Abstract
Background
Effective health communication to encourage participation in COVID-19 preventive behaviours is crucial in helping mitigate viral spread. Intentions and beliefs are known determinants of adherence to these behaviours, therefore, health communication interventions based on these constructs may be effective. Visual languageless messages can be particularly useful in multilingual countries, where text-based communications can limit message exposure. This pre- and post-intervention study sought to identify the effect of exposure to languageless animated messages, presented in the Graphic Interchange Format (GIF), communicating COVID-19 preventive behaviours (physical distancing, handwashing, and mask-wearing) on behavioural intentions and beliefs.
Methods
Between February and March 2021, a nationally representative sample of 308 Guatemalan adults completed this online survey experiment. Self-reported performance of preventive behaviours, understanding of COVID-19 transmission risk, as well as intentions, self-efficacy, and outcome expectancy beliefs about preventive behaviours were assessed at baseline. Participants were then exposed to a random combination of three of four possible GIFs in random presentation order. Following exposure to each GIF, intentions, self-efficacy, and outcome expectancy beliefs were reassessed.
Results
In terms of main effects, GIF exposure was significantly associated with improved intentions, self-efficacy, and outcome expectancy beliefs in relation to physical distancing; intentions and outcome expectancy beliefs in relation to handwashing; and intentions and self-efficacy in relation to mask-wearing. These associations were not dependent on the combination of the three of four possible GIFs presented. Pairwise comparisons revealed that observed improvements in scores were most pronounced from baseline to the first GIF exposure and reduced thereafter.
Conclusions
Exposure to languageless GIFs communicating COVID-19 preventive behaviours is associated with improvements in key social-cognitive determinants of those behaviours. Dosage of GIF exposure and durability of effects are issues that warrant further attention so we can better understand the conditions and point at which benefits are maximised. Moreover, the effect on behavioural adherence is yet to be determined. GIFs provide a valuable means to widely disseminate health messages via social media during public health crises, such as COVID-19. When these messages are languageless, the potential reach of dissemination can be maximised.
Effective public health communications are critical in preventing the spread of COVID-19. Globally, government guidance and legislation have advocated and coerced evidence-based transmission preventive behaviours including physical distancing, good hygiene practices such as handwashing, and mask-wearing. Encouraging individual adherence to these behaviours is challenging, requiring input and evidence from behavioural science [1,2].
Increasing knowledge through information provision is generally considered necessary, but insufficient for health behaviour change [3,4]. Research on the individual determinants of transmission-preventive behaviours provides evidence of other potentially modifiable targets for behaviour change interventions to help during the COVID-19 pandemic. Intention, self-efficacy (ie, confidence in performing the behaviour) and outcome expectancy or behavioural efficacy (ie, anticipated consequences of the behaviour) have been shown to predict preventive behaviours of physical distancing (ie, maintaining 1-2 m of distance from people in other households), handwashing and mask-wearing [5-12].
Social Cognitive Theory (SCT) [13] is suitable for understanding how such beliefs impact adherence to COVID-19 preventive behaviours and provides a theoretical basis for behaviour change interventions designed to modify them. Self-efficacy, a key construct of SCT, is an important predictor of behaviour; the more confident an individual feels about engaging in a preventive behaviour, the more likely they will engage in it. Outcome expectancy, another key construct within SCT, is the belief that the behaviour will yield a particular result. SCT proposes that providing opportunities for individuals to instil expectations and self-efficacy by obtaining mastery and vicarious (modelling) experiences can produce behaviour change [14]. Self-efficacy can predict behavioural intentions to engage in COVID-19 preventive behaviours [15-16], and intentions often, but not always, predict behaviour performance [17].
Evidence suggests that information is better retained when health communications include visuals rather than text alone [18]. Unlike text-based health communications, visual communications do not rely on language but use images, animations, and videos to tell the message narrative. One such type of animated communication is the Graphics Interchange Format (GIF), a digital file format frequently used within digital communication with endless looping repetition and no sound. GIFs are easily shared within internet-based communication due to their small file size [19]. The important global role of languageless, animated messages promoting COVID-19 preventive behaviours has been recognised [20] and preliminary evidence has demonstrated its positive impact on behaviour change [21]. In countries with multiple official languages, languageless animated communications may provide a solution to effectively disseminate messages to the entire population.
Guatemala is one such country, with 25 official languages spoken (24 indigenous and Spanish). It is the most populous country in Central America with significant socioeconomic inequalities, a weak underfunded public health system, and some of the worst health issues globally [22,23]. As of January 7, 2022, Guatemala is one of the Central American countries most affected by COVID-19 with 631 730 confirmed cases, 16 114 deaths and 28.5% of the population fully vaccinated [24].
The present study aimed to identify the effect of exposure to languageless messages, in the form of original animated GIF images, communicating COVID-19 preventive behaviours on intentions, self-efficacy, and outcome expectancy beliefs in relation to physical distancing, handwashing and mask-wearing behaviours. We hypothesised that GIF exposure would be associated with improvements in intentions and beliefs about preventive behaviours.
METHODS
Study design
This study used a pre- and post-intervention repeated measures design.
Sample
Data were collected via an online survey in Spanish. Adults (18+ years) who lived in Guatemala and spoke Spanish, were eligible to participate and were recruited through QualtricsXM panel of respondents. Demographic quotas based on the 2018 census of Guatemala (ie, males = 58%; 18-24 years = 35%, 25-34 years = 41%, 35-44 years = 16%, 45-54 years = 6%, 55+ years = 2%) were used to provide a representative sample. Data collection occurred between February 18 and March 8, 2021, using the QualtricsXM survey platform (Version February 2021; Qualtrics, 2005; Provo, Utah, USA). At that time, Guatemala’s COVID-19 recommendations included keeping 1.5 m away from others, wearing a mask in public places and frequent handwashing with soap and water.
