Abstract
Coronavirus disease 2019 (COVID-19) emerged as a global pandemic in March 2020 and caused a big crisis, especially the health crisis. Pregnant and postpartum women experienced significant physical, social, and mental changes that put them at higher risk for several conditions during the pandemic. This study aimed to report the prevalence of depression in pregnant and postpartum women during the COVID-19 pandemic. Eligible studies were identified using several databases. Prevalence analysis was conducted using MedCalc ver. 19.5.1. This systematic review and meta-analysis was registered in PROSPERO on July 12, 2021 with registration number CRD42021266976. We included 54 studies with 95.326 participants. The overall prevalence of depression was 32.60% among pregnant and postpartum women during the COVID-19 pandemic. The rate was higher among pregnant women (31.49%) compared to postpartum women (27.64%). The prevalence of depression among pregnant and postpartum women increased during the COVID-19 pandemic.
Keywords: Depression, Pregnant women, Postpartum period, COVID-19, Meta-analysis
Introduction
Coronavirus disease 2019 (COVID-19), a novel infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a global pandemic by the World Health Organization (WHO) on March 11, 2020 [1]. As of July 4, 2021, over 182 million people had been infected with SARS-CoV-2, causing a global health crisis [2]. The uncertainty caused by the lack of an endpoint for the pandemic, while treatment is still not assurance, significantly impacts individuals’ psychology [3]. Because pregnancy is a period in which subtle changes occur both mentally and physically, pregnant women are considered vulnerable to severe forms of COVID-19 [4]. The COVID-19 pandemic mainly affects pregnant women, as the infection affects both mother and child during and after pregnancy [5]. Pregnant women are prone to developing psychological problems such as mood changes, fatigue, emotional disorders, mixed anxiety-depressive disorders, and pregnancy-related anxiety [6]. Depression and anxiety are the most common psychiatric disorders during pregnancy [7]. Antenatal maternal depression is associated with adverse effects on pregnancy and neonatal outcomes, including spontaneous abortion, bleeding, operative delivery, and preterm birth [8,9].
The incidence of depression during pregnancy and the postpartum period is 20.7% and 17%, respectively [10,11]. According to the WHO, approximately 10% of pregnant women and 13% of postpartum women have mental disorders, the most common of which is depression [12].
Understanding the implications of the COVID-19 pandemic on psychological changes in pregnant and postpartum women is essential to avoid its negative impacts and secondary consequences [13]. To date, there have been various publications on the impact of the COVID-19 pandemic on depressive symptoms in pregnant and postpartum women; however, to the best of our knowledge, this is the most updated meta-analysis regarding depression in pregnant and postpartum women. This review aimed to report the prevalence of depression in pregnant and postpartum women during the COVID-19 pandemic.
Methods
1. Eligibility criteria
The literature search was limited to retrospective and prospective studies published in English or Indonesian. Eligible studies had to meet all of the following inclusion criteria: 1) participants were pregnant or delivery women; 2) participants met the clinical cut-off point for depression, assessed through validated questionnaire/healthcare professional diagnosis; 3) data were obtained during the COVID-19 pandemic; 4) empirical or original research studies; and 5) studies that reported the prevalence rates of depression among pregnant and postpartum women during the COVID-19 pandemic.
Single case reports, editorials, commentaries, letters, nonfull-texts, and unpublished or non-peer-reviewed articles were excluded from our review. Single case reports were excluded because they tend to report only severe or unique cases and have the lowest evidence quality. Studies that reported only patients with severe features were also excluded from this review.
2. Information sources
A systematic search of studies was conducted electronically on several databases, including PubMed, EBSCO, and ProQuest, until June 30, 2021. MeSH terms, keywords, and word variants for “COVID-19,” “SARS-CoV-2,” and “pregnancy” were used. References of relevant articles or reviews were searched for additional studies.
3. Search strategy
To perform a systematic review and meta-analysis of studies evaluating depression in pregnant and postpartum women, we used the retrieval expressions: “pregnant women or pregnancy or perinatal or postpartum;” “SARS-CoV-2 or COVID-19 or coronavirus;” and “stress or psychological or mental or depression or depressive or psychology.”
4. Selection process
The articles used in this systematic review and meta-analysis were assessed independently by two authors (NA and JC) for study quality using the Newcastle-Ottawa Scale et al. [14]. This study was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines [15,16]. All abstracts were reviewed by two authors independently. Any disagreement regarding the relevance of a study was resolved through discussion with a third author (FBP). In cases of studies with the same cohort and identical endpoints, the study with the most comprehensive information was used, while the others were excluded to avoid overlapping cases.
5. Statistical analysis
Meta-analysis of proportions was used to combine all the data; logit transformations were conducted before meta-analysis, and the reported pooled proportions of depression were calculated using a random-effects model. All meta-analyses were performed using MedCalc, version 19.5.1 (MedCalc Software Ltd, Ostend, Belgium). [17]. The P-value for the overall effect, P<0.05 with two-tailed, was considered statistically significant. I2 was used to assess the heterogeneity of all the detailed studies. When it was lower than 50%, studies with acceptable heterogeneity were considered, and the fixed-effects model with the Mantel-Haenszel method was used; otherwise, a random-effects model with the DerSimonian and Laird method was adopted.
Publication bias was assessed for each pooled study group using Egger’s linear regression test. As a supplementary approach, Begg’s rank correlation was also applied to assess potential publication bias; when P was >0.05, there was no publication bias in the study.
Results
1. Search results
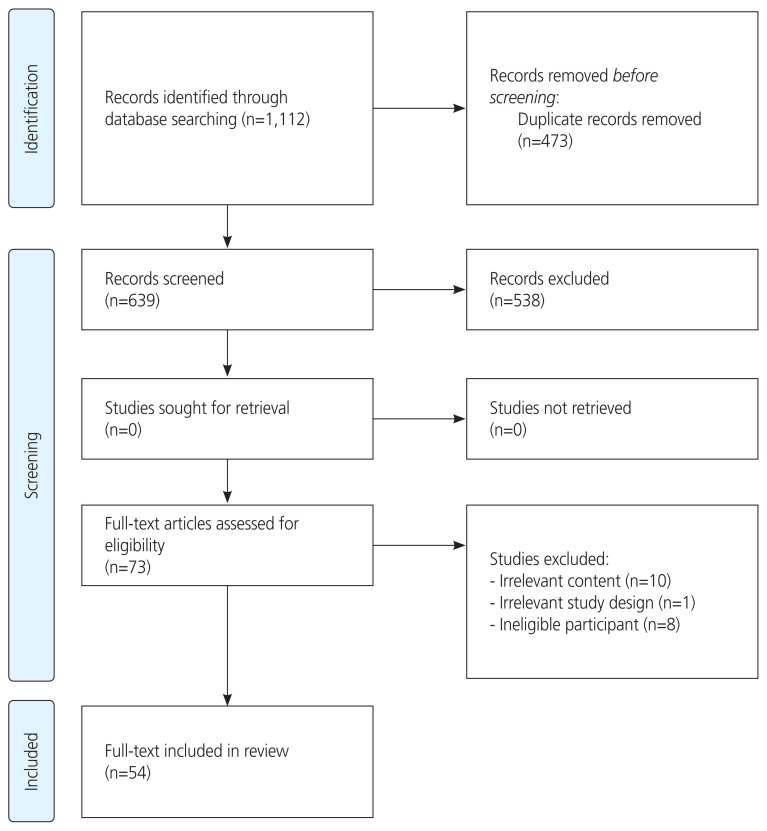
The initial articles identified from the electronic database yielded 1,112 studies. After screening the titles and abstracts, 73 articles were identified. Finally, 54 studies were included in this meta-analysis. The search flowchart and selection methods used in this study are summarized in Fig. 1.
