Abstract
Background
The objective of this study was to compare inpatient mortality rates for patients with operatively treated closed femoral shaft fractures (AO/OTA 32 A-C) who received venous thromboembolism (VTE) prophylaxis with either low molecular weight heparin (LMWH) or unfractionated heparin.
Methods
This was a retrospective cohort study of a national database of patients presenting to Level I through IV trauma centers in the United States. All patients ≥18 years of age who sustained an operatively treated closed femoral shaft fracture were included. The primary outcome of inpatient mortality was compared between two groups: those who received LMWH or unfractionated heparin for VTE prophylaxis. Secondary outcomes were complications including VTE and bleeding events. Groups were compared using a multivariate regression model.
Results
There were 2058 patients included in the study. Patients who received VTE prophylaxis with LMWH had lower odds of inpatient mortality compared to patients who received VTE prophylaxis with unfractionated heparin (OR 0.19; 95% CI 0.05 to 0.68, p = 0.011).
Conclusions
VTE prophylaxis with LMWH is associated with lower inpatient mortality compared to VTE prophylaxis with unfractionated heparin for patients undergoing operative treatment of closed femoral shaft fractures. To our knowledge this is the first study to report these associations for a specific subset of orthopedic trauma patients.
Keywords: Femoral shaft fracture, Venous thromboembolism, Low molecular weight heparin, Mortality, National trauma data bank
1. Introduction
1.1 Venous thromboembolism (VTE) is a leading cause of inpatient mortality in the United States.1, 2, 3, 4 Hospital admission for any trauma is one of the most common risk factors for the development of VTE.1 Acutely traumatized patients with a diagnosis of VTE not only have higher mortality rates than those without, they also have a higher morbidity profile including increased risk for longer hospital stay and development of sepsis and multi-organ system failure.5 Patients who sustain a fracture or other injury requiring orthopaedic care are particularly at risk for VTE. Approximately 0.8 to five percent of orthopaedic trauma patients are diagnosed with symptomatic VTE, with rates varying by injury severity and body location of injury.6,7 The incidence of occult deep vein thrombosis (DVT) diagnosed on surveillance ultrasound after surgery for lower extremity fracture is 28%.8
1.2 Given the ubiquity and severity of the problem for orthopedic trauma patients, clinicians and investigators have attempted many ways to prevent VTE in patients admitted after orthopaedic trauma. Two of the most common types of chemical VTE prophylaxis are low molecular weight heparin (LMWH) and unfractionated heparin. Data suggest that for all trauma patients, as well as specific subsets of trauma patients such as those sustaining traumatic spine injuries, LMWH may be superior to unfractionated heparin with regard to mortality.9, 10, 11, 12
1.3 Despite its widespread use in orthopedic trauma patients, there is a lack of data that compares these two common types of VTE prophylaxis. The objective of this study was therefore to compare inpatient mortality rates for patients with operatively treated closed femoral shaft fractures (AO/OTA 32 A-C) who received VTE prophylaxis with either LMWH or unfractionated heparin. We hypothesized that for patients who undergo fixation of closed femoral shaft fractures, low molecular weight heparin (LMWH) would have an inpatient mortality benefit compared to patients who did not receive VTE prophylaxis with LMWH.
2. Methods
2.1. Study design, participants, and data collection
We conducted an analysis of the National Trauma Data Bank (NTDB) using data from the year 2013 with the purpose of comparing inpatient mortality rates for patients with closed, operatively-treated femoral shaft fractures who receive chemical VTE prophylaxis with either LMWH or unfractionated heparin. The NTDB is a prospectively collected registry of trauma data maintained by the Committee on Trauma of the American College of Surgeons. With over 7.5 million patient records from more than 900 trauma centers, it is the largest repository of trauma data in the world.13 As a convenience sample, the NTDB is not nationally-representative of all trauma incidents in the United States, though it is considered to be representative of all level I/II trauma facilities.13 The data set is de-identified and no protected health information is provided.
