To the Editor: Wildfires are becoming more frequent and severe, causing increased air pollution exposure.1 Wildfire smoke has been associated with increased rates of clinic visits for atopic dermatitis (AD) and itch.1 We hypothesized that exposure to local wildfire air pollution would increase interest in skin-related topics, as detected by online search trends. They reflect shifts in population-level information-seeking behaviors related to short-term events that could indicate environmental impacts on skin health.
From June 1 to November 30, 2020 (wildfire season) and the corresponding months in 2016, when there were no nearby wildfires, we obtained daily particulate matter (PM2.5) concentration data from the only Bay Area Air Quality Monitoring District ground-level monitor in San Francisco, CA. We collected online search data for San Francisco from Google Trends: the daily aggregated search volume index (SVI) for terms pertaining to skin symptoms, skin diseases, and positive and negative controls. The SVI ranges from 0 to 100 (most interest) for each term according to its number of queries relative to that of other terms in a temporal and geospatial framework. SVI data have been used for health care research and validated against external data sets.2 Data for each term were collected on 3 days (December 15, 2021 and February 7 and 13, 2022) and found to be closely correlated: Spearman correlation coefficients >0.86. Multivariable linear regression was conducted to examine associations between PM2.5 and SVI, adjusting for temperature, relative humidity, and year.
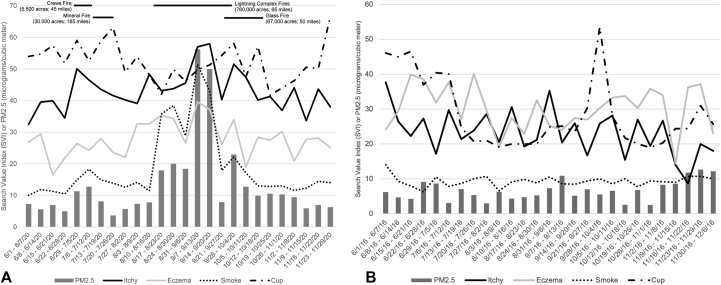
In 2020, mean weekly PM2.5 concentration increased 6-fold from baseline during the Lightning Complex fires, with concomitant increases in the SVI for selected skin disease and symptom search terms, compared to 2016 (Fig 1). In adjusted regression analyses (Table I), a 10 μg/m3 increase in mean weekly PM2.5 was associated with an increased mean weekly SVI of 2.9 (95% CI: 0.34-5.9) for “eczema,” 1.7 (0.1-3.8) for “acne,” 2.4 (0.78-4.1) for “itchy,” 1.9 (0.16-3.3) for “itchy skin,” and 2.2 (0.45-4.8) for “red skin.”
Fig 1.
Average weekly air pollution (PM2.5) in San Francisco and search volume index (SVI) for representative search terms. A, The San Francisco search volume index for representative positive control (“smoke”), negative control (“cup”), and skin (“eczema” and “itchy”) search terms in 2020. The horizontal lines at the top correspond to the dates on the x-axis to indicate the time frame of wildfires as well as the approximate number of acres burned and distance from San Francisco. Bars represent the concentration of particulate matter (PM2.5) in micrograms/cubic meter, and lines represent the search volume index for representative terms in each category: symptoms, diseases, and controls. B, The San Francisco search volume for representative positive control (“smoke”), negative control (“cup”), and skin (“eczema” and “itchy”) search terms in 2016. No wildfires affected San Francisco air quality during this year. Bars represent the concentration of particulate matter (PM2.5) in micrograms/cubic meter, and lines represent the search volume index for representative terms in each category: symptoms, diseases, and controls.
Table I.
