Abstract
Objective
To assess effective breastfeeding technique (EBT) and associated factors among lactating mothers in Gidan District, North-East Ethiopia.
Design
A community-based cross-sectional study.
Setting
Gidan District, North-East Ethiopia.
Participants
A total of 786 lactating mothers were included between 30 March and 29 April 2021.
Outcome
EBT.
Methods
A multistage sampling technique was employed to recruit participants. Pretested interviewer-administered questionnaires and an observational checklist were used to collect the data. Individual scores of three variables about breast feeding, namely positioning, attachment and suckling, were computed to generate the outcome variable, that is, breastfeeding technique. Binary logistic regression analyses were carried out to determine the association between independent variables and EBT. Statistical significance was declared at a value of p≤0.05 with a corresponding 95% CI.
Results
Overall, the prevalence of EBT was 42.9% (326/760). Having antenatal care follow-up (adjusted OR (AOR)=1.75; 95% CI 1.10 to 2.77), delivering at health institutions (hospital AOR=2.85; 95% CI 1.22 to 6.66 and health centre AOR=2.15; 95% CI 1.25 to 3.68), and receiving postpartum home visits by the health extension workers (HEWs) (AOR=2.12; 95% CI 1.55 to 2.92) were significantly associated with the practice of EBT.
Conclusion
The study showed that the prevalence of EBT was low. The finding highlights the importance of promoting utilisation of antenatal care follow-up, institutional delivery and postpartum home visits by HEWs, which play a substantial role in promoting EBT.
Keywords: Sexual dysfunction, Nutrition, Respiratory infections, PUBLIC HEALTH, Infectious diseases & infestations
Strengths and limitations of this study.
Since the outcome variable was computed by scores given by different observers, some necessary measures, including delivering training and providing time to practice in a real environment before the data collection, were incorporated to reduce measurement errors and interobserver variability.
Due to interobserver variability and the Hawthorne effect, the study might not be free from bias.
Using the registration book as a sampling frame may introduce selection bias as new lactating mothers might not get registered.
Introduction
Breastfeeding technique (BFT) is defined as the composite of positioning, attachment and suckling during breast feeding.1 Position indicates the capacity of the mother to carry her child on her body. At the same time, attachment denotes whether the mother attaches the baby to her breast and to her nipple, keeping most of the areola in the baby’s mouth.2 Similarly, suckling is a part of the BFT, which reflects the infant’s performance of expressing milk, which can be explained by the depth and speed of sucking.1 These techniques collectively imply the status of breastfeeding infants. The WHO and UNICEF recommend breast feeding within 1 hour of birth and exclusive breast feeding (EBF) for the first 6 months.3 As a result, infants can get the required amount of energy and nutrients. Applying effective breastfeeding techniques (EBTs) can foster sufficient milk production and release.4 In addition, appropriate breast feeding helps prevent communicable and non-communicable diseases.5
On the other hand, ineffective breastfeeding technique (IBT) is attributed to poor positioning, attachment and suckling, which could result in early cessation of EBF and put infants at risk.6 Several pieces of evidence show that more than half of mothers with IBT discontinue EBF earlier, resulting in severe infectious and non-infectious chronic diseases in their children.6–9 Globally, more than half a million infants die each year due to nutritional deficiency attributed to suboptimal breastfeeding.10 Aside from the mortality, there are hundreds of thousands of children whose growth and development is impaired.11 In Ethiopia, suboptimal breastfeeding practices (including IBTs) contribute to the higher under-five mortality resulting from malnutrition.12 13 In the country, the burden of malnutrition, particularly undernutrition, begins at an early stage of life, and it is believed to be due to suboptimal breastfeeding practices.13 14
IBT not only threatens infants' lives but also negatively impacts the health of the mother.15 IBT is one of the major causes of cracked nipples among lactating mothers.15 Nipple damage, mastitis and other similar complications are more common among lactating mothers with IBT.7
The practice of EBT varies across different settings. For instance, in South Ari district, southern Ethiopia 36.5%,9 Harar city, eastern Ethiopia 43.4%,16 Gondar town, Ethiopia 48%,17 West Denmark 52%,18 Libya 48%.7 Furthermore, small localised studies in India found that the practice of EBT ranged from 30.3% to 51%.19–21 Multiple factors like parity, maternal and child age, level of education, place of delivery, antenatal care (ANC), postnatal care (PNC), knowledge of BFTs, and counselling about EBT are some of the identified factors that can affect the practice of EBT.9 17 22 23
There have been several strategies to avert the problem, although sufficient improvement has not been observed in the past decade.11 The WHO and the baby-friendly hospital initiative have designed EBT counselling, teaching and demonstrations for mothers in all maternity care services and all mothers with sick children in accordance with the Integrated Management of Neonates and Childhood Illness guidelines.6 24 Ethiopia has also recently incorporated IBT into the national acute malnutrition management guidelines as a diagnostic criterion for severe acute malnutrition among infants under 6 months.25
Nutritional problems among children remain the most significant challenge towards achieving the Ethiopian government’s target to end childhood undernutrition by 2030 with a commitment to the ‘Seqota’ Declaration.26 To achieve the aforementioned target, we need to encourage EBT during infancy, and early childhood and science-backed interventions would have a significant role.
