Abstract
Purpose
Outdoor light exposure is considered a safe and effective strategy to reduce myopia development and aligns with existing public health initiatives to promote healthier lifestyles in children. However, it is unclear whether this strategy reduces myopia progression in eyes that are already myopic. This study aims to conduct an overview of systematic reviews (SRs) reporting time spent outdoors as a strategy to prevent myopia or slow its progression in children.
Methods
We searched the Cochrane Library, EMBASE, MEDLINE and CINAHL from inception to 1 November 2020 to identify SRs that evaluated the association between outdoor light exposure and myopia development or progression in children. Outcomes included incident myopia, prevalent myopia and change in spherical equivalent refraction (SER) and axial length (AL) to evaluate annual rates of myopia progression. The methodological quality and risk of bias of included SRs were assessed using the AMSTAR‐2 and ROBIS tools, respectively.
Results
Seven SRs were identified, which included data from 47 primary studies with 63,920 participants. Pooled estimates (risk or odds ratios) consistently demonstrated that time outdoors was associated with a reduction in prevalence and incidence of myopia. In terms of slowing progression in eyes that were already myopic, the reported annual reductions in SER and AL from baseline were small (0.13–0.17 D) and regarded as clinically insignificant. Methodological quality assessment using AMSTAR‐2 found that all reviews had one or more critical flaws and the ROBIS tool identified a low risk of bias in only two of the included SRs.
Conclusion
This overview found that increased exposure to outdoor light reduces myopia development. However, based on annual change in SER and AL, there is insufficient evidence for a clinically significant effect on myopia progression. The poor methodological quality and inconsistent reporting of the included systematic reviews reduce confidence in the estimates of effect.
Keywords: children, intervention, light exposure, Myopia, outdoor time, overview
Key points.
Overviews of systematic reviews (SRs) provide a comprehensive evidence map in a particular subject area.
Pooled effect estimates from SRs demonstrate that increased time outdoors is associated with a reduction in myopia development, with small and clinically insignificant reductions in refractive error and axial length in eyes that are already myopic.
Outdoor light exposure remains a safe and effective strategy to reduce myopia development and aligns with existing public health initiatives to promote healthier lifestyles in children.
INTRODUCTION
Myopia is a complex ocular refractive condition with a multifactorial aetiology. 1 , 2 The rapid worldwide rise in the prevalence of myopia in the last two to three decades suggests a strong link between environmental factors and development of myopia. 3 Various animal and human studies have reported that exposure to outdoor ambient light plays a protective role in myopia development. 4 , 5 , 6 , 7 , 8 , 9 While recent publications have reported that increasing time spent outdoors might also have an impact on myopia progression, there is some uncertainty regarding its inhibitory role on axial elongation. 6 , 9 , 10 Although a number of hypotheses have been proposed for the protective effect of outdoor light including triggering dopamine release from the retina, 11 , 12 decreased pupil size due to high illumination thereby increasing the depth of focus and reducing retinal image blur 13 , 14 and exposure to shorter wavelengths of light, 15 , 16 , 17 , 18 , 19 , 20 , 21 the precise mechanism still remains unclear.
Overviews of systematic reviews (SRs) aim to systematically retrieve and summarise the results of multiple SRs to provide a comprehensive evidence map in a particular subject area. An initial scoping of the literature on the role of time outdoors and myopia identified at least five recently published SRs. 22 , 23 , 24 , 25 , 26 The objective of this overview is to synthesise and summarise the evidence on efficacy of outdoor light exposure on myopia prevalence, incidence and progression.
METHODS
This overview was conducted in accordance with the criteria for conducting overviews of SRs described in Chapter 5 of the Cochrane Handbook for Systematic Reviews of Interventions. 27 Prior to the start of the review process, the protocol was registered with the International prospective register of systematic reviews (PROSPERO registration number CRD42020214523). 28
Search methods for identification of reviews
We searched the following electronic databases: Cochrane Database of Systematic Reviews (CDSR), Database of Abstracts of Reviews of Effects (DARE), EMBASE, MEDLINE and CINAHL for relevant SRs. No date or language restriction was incorporated in the search strategy. The last date of search was 1 November, 2020. The search was supplemented by scanning the reference list of included reviews. To identify any ongoing SRs, protocols were searched in SRs registries, such as CDSR and PROSPERO. The search strategy for MEDLINE Central is provided in Appendix 1, and an individual search strategy for each of the databases is provided in File S1.
Selection of reviews and assessment of eligibility criteria
Two reviewers (RD and RS) independently screened the titles and abstracts to identify potentially relevant studies for full text review. The full text of potentially relevant studies was assessed independently by the same reviewers to determine if they met the inclusion criteria. The inclusion criteria were: (i) any SRs (with or without meta‐analysis) that had evaluated the association between outdoor light exposure and myopia incidence, prevalence or progression in children; (ii) outdoor light exposure quantified either in the form of illuminance level (measured as lux) or total time spent outdoors (measured as number of exposure hours per day or per week) and (iii) age of participants ≤18 years, with or without myopia at baseline. Reviews were not excluded based on the type/form of interventions assigned to the participants for outdoor light exposure, nor the design of included studies e.g., cross‐sectional, cohort or randomised controlled trials. If a review included both children and adults, the required data from children only were extracted. Pairs of review authors (RD and BH, or RD and RS) independently extracted data from the included reviews on a previously piloted data extraction form. These data are represented in Table 1. The criteria for defining a systematic review were adopted from Martinic et al. 29 Discrepancies were resolved through discussion between the two reviewers and when required, a third reviewer was consulted (JGL).
TABLE 1.