Inclusion criteria were all patients age greater than or equal to 18 years with a diagnosis of closed femoral shaft fracture (AO/OTA type 32A through C) treated with open reduction and internal fixation who received VTE prophylaxis using LMWH or unfractionated heparin. The diagnosis of closed femoral shaft fracture and the procedural code for open reduction and internal fixation were recorded in the NTDB using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9 CM) coding. ICD-9 CM diagnosis code 821.01 and ICD-CM procedure code 79.35 were used to identify patients with closed femoral shaft fractures and those who underwent open reduction and internal fixation of the femur, respectively. The ICD-9 CM procedural coding does not allow differentiation between methods of fixation, for example between internal fixation using a plate versus an intramedullary nail. Exclusion criteria were patients less than 18 years of age and patients with missing treatment, demographic, or injury data.
2.2. Variables
Demographic data were age, gender, race, comorbidities (alcoholism, bleeding disorder, congestive heart failure, current smoker, chronic renal failure, history of cerebral vascular accident (CVA) or residual neurological deficit, diabetes mellitus types I or II, functionally dependent health status, history of myocardial infarction (MI), hypertension requiring medication, obesity, respiratory disease, cirrhosis, dementia), modified Charlson Comorbidity Index (mCCI), primary payment method, and hospital trauma level designation. The modified CCI has comparable predictive value to the original CCI and may be superior to the American Society of Anesthesiologists (ASA) score in predicting adverse outcomes.14,15 Injury characteristics, treatment, and hospital course data were injury severity score (ISS), body region of injury (head, face, neck, thorax, abdomen, spine, upper and lower extremity), emergency medical services (EMS) response time, type of VTE prophylaxis (LMWH or unfractionated heparin) and time to VTE prophylaxis. The NTDB specifies use of a given anticoagulant by recording it as VTE prophylaxis as opposed to treatment.16
The primary outcome variable was in-hospital mortality. The NTDB provides data for hospital admissions only and therefore our follow-up was end of hospital admission. The secondary outcome variables were diagnosis of VTE, both combined and separated into DVT and pulmonary embolism (PE), acute respiratory distress syndrome (ARDS), cardiac arrest, MI, CVA, unplanned intubation, bleeding events, and any combined complication. Bleeding events were defined by combining ICD-9 CM codes 530.82 (esophageal hemorrhage), 535.31 (alcoholic gastritis with hemorrhage), 535.51 (unspecified gastritis and gsatroduodenitis with hemorrhage), 578.9 (unspecified hemorrhage of the gastrointestinal tract), 578.0 (hematemesis), 578.1 (blood in stool), 599.71 (gross hematuria), and 784.7 (epistaxis). These codes have been used to study warfarin-related bleeding events.17 Additional secondary outcome variables were hospital length of stay and intensive care unit (ICU) length of stay.
2.3. Statistical analyses
Descriptive statistics were counts and percent of total study population for categorical variables. The study groups were compared across categorical baseline demographic and injury variables using Pearson's chi-squared analysis. We performed univariate regression to compare outcomes between groups. Significant results from the baseline demographic and injury variable comparisons were used in an adjusted multivariate regression. Multivariate analysis was used preferentially over propensity score matching because of the number of events per confounding variable.18 Because patients with an ISS of greater than 15 have a higher risk of mortality after trauma compared to those with an ISS of less than or equal to 15, we performed a subgroup analysis of patients with an ISS greater than 15 to determine the association between VTE prophylaxis type and outcomes for patients with an already-elevated risk of mortality, in which complications with minimum 10 cases were analyzed to fulfill multiple regression criteria.19 To correct for multiple group comparisons, a Bonferroni correction was applied with statistical significance set to p < 0.05 at baseline. All statistical analyses were conducted using R version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria).
