Abstract
Background
The objective of this study was to investigate the prognostic impact of right ventricular (RV) function at rest and during exercise in patients with systemic sclerosis (SSc) presenting for a screening for pulmonary hypertension (PH).
Methods
In this study, data from SSc patients who underwent routinely performed examinations for PH screening including echocardiography and right heart catheterization at rest and during exercise were analysed. Uni- and multivariable analyses were performed to identify prognostic parameters.
Results
Out of 280 SSc patients screened for PH, 225 were included in the analysis (81.3% female, mean age 58.1±13.0 years, 68% limited cutaneous SSc, WHO-FC II–III 74%, 24 manifest PH). During the observation period of 3.2±2.7 (median 2.6) years 35 patients died. Tricuspid annular plane systolic excursion (TAPSE) at rest <18 mm (p=0.001), RV output reserve as increase of cardiac index (CI) during exercise <2 l/min (p<0.0001), RV pulmonary vascular reserve (Δ mean pulmonary artery pressure/Δ cardiac output) ≥3 mmHg/l/min (p<0.0001), peak CI <5.5 l/min/m2 (p=0.001), pulmonary arterial compliance <2 ml/mmHg (p=0.002), TAPSE/systolic pulmonary arterial pressure (sPAP) ratio ≤0.6 ml/mmHg (p<0.0001) and echocardiographic qualitative RV function at rest (p<0.0001) significantly predicted worse survival. In the multivariable analysis TAPSE/sPAP ratio and diffusion capacity for carbon monoxide ≤65% were identified as independent prognostic predictors and had 75% sensitivity and 69% specificity to predict future development of pulmonary vascular disease (PVD) during follow-up.
Conclusions
This study demonstrates that assessment of RV function at rest and during exercise may provide crucial information to identify SSc patients who are at a high risk of poor outcome and for the development of PH and/or PVD.
Keywords: Systemic sclerosis, Right ventricular reserve, Pulmonary hypertension, Screening, Echocardiography, Right heart catheterisation
Introduction
Systemic sclerosis (SSc) is a rare autoimmune connective tissue disorder, affecting skin and different internal organs [1]. In about 15–25% of symptomatic and 8-12% of asymptomatic SSc patients the disease manifests in a concomitant pulmonary hypertension (PH) [2, 3]. In absence of comorbidities, such as heart disease or lung fibrosis, the disease can be classified as SSc-associated pulmonary arterial hypertension (SSc-APAH). At pulmonary arterial hypertension (PAH) diagnosis, >85% of patients with SSc are already in advanced stages of the disease (World Health Organization functional classes (WHO-FC) III and IV) [4]. Untreated patients present with a markedly reduced 3-year survival of 56%, compared with 91% in SSc patients without PAH [5]. Another study showed a short median survival in SSc-APAH patients of only four years despite an advanced PAH therapy [6]. Therefore, an early diagnosis of pulmonary vascular disease (PVD) is essential and screening programmes in SSc patients are recommended [7–10]. The DETECT study developed an evidence-based algorithm for the early detection of APAH in SSc patients [11] using clinical and echocardiographic data to determine patient referral for right heart catheterisation (RHC) to confirm PH/PAH diagnosis. At the time of the DETECT algorithm development, pre-capillary PH was haemodynamically defined as mean pulmonary arterial pressure (mPAP) ≥25 mmHg and pulmonary capillary wedge pressure (PAWP) ≤15 mmHg, measured by RHC [7]. In the following ESC/ERS guidelines 2015, pulmonary vascular resistance (PVR) >3 Wood Units (WU) was included in the haemodynamic definition of PAH [10].
Using the DETECT algorithm or RHC at rest for screening, the majority of the newly diagnosed pre-capillary PH patients presented with only slightly elevated mPAP, normal or near-normal mean cardiac output (CO) at rest, slightly elevated right atrial size and a PVR value <3 WU [11–14].
During the 6th World Symposium on PH, a new haemodynamic definition was suggested to enable early diagnosis, by lowering the mPAP threshold to >20 mmHg and to include PVR ≥3 WU as part of the haemodynamic definition for all forms of pre-capillary PH [15–17]. More recently, studies provided evidence that even a lower threshold of ≥2 WU indicates abnormal PVR [18–20].