Although few studies have been conducted in Ethiopia, almost all of them were conducted among mothers who pursued health services (institution-based) in which those women considerably have better knowledge about healthy practices.7 9 16 17 In addition, previous studies have been conducted, including on mothers soon after birth, before the mother is stabilized and becomes comfortable, which could ultimately affect the BFTs.8 9 18 Moreover, there was a paucity of evidence concerning EBT in northern Ethiopia. Therefore, this study aimed to assess EBT and identify its associated factors among lactating mothers. The findings will provide evidence for policy makers and the concerned bodies to work on identified attributes to further improve the practice of EBT.
Methods
Study setting, design and period
A community-based cross-sectional study was conducted from 30 March to 29 April 2021, in Gidan District, North Wollo Zone, North-East Ethiopia. The district is 595 km from Addis Ababa, the capital of Ethiopia, and it has 2 urban and 21 rural kebeles (the lowest administrative unit). Close to half (49.7%) of the population in the district is female. Under-five children and lactating mothers account for 15.2% (22523) and 4.3% (6320) of the population, respectively. The district has 6 health centres and 23 health posts that provide routine health services to the catchment population.27
Study participants
All lactating mothers (mother-infant pairs) having infants under 6 months of age in the selected kebeles in Gidan District were included. Lactating mothers who were critically ill or unable to breast feed their infants and infants with a critical illness at the time of data collection were excluded from the study.
Sample size determination and sampling procedures
The sample size was calculated using a single population proportion formula, considering the following statistical assumptions: margin of error 5% (0.05), Z-value 1.96 corresponding to 95% confidence level, 10% non-response, design effect of 2, and the proportion of EBT 36.5%, which gave a final sample size of 786.9
A multistage sampling technique stratified by urban and rural kebeles was employed. Of the 21 rural and 2 urban kebeles found in the district, 30% of the total kebeles (6 rural kebeles and 1 urban kebele) were selected by a simple random sampling technique. The list of lactating mothers with children aged under 6 months was taken from the health extension workers’ (HEWs’) registration book of each selected kebele’s health post and considered as a sampling frame. Then, the sample size was proportionally allocated to each selected kebele considering the number of lactating mothers. Simple random sampling using the OpenEpi random program V.3 was used to draw the participants from each kebele.
Variable measurement and definition of terms
Positioning
Positioning was defined as good when at least three out of four criteria for infant positioning were fulfilled. Positioning was defined as average if any two of the four criteria were correctly applied, whereas positioning was defined as poor when only one or none of the criteria had been fulfilled.9 28
Attachment
The attachment was described as good when at least three out of four criteria had been fulfilled. The attachment was described as average if any two of the four criteria had been fulfilled. The attachment was described as poor when only one or none of the four criteria had been fulfilled.
Suckling
Suckling was described as effective when at least two out of three criteria had been fulfilled. Suckling was described as ineffective if only one or none of the three criteria had been fulfilled.9 28
Effective BFT
EBT is the combination of at least two criteria from positioning, three criteria from attachment and two criteria from suckling.16 18
Breast problem
A mother is said to have breast problems if she has any of the following:
Inverted nipple: A portion of or the entire nipple is buried below the plane of the areola and does not evert at all.30
Engorgement: Breasts are painfully overfull.
Cracked nipple: Any damage and excoriation to the integrity of the skin on the nipple.
Mastitis: An inflammatory condition of the breast, which may or may not be accompanied by infection.31
Data collection tools and quality control
A structured observational checklist adopted from the WHO breastfeeding observational checklist and interviewer-administered questionnaires was developed on reviewing different related literature.8 9 22 23 32 According to the WHO criteria, we developed and adopted an arbitrary scoring and grading system to grade positioning, infant’s mouth attachment and effective suckling during breast feeding.33 Each criterion scored 1 point (table 1).
Table 1.
Criteria and grading system for positioning, attachment and suckling among lactating mothers in Gidan District, North-East Ethiopia, 2021 (n=760)
| Criteria for correct body positioning: |
|
|
|
|
| Criteria for grading body positioning: | Grade | Score |
| None or only one out of four criteria has been fulfilled | Poor | 0–1 |
| Any two of the four criteria have been fulfilled | Average | 2 |
| Three/all the four criteria for body positioning have been fulfilled | Good | 3–4 |
| Criteria for correctness of attachment: |
|
|
|
|
| Criteria for grading of correct attachment: | Grade | Score |
| None or only one out of four criteria has been fulfilled | Poor | 0–1 |
| Any two of the four criteria have been fulfilled | Average | 2 |
| Any three or all the four criteria have been fulfilled | Good | 3–4 |
| Criteria for correctness of effective suckling: |
|
|
|
| Criteria for grading of effective suckling: | Grade | Score |
|
Ineffective | 0–1 |
|
Effective | 2–3 |
Eight female BSc midwives (data collectors) and two supervisors from the same field with experience in research and fieldwork coordination participated in the data collection process. Data collectors and supervisors were oriented and trained for 1 day, with a focus on how to interview, examine and diagnose mothers with breast problems, tips to score the observational checklist, and bias controlling mechanisms. The data collectors also received simulation/real-environment training, and their score was compared with see the effect of interobserver variability. This was repeated until the result of two data collectors on the same participant became approximately the same by helping and providing corrective measures. Moreover, we recruited data collectors having similar educational statuses and considerable similar experiences to reduce interobserver variability.
