Abstract
Background
Referral linkages are crucial for efficient functioning of primary health care (PHC) systems. Fast Healthcare Interoperability Resource (FHIR) is an open global standard that facilitates structuring of health information for coordinated exchange among stakeholders.
Objective
The objective of this study is to design FHIR profiles and present methodology and the profiled FHIR resource for Maternal and Child Health referral use cases in Ebonyi state, Nigeria—a typical low- and middle-income country (LMIC) setting.
Methods
Practicing doctors, midwives, and nurses were purposefully sampled and surveyed. Different referral forms were reviewed. The union of data sets from surveys and forms was aggregated and mapped to base patient FHIR resource elements, and extensions were created for data sets not in the core FHIR specification. This study also introduced FHIR and its relation to the World Health Organization’s (WHO’s) International Classification of Diseases.
Results
We found many different data elements from the referral forms and survey responses even in urban settings. The resulting FHIR standard profile is published on GitHub for adaptation or adoption as necessary to aid alignment with WHO recommendations. Understanding data sets used in health care and clinical practice for information sharing is crucial in properly standardizing information sharing, particularly during the management of COVID-19 and other infectious diseases. Development organizations and governments can use this methodology and profile to fast-track FHIR standards adoption for paper and electronic information sharing at PHC systems in LMICs.
Conclusions
We presented our methodology for profiling the referral resource crucial for the standardized exchange of new and expectant moms’ information. Using data from frontline providers and mapping to the FHIR profile helped contextualize the standardized profile.
Keywords: FHIR, COVID-19, digital health, eHealth, mHealth, BlockMom, Nigeria, primary health care, health information, health information exchange, interoperability
Introduction
Background
Health care is a complex sector that involves medical professionals, allied health workers, the information and communication technology (ICT) workforce, and various other stakeholders. The World Health Organization (WHO) highlights the importance of 6 building blocks of any health system: service delivery, health workforce, health information systems, access to essential medicines, financing, and leadership or governance [1]. Therefore, the health information systems block is very critical and plays an important role in data capture, processing, and usage. Substantial investments have been made in the development and strengthening of routine health information systems (RHIS) in many low- and middle-income countries (LMICs) over the past 2 decades [2,3]. Although early RHISs were produced using paper-based health facility reports, many LMICs have implemented newer web-based systems over the past decade [4,5]. Given that substantial investments have been made in strengthening RHISs in LMICs in recent years, researchers have a growing demand for more real-time data [6]. Besides, data for policy and operational decision-making in LMICs, including Nigeria, have been largely limited to report generation, process monitoring, and early surveillance responses. Reliable, quality, timely, and transparent health service data are essential for an efficient health system [7]. Globally, health care interoperability has been identified as vital to seamless care coordination among the different stakeholders.
Global Health Care Interoperability
According to the World Health Organization (WHO) Europe’s 2016 e-Health in practice report, Estonia is the first country to implement electronic health records (EHRs) [8]. The famous X-Road facilitates Estonia's exchange network, an interoperability layer launched in 2001, with several different services added over the years. Estonia achieved success with over 99% of electronic medical subscriptions in 2018. Estonia's X-Road interoperability layer connects over 2700 services across 700 institutions and enterprises across several sectors, including health care. The United Kingdom’s national service specification was based on the Health Level 7 (HL7) version 3 standard and is now transitioning to the HL7 Fast Healthcare Interoperability Resource (FHIR). However, local implementation was left to providers to determine, most of whom already run different versions of HL7 version 2 [9]. This National Health Service project started with 2 main use cases: the Summary Care Records and the Detailed Care Records [9]. Canada launched a national Infoway project to standardize and foster collaboration among pan-Canadian health care solutions [10]. After leveraging the CEN TC251 standards for referrals, discharge letters, laboratory, prescriptions, reimbursements, radiology requests, and reports, a national program was deemed successful in Denmark. These use cases were pilot-tested via 15 independently managed projects [10]. In 2008, a report highlighted that in the United States, “only 15 to 20 percent of medical doctors have access to computerized patient records and only a small fraction of the billions of medical transactions happen electronically” [10]. Such a low usage led to the creation of Health Information Technology for Economic and Clinical Health, which was launched in 2009 to incentivize digitization, and things have since changed.