Characteristics of included systematic reviews in the overviews
| Review (Study design) | Number and name of databases searched (last date of search) | No. of primary studies included & type of study design | Definition of myopia | Total population included in review | Ethnicity & age groups (years) | Details of intervention | Review outcomes |
|---|---|---|---|---|---|---|---|
| Sherwin et al. 23 (SR & MA) | 4, MEDLINE, Web of Science, EMBASE and CENTRAL (Sept 2011) | 23; 15 CS, 7 cohort and 1 RCT. MA was performed only in 7 CS | ≤−0.50 D | 23,739 | Caucasian, Turkish, Asian; 0.5–20 | CS‐ Duration of outdoor exposure was recorded through questionnaires. Definition of exposure were sports, outdoor and sports, & only outdoor sports. | Quantitative‐ Myopia prevalence; Narrative‐ Myopia prevalence, myopia incidence and change in SER |
| Xiong et al. 24 (SR & MA) | 3, PubMed, EMBASE and Cochrane library (Dec 2015) | 51; 4 CT, 17 cohort studies, and 30 CS. MA was performed in 25 studies | NR | 72,327 | Chinese, Caucasian, Indian, Malays, Mongolian, East Asian, African‐American, Turkish; 4–79 |
CT‐ 40 min additional outdoor activities during school days vs. control; additional 40 min ROC programme vs. control; 80 min ROC programme vs. control and >14 h/week outdoor activities vs. control. Cohort studies‐ Duration of outdoor exposure were recorded through interview or questionnaires administered to parents. CS‐ Duration of outdoor exposure was recorded through questionnaires administered either to participants or parents |
Quantitative‐ Myopia prevalence, myopia incidence, and change in SER |
| Deng and Pang 26 (SR & MA) | 6, Scopus, MEDLINE, EMBASE, VisionCite, PubMed and Cochrane library (March 2016) | 5; 2 RCT, 2 cluster RCT and 1 NR about randomization | NR | 3,272 | Chinese; 6–18 | CT‐ 40 min additional outdoor activities during school days vs. control; 80 min ROC programme vs. control; ROC programme vs. control; additional 40 min ROC programme vs. control and >14 h/week outdoor activities vs. control | Quantitative‐ Myopia incidence, change SER, change in AL |
| Ho et al. 22 (SR & MA) | 6, Cochrane Library, MEDLINE, CINAHL, PubMed, China Academic Journals full‐text database and National Digital Library of Theses and Dissertations in Taiwan (2019) | 13; 6 CT, 3 cohort studies, and 4 CS | NR | 15,081 | Chinese, East Asian, Hispanic, Caucasian; 4–14 |
CT‐ 7 h/week of outdoor exposure including recess and physical education vs. control; 7 h/week of exposure and extra 5 h/week after school vs. control; 80 min ROC programme vs. no special programme; ROC programme for 200 min/5 days vs. control; 40 min additional outdoor activities during school days vs. control; 2 additional 20 min recess programmes vs. control and >14–15 h/week of outdoor activities vs. control Cohort studies‐ Outdoor light exposure was recorded through questionnaires CS‐ Outdoor light exposure was recorded through questionnaires |
Quantitative‐ Myopia prevalence, myopia incidence, change in SER and change in AL |
| Cao et al. 25 (SR & MA) | 5, PubMed, Science Direct, Cochrane Library, Chinese National Knowledge Infrastructure and Wanfang (Oct 2018) | 5; 1 RCT, 4 cluster RCT | <−0.50 D | 3,014 | Chinese; 6–12 | CT‐ >14–15 h/week of outdoor activities vs. control; 2–3 h outdoor hikes/sports/activities on weekends at least twice/month vs. control; additional 40‐min outdoor activity in school days vs. control; 2 additional recess programmes of 20 min each in school days vs. control and ≥11 h of outdoor activities in 7 days vs. control | Quantitative‐ Myopia incidence, change in SER and change in AL |
| Anandita and Barliana 37 (Narrative review) | 1, MEDLINE (NR) | 13; 8 CS, 5 Cohort | Ranged from <−0.50 to ≤−1.00 D | 29,301 | Chinese, East Asian, African, Caucasian, Arabian, Hispanic; 0–18 |
Cohort studies‐ Outdoor light exposure was recorded through questionnaires CS‐ Outdoor light exposure was recorded through questionnaires |
Narrative: Myopia prevalence and myopia incidence |
| Eppenberger and Sturm 36 (Narrative review) | 2, PubMed and Cochrane Library (Jan 2019) | 12; 3 CT, 7 cohort and 2 CS | Ranged from ≤−0.50 to ≤−1.00 D | 32,381 | Chinese, Malay, East Asian, Indian, African, Hispanic; 6–18 |
CT‐ Additional 40 min of outdoor activities on each school day vs. control; 2 additional 20 min of ROC programme vs. control; ≥11 h of outdoor activities in 7 days vs. control Cohort studies‐ Outdoor light exposure was recorded through questionnaires CS‐ Outdoor light exposure was recorded through questionnaires |
Narrative: Myopia prevalence, myopia incidence and change in SER |
Abbreviations: CS, Cross‐sectional; CT, Clinical trial; MA, Meta‐analysis; NR, Not reported; RCT, Randomised clinical trial; ROC, Recess outside classroom; SER, Spherical equivalent refraction; SR, Systematic review; TSO, Time spent outdoors.
Types of outcome measures
Primary outcomes
Efficacy of outdoor light exposure to prevent myopia onset measured as the number of cases of incident myopia for each year of follow‐up.
Efficacy of outdoor light exposure to control myopia progression measured as change in spherical equivalent refraction (SER) for each year of follow‐up.
Secondary outcomes
Association between outdoor light exposure and myopia prevalence.
Efficacy of outdoor light exposure to control myopia progression measured as change in axial length (AL) for each year of follow up.
Quality and risk of bias assessment
The assessment of methodological quality and risk of bias (ROB) of the included SRs were conducted by pairs of review authors (RD and JGL, or RD and PKV). The methodological quality was assessed according to the criteria specified in the ‘A Measurement Tool to Assess Systematic Reviews 2’ (AMSTAR‐2) tool, 30 and risk of bias was assessed using the ‘Risk of Bias in Systematic Reviews’ (ROBIS) tool. 31 Discrepancies between the two authors were resolved through discussion, or when required, a third reviewer was consulted (PKV or JGL).
Data synthesis, presentation and analysis
A PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐analysis) 2020 flow diagram 32 was used to summarise the selection of SRs. The characteristics of included and excluded SRs are tabulated descriptively and presented in Table 1. The outcome of AMSTAR‐2 and ROBIS assessments were represented in tabular and graphical format, respectively. Quantitative outcome data i.e., pooled estimates of primary and secondary outcome measures were presented as they were reported in the SRs i.e., odds ratio (OR) with 95% confidence interval (CI) for myopia prevalence, odds ratio or risk ratio (RR) with 95% CI for myopia incidence, mean difference (MD) with 95% CI for change in SER and AL. Forest plots were used to compare pooled estimates graphically, constructed using Review Manager (RevMan) software version 5.4.1 (The Cochrane Collaboration, revman.cochrane.org). 33
For reviews reporting myopia incidence as an OR, the OR was converted to a RR using the formula described by Zhang and Yu. 34 Continuous outcome data, i.e., change in SER and AL, were summarised as MD with 95% CI in the forest plot. The outcome measures for change in SER and AL were standardised to 1‐year time duration. One of the reviews reported a pooled estimate of change in SER over a period of 3 years. This was standardised to 1 year by dividing the overall MD by 2.3, because this review multiplied 1‐year follow‐up data from the primary studies by 2.3 to convert to 3‐years follow‐up data, considering reduction in myopia progression with age. 24
A citation matrix was created to demonstrate the amount of overlap of primary studies between the included systematic reviews. The Corrected Covered Area (CCA) was calculated to provide a quantitative measure of the extent of overlap in the primary studies. 35 CCA was calculated using the formula: CCA = (N−r)/(rc−r), where N = sum of total primary studies included in all the reviews, r = number of rows containing unique primary studies and c = number of columns, i.e., number of reviews.