The questionnaires were pretested on 40 study participants (5%) in Gubalafto district, and modifications were made according to the pretest results. The data collectors approach the participants by introducing themselves and interviewing the selected respondent after obtaining oral informed consent.
The data collectors observed BFT while the mother was at home in a private place. To reduce the Hawthorne effect, mothers were oriented to show how they routinely breast fed their infant, and that they won’t be judged by their way of doing it. The observation lasted at least 5 min, and the data collectors recorded the breastfeeding positioning, attachment and suckling as per the WHO breastfeeding observation checklist. If the infant had breast fed in the previous 1 hour, the mother was asked when the infant would have the next feed, and the observation assessment was planned accordingly. After observation, the participants were interviewed for the interviewer-administered questionnaires. The data collectors linked the mothers who had breast problems such as mastitis, engorgement and crackle nipple, to the nearest health facilities.
Data processing and analysis
The collected data were checked manually for completeness and consistency. Then the data were entered into the EpiData V.4.6 software package and exported to Stata V.14 for cleaning, coding and analysis. Descriptive statistics were described using frequencies, percentages, mean and SD, and presented using tables, figures and text. Normality tests such as kurtosis and skewness were employed to examine the distribution of continuous variables and identify the appropriate summary measures.
EBT was ascertained by computing the positioning, attachment and suckling scores. The scores of each item of the three techniques have been computed first. In other words, questions to measure positioning were computed and categorised as good, average and poor. Then, to create a dummy variable, good and average positioning were merged as good and labelled as ‘1’ and poor positioning was coded as ‘0’. The same procedure was applied for attachment. Moreover, suckling was categorised and coded as effective and ineffective suckling.
The outcome variable was dichotomised as ‘effective’ and ‘ineffective’ BFT, and it was labelled as ‘1’ and ‘0’, respectively. Binary logistic regression analysis was applied. Independent variables with a value of p=0.2 in the bi-variable analysis were considered in the multivariable model. Variables with a value of p≤0.05 were regarded as statistically significant. Adjusted OR (AOR) with its corresponding 95% CI was used to examine the strength and direction of the association.
Ethical approval
A letter of support was taken from the district administrative office and handed to the selected kebeles. After a brief explanation of the study objective and purpose, oral informed consent was obtained from each participant. Participants were also informed that participation was voluntary, and they had the right to withdraw from the study at any time during the data collection. After the interview, the data collectors advised/demonstrated to the mother the EBT if the mother-infant pair had an IBT. Furthermore, all data obtained from participants were kept confidential and used for this study only. The study was also conducted according to the recommendations of the Helsinki declaration.
Patient and public involvement statement
Lactating mothers were included in this study by providing valuable information, including measurements. Nevertheless, they have never been involved in the study design, protocol, data collection tools, and reporting and disseminating the findings.
Results
Sociodemographic characteristics
A total of 760 breastfeeding mothers participated, resulting in a response of 96.7%. The mean age of participants was 26.98 (±5.3) years. About 40.3% of participants fell within the age category of 26–30 years. A bit more than three-fourths (75.4%) of the respondents were rural dwellers, and almost all (99.6%) participants were orthodox Christian followers. Regarding the educational status of the mothers, more than half (57.2%) of them had no formal education (table 2).
Table 2.
Sociodemographic characteristics of respondents at Gidan District, North-East Ethiopia, 2021 (n=760)
| Variables | Categories | Frequency | Per cent (%) |
| Age of the mother, years | <20 | 74 | 9.7 |
| 20–25 | 197 | 25.9 | |
| 26–30 | 306 | 40.3 | |
| >30 | 183 | 24.1 | |
| Religion | Orthodox | 757 | 99.6 |
| Muslim | 3 | 0.4 | |
| Educational status of the mother | Not attending formal education | 435 | 57.2 |
| Primary school | 233 | 30.7 | |
| Secondary school and above | 92 | 12.1 | |
| Occupation of the mother | Housewife | 645 | 84.9 |
| Government employed | 83 | 10.9 | |
| Self employed | 24 | 3.1 | |
| Other* | 8 | 1.1 | |
| Marital status | Married | 684 | 90.0 |
| Single | 53 | 7 | |
| Windowed | 16 | 2.1 | |
| Other† | 7 | 0.9 | |
| Educational status of the husband | Not attending formal education | 372 | 54.3 |
| Primary school | 202 | 29.4 | |
| Secondary school and above | 110 | 16 | |
| Occupation of the husband | Farmer | 552 | 80.7 |
| Government employed | 51 | 7.4 | |
| Self employed | 61 | 8.9 | |
| Other‡ | 20 | 2.9 | |
| Residence | Rural | 573 | 75.4 |
| Urban | 187 | 24.6 |
*Student
†Divorced and separated
‡Daily labour and soldier
Obstetric and infant characteristics
About 80.5% and 85.5% of the mothers were multipara and had an ANC visit for their index child, respectively. More than half (55%) of the participants received BFT counselling immediately after delivery (table 3).
