Abstract
Issue
Alcohol consumption during pregnancy and breastfeeding cause adverse health outcomes to the mother and child, including Fetal Alcohol Spectrum Disorder (FASD).
Approach
Systematic literature review and thematic synthesis. Original studies that contained reasons for alcohol consumption in pregnancy and while breastfeeding were included. The Mixed Methods Appraisal Tool (MMAT) and the Confidence in the Evidence of Reviews of Qualitative Research (CerQUAL) approach were utilised. The review protocol is available on PROSPERO (registration number: CRD42018116998).
Key Findings
Forty‐two eligible studies comprising women from 16 countries were included. Most commonly reported reasons of alcohol use in pregnancy were societal pressure and the belief that only “strong” alcohol and alcohol in large quantities is harmful. Other reasons were: a lack of awareness of adverse effects on the fetus; coping with adverse life experiences; consumption based on intuitive decision‐making and influenced by personal/peer experiences; belief in the beneficial properties of alcohol; advice from medical practitioners; unwanted or unplanned pregnancy; alcohol dependence; and consumption as a cultural/traditional custom. Reasons for alcohol use during breastfeeding included the belief that alcohol stimulates breast milk production, unclear advice from medical practitioners, unawareness of the risks of infant exposure and to improve mood and celebrate events.
Implications
Understanding the context of reasons for alcohol use in pregnancy is crucial for implementing prenatal health education, and preventing FASD and other adverse maternal and child health outcomes.
Conclusion
Individual beliefs, knowledge/advice, culture and personal circumstances influence alcohol use in pregnancy. Data are limited for reasons surrounding alcohol use while breastfeeding.
Keywords: alcohol, pregnancy, breastfeeding, Fetal Alcohol Spectrum Disorder, reasons
Introduction
It is well established that alcohol is a teratogen and numerous existing guidelines advise women to abstain from alcohol during pregnancy and while breastfeeding [1, 2]. However, many women consume alcohol in pregnancy even after learning they are pregnant [3]. Worldwide, approximately 10% of women in the general population consume alcohol in pregnancy, although the European region has the highest rate of consumption (25%) [3].
Prenatal alcohol exposure (PAE) may cause several adverse health effects for the developing fetus including stillbirth, spontaneous abortion, low birthweight, prematurity, intrauterine growth restriction and birth defects [4, 5, 6, 7, 8]. PAE can also cause Fetal Alcohol Spectrum Disorder (FASD), which is a serious, chronic and systemic disease characterised by central nervous system damage and physical disabilities, that lead to a wide range of lifelong health and social consequences. Approximately 1 in every 13 infants prenatally exposed to alcohol will develop FASD, placing a significant portion of pregnancies at risk worldwide [3, 9, 10]. FASD also imposes a significant cost burden on health care and service systems, as the daily estimated cost of care per individual with FASD is over $20 000 per day [11]. In Canada, the annual cost burden associated with FASD is estimated to range from $1.8 billion [12] to $5.3 billion [13]. With respect to breastfeeding, infant exposure to alcohol through breastmilk can cause delayed cognitive development, infant agitation and disrupted sleep patterns [14, 15, 16]. Furthermore, research indicates that child development is more compromised in children exposed to alcohol during both pregnancy and breastfeeding periods, as compared to pregnancy alone [17]. Effects of infant exposure to alcohol via breastmilk are moderated by the timing of breastfeeding in relation to maternal alcohol use, nutrition and PAE, as well as other sources of ethanol exposure (e.g. medicine) [16]. Alcohol use after birth and during breastfeeding is increasing [15], though women typically take precautionary measures to reduce alcohol exposure to their infant [16].
Alarmingly, levels of consumption and binge drinking are increasing among young women of childbearing age in many countries around the globe [18]. In this age cohort, a significant proportion (44–65%) of pregnancies is unplanned [19], resulting in a high risk for infants to be unintentionally prenatally exposed to alcohol. Beyond the significant adverse health effects of alcohol use in pregnancy, alcohol use/dependence in general can also severely impair maternal/paternal functioning [20], trigger and exacerbate patterns of intimate partner violence [21] and thus, can negatively affect child development and safety. Rates of alcohol use during pregnancy vary across countries and across subpopulations, with global trends of alcohol use impacting each country differently. For example, there is some evidence to suggest that rates of alcohol use in pregnancy have decreased in Australia from 2000 to 2016 [22], while USA data show an increase from 2011–2013 to 2015–2017 [23]. However, there is some evidence to suggest that alcohol use in pregnancy has increased in some countries during the COVID‐19 pandemic [24, 25, 26, 27].
While numerous FASD prevention efforts exist and many service providers do screen for alcohol use in pregnancy and work to encourage alcohol‐free pregnancies, many women continue to consume alcohol in pregnancy for a variety of reasons. Some of the risk factors associated with consuming alcohol in pregnancy related to various impacts on women's wellbeing are well‐documented, such as experiencing violence during pregnancy, pre‐pregnancy alcohol consumption patterns and inadequate access to prenatal care [28]. Contextual factors related to women's wellbeing and circumstances greatly affect alcohol use behaviour, including access to health care and substance use treatment services, education, food security and experiences of systemic racism, stigma or discrimination [29, 30]. Though various systemic barriers such as stigma are rampant and continue to pose a challenge to enhancing pregnant women's wellbeing, there is less focus globally on how systems can address these barriers to facilitate positive outcomes [30]. Often, approaches to prevention of alcohol use during pregnancy and FASD are child‐centred, and may include punitive approaches that tend to minimise the impacts of alcohol use and addiction on maternal wellbeing [31]. Ideally, these prevention approaches would be linked to accessible treatment services and additional public health interventions that can benefit families in the long term [31].
Existing literature indicates a variety of individual risk and protective factors for alcohol use during pregnancy, obtained from robust quantitative data analysis. These risk and protective factors may be useful in identifying pregnant women who may need extra screening or access to brief interventions during pregnancy. For example, it has been shown that age cohorts and education levels affect alcohol use behaviour during pregnancy, though these effects vary based on country and subpopulation [23, 32]. For example, one study from Australia reported that being older and more educated are associated with a greater likelihood of alcohol use during pregnancy in the general population [22]. Another study from Canada found that being younger and having a history of mental illness are associated with alcohol use during pregnancy [32].
While individual‐level risk factors are important to examine in order to create country‐specific efforts, these efforts can be strengthened if they are informed by the women themselves. Understanding the self‐identified reasons for alcohol use among women who are pregnant or breastfeeding empowers them to speak on their own experiences, describe their systemic barriers that are typically left unaddressed and identify contributing factors to alcohol use during pregnancy themselves as opposed to associations and conclusions made by researchers. Learning from women directly can allow researchers to understand circumstances in an open, non‐judgemental way, which is key to developing targeted interventions in various countries. Tailored prevention strategies can then have the potential to reduce harm to women and their children, improve engagement and avoid stigmatisation of the women they target [29]. Currently, less is known about the specific motivations to use alcohol during pregnancy and breastfeeding that are self‐identified by women. As such, a systematic review and thematic analysis on existing studies, which provide self‐identified reasons for alcohol consumption during pregnancy and breastfeeding were conducted to inform both aims.
Methods
Comprehensive systematic literature search
A comprehensive systematic literature search was conducted and reported according to the standards set in the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) [33]. The literature search was performed to identify all studies of pregnant or postpartum women who have consumed alcohol during pregnancy and have explicitly stated or identified reasons for the alcohol consumption via an open‐ended or structured response (See Appendix S1). The full protocol, containing the literature search strategy and study screening process, is registered and available on PROPERO: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=116998.
Inclusion/exclusion criteria
Articles were retained if they consisted of original research published in peer‐reviewed journals or scholarly reports and contained self‐identified maternal reasons for alcohol consumption in pregnancy. Eligible study designs included cohort, cross‐sectional quantitative studies, qualitative and mixed methods studies. There were no geographical or language restrictions, and the search was performed to identify all studies published by July 2020. Articles were excluded if they lacked information about maternal alcohol use behaviour in pregnancy or breastfeeding, or if they did not indicate specific reasons for alcohol use only.