RESULTS
Search results
Bibliographic database searches identified 124 studies, of which 11 were duplicates. After screening titles and abstracts, 108 studies were excluded, and the full text of the remaining five studies were assessed for eligibility. All five SRs were included in this overview. 22 , 23 , 24 , 26 , 36 Reference list scanning of included reviews identified four additional records that were assessed for eligibility, 25 , 37 , 38 , 39 of which two were included. 25 , 37 Thus, a total of seven studies were included in the overview (Figure 1).
FIGURE 1.
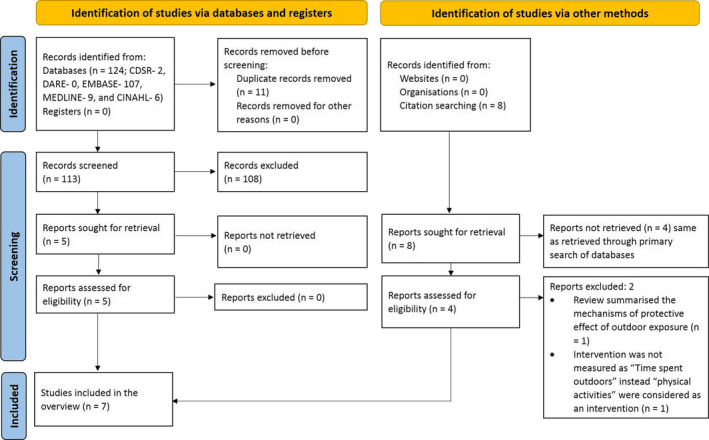
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram presenting the process of study identification, screening and selection of systematic reviews
Characteristics of included reviews
Table 1 summarises the characteristics of the included SRs. The total number of participants included in the reviews was 179,115 (63,920 unique participants), of which 117,433 (40,981 unique participants) were included in the quantitative synthesis. The definition of myopia was reported in four SRs, ranging from ≤−0.50 to ≤−1.00 D. 23 , 25 , 36 , 37 The majority of participants were younger than 18 years, although two reviews included older adults. 23 , 24 The included population were Caucasian, Turkish, East Asian, Chinese, Indian, Malay, Mongolian, African‐American and Hispanic. 22 , 23 , 24 , 25 , 26 , 36 , 37 The details of interventions and reported outcomes are provided in Table 1. The characteristics of excluded SRs along with the justification for exclusion are detailed in the File S2.
Risk of bias assessment
Table 2 summarises the methodological quality of included SRs, assessed using AMSTAR‐2. None of the SRs had registered or published a protocol prior to conducting the review, nor reported a list of excluded studies. Four SRs formally conducted a ROB assessment of included studies using a validated tool, one partially assessed ROB, and two SRs did not conduct an assessment of bias. Other methodological limitations included the lack of a comprehensive search strategy and poor justification for included study designs; three SRs failed to perform data extraction in duplicate.
TABLE 2.
Methodological quality of the included systematic reviews as judged by the AMSTAR‐2 instrument
| Items | Deng and Pang 26 | Sherwin et al. 23 | Anandita and Barliana 37 | Xiong et al. 24 | Ho et al. 22 | Cao et al. 25 | Eppenberger and Sturm 36 |
|---|---|---|---|---|---|---|---|
| 1. Did the research questions and inclusion criteria for the review include the components of PICO? | |||||||
| 2. Did the report of the review contain an explicit statement that the review methods were established prior to conduct of the review and did the report justify any significant deviations from the protocol? | |||||||
| 3. Did the review authors explain their selection of the study designs for inclusion in the review? | |||||||
| 4. Did the review authors use a comprehensive literature search strategy? | |||||||
| 5. Did the review authors perform study selection in duplicate? | |||||||
| 6. Did the review authors perform data extraction in duplicate? | |||||||
| 7. Did the review authors provide a list of excluded studies and justify the exclusions? | |||||||
| 8. Did the review authors describe the included studies in adequate detail? | |||||||
| 9. Did the review authors use a satisfactory technique for assessing the risk of bias (ROB) in individual studies that were included in the review? | |||||||
| 10. Did the review authors report on the sources of funding for the studies included in the review? | |||||||
| 11. If meta‐analysis was justified, did the review authors use appropriate methods for statistical combination of results? | |||||||
| 12. If meta‐analysis was performed, did the review authors assess the potential impact of ROB in individual studies on the results of the meta‐analysis or other evidence synthesis? | |||||||
| 13. Did the review authors account for ROB in individual studies when interpreting/ discussing the results of the review? | |||||||
| 14. Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review? | |||||||
| 15. If they performed quantitative synthesis, did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review? | |||||||
| 16. Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review? |
Abbeviations: PICO, Patient Intervention Comparator Outcom.
Note: Colour coding indicates whether the study satisfied each AMSTAR‐2 item. Red = no; Green = yes; Blue = partially yes, and Yellow = not applicable. The grey shaded items represent critically important domains.
Figure 2 shows the results of the ROBIS assessment. The ROBIS tool is divided into four domains. For Domain 1 (Study eligibility criteria), two reviews 36 , 37 were rated as ‘high concern’ based on restricted eligibility criteria of the included studies. For Domain 2 (Identification and selection of studies), five SRs 24 , 25 , 26 , 36 , 37 were judged to be of high concern due to lack of a comprehensive search strategy or imposing language restrictions (studies published in English only). Furthermore, two SRs had no information on the number of authors involved in the identification and selection of the primary studies. 36 , 37 With regards to Domain 3 (Data collection and study appraisal), four SRs 23 , 26 , 36 , 37 were judged to be of high concern due to issues regarding the methods used to collect data and appraise studies (no formal ROB assessment was undertaken in two SRs). In Domain 4 (Synthesis and findings), high concerns were identified in four out of five reviews. The major concern in two reviews 22 , 26 was inappropriately combining results from different study designs. Two reviews 24 , 37 did not include results from all of the included primary studies to pool final estimates and the reason for excluding them was not reported. The ROBIS assessment for each of the included SRs is available in File S3.
FIGURE 2.