Fig. 1.
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis flow diagram. The diagram summarizes the search strategy and selection process applied to include articles eligible for this meta-analysis.
2. Characteristics of the included studies
Fifty-four studies were included in this systematic review and meta-analysis (Table 1) [18–70]. The included studies were conducted between January 1, 2020 and June 30, 2021 with 95.326 participants. Among the 54 studies, 42 were cross-sectional, 10 were cohort, one was case-control, and one was mixed. Approximately 32 studies were conducted with Edinburgh Postnatal Depression Scale (EPDS), eight with Patient Health Questionnaire-9 (PHQ-9), three with Patient Health Questionnaire-2 (PHQ-2), two with Hospital Anxiety and Depression Scale (HADS), two with Edinburgh Depression Scale (EDS), two with Depression Anxiety and Stress Scale (DASS), one with Patient Health Questionnaire-4 (PHQ-4), one study with Kessler Psychological Distress Scale (K-10), one with Self-Depression Scale (SDS), one with the 10 item Center for Epidemiologic Studies Depression Scale (CES-D-10), and one with professional health diagnosis. The mean maternal age and gestational age in this research was 30.26 years and 25.73 weeks, respectively. This review included studies from many countries. However, most studies were conducted in a single country, with only a few conducted multinationally. These countries include China, Hong Kong, Japan, Iran, Qatar, Israel, Egypt, Turkey, Italy, Switzerland, the Netherlands, Greece, Spain, the United Kingdom, Ireland, Norway, Poland, the United States of America, Canada, and Mexico. All studies were assessed for quality using the New-castle-Ottawa Scale (Tables 2, 3).
Table 1.
Characteristics of studies included
| Study | Country | Study design | Mean MA (years) | Mean GA (weeks) | Depression scale | Depression (%) | Sample size | ||
|---|---|---|---|---|---|---|---|---|---|
| Pregnant (%) | Postpartum (%) | Total (%) | |||||||
| Ahlers-Schmidt et al. [18] (2020) | USA | Cohort | 25.3 | - | Diagnosis (58-item electronic survey) | - | - | 9 (7.9) | 114 |
| An et al. [19] (2021) | China | Cross-sectional | 30.39 | - | EPDS (≥10) | 0 | 119 (56.9) | 119 (56.9) | 209 |
| Basu et al. [20] (2021) | 64 countries | Cross-sectional | 31.3 | PHQ-4 (≥6) | 1,775 (31) | 363 (30.7) | 2,138 (31.0) | 6,894 | |
| Berthelot et al. [21] (2020) | Canada | Cohort | 29.27 | 24.8 | K10 (≥30) | 30 (2.38) | - | 30 (2.38) | 1,258 |
| Brik et al. [22] (2021) | Spain | Cohort | 32.3 | - | EPDS (≥10) | 62 (38) | - | 62 (38) | 164 |
| Ceulemans et al. [23] (2021) | Ireland, Norway, Switzerland, the Netherlands, and UK | Cross-sectional | - | - | EDS (≥13) | 533 | 592 | 1,125 | 8,087 |
| Chrzan-Dętkoś et al. [24] (2021) | Poland | Cross-sectional | 31.74 | 38.88 | EPDS (≥10) | 0 | 65 (83.32) | 65 (83.32) | 78 |
| Dong et al. [25] (2021) | China | Cross-sectional | - | - | SDS (>50) | 79 (50.6) | 0 | 79 (50.6) | 156 |
| Durankuş et al. [26] (2020) | Turkey | Cross-sectional | 29.56 | 7.04 | EPDS (≥13) | 92 (35.4) | 0 | 92 (35.4) | 260 |
| Fallon et al. [27] (2021) | UK | Cross-sectional | 30.9 | - | EPDS (≥13) | 0 | 264 (43) | 264 (43) | 614 |
| Farewell et al. [28] (2020) | USA | Mixed-method pilot | - | - | PHQ-2 (≥3) | - | - | 3 (12) | 27 |
| Farrell et al. [29] (2020) | Qatar | Cross-sectional | 30.5 | 26.1 | PHQ-9 (≥5) | - | - | 113 (39.2) | 288 |
| Gur et al. [30] (2020) | USA | Cross-sectional | 32.45 | 24.86 | PHQ-2 (>2) | 78 (9.9) | 0 | 78 (9.9) | 787 |
| Hiiragi et al. [31] (2021) | Japan | Retrospective cohort | - | - | EPDS (≥9) | 0 | 38 (14) | 38 (14) | 279 |
| Hui et al. [32] (2021) | Hong Kong | Retrospective cohort | 33.1 | - | EPDS (≥10) | 0 | 133 (14.4) | 133 (14.4) | 954 |
| Janevic et al. [33] (2021) | USA | Cross-sectional | - | - | PHQ-2 (3–6) | 0 | 13 (5.83) | 13 (5.83) | 223 |
| Jiang et al. [34] (2021) | China | Cross-sectional | 29 | - | EDS (≥10) | 859 (45.9) | 0 | 859 (45.9) | 1,873 |
| Khamees et al. [35] (2021) | Egypt | Cross-sectional | 25.08 | 6.58 | EPDS (≥14) | 53 (44.2) | 0 | 53 (44.2) | 120 |
| King et al. [36] (2021) | USA | Cohort | 33.69 | 26.79 | EPDS (≥11) | 144 (42) | 0 | 144 (42) | 343 |
| Lebel et al. [37] (2020) | Canada | Cross-sectional | 32.4 | 22.5 | EPDS (≥13) | 653 (37) | 0 | 653 (37) | 1,764 |
| Li et al. [38] (2021) | China | Cross-sectional | 30.19 | - | PHQ-9 (≥5) | - | - | 778 (35.34) | 2,201 |
| Li et al. [39] (2020) | China | Cross-sectional | - | - | PHQ-9 (≥5) | 29 (64.4) | 0 | 29 (64.4) | 45 |
| Liang et al. [40] (2020) | China | Cross-sectional | - | - | EPDS (≥10) | 0 | 253 (30) | 253 (30) | 845 |
| Lin et al. [41] (2021) | China | Cross-sectional | 30.51 | - | PHQ-9 (≥5) | 266 (35.4) | 0 | 266 (35.4) | 751 |
| Liu et al. [42] (2021) | USA | Cross-sectional | - | - | EPDS (>13) | 260 (36.4) | 0 | 260 (36.4) | 715 |
| Lubián López et al. [43] (2021) | Spain | Cross-sectional | - | - | EPDS (>10) | 182 (35.4) | 0 | 182 (35.4) | 514 |