Interoperability in LMICs
Some LMIC health systems services are still paper-dependent for recording and transmitting health information. Paper records are limited because only one person can access them at a time. Systematic digitization of health systems has driven the development and implementation of national digital health strategies in Nigeria and other LMICs [11,12]. From our literature search [13] and to our knowledge, LMICs still struggle with patient-level interoperability project implementations, which has limited recording successes. Nigeria is a typical LMIC because it has one of the highest global burdens of maternal mortality [14]. Furthermore, there are more primary health care (PHC) facilities (approximately 10 times) than hospitals in Nigeria; hence, here we focus on PHCs. PHCs have the highest potential for impact in the Nigerian health system because most health services are delivered at the PHC level. In a typical PHC network, the possible use cases for health information interchange may include the following:
Interdepartmental care communication
Inter-PHC or PHC to secondary hospital referral
Reporting of decentralized laboratory results
Triangulation of immunization and surveillance information
Payment settlement
Diagnostic information exchange
Nigeria used the DHIS2 for routine reporting of the delivery of health information system services. Routine health information systems (RHISs) continue to collect data on a wide range of diseases and conditions [6]. These RHIS data are analyzed to assess community-level initiatives such as policies to boost community engagement and strengthen referrals from traditional birth attendants to increase demand for maternal and child care [15-17]. The COVID-19 pandemic has further exposed the weakness in health systems worldwide and the value of linkages.
Health Care Interoperability Standards
The international organizations for certifying and ratifying widely used digital health standards are the ISO/TC (International Organization for Standards’ Health Informatics Technical Committee) 215 and CEN/TC (European Committee for Standards’ Health ICT Technical committee) 251. For instance, ISO 21090:2011 is a ratified HL7 version 3 data type for information interchange. Similarly, ISO 13606-1:2019 is a ratified description of archetype reference models. HL7 is a leading health care standard development organization that has facilitated many standards, including the HL7 version 2 messaging standard, HL7 version 3 Clinical Document Architecture document exchange standard, and the HL7 FHIR. FHIR was popularized because it supports REpresentational State Transfer (REST)–based web-based (real-time) transactions and its extension for services. FHIR is now emerging as the de facto global standard for health care data interchange. The FHIR community includes Microsoft, Google, Apple, and many electronic medical record and EHR vendors [18-20]. In addition, the WHO has recently published a digital adaptation kit to support countries deploying standards for antenatal care [21].
Terminologies
In addition to data interchange standards, terminology categorization helps guarantee consistent and uniform understanding (and meaning) of terms in health care systems (within and across geographies). The leading terminologies for disease, procedure, and other concept classification are Systematized Nomenclature of Medicine–Clinical Terms (SNOMED-CT) and the International Classification of Diseases (ICD). Other technology providers are Logical Observation Identifiers Names and Codes (LOINC) for laboratory result reporting and Digital Imaging and Communication in Medicine (DICOM) for imaging data reporting. This study used ICD because it uses a free license compared to the better developed SNOMED-CT for disease classification. Code systems such as the WHO ICD-10 use statistical classification of medical concepts and entities into coded groups, assigning identifiers [22]. Codes allow for the unique identification of these concepts in an information processing system. These codes classify diseases, procedures, billing, history or symptoms, and case summaries (jurisdictional and international aggregate reporting). Simultaneously, service providers, including clinicians, use clinical terms in information processing tools.
Study Objectives
The project's main objective is to use a referral use case to profile, validate, and present data elements relevant to exchanging health information at the PHC level of care. Profiling is the strategy for defining FHIR models by domesticating the international core standard through specific use cases by structured authoring and publishing. Global best practices facilitate digital health information exchange for better care by using standardized data. Digital tools can only communicate using data in certain formats (eg, XML or JSON), organized in an agreed structure [23].
Methods
Overview
We reviewed paper referral forms and surveyed frontline health workers, drawing inspiration from similar work conducted by Odisho et al [24]. We checked how consistent the referral data sets were. Aggregated referral data sets were then mapped to and FHIR extensions profiled. We also modeled data types and cardinalities, including references to other profiles, resources, and terminology binding to ICD-10.
Stakeholder Interviews and Data Set Identification
We established the research focus by addressing the data flow in the maternal and child health information flow value chain in Ebonyi State, Nigeria. Nigeria has between 28,000 and 36,000 health facilities overall. Ebonyi state is one of the 36 subregional governments in Nigeria with 171 “functional” PHC centers and 13 general hospitals [25]. Although from the National Health workforce Registry, there are up to 830 health facilities in the state [26]. Based on our use case, a strategic point of data exchange among multiple PHC centers or PHC centers and hospitals is the referral chain for pregnant women. We used the purposeful snowball sampling technique to identify health care providers in Ebonyi State and share the survey questionnaire.
We sent out questionnaires and a request for a copy of “referral forms” was used for 24 health workers in their respective health facilities in Ebonyi State. Between June 10 and 17, 2019, all 24 health workers completed and returned the questionnaires, and only 3 provided referral paper forms. Respondents were a mix of medical doctors, midwives, and nurses, as shown in Table 1.
Table 1.