Study selection and data abstraction
Two reviewers independently conducted screening at two levels: title and abstract screening and full‐text screening. The following variables were abstracted and recorded in an excel sheet: country, study design, methods, measurements, setting, population demographics (age, ethnicity, income, etc.), and reasons for alcohol use during pregnancy and/or breastfeeding. (See Table S1, Supporting Information). The abstracted data were then independently cross‐checked by a second investigator. Discrepancies at all stages were reconciled through team discussion. Non‐English language studies deemed to be potentially relevant were translated using Google Translate or by colleagues fluent in the respective language (and subsequently cross‐checked by a native speaker). Findings of studies related to the main outcome were entered verbatim into the data abstraction sheet.
Data analysis
Data were abstracted and analysed manually, without any advanced software. A thematic analysis approach [34, 35] was used to identify the most common themes in the studies, describing reasons of alcohol consumption during pregnancy and breastfeeding.
Data on alcohol use during pregnancy and breastfeeding were analysed separately. First, two reviewers (SAL and DD), independently abstracted and coded the data. The third reviewer (KB) crossed‐checked all corresponding data and coding. Then the researchers (SAL, DD and SP) discussed where codes appeared to overlap, consolidated and merged codes where necessary and agreed on the final theme structure.
Quantitative data were not coded but were included as part of the abstracted qualitative data, where applicable. Findings from qualitative data were interpreted based on the year and method of each study, as well as the economic and cultural context (e.g. lower‐middle income; collectivistic culture) [36] of each country, so as to separate individual and collective choices affecting alcohol use behaviour. Categorisations of individualistic and collectivistic cultures were adapted from Oyserman et al. [37].
Assessment of quality
The methodological quality assessment of each study (quantitative, qualitative and mixed) was done using the Mixed Methods Appraisal Tool (MMAT) [38] (See Table S2, Supporting Information). To summarise the confidence in cumulative evidence (all included studies), the Confidence in the Evidence from Reviews of Qualitative research (CERQual) [39] approach was used to assess the likelihood that the cumulative research findings represent real phenomena; each research finding was evaluated separately.
Results
A total of 3189 studies were identified in the search and screened at the title and abstract level. Of these, 183 articles were selected for full‐text screening, upon which a total of 42 studies were retained for data abstraction and thematic analysis. Forty studies examined women's alcohol consumption during pregnancy (22 qualitative studies; 2 mixed methods and 16 quantitative) and two qualitative studies focused exclusively on alcohol use during breastfeeding. A flow chart of the employed comprehensive search strategy is presented in Figure 1.
Figure 1.
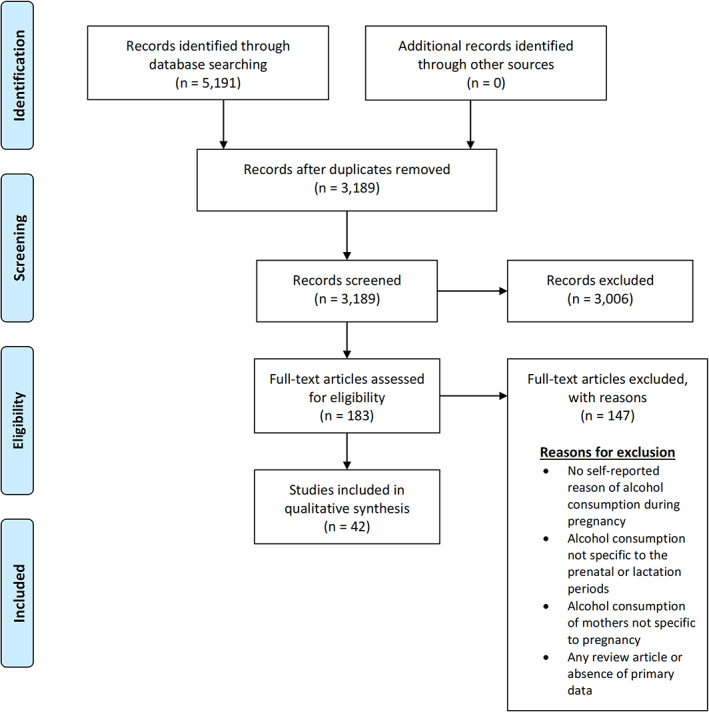
PRISMA flow diagram of search strategy and study selection.
Quality appraisal
The individual quality appraisals of the included studies (n = 42) using the Mixed Methods Appraisal Tool indicated that over half (26) had no methodological limitations and the remaining studies had minor to moderate limitations. Using the CERQual approach to assess the 12 review findings based on the thematic synthesis, four (33%) were ascertained to have high confidence, indicating they are an accurate representation of the phenomenon of interest. Three (25%) indicated moderate confidence, and an additional five (42%) were of low or low‐to‐moderate confidence.
Thematic synthesis findings
Reasons for consuming alcohol during pregnancy
The analysis identified four overarching themes that influenced alcohol consumption during pregnancy: individual beliefs; culture; knowledge/advice; and influence of pregnancy circumstances (Table 1).
Table 1.
Themes and subthemes: reasons for alcohol use during pregnancy and breastfeeding
| Alcohol use during pregnancy |
|---|
| Theme 1: Influence of individual beliefs |
|
|
|
| Theme 2: Influence of culture |
|
|
|
| Theme 3. Influence of knowledge and advice |
|
|
|
| Theme 4. Influence of pregnancy circumstances |
|
| Alcohol use during breastfeeding |
|
These themes are not mutually exclusive and often interacted with one another in women's experiences. Further, some themes were identified more prominently in certain countries. These core themes and their subthemes are discussed with illustrative examples from the literature. For detailed information on identified themes and subthemes presented within the structured CERQual approach, please see Table A1.
Theme 1: Influence of individual beliefs
Individual beliefs surrounding alcohol use in pregnancy were articulated by the women and described in the context of their environment and experiences. Women across countries cited their reasons for consuming alcohol as being tied to their beliefs about alcohol having beneficial properties, being harmful only in specific types and quantities, and as less damaging compared to other prenatal exposures.
Belief alcohol has beneficial properties
Women across several countries (Ghana, Australia, Brazil, India, USA, Nigeria, South Wales) personally believed that alcohol has beneficial properties that support maternal or fetal health [40, 41, 42, 43, 44, 45, 46, 47, 48]. In many cases, the individual belief surrounding specific benefits could be tied to cultural influences and knowledge the women had, demonstrating the linkages between those three overarching themes to understanding the reasons for consumption. Specifically, women identified such benefits as ‘cleaning’ the baby in the womb [41], developing the brain of the fetus [46] and improving fetal movements [48]. Women also indicated that alcohol reduced stress during pregnancy, helped with sleeping [42], and was a relaxant that would help with labour and delivery [43]. As one participant noted:
‘It relaxes you … which is true when I went into labor with my daughter they sent me home and said, 'Well, have a small glass of wine and it will help you ease a little'.’ [43]
Belief alcohol is harmful only in specific quantities and types
Women across countries (Ghana, Australia, France, UK, USA, Canada, Switzerland) believed that alcohol was not harmful to the fetus if consumed in small quantities or in the form of wine or beer [41, 44, 45, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64]. Women held the belief that alcohol consumed ‘in moderation’ or in low doses was acceptable. Similarly, they reasoned that wine and beer were less harmful to the pregnancy than were hard liquor or spirits, with 41% of women in one study identifying a greater risk to the fetus with hard alcohol than wine or beer [54]. Based on these individual beliefs, women justified their consumption of alcohol in low quantities, on an occasional basis only, or in the forms of wine or beer. For example, one woman noted:
‘I was of the view again based on some of the advice from my close friend that a small amount of alcohol is fine. In fact, there are some studies to suggest that small amounts of alcohol can actually be beneficial for childhood development.’ [58]
There was variation across individual beliefs regarding definitions of ‘harm’ or ‘moderation’. In some literature, women expressed it was safe to consume up to one or two drinks a week, with higher amounts potentially being risky [62]. Whereas, in another, 92.3% of women in their sample identified ‘it is harmful to the fetus if women drink more than five alcoholic drinks on a single occasion’ [65], which can be conceptualised as binge drinking. This particular belief of specific risk thresholds, or that certain amounts would be safe, was identified in most countries in the included studies, suggesting minimal influence by culture. One cultural variant was identified in this finding specific to Ghana and India, where women cited homemade spirits as being less harmful than other forms of alcohol [52].