| Matsushima and Horiguchi [44] (2022) | Japan | Cross-sectional | - | - | EPDS (≥13) | 303 (17) | 0 | 303 (17) | 1,777 |
| Medina-Jimenez et al. [45] (2020) | Mexico | Cross-sectional | 28.1 | 27.9 | EPDS (≥14) | 88 (17.5) | 0 | 88 (17.5) | 503 |
| Mo et al. [46] (2021) | China | Cross-sectional | - | - | PHQ-9 (≥5) | 1,989 (48.7) | 0 | 1,989 (48.7) | 4,087 |
| Molgora et al. [47] (2020) | Italy | Cross-sectional | - | - | EPDS (≥13) | 133 | 49 | 182 (31.65) | 575 |
| Ng et al. [48] (2020) | Singapore | Cross-sectional | 31.8 | - | DASS-21 (>9) | 59 (18.4) | 0 | 59 (18.4) | 324 |
| Nodoushan et al. [49] (2020) | Iran | Cross-sectional | - | 39.4 | DASS | 220 (39.2) | 0 | 220 (39.2) | 560 |
| Obata et al. [50] (2021) | Japan | Cross-sectional | - | 23.3 | EPDS (≥9) | 1,608 (31.83) | 867 | 2,475 (31.83) | 7,775 |
| Oskovi-Kaplan et al. [51] (2021) | Turkey | Cross-sectional | 26 | - | EPDS (≥13) | 0 | 33 (14.79) | 33 (14.79) | 223 |
| Ostacoli et al. [52] (2020) | Italy | Cross-sectional | 34.77 | - | EPDS (≥11) | 0 | 72 (44.2) | 72 (44.2) | 163 |
| Pariente et al. [53] (2020) | Israel | Cohort | 29.1 | - | EPDS (≥10) | 0 | 38 (23.5) | 52 (23.5) | 223 |
| Perzow et al. [54] (2021) | USA | Prospective cohort | 31.81 | - | EPDS (≥10) | - | - | 45 (33.3) | 135 |
| Racine et al. [55] (2021) | Canada | Prospective cohort | - | - | CES-D-10 (≥10) | 458 (35.21) | - | 458 (35.21) | 1,301 |
| Sade et al. [56] (2020) | Israel | Cross-sectional | - | - | EPDS (≥10) | 84 (25) | - | 21 (25) | 84 |
| Silverman et al. [57] (2020) | New York, USA | Cohort | 27 | 27.3 | EPDS (≥9) | - | 97 (18.8) | 97 (18.8) | 516 |
| Suárez-Rico et al. [58] (2021) | Mexico | Cross-sectional | 29.9 | EPDS (≥13) | - | 115 (39.2) | 115 (39.2) | 293 | |
| Sun et al. [59] (2020) | Wuhan, China | Cross-sectional | - | - | EPDS | 234 (31.7) | 714 (34.1) | 972 (33.71) | 2,830 |
| Kahyaoglu Sut and Kucukkaya [60] (2021) | Turkey | Cross-sectional | 28.2 | - | HADS-D (≥8) | 227 (56.3) | - | 227 (56.3) | 403 |
| Thayer et al. [61] (2021) | USA | Cross-sectional | - | - | EPDS (≥15) | 496 (23.6) | - | 496 (23.6) | 2,099 |
| Tsakiridis et al. [62] (2021) | Greece | Cross-sectional | - | 25.4 | EPDS (≥13) | 68 (13.5) | - | 68 (13.5) | 505 |
| Wang et al. [5] (2021) | China | Cross-sectional | - | - | PHQ-9 (>5) | 6,723 (43.6) | - | 6,723 (43.6) | 15,328 |
| Wu et al. [63] (2020) | China | Cross-sectional | - | 39.41 | EPDS (≥10) | 381 (29.6) | - | 381 (29.6) | 1,285 |
| Xu et al. [64] (2021) | China | Cross-sectional | 30.4 | - | EPDS (≥10) | 44 (16.1) | - | 44 (16.1) | 274 |
| Yang et al. [65] (2021) | China | Cross-sectional | - | - | PHQ-9 (≥5) | 8,712 (44.6) | - | 8,712 (44.6) | 19,515 |
| Zanardo et al. [66] (2020) | Northeastern Italy | Case–control | 33.73 | - | EPDS (>12) | - | 26 (28.6) | 26 (28.6) | 91 |
| Zeng et al. [68] (2020) | China | Cross-sectional | 29.2 | - | EPDS | 109 (21.12) | 11 (10.1) | 625 (19.2) | 625 |
| Zhang et al. [67] (2020) | China | Cross-sectional | 28.9 | - | EPDS (≥10) | 1,094 (58) | - | 1,094 (58) | 1,901 |
| Zhou et al. [69] (2021) | China | Cross-sectional | 29.95 | - | PHQ-9 | 527 (41.63) | - | 527 (41.63) | 1,266 |
| Zilver et al. [70] (2021) | The Netherlands | Cohort | 32.02 | - | HADS-D (≥8) | 145 (13.2) | - | 145 (13.2) | 1,102 |
MA, maternal age; GA, gestational age; EPDS, edinburgh postnatal depression scale; PHQ, patient health questionnaire; K-10, kessler psychological distress scale; EDS, Edinburgh depression scale; SDS, self-depression rating scale; DASS, depression anxiety and stress scale; CES-D-10, the 10 item center for epidemiologic studies depression scale; HADS, hospital anxiety and depression scale-depression.
Table 2.
Criteria of the new Ottawa scale scoring
| Score | |
|---|---|
| 1. Validated measure | |
| Was the measure of depression or anxiety clearly defined, valid, reliable, and implemented consistently across all study participants? | 0=no, 1=yes |
| 2. Peer review | |
| Was the study published in a journal (i.e., peer reviewed) | 0=no (unpublished), 1=yes |
| 3. Response rate | |
| Was the participation rate of eligible persons at least 50%? measured consistently across participants? |
0=no, 1=yes |
| 4. Objectivity of measure | |
| Does the study rely on self-report of depression or anxiety symptoms, or does it use an objective measure (i.e., diagnostic interview)? | 0=self-report, 1=diagnostic interview |
| 5. Exposure time | |
| Was the measurement time frame of anxiety or depression sufficient so that one could reasonably expect to see an association between COVID-19 and any symptoms if they existed (i.e., at least one week since the onset of COVID-19 in the country in which the study was conducted)? | 0=no, 1=yes |
| 6. Representativeness of the sample | |
| Was the sample truly representative of the target population? | 0=no, 1=yes |
Adapted from the National Institutes of Health (NIH) assessment tool for observational cohort and cross-sectional studies and the Newcastle-Ottawa quality assessment scale for cross-sectional studies.
Table 3.