Distribution of respondents and their roles.
| Workstation | Roles, n | ||
|
|
Nurse | Midwife | Doctor |
| Primary health care clinics | 3 | 3 | 4 |
| Secondary health care (general hospitals) | 4 | 2 | 3 |
| Tertiary health care (teaching hospital) | 0 | 1 | 3 |
| State Ministry of Health | 0 | 1 | 0 |
We acknowledge the possibility of selection bias, and, for instance, these providers were mostly from health facilities in Abakaliki, the state capital and the main metropolitan city. We consider this bias insignificant as we measured consistency or variation in referral data sets among providers, which was significant. Each provider was from a different health facility (except the tertiary hospital doctors).
The structured questionnaire used asked the following questions:
What information is shared when referring-out a pregnant woman?
What information is expected when referring-in a pregnant woman?
What forms are used, and what are the contents of these forms?
What information is the client or caregiver expected to know or have at the recipient end?
Profiling, Validation, and Publishing
We started by creating a default patient profile with no extension by using the Forge tool and uploading it on the simplifier.net web interface under the BlockMom project for validation [27]. This first step was to confirm that the example of the base patient resource instance is FHIR-conformant. From the stakeholder interviews, we aggregated information data sets. We then mapped them to the standard patient resource to create a referral resource with extensions that capture all the identified data points. We further created the bare XML schema for easy file-based resource instance validation. The codes in XML and JSON formats are freely available on the GitHub directory [28]. Our steps and tools used are shown in Figure 1.
Figure 1.
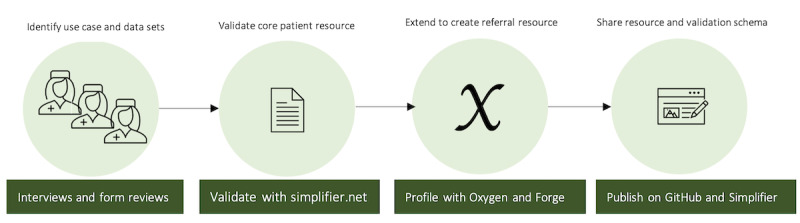
Steps to profiling and publishing the Fast Healthcare Interoperability Resource.
We modeled the FHIR referral use case profile of information flow regarding pregnant women from one PHC center—for example, PHC center 1 to PHC center 2—or general hospital. Afterward, these resource mapping outputs were then synthesized into JSON and XML machine-readable data formats on the basis of FHIR resources for antenatal referral. We have further indicated the resources category affected by our referral bundle in green in Figure 2.
Figure 2.
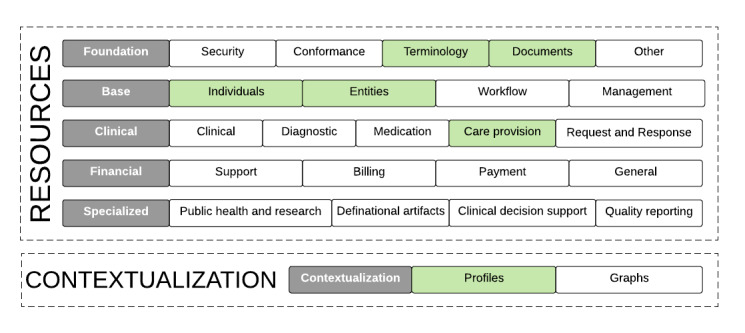
Resources considered for the Referral bundle.
Binding With ICD-10 Terminology
An example referral use case is described in Sierra Leone’s digital health strategy 2018-2023, “Table 2- Scenario: The vision in Practice” [12]. Asuma, a pregnant woman described in the use case, was referred to the clinic from the community by a roaming community health extension worker. See page 25 of Sierra Leone’s national digital health strategy for more information on this use case. In ICD-10, the “Personal History of malaria” code is Z8613. The code allows for unique identification in any information system using the same coding system, thus distinguishing this from, say, B500, which represents “Plasmodium falciparum malaria with cerebral complication,” which is a case of complicated malaria with intermittent coma. We analyzed the 21 chapters of ICD-10. Table 2 highlights those that are most relevant for in-depth study when designing a Maternal and Child Health (MNCH) information management system [10].
Table 2.
Key Maternal and Child Health chapters of the International Classification of Diseases, Tenth Revision coding system.
| Chapter | Description | Code range |
| XV | Pregnancy, childbirth, and the puerperium | O00xx to O99xx |
| XVI | Certain conditions originating in the perinatal period | P00xx to P96xx |
| XVIII | Symptoms, signs, and abnormal clinical and laboratory findings not elsewhere classified | R00xx to R99xx |
| XX | External causes of morbidity and mortality | V01xx to Y98xx |
| XXI | Factors influencing health status and contact with health services | Z00xx to Z99xx |
Code O98.6 represents “Protozoal disease complicating pregnancy, childbirth, and the puerperium.” This is synonymous with “Malaria in pregnancy” or “Maternal malaria during pregnancy,” both not explicitly coded in ICD-10 [29]. “Malaria in pregnancy” is the scenario described in the Sierra Leone MNCH digital health use case from the preceding paragraph.
