restrictions thus providing sensitive test of our hypothesis, that is, that psychological symptoms would likely be higher and therefore maximise the focal relationship between the factors of interest. Nonetheless, increasing sensitivity brings with it the possibility that the results may not be generalisable to non-pandemic times. Finally, our cross-sectional design cannot draw causal conclusions. Particularly, cognitive failures have been found to precede anxiety (Broadbent et al., 1982) thus the use of a longitudinal design is warranted to examine the reciprocal nature of the pattern of results reported here. It is hoped the present study will be the catalyst for future work.
4.1. Practical implications and conclusions
The present study examined students studying during the pandemic and took a novel approach by contrasting those living with friends and family with those living alone. The main finding of the importance of a significant other for those who live alone has practice implications for staff involved in student support services. That is, university student counsellors could highlight the need for a single close friend or family member to become the support network for a student. Lecturers could also reinforce this message and check in with students to ensure they have someone to support them. It is essential to raise awareness of the importance of building meaningful relationships. Given the social distancing and isolation restrictions of the pandemic, and the reduced capacity to provide face-to-face activities for students, it is crucial that meaningful relationships are developed and sustained through online and virtual means in order to support not only the mental health but also, as a consequence, the cognitive performance of university students.
In sum, the present study found that during COVID-19 students who experienced elevated anxiety also reported cognitive deficits. Nevertheless, social support from family, friends, and significant others, have vital roles to play. Most importantly, for students who live alone, social support from a significant other can buffer the negative influence of anxiety on cognitive performance. We suggest that the key to maintaining good mental health during the global pandemic is to prioritize the importance of building and maintaining healthy, meaningful relationships so that these social supports can afford protective properties for the effect of anxiety.
CRediT authorship contribution statement
Elizabeth Edwards and Robert Vaughan: Conceptualization, Methodology, Supervision, Data Analyses, Writing – Reviewing & Editing. Xiaohan Zhang and Khanh Linh Chu: Project Administration, Data Collection, Interpretation, Writing - Original Draft. Louise Cosgrove: Conceptualization, Interpretation, Writing – Reviewing & Editing.
Acknowledgements
We are grateful for the insightful comments provided by Dr. Irena Buric the Associate Editor and two anonymous reviewers who helped us to improve this manuscript.
Data availability
Data will be made available on request.
References
- Auerbach R.P., Alonso J., Axinn W.G., Cuijpers P., Ebert D.D., Green J.G., Bruffaerts R.… Mental disorders among college students in the World Health Organization world mental health surveys. Psychological Medicine. 2016;46(14):2955–2970. doi: 10.1017/S0033291716001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley B.P., Mogg K., Millar N., White J. Selective processing of negative information: Effects of clinical anxiety, concurrent depression, and awareness. Journal of Abnormal Psychology. 1995;104(3):532–536. doi: 10.1037/0021-843X.104.3.532. [DOI] [PubMed] [Google Scholar]
- Broadbent D.E., Cooper P.F., FitzGerald P., Parkes K.R. The cognitive failures questionnaire (CFQ) and its correlates. British Journal of Clinical Psychology. 1982;21(1):1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T., Lucock M. The mental health of university students during the COVID-19 pandemic: An online survey in the UK. PLoS One. 2022;17(1) doi: 10.1371/journal.pone.0262562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon D.G., Pizzagalli D.A. Mechanisms of memory disruption in depression. Trends in Neurosciences. 2018;41(3):137–149. doi: 10.1016/j.tins.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy A., Saunders K.E., Malhi G.S., Patten S., Cipriani A., McNevin S.H., Geddes J.… Mental health care for university students: A way forward? The Lancet Psychiatry. 2019;6(11):885–887. doi: 10.1016/S2215-0366(19)30275-5. [DOI] [PubMed] [Google Scholar]
- Edwards E.J., Edwards M.S., Lyvers M. Individual differences in trait anxiety and goal-commitment predict updating efficiency on the reading span task. Motivation and Emotion. 2016;40(6):936–945. doi: 10.1007/s11031-016-9572. [DOI] [Google Scholar]
- Eysenck M.W., Derakshan N., Santos R., Calvo M.G. Anxiety and cognitive performance: Attentional control theory. Emotion. 2007;7(2):336. doi: 10.1037/1528-3542.7.2.336. [DOI] [PubMed] [Google Scholar]