Belief alcohol is less harmful than other prenatal exposures
In several studies, women held the individual belief that alcohol is less harmful than other substances, carcinogens, stressors or other harms [42, 44, 49, 65]. Women specifically identified alcohol as being less harmful than stress, second‐hand smoke, smoking and caffeine [49]. Women perceived alcohol as being safe because it acted as a relaxant and decreased stress levels during pregnancy [42]. Studies seemed to suggest that women bargained with themselves or justified alcohol use because they believed that alcohol is less harmful than other exposures or because they did not consume other drugs, so alcohol was permissible [62]. As one woman stated:
‘I sort of figured if I wasn't drinking any caffeine then maybe a tiny bit of wine is ok. That was my logic behind it, maybe not very good logic, but.’ [44]
Theme 2: Influence of culture
In this context, cultural influence can be understood as the collective shared customary beliefs, values, attitudes, and conventions that underpin women's alcohol consumption during pregnancy. Women often described their alcohol consumption as part of the social fabric of their life within their family units and the larger community, driven by cultural norms and values. Three subthemes emerged as reasons for consumption: social acceptability and pressure, alcohol as tradition and custom, and intuitive decision‐making influenced by personal/peer experiences, all driven by cultural norms and values. Some of the reasons specified were deeply rooted in cultural tradition and were more common in countries with a greater sense of tradition and collectivistic culture (e.g. Ghana, India, Bhutan) [36]. Other reasons were common across countries with collectivistic cultures and those with weaker tradition‐focused cultures, whereby there are more individualistic attitudes with fewer traditions and customs that guide behaviour (e.g. USA, Canada, Australia) [36].
Social acceptability and pressure for consumption of alcohol
One of the most consistent reasons for consuming alcohol when pregnant regardless of location or study group (e.g. Australia, Ghana, Switzerland, UK, USA, India, South Africa) was linked to the social acceptability of consuming alcohol and social pressure to consume alcohol when pregnant [43, 45, 49, 50, 52, 55, 61, 62, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75]. In many cases, drinking alcohol was socially acceptable and part of everyday social life [67]. As one woman noted:
‘Drinking during pregnancy is very common because my other friends were also drinking while they were pregnant. I also know of many women who are drinking, and they are still pregnant, especially in [this community].’ [74]
Alcohol was part of celebratory events and there was a social obligation to consume alcohol during these events [68]. Some women noted that their partner or friends and family encouraged them to drink alcohol [50, 66, 70]. The acceptability of consuming alcohol in the diverse cultures and countries identified in the review created social pressures either directly from family, friends and community or indirectly through a feeling of obligation to consume alcohol while pregnant. In many cases, the women noted that they had consumed alcohol in front of family, friends and community, without receiving any negative feedback [73]. In some cases, when the women refused alcohol, they experienced direct pressure to consume from friends and family [72]. Women also reported consuming alcohol to maintain social connections with friends and family, fearing they would lose the connections because of their transition to motherhood [74]. The consistency of this finding in the literature speaks to the powerful influence of the cultural and social context on alcohol use.
Alcohol as tradition and custom
The second subtheme within the influence of culture included reasons for consuming alcohol that were directly tied to the tradition and customs of specific cultural groups [40, 52, 65]. This theme was predominantly noted in collectivistic cultures with strong traditions in locations such as Ghana, Bhutan and India [36]. Women described drinking specific cultural beverages during their pregnancy, such as ‘changkey’ [65], herbal brews [40] or ‘handia’ [52]. These specific alcoholic beverages had cultural and traditional significance and were part of honouring tradition and custom in their cultures. Pregnant women drank alcohol as part of specific cultural events such as during worship or in celebrations of life (birth) and death [52]. As one participant noted:
‘Tradition for celebrating birth, as part of our lifestyle, eating and drinking during bonga (worship).’ [52]
Although tradition and custom as a reason for consumption were not indicated by women in more individualistic cultures, for those women located in countries with more collectivistic cultures with strong traditions, the significance of custom and tradition overpowered the relative importance of abstinence during pregnancy. In these cases, a cultural or traditional violation was perceived as more damaging than alcohol consumption.
Intuitive decision‐making based on personal and peer experiences
The final theme linked to culture was a reason for consuming alcohol that was reliant on the autonomy women felt for intuitive decision‐making, based on personal and peer experiences [42, 50, 52, 53, 58, 63, 68, 76]. This theme was more prevalent in countries with individualistic cultures (Canada, USA, Australia, UK) where women positioned themselves in control over their decision to consume alcohol during pregnancy. Women in these studies expressed the importance of being able to decide for themselves whether to consume and how much to consume, noting their sense of self and bodily awareness [68]. In some cases, women used previous pregnancies and experiences as a benchmark in their choice for consumption and quantity of consumption [63]. Other women observed family and friends to have consumed alcohol and had healthy pregnancies and stated this was part of their choice to consume [42], noting the important influence of the culture around alcohol use in general and during pregnancy. In addition, women stated their choice to consume was a result of wanting to enjoy and maintain a pleasurable aspect of their life [53]. As one woman noted:
‘I'd give myself a break and not give up everything that I enjoy so the odd glass of wine I thought was fine.’ [76]
As a result, the reasons women self‐identified for consumption were around their autonomy as the mother to make decisions for herself or her child on the safety and moderation of consumption. In some studies, this was expressed regretfully after the pregnancy, as one woman stated:
‘[I drank during my pregnancy because] I believed that nothing would happen to my baby, maybe I was in denial or something.’ [67]
Theme 3: Influence of knowledge and advice
The third overarching theme describing the reasons women self‐identified for consuming alcohol during pregnancy is summarised as the knowledge and advice the women had or received related to alcohol and pregnancy. The specific reasons within this theme also incorporated components of beliefs and culture, demonstrating the nonlinearity of reasons for alcohol consumption.
Consumption of alcohol for other health conditions in pregnancy
Women reported reasons for consuming alcohol as a remedy to other health conditions during pregnancy [40, 46, 47]. This theme was more common in countries with more collectivistic cultures (e.g. Ghana, Nigeria, India) [36]. It was also tied to women's belief in the ability of the alcohol to act as a remedy, in their knowledge, and a result of the advice of others in their community. Women reported consuming alcohol for abdominal problems, fever, gynecological conditions [40], relieving nausea and vomiting, improving appetite [46] and for prolonged labour as a pain reliever [47]. The women identified the reasons for consumption as appropriate because of the ability of alcohol to relieve other, painful health conditions. As one woman stated:
‘Palm wine is medicinal. Like a pregnant woman… it is used for making drugs for her.’ [47]
Insufficient awareness/knowledge of the adverse impacts of alcohol and FASD
Women across Australia, Bhutan, Canada, Switzerland, UK, Denmark and the USA attributed alcohol consumption in pregnancy as being due to a lack of awareness or lack of belief in its adverse effects, including FASD [42, 44, 45, 50, 59, 60, 64, 68, 77]. Pregnant women were unaware of the impact of PAE and thus, did not alter their drinking behaviours [44, 65]. In some studies, although women stated awareness of some potential adverse effects, they expressed being unconvinced about this risk overall or did not believe there was sufficient evidence or guidelines to justify completely abstaining from alcohol [42, 50, 58]. While describing their reasoning, women also indicated the lack of evidence in favour of total abstinence [58] and lack of minimum threshold for alcohol use [49]. As one woman noted:
‘The alcohol thing changes all the time doesn't it? Like I think with (previous pregnancy) it was a nono and I think now you can have one, they don't recommend it obviously…’ [45]
Advice from medical practitioners
Women also identified reasons for consuming alcohol during pregnancy that were related to advice from medical practitioners (doctors, midwives) or pregnancy resource documents (pamphlets, books). This theme was more prevalent in individualistic and largely European‐influenced cultures (England, Sweden, Australia, USA). Women noted that in some cases their physicians or midwives stated alcohol was permissible [44, 76]. Women were relying on the knowledge and advice of trusted health professionals or guidelines and tended to follow that advice to supplement their knowledge. In one study, women had an increased likelihood of drinking after reviewing guidelines that noted it was permissible [76]. Women indicated they found it difficult to navigate the conflicting advice they received from sources, noting some practitioners and books said alcohol in small quantities was not harmful, while others highlighted the importance of abstinence [63]. As one woman noted:
‘Some books say you should avoid it all together and others say it's OK to perhaps have one glass. So even in the pregnancy books you get a confusing message.’ [63]
Other women provided reasons for consumption related to their medical practitioners not explicitly stating that alcohol should be avoided or being asked about their consumption during appointments [62].
