Abstract
Objective
This study aims to explore health beliefs toward lung cancer screening with low dose computed tomography among Chinese American high-risk smokers.
Methods
Guided by the Health Belief Model, semi-structured individual interviews were conducted with Chinese American high-risk smokers via phone. Additional questionnaires on demographic information, history of smoking and lung cancer screening were collected via email or phone before the interview, depending on participants’ preference. Content analysis was used to extract meaningful and significant themes in the dataset. Constant comparison analysis and process coding were used to categorize and code data.
Results
Data saturation was reached after interviewing 12 participants. Chinese American high-risk smokers perceived a low susceptibility to lung cancer, since they believed various protective factors of lung cancer (e.g., doing exercise, healthy diet, etc.) reduced their risk of getting lung cancer. All the participants perceived a high severity of lung cancer. They acknowledged lung cancer would have a huge impact on their life. Perceived benefits of lung cancer screening were accurate in most aspects although minor confusions were still noticed among this population. Perceived barriers varied on participants’, physicians’, and institutional levels. High-risk Chinese American smokers had little confidence to screening for lung cancer. Cues to action for them to screening for lung cancer included recommendations from health care providers, support from family members and friends, and information shared on Chinese-based social media.
Conclusions
Misconceptions and barriers to screening for lung cancer existed widely among Chinese American high-risk smokers. Intervention programs and targeted health education should be implemented to promote lung cancer screening among this population.
Keywords: Asian Americans, Early detection of cancer, Health belief model, Lung neoplasms, Smokers
What is known
-
•
Screening for individuals at high risk for lung cancer has the potential to improve lung cancer survival by finding the disease at an earlier stage when it is more likely to be curable through surgical intervention and other therapeutic treatments.
-
•
Health beliefs about lung cancer screening were significantly associated with the uptake of lung cancer screening.
-
•
Although previous studies provided some information on Chinese Americans’ health belief toward other types of cancer screening, however, data on the health beliefs of cancer screening is limited.
What is new
-
•
Chinese American high-risk smokers perceived a low susceptibility to lung cancer, since they believed various protective factors of lung cancer (e.g., doing exercise, healthy diet, etc.) reduced their risk of getting lung cancer. All the participants perceived a high severity of lung cancer.
-
•
They acknowledged lung cancer would have a huge impact on their life.
-
•
Perceived benefits of lung cancer screening were accurate in most aspects although minor confusions were still noticed among this population.
-
•
Perceived barriers varied on participants’, physicians’, and institutional levels.
-
•
High-risk Chinese American smokers had little confidence to screening for lung cancer.
-
•
Cues to action for them to screen for lung cancer included recommendations from health care providers, support from family members and friends, and information shared on Chinese-based social media.
1. Introduction
1.1. Background
1.1.1. Lung cancer and lung cancer screening
Lung cancer is the leading cause of cancer deaths in Chinese Americans [1]. Among all Asian American subgroups, Chinese Americans have the highest mortality rate of lung cancer [2]. As the second and fourth most common cancer among U.S. Chinese men and women, respectively, lung cancer accounted for approximately 30% of all cancer-related deaths in Chinese Americans [1].
Lung cancer screening with low dose computed tomography (CT) is an effective secondary prevention method for lung cancer [3]. Screening for individuals at high risk for lung cancer has the potential to improve lung cancer survival by finding the disease at an earlier stage when it is more likely to be curable through surgical intervention and other therapeutic treatments. Lung cancer screening with low dose CT has been proved to reduce the mortality rate of lung cancer by 20%, compared to the standard chest X-ray, among current or former smokers who had smoked at least 30 pack-year (smoked one pack of cigarettes per day for 30 years) or had quit smoking within the past 15 years [3,4]. Since 2013, the United States Preventive Services Task Force (USPSTF) and other organizations have issued guidelines for the early detection of lung cancer with yearly low dose CT among the high-risk population [5]. Screening for lung cancer with low dose CT was covered both by the private and public health insurances for the high-risk population (adults aged 50–80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years) [6].
1.1.2. Uptake rate of lung cancer screening
Although the supportive landscape has changed, uptake rates of lung cancer screening with low dose CT remain low after the USPSTF guideline was published [7,8]. The percentage of the eligible population who had received lung cancer screening with low dose CT just increased from 3.3% in 2010 to 3.9% in 2015 among the U.S. population [9]. Reports about the uptake rates of lung cancer screening among minority populations were lacking. Although the uptake rate of lung cancer screening with low dose CT among Chinese Americans was not reported in the literature, a recent study showed that 22% of the elderly Chinese men in Chicago met the eligibility criteria of the USPSTF low dose CT screening [10].
1.1.3. Health beliefs and behaviors of lung cancer screening
Previous studies indicated that health beliefs of lung cancer screening were significantly associated with the uptake of lung cancer screening. Reports showed people who were significantly more likely to have a low dose CT screening had several common health beliefs toward lung cancer screening [11]. In a cross-sectional survey study among 338 older smokers (aged older than 55 years) with a smoking history of more than 30 pack-year, the results showed the participants were more likely to say they would get screened if they perceived high risk for lung cancer, were not afraid of CT scans, believed low dose CT screening results were accurate and detecting lung cancer earlier would more likely improve lung cancer prognosis [11]. Several other studies also indicated that cultural factors such as beliefs and attitudes about lung cancer screening process or illness, knowledge, mistrust of the healthcare system, and fatalistic beliefs were related to high-risk population’s participation in lung cancer screening programs [[12], [13], [14], [15], [16]], especially among minorities (e.g., Blacks and Hispanics) [17].
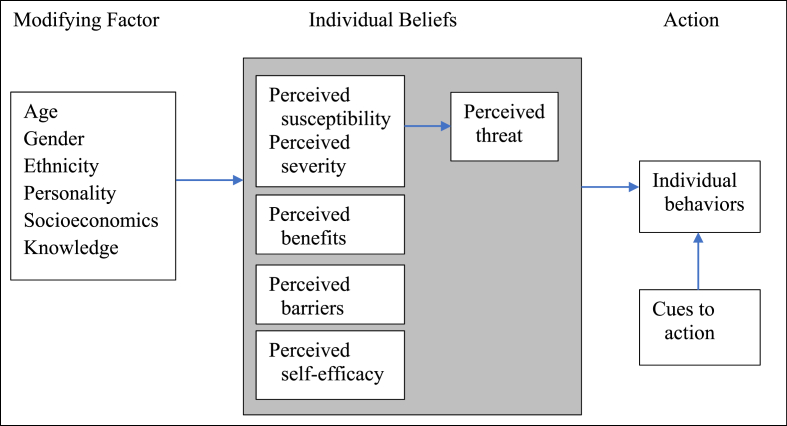
1.1.4. Health Belief Model
Instead of building a grounded theory in this study, we used an epistemological paradigm that guided the study [18]. Being consistent with the theory model used by the Lung Cancer Screening Health Belief Scale, the interview questions in this study were developed based on the Health Belief Model (Fig. 1). The Health Belief Model is a social cognition model focusing on health behavior change [19]. It originated from psychological science [20], and was developed in the 1950s by Rosenstock, Hochbaum, Kegeles, and Leventhal, four social psychologists at the United States Public Health Service Organization [21]. Amendments to the model were made in the late 1980s to incorporate emerging evidence about the role of self-efficacy in decision-making and health behavior [22].