- Favale T., Soro F., Trevisan M., Drago I., Mellia M. Campus traffic and e-learning during COVID-19 pandemic. Computer Networks. 2020;176 doi: 10.1016/j.comnet.2020.107290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Internal Medicine. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Grav S., Hellzèn O., Romild U., Stordal E. Association between social support and depression in the general population: The HUNT study, a cross-sectional survey. Journal of Clinical Nursing. 2012;21(1–2):111–120. doi: 10.1111/j.1365-2702.2011.03868.x. [DOI] [PubMed] [Google Scholar]
- Grey I., Arora T., Thomas J., Saneh A., Tohme P., Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Research. 2020;293 doi: 10.1016/j.psychres.2020.113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo K., Zhang X., Bai S., Minhat H.S., Nazan A.I.N.M., Feng J., Saliluddin S.… Assessing social support impact on depression, anxiety, and stress among undergraduate students in Shaanxi province during the COVID-19 pandemic of China. PloS one. 2021;16(7) doi: 10.1371/journal.pone.0253891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. Guilford; London: 2012. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Huang Y., Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102052. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Liu C., McCabe M., Dawson A., Cyrzon C., Shankar S., Gerges N., Cornish K.… Identifying predictors of university students' wellbeing during the COVID-19 pandemic-a data-driven approach. International Journal of Environmental Research and Public Health. 2021;18(13):6730. doi: 10.3390/ijerph18136730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behavior Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Ortenburger D., Mosler D., Pavlova I., Wąsik J. Social support and dietary habits as anxiety level predictors of students during the COVID-19 pandemic. International Journal of Environmental Research and Public Health. 2021;18(16):8785. doi: 10.3390/ijerph18168785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. New England Journal of Medicine. 2020 doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Royal College of Psychiatrists . Royal College of Psychiatrists; London: 2021. The mental health of higher education students CR231.https://www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/college-reports/mental-health-of-higher-education-students-(cr231).pdf [Google Scholar]
- Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): Impact on education and mental health of students and academic staff. Cureus. 2020;12(4) doi: 10.7759/cureus.7541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saltzman L.Y., Hansel T.C., Bordnick P.S. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychological Trauma: Theory, Research, Practice, and Policy. 2020 doi: 10.1037/tra0000703. [DOI] [PubMed] [Google Scholar]
- Smith K.J., Victor C. Typologies of loneliness, living alone and social isolation, and their associations with physical and mental health. Ageing & Society. 2019;39(8):1709–1730. doi: 10.1017/S0144686X18000132. [DOI] [Google Scholar]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. Effects of COVID-19 on college students' mental health in the United States: Interview survey study. Journal of Medical Internet Research. 2020;22(9) doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Lin S.Y., Chung K.K.H. University students' perceived peer support and experienced depressive symptoms during the COVID-19 pandemic: The mediating role of emotional well-being. International Journal of Environmental Research and Public Health. 2020;17(24):9308. doi: 10.3390/ijerph17249308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkody E., Stearns M., Stanhope L., McKinney C. Stress-buffering role of social support during COVID-19. Family Process. 2020 doi: 10.1111/famp.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B.G., Fidell L.S., Ullman J.B. Pearson; Boston, MA: 2007. Using multivariate statistics. [Google Scholar]
- Uddin M.K., Reberio M., Khatun R., Shama A., Rahman J. Anxiety, depression, and everyday memory among female students pursuing diploma in nursing. International Journal. 2021;2(1):93–100. [Google Scholar]
- Wallace J.C. Confirmatory factor analysis of the cognitive failures questionnaire: Evidence for dimensionality and construct validity. Personality and Individual Differences. 2004;37(2):307–324. doi: 10.1016/j.paid.2003.09.005. [DOI] [Google Scholar]
- Wallace J.C., Kass S.J., Stanny C.J. The cognitive failures questionnaire revisited: Dimensions and correlates. The Journal of General Psychology. 2002;129(3):238–256. doi: 10.1080/00221300209602098. [DOI] [PubMed] [Google Scholar]
- Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52(1):30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.