Materials
Four languageless GIFs were developed iteratively between June and December 2020. GIFs are usually created by taking a small section from existing media; however, the GIFs in this study were original artworks designed by the research team. Evidence from a review of existing COVID-19 visual health communications, qualitative interviews with professionals, and behaviour change and health communication literature was integrated with stakeholder involvement through a series of co-design workshops [25]. The GIFs were based around SCT, expected to increase intentions, self-efficacy, and outcome expectancies about physical distancing (hereafter referred to as “distancing”), handwashing, and mask-wearing. The four GIF designs and narratives were developed to be culturally relevant and sensitive to the Guatemalan population; they recognise high collectivism, focus on families or youths, and are centred within a rural (total = 2) or urban (total = 2) context (see Figure 1). Each participant was presented with three of the four GIFs. GIF selection was randomised automatically: Combination 1 (GIFs A, B, C), n = 80/308 (26%); Combination 2 (GIFs A, B, D), n = 75/308 (24%); Combination 3 (GIFs A, C, D), n = 82/308 (26%); Combination 4 (GIFs B, C, D), n = 71/308 (23%).
Figure 1.

The GIFs focussing on families or youths, centred either within a rural or urban context. GIF 1 Rural family; GIF 2 Rural youth; GIF 3 Urban family; GIF 4 Urban youth. Available at: https://www.youtube.com/channel/UCbeGGPYy1PDdb3xLHC_jTSw
Measures
Intentions, self-efficacy, and outcome expectancy beliefs about each of the COVID-19 preventive behaviours were probed using questions based upon previously used measures [8]. Intention was measured on a 5-point Likert scale (always, most times, sometimes, rarely, never; scale range 1-5), self-efficacy was measured on a 4-point Likert scale (very confident, fairly confident, not very confident, not at all confident; scale range = 1-4) and outcome expectancy was measured on a 4-point scale (strongly agree, tend to agree, tend to disagree, strongly disagree; scale range = 1-5). “Don’t know” and “Prefer not to say” were alternative available responses. No items were reverse coded; a lower score reflected a stronger intention and belief.
For distancing and handwashing behaviours, the following single items were used:
Intention – “How often do you intend to stay 1.5 metres away from other people, except those who live in your household, all or most of the time?” and “How often do you intend to wash your hands as soon as you get home?”;
Self-efficacy – “How confident are you that you can stay 1.5 metres away from other people, except those who live in your household, all or most of the time?” and “How confident are you that you can wash your hands as soon as you get home?”;
Outcome expectancy – “How much do you agree with the statement “I will reduce my chances of getting COVID-19” in relation to washing your hands as soon as you get home?” And “In relation to keeping a 1.5-metre distance from people outside of your household?”.
Single items for intentions and beliefs have been found to be psychometrically sound and favourable to multiple item measures reducing monotony and burden on participants [26,27].
For mask-wearing behaviour, intention, self-efficacy. and outcome expectancy were checked using the same question format but applied to four common behavioural settings:
Outside of your home;
On public transport;
In the street with friends or family;
When other people around you are NOT wearing a face mask correctly.
Cronbach’s reliability analyses confirmed acceptable reliability between mask-wearing sub-scores in each testing phase for each type of belief: intention α>0.697, self-efficacy α>0.771, and outcome expectancy α>0.801, in all cases. To this end, for each phase, sub-scores were averaged into single mean scores for analyses. Attitudes to the behaviours were also elicited but data are not reported here.
Procedure
The survey was drafted in English and then translated into Spanish and back-translated by research team members fluent in English and Spanish, including a language expert. The Guatemala-based team provided feedback on the clarity of questions and accuracy concerning government recommendations at that time. The survey was conducted using QualtricsXM and piloted in 10% of the target sample to ensure accuracy of data collection before continuing recruitment.
Participants first rated their engagement in preventive behaviours (distancing, handwashing, and mask-wearing) during the week preceding the study. Understanding of COVID-19 threat was probed along with knowledge of COVID-19 transmission risk from different situations (eg, not washing hands). Intentions, self-efficacy, and outcome expectancies in relation to distancing, handwashing, and mask-wearing, in that order, were assessed.
Participants were then presented with three GIFs sequentially. Using the QualtricsXM platform, the presented GIFs were randomly selected from a set of four (Figure 1) and their delivery order was randomised. GIF viewing was self-paced, and no time limit was placed on subsequent completion of the intention and belief measures. Following each GIF, participants completed the same intention and belief measures as they did at baseline. Post-GIF measurements were collected on three occasions. Further questions explored which GIF participants liked the most, liked the least, and narrative or emotive responses; these data are not reported here.