3. Results
3.1. Patient demographics
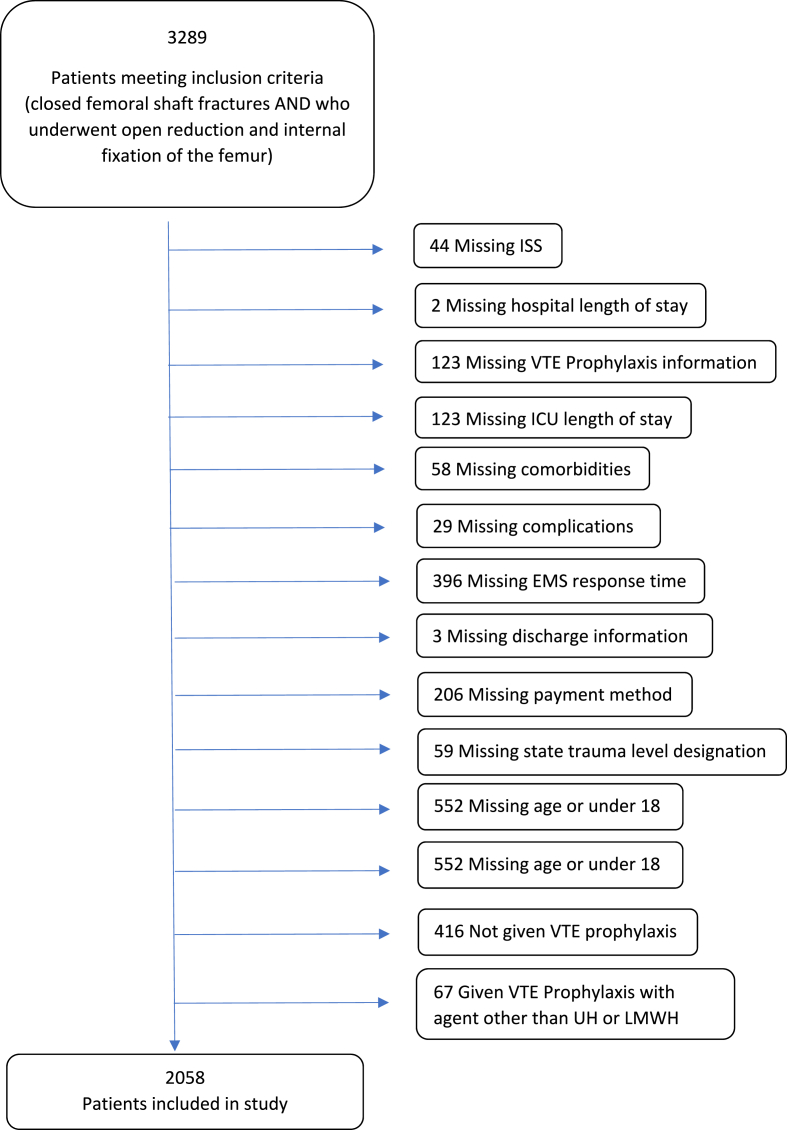
Query of the NTDB yielded 2058 patients with a closed femoral shaft fracture treated operatively (Fig. 1). Of these patients, 1766 (85.8%) had VTE prophylaxis with LMWH and 292 (14.2%) had VTE prophylaxis with unfractionated heparin (Table 1).
Fig. 1.
Flowsheet of included patients.
Table 1.
Operatively treated closed femoral shaft fractures by VTE prophylaxis agent.
| VTE Prophylaxis Agent |
|||
|---|---|---|---|
| Patients (N) | UH (%) | LMWH (%) | |
| Closed femoral shaft fracturea | 2058 | 292 (14.2) | 1766 (85.8) |
VTE: venous thromboembolism, UH: unfractionated heparin, LMWH: low molecular weight heparin.
ICD 9 code 821.01 (closed femoral shaft fracture, middle or upper third) AND ICD 9 code 79.35 (open reduction or fracture with internal fixation, femur)97 patients (3.0%) had an invalid value recorded and 85 (2.6%) had no value recorded.
Patients more commonly had VTE prophylaxis with LMWH if they were age 18–34 years compared to 35 to 59 and 60 or greater (Supplemental Table 1). There was no significant difference in chemical VTE prophylaxis method by time to initiation of VTE prophylaxis. Other statistically significant and non-significant variations by patient baseline demographics and injury characteristics are presented in Supplemental Table 1.
3.2. Univariate model
The primary outcome of in-hospital mortality occurred in 16 patients (0.8%) and is presented along with secondary outcomes in Table 2. VTE was diagnosed in 108 (5.2%) patients, with DVT more common than PE (74 or 3.6% versus 48 or 2.3%). Univariate analysis revealed a statistically significant association between VTE prophylaxis type and in-hospital mortality (p = 0.0007), diagnosis of VTE (PE or DVT) (p = 0.0003), any complication (p < 0.001), and hospital length of stay (p < 0.0001). There was no significant association between VTE prophylaxis type and other secondary outcomes including diagnosis of PE or DVT (p = 0.02 and 0.010 respectively, not significant after correcting for multiple comparisons) and bleeding events (p = 1.0).