Patients with mildly elevated mPAP (who would meet the new diagnostic criteria for precapillary PH) showed already a reduced right ventricular (RV) output reserve (defined as reduced cardiac index (CI)-increase during exercise) and reduced pulmonary arterial compliance (PAC) suggestive for an early PVD [13].
It remains unclear, if RV function during exercise (RV output reserve) is of prognostic relevance for these patients. Furthermore, various parameters reflecting right heart size and RV function have been shown to be prognostically important in patients with PAH [21–25]. It is unclear, whether these parameters may also be used for estimation of prognosis in SSc patients (with or without PH) assessed for PH screening.
Therefore, the aim of this study was to investigate the prognostic impact of RV function and output reserve in patients with SSc presenting for PH screening and to compare them to established prognostic predictors. Furthermore, we aimed to assess, if changes in RV function at rest or during exercise are predictive for the development of PH during follow-up in this SSc cohort.
Methods
Study population and design
In this retrospective, monocentric cohort study adult patients with SSc who were assessed by both, non-invasive clinical procedures such as echocardiography and by RHC at rest and during exercise, at the PH-Centre in the Thoraxklinik Heidelberg gGmbH at Heidelberg University Hospital were enrolled. All retrospectively analysed patients were already diagnosed with SSc fulfilling the classification criteria of the American College of Rheumatology/European League against Rheumatism [26] and were categorised as patients with diffuse cutaneous SSc (dcSSc) or limited cutaneous SSc (lcSSc) [27]. Referring specialists were rheumatologists, cardiologists, pulmonologists and general practitioners.
Individuals were excluded, if they had no screening for PH, had rheumatic diseases other than SSc or were unable to give informed consent. Patients with missing haemodynamic assessment during exercise were excluded from data analysis. A part of this cohort has already been analysed and published before [11, 13, 18, 28].
All patients underwent a detailed screening for PH including medical history and physical examination, WHO-FC assessment, 6-min walking distance (6MWD), electrocardiogram, body plethysmography, diffusion capacity measurement of the lung for carbon monoxide (DLCO), blood gas analysis (capillary), computed tomography scan of the lung or other imaging, determination of laboratory parameters (especially N-terminal pro-brain natriuretic peptide (NT-proBNP) level), echocardiography at rest and during exercise, as well as RHC at rest and during exercise, standardised according to the current recommendations, as described before [29–31]. All data were pseudonymized. The study was approved by the ethics committee of the Medical Faculty of Heidelberg University (internal number S-305/2021). The study complied with the Declaration of Helsinki in its current version.
Parameters of right ventricular function and reserve
Parameters reflecting RV function and output reserve were obtained from echocardiographic assessments [21, 32] and by right heart catheterisation at rest and during exercise [31, 33–37]. Echocardiographic parameters included right ventricular fractional area change (RV-FAC), tissue Doppler imaging tissue velocity (TDI TV s), qualitative right ventricular function, tricuspid annular plane systolic excursion (TAPSE) and TAPSE/systolic pulmonary arterial pressure ratio (sPAP) assessed by echocardiography. Qualitative function assessed during echocardiography was expressed as normal, mild, moderate or severe impairment. RV-FAC is a global measure of RV systolic function and was calculated as the difference between end-diastolic and end-systolic area, divided by the end-diastolic area. Furthermore, the velocity of the tricuspid valve characterises the pulmonary vascular flow.
Parameters determined by RHC included CI at rest and during exercise, mPAP, stroke volume, PVR, PAC, and RV pulmonary vascular reserve (mPAP increase/CO increase = ΔmPAP/ΔCO) and peak CI. CI at rest was used to describe RV function at rest, while an increase of CI defines RV output reserve. PAC was calculated as a specific measure to define abnormal vascular elasticity and was calculated as stroke volume/pulse pressure (stroke volume = CO/heart rate; pulse pressure = systolic pulmonary arterial pressure/diastolic pulmonary arterial pressure) [38]. All parameters were assessed according to current standards [29–31] and as described previously [18, 28].
Known thresholds for the above-listed parameters include TAPSE <18 mm, having already shown prognostic significance [39, 40], TAPSE/sPAP ratio ≤0.6 mm/mmHg [41] and RV pulmonary vascular reserve of ≥3 ml/min/mmHg [42], which has been used as the definition of exercise pulmonary hypertension [43].