Analyses
A priori power calculation using G*Power (Version 3.1.9.7; 2020) yielded a sample size of 148 to detect within-subject, between-subject, and interaction effects, a medium effect size (f = 0.25), 0.05 probability of error and 0.90 power. Other analyses were performed using IBM SPSS (Version 26.0; IBM Corp, 2019; Armonk, NY). Response options “Don’t know” and “Prefer not to say” were treated as missing values and removed. There were 351 missing values, which accounted for 1.19% of all data points. Repeated measures (RM) ANOVAs with within-subject factor GIF exposure (baseline, GIF1, GIF2, GIF3) were performed to examine possible changes in responses to intention, self-efficacy, and outcome expectancy measures. As each participant was presented with three randomly selected GIFs of a possible four, GIF combination was included in all RMANOVAs as a between-subject factor. In all cases, reporting of RMANOVA outcomes include F (variation between sample means), df (degrees of freedom), P (probability), and ηp2 (partial eta squared effect size) values, eg, (F (3903) = 53.000, P < 0.001, ηp2 = 0.150). Planned pairwise comparisons examined possible differences in scores between testing phases, eg, baseline vs post-GIF1. Reporting of t test outcomes included a t (difference between means), df and P-values, eg, (t (303) = 0.232, P = 0.817). A Bonferroni-corrected alpha level of P = 0.008 (P = 0.05/6 pairwise tests) was applied to account for multiple comparisons. These corrections were applied to within-family pairwise comparisons, eg, for the “intention” measure of distancing or “outcome expectancy” measure of mask-wearing. Significant outcomes that survived Bonferroni correction are denoted in the results section through an asterisk, eg, “P = 0.003*”.
Ethical approval
This study was approved by Northumbria University Research Ethics Committee (Ref: 26593). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
RESULTS
Sample characteristics
A total of 308 adults (mean age = 29.69 years, SD = 9.11; range = 18-62; 58.4% male) participated in this study. Most participants identified as Latino (82.5%) with others identifying as Maya (10.7%), Garifuna (2.3%), and Xinca (1.0%). Spanish was the dominant mother language reported by 93.5% of participants. Participants reported living in their household with a mean of 3.16 adults aged ≥18 years (SD = 1.92; range = 0-15) and 1.27 children aged <18 years (SD = 1.38; range = 0-13). 138 participants (44.8%) reported being in full or part-time employment, 17.5% were self-employed, 13.6% were studying at school, college or university, and 23.1% were not employed (see Table 1 for sample data).
Table 1.
Sample characteristics
| Variable | Categories | n (%) | Variable | Categories | n (%) |
|---|---|---|---|---|---|
| Age |
18-24 y |
107 (34.7%) |
Employment status |
Full- or part-time |
138 (44.8%) |
|
|
25-34 y |
127 (41.2%) |
|
Self-employed |
54 (17.5%) |
|
|
35-44 y |
50 (16.2%) |
|
Unemployed |
56 (23.1%) |
|
|
45-54 y |
22 (7.1%) |
|
Studying |
42 (13.6%) |
|
|
55+ years |
4 (1.3%) |
|
Looking after the home |
10 (3.2%) |
|
|
|
|
|
Retired |
1 (0.3%) |
| Gender |
Male |
180 (58.4%) |
|
Not working due to disability or illness |
4 (1.3%) |
|
|
Female |
123 (39.9%) |
|
Prefer not to say |
3 (1.0%) |
|
|
Other |
1 (0.4%) |
|
|
|
|
|
Prefer not to say |
4 (1.3%) |
Adults in household |
0 |
24 (7.8%) |
|
|
|
|
|
1 |
19 (6.2% |
| Self-identified ethnicity |
Latino |
254 (82.5%) |
|
2 |
75 (24.4%) |
|
|
Maya |
33 (10.7%) |
|
3 |
61 (19.8%) |
|
|
Garifuna, |
7 (2.3%) |
|
4 |
65 (21.1%) |
|
|
Xinca |
3 (1.0%) |
|
5 |
33 (10.7%) |
|
|
Prefer not to say |
2 (0.6%) |
|
6 |
11 (3.6%) |
|
|
|
|
|
7 |
4 (1.3%) |
| Mother language |
Spanish |
288 (93.5%) |
|
8 |
5 (1.6%) |
|
|
Achi’ |
1 (0.3%) |
|
9 |
1 (0.3%) |
|
|
K’iche’ |
3 (1.0%) |
|
10+ |
1 (0.3%) |
|
|
Mam |
2 (0.6%) |
|
|
|
|
|
Poqomchi’ |
1 (0.3%) |
Children in household |
0 |
90 (29.2%) |
|
|
Q’eqchi’ |
1 (0.3%) |
|
1 |
98 (31.8%) |
|
|
Tz’utujil |
1 (0.3%) |
|
2 |
65 (21.1%) |
|
|
Garifuna |
3 (1.0%) |
|
3 |
24 (7.8%) |
|
|
Kaqchikel |
6 (1.9%) |
|
4 |
8 (2.6%) |
| Ixil | 1 (0.3%) | 5+ | 4 (1.2%) |
Pre-study self-reported performance of preventive behaviours
In the week preceding the study, 220 participants (71.4%) reported leaving their homes at least once. Among those, 45.9% reported always performing distancing, 85.0% handwashing and 90.9% mask-wearing (see Table 2).
Table 2.
Self-reported performance of preventive behaviours in the week preceding the study in the subset (n = 220) of participants who reported having left their home at least once
| How often did you engage in these behaviours in the past week? |
|||||||
|---|---|---|---|---|---|---|---|
|
Behaviour
|
Always
|
Most times
|
Sometimes
|
Rarely
|
Never
|
Prefer not to say
|
Total n of subset
|
| Stayed 1.5m away from people outside of home |
101 (45.9%) |
90 (40.9%) |
19 (8.6%) |
7 (3.2%) |
2 (0.9%) |
1 (0.5%) |
220 |
| Stayed 1.5m away from all people |
42 (19.1%) |
46 (20.9%) |
43 (19.5%) |
52 (23.6%) |
28 (12.7%) |
9 (4.1%) |
220 |
| Wore a mask correctly when outside of home |
200 (90.9%) |
14 (6.4%) |
4 (1.8%) |
1 (0.5%) |
0 (0.0%) |
1 (0.5%) |
220 |
| Washed your hands as soon as you got home | 187 (85.0%) | 19 (8.6%) | 11 (5.0%) | 2 (0.9%) | 0 (0.0%) | 1 (0.5%) | 220 |
Pre-study understanding of COVID-19 behavioural transmission risks
In relation to understanding the risks of COVID-19 transmission, participants felt that too much contact with others (76.9%), not washing hands enough (67.5%) and not wearing a mask correctly (80.8%) increased their risk to a great extent (see Table 3).