Table 3.
Obstetric and infant characteristics of the respondent at Gidan District, North-East Ethiopia, 2021 (n=760)
| Variables | Categories | Frequency (n) | Per cent (%) |
| Parity | Primipara | 148 | 19.5 |
| Multipara | 612 | 80.5 | |
| Antenatal care visit | Yes | 650 | 85.5 |
| No | 110 | 14.5 | |
| BFT counselling during ANC | Yes | 492 | 75.7 |
| No | 158 | 24.3 | |
| Place of delivery | Hospital | 40 | 5.2 |
| Health centre | 632 | 83.2 | |
| Home | 88 | 11.6 | |
| BFT counselling immediately after delivery | Yes | 378 | 56.3 |
| No | 294 | 43.7 | |
| Postnatal care | Yes | 143 | 18.8 |
| No | 617 | 81.2 | |
| Age of the infants | ≤60 days | 307 | 40.4 |
| 60–120 days | 249 | 32.7 | |
| 121–179 days | 204 | 26.9 | |
| Sex of the infants | Male | 322 | 42.4 |
| Female | 438 | 57.6 | |
| Breast problems | Yes | 21 | 2.8 |
| No | 739 | 97.3 | |
| Breastfeeding experiences | Yes | 616 | 81.0 |
| No | 144 | 19.0 | |
| Received postpartum home visit by HEW | Yes | 374 | 49.2 |
| No | 386 | 50.8 | |
| Being member of WDA | Yes | 156 | 20.5 |
| No | 604 | 79.5 | |
| Previous information about BFT | Yes | 506 | 66.6 |
| No | 254 | 33.4 |
ANC, antenatal care; BFT, breastfeeding technique; HEW, health extension worker; WDA, woman development army.
Prevalence of EBT
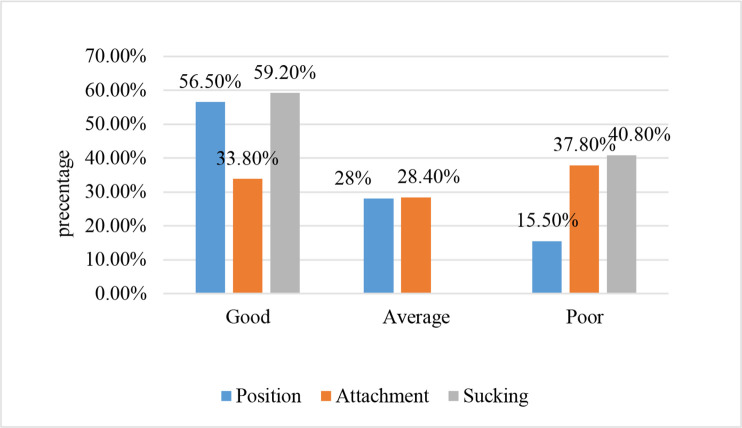
The overall prevalence of mothers who practised EBT was 42.9% (95% CI 39.4% to 46.4%). Good breastfeeding positioning, attachment and sucking were observed among 56.5%, 33.8% and 59.2% of mothers, respectively (figure 1).
Figure 1.
Positioning, attachment and suckling of infant during feeding at Gidan District, North-East Ethiopia, 2021 (n=760).
Factors associated with EBT
After adjusting for potential confounding factors, variables such as ANC follow-up, place of delivery and receiving postpartum home visits by HEWs remained significantly associated with EBT. The odds of EBT among mothers who had ANC follow-up during their index pregnancy was 1.75 times (AOR=1.75, 95% CI 1.10 to 2.77) higher than their counterparts. Similarly, the odds of practising EBT was 2.15 (AOR=2.15, 95% CI 1.25 to 3.68) and about 2.85 (AOR=2.85, 95% CI 1.22 to 6.66) times higher among mothers who had delivered at health centres and hospitals, respectively, compared with those who had delivered at home. Likewise, EBT was twice higher (AOR=2.12, 95% CI 1.55 to 2.92) among respondents who had received postpartum home visits by the HEWs as compared with those who had received no postpartum home visits by the HEWs (table 4).
Table 4.