Ethics Consideration
This study was exempted from ethics approval by the University of Malta ethics review board.
Results
Survey Outputs
In addition to responses from these surveys, 3 different referral forms for referral tracking among pregnant women used in the state were made available by respondents. The forms were then mapped to survey questions to generate a unified form with a union of content from the 3 forms in Table 3.
Table 3.
Form contents and their mapping.
| Ebonyi State Ministry of Health referral slip | National Health Insurance Scheme (NHIS) referral form | Women, infants, and children referral form for pregnant women |
| Facility name |
|
N/Aa |
| N/A |
|
|
| Patient number and social insurance number |
|
— |
| Name of patient |
|
|
| Age |
|
|
| Sex |
|
— |
| Address | N/A |
|
| N/A | N/A |
|
| Complaints |
|
— |
| Findings on examination |
|
|
| Investigations performed, if any |
|
— |
| Provisional diagnosis |
|
— |
| N/A |
|
|
| Current and recent medication | N/A |
|
| N/A |
|
|
| Name of officer |
|
|
| Designation | N/A | — |
| Signature |
|
|
| To |
|
— |
aN/A: not applicable.
Survey responses from care providers varied widely and included extraneous information than in the referral forms. Based on the 24 health care providers' responses for the first 2 questions—“What Information is shared when referring a pregnant woman?” and “what information is expected when receiving a pregnant woman?”—none of the responses matched for all respondents. In response to question 3—“what forms are used?”—3 respondents said “referral letter” and 7 said “referral form.” Three respondents noted that referral forms varied by health institutions, while one indicated that they do not use any forms for referral. Other forms listed by respondents are the consent form, investigation form, chemistry form, hematology form, results form, ultrasound form, laboratory form, radiology form, and virology form. In response to the question, “What information is the client, or their caregiver expected to have or know?” At the same time, 2 respondents said “nill,” the rest of them listed information that completely varied. When we mapped the aggregated responses with the form details from Table 3, the list of data sets will be similar to that shown in Textbox 1.
List of data sets.
Source health facility name
Source health facility ID
Destination health facility name
Destination health facility ID
Date of referral
Patient name
Patient number
Patient no type (Health Management Organization, National Health Insurance Scheme, softwareVendor)
Patient age
Sex
Address
Complaint
Presenting complaint
Investigation done
Findings on examination
Provisional diagnosis
Reason for referral
Current medication
Recent medication
Name of referring officer
ID of referring officer (Medical and Dental Council of Nigeria)
Designation of the referring officer
Other relevant information
Referrals direction (in or out)
Referrals by disease
Malaria case referred for adverse drug reaction (Health Management Information System)
Referral disease (tracked by age and case)
Referral FHIR Resource (Known as Referral Letter or Discharge Letter)
The profile developed in this paper is only considered a provisional national profile suggestion for consideration and should not be relied on for clinical decisions. The resource mapping's final output is in XML and JSON formats and is freely available on GitHub [28]. The resource file is shown in Figure 3.
Figure 3.
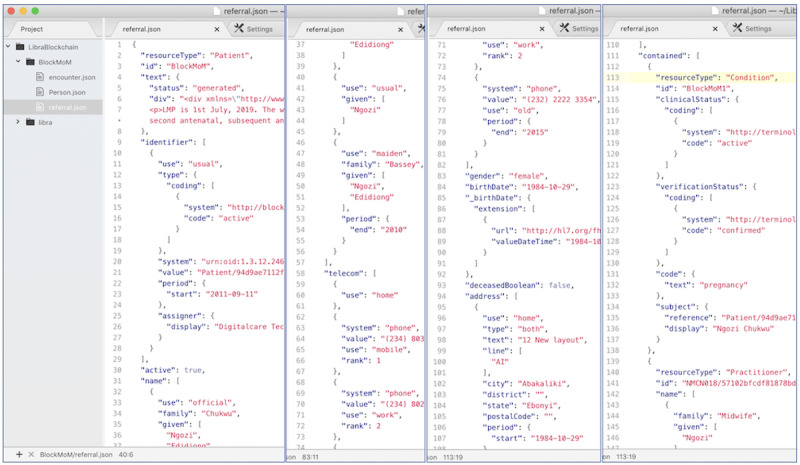
The profiled referral resource in picture.
REST and FHIR
Our artifact assumes the use of the REST paradigm for information exchange. In this section, we explain the technicalities of REST. REST is the foundation for the scale of the internet as we know it today [30]. While FHIR supports many different communication paradigms, REST is responsible for its popularity. The REST paradigm leverages the HTTP protocol with the simple client-server architecture with variants of catch-less/catching, stateless/stateful, or n-tired architectures and hierarchies. For further technical details of these ICT concepts, please refer to Thomas Fielding’s thesis introducing REST in 2000 [30].