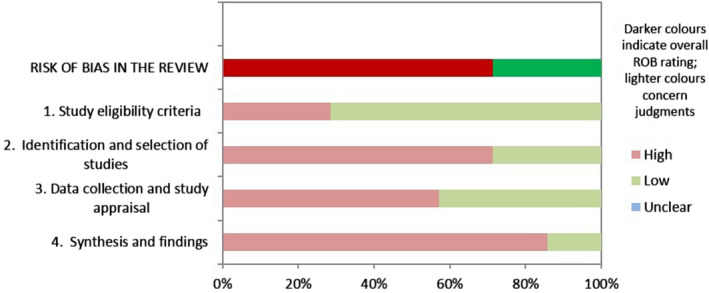
Graphical representation of Risk of Bias Assessment Tool for Systematic Reviews (ROBIS) assessment in seven included systematic reviews
Overlapping of primary studies
The citation matrix showing the overlap of primary studies among seven SRs is presented in File S4. Using the formula mentioned in the methods section, we found CCA of 17.7%. Guidelines for interpreting CCA 35 suggest that values greater than or equal to 15% indicate high overlap.
Efficacy of outdoor light exposure
Myopia prevalence
Three out of the seven SRs synthesising data from a total of 24,889 unique participants reported the association between outdoor light exposure and myopia prevalence (Table 3 and Figure 3). 22 , 23 , 24 All the reviews found a weak association between outdoor light exposure and myopia prevalence with an overall 2%–5% reduction in the odds of developing myopia for each additional hour spent outdoors per week.
TABLE 3.
Myopia prevalence reported in included systematic reviews and meta‐analyses
| Review study | Number of subjects (Number and design of primary studies) | Duration of effect (years) | Measure of effect (95% CI) | Direction of effect |
|---|---|---|---|---|
| Sherwin et al. 23 | 9,885 (7, CS) | NA | OR 0.98 (0.97, 0.99) | Favours high outdoor exposure |
| Xiong et al. 24 | 23,112 (13, CS) | NA | OR 0.96 (0.94, 0.98) | Favours high outdoor exposure |
| Ho et al. 22 | 5,745 (4, CS) | NA | OR 0.95 (0.92, 0.99) | Favours high outdoor exposure |
Abbreviations: CI, Confidence interval; CS, Cross‐sectional studies; NA, Not applicable; OR, Odds ratio.
FIGURE 3.
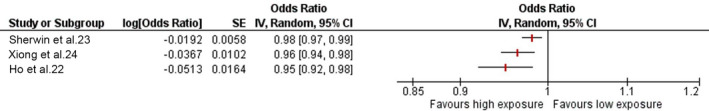
Forest plot showing pooled estimates of association between outdoor light exposure and myopia prevalence
Myopia incidence
Four out of the seven SRs synthesising data from a total of 7783 unique participants (3161 participants from clinical trials and 4622 participants from cohort studies) reported the association between outdoor light exposure and myopia incidence (Table 4 and Figure 4). Two of the reviews reported outcomes over a period of 1 year, 22 , 26 one review reported outcomes over a period of 3 years 24 and one did not report the duration over which the effect was observed. 25 Likewise, one of the four reviews reported measure of outcome as OR, whilst the others reported as RR with 95% CI.
TABLE 4.
Myopia incidence reported in included systematic reviews and meta‐analyses
| Review study | Number of subjects (Number and design of primary studies) | Duration of effect (years) | Measure of effect (95% CI) | Measure of effect standardised to RR (95% CI) | Direction of effect |
|---|---|---|---|---|---|
| Xiong et al. 24 | 2,865 (3, CT) | 3 | RR 0.54 (0.34, 0.85) | RR 0.54 (0.34, 0.85) | Favours high outdoor exposure |
| Deng and Pang 26 | 2,885 (4, CT) | 1 | RR 0.66 (0.49, 0.89) | RR 0.66 (0.49, 0.89) | Favours high outdoor exposure |
| Cao et al. 25 | 2,590 (3, CT) | NR | RR 0.76 (0.67, 0.87) | RR 0.76 (0.67, 0.87) | Favours high outdoor exposure |
| Ho et al. 22 | 4,714 (5, CT) | 1 | OR 0.50 (0.37, 0.69) | RR 0.54 (0.37, 0.79) | Favours high outdoor exposure |
| Xiong et al. 24 | 4,064 (2, Cohort) | 3 | RR 0.57 (0.40, 0.83) | RR 0.57 (0.40, 0.83) | Favours high outdoor exposure |
| Ho et al. 22 | 4,622 (3, Cohort) | 1 | OR 0.57 (0.35, 0.92) | RR 0.61 (0.41, 0.92) | Favours high outdoor exposure |
Abbreviations: CI, Confidence interval; CT, Clinical trial; NR, Not reported; OR, Odds ratio; RR, Risk ratio.
FIGURE 4.
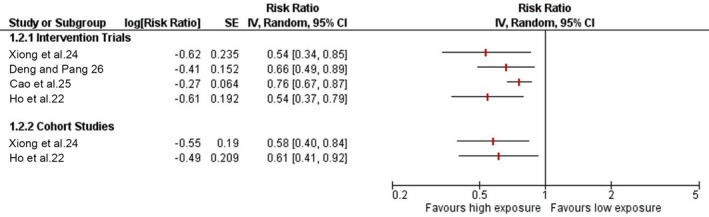
Forest plot showing pooled estimates of myopia incidence over a period of 1 year from baseline. *Reported change in 3 years
All four SRs reported a significantly reduced risk of myopia development in children with increased hours of outdoor activities (Table 4 and Figure 4). Of the SRs which included only clinical trials, the risk of developing myopia from baseline ranged from 0.54 to 0.76. The estimates from cohort studies were similar to that of intervention studies.
Change in myopic refractive error
Four out of seven SRs synthesising data from a total of 4406 unique participants reported the effect of outdoor light exposure against change in SER (Table 5 and Figure 5). Two reviews reported the change over a period of 1 year, 22 , 26 one over a period of 3 years 24 and one did not report the duration of effect. 25 All included SRs reported lower rates of myopia progression in the higher light exposure group with annual mean reduction in progression ranging between 0.13 to 0.17 D.
TABLE 5.
Change in spherical equivalent refractive error reported in included systematic reviews and meta‐analyses
| Review study | Number of subjects (Number and design of primary studies) | Duration of effect (years) | Measure of effect (D), MD (95% CI) | Measure of effect standardised to 1 year (D) MD (95% CI) | Direction of effect |
|---|---|---|---|---|---|
| Xiong et al. 24 | 2,865 (3, CT) | 3 | 0.30 (0.18, 0.41) | 0.13 (0.08, 0.18) | Favours high outdoor exposure |
| Ho et al. 22 | 4,406 (6, CT) | 1 | 0.15 (0.09, 0.22) | 0.15 (0.09, 0.22) | Favours high outdoor exposure |
| Cao et al. 25 | 2,729 (4, CT) | NI | 0.17 (0.16, 0.18) | 0.17 (0.16, 0.18) | Favours high outdoor exposure |
| Deng and Pang 26 | 3,272 (5, CT) | 1 | 0.13 (0.08, 0.18) | 0.13 (0.08, 0.18) | Favours high outdoor exposure |
Abbreviations: CI, Confidence interval; CT, Clinical trials; D, Dioptres; MD, Mean difference.