Table 2.
Analysis of VTE and other adverse events by prophylaxis type.
| Patients (N) | VTE Prophylaxis Agent |
P-value | ||
|---|---|---|---|---|
| UH (%) | LMWH (%) | |||
| Outcome | ||||
| VTE (PE or DVT) | 108 | 29 (9.9) | 79 (4.5) | 0.0003 |
| PE | 48 | 13 (4.5) | 35 (2) | 0.019 |
| DVT | 74 | 19 (6.5) | 55 (3.1) | 0.0097 |
| ARDS | 36 | 7 (2.4) | 29 (1.6) | 0.338 |
| Cardiac arrest | 13 | 4 (1.4) | 9 (0.5) | 0.101 |
| MI | 9 | 3 (1) | 6 (0.3) | 0.124 |
| Stroke/CVA | 9 | 1 (0.3) | 8 (0.5) | 1.000 |
| Unplanned Intubation | 26 | 7 (2.4) | 19 (1.1) | 0.083 |
| Bleed Event | 1 | 0 (0) | 1 (0.1) | 1.000 |
| Any complication | 179 | 45 (15.4) | 134 (7.6) | <.0001 |
| Death | 16 | 8 (2.7) | 8 (0.5) | 0.0007 |
| Hospital Length of Stay (Days) | <.0001 | |||
| 1 to 4 | 729 | 40 (13.7) | 505 (28.6) | |
| 5 to 9 | 1153 | 119 (40.8) | 771 (43.7) | |
| 10 or greater | 780 | 133 (45.5) | 489 (27.7) | |
| ICU length of stay (Days) | 0.0049 | |||
| 1 to 4 | 437 | 49 (16.8) | 287 (16.3) | |
| 5 to 9 | 223 | 39 (13.4) | 140 (7.9) | |
| 10 or greater | 235 | 49 (16.8) | 141 (8) | |
†Significant P-values are defined as <0.05/12 = 0.0041 after Bonferroni correction and are presented in bold.
VTE: venous thromboembolism, UH: unfractionated heparin, LMWH: low molecular weight heparin, DVT: deep vein thrombosis, PE: pulmonary embolism, ARDS: acute respiratory distress syndrome, MI: myocardial infarction, CVA: cerebrovascular accident.
3.3. Multivariate model
The potentially confounding variables incorporated into the multivariate regression model were age; gender; injury region (head injury); significantly different comorbidities of CHF, chronic renal failure, diabetes mellitus, functionally dependent health status, HTN requiring medication, and dementia; Injury Severity Score range; primary payment method; hospital trauma level designation; number of days to VTE prophylaxis, and time to procedure.
Patients who received VTE prophylaxis with LMWH had lower odds of inpatient mortality compared to patients who received VTE prophylaxis with unfractionated heparin (OR 0.19; 95% CI 0.05 to 0.68, p = 0.011). Patients who received VTE prophylaxis with LMWH also had lower odds of VTE (PE and DVT combined; OR 0.53; 95% CI 0.32 to 0.90, p = 0.016) and PE (OR 0.41; 95% CI 0.2–0.86, p = 0.014). Patients who had chemical VTE prophylaxis did not have increased odds of being diagnosed with a bleeding event (Table 3).
Table 3.
Adjusted multivariate regression analysis of adverse outcomes by prophylaxis type.
| Outcome | OR (95% CI) | P-value |
|---|---|---|
| Death | 0.19 (0.05–0.68) | 0.0108 |
| Any Complication | 0.58 (0.38–0.89) | 0.0105 |
| VTE (PE or DVT) | 0.53 (0.32–0.90) | 0.0155 |
| PE | 0.41 (0.20–0.86) | 0.0143 |
| DVT | 0.68 (0.37–1.33) | 0.239 |
| ARDS | 1.03 (0.41–3.05) | 0.959 |
| Cardiac arrest | 0.23 (0.05–1.12) | 0.059 |
| MI | 0.74 (0.11–6.56) | 0.762 |
| Stroke/CVA | 2.96 (0.35–83.66) | 0.411 |
| Unplanned Intubation | 0.63 (0.25–1.77) | 0.351 |
Reference group for multivariable analysis was prophylactic agent of ‘Unfractionated Heparin’.