New Ottawa scale of the studies included in this review
| Study | Validated measure | Published | Response rate | Measure objectivity | Sufficient exposure | Representative Sample | Total |
|---|---|---|---|---|---|---|---|
| Ahlers-Schmidt et al. [18] (2020) | Yes | Yes | Yes | Yes | Yes | No | 5 |
| An et al. [19] (2021) | Yes | Yes | Yes | No | Yes | No | 4 |
| Basu et al. [20] (2021) | Yes | Yes | No | No | Yes | No | 3 |
| Berthelot et al. [21] (2020) | Yes | Yes | Yes | No | Yes | Yes | 5 |
| Brik et al. [22] (2021) | Yes | Yes | Yes | No | Yes | Yes | 5 |
| Ceulemans et al. [23] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Chrzan-Dętkoś et al. [24] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Dong et al. [25] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Durankuş et al. [26] (2020) | Yes | Yes | Yes | No | Yes | No | 4 |
| Fallon et al. [27] (2021) | Yes | Yes | Unknown | No | Yes | Unknown | 3 |
| Farewell et al. [28] (2020) | Yes | Yes | Yes | No | Yes | No | 3 |
| Farrell et al. [29] (2020) | Yes | Yes | Unknown | No | Yes | Yes | 4 |
| Gur et al. [30] (2020) | Yes | Yes | No | No | Yes | Yes | 4 |
| Hiiragi et al. [31] (2021) | Yes | Yes | Yes | No | Yes | No | 3 |
| Hui et al. [32] (2021) | Yes | Yes | Yes | No | Yes | No | 4 |
| Janevic et al. [33] (2021) | Yes | Yes | No | No | Yes | Unknown | 3 |
| Jiang et al. [34] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Khamees et al. [35] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| King et al. [36] (2021) | Yes | Yes | No | No | Yes | No | 3 |
| Lebel et al. [37] (2020) | Yes | Yes | Unknown | No | Yes | No | 4 |
| Li et al. [38] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Li et al. [39] (2020) | Yes | Yes | Yes | No | Yes | No | 4 |
| Liang et al. [40] (2020) | Yes | Yes | Yes | No | Yes | No | 3 |
| Lin et al. [41] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Liu et al. [42] (2021) | Yes | Yes | Yes | No | Yes | No | 4 |
| Lubián López et al. [43] (2021) | Yes | Yes | Unknown | No | Yes | Unknown | 3 |
| Matsushima and Horiguchi [44] (2022) | Yes | Yes | No | No | Yes | No | 3 |
| Medina-Jimenez et al. [45] (2020) | Yes | Yes | Yes | No | Yes | Yes | 5 |
| Mo et al. [46] (2021) | Yes | Yes | Yes | No | Yes | No | 4 |
| Molgora et al. [47] (2020) | Yes | Yes | Yes | No | Yes | Unknown | 4 |
| Ng et al. [48] (2020) | Yes | Yes | Yes | No | Yes | No | 4 |
| Nodoushan et al. [49] (2020) | Yes | Yes | Unknown | No | Yes | Yes | 4 |
| Obata et al. [50] (2021) | Yes | Yes | Yes | No | Yes | Yes | 5 |
| Oskovi-Kaplan et al. [51] (2021) | Yes | Yes | No | No | Yes | No | 3 |
| Ostacoli et al. [52] (2020) | Yes | Yes | Yes | No | Yes | No | 4 |
| Pariente et al. [53] (2020) | Yes | Yes | Yes | No | Yes | Unknown | 4 |
| Perzow et al. [54] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Racine et al. [55] (2021) | Yes | Yes | Yes | No | Yes | No | 4 |
| Sade et al. [56] (2020) | Yes | Yes | Yes | No | Yes | No | 4 |
| Silverman et al. [57] (2020) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Suárez-Rico et al. [58] (2021) | Yes | Yes | Yes | No | Yes | Yes | 5 |
| Sun et al. [59] (2020) | Yes | Yes | Yes | No | Yes | No | 4 |
| Kahyaoglu Sut and Kucukkaya [60] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Thayer et al. [61] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Tsakiridis et al. [62] (2021) | Yes | Yes | Yes | No | Yes | Unknown | 4 |
| Wang et al. [5] (2021) | Yes | Yes | Unknown | No | Yes | Yes | 4 |
| Wu et al. [63] (2020) | Yes | Yes | Unknown | No | Yes | Yes | 4 |
| Xu et al. [64] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Yang et al. [65] (2021) | Yes | Yes | Yes | No | Yes | Yes | 5 |
| Zanardo et al. [66] (2020) | Yes | Yes | Yes | No | Yes | No | 4 |
| Zeng et al. [67] (2020) | Yes | Yes | Yes | No | Yes | Yes | 5 |
| Zhang et al. [68] (2020) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Zhou et al. [69] (2021) | Yes | Yes | Unknown | No | Yes | No | 3 |
| Zilver et al. [70] (2021) | Yes | Yes | Unknown | No | Yes | Yes | 4 |
3. Prevalence of depression among pregnant and postpartum women during the COVID-19 pandemic
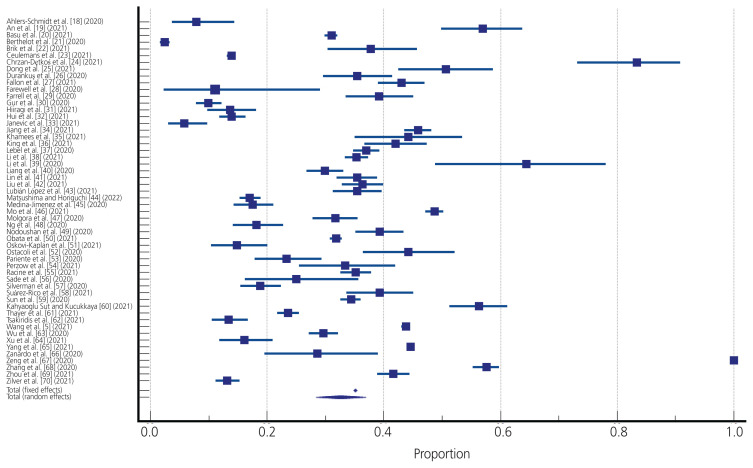
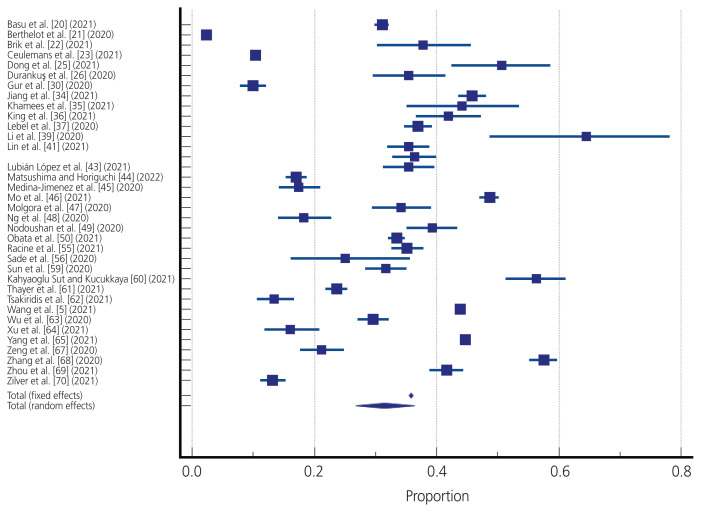
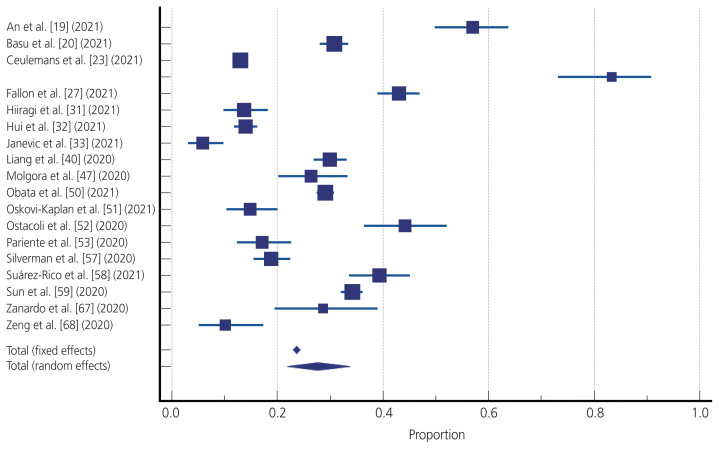
A random-effects meta-analysis of 54 studies revealed a pooled event rate of 0.326 (95% confidence interval [CI], 0.284–0.369), which suggested that the prevalence of depression was 32.6% across the study. This meta-analysis found no evidence of publication bias, which was confirmed statistically by the Begg’s test and Egger’s test of intercept. There was significant between-study heterogeneity (Q=9778.38, P<0.001, I2=99.46). For the pregnant and post-partum women subgroups, a random-effects meta-analysis of 36 and 19 studies revealed pooled event rates of 0.314 (95% CI, 0.268–0.363) and 0.276 (95% CI, 0.219–0.337), respectively. Both results suggested that the prevalence of depression across the studies were 31.4% and 27.6% for pregnant and postpartum women, respectively. Significant heterogeneity between-studies was also demonstrated in both the pregnant and postpartum women subgroups (Q=6728.83, P<0.001, I2=99.48 and Q=1132.91, P<0.001, I2=98.41). The forest plots of the data are shown in Figs. 2–4.