FIGURE 5.
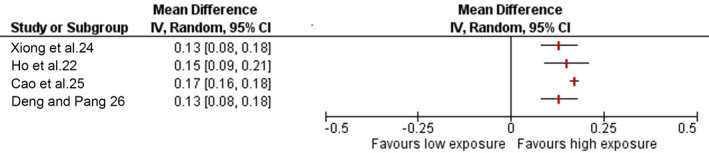
Forest plot showing pooled estimates of change in spherical equivalent refraction (SER) from baseline (1 year). *Did not report duration over which change was assessed
Change in axial length
Three of the seven SRs synthesising data from a total of 3,903 unique participants reported the effect of high outdoor light exposure against change in axial length (Table 6 and Figure 6). 22 , 25 , 26 The forest plot in Figure 6 shows the direction of effect for all of the three SRs. The pooled MD change over a period of 1 year from baseline ranged from −0.03 mm to −0.08 mm.
TABLE 6.
Change in axial length reported in included systematic reviews and meta‐analyses
| Review study | Number of subjects (Number and design of primary studies) | Duration of effect (years) | Measure of effect (mm) (95% CI) | Direction of effect |
|---|---|---|---|---|
| Deng and Pang 26 | 2,658 (3, CT) | 1 | MD −0.03 (−0.05, 0.00) | Favours high outdoor exposure |
| Cao et al. 25 | 2,658 (3, CT) | NI | MD −0.03 (−0.03, −0.03) | Favours high outdoor exposure |
| Ho et al. 22 | 3,903 (4, CT) | 1 | MD −0.08 (−0.14, −0.02) | Favours high outdoor exposure |
Abbreviations: CI, Confidence interval; CT, Clinical trials; MD, Mean difference.
FIGURE 6.
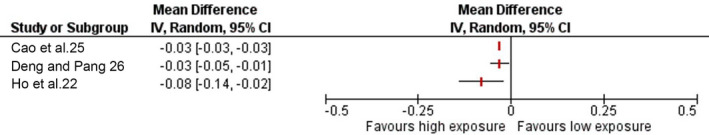
Forest plot showing pooled estimates of change in axial length from baseline (1 year). *Did not report duration over which change was assessed
The conclusions of the two narrative reviews were consistent with those having a quantitative synthesis. Eppenberger and Sturm critically analysed the role of time exposed to outdoor light and concluded that increased outdoor light exposure could potentially lower the rate of myopia prevalence and incidence, as well as slow its progression. 36 Likewise, Anadita and Barliana also reported the protective effect of outdoor light exposure against myopia incidence. 37
DISCUSSION
This overview aimed to bring together, appraise and synthesise the results of related systematic reviews that evaluated the relationship between outdoor light exposure and myopia. The overview summarised the results of seven SRs that included data from 47 unique primary studies published between 1977 and 2018, and synthesising data from 63,920 participants. The cumulative evidence suggests that exposure to higher outdoor light levels is associated with a reduction of myopia prevalence and incidence in children and provides equivocal evidence for a reduction in myopia progression (based on change in SER and axial length) in those who were already myopic.
The earlier the onset of myopia, the greater the likelihood of high myopia later in life, 40 , 41 increasing the risk of developing myopia related pathology, 42 , 43 , 44 with a reduction in quality of life 45 and an associated economic burden. 46 , 47 Each dioptre progression of myopia is shown to increase the likelihood of developing myopic maculopathy by 40% irrespective of the degree of myopic refractive error. 48 Although the sight‐threatening pathologies associated with myopia usually occur later in life, the underlying myopia develops during childhood, and therefore interventions to prevent or reduce the progression of myopia need to be delivered during this period. Increased exposure to outdoor light is the safest, most cost‐effective and non‐invasive intervention to prevent or delay the onset of myopia.
Three SRs investigated the relationship between outdoor light exposure and myopia prevalence and reported pooled estimates from a meta‐analysis of cross‐sectional studies. 22 , 23 , 24 These reviews reported effect sizes ranging from a 2%–5% reduction in the odds of developing myopia for each additional hour spent outdoors per week. Estimates of incident myopia were reported in four reviews. 22 , 24 , 25 , 26 The pooled effect sizes from cohort and intervention studies were similar; exposure to higher level of outdoor light was associated with a 39%–43% relative risk reduction in incident myopia from cohort studies, and 24%–46% relative risk reduction from clinical trials.
In addition to the reported benefits of outdoor light exposure on preventing myopia, time spent outdoors also has other health benefits. The most recent report from International Myopia Institute concluded that ‘compared with other measures, spending more time outdoors is the safest strategy and aligns with other existing health initiatives, for example, obesity prevention, by promoting a healthier lifestyle for children and adolescents’. 49 Several public health policies based on outdoor light exposure are already implemented in China, Taiwan, Singapore and other East Asian countries at school level to prevent or delay the onset of myopia. 6 , 10 , 50 , 51 Some interventions suggested in the literature include a minimum one hour of recess outside the classroom; classrooms with many large windows; increasing awareness among parents and school children on the importance of outdoor light exposure; community centres to organise outdoor games/programmes to motivate children's participation; concept of nature kindergartens and school excursions to outdoor areas. 52 , 53 , 54
Whilst there is a consensus on the protective effect of outdoor light exposure on preventing the onset of myopia, its role in slowing progression in eyes that are already myopic remains controversial. Four SRs 22 , 24 , 25 , 26 provided pooled estimates of changes in SER and AL from prospective intervention trials. One review 24 reported that additional time outdoors was ineffective in slowing myopia progression, based on a sub‐group analysis of SER in myopic subjects only and the lack of a dose‐response relationship. By contrast, three other reviews 22 , 25 , 26 concluded that additional time spent outdoors helped to slow progression in terms of change in SER and AL. The magnitude of the annual reduction in SER ranged from 0.13 to 0.17 D, which is consistent with a reduction of 0.03 to 0.08 mm change in AL. A consensus workshop, Controlling the Progression of Myopia, sponsored by the United States Food and Drug Administration (FDA) and attended by experts in myopia from several professional organisations, concluded that a minimum difference in refractive error of 0.75 D between the treatment groups would be considered clinically significant over a period of 3 years (change of 0.25 D annually). 55 This corresponds to an approximate change of 0.11 mm/year in axial length. Based on these minimal changes needed in SER or AL to claim clinical significance, the estimates of annual change in SER and AL reported in the included reviews are noticeably lower than 0.25 D and 0.11 mm, respectively.