Fig. 1.
Health belief model.
The key concepts of Health Belief Model are perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and cues to action [22]. 1) Perceived susceptibility is individuals’ subjective beliefs on the risk of getting a disease [22], which refers to how strongly people believe that they are susceptible to the disease [22]. 2) Perceived severity is a personal evaluation of the seriousness of the consequences related to a disease, which refers to individuals’ perception on whether the disease will have serious effects on their lives if they contract it [22]. 3) Perceived benefit is people’ s assessment of the value to take the advised action to reduce risks or seriousness of diseases [22]. 4) Perceived barriers are people’s belief about the negatively valued aspects of taking actions, which are the obstacles to the behavior change [22]. 5) Self-efficacy refers to individuals’ own confidence in their personal ability to successfully take action to achieve outcomes by responding to unfamiliar or difficult situations and dealing with any associated setbacks or obstacles [22]. 6) Cues to action refers to the strategies used to activate one’s readiness to take action [22].
1.1.5. Health Belief Model and screening behaviors among Chinese Americans
The Health Belief Model has been used in several studies among Chinese American populations to explore their screening behaviors. One quantitative study based on the Health Belief Model conducted with 125 Asian American women in southeastern Michigan showed that Chinese women were five times more likely than others to identify “do not need a mammogram if I feel ok” and “waiting time is too long” as perceived barriers for screening mammogram (OR = 5.450, 95% CI = 1.643, 18.081, and OR = 5.070, 95% CI = 1.674, 15.351, respectively), controlling for income [23]. Another qualitative study conducted in 14 in-depth interviews and 4 focus groups with 39 low-income Chinese immigrants in New York City showed a strong influence of Chinese culture on Chinese immigrants’ health beliefs toward breast, cervical, and prostate cancer, and their cancer screening behaviors. Based on the Health Belief Model, common misconceptions about the causes of cancer included: excessive sexual activities, having a certain blood type, cancer being “contagious”, and women ignoring their reproductive or natural functions by using birth control or not breastfeeding [24].
1.2. Knowledge gap
Although previous studies provided some information on Chinese Americans’ beliefs and attitudes toward other types of cancer screening, however, data on the health beliefs of cancer screening is limited. In addition, up to date, to our knowledge, no study has explored Chinese American high-risk smokers’ health beliefs toward lung cancer screening with low dose CT. When information is limited for us to understand certain populations’ health beliefs toward certain phenomena or behavior, qualitative research is necessary to be conducted to facilitate our understating of the phenomenon or behavior [25]. Given a high mortality rate and a low screening rate of lung cancer among the Chinese American population, exploring their health beliefs regarding their utilization of screening is necessary. By filling this gap, a better understanding toward Chinese American high-risk smokers’ health beliefs about lung cancer screening could be reached.
1.3. Aim and significance of the study
This study was included in a mixed-method research project. The research project aims to cross-culturally adapt and validate the Lung Cancer Screening Health Belief Scale to be used in Chinese Americans. It included the instrument translation, modification, and validation processes, in which both qualitative interview and quantitative survey were used.
The purpose of this study was to explore health beliefs toward lung cancer screening with low dose CT among Chinese American high-risk smokers. Findings from this study can help the researchers culturally adapt the Lung Cancer Screening Health Belief Scale to be used in Chinese Americans. It can also help health care providers get more insight into Chinese Americans’ health behaviors regarding lung cancer screening. By knowing Chinese Americans’ health beliefs toward lung cancer screening, culturally tailored intervention programs could be designed to help to increase the uptake rate of lung cancer screening among Chinese Americans.
2. Martial and methods
2.1. Design and ethical consideration
This qualitative study was guided by the semi-structured interview guide which was developed based on the Health Belief Model. In-depth individual phone interviews were conducted with the participants and recorded by digital recorder. This study was approved by the university Institution of Research Board (IRB) (IRB#19-001464). Due to the minor risk of the study design, written informed consent was waived by the university IRB. However, the study information sheet was distributed to the participants via email or phone to inform their rights in the study. In addition, participants’ privacy and confidentiality were strictly protected in the study by following the research ethical rules enacted by the university IRB. Each participant was assigned a study number to protect their personal information from accidental disclosure, and no information was identifiable.
2.2. Setting, inclusion and exclusion criteria
The inclusion criteria for the participants to be included in this study were: 1) Aged 50–80 years old, 2) residing in the United States and self-identified as descendants of Chinese, 3) current smokers or quit smoking in the past 15 years, with a smoking history over 20 package-year, 4) can speak Cantonese or Mandarin, and 5) can read Chinese at the 6th-grade level. The inclusion criteria for this study were consistent with the inclusion criteria of lung cancer screening recommendations by USPSTF [26]. The exclusion criterion for the participants was having been diagnosed with lung cancer. The sample size of this study was determined by data saturation toward the study aim.
2.3. Recruitment and data collection
Data in this study were collected from March 2021 to January 2022. Participants in this study were recruited using the purposive and snowball sampling methods. To ensure sample diversity, we used different methods to recruit participants. English and Chinese version flyers including information on the purpose of the study, inclusion and exclusion criteria, and the primary investigator’s contact information were posted on a popular website (https://www.chineseinla.com) and WeChat friend groups among Chinese Americans. After the participants contacted the primary investigator, they were screened for eligibility to participate in the study via phone, and a follow-up formal interview was scheduled with the participants. Before the interviews, a questionnaire package was sent to the participants to fill out. Some participants were not able to fill out the questionnaires by themselves. Following their requests, the questions were asked, and the questionnaires were filled out item by item in the individual interviews by the primary investigator. The individual interviews were conducted in Chinese by the primary investigator, recorded by the digital recorder, translated to English, and stored in a passworded encrypted laptop. Pilot interviews were conducted with the participants to clarify any misconceptions regarding the interview questions. Also, during the interviews, all raised confusions were answered by the interviewer. For reimbursing the participants’ time and effort in this study, a 25-dollar and 5-dollar amazon gift card was sent to the participants and referrals, respectively, through email after the interviews were completed.
2.4. Instruments
The semi-structured interview guide (Table 1) included questions asking about participants’ health beliefs toward lung cancer screening. Further, a questionnaire was developed to collect 1) the demographic information, including questions asking about participants’ age, gender, marital status, number of children, education level, income, insurance status, religious status, age when moved to the US, residence years in the US, occupation, and language or dialect; and 2) the smoking and lung cancer screening history, including participants’ smoking amount, frequency, length, intention and confidence to quitting smoking/screening for lung cancer, family history of lung cancer, and lung cancer screening history.