Theme 4: Influence of pregnancy circumstances
The final overarching theme of the influence of pregnancy circumstances included three subthemes for alcohol consumption: using alcohol as a coping mechanism, alcohol dependence, and unplanned or unwanted pregnancy. Many psychosocial factors may affect patterns of alcohol use in pregnancy, which may interact with individual beliefs, individual knowledge about its impacts, and social norms related to alcohol consumption. In this review, several studies were identified wherein women explicitly stated specific psychosocial and environmental factors, and therefore circumstances of their pregnancy, as influencing their decision to consume alcohol during pregnancy.
Using alcohol as a coping mechanism in response to adverse events during the pregnancy
Within several studies, women from Ghana, South Africa, England and the USA reported consuming alcohol during pregnancy as a coping mechanism [63, 66, 67, 70, 71, 72, 74, 78, 79]. The use of alcohol as a coping mechanism reflects common harmful, cultural narratives that attribute alcohol as being helpful during grief or trauma, which then impact resilience and healing. In many cases, women utilised alcohol as a coping mechanism through some very significant and horrific circumstances during their pregnancy such as family violence, mental illness, or familial conflict [67, 72, 78]. Specifically, women experiencing adverse circumstances related to abuse noted they used alcohol as the only way to cope with the abuse [67]. Others described their use of alcohol as a coping mechanism to get through the pregnancy itself [74], due to life pressure or emotional stress from events that occurred during the pregnancy [63, 66] such as the death of a partner [71]. As one woman stated when her partner was unfaithful to her during her pregnancy:
‘It hurt a lot. That's why I drank. . .Then I pass out and forget for that moment.’ [70]
Women expressed being aware of the impacts of alcohol but required alcohol to cope with their circumstances.
Alcohol dependence
A few studies (USA and South Africa) explicitly mentioned alcohol use problems as being related to PAE. In a study of birth mothers of children with Fetal Alcohol Syndrome, 84% felt they had a problem with alcohol use [78]. Similarly, it was found that some pregnant women used drinking to relieve a range of negative psychological symptoms and were dependent on alcohol use to alter mood and perception [72]. Unfortunately, alcohol treatment may not be sought by this population for several reasons, including not wanting to give up alcohol; fears of child apprehension; lack of access to child care; and lack of support from their partner to seek treatment [78]. Watt et al. [74] suggest that women were physiologically driven by alcohol addiction, with one woman stating ‘I drink too much… I never intended to become this way.’
Unplanned or unwanted pregnancy
Women's awareness of pregnancy and/or pregnancy planning was also found to have influenced alcohol consumption [55, 67, 71, 74]. In a study by Miller et al. [71], the unexpectedness of the pregnancy had influenced one woman to drink, prior to the sudden passing of her partner, which contributed to further alcohol use. In another study [67], one woman explained that she did not know she was pregnant, but also did not stop or cut down drinking when she found out about the pregnancy. Similarly, some women stated they were willing to drink until they found out for sure that they were pregnant [55].
Feelings about the respective pregnancy also influenced alcohol consumption. Some pregnant women who drank alcohol were lacking attachment to the pregnancy and resistant to motherhood, or not being ready to accept the pregnancy [55, 67, 74]. As one woman stated:
‘Yes, I was still drinking. I didn't care about this child. It was almost as if I hated this child. So whether I was drinking or not, I didn't care.’ [67]
In some cases, the pregnancy was unwanted and alcohol was used as an extreme means to abort the baby [55, 67, 74].
Reasons for consuming alcohol while breastfeeding
Only two studies looked exclusively at women's reasons for consuming alcohol while breastfeeding [80, 81]. One study found that women consumed alcohol to increase or stimulate the production of breast milk [80]. Another study reported that women received unclear advice from medical practitioners or they simply were not aware of the risks of infant exposure to alcohol or used alcohol to improve mood and celebrate events [81]. Some women understood the negative consequences of infants' exposure to alcohol through breast milk and attempted to minimise the effect to the baby, but inevitably exposed the baby due to unpredictable eating and sleeping patterns of the baby during a time in which alcohol was consumed [81].
Discussion
This systematic review sought to summarise women's self‐identified reasons for consuming alcohol while pregnant or breastfeeding. Four overarching themes were identified: individual beliefs, culture, knowledge/advice and personal circumstances of the pregnancy. The rationales in many cases were influenced by one another to contribute to the specific self‐identified reasons for alcohol use. Thus, women's reasoning for consuming alcohol during pregnancy is multifaceted and complex. The most common self‐identified motivation was the belief that only strong types (liquor as opposed to wine or beer) or large quantities of alcohol may be harmful. Other reasons included: a lack of awareness of adverse effects on the fetus; coping with adverse life experiences; consumption based on intuitive decision‐making and influenced by personal/peer experiences; belief in the beneficial properties of alcohol; advice from medical practitioners; unwanted or unplanned pregnancy; alcohol dependence; and consumption as a cultural/traditional custom.
Although only a handful of studies reported reasons for alcohol use during breastfeeding, it was found that women believed that alcohol stimulates the production of breast milk, received unclear advice from medical practitioners, were unaware of the risks of infant exposure and/or consumed alcohol to improve mood and celebrate events.
Based on the CERQual assessments of confidence in the evidence, ‘misconceptions about safe amounts/forms of alcohol during pregnancy’, ‘societal pressure to drink alcohol’, and ‘lack of awareness of harmful effects’ were rated as ‘high confidence’ demonstrating accurate representation of the phenomena examined in this review. ‘The consumption of alcohol to cope with adverse life experiences’ and ‘consumption based on experiences and intuitive decision‐making’ were rated as ‘moderate confidence’, meaning likely accurate representation of the phenomena.
Strengths of this review include its incorporation of research from a variety of countries published in several different languages, as well as the inclusion of articles with a range of methodologies (e.g. quantitative and qualitative), thus improving the breadth of included information. The limitations of this review include the lack of information in reviewed studies regarding important social determinants of health such as socio‐economic status and racial marginalisation. Also, included studies ranged in their date of publication, and women's opinions and beliefs may have changed over time due to public health messaging, education, level of economic development, shifting gender roles, social acceptability of drinking among women and alcohol marketing.
Women receive mixed messages about the harmful effects of PAE and various maternal drinking thresholds [82]. However, extant research has demonstrated that even small amounts of alcohol can significantly increase the risk of FASD [83]. Unfortunately, many countries are lacking in large‐scale FASD education and prevention efforts [84], which may contribute to a lack of awareness about the detrimental effects of alcohol among prenatal care providers, as well as pregnant women and their partners, families and communities.
Several motives for alcohol consumption in pregnancy found in this review are similar to what has been described in the general population, including social pressure, coping with stress, and pre‐existing substance abuse [28, 85, 86, 87]. Social motives and pressures to drink occur across a wide range of groups and populations [86, 88], and pregnant women are clearly not immune to or exempt from these influences. As well, research with both young [87] and middle‐aged [88] women and men has shown that consuming alcohol to cope with stress is a common challenge across age groups and gender.
Congruent with the theme of drinking due to stress, women who drink in pregnancy report more mental health problems and a greater incidence of abuse/violence compared to women who do not drink [21, 32]. Not surprisingly, this review found that pre‐existing substance abuse/dependence problems influenced alcohol consumption in pregnant women (as they do in other groups), again highlighting the importance of early screening and addiction treatment for women of childbearing age. Unfortunately, pregnant or breastfeeding women with alcohol or substance dependence may not seek treatment due to stigma or fears of child apprehension [89], which may only precipitate other adverse life circumstances for them. Furthermore, much of the literature and clinical practice related to maternal alcohol use is focused on reducing risk to the child [58, 90, 91]; however, women's wellbeing and the underpinnings of alcohol and substance use must also be addressed to sufficiently prevent prenatal alcohol exposure.