Known prognostic predictors in SSc
Parameters which have already been identified as prognostic predictors in SSc were used for comparison with parameters of RV function and reserve. Known prognostic predictors included age ≥60 years at baseline, DLCO ≤65% predicted [44–46], presence of pulmonary fibrosis [46] and PVR ≥2 WU [28].
Statistical methods
Statistical analyses were conducted by a medical statistician (NB). Data are described as mean ± standard deviation (SD) with 95% confidence interval of the mean. Frequency data is given as number and percent.
Variables were evaluated by uni- and multivariable analysis to identify their impact on survival. Survival time was estimated from baseline (time of first screening assessment) until the end of follow-up in this study. Death was defined as death due to any cause. Cox regression analysis was used for survival analysis of continuous parameters. Parameters with significant prediction of survival in Cox regression analysis were dichotomized by receiver operating characteristic (ROC), or by threshold values from the literature. Kaplan-Meier analysis was performed with categorial parameters. Multivariable analysis was performed including significant predictors of RV function or output reserve and known prognostic predictors of SSc. Qualitative RV function was dichotomised as normal function vs. any impairment (including mild, moderate and severe impairment) due to insufficient sample size within the categories.
A multivariable risk set was analysed regarding prognostic prediction by Kaplan-Meier analysis including combination of independent prognostic predictors. An age-corrected Cox regression of the multivariable risk set was performed as sensitivity analysis. Multivariable analysis was performed leaving out patients with cancer as cause of death as sensitivity analysis. Furthermore, the multivariable analysis was performed in a subset of SSc patients without any signs of PVD, i.e. patients with mPAP 21-24 mmHg and PVR ≥2 WU, patients with mPAP ≥25 mmHg were excluded from the analysis. Differences of clinical parameters between patients presenting with none or a single vs. two or more risk factors were analysed. Clinical parameters were compared with the two-sided Student’s t-test for independent random samples. Frequency data were analysed using the chi-square test.
P-values <0.05 were considered to indicate statistical significance. All analyses have been performed using IBM SPSS 27 (SPSS Statistics V.27, IBM Corporation, Somers, NY, USA).
Results
Baseline characteristics (Table 1)
Table 1.
Characteristics of study cohort
| Whole cohort (n=225) | |||||
|---|---|---|---|---|---|
| mean ± SD or n and (%) | 95% confidence interval | n* | |||
| Characteristics | |||||
| Female sex, no [%] | 183 | 81.3 % | |||
| Age [years] | 58.14 | ± | 12.95 | 56.44 to 59.84 | 225 |
| Height [cm] | 166.13 | ± | 08.63 | 165.00 to 167.26 | 225 |
| Weight [kg] | 70.85 | ± | 15.80 | 68.78 to 72.93 | 225 |
| Systolic blood pressure [mmHg] | 133.00 | ± | 21.14 | 130.19 to 135.82 | 219 |
| Diastolic blood pressure [mmHg] | 76.02 | ± | 10.93 | 74.57 to 77.48 | 219 |
| Heart rate at rest [/min] | 75.63 | ± | 12.36 | 73.46 to 77.80 | 127 |
| Type of systemic sclerosis | 225 | ||||
| Limited cutaneous SSc [%] | 152 | 67.6% | |||
| Diffuse cutaneous SSc [%] | 54 | 24.0% | |||
| Early SSc | 19 | 8.4% | |||
| Duration SSc [days] | 3420.54 | ± | 3325.72 | 2980.65 to 3860.42 | 222 |
| SSc characteristics | |||||