Table 3.
Pre-study understanding of risk of COVID-19 transmission by behaviours
| Would the behaviour increase your risk of contracting COVID-19? |
|||||||
|---|---|---|---|---|---|---|---|
|
Risk behaviour
|
To a great extent
|
To some extent
|
Hardly at all
|
Not at all
|
Don't know
|
Prefer not to say
|
Total n
|
| Too much contact with others |
237 |
58 |
7 |
3 |
3 |
0 |
308 |
| Not washing hands enough |
208 |
82 |
6 |
9 |
2 |
1 |
308 |
| Not wearing a mask correctly |
249 |
39 |
6 |
12 |
2 |
0 |
308 |
| A member of family brought it home |
113 |
56 |
13 |
116 |
8 |
2 |
308 |
| Others didn't keep distance when out of the home | 132 | 126 | 14 | 22 | 11 | 3 | 308 |
Effect of GIF exposure on intentions and beliefs in relation to preventive behaviours
Table 4 provides an overview of all RMANOVA main and interaction effects for the distancing, handwashing, and mask-wearing measures.
Table 4.
Overview of RMANOVA main and interaction effects for the three measures, distancing, handwashing, and mask-wearing†
| GIF exposure‡ | GIF combination | GIF exposure × Gif combination | |
|---|---|---|---|
|
Distancing
| |||
| Self-efficacy |
F (3903) = 53.000, P < 0.001* |
F (3301) = 0.841, P = 0.472 |
F (9903) = 1.628, P = 0.122 |
| Intention |
F (3897) = 39.752, P < 0.001*† |
F (3299) = 0.146, P = 0.932 |
F (9897) = 2.307, P = 0.026† |
| Outcome expectancy |
F (3900) = 16.907, P < 0.001*† |
F (3300) = 0.384, P = 0.764 |
F (9300) = 0.859, P = 0.542 |
|
Handwashing
| |||
| Self-efficacy |
F (3909) = 3.448, P = 0.025† |
F (3303) = 0.376, P = 0.771 |
F (9909) = 0.714, P = 0.664 |
| Intention |
F (3903) = 3.113, P = 0.026† |
F (3301) = 0.725, P = 0.538 |
F (9903) = 0.601, P = 0.750 |
| Outcome expectancy |
F (3906) = 6.050, P = 0.001*† |
F (3302) = 1.116, P = 0.343 |
F (9906) = 0.609, P = 0.748 |
|
Mask-wearing
| |||
| Self-efficacy |
F (3915) = 44.903, P < 0.001*† |
F (3305) = 0.520, P = 0.669 |
F (9915) = 1.019, P = 0.422 |
| Intention |
F (3915) = 7.726, P < 0.001*† |
F (3305) = 1.267, P = 0.286 |
F (9915) = 1.063, P = 0.388 |
| Outcome expectancy | F (3900) = 0.769, P = 0.508 | F (3300) = 0.306, P = 0.821 | F (9900) = 0.585, P = 0.805 |
*Significant findings that survived a Bonferroni-corrected P-value of 0.002 (P = 0.05/27 comparisons).
†Significant findings.
Distancing
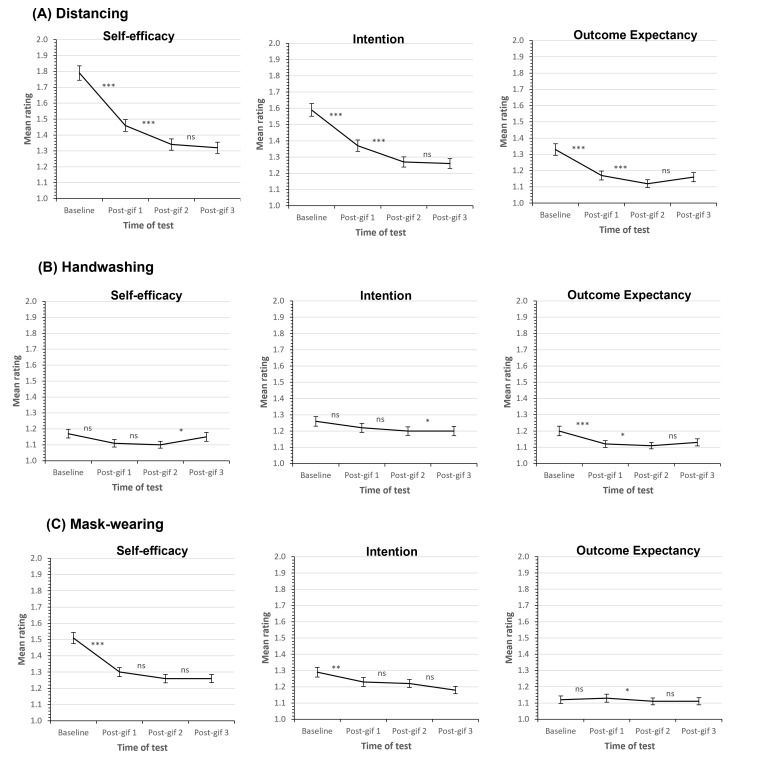
GIF exposure significantly improved participants’ self-efficacy (F (3903) = 53.000, P < 0.001, ηp2 = 0.150), intentions (F (3897) = 39.752, P < 0.001, ηp2 = 0.117), and outcome expectancy beliefs (F (3,900) = 16.907, P < 0.001, ηp2 = 0.053) (see Figure 2, panel A).