Fig. 2.
Forest plot of 54 studies assessing the prevalence of depression in pregnant and postpartum women.
Fig. 3.
Forest plot of 36 studies assessing the prevalence of depression in pregnant women.
Fig. 4.
Forest plot of 19 studies assessing depression prevalence among postpartum women.
Discussion
In this meta-analysis, we found significantly elevated rates of depression among pregnant and postpartum women during the COVID-19 pandemic compared with the global prevalence of depression before the COVID-19 pandemic, which ranged from 17–20.7% [10,11]. Approximately one-third of the pregnant and postpartum women in this study developed depression during the COVID-19 pandemic. Pregnant and postpartum women undergo significant physical, social, and psychological changes. Consequently, they may be at higher risk of developing mental health problems, particularly depression. Several studies have revealed that depression was prevalent among pregnant women and those in the post-partum period before the COVID-19 pandemic [13,71–78]. In addition, the present study showed a higher prevalence of depression in pregnant and postpartum women during the COVID-19 pandemic than in the general population, which was 28.0% [79].
Since its recognition in December 2019, COVID-19 has spread rapidly worldwide, with serious health, social, and financial consequences. The COVID-19 pandemic has caused significant public health emergencies and resulted in increased fear, anxiety, and uncertainty, especially among pregnant women who are more susceptible to respiratory pathogens and are at an increased risk of severe pneumonia due to the immunological and physiological changes that occur during pregnancy [80]. The prevalence of depression in pregnant and postpartum women increased during the COVID-19 pandemic, ranging from 17% to 31% [13,80–85]. A systematic review and meta-analysis of 19 studies revealed that the pooled prevalence of depression in pregnant and postpartum women during the COVID-19 pandemic was 25% [82]. Another meta-analysis of 15 studies with 11.187 pregnant women found the prevalence of depression to be 30% [85]. A study conducted by Yan et al. [86] (that included 23 studies with 20.569 participants) also found that the prevalence of depression in pregnant and postpartum women was high during the COVID-19 pandemic. Fears of contracting or transmitting COVID-19, worry about their pregnancy and the health of their newborn, the lockdowns/ quarantine, poor economic conditions, loss of income, insufficient social support, and lack of access to healthcare professionals contributed significantly to the mental health of pregnant and postpartum women during the COVID-19 pandemic [28,29,35,40].
During the COVID-19 pandemic, meeting the mental health needs of pregnant and postpartum women was a considerable challenge. Prenatal and postnatal psychiatric problems have substantial long-term adverse effects on mothers, fetuses, and children. The negative consequences include complications during pregnancy and childbirth (pre-eclampsia, miscarriage, preterm birth, gestational hypertension, low infant birth weight, and stillbirth) [87,88]. A systematic review and meta-analysis conducted by Chmielewska et al. [89] revealed that the incidence of maternal mortality, maternal stress, stillbirth, and ruptured ectopic pregnancy was higher during the COVID-19 pandemic compared to that before the COVID-19 pandemic.
Several factors increased the risk of depression in pregnant women during the COVID-19 pandemic, including COVID-19-related worries (fear of infection, worry about the baby’s safety during pregnancy, and the health of family members) [80]. Social restrictions arising from the pandemic constrained pregnant women from accessing healthcare services. Moreover, pregnant women may have been concerned about the possibility of exposure to SARS-CoV-2 when visiting medical facilities, which compelled them to delay antenatal care visits, obstetric examinations, and hospitalization before delivery. In addition, they also wanted to give birth by cesarean section rather than wait for delivery in the hospital [90]. Depression during pregnancy, if left untreated, can have negative obstetric consequences and is linked to inadequate prenatal care, poor maternal health, and postpartum depression [91].
Similar to other mental disorders, biopsychosocial factors are implicated in the etiology of postpartum depression. The possibility of getting infected by SARS-CoV-2 became a new stressor for postpartum women during the pandemic. The uncertainty and unpredictability of the pandemic, which caused fluctuations in regulations, could have played a role [40]. Some situations related to the pandemic such as decreased socioeconomic status and the absence of visitors were risk factors. Lack of support from healthcare staff due to the hospitals’ rush during the pandemic was also a risk factor. Postpartum women living in high-risk COVID-19 transmission areas have a higher risk of developing postpartum depression [52]. We cannot ignore the role factors such as mother’s personal history, poor marital relationship, and prior negative pregnancy experience play in the development of depression, in addition to pandemic-related risk factors [52].
We included all available high-quality studies and updated the literature on depression among pregnant and postpartum women. Our study also highlighted the vulnerable groups among the study population.
This study has some limitations. First, there was high heterogeneity between the included studies; however, the funnel plot was symmetrical. The primary cause of heterogeneity is thought to be the various scales and cut-offs used for its analysis (EPDS, PHQ-9, PHQ-2, HADS, EDS, DASS, PHQ-4, K-10, SDS, and CES-D-10), with only one study conducted by professional health diagnosis. Samples were collected at different times and in different countries in each study. Hence, the challenge faced during the COVID-19 pandemic that served as a stressor differed in every study. Furthermore, the use of self-reported questionnaires may indicate the presence of biases such as social desirability bias, such that pregnant women may have underreported or overreported their data. Second, most of the included studies collected data through online surveys, resulting in a selection bias [92,93]. Finally, majority of included studies were cross-sectional. Hence, further studies on the long-term impact of the COVID-19 pandemic on the mental health of pregnant and postpartum women, particularly depression, are needed.
Conclusion
In conclusion, we demonstrated that the prevalence of depression among pregnant and postpartum women during the COVID-19 pandemic was higher than that before the COVID-19 pandemic. The rate of depression is higher in pregnant women than in postpartum women.
Footnotes
Conflict of interest
There is no conflict of interest in this research.
Ethical approval
No ethical approval was required because this review analyzed published data.
Patient consent
No patient consent was needed for this research.
Funding information
None.