Table 1.
Semi-structured interview guide.
| Categories | Interview Questions | ||
|---|---|---|---|
| Entry question |
|
||
| Perceived susceptibility |
|
||
| Perceived severity |
|
||
| PROBE: | (If yes) How does that impact their life? What if it happened in your case? (If no) What impact do you think it will be on a person's life, if he/she diagnosed with lung cancer? Why do you think like that? |
||
| Perceived benefits |
|
||
| PROBE: | (If yes) How do you/they benefit from screening lung cancer? (If no) What benefits do you think a smoker can get from screening lung cancer? Why do you think like this? |
||
| Perceived barriers |
|
||
| PROBE: | (If yes) Tell me more about the difficulties that you/they encountered or what you think could be improved in the screening processes. (If no) What could be reasons for you not having a lung cancer screening? What help do you think is necessary for you to obtain lung cancer screening? |
||
| |||
| Self-efficacy |
|
||
| PROBE: | (If yes) Tell me more about the places and procedures for screening lung cancer. (If no) What could be done to make that information more accessible to smokers like you? |
||
| |||
| PROBE: | (If yes) Tell me more about the processes to schedule the appointment. (If no) What could be done by you or health care providers to make it feasible? |
||
| |||
| PROBE: | (If yes) Tell me more about your interpretation of the screening results. (If no) What could be improved to make it feasible? |
||
| Cues to action |
|
||
| PROBE: | (If yes) Where did you get the information? How do you feel when you got that information? (If no) Who do you want to get the information from? What do you like to know most? |
||
| |||
| Ending Question |
|
||
All the instruments used in this study were developed based on the literature search and back-and-forth discussions among the authors of this study. The instruments were developed in English initially, reviewed by all authors of this study, further revised, and translated to Chinese by the primary investigator. The translated Chinese version of the instruments was reviewed and revised again, which aims to achieve cultural clarity and make the instruments easy understandable.
2.5. Data analysis
Data collected in this study were analyzed using the content analysis method [27]. Constant comparison analysis was conducted to extract emerging subthemes and main themes in the content. Four coding phases including initial, focused, axial, and theoretical coding were conducted through constant comparison of the content. In the initial coding phase, line by line coding was done manually using the process coding method [28]. Then a cross-transcription comparison was conducted in the focused coding phase to identify the most frequent and significant codes. The codes were linked to subcategories, properties and dimensions in the axial coding phase, and the main categories for themes were identified in the final theoretical coding phase [29]. The SRQR reporting guideline was followed to report findings from this study [30].
2.6. Trustworthiness
To ensure the credibility, dependability, transferability, and confirmability of the results, we used several methods to increase the trustworthiness of the study. The data analysis was done by the primary investigator and reviewed by the last author of this study. Subthemes that emerged from the data analysis were further reviewed and verified by other authors of this study to ensure the consistency of the findings. Also, the results of the study were reviewed by the participants to member-check the findings. The subthemes which caused confusion and misunderstanding were revised upon participants’ checking. Furthermore, audit trail and reflexivity techniques were used during the data analysis process by tracking the interview and data analysis notes and memos.
3. Results
3.1. Participants’ characteristics
After interviewing 12 participants, data reached “theoretical saturation” for the study purpose. No new information emerged regarding the main themes extracted from the interviews. For the 12 individual interviews with participants, each interview time ranged from 30 to 60 min, with a mean interview time of 48 min. In the sample, gender disparity of the high-risk Chinese American smokers was reflected, which included one female and 11 males in the study. Ten of them speak Mandarin, with at least one speaking another dialect. Eight of the 12 participants quit smoking in the past 15 years, and four of them were current smokers. Among the current smokers, all of them planned to quit after six months. In a scale ranging from 1 to 10, median scores for the importance to them to quit smoking and screening for lung cancer are 7 respectively (1 = not at all important, 10 = extremely important); and 4 and 8 for their confidence to quit smoking and screening for lung cancer, respectively (1 = not at all confident, 10 = extremely confident). More demographic characteristics can be found in Table 2.
Table 2.
Sample characteristics.
| Item | Category | n |
|---|---|---|
| Age (years, Median) | 60 | |
| Gender | Female | 1 |
| Male | 11 | |
| Marital status | Married | 9 |
| Divorced | 3 | |
| Number of children | 1 Child | 8 |
| 2 Children | 4 | |
| Education level | Less than high school diploma | 1 |
| Some college | 2 | |
| Bachelor’s degree | 7 | |
| Master’s degree | 2 | |
| Annual income, $ | <20,000 | 2 |
| 20,000–44,999 | 6 | |
| 45,000–139,999 | 4 | |
| Insurance status | Medical or Medicare | 4 |
| Company’s insurance | 8 | |
| Religious status | Catholic | 5 |
| None | 7 | |
| Age when moved to the US (years, Median) | 42 | |
| Residence years (years, Median) | 18 | |
| Occupation | Export sale | 1 |
| Tourist | 2 | |
| Hotel management | 1 | |
| Fast food service | 2 | |
| Uber eat driver | 3 | |
| No/Retired | 3 | |
| Smoking status | Quit smoking in the past 15 years | 8 |
| Smoking regularly, 1 package/day | 3 | |
| Smoking regularly, 0.5 package/day | 1 | |
| Planning to quit for current smokers | After 6 months | 4 |
| Length of smoking (years) | >10 | 10 |
| 7–10 | 2 | |
| Family history of lung cancer | Yes | 2 |
| No | 10 | |
| Lung cancer screening history | Yes | 2 |
| No | 10 | |
| Intention to screen for lung cancer | Per doctor’s recommendation | 4 |
| After 6 months | 5 | |
| No | 3 |
Note: Data are n, unless otherwise indicated.
3.2. Qualitative results
Based on the Health Belief Model, high-risk Chinese American smokers’ health beliefs toward lung cancer screening with low dose CT were reported by the categories of perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and cues to action (Table 3). Also, representative quotes from the participants were cited in Table 3.
Table 3.