| Modified Rodnan skin score | 12 | ± | 10 | 10 to 13 | 160 |
| Digital ulcers | 76 | 33.9% | 224 | ||
| WHO-FC, no [%] | |||||
| I | 54 | 24.0% | 54 | ||
| II | 108 | 48.0% | 108 | ||
| III | 59 | 26.3% | 53 | ||
| IV | 4 | 1.8% | 4 | ||
| Lung function | |||||
| Vital capacity max [l] | 2.96 | ± | 0.95 | 2.84 to 3.09 | 221 |
| Forced expiratory volume in one second [l] | 2.35 | ± | 0.78 | 2.25 to 2.45 | 222 |
| Total lung capacity [l] | 5.05 | ± | 1.29 | 4.88 to 5.22 | 221 |
| Diffusion capacity of the lung for carbon monoxide SB [%] | 57.50 | ± | 18.27 | 55.02 to 59.98 | 211 |
| Diffusion capacity of the lung for carbon monoxide/VA [%] | 72.51 | ± | 19.90 | 69.82 to 75.20 | 213 |
| Mixed venous oxygen saturation [%] | 72.13 | ± | 12.93 | 69.36 to 74.90 | 86 |
| Laboratory | |||||
| N-terminal pro-brain natriuretic peptide [ng/l] | 374.31 | ± | 718.49 | 274.12 to 474.49 | 200 |
| C-reactive protein [mg/l] | 6.95 | ± | 9.42 | 5.7 to 8.19 | 222 |
| Troponin T [μg/l] | 125 | ± | 11.62 | 8.45 to 12.57 | 125 |
| Glomerular filtration rate [ml/min/1.73m2] | 85.81 | ± | 26.36 | 82.2 to 89.43 | 207 |
| Creatinine [mg/dl] | 0.88 | ± | 0.88 | 0.76 to 1.0 | 222 |
| 6-minute walking distance [meters] | 439.93 | ± | 96.18 | 426.72 to 453.14 | 206 |
| Echocardiography | |||||
| Right atrial area [cm2] | 12.38 | ± | 3.73 | 11.88 to 12.88 | 214 |
| Right ventricular area [cm2] | 14.81 | ± | 3.66 | 14.33 to 15.30 | 218 |
| Systolic pulmonary arterial pressure [mmHg] | 32.10 | ± | 13.43 | 30.30 to 33.90 | 216 |
| Tricuspid annular plane systolic excursion [mm] | 23.93 | ± | 4.45 | 23.34 to 24.53 | 218 |
| Right ventricular fractional area change [%] | 0.71 | ± | 0.32 | 0.63 to 0.78 | 69 |
| Tissue Doppler imaging tissue velocity S | 14 | ± | 3 | 13 to 14 | 182 |
| Increase of systolic pulmonary arterial pressure during exercise [mmHg] | 25.78 | ± | 10.65 | 23.80 to 27.76 | 114 |
| Right heart catheter | |||||
| Mean pulmonary arterial pressure [mmHg] | 20.41 | ± | 8.43 | 19.31 to 21.52 | 225 |
| Cardiac output [l/min] | 5.39 | ± | 1.42 | 5.20 to 5.57 | 225 |
| Pulmonary arterial wedge pressure [mmHg] | 9.39 | ± | 4.18 | 8.84 to 9.94 | 225 |
| Pulmonary vascular resistance [WU] | 2.22 | ± | 1.73 | 1.99 to 2.45 | 225 |
| Pulmonary arterial compliance [ml/mmHg] | 4.41 | ± | 2.31 | 4.08 to 4.74 | 195 |
| RV pulmonary vascular reserve [mmHg/l/min] | 7.79 | ± | 43.62 | 2.06 to 13.52 | 225 |
| Cardiac index [l/min/m2] | 3.08 | ± | 0.78 | 2.98 to 3.18 | 225 |
| Cardiac index increase during exercise [l/min/m2] | 2.78 | ± | 1.59 | 2.57 to 2.98 | 225 |
| Peak cardiac index [l/min/m2] | 5.86 | ± | 1.69 | 5.63 to 6.08 | 225 |
| Right ventricular pump function | 221 | ||||
| Normal | 199 | 90.0% | |||
| Mild impairment | 11 | 5.0% | |||
| Moderate impairment | 4 | 1.8% | |||
| Severe impairment | 7 | 3.2% | |||
SB single breath, SSc systemic sclerosis, VA alveolar volume, WHO-FC World Health Organization functional class
*In case of missing values, n is provided
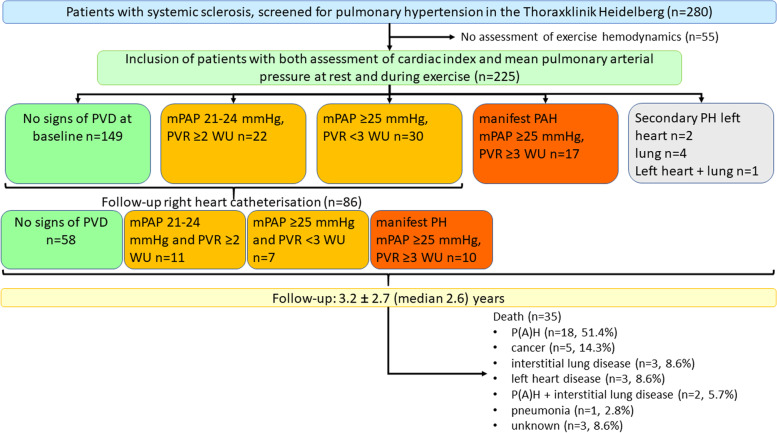
A total of 280 patients with SSc were screened for PH at the Centre for Pulmonary Hypertension at the Thoraxklinik Heidelberg between 2008 and 2020. Fifty-five patients were excluded from the study due to missing haemodynamic assessments during exercise (Fig. 1). Thus, the final dataset consisted of 225 patients (mean age 58.14 ± 12.95 years, 81.3% female, 67.6% lcSSc, 24.0% dcSSc) who had been assessed at baseline and during a follow-up time of 3.2±2.7 (median 2.6) years (Table 1).