Figure 2.
Intentions and beliefs in relation to the behaviours. Line graphs show mean self-efficacy, intention, and outcome expectancy Likert scale ratings in the pre- and post-GIF exposure phases for (A) distancing, (B) handwashing and (C) mask-wearing. In all cases, lower ratings reflect stronger intentions and beliefs. Error bars show the standard error of the mean. Significance values from pairwise comparisons (baseline vs post-GIF1, post-GIF1 vs post-GIF2, and post-GIF2 vs post-GIF3) are shown, where ns = non-significant, * = P < 0.05, ** = P < 0.01, and *** = P < 0.001. Panel A. Distancing; Panel B. Handwashing; Panel C. Mask-wearing.
Handwashing
GIF exposure significantly improved participants’ self-efficacy (F (3909) = 3.448, P = 0.025, ηp2 = 0.011), intentions (F (3903) = 3.113, P = 0.026, ηp2 = 0.010), and outcome expectancy beliefs (F (3906) = 6.050, P = 0.001, ηp2 = 0.020) (see Figure 2, panel B).
Mask-wearing
GIF exposure significantly improved participants’ self-efficacy (F (3915) = 44.903, P < 0.001, ηp2 = 0.128), and intentions (F (3915) = 7.726, P < 0.001, ηp2 = 0.025). There was no significant effect of GIF exposure on outcome expectancy beliefs (F (3900) = 0.769, P = 0.508, ηp2 = 0.003) (see Figure 2, panel C).
Between subject and interaction effects
GIF combination did not significantly affect ratings of intentions or beliefs in relation to any of the three behaviours (all Ps >0.471 for distancing; all Ps >0.342 for handwashing; all Ps >0.285 for mask-wearing). In addition, no significant interactions between GIF exposure and GIF combination were identified for handwashing (all Ps >0.663) and mask-wearing (all Ps >0.387). We did observe a significant interaction for the distancing intention behaviour (P = 0.026) but this did not survive Bonferroni correction for multiple comparisons (see Table 4). Together, these findings indicate that the effects of GIF exposure are unlikely to be dependent on the combination of GIFs presented.
Post hoc comparisons: exposure-by-exposure changes in ratings
Figure 2 provides a visual overview of changes in ratings across the measures on an exposure-by-exposure basis, ie, from baseline to post-GIF1, post-GIF2 to post-GIF3 phases of our study procedure.
Distancing
Pairwise comparisons revealed that, relative to baseline, participants’ responses were significantly improved in the post-GIF1 (t (305) = 7.066, P < 0.001*), post-GIF2 (t (306) = 9.647, P < 0.001*) and post-GIF3 (t (305) = 8.981, P < 0.001*) phases for self-efficacy (see Figure 2, panel A, left); in the post-GIF1 (t (303) = 5.570, P < 0.001*), post-GIF2 (t (304) = 7.903, P < 0.001*) and post-GIF3 (t (303) = 7.747, P < 0.001*) phases for intention (see Figure 2, panel A, middle); and in the post-GIF1 (t (305) = 5.047, P < 0.001*), post-GIF2 (t (306) = 5.916, P < 0.001*) and post-GIF3 (t (304) = 4.266, P < 0.001*) phases for outcome expectancy (see Figure 2, panel A, right).
Self-efficacy and intention improved significantly from the post-GIF1 to the post-GIF2 phase (self-efficacy: t (306) = 3.752, P < 0.001*; intention: t (306) = 3.838, P < 0.001*), but there was no significant change in ratings between the post-GIF2 and post-GIF3 testing points (self-efficacy: t (307) = 0.588, P = 0.557; intention: t (305) = 0.262, P = 0.793). Improvement from the post-GIF1 and post-GIF3 phases was significant (self-efficacy: t (304) = 3.927, P < 0.001*; intention: t (304) = 3.927, P < 0.001*). In terms of outcome expectancy, there was no significant change in scores from the post-GIF1 to post-GIF2 phases (t (306) = 1.814, P = 0.071) or post-GIF2 to post-GIF3 phases (t (304) = -1.503, P = 0.134), nor was there a significant difference between post-GIF1 and post-GIF3 ratings (t (303) = 0.232, P = 0.817).
Handwashing
Pairwise comparisons of intention scores revealed no significant difference between baseline, post-GIF1 (t (305) = 1.727, P = 0.085) and post-GIF3 (t (305) = 01.897, P = 0.059) scores (see Figure 2, panel B, middle). There were also no differences between post-GIF1 and post-GIF2 (t (306) = 1.301, P = 0.194) or post-GIF1 and post-GIF3 (t (304) = -1.589, P = 0.113). There was a significant improvement in intention from baseline to post-GIF2 phase (t (306) = 2.482, P = 0.014) and worsening between post-GIF2 and post-GIF3 phases (t (305) = -2.445, P = 0.015).
Pairwise comparisons of outcome expectancy scores revealed that, relative to baseline, ratings significantly improved in the post-GIF1 (t (306) = 3.006, P = 0.003*), post-GIF2 (t (307) = 3.360, P = 0.001*) and post-GIF3 (t (306) = 2.449, P = 0.015) phases (see Figure 2, panel B, right). There was no significant improvement in outcome expectancy from post-GIF1 to post-GIF2 phase (t (306) = 0.648, P = 0.517) or post-GIF2 to post-GIF3 phase (t (306) = -1.301, P = 0.194), nor was there a difference in outcome expectancy between post-GIF1 and post-GIF3 phases (t (305) = -0.324, P = 0.746).