Example quotes and codes for each category.
| Concept | Example Quote | Example Code |
|---|---|---|
| Perceived susceptibility | “Angry, in bad mood, easy to have cancers. Some people smoke for a whole life, but they don’t have cancer. Some people don’t smoke but they still have lung cancer.” (Participant 2, female, 63y) |
|
| “I don’t think my risk is high. Because currently I am living at a house. The air quality is good. Few people live nearby. I retired and I don’t go to factory to work. I don’t smoke now, and my friends don’t smoke. People live nearby don’t smoke too. So, I don’t concern about it.” (Participant 9, male, 78y) |
|
|
| Perceived severity | “First, you are not normal. Second, you are not healthy. Third, if you interact with your friends, you cannot stay too closely when you talk. Other people will also dislike you. Your disease can transmit to others. I think the bacteria will transmit to other. I don’t know whether the bacteria of lung cancer can be passed through sputum. But I think it is not good because you cough frequently.” (Participant 9, male, 78y) |
|
| Perceived benefits | “Know early and prevent early. No, it is not that know early and prevent early. It is … know early and treat early. I think smoking is very common in Asian population. If lung cancer screening is a regular test, it is a good thing for smokers. If lung cancer is screened regularly, it can facilitate (their health) and raise their awareness toward the risk brought by lung cancer. Only if they screen lung cancer, they will know the severity of lung cancer.” (Participant 3, male, 50y) |
|
| “Because if we want to prevent lung cancer, we need to do the test. We can know our lung function after the test. Although I quit smoking for a long time, screening can tell me how my lungs currently function.” (Participant 5, male, 57y) |
|
|
| “Screening lung cancer can tell you what your lungs look like now. If smokers do the test, I think the situation is definitely not good. If the situation is not good, they need to quit smoking as soon as possible. In order to live for a longer time, they need to quit smoking.” (Participant 5, male, 57y) |
|
|
| Perceived barriers | “I didn't do it before. I don’t know whether it is painful. It seems that it needs to inject something, right? Contract agent, right?” (Participant 4, male, 58y) |
|
| “I will follow Jesus’arrangement. Also, I heard lots of diseases are determined by genes or DNA. If I have lung cancer, I will accept my fate.” (Participant 8, male, 51y) |
|
|
| “For disease prevention, I feel … if you are very sick, they will treat you. If you can tolerate the symptoms by yourself, they will not treat you … There is very little work the doctor does for disease prevention.” (Participant 8, male, 51y) |
|
|
| “The time interval for the appointment is very long. Maybe I will use other methods, e.g., go to see urgent care, or buy some medicine to overcome it. I feel it is very inconvenient. Furthermore, they see patients too fast. They don’t have time to listen to your complaint. I feel I don't have time to tell them all my concern. They also don’t have time to tell you what you need to prevent and how you need to prevent.” (Participant 8, male, 51y) |
|
|
| “…What you said just now that my doctor didn’t tell me, is it possible that this is the responsibility of expertise physicians? So, they don’t know?” (Participant 8, male, 51y) |
|
|
| “Chinese people are conservative. Chinese people care about their face, and they are shy. They don’t want others to know their problems. If you make them convenient and keep their privacy, or they can do the screening without other knowing … If you let them do the exam publicly, they will feel shame and they will not accept it on purpose. If you have some methods to help them to do the exam conveniently without costing money and shading shame on them, I think they are willing to do the exam.” (Participant 9, male, 78y) |
|
|
| Self-efficacy | “If I need to make the appointment for the screening, I will let my daughter help me to find the place to schedule.” (Participant 2, female, 63y) |
|
| “For every test, what I wish to see is that the doctor would not tell me the result of the test. If the doctor doesn’t tell me the result, it means nothing wrong.” (Participant 3, male, 50y) |
|
|
| “I felt if you have no diseases or symptoms, if you require to do the X-ray or CT, the doctor will not let you do. So, I am not confident to see my doctor and tell him, ‘I have no discomfort of my lungs. I want to screen lung cancer with low dose CT.’ The doctor will ask me, ‘What discomfort do you have?’ For me, they will only let you do the CT when you don’t feel well.” (Participant 8, male, 51y) |
|
|
| Cues to action | “…So first it is the introduction by social media, second family members’advice, and doctor’s suggestions and command. Of course, we can also tell the doctor, ‘There is the lung cancer screening test. Can we do the screening? Whether I can make an appointment for it?’ We can ask doctors' actively.” (Participant 3, male, 50y) |
|
3.2.1. Perceived susceptibility
When asked about who was at a high risk of lung cancer, all participants acknowledged that smokers were susceptible to lung cancer. They also mentioned secondhand smokers, smokers with alcohol use, and the person who had a family history of lung cancer could have a high risk of lung cancer. Although all participants were able to identify the risk factors of lung cancer, some confusions around the risk of lung cancer were still noticed. While some participants can correctly identify the environment factor which led to lung cancer (e.g., dusty, and smoky working environment), some participants thought bad mood can cause lung cancer (e.g., cited in Table 3, per participant 2). In addition, most of the participants thought smoking did not definitely lead to lung cancer. They gave evidence by the smokers who they know but didn’t get lung cancer and non-smokers who were diagnosed with lung cancer to support their opinions.
Most of the participants thought their personal risk of lung cancer was low. Only one participant thought he was possible to get lung cancer, and one participant thought everyone’s risk for lung cancer was the same. The participants attributed their low risk of lung cancer to their regular work and life schedule, family history (without lung cancer history), healthy behaviors (quitting smoking in the past 15 years, not drinking, doing exercise, and healthy diet), good health status (no problems or symptoms of their lungs), and environmental factors (good air quality, and good work and life environment) (e.g., e.g., cited in Table 3, per participant 9). One participant stated getting old made him worried and scared about his lung cancer risk.
3.2.2. Perceived severity
All the participants acknowledged lung cancer would have a huge impact on their life. Most of them mentioned lung cancer could cause personal health problems (e.g., discomfort when breathing, shortness of breath, short of life, fatigue and easy to get tired, and death), with one participant thinking that lung cancer patients were discriminated by others because lung cancer could transmit to others (e.g., cited in Table 3, per participant 9). Also, they stated lung cancer could cause family problems and impact social interaction with others. All the participants reported lung cancer brought emotional distress/despair/frustration/fear to them and their family members. They also mentioned the heavy financial burden brought by lung cancer treatment, with one participant emphasizing that being a household head diagnosed with lung cancer brought a disaster to the whole family.
3.2.3. Perceived benefits
All the participants realized the benefits of lung cancer screening with low dose CT. All of them agreed lung cancer screening can help them to detect and treat lung cancer earlier. Most of them thought screening can help to prevent lung cancer (e.g., cited in Table 3, per participant 3). Some participants stated screening for lung cancer could tell them about their current lung status, help with emotion management (not so worried about their smoking history, and make people ease), and raise smokers’ concern about their health. They thought a bad lung situation would help smokers to quit smoking, and screening could increase smokers’ perceived risk and severity of lung cancer (e.g., cited in Table 3, per participant 5).
3.2.4. Perceived barriers
Barriers to lung cancer screening were noticed from participants’ personal factors, physicians’ factors, and institutional factors. Participants’ personal factors hindering their lung cancer screening behaviors included emotional factor, lack of knowledge about lung cancer screening, financial factor, physical barriers, incorrect health maintenance beliefs and behaviors, fatalism beliefs, and language barriers. Most of the participants reported being scared/worried about a lung cancer diagnosis would hinder them to screen for lung cancer. One participant reported that she was not willing to bother doctors and she thought lung cancer would be a result of her fault. One participant pointed out that the discrimination/stigma/shame around screening was a reason for smokers to opt out of screening (e.g., cited in Table 3, per participant 9).