Adjusted∗ and unadjusted regression results for wildfire air pollution (PM2.5) and the search value index
| Search term | Adjusted∗ models |
Unadjusted models |
|||||
|---|---|---|---|---|---|---|---|
| Beta | 95% CI | P value | Beta | 95% CI | P value | ||
| Skin symptoms | Itchy | 2.4 | (0.78, 4.1) | <.001 | 8.8 | (5.5, 9.9) | <.001 |
| Itchy skin | 1.9 | (0.16, 3.3) | .039 | 1.3 | (-0.90, 3.8) | .31 | |
| Red skin | 2.2 | (0.45, 4.8) | .021 | 4.1 | (1.6, 6.7) | <.001 | |
| Skin diseases | Eczema | 2.9 | (0.34, 5.9) | .0093 | 3.5 | (0.12, 5.1) | .034 |
| Psoriasis | −0.75 | (−3.6, 1.9) | .45 | −0.56 | (−3.1, 1.8) | .59 | |
| Acne | 1.7 | (0.1, 3.8) | .045 | 2.6 | (0.57, 4.8) | .024 | |
| Positive controls | Wildfire | 6.2 | (3.1, 8.6) | <.001 | 6.9 | (4.0, 9.9) | <.001 |
| Smoke | 7.1 | (5.8, 8.9) | <.001 | 7.8 | (6.8, 9.7) | <.001 | |
| Negative controls | Cup | −0.35 | (−3.2, 2.6) | .82 | 0.37 | (−0.51, 0.79) | .58 |
| Dog | −0.70 | (-2.2, 0.86) | .33 | −0.025 | (−1.7, 1.5) | .93 | |
The results reflect change in the SVI for a 10 μg/cubic meter increase in PM2.5 concentration. Bolded values represent statistically significant results with a P value <.05.
PM, Particulate matter.
Adjusted for temperature, relative humidity, and year.
Wildfire air pollution in San Francisco in 2020 had significant positive associations with concurrent public search interest for certain skin symptoms and diseases, such as AD, acne, and itchy skin, but not psoriasis—consistent with a report showing delayed pollution-induced psoriasis flares.3 Our findings expand upon prior research on general air pollution and the itch SVI.4 This study also strengthens the previously noted associations of AD and itch flares with wildfires1 by using a different methodology, assessing effects for a different wildfire, and not being confined to patients at a tertiary care center. However, the results are limited by the lack of individual-level data. Our approach can identify other disorders, such as acne, for future research on the dermatologic impacts of environmental events and could be a useful tool for dermatologists to anticipate and prepare for patient concerns with regard to specific skin disorders and changing environmental conditions. Google search term data may give early warning of emerging spikes in dermatological diseases, similar to infectious diseases,5 and could be used, for example, to ensure pharmacies are stocked and patients with pre-existing diseases like AD are informed to take preventive action.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Exempt from review.
Key words: acne; air pollution; atopic dermatitis; digital epidemiology; eczema; google trends; itch; online search; particulate matter; PM2.5; pruritus; search volume index; wildfire.
References
- 1.Fadadu R., Grimes B., Jewell N., et al. Association of wildfire air pollution and health care use for atopic dermatitis and itch. JAMA Dermatol. 2021;157(6):658–666. doi: 10.1001/jamadermatol.2021.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nuti S.V., Wayda B., Ranasinghe I., et al. The use of google trends in health care research: a systematic review. PLoS One. 2014;9(10) doi: 10.1371/journal.pone.0109583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellinato F., Adami G., Vaienti S., et al. Association between short-term exposure to environmental air pollution and psoriasis flare. JAMA Dermatol. 2022;158(4):375–381. doi: 10.1001/jamadermatol.2021.6019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whang K.A., Huang A.H., Miller L.S., Kang S., Kwatra S.G. Association of particulate matter air pollution and itch: a digital epidemiology approach. J Am Acad Dermatol. 2019;81(6):1409–1410. doi: 10.1016/j.jaad.2019.04.069. [DOI] [PubMed] [Google Scholar]
- 5.Yang S., Santillana M., Kou S.C. Accurate estimation of influenza epidemics using Google search data via ARGO. Proc Natl Acad Sci U S A. 2015;112(47):14473–14478. doi: 10.1073/pnas.1515373112. [DOI] [PMC free article] [PubMed] [Google Scholar]