We used two validated critical appraisal tools to evaluate the methodological quality and ROB of the included SRs in this overview. Five out of seven SRs were judged as “high concern” in ROBIS assessment. The major concerns were the lack of a registered or published protocol before conducting SR, language restriction during the search process, not conducting study selection and data extraction in duplicate and inappropriately combining results during meta‐analysis. Two SRs inappropriately combined results from different study designs. 25 , 26 The Cochrane Handbook for Systematic Reviews of Interventions recommends not to combine results from different study designs in view of high heterogeneity and different sources of bias that could lead to imprecise estimates. 56 Three SRs did not mention involvement of two authors to independently duplicate the steps of review process. 23 , 36 , 37 Involvement of two review authors working independently and the presence of a third author in the review process to resolve discrepancies is a vital step of a systematic review that helps in minimising errors in selecting studies, extracting data and conducting ROB. 57 The limitations in the conduct of the SRs included in this overview need to be taken into account when considering the precision of the pooled estimates and how certain we can be that the effect estimates are adequate to support a recommendation.
A strength of the current overview is the methodology adopted to conduct the review process, which is consistent with best practice. 27 A protocol was registered prior to conducting the overview, a robust search matrix was designed, multiple authors were involved in the review process and standard tools were used to assess the methodological quality and ROB of the reviews. Given that majority of these reviews included children younger than 18 years of age and of different ethnicities, the results of this overview are generalisable to most ethnic groups, with cautious application in context to an adult population above 18 years of age. There are several limitations of the evidence base that are worth highlighting. First, despite axial length being the most reliable and repeatable parameter to measure myopia progression, relatively few of the included clinical trials (n = 4) measured axial length. It is important that future longitudinal studies and clinical trials investigating efficacy of time spent outdoors in controlling myopia include axial length as well as refractive error as primary outcome measures. Second, many of the included studies used participant self‐reporting to obtain information about time spent outdoors from parents and/or children. Studies have identified a poor correlation between subjectively obtained versus objectively measured information on outdoor activity. 58 , 59 More recent observational studies and clinical trials have used light trackers to quantify the amount of light exposure and total duration of time spent outdoors objectively. 8 , 9 , 60 , 61 , 62 Future trials should continue to use such objective measures to define light exposure more accurately. Third, the majority of studies investigated the role of outdoor light exposure in isolation. However, there are several other factors such as parental myopia, urbanisation, educational level, duration and distance of near work, which could interact and contribute to myopiogenesis. 63 , 64 , 65 Interaction between near work and outdoor light exposure has been reported in the literature suggesting slower myopia progression in children who spent more time outdoors and less time performing near work and vice‐versa. 64 , 66 These complex behavioural variables act as confounders which need to be considered when investigating the causal relationship between environmental factors and myopia development.
There is a paucity of evidence concerning the efficacy of outdoor light exposure against myopia onset or progression in adults. Likewise, the dose‐response relationship between (a) the illuminance level and (b) the duration of exposure to outdoor light and myopia warrants further investigation. While the role of different wavelengths of light in myopiogenesis is being investigated through short‐term experimental designs in humans, 15 , 67 the potential role of wavelength of light in controlling myopia progression needs to be explored further through clinical trials.
In conclusion, the current overview of SRs provides evidence for the protective effect of outdoor light exposure against the development of incident myopia. Increased outdoor light exposure should therefore be recommended as a safe and effective strategy to reduce myopia development. Furthermore, the intervention aligns with existing public health initiatives to promote healthier lifestyles in children. However, the impact of time outdoors in slowing myopia progression in eyes that are already myopic remains uncertain. Poor methodological quality and inconsistent reporting of the included systematic reviews reduces the confidence in the estimates of effect. We recommend that systematic reviewers should consult PRISMA and AMSTAR when conducting and reporting systematic reviews. Furthermore, developers of clinical practice guidelines should consider methodological quality when guideline recommendations are underpinned by systematic reviews.
CONFLICT OF INTEREST
The authors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article.
AUTHOR CONTRIBUTIONS
Rohit Dhakal: Data curation (equal); Formal analysis (lead); Methodology (lead); Project administration (lead); Writing – original draft (lead); Writing – review & editing (lead). Rakhee Shah: Data curation (equal); Methodology (equal); Writing – review & editing (equal). Byki Huntjens: Data curation (equal); Methodology (equal); Writing – review & editing (equal). Pavan K Verkicharla: Data curation (equal); Methodology (equal); Writing – review & editing (equal). John G Lawrenson: Conceptualization (lead); Data curation (equal); Methodology (equal); Supervision (lead); Writing – review & editing (equal).
Supporting information
File S1
File S2
File S3
File S4
ACKNOWLEDGEMENT
We acknowledge Steve O’Driscoll, Information Specialist at City, University of London for his help in creating the search matrix for each database. This work was partly supported by the DST ‐ Inspire Faculty Award (DST/INSPIRE/04/2018/003087) to PKV.
Biography

John Lawrenson studied optometry at Aston University, graduating with a first class honours degree. After a pre‐registration year at Moorfields Eye Hospital London, he completed a College of Optometrists‐funded postgraduate scholarship at City, University of London, leading to a PhD in Visual Science. Following a post‐doctoral research fellowship in neuroscience at University College London, he returned to join the academic staff at City, where he currently holds a chair in Clinical Visual Science.
Professor Lawrenson’s interests lie in basic and clinical medical sciences. He has edited the eye and orbit sections in the last three editions of Grays Anatomy, probably the best‐known anatomy textbook in the world. He is an advocate for evidence‐based clinical practice, holds a Master’s degree in Evidence‐based Healthcare from the University of Oxford, and is a Co‐ordinating Editor for the Cochrane Eyes and Vision review group.
Professor Lawrenson’s main research interests lie in the diagnosis and management of age‐related eye disease; particularly glaucoma, diabetic eye disease and age‐related macular degeneration (AMD). He has published over 100 peer‐reviewed papers and authored 8 book chapters.
APPENDIX 1.