Association of EBT with different characteristics of lactating mothers in Gidan District, North-East Ethiopia, 2021 (n=760)
| Variables | EBT | COR (95% CI) | AOR (95% CI) | |
| Yes (n, %) | No (n, %) | |||
| Age of the mother, years | ||||
| <20 | 19 (27) | 55 (73) | 1 | 1 |
| 20–25 | 77 (38.6) | 120 (61.4) | 1.86 (0.94 to 3.05) | 1.48 (0.78 to 2.81) |
| 26–30 | 147 (48) | 159 (52) | 2.68 (1.43 to 4.37) | 2.31 (0.91 to 3.70) |
| >30 | 83 (45.4) | 100 (54.6) | 2.40 (1.24 to 4.04) | 1.85 (0.95 to 3.63) |
| Educational status of the mother | ||||
| No formal education | 189 (43.4) | 246 (56.6) | 1 | 1 |
| Primary education | 88 (37.8) | 145 (62.2) | 0.79 (0.57 to 1.09) | 0.79 (0.56 to 1.12) |
| Secondary education and above | 49 (57.3) | 43 (42.7) | 1.48 (0.94 to 2.33) | 1.18 (0.71 to 1.96) |
| Parity | ||||
| Primipara | 49 (33.1) | 99 (66.9) | 1 | 1 |
| Multipara | 277 (45.3) | 335 (54.7) | 1.67 (1.15 to 2.44) | 1.17 (0.75 to 1.83) |
| Antenatal care | ||||
| Yes | 293 (45.1) | 357 (54.9) | 1.92 (1.24 to 2.96) | 1.75 (1.10 to 2.77)* |
| No | 33 (30) | 77 (70) | 1 | 1 |
| Place of delivery | ||||
| Hospital | 22 (57.5) | 18 (42.5) | 3.40 (1.77 to 8.61) | 2.85 (1.22 to 6.66)* |
| Health centre | 283 (44.6) | 349 (55.4) | 2.59 (1.55 to 8.61) | 2.15 (1.25 to 3.68)† |
| Home | 21 (23.9) | 67 (76.1) | 1 | 1 |
| Membership of WDA | ||||
| Yes | 86 (55.1) | 70 (44.9) | 1.86 (1.26 to 2.57) | 1.41 (0.96 to 2.07) |
| No | 240 (39.8) | 364 (60.2) | 1 | 1 |
| Received postpartum visit by HEW | ||||
| Yes | 205 (54.5) | 169 (45.5) | 2.66 (1.93 to 3.49) | 2.12 (1.55 to 2.92)† |
| No | 121 (31.6) | 265 (68.4) | 1 | 1 |
| Brest problem | ||||
| Yes | 6 (28.6) | 15 (71.4) | 0.52 (0.2 to 1.36) | 0.55 (0.20 to 1.51) |
| No | 320 (43.3) | 419 (66.7) | 1 | 1 |
| Residency | ||||
| Urban | 94 (50.3) | 93 (49.7) | 1.49 (1.07 to 2.07) | 1.41 (0.97 to 2.05) |
| Rural | 232 (40.5) | 341 (59.5) | 1 | 1 |
Hosmer-Lemeshow goodness of fit (p=0.22), Multicollinearity test (VIF)=1.68.
*Significant at p<0.05
†Significant at p<0.01
AOR, adjusted OR; COR, Crude Odd Ratio; EBT, effective breastfeeding technique; HEW, health extension workers; VIF, Variance inflation factor; WDA, women development army.
Discussion
EBT is the ideal way of promoting EBF. A baby who breast feeds effectively shows readiness for feeding and latches on deeply at the breast that satisfies the infant’s nutritional requirements and maintains the mother’s comfort.34 This study aimed to determine the prevalence of EBT and identify associated factors among lactating mothers in Gidan District, North-East Ethiopia.
The prevalence of EBF was 42.9% (95% CI 39.4% to 46.4%), which implies that several infants in the study areas are suffering from the aftermaths of suboptimal breastfeeding, such as malnutrition. This finding is in line with the studies conducted in India (43%) and Harar, Ethiopia (43.4%).21 35 However, the result of this study is higher than that of studies conducted in a West Bengal hospital, India (30.3%) and Ari District, southern Ethiopia (36.5%).9 19 The observed discrepancy might be due to the time gap between the studies. Since the former studies were conducted in 2013, in which there have been different strategies, including BFT counseling, promoting institutional delivery, and postpartum home visits by HEWs, that are presumed to improve maternal practices in EBT.36 The existence of some variability in the obstetric characteristics of participants between the studies could also be another reason for the above variation. For instance, the proportion of mothers who had ANC visits and received counselling during the ANC follow-up in this study was higher (75.4%) as compared with the study conducted in southern Ethiopia (59.2%), where having ANC visits and obtaining breastfeeding counselling service during the follow-up showed an improved practice of EBT.9 21 In light of this, the current promotion strategies to improve ANC follow-up and breast feeding should be strengthened to improve BFT and maintain the health of children.