Similar to traditional REST, FHIR’s REST paradigm considers entities and concepts as resources. Each of the resource instances is unique and is represented using a uniform resource identifier (URI). The URI may also be used for locating the resource if it points to the location on a given server (in which case, it can also be referred to as URL). There are a finite number of ways a client can manipulate entities and concepts (resources) located in an FHIR server using REST requests of get, put, post, delete, options, head, trace, and connect.
The server responds to the client’s HTTP requests after performing internal business logics unique to each server implementation. The clients will receive the same response for similar HTTP requests irrespective of whether they are for a mobile app, web browser, computer application, or embedded device, as shown in Figure 4.
Figure 4.
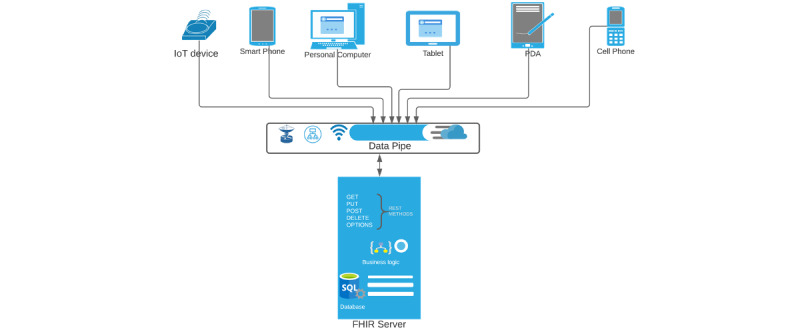
A typical client-server REpresentational State Transfer interface. FHIR: Fast Healthcare Interoperability Resource; IoT: Internet of Things; PDA: personal digital assistant.
Both the client and server use the header and body components of the HTTP request or response for their information exchange, depending on the HTTP method used. The server always returns a status code indicating success or failure or a variant of either with further detail for each request. FHIR servers can use the OperationOutcome resource to provide structured details of request failure to the clients in the event of failure. There are over 100 different FHIR resources [31]. When the request succeeds, the client is sent the resource by the server.
Methods may or may not be allowed (or even implemented) by the server for a particular resource and may be specified by the client's server response. The header has many attributes that can be set, for instance, to indicate the data type it accepts, authorization credentials, connection, content encoding, caching, and more. The content-type attribute can indicate the resource as either XML or JSON format—both native to FHIR. FHIR, similar to REST, is an open standard and thus aligns with key principles of digital development [32].
Discussion
Principal Findings
We could not use the core FHIR resource because it did not contain all the data sets as aggregated in Figure 4. To add and extend the outstanding data sets, FHIR designers provide for and allow extendibility using profile extensions. FHIR contributors and balloting-process use the 80-20 rule to determine what makes it into the core FHIR resource [33]. It is understandable if there are no contributions from Nigeria or many other LMICs because they are often not represented at HL7 FHIR balloting. Our referral form reviews and data set mapping also lay credence to our hypothesis that the core patient resource needs an extension for our use case.
Our study shows that traditional paper referral forms currently in use vary widely in Nigeria’s PHC system as illustrated in the word art in Multimedia Appendix 1. The implication is that interinstitution care coordination will remain suboptimal as much of the essential information will be missing. This work will help policy makers and PHC centers in Nigeria understand the need to standardize or enforce agreed referral standards. In addition, the steps we have outlined in this work will help guide institutions as they standardize or adopt FHIR.
While the surveys were conducted before the COVID-19 pandemic, their findings are relevant for continued functioning of the PHC centers even amid and after the COVID-19 pandemic. The pandemic has exposed the weakness of health systems and shown the importance of interconnected and interoperable health systems. Emerging technologies are being proposed in response to the pandemic [34] and new models are emerging for health information interoperability [35] in LMICs. Even when PHC centers are digitized, referrals among health facilities in many LMICs with different software vendors do not happen seamlessly. Our research shows that referral practices for pregnant women varied significantly even in urban settings.
The key output of this study is the FHIR referral resource artifact, which will help vendors design consistent referral data sets and ensure out-of-the-box interoperability. This resource remains broad and from the core patient resource. FHIR allows for organizational or national extensions and adaptations [33]. Health authorities in many LMIC countries will benefit from standardizing and exposing its required referral data model for Women and Child Health, which encompasses MNCH [24]. Publishing a public FHIR specification that can be leveraged by MNCH solution implementers will help simplify interface implementations.