VTE: venous thromboembolism, DVT: deep vein thrombosis, PE: pulmonary embolism, ARDS: acute respiratory distress syndrome, MI: myocardial infarction, CVA: cerebrovascular accident.
3.4. Subgroup analysis
There were 566 patients included in the subgroup analysis of patients with an ISS of greater than 15. There were no significant differences among groups for any baseline demographic or injury characteristic (Supplemental Table 2). There were 7 deaths (1.2% of patients) in the subgroup. Univariate analysis did not show a significant difference between groups for in-patient mortality (Table 4). However, on multivariate analysis, patients who received VTE prophylaxis with LMWH had lower odds of any complication (OR 0.48; 95% CI 0.26 to 0.88, p = 0.015), VTE (OR 0.42; 95% CI 0.21 to 0.87, p = 0.016), and PE (OR 0.22; 95% CI 0.07 to 0.67, p = 0.007) compared to patients who received VTE prophylaxis with unfractionated heparin (Table 5).
Table 4.
Subgroup analysis of VTE and other adverse events by prophylaxis type for ISS>15.
| Patients (N) | VTE Prophylaxis Agent |
P-value | ||
|---|---|---|---|---|
| UH (%) | LMWH (%) | |||
| Outcome | ||||
| VTE (PE or DVT) | 53 | 18 (18.8) | 35 (7.4) | 0.0017 |
| PE | 20 | 8 (8.3) | 12 (2.6) | 0.012 |
| DVT | 41 | 13 (13.5) | 28 (6) | 0.016 |
| ARDS | 19 | 2 (2.1) | 17 (3.6) | 0.755 |
| Cardiac arrest | 8 | 3 (3.1) | 5 (1.1) | 0.141 |
| MI | 2 | 1 (1) | 1 (0.2) | 0.314 |
| Stroke/CVA | 3 | 0 (0) | 3 (0.6) | 1.000 |
| Unplanned Intubation | 17 | 4 (4.2) | 13 (2.8) | 0.509 |
| Bleed Event | 0 | 0 (0) | 0 (0) | 1.000 |
| Any complication | 90 | 26 (27.1) | 64 (13.6) | 0.0021 |
| Death | 7 | 4 (4.2) | 3 (0.6) | 0.0181 |
| Hospital Length of Stay (Days) | 0.026 | |||
| 1 to 4 | 39 | 3 (3.1) | 36 (7.7) | |
| 5 to 9 | 193 | 25 (26) | 168 (35.7) | |
| 10 or greater | 333 | 68 (70.8) | 265 (56.4) | |
| ICU length of stay (Days) | 0.067 | |||
| 1 to 4 | 154 | 21 (21.9) | 133 (28.3) | |
| 5 to 9 | 116 | 22 (22.9) | 94 (20) | |
| 10 or greater | 150 | 36 (37.5) | 114 (24.3) | |
†Significant P-values are defined as <0.05/12 = 0.0041 after Bonferroni correction and are presented in bold.
ISS: Injury Severity Scale, VTE: venous thromboembolism, UH: unfractionated heparin, LMWH: low molecular weight heparin, DVT: deep vein thrombosis, PE: pulmonary embolism, ARDS: acute respiratory distress syndrome, MI: myocardial infarction, CVA: cerebrovascular accident.
Table 5.
Subgroup multivariate regression analysis of adverse outcomes by prophylaxis.
| Outcome | OR (95% CI) | P-value |
|---|---|---|
| Any Complication | 0.48 (0.26–0.88) | 0.0151 |
| VTE (PE or DVT) | 0.42 (0.21–0.87) | 0.0161 |
| PE | 0.22 (0.07–0.67) | 0.0069 |
| DVT | 0.53 (0.24–1.24) | 0.126 |
| ARDS | 2.16 (0.49–16.89) | 0.374 |
VTE: venous thromboembolism, DVT: deep vein thrombosis, PE: pulmonary embolism, ARDS: acute respiratory distress syndrome.
Reference group for multivariable analysis was prophylactic agent of ‘Unfractionated Heparin’.