Pairwise comparisons of self-efficacy scores revealed that, relative to baseline, self-efficacy significantly improved in post-GIF1 (t (307) = 2.230, P = 0.026) and post-GIF2 (t (308) = 2.812, P = 0.005*) phases (see Figure 2, panel B, left). Self-efficacy did not change from post-GIF1 to post-GIF2 phases (t (307) = 0.185, P = 0.853) and there was a significant worsening between post-GIF1 and post-GIF3 phases (t (306) = -2.031, P = 0.043), and post-GIF2 and post-GIF3 phases (t (307) = 2.421, P = 0.016). Additionally, there was no overall difference between baseline and post-GIF3 data (t (307) = 0.632, P = 0.528).
Mask-wearing
Pairwise comparisons of self-efficacy scores revealed a significant improvement in self-efficacy from baseline to post-GIF1 (t (308) = 7.775, P < 0.001*), post-GIF2 (t (308) = 8.177, P < 0.001*) and post-GIF3 (t (308) = 8.168, P < 0.001*) phases (see Figure 2, panel C, left). There was no difference in self-efficacy between post-GIF1 and post-GIF2 phases (t (308) = 1.878, P = 0.061), post-GIF1 and post-GIF3 phases (t (308) = 1.802, P = 0.073), or post-GIF2 and post-GIF3 phases (t (308) = -0.275, P = 0.783).
Pairwise comparisons of intention scores revealed the cause of the main effect of exposure was the significant improvement in intention from baseline to post-GIF1 (t (308) = 2.788, P = 0.006*), post-GIF2 (t (308) = 2.853, P = 0.005*) and post-GIF3 (t (308) = 4.351, P < 0.001*) phases (see Figure 2, panel C, middle). There was no difference in intention between the post-GIF1 and post-GIF2 phases (t (308) = 0.349, P = 0.727) or post-GIF2 and post-GIF3 (t (308) = 1.704, P = 0.089), but we did observe a significant difference between the post-GIF1 and post-GIF3 phases (t (308) = 2.070, P = 0.039).
Pairwise comparisons of outcome expectancy scores revealed no significant difference in scores between baseline and post-GIF1 (t (305) = -0.316, P = 0.752), post-GIF2 (t (305) = 0.949, P = 0.344), or post-GIF3 (t (305) = 0.780, P = 0.436) phases (see Figure 2, panel C, right). There were also no differences between post-GIF1 and post-GIF2 phases (t (304) = 1.266, P = 0.206), post-GIF2 and post-GIF3 phases (t (304) = 1.258, P = 0.209), and post-GIF2 and post-GIF3 phases (t (304) = -0.174, P = 0.862).
DISCUSSION
Many GIFs related to the health, political and social aspects of COVID-19 have been circulating on social media as a communication device. However, despite public health agencies having used this medium to disseminate preventive messages about various health issues ranging from antibiotic resistance to heart disease and mosquito-borne diseases, GIF messaging to promote COVID-19 preventive behaviours has been surprisingly underutilized, and an evaluation of its effectiveness in shifting cognitive beliefs around these behaviours correspondingly scant. Our study sought to address these gaps in public health communication intervention design and evaluation. We found that GIFs were associated with an increase in intentions, self-efficacy, and outcome expectancy beliefs around three COVID-19 preventive behaviours – distancing, handwashing, and mask-wearing. In this section, we discuss these findings in the context of regulation surrounding these behaviours in Guatemala, reflect on study limitations, and present implications of public health communication policy and practice.
Of the three preventive behaviours, exposure to the GIFs had the most pronounced effect on distancing. This finding needs to be considered in the context of the shifts in policies surrounding distancing; the Guatemalan government published a decree called a ‘State of Calamity’ in March 2020 [28] which legally enforced preventive behaviours, including distancing of 1.5 m in public places [29]. This decree was withdrawn in September 2020 [30] to allow businesses to reopen and it remained withdrawn during the study period (February-March 2021) when the public were ‘urged’ to practice distancing [31]). Our finding can possibly be explained by the low baseline levels of self-efficacy around distancing, given the challenges of practising it in the face of overcrowding and the economic hardships it imposed [28]. Consequently, it appears that study respondents were reconciling the need for practising distancing to prevent COVID-19 transmission with its potential downsides. Similar barriers to practising distancing including social responsibilities, lack of trust in the government, and stress due to isolation have been observed elsewhere [32]. Ensuring public adherence to distancing is a complex socio-behavioural intervention that requires strategic messaging and structural reconfiguration of social spaces [33]. This complexity is reflected in low self-efficacy among the public and opens the need for communication interventions that visually demonstrate behaviours, providing vicarious learning opportunities as set out in SCT [14].
At the time of data collection, the Guatemalan public were required to wear face masks in public places [31]. This requirement, coupled with baseline data indicating that 91% of participants reported consistent mask-wearing in the week preceding the study and 81% strongly felt that not wearing a mask correctly would increase transmission risk, suggest that respondents might have habituated to the behaviour. Consequently, we observed relatively higher levels of self-efficacy and a potential ceiling effect for outcome expectancies with minimal room for increase through further communication interventions.
We observed similar trends in relation to handwashing, with a potential ceiling effect for self-efficacy. Handwashing is more commonplace than mask-wearing and respondents are likely to have had frequent mastery experiences. In situations where baseline beliefs are high, messages like those used in this study may serve to reinforce beliefs and strengthen intentions.