We here illustrate that our approach differs from traditional health information exchange approaches. Figure 5A shows the traditional document- and message-based information (which is still supported by FHIR) where both databases are required to retain the messages being exchanged. Figure 5B shows that the end point query approach using REST method calls is used to access or share FHIR resources being exchanged.
Figure 5.
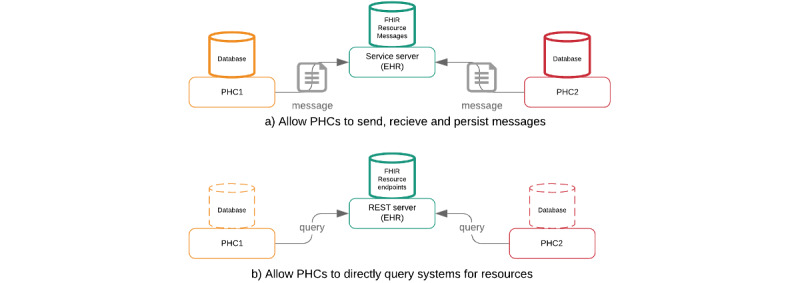
Fast Healthcare Interoperability Resource (FHIR) paradigms in a 2–public health care (PHC) system referral exchange scenario. EHR: electronic health record. REST: REpresentational State Transfer.
Women continue to die owing to preventable causes at the point of giving birth. Many of these deaths happen before, during, and after delivery. In addition, maternal health has been highlighted in some LMIC national digital health strategies (ie, Nigeria and Sierra Leone) as a priority health area [11]. Furthermore, our BlockMom model used the ICD terminology over the SNOMED-CT model owing to its favorable pricing license. For instance, SNOMED licenses are based on the number of health facilities using the terminology service, though there are requirements to apply for a waiver for certain implementations in LMICs. Moreover, the model’s deliberate focus on FHIR over other HL7 or ISO standards was because it is free and open for adaptation, adoption, and testing in LMICs.
Limitations
We used on-file schema and the ICD-10 version 2021 text file to validate profiled resources. Even though the bare schema was provided in the GitHub directory, standard practice would be to set up an FHIR server for this purpose. This is the focus of our future study. Although many mobile-based solutions are available in PHC centers in LMICs, these profiles can only be used with a mobile-based solution that uses patient-specific information rather than aggregated information, as is the case with many community health worker information systems. Furthermore, ICD-11 2022 release has just been launched by the WHO, which emphasizes following the profiling process and not necessarily the output [36].
We also noted that unique identification metrics and characteristics, as explained by McFarlane et al [37] and Chukwu [38], were not part of the data sets proposed and made available during referral. This aspect was profiled as part of the FHIR resource. Besides, this may be the case as the patient-required abridged historical information is assumed to be comprehensive enough. Nevertheless, in a digital platform where a unique identifier is important, this assumption will not hold true. We assumed cryptographically generated unique identification mechanisms in this prototype.
A key limitation of our survey approach was that we did not prevalidate the questionnaire before use. In addition, our sampling methodology used a snowball strategy that targeted health workers from the most urban part of Ebonyi State, Nigeria. We are aware and acknowledge that this may seem inherently biased. However, our aim for the survey was to determine consistency or otherwise of the referral data sets, which we determine to vary widely across all respondents. In addition, since Abakaliki is the state capital and the main metropolitan city in the state, it is expected to have a standardized referral form; however, it does not.
Conclusions
Questionnaire responses were collected from health care providers, and referral forms from health institutions in Nigeria were reviewed. Survey responses and fields of referral forms show variability in referral data sets across respondents and forms. Here we have made a case for FHIR, an emerging health care data interchange standard, and have profiled a referral resource for PHC information exchange targeted at LMICs. This paper describes the profiling steps, including key questionnaire responses and mapping of referral forms. We have proposed the use of ICD-10 terminology and used file-based schema validation. The methodology and artifacts will be invaluable for the research and implementation community targeting LMICs. Our future work will set up the server and configure the appropriate binding for this and other resources.
Abbreviations
- CEN
European Committee for Standards’ Health ICT
- DICOM
Digital Imaging and Communication in Medicine
- EHR
electronic health record
- FHIR
Fast Healthcare Interoperability Resource
- ICD
International Classification of Diseases
- ICT
Information and Communication Technologies
- ISO
International Organization for Standards
- LMIC
low- and middle-income country
- LOINC
Logical Observation Identifiers Names and Codes
- MNCH
Maternal and Child Health
- PHC
primary health care
- REST
REpresentational State Transfer
- RHIS
routine health information systems
- SNOMED-CT
Systematized Nomenclature of Medicine–Clinical Terms
- URI
uniform resource identifier
- WHO
World Health Organization
Survey respondents' referral keywords.
Footnotes
Conflicts of Interest: None declared.