Search strategy for medline central database
S1. (MH "Child") OR (MH "Child, Preschool") OR (MH "Adult") OR (MH "Adolescent")
S2. AB child* OR AB student* OR AB "school age*" OR AB "school children" OR AB juvenile OR AB kid* OR AB teen* OR AB adolescen* OR AB youth* OR AB preschool* OR AB adult* OR AB p#ediatric
S3. S1 OR S2
S4. AB "Time N3 outdoor*" OR AB "environment* N3 exposure*" OR AB outdoor* OR AB "physical activit*" OR AB "outdoor activiti*" OR AB outside OR AB natur* OR AB exercise* OR AB "play* N3 outdoor" OR AB "light N3 expos*" OR AB leisure OR AB sport* OR sunlight OR daylight OR daytime
S5. (MH "Myopia") OR (MH "Myopia, Degenerative")
S6. AB myopi* OR AB myope* OR AB nearsight* OR AB near‐sight* OR AB shortsight* OR AB short‐sight* OR AB "refractive error*" OR AB refracti*
S7. S5 OR S6
S8. (MH "Control")
S9. AB prevent* OR AB control OR AB prophyla* OR AB therapy OR AB intervention* OR AB strateg*
S10. S8 OR S9
S11. S7 AND S10
S12. (MH "Systematic Review") OR (MH "SRs as Topic")
S13. AB "systematic review" OR AB ("systematic review and meta‐analysis") OR AB "intervention review"
S14. S11 OR S12
S15. S3 AND S4 AND S7 AND S14
S16. S3 AND S4 AND S11 AND S14
Dhakal R, Shah R, Huntjens B, Verkicharla PK, Lawrenson JG. Time spent outdoors as an intervention for myopia prevention and control in children: an overview of systematic reviews. Ophthalmic Physiol Opt 2022;42:545–558. doi: 10.1111/opo.12945
REFERENCES
- 1. Cooper J, Tkatchenko AV. A review of current concepts of the etiology and treatment of myopia. Eye Contact Lens 2018;44:231–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vision NRCUCo . Myopia: prevalence and progression. Washington, DC: National Academies Press (US); 1989. [PubMed] [Google Scholar]
- 3. Hysi PG, Wojciechowski R, Rahi JS, Hammond CJ. Genome‐wide association studies of refractive error and myopia, lessons learned, and implications for the future. Invest Ophthalmol Vis Sci 2014;55:3344–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cohen Y, Belkin M, Yehezkel O, Solomon AS, Polat U. Dependency between light intensity and refractive development under light‐dark cycles. Exp Eye Res 2011;92:40–6. [DOI] [PubMed] [Google Scholar]
- 5. Ashby R, Ohlendorf A, Schaeffel F. The effect of ambient illuminance on the development of deprivation myopia in chicks. Invest Ophthalmol Vis Sci 2009;50:5348–54. [DOI] [PubMed] [Google Scholar]
- 6. Wu P‐C, Tsai C‐L, Wu H‐L, Yang Y‐H, Kuo H‐K. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 2013;120:1080–5. [DOI] [PubMed] [Google Scholar]
- 7. Jin J‐X, Hua W‐J, Jiang X, et al. Effect of outdoor activity on myopia onset and progression in school‐aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmol 2015;15:1–11. 10.1186/s12886-015-0052-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Read SA, Collins MJ, Vincent SJ. Light exposure and eye growth in childhood. Invest Ophthalmol Vis Sci 2015;56:6779–87. [DOI] [PubMed] [Google Scholar]
- 9. Wu P‐C, Chen C‐T, Lin K‐K, et al. Myopia prevention and outdoor light intensity in a school‐based cluster randomized trial. Ophthalmology 2018;125:1239–50. [DOI] [PubMed] [Google Scholar]
- 10. He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA 2015;314:1142–8. [DOI] [PubMed] [Google Scholar]
- 11. Feldkaemper M, Schaeffel F. An updated view on the role of dopamine in myopia. Exp Eye Res 2013;114:106–19. [DOI] [PubMed] [Google Scholar]
- 12. McCarthy C, Megaw P, Devadas M, Morgan I. Dopaminergic agents affect the ability of brief periods of normal vision to prevent form‐deprivation myopia. Exp Eye Res 2007;84:100–7. [DOI] [PubMed] [Google Scholar]
- 13. Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008;115:1279–85. [DOI] [PubMed] [Google Scholar]
- 14. Rose KA, Morgan IG, Smith W, et al. Myopia, lifestyle, and schooling in students of Chinese ethnicity in Singapore and Sydney. Arch Ophthalmol 2008;126:527–30. [DOI] [PubMed] [Google Scholar]
- 15. Lou L, Ostrin LA. Effects of narrowband light on choroidal thickness and the pupil. Invest Ophthalmol Vis Sci 2020;61:40. 10.1167/iovs.61.10.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Foulds WS, Barathi VA, Luu CD. Progressive myopia or hyperopia can be induced in chicks and reversed by manipulation of the chromaticity of ambient light. Invest Ophthalmol Vis Sci 2013;54:8004–12. [DOI] [PubMed] [Google Scholar]
- 17. Long Q, Chen D, Chu R. Illumination with monochromatic long‐wavelength light promotes myopic shift and ocular elongation in newborn pigmented guinea pigs. Cutan Ocul Toxicol 2009;28:176–80. [DOI] [PubMed] [Google Scholar]
- 18. Rucker F, Britton S, Spatcher M, Hanowsky S. Blue light protects against temporal frequency sensitive refractive changes. Invest Ophthalmol Vis Sci 2015;56:6121–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rucker F, Henriksen M, Yanase T, Taylor C. The role of temporal contrast and blue light in emmetropization. Vision Res 2017;151:78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Torii H, Kurihara T, Seko Y, et al. Violet light exposure can be a preventive strategy against myopia progression. EBioMedicine 2017;15:210–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Torii H, Ohnuma K, Kurihara T, Tsubota K, Negishi K. Violet light transmission is related to myopia progression in adult high myopia. Sci Rep 2017;7:14523. 10.1038/s41598-017-09388-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ho CL, Wu WF, Liou YM. Dose‐response relationship of outdoor exposure and myopia indicators: a systematic review and meta‐analysis of various research methods. Int J Environ Res Public Health 2019;16:2595. 10.3390/ijerph16142595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sherwin JC, Reacher MH, Keogh RH, et al. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta‐analysis. Ophthalmology 2012;119:2141–51. [DOI] [PubMed] [Google Scholar]
- 24. Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta‐analysis and systematic review. Acta Ophthalmol 2017;95:551–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cao K, Wan Y, Yusufu M, Wang N. Significance of outdoor time for myopia prevention: a systematic review and meta‐analysis based on randomized controlled trials. Ophthalmic Res 2020;63:97–105. [DOI] [PubMed] [Google Scholar]
- 26. Deng L, Pang Y. Effect of outdoor activities in myopia control: meta‐analysis of clinical studies. Optom Vis Sci 2019;96:276–82. [DOI] [PubMed] [Google Scholar]
- 27. Pollock M, Fernandes RM, Becker LA, et al. Chapter V: overviews of reviews. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, editors. Cochrane handbook for systematic reviews of interventions. Cochrane; 2020. [Google Scholar]
- 28.Available at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020214523. Accessed January 4, 2022.
- 29. Martinic MK, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta‐epidemiological studies and textbooks. BMC Med Res Methodol 2019;19:1–12. 10.1186/s12874-019-0855-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non‐randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Whiting P, Savović J, Higgins JPT, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 2016;69:225–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Review Manager (RevMan) [Computer program] . Version 5.4, The Cochrane Collaboration, 2020. The format of the citation follows guidance issued by the Cochrane collaboration. Available at: https://training.cochrane.org/online‐learning/core‐software‐cochrane‐reviews/revman/revman‐non‐cochrane‐reviews. Accessed January 11, 2022.