While the combinations in which GIFs were presented bore minimal impact, what commands our attention is the dosage of GIF exposure. Across the three behaviours, where improvements were observed, they were most pronounced from baseline to early exposures, after which they plateaued. In some cases, such as those of self-efficacy for handwashing and outcome expectancy for handwashing and distancing, we observed slightly (statistically insignificant) counter-productive outcomes suggesting that calibrating the dosage of communication might be a critical consideration for health communication. User fatigue, which can explain discontinued social media use [34], can be considered as important to this end.
These findings must be considered against three main limitations of our study. One, a cross-sectional study design offers useful insights at one point in time, but beliefs around such behaviours may shift over time as part of their ‘natural history’ or in response to the state of the pandemic and current government guidance. Two, we collected data on immediate effects of GIF exposure and therefore cannot comment on the durability or resilience of effects. Three, we report effects in terms of associations between GIF exposure and theoretical and evidence-based determinants of preventive behaviours; therefore, more research is needed to identify associations with adherence to the behaviours.
CONCLUSION
Our study offers three new insights for public health communication researchers and practitioners. First, languageless GIFs offer public health agencies a valuable and potentially cost-effective multimedia tool to widely disseminate messages via social media in multilingual countries during health crises such as COVID-19; their contribution to global “vaccines-plus” action [35] to communicate vaccination and preventive public health measures for COVID-19 should be recognised and welcomed. Second, the effectiveness of GIF interventions may be affected by prevailing levels of health beliefs, which suggests that understanding public sentiment prior to their design and dissemination might be important. Third, while the seeming ease of scaling GIF interventions might tempt an “all-out” approach in terms of quantity, more might not necessarily be better. Specifically, it is important to strategically calibrate the dosage in which GIFs are delivered, bearing in mind that their ability to play in a ‘looping repetition’ [19] can reinforce messages, using approaches from simple awareness to satire and humour. Finally, we recommend that health and risk communication researchers and practitioners adapt our evaluation – preferably through more scaled-up, representative designs – in different countries, to examine how local restrictions and cultural variables might mediate the associations between GIF exposure and behavioural intentions and beliefs.
Acknowledgements
The authors would like to thank Lottie Kingslake for contributing animation expertise, Margarita Lara for providing language interpretation, Angela Long for cleaning and preparing the dataset, and survey participants.
Footnotes
Funding: This study was supported by funding from Northumbria University QR Global Challenges Research Fund strategy. The funders had no role in study design, data collection, data analysis, data interpretation or writing of the report.
Authorship contributions: NO, SV, EL and LFNO conceived the study. NO, SV, EL, SMAJ, XGBM, RdC, EANG and LFNO designed the study and data collection. MC conducted the statistical analysis. NO wrote the first full draft of the article. All authors critically reviewed the article and approved the final draft. All authors confirm that they had full access to all the data in the study and accept responsibility to submit for publication.
Competing interests: The authors completed the ICMJE Unified Competing Interest Form (available upon request from the corresponding author) and declare no conflicts of interest.
REFERENCES
- 1.Bavel JJV, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4:460-71. 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- 2.West R, Michie S, Rubin GJ, Amlôt R.Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat Hum Behav. 2020;4:451-9. 10.1038/s41562-020-0887-9 [DOI] [PubMed] [Google Scholar]
- 3.Arlinghaus KR, Johnston CA.Advocating for behavior change with education. Am J Lifestyle Med. 2017;12:113-6. 10.1177/1559827617745479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly MP, Barker M.Why is changing health-related behaviour so difficult? Public Health. 2016;136:109-16. 10.1016/j.puhe.2016.03.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hagger MS, Smith SR, Keech JJ, Moyers SA, Hamilton K.Predicting social distancing intention and behavior during the COVID-19 pandemic: an integrated social cognition model. Ann Behav Med. 2020;54:713-27. 10.1093/abm/kaaa073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamilton K, Smith SR, Keech JJ, Moyers SA, Hagger MS.Application of the Health Action Process Approach to social distancing behavior during COVID-19. Appl Psychol Health Well-Being. 2020;12:1244-69. 10.1111/aphw.12231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayre J, Cvejic E, McCaffery K, Copp T, Cornell S, Dodd RH, et al. Contextualising COVID-19 prevention behaviour over time in Australia: patterns and long-term predictors from April to July 2020 in an online social media sample. PLoS One. 2021;16:e0253930. 10.1371/journal.pone.0253930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dixon D, Den Daas C, Hubbard G, Johnston M.Using behavioural theory to understand adherence to behaviours that reduce transmission of COVID-19; evidence from the CHARIS representative national study. Br J Health Psychol. 2022;27:116-35. 10.31234/osf.io/r3xn5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang CQ, Chung PK, Liu JD, Chan DKC, Hagger MS, Hamilton K.Health beliefs of wearing facemasks for Influenza A/H1N1 prevention: a qualitative investigation of Hong Kong older adults. Asia Pac J Public Health. 2019;31:246-56. 10.1177/1010539519844082 [DOI] [PubMed] [Google Scholar]