References
- 1.World Health Organization . Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva: World Health Organization; 2011. [Google Scholar]
- 2.Mutale W, Chintu N, Amoroso C, Awoonor-Williams K, Phillips J, Baynes C, Michel C, Taylor A, Sherr K. Improving health information systems for decision making across five sub-Saharan African countries: Implementation strategies from the African Health Initiative. BMC Health Serv Res. 2013 May 31;13(S2) doi: 10.1186/1472-6963-13-s2-s9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Warren AE, Wyss K, Shakarishvili G, Atun R, de Savigny D. Global health initiative investments and health systems strengthening: a content analysis of global fund investments. Global Health. 2013 Jul 26;9(1):30. doi: 10.1186/1744-8603-9-30. https://globalizationandhealth.biomedcentral.com/articles/10.1186/1744-8603-9-30 .1744-8603-9-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kiberu VM, Matovu JK, Makumbi F, Kyozira C, Mukooyo E, Wanyenze RK. Strengthening district-based health reporting through the district health management information software system: the Ugandan experience. BMC Med Inform Decis Mak. 2014 May 13;14(1):40. doi: 10.1186/1472-6947-14-40. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-14-40 .1472-6947-14-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hazel E, Wilson E, Anifalaje A, Sawadogo-Lewis T, Heidkamp R. Building integrated data systems for health and nutrition program evaluations: lessons learned from a multi-country implementation of a DHIS 2-based system. J Glob Health. 2018 Dec;8(2):020307. doi: 10.7189/jogh.08.020307. doi: 10.7189/jogh.08.020307.jogh-08-020307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hung YW, Hoxha K, Irwin BR, Law MR, Grépin KA. Using routine health information data for research in low- and middle-income countries: a systematic review. BMC Health Serv Res. 2020 Aug 25;20(1):790. doi: 10.1186/s12913-020-05660-1. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-05660-1 .10.1186/s12913-020-05660-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Health Metrics Network. World Health Organization . Framework and standards for country health information systems (2nd edition) Geneva: World Health Organization; 2008. [Google Scholar]
- 8.European Programme of Work: United Action for Better Health. World Health Organization. [2020-08-30]. https://www.euro.who.int/en/countries/estonia/news/news/016/03/e-health-in-practice .
- 9.Greenhalgh T, Stramer K, Bratan T, Byrne E, Russell J, Potts HWW. Adoption and non-adoption of a shared electronic summary record in England: a mixed-method case study. BMJ. 2010 Jun 16;340(jun16 4):c3111–c3111. doi: 10.1136/bmj.c3111. [DOI] [PubMed] [Google Scholar]
- 10.Benson T, Grieve G. Principles of Health Interoperability. Cham: Springer; 2016. Coding and Classification Schemes; pp. 135–154. [Google Scholar]
- 11.National Health ICT Strategic Framework 2015-2020. Federal Ministry of Health. 2016. [2022-06-13]. http://www.health.gov.ng/doc/HealthICTStrategicFramework.pdf .
- 12.National Digital Health Strategy 2018-2023. Ministry of Health and Sanitation. 2018. [2021-01-16]. https://mohs2017.files.wordpress .com/2019/02/sl-national-digital-health-strategy-nov-2018.pdf .
- 13.Chukwu E, Garg L. A Systematic Review of Blockchain in Healthcare: Frameworks, Prototypes, and Implementations. IEEE Access. 2020;8:21196–21214. doi: 10.1109/access.2020.2969881. [DOI] [Google Scholar]
- 14.World Health Organization . World Health Statistics 2018: Monitoring Health for the SDGs, Sustainable Development Goals. Geneva: World Health Organization; 2018. [Google Scholar]
- 15.Mochache V, Irungu E, El-Busaidy H, Temmerman M, Gichangi P. "Our voices matter": a before-after assessment of the effect of a community-participatory intervention to promote uptake of maternal and child health services in Kwale, Kenya. BMC Health Serv Res. 2018 Dec 04;18(1):938. doi: 10.1186/s12913-018-3739-9. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3739-9 .10.1186/s12913-018-3739-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kitui JE, Dutton V, Bester D, Ndirangu R, Wangai S, Ngugi S. Traditional Birth Attendant reorientation and Motherpacks incentive's effect on health facility delivery uptake in Narok County, Kenya: An impact analysis. BMC Pregnancy Childbirth. 2017 Apr 21;17(1):125. doi: 10.1186/s12884-017-1307-7. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-017-1307-7 .10.1186/s12884-017-1307-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paudel D, Shrestha IB, Siebeck M, Rehfuess E. Impact of the community-based newborn care package in Nepal: a quasi-experimental evaluation. BMJ Open. 2017 Oct 05;7(10):e015285. doi: 10.1136/bmjopen-2016-015285. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=28982810 .bmjopen-2016-015285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.A Free and Open Source Global Good: Powering Interoperability Around the World for 18 Years. HAPI FHIR. [2021-01-16]. https://hapifhir.io .