Results showed that all the participants lacked knowledge about lung cancer screening: They never heard about the lung cancer screening with low dose CT before, and neither of them did lung cancer screening previously (e.g., cited in Table 3, per participant 4). Most of the participants thought knowledge of lung cancer screening was a factor impacting lung cancer screening behaviors. Some participants described their confusion around the procedures of lung cancer screening, including not knowing whether lung cancer is painful or not, thinking radiation from screening is harmful to people, etc. Some participants expressed their confusion about the performance of lung cancer screening, including mixing up screening with clinical trial exams and medicine treatment, and mixing up low dose CT lung cancer screening with normal CT scan for diagnosing lung cancer among symptomatic patients. One participant pointed out that he did not know whether he had a high risk for lung cancer or not. Upon further discussions with the participants, all of them attributed the insufficient information on lung cancer screening to their lack of knowledge on screening with low dose CT.
Barriers related to financial and physical factors were noticed in the interviews. Some of the participants pointed out financial cost was a reason for smokers’ opting out of lung cancer screening. They thought screening was not worthy given money was cost. Further, some participants reported physical barriers such as transportation, time conflict (have to ask a leave from work to go to screening), and time consuming (have to wait for a long time before the appointment time and need to go to different places to see doctors and do exams) would hinder them to screening for lung cancer.
Incorrect health maintenance beliefs and behaviors also hindered the high-risk Chinese American participants’ lung cancer screening behaviors. All the participants reported good health (without problems or symptoms of their lungs) was a reason for their not thinking about lung cancer screening. One participant mentioned his father’s diagnosis with lung cancer due to not getting further screening since the nodule in his lung didn’t change. One participant pointed out his friends being diagnosed with lung cancer due to their not caring about their lung symptoms and mistakenly believing their symptoms would get better with time went by. Some participants agreed that they did not think about screening actively. They mentioned a common problem related to smokers’ screening behavior---take the chance if no symptoms occur. One participant said that she tended to take medicines by herself to treat health problems without seeing the doctor or doing exams.
Furthermore, fatalism beliefs and language barriers were acknowledged barriers for the high-risk Chinese American participants’ to screening for lung cancer. When talking about perceptions toward lung cancer, all the participants tended to use the second-personal pronoun (“you”) to explain everything, instead of using the first-personal pronoun (e.g., I will get lung cancer if …). One participant mentioned twice in his conversation that lung cancer was determined by genes or DNA, and one participant believed Jesus arranged everything no matter screening was done or not (e.g., cited in Table 3, per participant 8). Most of the participants mentioned communication with doctors in the English language is a difficulty for them to access health care services. They tended to choose Chinese-speaking doctors for treating their health problems.
Physicians’ factors related to the four sub-barriers to screening for lung cancer included neglect of prevention, time limitation, possible lack of knowledge about lung cancer screening, and possible ambiguous obligation. When talking about the reasons for not having a discussion with doctors about lung cancer screening, all the participants mentioned that they had never received a recommendation about lung cancer screening from their doctors. Some participants emphasized doctors did little about disease prevention (e.g., cited in Table 3, per participant 8). One participant mentioned doctors did not take lung cancer screening seriously (thought lung cancer screening was not important). The findings clearly suggest physicians who provided care to Chinese Americans tended not to recommend lung cancer screening to their patients. Further, some participants mentioned the consultation time was not enough when seeing a doctor, and the doctor was too busy to tell patients about other information. One participant reported feeling awkward to discuss with doctors about disease prevention due to doctor’s lack of time (e.g., cited in Table 3, per participant 8). Lastly, some participants talked about their confusion about the responsibility of ordering lung cancer screening by doctors. They wondered whether it is their family doctors’ or the expertise doctors’ responsibility to order the screening since none of them did that for them previously (e.g., cited in Table 3, per participant 8).
The participants also mentioned the institutional factors which hindered their screening behaviors. All the participants thought the education on lung cancer screening was insufficient. Some participants pointed out that lack of attention about lung cancer screening from the health care system was a reason for their not screening for lung cancer. Some participants complained about the inconvenience to go to different places to see doctors and do exams, and they pointed out the appointment time interval was too long for seeing a doctor or receiving physical exams.
3.2.5. Self-efficacy
When asked about where and how to screen for lung cancer, even though some participants had the experience of receiving CT previously due to diseases, most of the participants were not confident about where to receive the low dose CT test and how to get it. Some participants thought only family doctors could order the screening. Some participants felt not confident to suggest their doctors order lung cancer screening for them, if they had no symptoms (e.g., cited in Table 3, per participant 8). One participant thought doing a CT was comfortable and the procedure was convenient. When asked about their confidence to schedule the appointment for screening, most of the participants depended on their family doctor to schedule the appointment. One participant reported she needed help from her daughter to arrange the appointment (e.g., cited in Table 3, per participant 2). Regarding their confidence to discuss the results of lung cancer screening with their doctors, most of the participants were confident to accept the results of the screening. Some participants were not willing to know the results or accept a bad result of lung cancer screening (e.g., cited in Table 3, per participant 3). One participant mentioned his confusion about the results of the CT exam by talking about his father’s diagnosis of lung cancer although he had done lung CT exams several times. Even though confusions about the results of lung cancer screening presented, all of them acknowledged feeling frustrated about getting a bad result from screening.
Following discussions about their confidence to treat lung cancer after a positive result from screening, most of the participants expressed their confidence to follow the doctor’s instruction on the treatment. One participant stated that she would only be willing to treat if the status of lung cancer was not serious, and she thought treatment of late-stage lung cancer was not worthy. The other participant pointed out that he would only see a doctor if the result of screening was not so bad; if lung cancer was diagnosed at a late stage and the prognosis was not good, he would wait to die and not treat, with a hope that he would die quickly since he believed Jesus would arrange his life.
3.2.6. Cues to action
When talking about getting information on lung cancer screening, all the participants did not know lung cancer screening was performed using low dose CT, although some of them received CT exam before. Most of the participants did not know how to get information to screen for lung cancer. Some of them thought getting information from hospitals or doctors, consulting others, or family members’ help. Although some of the participants thought the internet could make information more accessible to smokers, one of them agreed she did not like to search for information online, neither did she know how to search for information through websites, and another participant pointed out he preferred simple and easily understandable text information with pictures.
Regarding the triggers for smokers to decide to screen for lung cancer, all the participants agreed having symptoms or problems with lungs would trigger smokers’ wiliness to screen. Some of the participants thought being old was a reason for them to receive screening. One participant emphasized the importance to aware of the harm of smoking and the risky smoking amount for the smokers to screen for lung cancer. For the external cues to action, all the participants thought doctors’ recommendation to screen was very important. In addition, family members’ suggestions and social media information were important to their screening behaviors (e.g., cited in Table 3, per participant 3). Some participants thought smokers would take screening seriously if it was a normal regular exam, and they suggested the request and discussion of screening with doctors could be done by smokers actively.