References
- 1.Khoury R, Bernstein PS, Debolt C, Stone J, Sutton DM, Simpson LL, et al. Characteristics and outcomes of 241 births to women with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection at five New York City medical centers. Obstet Gynecol. 2020;136:273–82. doi: 10.1097/AOG.0000000000004025. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) Rolling updates on coronavirus disease (COVID-19) [Internet] Geneva: WHO; c2020. [cited 2021 July 15]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen . [Google Scholar]
- 3.Tsamakis K, Triantafyllis AS, Tsiptsios D, Spartalis E, Mueller C, Tsamakis C, et al. COVID-19 related stress exacerbates common physical and mental pathologies and affects treatment (review) Exp Ther Med. 2020;20:159–62. doi: 10.3892/etm.2020.8671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wastnedge EAN, Reynolds RM, van Boeckel SR, Stock SJ, Denison FC, Maybin JA, et al. Pregnancy and COVID-19. Physiol Rev. 2021;101:303–18. doi: 10.1152/physrev.00024.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Q, Mo PKH, Song B, Di JL, Zhou FR, Zhao J, et al. Mental health and preventive behaviour of pregnant women in China during the early phase of the COVID-19 period. Infect Dis Poverty. 2021;10:37. doi: 10.1186/s40249-021-00825-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamzehgardeshi Z, Omidvar S, Amoli AA, Firouzbakht M. Pregnancy-related anxiety and its associated factors during COVID-19 pandemic in Iranian pregnant women: a web-based cross-sectional study. BMC Pregnancy Child-birth. 2021;21:208. doi: 10.1186/s12884-021-03694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alipour Z, Lamyian M, Hajizadeh E. Anxiety and fear of childbirth as predictors of postnatal depression in nulliparous women. Women Birth. 2012;25:e37–43. doi: 10.1016/j.wombi.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Pearlstein T. Depression during pregnancy. Best Pract Res Clin Obstet Gynaecol. 2015;29:754–64. doi: 10.1016/j.bpobgyn.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Lupattelli A, Spigset O, Koren G, Nordeng H. Risk of vaginal bleeding and postpartum hemorrhage after use of antidepressants in pregnancy: a study from the Norwegian mother and child cohort study. J Clin Psychopharmacol. 2014;34:143–8. doi: 10.1097/JCP.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 10.Yin X, Sun N, Jiang N, Xu X, Gan Y, Zhang J, et al. Prevalence and associated factors of antenatal depression: systematic reviews and meta-analyses. Clin Psychol Rev. 2021;83:101932. doi: 10.1016/j.cpr.2020.101932. [DOI] [PubMed] [Google Scholar]
- 11.Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. J Psychiatr Res. 2018;104:235–48. doi: 10.1016/j.jpsychires.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Sidhu GS, Sidhu TK, Kaur P, Lal D, Sangha NK. Evaluation of peripartum depression in females. Int J Appl Basic Med Res. 2019;9:201–5. doi: 10.4103/ijabmr.IJABMR_23_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Demissie DB, Bitew ZW. Mental health effect of COVID-19 pandemic among women who are pregnant and/or lactating: a systematic review and meta-analysis. SAGE Open Med. 2021;9:20503121211026195. doi: 10.1177/20503121211026195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet] Ottawa: Ottawa Hospital Research Institute; 2015. [cited 2021 July 12]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm . [Google Scholar]
- 15.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenwood DC. Meta-analysis of Observational Studies. In: Tu YK, Greenwood D, editors. Modern Methods for Epidemiology. Dordrecht: Springer, Dordrecht; 2012. pp. 173–90. [Google Scholar]
- 17.MedCalc Software . MedCalc, version 19.5.1. Ostend: MedCalc, Software Ltd; 2020. [Google Scholar]
- 18.Ahlers-Schmidt CR, Hervey AM, Neil T, Kuhlmann S, Kuhlmann Z. Concerns of women regarding pregnancy and childbirth during the COVID-19 pandemic. Patient Educ Couns. 2020;103:2578–82. doi: 10.1016/j.pec.2020.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.An R, Chen X, Wu Y, Liu J, Deng C, Liu Y, et al. A survey of postpartum depression and health care needs among Chinese postpartum women during the pandemic of COVID-19. Arch Psychiatr Nurs. 2021;35:172–7. doi: 10.1016/j.apnu.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Basu A, Kim HH, Basaldua R, Choi KW, Charron L, Kelsall N, et al. A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLoS ONE. 2021;16:e0249780. doi: 10.1371/journal.pone.0249780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berthelot N, Lemieux R, Garon-Bissonnette J, Drouin-Maziade C, Martel É, Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand. 2020;99:848–55. doi: 10.1111/aogs.13925. [DOI] [PubMed] [Google Scholar]
- 22.Brik M, Sandonis MA, Fernández S, Suy A, Parramon-Puig G, Maiz N, et al. Psychological impact and social support in pregnant women during lockdown due to SARS-CoV2 pandemic: a cohort study. Acta Obstet Gynecol Scand. 2021;100:1026–33. doi: 10.1111/aogs.14073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ceulemans M, Foulon V, Ngo E, Panchaud A, Winterfeld U, Pomar L, et al. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic-A multinational cross-sectional study. Acta Obstet Gynecol Scand. 2021;100:1219–29. doi: 10.1111/aogs.14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chrzan-Dętkoś M, Walczak-Kozłowska T, Lipowska M. The need for additional mental health support for women in the postpartum period in the times of epidemic crisis. BMC Pregnancy Childbirth. 2021;21:114. doi: 10.1186/s12884-021-03544-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dong H, Hu R, Lu C, Huang D, Cui D, Huang G, et al. Investigation on the mental health status of pregnant women in China during the pandemic of COVID-19. Arch Gynecol Obstet. 2021;303:463–9. doi: 10.1007/s00404-020-05805-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Durankuş F, Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J Matern Fetal Neonatal Med. 2020;35:205–11. doi: 10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- 27.Fallon V, Davies SM, Silverio SA, Jackson L, De Pascalis L, Harrold JA. Psychosocial experiences of postnatal women during the COVID-19 pandemic. A UK-wide study of prevalence rates and risk factors for clinically relevant depression and anxiety. J Psychiatr Res. 2021;136:157–156. doi: 10.1016/j.jpsychires.2021.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Farewell CV, Jewell J, Walls J, Leiferman JA. A mixed-methods pilot study of perinatal risk and resilience during COVID-19. J Prim Care Community Health. 2020;11:2150132720944074. doi: 10.1177/2150132720944074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farrell T, Reagu S, Mohan S, Elmidany R, Qaddoura F, Ahmed EE, et al. The impact of the COVID-19 pandemic on the perinatal mental health of women. J Perinat Med. 2020;48:971–6. doi: 10.1515/jpm-2020-0415. [DOI] [PubMed] [Google Scholar]
- 30.Gur RE, White LK, Waller R, Barzilay R, Moore TM, Kornfield S, et al. The disproportionate burden of the COVID-19 pandemic among pregnant black women. Psychiatry Res. 2020;293:113475. doi: 10.1016/j.psychres.2020.113475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hiiragi K, Obata S, Misumi T, Miyagi E, Aoki S. Psychological stress associated with the COVID-19 pandemic in postpartum women in Yokohama, Japan. J Obstet Gynaecol Res. 2021;47:2126–30. doi: 10.1111/jog.14776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hui PW, Ma G, Seto MTY, Cheung KW. Effect of COVID-19 on delivery plans and postnatal depression scores of pregnant women. Hong Kong Med J. 2021;27:113–7. doi: 10.12809/hkmj208774. [DOI] [PubMed] [Google Scholar]