Fig. 1.
Study flow-chart. The graph provides information on patient-flow, baseline haemodynamics and follow-up. mPAP, mean pulmonary artery pressure; P(A)H, pulmonary (arterial) hypertension; PAWP, pulmonary arterial wedge pressure; PVD, pulmonary vascular disease; PVR, pulmonary vascular resistance
Concomitant arterial hypertension was present in 77 patients (34.4%) and 90 patients (40%) presented with pulmonary fibrosis. In 76.1% of the patients, a functional impairment was described with WHO-FC ≥II (Table 1). Haemodynamic assessments generally showed normal mean values of right heart size and function (Table 1) [47]. In 22 patients, RV pump function was impaired at baseline (mild to severe impairment).
At baseline 149 of 225 patients (66.2%) had normal pulmonary haemodynamics at rest (Fig. 1). In 24 patients (10.6%) mPAP and PVR were increased, meeting the definition of manifest PH (Fig. 1). Out of these patients, 17 (7.6%) were classified as SSc-APAH, two presented with PH due to left heart disease, four with PH due to lung disease and one PH patient had both left heart and lung disease. In further 52 patients (23.1%), early signs of PVD were detected at baseline with mildly elevated mPAP 21-24 mmHg and PVR ≥2 WU at rest (n=22) or mPAP ≥25 mmHg and PVR ≤3 WU (n=30).
Survival in SSc patients and prognostic predictors
During an observation period of 3.2±2.7 (median 2.6) years 35 patients died. Reasons for death were P(A)H (n=18, 51.4%), cancer (n=5, 14.3%), pulmonary fibrosis (n=3, 8.6%), left heart disease (n=3, 8.6%), P(A)H and pulmonary fibrosis (n=2, 5.7%), pneumonia (n=1, 2.8%) and unknown cause of death (n=3, 8.6%).