4. Discussion
4.1. Chinese American high-risk smokers’ health beliefs toward lung cancer screening
This qualitative study explored Chinese American high-risk smokers’ perceptions and beliefs toward lung cancer screening with low dose CT based on the Health Belief Model. This is one of the first studies focusing on Chinese Americans’ perceptions of lung cancer screening. Findings from this study could benefit both health care providers and high-risk Chinese American smokers by helping them to identify the barriers and facilitators for lung cancer screening, thus sensitive intervention programs could be designed and implemented to increase the uptake rate of lung cancer screening among Chinese Americans.
In the study, although all participants were able to identify the risk factors of lung cancer; however, some confusions around the risk of lung cancer were also noticed. The relationship between smoking and lung cancer was not clear among the participants. Witnessed by the evidence from smokers who did not get lung cancer and non-smokers who did get lung cancer, most participants thought their risk of lung cancer was not definitely high. Furthermore, by underlining other protective factors to health, such as a regular work and life schedule, quitting smoking in the past 15 years, not drinking, doing exercise and so on, the participants further refused their risk of lung cancer, although they smoked more than 20 package-year previously.
This should be an important point to initiate in-depth conversations about lung cancer screening with Chinese Americans at high-risk for lung cancer. Health education focusing on the aggressive factors and defensive factors of lung cancer should be taught to the high-risk smokers. Explanations about the relationship between smoking and lung cancer should be delivered to smokers to raise their awareness of their risk of lung cancer. Knowledge about smoking’s consequences on lung cancer should be clarified by mentioning other risk factors such as secondhand smoking and polluted air, which may lead to non-smokers getting lung cancer [24]. In addition, smokers not getting lung cancer should be clarified with the fact that multiple diseases could be caused by smoking (e.g., cardiovascular diseases, stroke, diabetes, and other sites of cancers, etc.) [31]; smokers may not be able to develop or discover lung cancer prior to the other kinds of diseases’ symptoms occur.
Given the low survival rate of lung cancer, all the participants agreed lung cancer would have a huge impact on their life, from the aspects of health, emotion, finance and social interactions with the family members and someone else. Although most of the participants were able to identify the consequences caused by lung cancer disease, understanding toward the cause of lung cancer and the consequence mentioned by one participant was inaccurate. Thinking lung cancer was a contagious disease and it could transmit to others made the participant think a lung cancer diagnosis could bring discrimination/stigma/shame to the smokers. Going from this, additional health education on the pathology of lung cancer should be delivered to high-risk smokers. It was necessary to let smokers know that more than 60 known carcinogens had been detected in cigarette smoke [32]. All the carcinogens played a crucial role in tumorigenesis [32], which activated smokers’ DNA that evoked genetic mutations and epigenetic reprogramming [32], and eventually led to uncontrollable cell mutation. Clarification should be made on the non-contagious characteristic of lung cancer. Instead of bacteria or viruses which could be contagious, the auto-cellular variation caused by the carcinogens in cigarette smoke should be emphasized as the reason for lung cancer, thus the perception of the consequence of transmitting lung cancer disease to others, and feeling discriminated/stigmatized/shame from others could be changed.
Regarding the perceived benefits of lung cancer screening, although all the participants agreed that screening for lung cancer could help to detect and treat lung cancer earlier, a misunderstanding of the benefits of lung cancer was noticed in the individual conversations with four participants who thought screening can help to prevent lung cancer. Although lung cancer screening with low dose CT is a secondary prevention method for lung cancer, by screening with low dose CT, lung cancer can be detected and treated at an earlier stage before the appearance of signs or symptoms [33]; however, screening cannot change the fact that lung cancer is developing or occurred. Smoking cessation is the optimal method for smokers to prevent lung cancer. As the primary prevention method for lung cancer, smoking cessation is found to be cost-effective both yielding immediate and long-term benefits to the health of lung cancer patients, including decreased risk of disease, increased survival time, decreased postoperative complications, increased efficacy of chemotherapy, decreased radiation therapy complications, and improved quality of life [34]. Thus, when a conversation about lung cancer screening is initiated with high-risk smokers, emphasis should be put both on screening and smoking cessation. In addition, some participants realized the benefits of lung cancer screening on smoking cessation. They stated that screening for lung cancer could raise smokers’ concern about their health and increase their perceived risk and severity toward lung cancer. Particularly, a bad lung situation would help smokers to quit smoking, which is also supported by the evidence that three of the participants in this study quit smoking in the past 15 years due to their fear of the “black and messy lungs” in the chest image exam.
In the study, barriers to screening for lung cancer existed at participants’, physicians’, and institutional levels. Efforts should be put to help high-risk smokers to overcome those barriers. Promotion programs focusing on the propaganda of lung cancer screening related knowledge should be implemented both among physicians and high-risk smokers. Attention should be raised to help physicians and high-risk smokers to realize their roles in preventing lung cancer. Information on the free cost, low radiation, and performing procedures should be delivered to the eligible high-risk smokers to ease their fear/worry/shame toward lung cancer screening. Flexible and convenient screening schedules with mandarin language services should be provided to help Chinese American high-risk smokers to get access to the services. Health education on disease prevention and health promotion should be delivered both to high-risk smokers and their significant others. Emotional care such as encouraging high-risk smokers to talk about what they were going through, to be strong, to maintain a positive environment and normalcy, and to use spirituality as a source of strength to help them change their negative fatalism attitude to a positive one [35].
When talking about the self-efficacy of lung cancer screening, most of the participants were not confident enough. They needed help with screening either from health care providers or family members. In addition, some of the participants were not ready to deal with the result of screening, and all the participants endorsed an emotional change upon getting a lung cancer diagnosis. Furthermore, the negative expectation of the treatment and confusion around the result of screening were also noticed in the study. To increase high-risk smokers’ self-efficacy in screening for lung cancer, one-on-one shared decision-making conversations should be initiated to help them better understand the benefits and harms of screening for lung cancer [36]. Explanations around the false negative and false positive results of screening and the possible consequences (e.g., missing detection of lung cancer, and following-up invasive procedures such as diagnostic needle biopsy, bronchoscopy, and thoracic surgery, etc.) should be informed to the high-risk smokers [37]. Also, mental health support following screening should be prepared to help this vulnerable population get through their life change. When it is necessary, palliative care should be provided at patients’ request after a comprehensive evaluation of patients’ quality of life and the disease progress.
Regarding the cues to action, disseminating information on lung cancer screening is an important external cue that could change high-risk smokers’ attitude toward lung cancer screening. Clarification on the low dose of CT and the difference between screening and normal CT for diagnosis should be provided to help high-risk smokers differentiate the concepts of screening and diagnosis. Easy understandable culturally sensitive Chinese text information flyers or pamphlets with pictures should be designed and distributed to high-risk smokers. Support from health care providers (by giving recommendations), family members, relatives, and friends (by providing suggestions), and social media (by increasing awareness and sharing knowledge) should be maintained to remind eligible high-risk smokers to screen for lung cancer annually. When it is necessary, an active request by eligible high-risk smokers to screen for lung cancer could be combined to the physicians’ recommendation of lung cancer screening. Working along both with high-risk smokers and physicians could ensure an increasing uptake rate of lung cancer screening among Chinese American smokers.