4. Discussion
4.1 Our data show that in a large national trauma database from which we extracted patients with closed femoral shaft fractures treated operatively, patients who received chemical VTE prophylaxis with LMWH had significantly lower odds of in-patient mortality compared to patients who received VTE prophylaxis with unfractionated heparin, even after adjusting for potential confounding variables. To our knowledge this is the first study of a cohort of orthopedic trauma patients to suggest that there is a mortality difference when comparing these two commonly used VTE prophylaxis agents.
4.2 These data are important because they may point toward ways to improve the risk of in-patient mortality for patients with operatively treated closed femoral shaft fractures. In-patient mortality after closed femoral shaft fracture is a significant problem, with mortality estimates ranging from 2 to 14%.20,21 Risk factors for in-patient mortality after femoral shaft fracture fixation are higher injury severity score, older age, and timing of surgical fixation, with some evidence suggesting that earlier fixation is better than late, depending on hemodynamic stability, associated cardiopulmonary injuries, and cranial injury burden.22, 23, 24, 25, 26 Recent evidence also suggests that pre-operative anticoagulation places trauma patients at higher risk of inpatient mortality compared to patients who are not on pre-operative anticoagulation, potentially due to increased number of patient comorbidities and higher patient age.27 Data such as ours may support the administration of LMWH for VTE prophylaxis as opposed to unfractionated heparin for patients with closed femoral shaft fracture.
4.3 Our finding of significantly lower odds of in-patient mortality for all study patients and patients with an ISS of greater than 15 who had VTE prophylaxis with LMWH compared to unfractionated heparin aligns with data from other trauma populations. Both registry data and a meta-analysis of prospective and retrospective data supports the administration of LMWH over unfractionated heparin for VTE prophylaxis in all trauma patients.10,12 Jacobs et al. found decreased odds of not only mortality but also PE and DVT for LMWH compared to unfractionated heparin in an analysis of the Michigan Trauma Quality Improvement Program.12 Additional data supporting the use of LMWH over unfractionated heparin comes from studies of spine trauma patients and patients who sustain traumatic brain injuries.9,11 To our knowledge our data is the first to report a similar finding for a cohort of orthopedic trauma patients, those with closed, operatively-treated femoral shaft fractures.
4.4 Our study strengths are the use of a large national dataset that is representative of a geographically diverse patient population and our inclusion of numerous patient demographic, comorbidity, and injury characteristics. Our study has various weaknesses. Database studies are limited by selection bias and by amount and quality of data. For example, we do not know the decision making that went into choice of VTE prophylaxis agent. We also do not know dosing of VTE prophylaxis, which is itself subject to variability, with data suggesting that LMWH may be underdosed 50% of the time based on anti-Xa levels.28,29 These data, which could have further stratified patients in terms of VTE risk, were not available for our patient population. We attempted to mitigate these limitations of selection bias and data quantity and quality by including numerous baseline patient characteristics such as comorbidities, body injury location (head, thorax, abdomen, and spine among them), and injury severity score into our multivariate model. We also attempted to mitigate these limitations by performing a subgroup analysis of patients with an ISS of greater than 15 to account for the multiple injuries that can confound an analysis such as ours.
4.5 A major opportunity for further investigation is a prospective randomized study comparing mortality and development of VTE among patients with operative extremity or pelvis fractures who receive VTE prophylaxis with LMWH to another VTE prophylaxis agent. A similar study is ongoing, and others like it will help establish guidelines for VTE prophylaxis in orthopedic trauma patients.30 This will address an important gap in orthopedic knowledge and may unify a currently fragmented approach to prophylaxis.31
4.6 In conclusion, VTE prophylaxis with LMWH is associated with lower inpatient mortality compared to VTE prophylaxis with unfractionated heparin for patients undergoing operative treatment of closed femoral shaft fractures. To our knowledge this is the first study to report these associations for a specific subset of orthopedic trauma patients.
Funding & submission statement
This study does not have any prior or duplicate submissions or publications elsewhere of any part of the work. Funding from the Orthopaedic Science Research Foundation was used to complete this study. No funding from the National Institutes of Health; Wellcome Trust; or Howard Hughes Medical Institute, were utilized to complete this study.