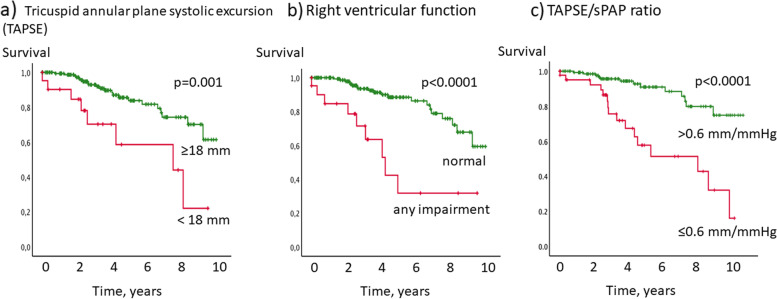
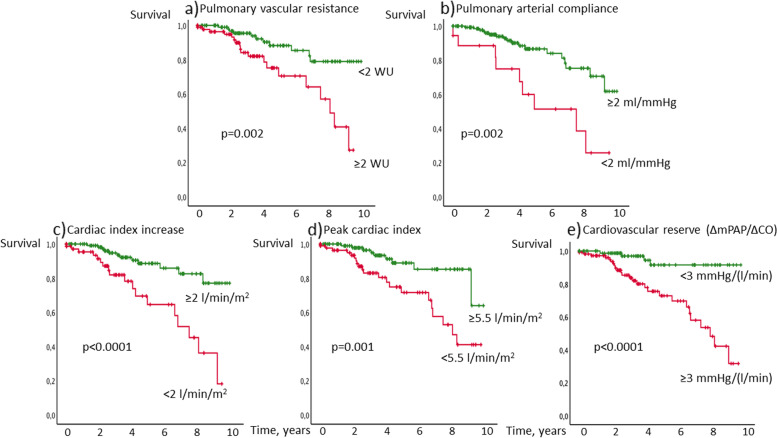
Significant predictors for survival in the univariable Cox regression analysis were TAPSE, TAPSE/sPAP, PAC, CI increase, RV pulmonary vascular reserve, peak CI and qualitative RV function (Table 2). The threshold for impaired RV function from the literature was <18 mm for TAPSE. RV pulmonary vascular reserve ≥3 mmHg/(l/min) was used as threshold for mPAP / CO slope, indicating exercise PH. For parameters with no established thresholds, ROC analysis was performed, leading to thresholds of <2 ml/mmHg for PAC, <5.5 l/min/m2 for peak CI, <2 l/min/m2 for CI increase indicating impaired RV function or reserve.
Table 2.
Univariable survival analysis
| Univariable analysis | ||||
| Cox Regression analysis | p-value | Exp(B) | ||
| Tricuspid annular plane systolic excursion (TAPSE) | 0.003 | 0.862 | ||
| Fractional area change | 0.918 | 0.919 | ||
| TDI TV s | 0.777 | 0.973 | ||
| Pulmonary arterial compliance | 0.001 | 0.759 | ||
| Cardiac index at rest | 0.314 | 0.707 | ||
| Cardiac index increase | 0.001 | 0.654 | ||
| RV pulmonary vascular reserve (mPAP increase/CO increase) | 0.049 | 1.006 | ||
| Cardiac index peak | 0.001 | 0.672 | ||
| Systolic pulmonary arterial pressure (sPAP) | 0.217 | 1.027 | ||
| TAPSE/sPAP | <0.0001 | 0.063 | ||
| Right ventricular function - normal vs. any impairment | <0.0001 | 0.205 | ||
| Kaplan-Meier analysis (categorial parameters) | Multivariable analysis stepwise forward selection | |||
| RV function and reserve | p-value | Exp(B) | ||
| Tricuspid annular plane systolic excursion <18 mm | 0.001 | |||
| Right ventricular function - normal vs. any impairment | <0.0001 | |||
| Pulmonary arterial compliance <2 ml/mmHg | 0.002 | |||
| Cardiac index increase <2 l/min/m2 | <0.0001 | |||
| RV pulmonary vascular reserve ≥3 mmHg/(l/min) (literature) | <0.0001 | |||
| Cardiac index peak <5.5 l/min | 0.001 | |||
| TAPSE/sPAP ≤0.6 mm/mmHg | <0.0001 | <0.0001 | 0.201 | |
| Known prognostic predictors | ||||
| Age ≥60 years | 0.004 | |||
| DLCO ≤65% predicted | <0.0001 | 0.003 | 0.297 | |
| Sex | 0.554 | |||
| Type of systemic sclerosis | 0.497 | |||
| Pulmonary fibrosis | 0.034 | |||
| Pulmonary vascular resistance ≥2 Wood Units | 0.002 | |||
| Combination of independent prognostic predictors (Kaplan-Meier) | ||||
| DLCO ≤65% and TAPSE/sPAP | <0.0001 | |||
TDI tissue Doppler imaging, TV tissue velocity, RV right ventricular, DLCO diffusion capacity of the lung for carbon monoxide
Parameters of RV function significantly predicted survival in this patient cohort (Table 2, Figs. 2 and 3). Interstitial lung disease was significantly more often in patients with CI increase during exercise <2 l/min/m2 (45.6% vs. 29.1%, p=0.012). For other parameters, presence of ILD did not significantly differ between groups.
Fig. 2.