The behaviour of pregnant women is influenced by broader cultural and contextual norms. As a broad cultural force, the media also has a significant effect on alcohol use behaviour in general [92] and in pregnancy [82]. It is important to note that differences in motivations to consume alcohol in pregnancy may vary from country to country, but emerging information on social media or other media forms may exert a powerful, international influence on maternal alcohol use behaviour [92]. Additionally, population‐based studies of alcohol consumption patterns show shifts in the collective population's consumption which can result in shifts in individual consumption [93, 94], supporting the importance of public health measures such as reduced alcohol advertising and educational campaigns to decrease overall consumption.
Maternal alcohol use is affected by many contextual and personal factors that must be understood on a clinical and population level so as to prevent alcohol use and prevent new cases of FASD. First, this review shows there are common misconceptions surrounding alcohol use during pregnancy that must be addressed. Currently, many countries, especially low‐ and middle‐income, lack obstetric guidelines explicitly promoting alcohol abstinence and these must urgently be developed. The broader population must receive accurate information regarding the teratogenic effects of alcohol, including a clear, consistent message that there is no safe type or amount of alcohol to consume during any point of pregnancy. This would refute common existing myths identified in the current review, such as the idea that some types or amounts of alcohol are safer, healthier or even not harmful to the mother and child. Even in countries where guidelines do exist (e.g. USA or Australia), there is still maternal alcohol use, and health care providers can work further to provide the appropriate screening and education for women at risk of alcohol‐exposed pregnancies, to ensure that women are aware of such guidelines. Women and girls of reproductive age must be educated on the negative consequences of alcohol use during pregnancy or breastfeeding while being empowered to navigate an environment where there are many mixed messages. Furthermore, providing this education on a population level may work to decrease societal pressure on women to drink alcohol when they are pregnant, at risk of becoming pregnant or while breastfeeding.
In cultures where pregnant or breastfeeding women feel pressured to consume alcohol, or alcohol is often used as part of celebrations or daily rituals, for example, women and girls can be provided with communication strategies to refuse alcoholic drinks in social settings if this is their choice. Women should also be provided with the opportunity to discuss their prepregnancy alcohol use patterns, during pregnancy and postpartum with their health‐care providers, in which they can be offered non‐judgemental support and access to treatment programs if needed. Of course, this is dependent not only on women's communication strategies, but also the training and practices of health‐care providers related to this topic. Supporting alcohol‐free pregnancies begins with routine alcohol use screening in pregnancy and engaging with women in conversations about factors affecting their alcohol intake while providing a clear message about the importance of abstinence. Care providers should strive to understand individual patient circumstances, which may affect PAE, such as the pregnancy being unplanned, so they may effectively provide appropriate advice and support during the prenatal and postpartum periods. For example, providers should routinely screen women with substance use disorders for alcohol use in pregnancy in a supportive, non‐punitive manner and facilitate access to brief interventions and specialised treatment services [95, 96]. Simply asking pregnant women about their alcohol use can increase awareness of the adverse effects of alcohol and can change alcohol use behaviour [97, 98]. Care providers are also in a position to inform women who consume alcohol about effective contraception, to assist them in developing healthy coping mechanisms, to refer women to mental health services, as well as to involve partners/families in supporting alcohol‐free pregnancies and lactation. This can facilitate healthy decision‐making, access to brief interventions if they are needed, and has the potential to reduce PAE and FASD.
Interventions must be designed to account for the local context of alcohol use during pregnancy, such as cultural traditions related to alcohol use. Such interventions can encourage cultural practices while educating women about the risks of alcohol use during pregnancy and while breastfeeding. Alternatives to cultural traditions involving maternal alcohol use can be explored, and where abstinence from alcohol is not possible, health‐care providers should encourage a significant reduction in alcohol use. Of course, such services necessitate secure access to holistic prenatal care, including prevention and substance use treatment services with respect of confidentiality and privacy and preventing stigmatisation, discrimination and marginalisation. As this review found, some women use alcohol to cope with adverse life circumstances during pregnancy, which is in accordance with the finding that women who experience violence [28], for example, are more likely to consume alcohol during pregnancy. Interventions must be designed to address not only societal factors, but the underpinnings of substance use which include targeting psychosocial stressors for pregnant women.
Public awareness campaigns must work synchronously to reduce stigma related to alcohol use in pregnancy and mothers of children with FASD, while also increasing awareness of the adverse impacts of PAE and promoting social environments that are supportive of abstinence from alcohol for men and women. This and the above strategies are all crucial for reducing or eliminating PAE and thus, the prevention of FASD and other adverse maternal and child health outcomes.
Future research should compare the predictors and patterns of women's alcohol use during pregnancy and breastfeeding across varying cultural contexts with consideration of individual and societal‐level variables. This information will inform the design and implementation of targeted and effective prevention initiatives of maternal alcohol consumption and, thus, reduce FASD and other negative outcomes in children, worldwide.
Conflict of Interest
All authors declare that they do not have any financial, personal, political, intellectual or religious competing interests relevant to this article to disclose.
Supporting information
Appendix S1: Supporting information for methodology.
Table S1: Summary of the included studies.
Table S2: Quality assessment of the included studies using Mixed Methods Appraisal Tool.
Acknowledgements
We would like to thank Jiaying Chen for their assistance with the literature search in the early stages of this project.
Appendix A.
Table A1.
CERQual evidence profile
| Summary of review finding | Studies contributing to the review finding | Countries included in studies | Methodological limitations | Coherence | Adequacy of data | Relevance | CERQual assessment of confidence in the evidence | Explanation of CERQual assessment |
|---|---|---|---|---|---|---|---|---|
| Alcohol use during pregnancy | ||||||||
Consumption affected by the belief that alcohol in pregnancy is only harmful in specific forms and/or quantities (n = 20):
|
[41, 44, 45, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65] | Ghana, Canada, USA, France, India, UK, Australia, Switzerland, Denmark, Israel, Bhutan | Moderate methodological limitations: seven studies with inadequate or missing information about outcome data or sampling methodology | No or very minor concerns about coherence | Moderate concerns about adequacy of data in seven studies | No or minor concerns about relevance | High confidence | Seven studies (out of 20) with moderate limitations regarding adequacy of data or missing relevant information. Data available from 10 countries which includes five continents. |
Experiences of social pressure to consume alcohol and/or social acceptability of alcohol use (n = 18)
|
[43, 45, 49, 50, 52, 55, 61, 62, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75] | Canada, USA, Australia, Brazil, Ghana, Switzerland, UK, India, South Africa | Minor methodological limitations: three studies with missing information to substantiate findings; two studies with minor concerns about design and analysis of outcome data. | No or very minor concerns about coherence | Minor concerns about adequacy of data in five studies | No or minor concerns about relevance | High confidence | Five studies (out of 18) with minor concerns regarding adequacy of data. Data available from nine countries across five continents. |
| Consumption of alcohol due to lack of awareness/knowledge on harmful effects and FASD, or unconvinced of available evidence (n = 9) | [42, 44, 45, 50, 59, 60, 64, 68, 77] | USA, Australia, Switzerland, UK, Denmark, Bhutan, Canada | Minor methodological limitations: two studies with inadequate information on methodology and data synthesis; one study with incomplete data presented. | No or very minor concerns about coherence | Minor concerns about adequacy of data in 3 studies | No or minor concerns about relevance | High confidence | Three studies (out of 10) with very minor concerns regarding adequacy of data due to missing information. Data is presented from seven countries across four continents. |
Consumption of alcohol to cope with adverse life experiences (n = 9), including:
|
[63, 66, 67, 70, 71, 72, 74, 78, 79] | USA, Ghana, South Africa, UK | Minor methodological limitation in one included quantitative randomised study (MMAT) due to inadequate control for confounders. | No or very minor concerns about coherence | No or very minor concerns about adequacy of data in one study | Minor concerns about relevance | Moderate confidence | One study (out of 10) has a methodological limitation in the control of quantitative data. Study data are included from four countries, though two are in Africa. |