On the other hand, the proportion of EBT in the current study is lower than in previous studies done in Gondar, North-West Ethiopia (48%), Libya (48%), the rural population of India (51%) and West Denmark (52%).7 17 18 20 The possible explanation might be the difference in the study setting, in which the former studies were based at health institutions that recruited mothers who came to the health facilities either for vaccination or PNC services. These populations are usually considered to have better health literacy and opportunities for breastfeeding counselling. In addition, the proportion of educated participants (secondary school and above) was lower (12.1%) in our study compared with the studies conducted earlier (in the rural populations of India (78.1%) and West Denmark (71.1%)). As a result, the prevalence of EBT may be lower than their findings.18 20 Although no association has been observed between the level of education and EBT practice in our study, several shreds of evidence indicate that the level of education impacts individuals' health literacy. It can also be an influencing factor for practising EBT.37
Mothers who had ANC follow-up had higher odds of exhibiting EBT than their counterparts. The finding is consistent with studies conducted in South-East Nigeria.38 Mothers who visit health institutions for ANC follow-up receive counselling about BFT that enhances their awareness, understanding and appreciation of the sequelae of IBT and further promotes their practice.9 39 Moreover, mothers who had ANC follow-up during pregnancy were more likely to have an institutional delivery that makes them lose the opportunity to receive postpartum breastfeeding counselling.9 21 40 Thus, strengthening the existing effort to improve ANC follow-up and institutional delivery would help improve breastfeeding practice beyond preventing life-threatening maternal and neonatal complications.
Likewise, the odds of EBT were 2.15 and 2.85 times higher among participants who had delivered at the health centre and hospital, respectively, as compared with mothers who had delivered at home. The finding is congruent with previous evidence from the Bhaktapur district of Nepal, and Harar, Ethiopia.35 41 Women who had delivered at health institutions might possibly have a better opportunity to receive counselling related to BFT immediately after delivery. That will further have a positive impact on the mothers’ BFT.35 Furthermore, women who had delivered at home were usually less educated and had less access to health messages, which might impact healthy practices, including EBT.42 43
Similarly, postpartum home visits by HEWs have a positive association with adopting EBT. The odds of having EBT was 2.12 times higher among mothers who had received postpartum home visits by HEWs compared with their counterparts. The possible reason could be that women who have received postnatal home visits by the HEW might get breastfeeding counselling and demonstration that will help mothers improve their attitude, knowledge and practice regarding BFT. Furthermore, women who receive postpartum home visits from HEWs may receive psychological support from the HEWs, which further promotes EBTs, as mothers' psychosocial well-being significantly impacts their care and practice towards their baby.44 45 The result is a call for action to further improve postnatal home visits to promote EBT and infant nutrition.
This finding shows more than half of lactating mothers are not practising EBT, which implies thousands of infants are receiving insufficient nutrients to maintain their growth and development. Therefore, it is crucial to counteract the problem by working on the mothers’ skills in BFT.
The study had better strength in measuring the outcome. Since the outcome variable was computed by scores given by different observers, different measures, including delivering training and providing time to practise in a real environment before the data collection, were done to reduce measurement errors and interobserver variability.
On the other hand, this study was not without limitations. Even though all possible strategies such as using female data collectors, providing training for data collectors, employing pretest, using standardised tools, and securing privacy were applied, the study might not be free from bias due to introducing interobserver variability and the Hawthorne effect. In addition, using the HEWs registration book as a sampling frame may introduce selection bias as new lactating mothers might not get registered.
Conclusion
The study revealed that the prevalence of EBT was low. The finding highlights the importance of promoting utilisation of ANC follow-up, institutional delivery and postpartum home visits by HEWs, which play a substantial role in promoting EBT.
Supplementary Material
Acknowledgments
The authors thank the University of Gondar for approving the ethical clearance. The authors also thank the Gidan District administrative offices, study participants, data collectors and supervisors.
Footnotes
Contributors: DBA conceived the idea for this study, developed the proposal, supervised fieldwork, and was involved with the analysis, interpretation and writing of the manuscript. YAH and EGM assisted with the conception of the study, and were involved with the method development, analysis and interpretation of the findings. DZD and WDN participated in the analysis, and were involved with the interpretation of the findings and writing of the manuscript. All the authors have read, revised and approved the final manuscript. DBA is acting as guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All the data generated in this study are included in this manuscript. The data sets used and analysed to produce the current manuscript can be obtained from the corresponding author upon request.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
This study involves human participants and was approved by the Institutional Review Board (IRB) of the University of Gondar, College of Medicine and Health Sciences, Institute of Public Health (Ref. No: IPH/142/2013). Participants gave informed consent to participate in the study before taking part.