- 33.Janevic T, Maru S, Nowlin S, McCarthy K, Bergink V, Stone J, et al. Pandemic birthing: childbirth satisfaction, perceived health care bias, and postpartum health during the COVID-19 pandemic. Matern Child Health J. 2021;25:860–9. doi: 10.1007/s10995-021-03158-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiang H, Jin L, Qian X, Xiong X, La X, Chen W, et al. Maternal mental health status and approaches for accessing antenatal care information during the COVID-19 epidemic in China: cross-sectional study. J Med Internet Res. 2021;23:e18722. doi: 10.2196/18722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khamees RE, Taha OT, Ali TYM. Anxiety and depression during pregnancy in the era of COVID-19. J Perinat Med. 2021;49:674–7. doi: 10.1515/jpm-2021-0181. [DOI] [PubMed] [Google Scholar]
- 36.King LS, Feddoes DE, Kirshenbaum JS, Humphreys KL, Gotlib IH. Pregnancy during the pandemic: the impact of COVID-19-related stress on risk for prenatal depression. Psychol Med. 2021. Mar 30, [Epub]. [DOI] [PMC free article] [PubMed]
- 37.Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020;277:5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li C, Huo L, Wang R, Qi L, Wang W, Zhou X, et al. The prevalence and risk factors of depression in prenatal and postnatal women in China with the outbreak of corona virus disease 2019. J Affect Disord. 2021;282:1203–9. doi: 10.1016/j.jad.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li X, Lu P, Hu L, Huang T, Lu L. Factors associated with mental health results among workers with income losses exposed to COVID-19 in China. Int J Environ Res Public Health. 2020;17:5627. doi: 10.3390/ijerph17155627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liang P, Wang Y, Shi S, Liu Y, Xiong R. Prevalence and factors associated with postpartum depression during the COVID-19 pandemic among women in Guangzhou, China: a cross-sectional study. BMC Psychiatry. 2020;20:557. doi: 10.1186/s12888-020-02969-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin W, Wu B, Chen B, Lai G, Huang S, Li S, et al. Sleep conditions associate with anxiety and depression symptoms among pregnant women during the epidemic of COVID-19 in Shenzhen. J Affect Disord. 2021;281:567–73. doi: 10.1016/j.jad.2020.11.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu J, Hung P, Alberg AJ, Hair NL, Whitaker KM, Simon J, et al. Mental health among pregnant women with COVID-19-related stressors and worries in the united states. Birth. 2021;48:470–9. doi: 10.1111/birt.12554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lubián López DM, Butrón Hinojo CA, Arjona Bernal JE, Fasero Laiz M, Alcolea Santiago J, Guerra Vilches V, et al. Resilience and psychological distress in pregnant women during quarantine due to the COVID-19 outbreak in Spain: a multicentre cross-sectional online survey. J Psychosom Obstet Gynaecol. 2021;42:115–22. doi: 10.1080/0167482X.2021.1896491. [DOI] [PubMed] [Google Scholar]
- 44.Matsushima M, Horiguchi H. The COVID-19 pandemic and mental well-being of pregnant women in Japan: need for economic and social policy interventions. Disaster Med Public Health Prep. 2022;16:449–54. doi: 10.1017/dmp.2020.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Medina-Jimenez V, Bermudez-Rojas ML, Murillo-Bargas H, Rivera-Camarillo AC, Muñoz-Acosta J, Ramirez-Abarca TG, et al. The impact of the COVID-19 pandemic on depression and stress levels in pregnant women: a national survey during the COVID-19 pandemic in Mexico. J Matern Fetal Neonatal Med. 2020. Nov 26, [Epub]. [DOI] [PubMed]
- 46.Mo PKH, Fong VWI, Song B, Di J, Wang Q, Wang L. Association of perceived threat, negative emotions, and self-efficacy with mental health and personal protective behavior among Chinese pregnant women during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2021;23:e24053. doi: 10.2196/24053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Molgora S, Accordini M. Motherhood in the time of coronavirus: the impact of the pandemic emergency on expectant and postpartum women’s psychological well-being. Front Psychol. 2020;11:567155. doi: 10.3389/fpsyg.2020.567155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ng QJ, Koh KM, Tagore S, Mathur M. Perception and feelings of antenatal women during COVID-19 pandemic: a cross-sectional survey. Ann Acad Med Singap. 2020;49:543–52. [PubMed] [Google Scholar]
- 49.Nodoushan RJ, Alimoradi H, Nazari M. Spiritual health and stress in pregnant women during the Covid-19 pandemic. SN Compr Clin Med. 2020;2:2528–34. doi: 10.1007/s42399-020-00582-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Obata S, Miyagi E, Haruyama Y, Umazume T, Kobashi G, Yoshimi A, et al. Psychological stress among pregnant and puerperal women in Japan during the coronavirus disease 2019 pandemic. J Obstet Gynaecol Res. 2021;47:2990–3000. doi: 10.1111/jog.14877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oskovi-Kaplan ZA, Buyuk GN, Ozgu-Erdinc AS, Keskin HL, Ozbas A, Moraloglu Tekin O. The effect of COVID-19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: a preliminary study. Psychiatr Q. 2021;92:675–82. doi: 10.1007/s11126-020-09843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ostacoli L, Cosma S, Bevilacqua F, Berchialla P, Bovetti M, Carosso AR, et al. Psychosocial factors associated with postpartum psychological distress during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20:703. doi: 10.1186/s12884-020-03399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pariente G, Wissotzky Broder O, Sheiner E, Lanxner Battat T, Mazor E, Yaniv Salem S, et al. Risk for probable post-partum depression among women during the COVID-19 pandemic. Arch Womens Ment Health. 2020;23:767–73. doi: 10.1007/s00737-020-01075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Perzow SED, Hennessey EP, Hoffman MC, Grote NK, Davis EP, Hankin BL. Mental health of pregnant and postpartum women in response to the COVID-19 pandemic. J Affect Disord Rep. 2021;4:100123. doi: 10.1016/j.jadr.2021.100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Racine N, Hetherington E, McArthur BA, McDonald S, Edwards S, Tough S, et al. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatry. 2021;8:405–15. doi: 10.1016/S2215-0366(21)00074-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sade S, Sheiner E, Wainstock T, Hermon N, Yaniv Salem S, Kosef T, et al. Risk for depressive symptoms among hospitalized women in high-risk pregnancy units during the COVID-19 pandemic. J Clin Med. 2020;9:2449. doi: 10.3390/jcm9082449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Silverman ME, Burgos L, Rodriguez ZI, Afzal O, Kalishman A, Callipari F, et al. Postpartum mood among universally screened high and low socioeconomic status patients during COVID-19 social restrictions in New York City. Sci Rep. 2020;10:22380. doi: 10.1038/s41598-020-79564-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Suárez-Rico BV, Estrada-Gutierrez G, Sánchez-Martínez M, Perichart-Perera O, Rodríguez-Hernández C, González-Leyva C, et al. Prevalence of depression, anxiety, and perceived stress in postpartum Mexican women during the COVID-19 lockdown. Int J Environ Res Public Health. 2021;18:4627. doi: 10.3390/ijerph18094627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sun G, Wang Q, Lin Y, Li R, Yang L, Liu X, et al. Perinatal depression of exposed maternal women in the COVID-19 pandemic in Wuhan, China. Front Psychiatry. 2020;11:551812. doi: 10.3389/fpsyt.2020.551812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kahyaoglu Sut H, Kucukkaya B. Anxiety, depression, and related factors in pregnant women during the COVID-19 pandemic in Turkey: a web-based cross-sectional study. Perspect Psychiatr Care. 2021;57:860–8. doi: 10.1111/ppc.12627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thayer ZM, Gildner TE. COVID-19-related financial stress associated with higher likelihood of depression among pregnant women living in the united states. Am J Hum Biol. 2021;33:e23508. doi: 10.1002/ajhb.23508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tsakiridis I, Dagklis T, Mamopoulos A, Athanasiadis A, Pearson R, Papazisis G. Antenatal depression and anxiety during the COVID-19 pandemic: a cross-sectional study in pregnant women from routine health care contact in Greece. J Perinat Med. 2021;49:656–63. doi: 10.1515/jpm-2020-0473. [DOI] [PubMed] [Google Scholar]