IRB statement
This study utilized national, de-identified data and is exempt from IRB review.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2022.101949.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ja H., Wm O., Tm P., et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med. 2002;162(11):1245–1248. doi: 10.1001/ARCHINTE.162.11.1245. [DOI] [PubMed] [Google Scholar]
- 2.Lindblad B., Eriksson A., Bergqvist D. Autopsy-verified pulmonary embolism in a surgical department: analysis of the period from 1951 to 1988. Br J Surg. 1991;78(7):849–852. doi: 10.1002/BJS.1800780725. [DOI] [PubMed] [Google Scholar]
- 3.Bergqvist D., Lindblad B. A 30-year survey of pulmonary embolism verified at autopsy: an analysis of 1274 surgical patients. Br J Surg. 1985;72(2):105–108. doi: 10.1002/BJS.1800720211. [DOI] [PubMed] [Google Scholar]
- 4.Cushman M., Tsai A.W., White R.H., et al. Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Am J Med. 2004;117(1):19–25. doi: 10.1016/J.AMJMED.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 5.T P., A W., R L., et al. Venous thromboembolism after severe trauma: incidence, risk factors and outcome. Injury. 2010;41(1):97–101. doi: 10.1016/J.INJURY.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 6.Ja L., Sm M., S A., Cb J. The incidence of venous thromboembolism following pelvic and lower extremity trauma despite adherence to modern prophylactic protocols. J Orthop Trauma. 2020;34(8):418–421. doi: 10.1097/BOT.0000000000001790. [DOI] [PubMed] [Google Scholar]
- 7.Cm T., Ml R., Rm V.H., et al. Venous thromboembolism after trauma: a never event? Crit Care Med. 2012;40(11):2967–2973. doi: 10.1097/CCM.0B013E31825BCB60. [DOI] [PubMed] [Google Scholar]
- 8.G A., Re B., Ge P., R H., Ms R. Incidence of deep-vein thrombosis in patients with fractures of the lower extremity distal to the hip. J Orthop Trauma. 1996;10(4):230–235. doi: 10.1097/00005131-199605000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Neifert S.N., Chapman E.K., Rothrock R.J., et al. Lower mortality and morbidity with low-molecular-weight heparin for venous thromboembolism prophylaxis in spine trauma. Spine. 2020;45(23):1613–1618. doi: 10.1097/BRS.0000000000003664. [DOI] [PubMed] [Google Scholar]
- 10.Tran A., Fernando S.M., Carrier M., et al. Efficacy and safety of low molecular weight heparin versus unfractionated heparin for prevention of venous thromboembolism in trauma patients: a systematic review and meta-analysis. Ann Surg. 2021 doi: 10.1097/SLA.0000000000005157. Published online August 13. [DOI] [PubMed] [Google Scholar]
- 11.Benjamin E., Recinos G., Aiolfi A., Inaba K., Demetriades D. Pharmacological thromboembolic prophylaxis in traumatic brain injuries: low molecular weight heparin is superior to unfractionated heparin. Ann Surg. 2017;266(3):463–469. doi: 10.1097/SLA.0000000000002359. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs B.N., Cain-Nielsen A.H., Jakubus J.L., et al. Unfractionated heparin versus low-molecular-weight heparin for venous thromboembolism prophylaxis in trauma. J Trauma Acute Care Surg. 2017;83(1):151–158. doi: 10.1097/TA.0000000000001494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zg H., Ah K., Ab N. Practical guide to surgical data sets: national trauma Data Bank (NTDB) JAMA Surg. 2018;153(9):852–853. doi: 10.1001/JAMASURG.2018.0483. [DOI] [PubMed] [Google Scholar]
- 14.D'Hoore W., Bouckaert A., Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996;49(12):1429–1433. doi: 10.1016/S0895-4356(96)00271-5. [DOI] [PubMed] [Google Scholar]
- 15.Lakomkin N., Zuckerman S.L., Stannard B., et al. Preoperative risk stratification in spine tumor surgery: a comparison of the modified Charlson index, frailty index, and ASA score. Spine. 2019;44(13):E782–E787. doi: 10.1097/BRS.0000000000002970. [DOI] [PubMed] [Google Scholar]
- 16.Trauma N. 2013. National Trauma Data Standard. Published online. [Google Scholar]