In the study, findings about Chinese American high-risk smokers’ health beliefs toward lung cancer screening are consistent with those reported in the US population. According to the focus group interview study conducted by Carter-Harris et al. [13], long term US smokers perceived insufficient association of long-term smoking with lung cancer risk. Their perceived benefits of screening included finding lung cancer early, giving peace of mind, and motivation to quit smoking. Their perceived barriers to screening included inconvenience, distrust, and stigma. These findings are echoed by the results from this study. However, it is noticeable that some of the Chinese American high-risk smokers’ health beliefs toward lung cancer screening are unique, e.g., protective factors to health are over emphasized in the population thus long-term smoking history is ignored by the Chinese American high-risk smokers. Given their unique aspects of health beliefs toward lung cancer screening, special attention should be paid to educate the high-risk Chinese American smokers to establish correct health beliefs toward lung cancer screening.
4.2. Strengths and limitations
This study explored Chinese American high-risk smokers’ health beliefs toward lung cancer screening for the first time. Findings from this study could help healthcare providers to identify the barriers/facilitators for Chinese American high-risk smokers to screening for lung cancer. Further actions/intervention programs could be implemented to help Chinese American high-risk smokers overcome the barriers to screening for lung cancer.
This study has some limitations. First, although we intended to recruit Chinese American high-risk smokers across the United States, most of the participants (n = 8) in this study resided in the Los Angeles area; thus, some of our findings may be not relevant to the high-risk Chinese American smokers who reside in other areas. However, given the cultural elements are mostly in common across Chinese Americans residing in different areas within the United States, the findings of this study could still mirror some issues related to Chinese American high-risk smokers’ health beliefs toward lung cancer screening and provide useful information to increase their awareness to screening for lung cancer. Secondly, same as in other qualitative studies, participants’ recall-bias and self-reflection may bring bias to the study. By recalling their past experiences and answering questions from their personal perceptions, individual opinions may deviate the results of the study. However, by triangulating and constantly comprising the significant and meaningful themes that emerged in the transcripts, bias brought up by individual participants could be reduced to an acceptable level.
4.3. Future directions for research and practice
Findings from this study indicate several directions for future research and clinical practice. First, culturally sensitive Chinese language education programs which focus on lung cancer screening need to be implemented among high-risk smokers and health care facilities. Health education tools such as flyers and pamphlets should be disseminated among this population to help them increase their knowledge level of lung cancer screening. Second, one-on-one pre-screening shared decision-making conversations and post-screening mental health support should be implemented in the clinical practice. Involving high-risk smokers’ family members and friends in the screening process could help to promote and remind high-risk smokers to screen for lung cancer. Third, smoking cessation education and lung cancer screening promotion should go hand in hand among current high-risk smokers. Without quitting smoking, by screening for lung cancer solely, current high-risk smokers’ risk of getting lung cancer is still at a high level. Supporting methods for quitting smoking such as language sensitive quitting smoking line and nicotine patch should be informed and promoted among current high-risk smokers.
5. Conclusions
Guided by the Health Belief Model, high-risk Chinese American Smokers’ health beliefs toward lung cancer screening with low dose CT were explored in this study. Findings from this study enable us to understand Chinese Americans’ lung cancer screening behaviors and suggest various strategies to increase lung cancer screening among this population. Given the prevalent smoking rate but low uptake rate of lung cancer screening among this population, we suggested that smoking cessation and lung cancer screening should be emphasized together for this population in the shared decision-making conversations with health care professionals; mental support should be provided to counter the effect of fatalism and negative emotion in this population; and support should be obtained from high-risk Chinese American smokers’ family members and friends. By using the Health Belief Model, targeted interventions could be designed and utilized more efficiently to deal with the barriers to screening for lung cancer among this population, and eventually, increase their self-efficacy in screening for lung cancer.
CRediT authorship contribution statement
Fang Lei: Conceptualization, Methodology, Writing - original draft. Wei-Ti Chen: Writing - review and editing. Mary-Lynn Brecht: Writing - review and editing. Zuo-Feng Zhang: Writing - review and editing. Eunice Lee: Writing - review and editing.
Funding
This study was supported by American Cancer Society, Sigma Theta Tau, and China Scholarship Council. Reimbursement for participants’ participation was supported by the funding.
Data availability statement
The qualitative datasets generated and/or analyzed during the current study are not publicly available due to the data containing information that could compromise research participant privacy/consent but are available from the corresponding author on reasonable request, and subject to approval from the institution of research board at the University of California, Los Angeles.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgments
The authors would like to thank the participants who participated in the study. This manuscript is based on a part of the PhD dissertation titled “Cross-cultural Adaptation and Validation of Lung Cancer Screening Health Belief Scale” written by the first author, which is stored in the UCLA Electronic Theses and Dissertations.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.06.005.
Contributor Information
Fang Lei, Email: airlf201314@gmail.com.
Wei-Ti Chen, Email: wchen@sonnet.ucla.edu.
Mary-Lynn Brecht, Email: LBrecht@sonnet.ucla.edu.
Zuo-Feng Zhang, Email: zfzhang@ucla.edu.