- 34. Zhang J, Kai FY. What's the relative risk?: A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 1998;280:1690–1. [DOI] [PubMed] [Google Scholar]
- 35. Pieper D, Antoine S‐L, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol 2014;67:368–75. [DOI] [PubMed] [Google Scholar]
- 36. Eppenberger LS, Sturm V. The role of time exposed to outdoor light for myopia prevalence and progression: a literature review. Clin Ophthalmol 2020;14:1875–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Anandita W, Barliana JD. Outdoors activity as a protective factor of myopia incidence in children. Ophthalmol Indones 2015;41:247–55. [Google Scholar]
- 38. Suhr Thykjær A, Lundberg K, Grauslund J. Physical activity in relation to development and progression of myopia–a systematic review. Acta Ophthalmol. 2017;95:651–9. [DOI] [PubMed] [Google Scholar]
- 39. Zhang J, Deng G. Protective effects of increased outdoor time against myopia: a review. J Int Med Res. 2020;48:0300060519893866. 10.1177/0300060519893866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chua SYL, Sabanayagam C, Cheung Y‐B, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt 2016;36:388–94. [DOI] [PubMed] [Google Scholar]
- 41. Pärssinen O, Kauppinen M. Risk factors for high myopia: a 22‐year follow‐up study from childhood to adulthood. Acta Ophthalmol 2019;97:510–8. [DOI] [PubMed] [Google Scholar]
- 42. Dhakal R, Goud A, Narayanan R, Verkicharla PK. Patterns of posterior ocular complications in myopic eyes of Indian population. Sci Rep 2018;8:13700. 10.1038/s41598-018-29536-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Guo Y, Liu L, Tang P, et al. Progression of myopic maculopathy in Chinese children with high myopia: a long‐term follow‐up study. Retina 2021;41:1502–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Fang Y, Yokoi T, Nagaoka N, et al. Progression of myopic maculopathy during 18‐year follow‐up. Ophthalmology 2018;125:863–77. [DOI] [PubMed] [Google Scholar]
- 45. Sankaridurg P, Tahhan N, Kandel H, et al. IMI impact of myopia. Invest Ophthalmol Vis Sci 2021;62:ARVO E‐Abstract 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lim MC, Gazzard G, Sim EL, Tong L, Saw SM. Direct costs of myopia in Singapore. Eye 2009;23:1086–9. [DOI] [PubMed] [Google Scholar]
- 47. Zheng YF, Pan CW, Chay J, et al. The economic cost of myopia in adults aged over 40 years in Singapore. Invest Ophthalmol Vis Sci 2013;54:7532–7. [DOI] [PubMed] [Google Scholar]
- 48. Bullimore MA, Brennan NA. Myopia control: why each diopter matters. Optom Vis Sci 2019;96:463–5. [DOI] [PubMed] [Google Scholar]
- 49. Jonas JB, Ang M, Cho P, et al. IMI prevention of myopia and its progression. Invest Ophthalmol Vis Sci 2021;62:ARVO E‐Abstract 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zhou Z, Chen T, Wang M, et al. Pilot study of a novel classroom designed to prevent myopia by increasing children’s exposure to outdoor light. PLoS One 2017;12:e0181772. 10.1371/journal.pone.0181772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hua W‐J, Jin J‐X, Wu X‐Y, et al. Elevated light levels in schools have a protective effect on myopia. Ophthalmic Physiol Opt 2015;35:252–62. [DOI] [PubMed] [Google Scholar]
- 52. Verkicharla PK, Chia NEH, Saw S‐M. What public policies should be developed to cope with the myopia epidemic? Optom Vis Sci 2016;93:1055–7. [DOI] [PubMed] [Google Scholar]
- 53. Dhakal R, Verkicharla PK. Increasing time in outdoor environment could counteract the rising prevalence of myopia in Indian school‐going children. Curr Sci 2020;119:1616–9. [Google Scholar]
- 54. Morgan IG. What public policies should be developed to deal with the epidemic of myopia? Optom Vis Sci 2016;93:1058–60. [DOI] [PubMed] [Google Scholar]
- 55. Walline JJ, Robboy MW, Hilmantel G, et al. Food and Drug Administration, American Academy of Ophthalmology, American Academy of Optometry, American Association for Pediatric Ophthalmology and Strabismus, American Optometric Association, American Society of Cataract and Refractive Surgery, and Contact Lens Association of Ophthalmologists Co‐Sponsored Workshop: controlling the progression of myopia: contact lenses and future medical devices. Eye Contact Lens 2018;44:205–11. [DOI] [PubMed] [Google Scholar]
- 56. Higgins J, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. Version 6.2 [updated February 2021]. Cochrane; 2021. [Google Scholar]
- 57. Tawfik GM, Dila KAS, Mohamed MYF, et al. A step by step guide for conducting a systematic review and meta‐analysis with simulation data. Trop Med Health 2019;47:1–9. 10.1186/s41182-019-0165-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Alvarez AA, Wildsoet CF. Quantifying light exposure patterns in young adult students. J Mod Opt 2013;60:1200–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Dharani R, Lee C‐F, Theng ZX, et al. Comparison of measurements of time outdoors and light levels as risk factors for myopia in young Singapore children. Eye 2012;26:911–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Read SA, Collins MJ, Vincent SJ. Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci 2014;91:330–41. [DOI] [PubMed] [Google Scholar]
- 61. Landis EG, Yang V, Brown DM, Pardue MT, Read SA. Dim light exposure and myopia in children. Invest Ophthalmol Vis Sci 2018;59:4804–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ostrin LA. Objectively measured light exposure in emmetropic and myopic adults. Optom Vis Sci 2017;94:229–38. [DOI] [PubMed] [Google Scholar]
- 63. Zhang X, Wang Y, Pan C, et al. Effect of genetic‐environmental interaction on Chinese childhood myopia. J Ophthalmol 2020;2020:6308289. 10.1155/2020/6308289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. French A, Rose KA, Morgan I. The interaction between time outdoors, near work and refractive error. Invest Ophthalmol Vis Sci 2018;59:ARVO E‐Abstract 3959. [Google Scholar]
- 65. Flitcroft D. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res 2012;31:622–60. [DOI] [PubMed] [Google Scholar]
- 66. Radhakrishnan H, Pardhan S. The influence of near work and time spent outdoors on refractive error and axial length in Indian children. Optom Vis Perf 2019;7:238–45. [Google Scholar]
- 67. Verkicharla P, Thakur SK. Impact of short‐term exposure to short, middle, and long‐wavelength of light and optical defocus on axial elongation in humans. Invest Ophthalmol Vis Sci 2021;62:ARVO E‐Abstract 1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File S1
File S2
File S3
File S4