Consumed alcohol based on intuitive decision‐making and personal/peer pregnancy experiences (n = 8)
|
[42, 50, 52, 53, 58, 63, 68, 76] | Australia, Switzerland, India, UK, USA, Canada, England, Sweden |
Minor methodological limitations: one study has inadequate information about data synthesis, one study has concerns with outcome data and sampling methodology. |
No or very minor concerns about coherence | Minor concerns about adequacy of data | Minor concerns about relevance | Moderate confidence | Two out of eight studies have minor methodological limitations with adequacy of data. Study data are available from eight countries in three continents but are limited to high income countries. |
Consumption of alcohol in pregnancy with the belief that it has beneficial properties (n = 6), including:
|
[41, 42, 43, 44, 45, 48] | Ghana, USA, Australia, UK, Brazil, India | Minor methodological limitations: one study has inadequate information about sampling methodology and data synthesis; one study has an identified risk of nonresponse bias. | No or very minor concerns about coherence | Moderate concerns about adequacy of data | No or minor concerns about relevance | Low to moderate confidence | Two studies (out of seven) have moderate methodological limitations. Data are available from six countries across six continents. |
Medical practitioners did not provide advice on alcohol in pregnancy or provided mixed advice (n = 4)
|
[56, 62, 63, 76] | England, Sweden, USA, Australia | No methodological limitations identified. | No or very minor concerns about coherence | No or very minor concerns about adequacy of data | No or minor concerns about relevance | High confidence | No methodological limitations identified. Study data are available from four countries in three continents, though these are only high‐income countries. |
| Consumption of alcohol related to the pregnancy being unwanted or unplanned (n = 4) | [55, 67, 71, 74] | South Africa, USA | No methodological limitations identified. | Moderate concerns about coherence. | No or very minor concerns about adequacy of data | Minor concerns about relevance | Moderate confidence | No methodological limitations identified. Study data are available from two high‐income countries in two continents. |
Consumption of alcohol is less harmful than other exposures (n = 4)
|
[42, 44, 49, 65] | Canada, Bhutan, Australia | Moderate methodological limitation in one study with an identified risk of non‐response bias in the methodology. | No or very minor concerns about coherence | Moderate concerns about adequacy of data | Moderate concerns about relevance | Low confidence | One study (out of four) has a moderate methodological limitation. Study data are from three countries in three continents. |
| Alcohol dependence during the time of pregnancy (n = 3) | [72, 74, 78] | South Africa, USA | Minor methodological limitation identified in one study: confounders not accounted for in design/analysis. | No or very minor concerns about coherence | Very minor concerns about the adequacy of the data | Moderate concerns about the relevance | Low confidence | One study (out of three) has a methodological limitation. Study data are exclusively derived from two high‐income countries from two different continents. |
Consumption of alcohol for other health conditions in pregnancy (n = 3), including:
|
[40, 46, 47] | Ghana, Nigeria, India | Minor methodological limitation identified in one study: inadequate information to assess risk of bias in sampling methodology and study data collection. | No or very minor concerns about coherence | No or very minor concerns about adequacy of data | Moderate concerns about relevance | Low confidence | One study (out of three) has a minor methodological limitation. Study data are derived exclusively from India and two west African countries. |
Consumption of alcohol as part of a cultural tradition, ritual or custom (n = 3)
|
[40, 52, 65] | Ghana, India, Bhutan | Moderate methodological limitation in one study with an identified risk of non‐response bias in the methodology. | No or very minor concerns about coherence | Moderate concerns about adequacy of data | Moderate concerns about relevance | Low confidence | One study (out of three) has a moderate methodological limitation. Study data are derived exclusively from Ghana and two South Asian countries. |
| Alcohol use during breastfeeding | ||||||||
Consumption of alcohol while breastfeeding (n = 2)
|
[80, 81] | Australia, Brazil | Moderate methodological limitation in one study where information is lacking to assess two risks of bias. | Moderate concerns about coherence | Minor concerns about the adequacy of data | Minor concerns about relevance | Low confidence | One study (of two) has a moderate methodological limitation. Study data are derived from Australia and one South American country. |
CERQual, Confidence in the Evidence from Reviews of Qualitative research; FASD, Fetal Alcohol Spectrum Disorder; MMAT, Mixed Methods Appraisal Tool.
Svetlana Popova MD, MPH, PhD, Senior Scientist, Centre for Addiction and Mental Health and Professor, University of Toronto, Danijela Dozet MPH, Research Analyst, Centre for Addiction and Mental Health and PhD Student, Institute of Medical Science, Shahela Akhand Laboni MBBS, MSc, Researcher III, Krista Brower, PhD (C), MEd, CE, PhD Candidate, Department of Educational Research, Valerie Temple PhD, Clinical Psychologist.
References
- 1. World Health Organization . Guidelines for the identification and management of substance use and substance use disorders in pregnancy. Geneva: World Health Organization, 2014. [PubMed] [Google Scholar]
- 2. Graves L, Carson G, Poole N et al. Guideline no. 405: screening and counselling for alcohol consumption during pregnancy. J Obstet Gynaecol Can 2020;42:1158–1173.e1. [DOI] [PubMed] [Google Scholar]
- 3. Popova S, Lange S, Probst C, Gmel G, Rehm J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta‐analysis. Lancet Glob Health 2017;5:e290–9. [DOI] [PubMed] [Google Scholar]
- 4. Lebel C, Roussotte F, Sowell ER. Imaging the impact of prenatal alcohol exposure on the structure of the developing human brain. Neuropsychol Rev 2011;21:102–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Henriksen TB, Hjollund NH, Jensen TK et al. Alcohol consumption at the time of conception and spontaneous abortion. Am J Epidemiol 2004;160:661–7. [DOI] [PubMed] [Google Scholar]
- 6. Nykjaer C, Alwan NA, Greenwood DC et al. Maternal alcohol intake prior to and during pregnancy and risk of adverse birth outcomes: evidence from a British cohort. J Epidemiol Community Health 2014;68:542–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O'Connor MJ, Kogan N, Findlay R. Prenatal alcohol exposure and attachment behavior in children. Alcohol Clin Exp Res 2002;26:1592–602. [DOI] [PubMed] [Google Scholar]
- 8. Patra J, Bakker R, Irving H, Jaddoe VWV, Malini S, Rehm J. Dose–response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)—a systematic review and meta‐analyses. BJOG 2011;118:1411–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lange S, Probst C, Rehm J, Popova S. Prevalence of binge drinking during pregnancy by country and World Health Organization region: systematic review and meta‐analysis. Reprod Toxicol 2017;73:214–21. [DOI] [PubMed] [Google Scholar]
- 10. Popova S, Lange S, Probst C, Gmel G, Rehm J. Global prevalence of alcohol use and binge drinking during pregnancy, and fetal alcohol spectrum disorder. Biochem Cell Biol 2018;96:237–40. [DOI] [PubMed] [Google Scholar]
- 11. Greenmyer JR, Klug MG, Kambeitz C, Popova S, Burd L. A multicountry updated assessment of the economic impact of fetal alcohol spectrum disorder: costs for children and adults. J Addict Med 2018;12:466–73. [DOI] [PubMed] [Google Scholar]
- 12. Popova SL, Lange S, Burd L, Rehm J. The economic burden of fetal alcohol spectrum disorder in Canada in 2013. Alcohol Alcohol 2016;51:367–75. [DOI] [PubMed] [Google Scholar]
- 13. Stade B, Ali A, Bennett D et al. The burden of prenatal exposure to alcohol: revised measurement of cost. Can J Clin Pharmacol 2009;16:e91–102. [PubMed] [Google Scholar]
- 14. LactMed, Drugs and Lactation Database . National Library of Medicine. Bethesda, MD: LactMed, Drugs and Lactation Database, 2006. [Google Scholar]
- 15. Popova S, Lange S, Rehm J. Twenty percent of breastfeeding women in Canada consume alcohol. J Obstet Gynaecol Can 2013;35:695–6. [DOI] [PubMed] [Google Scholar]
- 16. Genna CW. Alcohol use during lactation and offspring outcomes. Clin Lactat 2019;10:81–6. [Google Scholar]
- 17. May PA, Hasken JM, Blankenship J et al. Breastfeeding and maternal alcohol use: prevalence and effects on child outcomes and fetal alcohol spectrum disorders. Reprod Toxicol 2016;63:13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization . Global status report on alcohol and health, 2018. Geneva: World Health Organization, 2018. [Google Scholar]
- 19. Bearak J, Popinchalk A, Alkema L, Sedgh G. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a Bayesian hierarchical model. Lancet Glob Health 2018;6:e380–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Johnson AK, Fulco CJ, Augustyn MB. Intergenerational continuity in alcohol misuse: maternal alcohol use disorder and the sequelae of maternal and family functioning. Psychol Addict Behav 2019;33:442–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cafferky BM, Méndez M, Anderson JR, Stith S. Substance use and intimate partner violence: a meta‐analytic review. Psychol Violence 2018;8:110–31. [Google Scholar]
- 22. Stanesby O, Cook M & Callinan S. Examining trends in alcohol consumption during pregnancy in Australia, 2001 to 2016. Canberra: Foundation for Alcohol Research and Education; 2018.