References
- 1.Ahmed K, Page A, Arora A. Global Maternal and Child Health Research collaboration (GloMACH)(2020). Associations between infant and young child feeding practices and acute respiratory infection and diarrhoea in Ethiopia: A propensity score matching approach. PloS One 2020;15:e0230978. 10.1371/journal.pone.0230978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kent JC, Ashton E, Hardwick CM, et al. Nipple pain in breastfeeding mothers: incidence, causes and treatments. Int J Environ Res Public Health 2015;12:12247–63. 10.3390/ijerph121012247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedrich MJ. Early initiation of breastfeeding. JAMA 2018;320:1097. 10.1001/jama.2018.13372 [DOI] [PubMed] [Google Scholar]
- 4.Johnson R, Taylor W. Skills for midwifery practice. Elsevier Health Sciences, 2010. [Google Scholar]
- 5.Lassi ZS, Rind F, Irfan O, et al. Impact of infant and young child feeding (IYCF) nutrition interventions on breastfeeding practices, growth and mortality in low- and middle-income countries: systematic review. Nutrients 2020;12:722. 10.3390/nu12030722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHODo C, Health A, Organization WH U. Handbook IMCI: integrated management of childhood illness. World Health Organization, 2005. [Google Scholar]
- 7.Goyal RC, Banginwar AS, Ziyo F, et al. Breastfeeding practices: Positioning, attachment (latch-on) and effective suckling - A hospital-based study in Libya. J Family Community Med 2011;18:74. 10.4103/2230-8229.83372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parashar M, Singh S, Kishore J, et al. Breastfeeding attachment and positioning technique, practices, and knowledge of related issues among mothers in a resettlement colony of Delhi. ICAN: Infant, Child, & Adolescent Nutrition 2015;7:317–22. 10.1177/1941406415602528 [DOI] [Google Scholar]
- 9.Yilak G, Gebretsadik W, Tadesse H, et al. Prevalence of ineffective breastfeeding technique and associated factors among lactating mothers attending public health facilities of South ArI district, southern Ethiopia. PLoS One 2020;15:e0228863. 10.1371/journal.pone.0228863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arts M, Taqi I, Bégin F. Improving the early initiation of breastfeeding: the WHO-UNICEF breastfeeding advocacy initiative. Breastfeed Med 2017;12:326–7. 10.1089/bfm.2017.0047 [DOI] [PubMed] [Google Scholar]
- 11.Collective GB. Global breastfeeding scorecard, 2018: Enabling women to breastfeed through better policies and programmes. Retrieved from UNICEF & WHO website, 2018. Available: https://wwwwhoint/nutrition/publications/infantfeeding/global-bf-scorecard-2018pdf
- 12.Binns C, Lee MK, Low WY, et al. The role of public health nutrition in achieving the sustainable development goals in the Asia Pacific region. Asia Pac J Public Health 2017;29:617–24. 10.1177/1010539517736441 [DOI] [PubMed] [Google Scholar]
- 13.Federal Minstery of Health . National strategy for infant and young child feeding. Ethiopia: Addis Ababa, 2004. [Google Scholar]
- 14.survey DH. Key indicators report. 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA Ethiopia: Ethiopia Demographic and Health Survey, 2016. [Google Scholar]
- 15.KJdS S, Santana GS, TdO V. Prevalence and factors associated with cracked nipples in the first month postpartum. BMC Pregnancy Childbirth 2016;16:1–8. 10.1186/s12884-016-0999-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tiruye G, Mesfin F, Geda B, et al. Breastfeeding technique and associated factors among breastfeeding mothers in Harar City, eastern Ethiopia. Int Breastfeed J 2018;13:1–9. 10.1186/s13006-018-0147-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Safayi BL, Assimamaw NT, Kassie DG. Breastfeeding technique and associated factors among lactating mothers visiting Gondar town health facilities, Northwest Ethiopia: observational method. Ital J Pediatr 2021;47:1–10. 10.1186/s13052-021-01158-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kronborg H, Vaeth M. How are effective breastfeeding technique and pacifier use related to breastfeeding problems and breastfeeding duration? Birth 2009;36:34–42. 10.1111/j.1523-536X.2008.00293.x [DOI] [PubMed] [Google Scholar]
- 19.Dasgupta U, Mallik S, Bhattacharyya K. Breastfeeding practices: positioning, attachment and effective suckling—a hospital based study in West Bengal/Kolkata. Indian J Mater Child Health 2013;15:1–11. [Google Scholar]
- 20.Kishore MSS, Kumar P, Aggarwal AK. Breastfeeding knowledge and practices amongst mothers in a rural population of North India: a community-based study. J Trop Pediatr 2009;55:183–8. 10.1093/tropej/fmn110 [DOI] [PubMed] [Google Scholar]
- 21.Nagendra K, Shetty PN, Rudrappa S, et al. Evaluation of breast feeding techniques among postnatal mothers and effectiveness of intervention: experience in a tertiary care centre. Sri Lanka Journal of Child Health 2017;46:39. 10.4038/sljch.v46i1.8237 [DOI] [Google Scholar]
- 22.Tamiru D, Jisha H. Breastfeeding skills in Arba Minch Zuria: the positioning and attachment initiatives. International Journal of Nursing and Midwifery 2017;9:46–52. 10.5897/IJNM2016.0237 [DOI] [Google Scholar]
- 23.Rinata E, Sari PA. BREASTFEEDING PRACTICES [POSITIONING, ATTACHMENT/LATCH- ON AND EFFECTIVE SUCKLING. SEAJOM: The Southeast Asia Journal of Midwifery 2017;3:1–6. 10.36749/seajom.v3i2.6 [DOI] [Google Scholar]
- 24.World Health Organization . Guideline: protecting promoting and supporting breastfeeding in facilities providing maternity and newborn services. World Health Organization, 2017. [PubMed] [Google Scholar]
- 25.National Guideline for the Management of Acute Malnutrition . FMOH Addis Ababa, 2019. [Google Scholar]
- 26.. Ethiopia commits to ending undernutrition by 2030 with the Seqota Declaration; 2015.