- 17.Delate T., Jones A.E., Clark N.P., Witt D.M. Assessment of the coding accuracy of warfarin-related bleeding events. Thromb Res. 2017;159:86–90. doi: 10.1016/J.THROMRES.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Cepeda M.S., Boston R., Farrar J.T., Strom B.L. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;158(3):280–287. doi: 10.1093/aje/kwg115. [DOI] [PubMed] [Google Scholar]
- 19.Senkowski C.K., Mckenney M.G. 1999. Trauma Scoring Systems: A Review. Published online. [DOI] [PubMed] [Google Scholar]
- 20.Feldman G., Mosheiff R., Nasrallah K., Shabtai R., Davidson A., Weil Y.A. Evolution of treatment of femoral shaft fracture in polytrauma: did damage control orthopaedics improve the outcome? A retrospective study. Injury. 2021;52(7):1886–1890. doi: 10.1016/J.INJURY.2021.04.031. [DOI] [PubMed] [Google Scholar]
- 21.Nj N., Ha V. Timing of definitive treatment of femoral shaft fractures in patients with multiple injuries: a systematic review of randomized and nonrandomized trials. J Trauma Acute Care Surg. 2012;73(5):1046–1063. doi: 10.1097/TA.0B013E3182701DED. [DOI] [PubMed] [Google Scholar]
- 22.Jc D., Rv O. The evolution of damage control orthopedics: current evidence and practical applications of early appropriate care. Orthop Clin N Am. 2013;44(4):499–507. doi: 10.1016/J.OCL.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Morshed S., Miclau T., Bembom O., Cohen M., Knudson M.M., Colford J.M. Delayed internal fixation of femoral shaft fracture reduces mortality among patients with multisystem trauma. J Bone Joint Surg Am. 2009;91(1):3–13. doi: 10.2106/JBJS.H.00338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rv C., Sc G., Kf S. In-hospital mortality from femoral shaft fracture depends on the initial delay to fracture fixation and Injury Severity Score: a retrospective cohort study from the NTDB 2002-2006. J Trauma Acute Care Surg. 2014;76(6):1433–1440. doi: 10.1097/TA.0000000000000230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nahm N.J., Como J.J., Wilber J.H., Vallier H.A. Early appropriate care: definitive stabilization of femoral fractures within 24 hours of injury is safe in most patients with multiple injuries. J Trauma Inj Infect Crit Care. 2011;71(1):175–185. doi: 10.1097/TA.0B013E3181FC93A2. [DOI] [PubMed] [Google Scholar]
- 26.Nahm N.J., Vallier H.A. Timing of definitive treatment of femoral shaft fractures in patients with multiple injuries: a systematic review of randomized and nonrandomized trials. J Trauma Acute Care Surg. 2012;73(5):1046–1063. doi: 10.1097/TA.0B013E3182701DED. [DOI] [PubMed] [Google Scholar]
- 27.Rk N., Jh R., Mp D., et al. The impact of anticoagulation on trauma outcomes : an national trauma Data Bank study. Am Surg. 2020;86(7):773–781. doi: 10.1177/0003134820934419. [DOI] [PubMed] [Google Scholar]
- 28.D M., F J., T E., et al. Standard prophylactic enoxaparin dosing leads to inadequate anti-Xa levels and increased deep venous thrombosis rates in critically ill trauma and surgical patients. J Trauma. 2010;68(4):874–879. doi: 10.1097/TA.0B013E3181D32271. [DOI] [PubMed] [Google Scholar]
- 29.Singer G.A., Riggi G., Karcutskie C.A., et al. Anti-Xa-guided enoxaparin thromboprophylaxis reduces rate of deep venous thromboembolism in high-risk trauma patients. J Trauma Acute Care Surg. 2016;81(6):1101–1108. doi: 10.1097/TA.0000000000001193. [DOI] [PubMed] [Google Scholar]
- 30.Rv O., Dm S., Kp F., et al. PREVENTion of CLots in Orthopaedic Trauma (PREVENT CLOT): a randomised pragmatic trial protocol comparing aspirin versus low-molecular-weight heparin for blood clot prevention in orthopaedic trauma patients. BMJ Open. 2021;11(3) doi: 10.1136/BMJOPEN-2020-041845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hc S., J A., D C., et al. Venous thromboembolism prophylaxis in orthopaedic trauma patients: a survey of OTA member practice patterns and OTA expert panel recommendations. J Orthop Trauma. 2015;29(10):e355–e362. doi: 10.1097/BOT.0000000000000387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.