- 63.Wu Y, Zhang C, Liu H, Duan C, Li C, Fan J, et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol. 2020;223:240. doi: 10.1016/j.ajog.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xu K, Zhang Y, Zhang Y, Xu Q, Lv L, Zhang J. Mental health among pregnant women under public health interventions during COVID-19 outbreak in Wuhan, China. Psychiatry Res. 2021;301:113977. doi: 10.1016/j.psychres.2021.113977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yang X, Song B, Wu A, Mo PKH, Di J, Wang Q, et al. Social, cognitive, and ehealth mechanisms of COVID-19-related lockdown and mandatory quarantine that potentially affect the mental health of pregnant women in China: cross-sectional survey study. J Med Internet Res. 2021;23:e24495. doi: 10.2196/24495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zanardo V, Manghina V, Giliberti L, Vettore M, Severino L, Straface G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynaecol Obstet. 2020;150:184–8. doi: 10.1002/ijgo.13249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zeng X, Li W, Sun H, Luo X, Garg S, Liu T, et al. Mental health outcomes in perinatal women during the remission phase of COVID-19 in China. Front Psychiatry. 2020;11:571876. doi: 10.3389/fpsyt.2020.571876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang CJP, Wu H, He Z, Chan NK, Huang J, Wang H, et al. Psychobehavioral responses, post-traumatic stress and depression in pregnancy during the early phase of COVID-19 outbreak. Psychiatr Res Clin Pract. 2021;3:46–54. doi: 10.1176/appi.prcp.20200019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhou Y, Wang R, Liu L, Ding T, Huo L, Qi L, et al. The impact of lockdown policy on depressive symptoms among pregnant women in China: mediating effects of internet use and family support. Glob Health Res Policy. 2021;6:11. doi: 10.1186/s41256-021-00193-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zilver SJM, Broekman BFP, Hendrix YMGA, de Leeuw RA, Mentzel SV, van Pampus MG, et al. Stress, anxiety and depression in 1466 pregnant women during and before the COVID-19 pandemic: a Dutch cohort study. J Psychosom Obstet Gynaecol. 2021;42:108–14. doi: 10.1080/0167482X.2021.1907338. [DOI] [PubMed] [Google Scholar]
- 71.Tokumitsu K, Sugawara N, Maruo K, Suzuki T, Shimoda K, Yasui-Furukori N. Prevalence of perinatal depression among Japanese women: a meta-analysis. Ann Gen Psychiatry. 2020;19:41. doi: 10.1186/s12991-020-00290-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mu TY, Li YH, Pan HF, Zhang L, Zha DH, Zhang CL, et al. Postpartum depressive mood (PDM) among Chinese women: a meta-analysis. Arch Womens Ment Health. 2019;22:279–87. doi: 10.1007/s00737-018-0885-3. [DOI] [PubMed] [Google Scholar]
- 73.Upadhyay RP, Chowdhury R, Salehi A, Sarkar K, Singh SK, Sinha B, et al. Postpartum depression in India: a systematic review and meta-analysis. Bull World Health Organ. 2017;95:706–17C. doi: 10.2471/BLT.17.192237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zeleke TA, Getinet W, Tadesse Tessema Z, Gebeyehu K. Prevalence and associated factors of post-partum depression in Ethiopia. A systematic review and meta-analysis. PLoS One. 2021;16:e0247005. doi: 10.1371/journal.pone.0247005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tolossa T, Fetensa G, Yilma MT, Abadiga M, Wakuma B, Besho M, et al. Postpartum depression and associated factors among postpartum women in Ethiopia: a systematic review and meta-analysis, 2020. Public Health Rev. 2020;41:21. doi: 10.1186/s40985-020-00136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Özcan NK, Boyacıoğlu NE, Dinç H. Postpartum depression prevalence and risk factors in Turkey: a systematic review and meta-analysis. Arch Psychiatr Nurs. 2017;31:420–8. doi: 10.1016/j.apnu.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 77.Zegeye A, Alebel A, Gebrie A, Tesfaye B, Belay YA, Adane F, et al. Prevalence and determinants of antenatal depression among pregnant women in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2018;18:462. doi: 10.1186/s12884-018-2101-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mahendran R, Puthussery S, Amalan M. Prevalence of antenatal depression in South Asia: a systematic review and meta-analysis. J Epidemiol Community Health. 2019;73:768–77. doi: 10.1136/jech-2018-211819. [DOI] [PubMed] [Google Scholar]
- 79.Nochaiwong S, Ruengorn C, Thavorn K, Hutton B, Awiphan R, Phosuya C, et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep. 2021;11:10173. doi: 10.1038/s41598-021-89700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kajdy A, Feduniw S, Ajdacka U, Modzelewski J, Baranowska B, Sys D, et al. Risk factors for anxiety and depression among pregnant women during the COVID-19 pandemic: a web-based cross-sectional survey. Medicine (Baltimore) 2020;99:e21279. doi: 10.1097/MD.0000000000021279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shorey SY, Ng ED, Chee CYI. Anxiety and depressive symptoms of women in the perinatal period during the COVID-19 pandemic: a systematic review and meta-analysis. Scand J Public Health. 2021;49:730–40. doi: 10.1177/14034948211011793. [DOI] [PubMed] [Google Scholar]
- 82.Fan S, Guan J, Cao L, Wang M, Zhao H, Chen L, et al. Psychological effects caused by COVID-19 pandemic on pregnant women: a systematic review with meta-analysis. Asian J Psychiatry. 2021;56:102533. doi: 10.1016/j.ajp.2020.102533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ghazanfarpour M, Bahrami F, Rashidi Fakari F, Ashrafinia F, Babakhanian M, Dordeh M, et al. Prevalence of anxiety and depression among pregnant women during the COVID-19 pandemic: a meta-analysis. J Psychosom Obstet Gynaecol. 2021;24:1–12. doi: 10.1080/0167482X.2021.1929162. [DOI] [PubMed] [Google Scholar]
- 84.Tomfohr-Madsen LM, Racine N, Giesbrecht GF, Lebel C, Madigan S. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2021;300:113912. doi: 10.1016/j.psychres.2021.113912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sun F, Zhu J, Tao H, Ma Y, Jin W. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J Psychosom Obstet Gynaecol. 2021;42:91–9. doi: 10.1080/0167482X.2020.1857360. [DOI] [PubMed] [Google Scholar]
- 86.Yan H, Ding Y, Guo W. Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Front Psychol. 2020;11:617001. doi: 10.3389/fpsyg.2020.617001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ding XX, Wu YL, Xu SJ, Zhu RP, Jia XM, Zhang SF, et al. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159:103–10. doi: 10.1016/j.jad.2014.02.027. [DOI] [PubMed] [Google Scholar]
- 88.Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67:1012–24. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chmielewska B, Barratt I, Townsend R, Kalafat E, van der Meulen J, Gurol-Urganci I, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021;9:e759–72. doi: 10.1016/S2214-109X(21)00079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Desiyanti IW, Nuzuliana R. Mental health of pregnant women during the COVID-19 pandemic: scoping review. Women, Midwives and Midwifery. 2021;1:57–72. [Google Scholar]
- 91.Chen H, Selix N, Nosek M. Perinatal anxiety and depression during COVID-19. J Nurse Pract. 2021;17:26–31. doi: 10.1016/j.nurpra.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatry. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the zung scales. BMC Psychiatry. 2017;17:329. doi: 10.1186/s12888-017-1489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]