- 19.HL7 Launches Argonaut Project to Advance FHIR. Health IT Answers. 2014. [2021-01-16]. https://www.healthitanswers.net/hl7 -launches-argonaut-project-to-advance-fhir/ [PubMed]
- 20.Braunstein ML. Health Informatics on FHIR: How HL7's New API is Transforming Healthcare. Cham: Springer; 2018. FHIR; pp. 179–203. [Google Scholar]
- 21.Mehl G, Tunçalp Ö, Ratanaprayul N, Tamrat T, Barreix M, Lowrance D, Bartolomeos K, Say L, Kostanjsek N, Jakob R, Grove J, Mariano B, Swaminathan S. WHO SMART guidelines: optimising country-level use of guideline recommendations in the digital age. Lancet Digit Health. 2021 Apr;3(4):e213–e216. doi: 10.1016/S2589-7500(21)00038-8. https://linkinghub.elsevier.com/retrieve/pii/S2589-7500(21)00038-8 .S2589-7500(21)00038-8 [DOI] [PubMed] [Google Scholar]
- 22.International Statistical Classification of Diseases and Related Health Problems 10th Revision. ICD-10 Version:2019. [2021-01-10]. https://icd.who.int/browse10/2019/en .
- 23.Benson T. Prevention of errors and user alienation in healthcare IT integration programmes. Inform Prim Care. 2007 Jan 01;15(1):1–7. doi: 10.14236/jhi.v15i1.639. http://hijournal.bcs.org/index.php/jhi/article/view/639 .639 [DOI] [PubMed] [Google Scholar]
- 24.Odisho AY, Lui H, Yerramsetty R, Bautista F, Gleason N, Martin E, Young JJ, Blum M, Neinstein AB. Design and development of referrals automation, a SMART on FHIR solution to improve patient access to specialty care. JAMIA Open. 2020 Oct;3(3):405–412. doi: 10.1093/jamiaopen/ooaa036.ooaa036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Overview of the Ministry of Health, Abakaliki. [2019-06-30]. http://www.ebonyistate.gov.ng/Ministry/Health/resources/achievement.pdf .
- 26.NIGERIA Health Facility Registry (HFR) [2021-03-18]. https://hfr.health.gov.ng/statistics/tables .
- 27.MyPatient. Simplifier.net. [2020-01-14]. https://simplifier.net/BlockMom/MyPatient/~xml .
- 28.BlockMom. GitHub. [2021-01-14]. https://github.com/EmekaC/BlockMom .
- 29.Protozoal diseases complicating pregnancy, unspecified trimester. ICD10data.com. [2021-01-10]. https://www.icd10data.com/ICD10CM/Codes/O00-O9A/O94-O9A/O98-/O98.619 .
- 30.REST: Architectural Styles and the Design of Network-based Software Architectures. [2022-06-13]. http://www.ics.uci.edu/~fielding/pubs/dissertation/top.htm .
- 31.HL7 FHIR. [2021-01-10]. http://hl7.org/fhir .
- 32.Principles for Digital Development. [2019-05-31]. http://digitalprinciples.org .
- 33.FHIR and Architectural Principles. HL7 FHIR. [2022-06-13]. https://build.fhir.org/overview-arch.html#:~:text=In%20addition%2C %20FHIR%20aligns%20to,80%25%20of%20the%20interoperability%20needs .
- 34.Ye J. The Role of Health Technology and Informatics in a Global Public Health Emergency: Practices and Implications From the COVID-19 Pandemic. JMIR Med Inform. 2020 Jul 14;8(7):e19866. doi: 10.2196/19866. https://medinform.jmir.org/2020/7/e19866/ v8i7e19866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El Jabari C, Macedo M, Al-jabari MO. Towards a New Paradigm of Federated Electronic Health Records in Palestine. Informatics. 2020 Oct 05;7(4):41. doi: 10.3390/informatics7040041. [DOI] [Google Scholar]
- 36.ICD-11 2022 release. World Health Organization. [2022-02-12]. https://www.who.int/news/item/11-02-2022-icd-11-2022-release .
- 37.McFarlane TD, Dixon BE, Grannis SJ. Health Information Exchange. Cambridge, MA: Academic Press; 2016. Client Registries: Identifying and Linking Patients; pp. 163–182. [Google Scholar]
- 38.Chukwu E. The Case for a Unique Digital Patient ID Scheme in Nigeria. J Health Med Inform. 2017;08(03) doi: 10.4172/2157-7420.1000267. https://www.omicsonline.org/open-access/the-case-for-a-unique-digital-patient-id-scheme-in-nigeria-2157-7420-1000267.pdf . [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Survey respondents' referral keywords.