- 23. England LJ, Benett C, Denny CH et al. Alcohol use and co‐use of other substances among pregnant females aged 12‐44 years ‐ United States, 2015‐2018. MMWR Morb Mortal Wkly Rep 2020;69:1009–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kar P, Tomfohr‐Madsen L, Giesbrecht G, Bagshawe M, Lebel C. Alcohol and substance use in pregnancy during the COVID‐19 pandemic. Drug Alcohol Depend 2021;225:108760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rodriguez LM, Litt DM, Stewart SH. Drinking to cope with the pandemic: the unique associations of COVID‐19‐related perceived threat and psychological distress to drinking behaviors in American men and women. Addict Behav 2020;110:106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sher J. Fetal alcohol spectrum disorders: preventing collateral damage from COVID‐19. Lancet Public Health 2020;5:e424–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smith CL, Waters SF, Spellacy D et al. Substance use and mental health in pregnant women during the COVID‐19 pandemic. J Reprod Infant Psychol 2021. [Epub ahead‐of‐print]. https://www.tandfonline.com/doi/full/10.1080/02646838.2021.1916815?scroll=top&needAccess=true. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Skagerstróm J, Chang G, Nilsen P. Predictors of drinking during pregnancy: a systematic review. J Womens Health (Larchmt) 2011;20:901–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lyall V, Wolfson L, Reid N et al. “The problem is that we hear a bit of everything…”: a qualitative systematic review of factors associated with alcohol use, reduction, and abstinence in pregnancy. Int J Environ Res Public Health 2021;18:3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wolfson L, Schmidt RA, Stinson J, Poole N. Examining barriers to harm reduction and child welfare services for pregnant women and mothers who use substances using a stigma action framework. Health Soc Care Commun 2021;29:589–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Drabble LA, Poole N, Magri R, Tumwesigye NM, Li Q, Plant M. Conceiving risk, divergent responses: perspectives on the construction of risk of FASD in six countries. Subst Use Misuse 2011;46:943–58. [DOI] [PubMed] [Google Scholar]
- 32. Popova S, Dozet D, O'Hanlon G, Temple V, Rehm J. Maternal alcohol use, adverse neonatal outcomes and pregnancy complications in British Columbia, Canada: a population‐based study. BMC Pregnancy Childbirth 2021;21:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 35. Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods 2017;16:1–13. [Google Scholar]
- 36. Bhullar N, Schutte NS, Malouff JM. Associations of individualistic‐collectivistic orientations with emotional intelligence, mental health, and satisfaction with life: a tale of two countries. Indiv Diff Res 2012;10:165–75. [Google Scholar]
- 37. Oyserman D, Coon HM, Kemmelmeier M. Rethinking individualism and collectivism: evaluation of theoretical assumptions and meta‐analyses. Psychol Bull 2002;128:3–72. [PubMed] [Google Scholar]
- 38. Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health 2014;35:29–45. [DOI] [PubMed] [Google Scholar]
- 39. Lewin S, Glenton C, Munthe‐Kaas H et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE‐CERQual). PLoS Med 2015;12:e1001895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Adeyiga G, Udofia EA, Yawson AE. Factors associated with alcohol consumption: a survey of women childbearing at a national referral hospital in Accra. Ghana Afr J Reprod Health 2014;18:152–65. [PubMed] [Google Scholar]
- 41. Adusi‐Poku Y, Edusei AK, Bonney AA, Tagbor H, Nakua E, Otupiri E. Pregnant women and alcohol use in the Bosomtwe district of the Ashanti region‐Ghana. Afr J Reprod Health 2012;16:55–60. [PubMed] [Google Scholar]
- 42. Anderson AE, Hure AJ, Kay‐Lambkin FJ, Loxton DJ. Women's perceptions of information about alcohol use during pregnancy: a qualitative study. BMC Public Health 2014;14:1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Branco EI, Kaskutas LA. "if it burns going down… ": how focus groups can shape fetal alcohol syndrome (FAS) prevention. Subst Use Misuse 2001;36:333–45. [DOI] [PubMed] [Google Scholar]
- 44. Crawford‐Williams F, Steen M, Esterman A, Fielder A, Mikocka‐Walus A. “My midwife said that having a glass of red wine was actually better for the baby”: a focus group study of women and their partner's knowledge and experiences relating to alcohol consumption in pregnancy. BMC Pregnancy Childbirth 2015;15:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Grant A, Morgan M, Mannay D, Gallagher D. Understanding health behaviour in pregnancy and infant feeding intentions in low‐income women from the UKthrough qualitative visual methods and application to the COM‐B (capability, opportunity, motivation‐behaviour) model. BMC Pregnancy Childbirth 2019;19:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mutihir J, Musa J, Daru P, Nyango D, Audu M. Substance abuse among antenatal patients at Jos university teaching hospital, north Central Nigeria. J West Afr Coll Surg 2012;2:50–62. [PMC free article] [PubMed] [Google Scholar]
- 47. Nwagu EN, Dibia SIC, Odo AN. Socio‐cultural norms and roles in the use and abuse of alcohol among members of a rural community in Southeast Nigeria. Health Educ Res 2017;32:423–36. [DOI] [PubMed] [Google Scholar]
- 48. Potukuchi PS, Rao PG. Problem alcohol drinking in rural women of Telangana region. Andhra Pradesh Indian J Psychiatr 2010;52:339–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. April N, Audet C, Guyon L, Gagnon H. Représentations sociales et consommation d'alcool pendant la grossesse. Drog Santé Soc 2010;9:17–48. [Google Scholar]
- 50. Barbour BG. Alcohol and pregnancy. J Nurse Midwifery 1990;35:78–85. [DOI] [PubMed] [Google Scholar]
- 51. Brahic J, Thomas O, Dany L. Alcool et grossesse: une recherche qualitative auprès de femmes enceintes. Les Cahiers Int Psychol Soc 2015;107:403–34. [Google Scholar]
- 52. Pati S, Chauhan AS, Mahapatra P, Hansdah D, Sahoo KC, Pati S. Weaved into the cultural fabric: a qualitative exploration of alcohol consumption during pregnancy among tribal women in Odisha. India Subst Abuse Treat Prev Policy 2018;13:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Coathup V, Smith L, Boulton M. Exploration of dietary patterns and alcohol consumption in pregnant women in the UK: a mixed methods study. Midwifery 2017;51:24–32. [DOI] [PubMed] [Google Scholar]
- 54. Dumas A, Toutain S, Hill C, Simmat‐Durand L. Warning about drinking during pregnancy: lessons from the French experience. Reprod Health 2018;15:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Elek E, Harris SL, Squire CM et al. Women's knowledge, views, and experiences regarding alcohol use and pregnancy: opportunities to improve health messages. Am J Health Educ 2013;44:177–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. France KE, Donovan RJ, Henley N et al. Promoting abstinence from alcohol during pregnancy: implications from formative research. Subst Use Misuse 2013;48:1509–21. [DOI] [PubMed] [Google Scholar]
- 57. Herzberg J, Barrier B, Sprague DJ, Vinson DC. Substance use in women of reproductive age. Mo Med 2016;113:182–6. [PMC free article] [PubMed] [Google Scholar]
- 58. Holland K, McCallum K, Walton A. ‘I'm not clear on what the risk is’: women's reflexive negotiations of uncertainty about alcohol during pregnancy. Health Risk Soc 2016;18:38–58. [Google Scholar]
- 59. Howlett H, Gray WK, Dismore L et al. A survey of attitudes, beliefs and practice regarding alcohol use and screening in pregnancy: an opportunity for support and education? J Res Nurs 2017;22:618–33. [Google Scholar]
- 60. Kesmodel U, Schiøler KP. Drinking during pregnancy: attitudes and knowledge among pregnant Danish women, 1998. Alcohol Clin Exp Res 2002;26:1553–60. [DOI] [PubMed] [Google Scholar]