- 27.Yadav K, Agarwal M, Shukla M. Unmet need for family planning services among young married women (15–24 years) living in urban slums of India. BMC women’s health 2020;20:1–17. 10.1186/s12905-020-01010-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tella K, Guruvare S, Hebbar S, et al. Knowledge, attitude, and practice of techniques of breast-feeding among postnatal mothers in a coastal district of Karnataka. Int J Med Sci Public Health 2016;5:28–34. 10.5455/ijmsph.2016.100620159 [DOI] [Google Scholar]
- 29.Network EN. Infant feeding in emergencies. module 2 version 1.0 for health and nutrition workers in emergencies. ENN, 2007. Available: http://www.ennonline.net/ifemodule2
- 30.Stevens WG, Fellows DR, Vath SD, et al. An integrated approach to the repair of inverted nipples. Aesthet Surg J 2004;24:211–5. 10.1016/j.asj.2004.03.003 [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization . Mastitis: causes and management. World Health Organization, 2000. [Google Scholar]
- 32.Aswathaman N, Sajjid M, Kamalarathnam CN, et al. Assessment of breastfeeding position and attachment (abpA) in a tertiary care centre in Chennai, India: an observational descriptive cross-sectional study. Int J Contemp Pediatrics 2018;5:2209. 10.18203/2349-3291.ijcp20184282 [DOI] [Google Scholar]
- 33.World Health Organization . Breastfeeding counselling: a training course. World Health Organization, 1993. [Google Scholar]
- 34.Puapornpong P, Paritakul P, Suksamarnwong M, et al. Nipple pain incidence, the predisposing factors, the recovery period after care management, and the exclusive breastfeeding outcome. Breastfeed Med 2017;12:169–73. 10.1089/bfm.2016.0194 [DOI] [PubMed] [Google Scholar]
- 35.Tiruye G, Mesfin F, Geda B, et al. Breastfeeding technique and associated factors among breastfeeding mothers in Harar City, eastern Ethiopia. Int Breastfeed J 2018;13:5. 10.1186/s13006-018-0147-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.National Reproductive Health Strategy 2016-2020 . Federal Ministry of health (FMOH) Addis Ababa. Ethiopia, 2016. [Google Scholar]
- 37.Adnan N, Muniandy ND. The Relationship between Mothers’ Educational Level and Feeding Practices among Children in Selected Kindergartens in Selangor, Malaysia: A Cross-sectional Study. Asian Journal of Clinical Nutrition 2012;4:39–52. 10.3923/ajcn.2012.39.52 [DOI] [Google Scholar]
- 38.Nduagubam OC, Ndu IK, Bisi-Onyemaechi A, et al. Assessment of breastfeeding techniques in Enugu, south-east Nigeria. Ann Afr Med 2021;20:98. 10.4103/aam.aam_22_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mekuria G, Edris M. Exclusive breastfeeding and associated factors among mothers in Debre Markos, Northwest Ethiopia: a cross-sectional study. Int Breastfeed J 2015;10:1–7. 10.1186/s13006-014-0027-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abeje G, Azage M, Setegn T. Factors associated with institutional delivery service utilization among mothers in Bahir Dar City administration, Amhara region: a community based cross sectional study. Reprod Health 2014;11:1–7. 10.1186/1742-4755-11-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Paudel D, Giri S. Breast feeding practices and associated factors in Bhaktapur district of Nepal: a community based cross-sectional study among lactating mothers. Journal of the Scientific Society 2014;41:108. 10.4103/0974-5009.132851 [DOI] [Google Scholar]
- 42.Fikre AA, Demissie M. Prevalence of institutional delivery and associated factors in Dodota Woreda (district), Oromia regional state, Ethiopia. Reprod Health 2012;9:1–6. 10.1186/1742-4755-9-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wolelie A, Aychiluhm M, Awoke W. Institutional delivery service utilization and associated factors in Banja district, Awie zone, Amhara regional SATE, Ethiopia. Open J Epidemiol 2014;04:30–5. 10.4236/ojepi.2014.41006 [DOI] [Google Scholar]
- 44.Tesfau YB, Kahsay AB, Gebrehiwot TG, et al. Postnatal home visits by health extension workers in rural areas of Ethiopia: a cross-sectional study design. BMC Pregnancy Childbirth 2020;20:1–9. 10.1186/s12884-020-03003-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mannan I, Rahman SM, Sania A, et al. Can early postpartum home visits by trained community health workers improve breastfeeding of newborns? J Perinatol 2008;28:632–40. 10.1038/jp.2008.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data generated in this study are included in this manuscript. The data sets used and analysed to produce the current manuscript can be obtained from the corresponding author upon request.