Eunice Lee, Email: EELee@sonnet.ucla.edu.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Gomez S.L., Yang J., Lin S.W., McCusker M., Sandler A., Cheng I., et al. Incidence trends of lung cancer by immigration status among Chinese Americans. Cancer Epidemiol Biomarkers Prev. 2015;24(8):1157–1164. doi: 10.1158/1055-9965.epi-15-0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Association of Community Cancer Centers . Association of Community Cancer Centers; Rockville, MD: 2016. Understanding & improving lung cancer treatment in Asian Americans & Pacific Islanders in the community setting.https://www.accc-cancer.org/docs/projects/resources/pdf/LungCancerTools/aapi-whitepaper [Google Scholar]
- 3.Tota J.E., Ramanakumar A.V., Franco E.L. Lung cancer screening: review and performance comparison under different risk scenarios. Lung. 2014;192(1):55–63. doi: 10.1007/s00408-013-9517-x. [DOI] [PubMed] [Google Scholar]
- 4.Wender R., Fontham E.T., Barrera E., Colditz G.A., Church T.R., Ettinger D.S., et al. American Cancer Society lung cancer screening guidelines. CA A Cancer J Clin. 2013;63(2):107–117. doi: 10.3322/caac.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Latimer K.M., Mott T.F. Lung cancer: diagnosis, treatment principles, and screening. Am Fam Physician. 2015;91(4):250–256. [PubMed] [Google Scholar]
- 6.Bindman A. JAMA Forum: lung cancer screening and evidence-based policy. JAMA. 2015;313(1):17–18. doi: 10.1001/jama.2014.16429. [DOI] [PubMed] [Google Scholar]
- 7.Hoffman R.M., Sussman A.L., Getrich C.M., Rhyne R.L., Crowell R.E., Taylor K.L., et al. Attitudes and beliefs of primary care providers in New Mexico about lung cancer screening using low-dose computed tomography. Prev Chronic Dis. 2015;12:E108. doi: 10.5888/pcd12.150112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewis J.A., Petty W.J., Tooze J.A., Miller D.P., Chiles C., Miller A.A., et al. Low-dose CT lung cancer screening practices and attitudes among primary care providers at an academic medical center. Cancer Epidemiol Biomarkers Prev. 2015;24(4):664–670. doi: 10.1158/1055-9965.EPI-14-1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jemal A., Fedewa S.A. Lung cancer screening with low dose computed tomography in the United States-2010 to 2015. JAMA Oncol. 2017;3(9):1278–1281. doi: 10.1001/jamaoncol.2016.6416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li C.C., Matthews A.K., Dong X.Q. Examination of chronic smoking behavior and eligibility for low-dose computed tomography for lung cancer screening among older Chinese male smokers. J Gerontol A Biol Sci Med Sci. 2017;72(suppl_1):S22–S25. doi: 10.1093/gerona/glw202. [DOI] [PubMed] [Google Scholar]
- 11.Cataldo J.K. High-risk older smokers' perceptions, attitudes, and beliefs about lung cancer screening. Cancer Med. 2016;5(4):753–759. doi: 10.1002/cam4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carter-Harris L., Brandzel S., Wernli K.J., Roth J.A., Buist D.S.M. A qualitative study exploring why individuals opt out of lung cancer screening. Fam Pract. 2017;34(2):239–244. doi: 10.1093/fampra/cmw146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carter-Harris L., Ceppa D.P., Hanna N., Rawl S.M. Lung cancer screening: what do long-term smokers know and believe? Health Expect. 2017;20(1):59–68. doi: 10.1111/hex.12433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duong D.K., Shariff-Marco S., Cheng I., Naemi H., Moy L.M., Haile R., et al. Patient and primary care provider attitudes and adherence towards lung cancer screening at an academic medical center. Prev Med Rep. 2017;6:17–22. doi: 10.1016/j.pmedr.2017.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gressard L., DeGroff A.S., Richards T.B., Melillo S., Kish-Doto J., Heminger C.L., et al. A qualitative analysis of smokers' perceptions about lung cancer screening. BMC Publ Health. 2017;17(1):589. doi: 10.1186/s12889-017-4496-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanner N.T., Egede L.E., Shamblin C., Gebregziabher M., Silvestri G.A. Attitudes and beliefs toward lung cancer screening among US Veterans. Chest. 2013;144(6):1783–1787. doi: 10.1378/chest.13-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jonnalagadda S., Bergamo C., Lin J.J., Lurslurchachai L., Diefenbach M., Smith C., et al. Beliefs and attitudes about lung cancer screening among smokers. Lung Cancer. 2012;77(3):526–531. doi: 10.1016/j.lungcan.2012.05.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collins C., Stockton C. The central role of theory in qualitative research. Int J Qual Methods. 2018;17(1) doi: 10.1177/1609406918797475. [DOI] [Google Scholar]
- 19.Brink H. second ed. 1999. Fundamentals of research methodology for health care professionals. Cape Town, Juta. [Google Scholar]
- 20.Carpenter C.J. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010;25(8):661–669. doi: 10.1080/10410236.2010.521906. [DOI] [PubMed] [Google Scholar]
- 21.Glanz K., Rimer B.K., Viswanath K. Jossey-Bass; San Francisco, CA: 2008. Health behavior and health education: theory, research, and practice. [Google Scholar]
- 22.Siddiqui T.R., Ghazal S., Bibi S., Ahmed W., Sajjad S.F. Use of the health belief model for the assessment of public knowledge and household preventive practices in Karachi, Pakistan, a dengue-endemic city. PLoS Neglected Trop Dis. 2016;10(11) doi: 10.1371/journal.pntd.0005129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kwong K. Cancer beliefs and cancer screening behaviors among low income Chinese immigrants–Implications for culturally relevant interventions. J Nurs Educ Pract. 2016;6(10):130–140. doi: 10.5430/jnep.v6n10p130. [DOI] [Google Scholar]
- 24.Centers for Disease Control and Prevention . 2020. What are the risk factors for lung cancer?https://www.cdc.gov/cancer/lung/basic_info/risk_factors.htm 17 June 2021. [Google Scholar]
- 25.Sofaer S. Qualitative methods: what are they and why use them? Health Serv Res. 1999 Dec;34(5 Pt 2):1101–1118. PMID: 10591275; PMCID: PMC1089055. [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Preventive Services Task Force. Lung cancer: screening. [Accessed 20 April 2022].https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening.
- 27.Given Lisa M. Swinburne University; Australia: 2008. The sage encyclopedia of qualitative research methods. Charles Sturt University, Australia: Sage. [Google Scholar]
- 28.Saldaña J. Sage; Thousand Oaks, California: 2009. The coding manual for qualitative researchers. [Google Scholar]
- 29.Clarke V., Braun V. Sage; 2013. Successful qualitative research: a practical guide for beginners. [Google Scholar]
- 30.O'Brien B.C., Harris I.B., Beckman T.J., Reed D.A., Cook D.A. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention Health effects. 2020. https://www.cdc.gov/tobacco/basic_information/health_effects/index.htm
- 32.Hecht S.S. Tobacco carcinogens, their biomarkers and tobacco-induced cancer. Nat Rev Cancer. 2003;3(10):733–744. doi: 10.1038/nrc1190. [DOI] [PubMed] [Google Scholar]
- 33.Eddy D.M. Secondary prevention of cancer: an overview. Bull World Health Organ. 1986;64(3):421–429. [PMC free article] [PubMed] [Google Scholar]
- 34.Cataldo J.K., Dubey S., Prochaska J.J. Smoking cessation: an integral part of lung cancer treatment. Oncology. 2010;78(5–6):289–301. doi: 10.1159/000319937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hamilton J.B., Worthy V.C., Moore A.D., et al. Messages of hope: helping family members to overcome fears and fatalistic attitudes toward cancer. J Cancer Educ. 2017;32:190–197. doi: 10.1007/s13187-015-0895-z. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Medicare & Medicaid Services Decision memo for screening for lung cancer with low dose computed tomography (LDCT) 2015. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=274
- 37.National Cancer institution After lung cancer screening, follow-up procedures may be riskier than thought. 2019. https://www.cancer.gov/news-events/cancer-currents-blog/2019/lung-cancer-screening-complications-diagnostic-follow-up
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The qualitative datasets generated and/or analyzed during the current study are not publicly available due to the data containing information that could compromise research participant privacy/consent but are available from the corresponding author on reasonable request, and subject to approval from the institution of research board at the University of California, Los Angeles.