- 61. Loxton D, Chojenta C, Anderson AE, Powers JR, Shakeshaft A, Burns L. Acquisition and utilization of information about alcohol use in pregnancy among australian pregnant women and service providers. J Midwifery Womens Health 2013;58:523–30. [DOI] [PubMed] [Google Scholar]
- 62. Meurk CS, Broom A, Adams J, Hall W, Lucke J. Factors influencing women's decisions to drink alcohol during pregnancy: findings of a qualitative study with implications for health communication. BMC Pregnancy Childbirth 2014;14:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Raymond N, Beer C, Glazebrook C, Sayal K et al. Pregnant women's attitudes towards alcohol consumption. BMC Public Health 2009;9:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Senecky Y, Weiss N, Shalev SA et al. Alcohol consumption during pregnancy among women in Israel. J Popul Ther Clin Pharmacol 2011;18:e261–72. [PubMed] [Google Scholar]
- 65. Udon P, Areesantichai C. Assessment of alcohol consumption among pregnant women in antenatal clinic (ANC) at Jigmi Dorji Wangchuk National Referral Hospital (JDWNRH), Thimphu. Bhutan J Health Res 2012;26:105–8. [Google Scholar]
- 66. Da Pilma LJ, Dako‐Gyeke P, Agyemang SA, Aikins M. Alcohol consumption among pregnant women in James town community, Accra. Ghana Reprod Health 2017;14:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Fletcher OV, May PA, Seedat S, Sikkema KJ, Watt MH. Attitudes toward alcohol use during pregnancy among women recruited from alcohol‐serving venues in Cape Town, South Africa: a mixed‐methods study. Soc Sci Med 2018;215:98–106. [DOI] [PubMed] [Google Scholar]
- 68. Hammer R, Inglin S. ‘I don't think it's risky, but…’: pregnant women's risk perceptions of maternal drinking and smoking. Health Risk Soc 2014;16:22–35. [Google Scholar]
- 69. Jones SC, Telenta J. What influences Australian women to not drink alcohol during pregnancy? Aust J Prim Health 2012;18:68–73. [DOI] [PubMed] [Google Scholar]
- 70. Kelly JF, Ward CL. Women who drank while pregnant: the importance of social context in the lives of south African pregnant women. Drugs Educ Prev Policy 2018;25:438–45. [Google Scholar]
- 71. Miller SM. Case studies: profiles of women recovering from drug addiction. J Drug Educ 1995;25:139–48. [DOI] [PubMed] [Google Scholar]
- 72. Rosett HL, Weiner L, Edelin KC. Treatment experience with pregnant problem drinkers. JAMA 1983;249:2029–33. [PubMed] [Google Scholar]
- 73. Oliveira T, Simões S. The alcoholic beverage consumption by the pregnant women: an exploratory study. Escola Anna Nery 2007;11:632–8. [Google Scholar]
- 74. Watt MH, Eaton LA, Choi KW et al. "It's better for me to drink, at least the stress is going away": perspectives on alcohol use during pregnancy among south African women attending drinking establishments. Soc Sci Med 2014;116:119–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Watt MH, Eaton LA, Dennis AC et al. Alcohol use during pregnancy in a South African community: reconciling knowledge, norms, and personal experience. Matern Child Health J 2016;20:48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Schölin L, Hughes K, Bellis MA, Charli Eriksson C, Porcellato L. Exploring practices and perceptions of alcohol use during pregnancy in England and Sweden through a cross‐cultural lens. Eur J Public Health 2018;28:533–7. [DOI] [PubMed] [Google Scholar]
- 77. Peadon E, Payne J, Henley N et al. Attitudes and behaviour predict women's intention to drink alcohol during pregnancy: the challenge for health professionals. BMC Public Health 2011;11:584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Astley SJ, Bailey D, Talbot C, Clarren SK. Fetal alcohol syndrome (FAS) primary prevention through FAS diagnosis: II. A comprehensive profile of 80 birth mothers of children with FAS. Alcohol Alcohol 2000;35:509–19. [DOI] [PubMed] [Google Scholar]
- 79. Jones TC, Modeste N, Anderson B, Lee J, Lim VJ. Factors influencing the intention to quit drinking alcohol among African American/black pregnant women. Calif J Health Promot 2007;5:131–44. [Google Scholar]
- 80. Lima MML, Silva TKR, Tsupal PA, De Freitas Melhem AR, Brecailo MK, Dos Santos EF. The influence beliefs and taboos in breastfeeding. O Mundo Saude 2016;40:221–9. [Google Scholar]
- 81. Giglia RC, Binns CW. Alcohol and breastfeeding: what do Australian mothers know? Asia Pac J Clin Nutr 2007;16:473–7. [PubMed] [Google Scholar]
- 82. Lim AWY, van Schalkwyk MCI, Maani Hessari N, Petticrew MP. Pregnancy, fertility, breastfeeding, and alcohol consumption: an analysis of framing and completeness of information disseminated by alcohol industry‐funded organizations. J Stud Alcohol Drugs 2019;80:524–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Chambers CD, Coles C, Kable J et al. Fetal alcohol Spectrum disorders in a Pacific Southwest City: maternal and child characteristics. Alcohol Clin Exp Res 2019;43:2578–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Poole N, Schmidt RA, Green C, Hemsing N. Prevention of fetal alcohol Spectrum disorder: current Canadian efforts and analysis of gaps. Subst Abuse 2016;10:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Abbey A, Smith MJ, Scott RO. The relationship between reasons for drinking alcohol and alcohol consumption: an interactional approach. Addict Behav 1993;18:659–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Cooper ML. Motivations for alcohol use among adolescents: development and validation of a four‐factor model. Psychol Assess 1994;6:117–28. [Google Scholar]
- 87. Fernandes‐Jesus M, Beccaria F, Demant J et al. Validation of the drinking motives questionnaire – revised in six European countries. Addict Behav 2016;62:91–8. [DOI] [PubMed] [Google Scholar]
- 88. Windle M, Windle RC. A prospective study of stressful events, coping motives for drinking, and alcohol use among middle‐aged adults. J Stud Alcohol Drugs 2015;76:465–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice 2015;3:1–15. [Google Scholar]
- 90. Lupton D. 'Precious cargo': foetal subjects, risk and reproductive citizenship. Crit Public Health 2012;22:329–40. [Google Scholar]
- 91. Leppo A. The emergence of the foetus: discourses on foetal alcohol syndrome prevention and compulsory treatment in Finland. Crit Public Health 2012;22:179–91. [Google Scholar]
- 92. Pan American Health Organization . Technical note: background on alcohol marketing regulation and monitoring for the protection of public health. Washington, D.C: Pan American Health Organization, 2017. [Google Scholar]
- 93. Landberg J, Trolldal B, Norström T. Is the theory of collectivity of drinking cultures valid across educational groups? Drug Alcohol Rev 2021;40:472–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Raninen J, Livingston M, Leifman H. Declining trends in alcohol consumption among Swedish youth‐does the theory of collectivity of drinking cultures apply? Alcohol Alcohol 2014;49:681–6. [DOI] [PubMed] [Google Scholar]
- 95. Corrigan PW, Lara JJ, Shah BB, Mitchell KT, Diana Simmes D, Jones KL. The public stigma of birth mothers of children with fetal alcohol spectrum disorders. Alcohol Clin Exp Res 2017;41:1166–73. [DOI] [PubMed] [Google Scholar]
- 96. Schölin L, Fitzgerald N. The conversation matters: a qualitative study exploring the implementation of alcohol screening and brief interventions in antenatal care in Scotland. BMC Pregnancy Childbirth 2019;19:316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Tzilos GK, Sokol RJ, Ondersma SJ. A randomized phase I trial of a brief computer‐delivered intervention for alcohol use during pregnancy. J Womens Health (Larchmt) 2011;20:1517–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Floyd RL, Sobell M, Velasquez MM et al. Preventing alcohol‐exposed pregnancies: a randomized controlled trial. Am J Prev Med 2007;32:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting information for methodology.
Table S1: Summary of the included studies.
Table S2: Quality assessment of the included studies using Mixed Methods Appraisal Tool.