- 10.Dwipayanti NMU, Lubis DS, Harjana NPA.Public perception and hand hygiene behavior during COVID-19 pandemic in Indonesia. Front Public Health. 2021;9:621800. 10.3389/fpubh.2021.621800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seimetz E, Boyayo A-M, Mosler H-J.The influence of contextual and psychosocial factors on handwashing. Am J Trop Med Hyg. 2016;94:1407-17. 10.4269/ajtmh.15-0657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moorman C, Matulich E.A model of consumers’ preventive health behaviors: the role of health motivation and health ability. J Consum Res. 1993;20:208-28. 10.1086/209344 [DOI] [Google Scholar]
- 13.Bandura A.Social Cognitive Theory: an agentic perspective. Annu Rev Psychol. 2001;52:1-26. 10.1146/annurev.psych.52.1.1 [DOI] [PubMed] [Google Scholar]
- 14.Reesor L, Vaughan EM, Hernandez DC, Johnston CA.Addressing outcomes expectancies in behavior change. Am J Lifestyle Med. 2017;11:430-2. 10.1177/1559827617722504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mortada E, Abdel-Azeem A, Al Showair A, Zalat MM.Preventive behaviors towards Covid-19 pandemic among healthcare providers in Saudi Arabia using the Protection Motivation Theory. Risk Manag Healthc Policy. 2021;14:685-94. 10.2147/RMHP.S289837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berg MB, Lin L.Prevalence and predictors of early COVID-19 behavioral intentions in the United States. Transl Behav Med. 2020;10:843-9. 10.1093/tbm/ibaa085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ajzen I.The theory of planned behavior: frequently asked questions. Hum Behav Emerg Technol. 2020;2:314-24. 10.1002/hbe2.195 [DOI] [Google Scholar]
- 18.Houts PS, Doak CC, Doak LG, Loscalzo MJ.The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61:173-90. 10.1016/j.pec.2005.05.004 [DOI] [PubMed] [Google Scholar]
- 19.Miltner KM, Highfield T.Never Gonna GIF You Up: Analyzing the cultural significance of the animated GIF. Soc Media Soc. 2017;3:2056305117725223. 10.1177/2056305117725223 [DOI] [Google Scholar]
- 20.Adam M, Bärnighausen T, McMahon SA.Design for extreme scalability: A wordless, globally scalable COVID-19 prevention animation for rapid public health communication. J Glob Health. 2020;10:010343. 10.7189/jogh.10.010343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vandormael A, Adam M, Greuel M, Gates J, Favaretti C, Hachaturyan V, et al. The effect of a wordless, animated, social media video intervention on COVID-19 prevention: online randomized controlled trial. JMIR Public Health Surveill. 2021;7:e29060. 10.2196/29060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Institute for Health Metrics and Evaluation Guatemala. Available from: http://www.healthdata.org/guatemala. Accessed: 11 November 2021.
- 23.Avila C, Bright R, Gutierrez JC, Hoadley K, Manuel C, Romero N, et al. Guatemala Health System Assessment 2015. Bethesda, MD: 2015. Available from: https://www.hfgproject.org/guatemala-health-system-assessment-2015/. Accessed: 11 November 2021.
- 24.John Hopkins University of Medicine Coronavirus Resource Center Guatemala. Available from: https://coronavirus.jhu.edu/region/guatemala. Accessed: 08 January 2022.
- 25.O’Brien N, Land E, Vijaykumar S, De la Cruz R, Najera E, Bedoya X, et al. Languageless animated gifs to communicate COVID-19 preventive behaviours to adults in guatemala: development and evaluation of efficacy. Int J Behav Med. 2021;28:S11-2. [Google Scholar]
- 26.Hoeppner BB, Kelly JF, Urbanoski KA, Slaymaker V.Comparative utility of a single-item versus multiple-item measure of self-efficacy in predicting relapse among young adults. J Subst Abuse Treat. 2011;41:305-12. 10.1016/j.jsat.2011.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fishman J, Lushin V, Mandell DS.Predicting implementation: comparing validated measures of intention and assessing the role of motivation when designing behavioral interventions. Implement Sci Commun. 2020;1:81. 10.1186/s43058-020-00050-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vargas EN. Guatemala and the Covid 19 crisis: management balance and lessons for the future. Hanns Seidel Stiftung, 2020. Available from: https://www.hss.de/download/publications/Quo_vadis_Latin_America_neu.pdf. Accessed: 17 October 2021.
- 29.Garda World. Guatemala: Authorities renew COVID-19 restrictions until August 23 /update 18. 2020. Available from: https://www.garda.com/crisis24/news-alerts/359881/guatemala-authorities-renew-covid-19-restrictions-from-july-12-update-17. Accessed: 17 October 2021.
- 30.International Monetary Fund. Policy responses to Covid-19: Guatemala. 2021. Available from: https://www.imf.org/en/Topics/imf-and-covid19/Policy-Responses-to-COVID-19#G. Accessed: 17 October 2021.
- 31.Garda World. Guatemala: COVID-19 restrictions remain largely unchanged as of Feb. 26, though entry requirements have been revised /update 28. 2021. Available: https://www.garda.com/crisis24/news-alerts/448351/guatemala-covid-19-restrictions-remain-largely-unchanged-as-of-feb-26-though-entry-requirements-have-been-revised-update-28. Accessed: 17 October 2021.
- 32.Coroiu A, Moran C, Campbell T, Geller AC.Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLoS One. 2020;15:e0239795. 10.1371/journal.pone.0239795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bonell C, Michie S, Reicher S, West R, Bear L, Yardley L, et al. Harnessing behavioural science in public health campaigns to maintain ‘social distancing’ in response to the COVID-19 pandemic: key principles. J Epidemiol Community Health. 2020;74:617-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maier C, Laumer S, Weinert C, Weitzel T.The effects of technostress and switching stress on discontinued use of social networking services: a study of Facebook use. Inf Syst J. 2015;25:275-308. 10.1111/isj.12068 [DOI] [Google Scholar]
- 35.An open letter by a group of public health experts, clinicians, scientists. Covid-19: An urgent call for global “vaccines-plus” action. BMJ. 2022;376:o1. [DOI] [PubMed] [Google Scholar]