Kaplan-Meier survival analysis of echocardiographic right ventricular function. Patients with a tricuspid annular plane systolic excursion <18 mm assessed by echocardiography, b any impairment of RV function or with c TAPSE/sPAP ratio ≤0.6 mm/mmHg had significantly worse survival than patients with tricuspid annular plane systolic excursion ≥18 mm, normal RV function, or TAPSE/sPAP ratio >0.6 mm/mmHg
Fig. 3.
Kaplan-Meier analysis of invasively determined right ventricular function. Patients with a pulmonary vascular resistance ≥2 Wood Units, b pulmonary artery compliance <2 ml/mmHg, c cardiac index increase <2 l/min/m2, d peak cardiac index <5.5 l/min/m2 and/or e RV pulmonary vascular reserve (defined as the increase of mean pulmonary artery pressure/increase of cardiac output during exercise) ≥3 mmHg/(l/min) showed worse survival than SSc patients above the respective thresholds
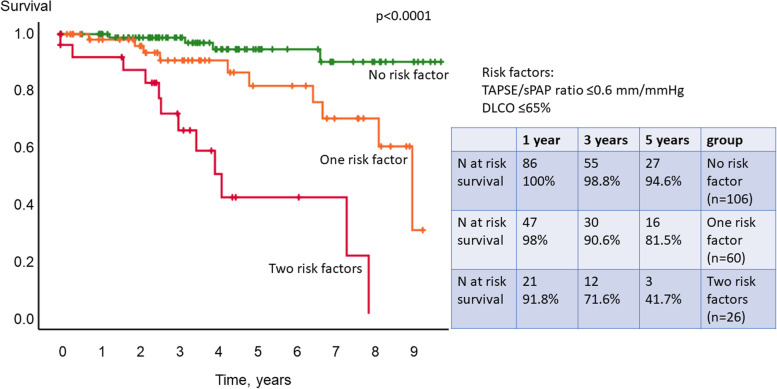
In the multivariable analysis, TAPSE/sPAP ratio and DLCO ≤65% were identified as independent predictors of survival (Table 2). When combining these independent predictors, patients with no risk factor had significantly better survival than patients with 1 or 2 risk factors with 1-, 3- and 5-year survival rates of 100%, 98.8% and 94.6%, vs. 98%, 90.6% and 81.5% and 91.8%, 71.6% and 41.7% (Kaplan-Meier p<0.0001, Fig. 4). Prediction of survival remained significant when adjusted for age (p<0.0001). Independent prognostic predictors were confirmed by the sensitivity analysis leaving out patients with cancer as cause of death. In addition to the already identified parameters, type of SSc (p=0.004) and RV pulmonary vascular reserve (p=0.003) were identified as independent prognostic predictors in the sensitivity analysis.
Fig. 4.
Kaplan-Meier analysis of multivariable risk set. Multivariable Cox regression analysis identified TAPSE/sPAP ratio ≤0.6 mm/mmHg and diffusion capacity for carbon monoxide of the lung (DLCO) ≤65% predicted as independent prognostic predictors of survival. Patients with none of these risk factors had significantly better survival than patients with one or two risk factors
When only patients with no signs of PVD at baseline (i.e. <21 mmHg mPAP or PVR <2 WU) were included in the multivariate analysis, CI increase during exercise <2 l/min/m2 was the only independent prognostic parameter for survival (p=0.028).
Characterisation of patients in different risk groups
Patients with no risk factor (i.e. TAPE/sPAP ratio ≤0.6 mm/mmHg and DLCO ≤65% predicted) presented with significantly less haemodynamic impairment, better physical exercise capacity and better lung function (Table 3).
Table 3.
Characteristics of different risk groups
| No risk factor (n=108) | One risk factor (n=66) | Two risk factors (n=26) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD or n and (%) | 95% confidence interval | n* | Mean ± SD or n and (%) | 95% confidence interval | n* | p-value (0 vs. 1 RF) | Mean ± SD or n and (%) | 95% confidence interval | n* | p-value (0 vs. 2 RF) | p-value (1 vs. 2 RF) | |||||||
| Characteristics | ||||||||||||||||||
| Female sex, no [%] | 90 | 83.3% | 53 | 80.3% | 23 | 88.5% | ||||||||||||
| Age [years] | 55.5 | ± | 12.1 | 53.2 to 57.9 | 59.4 | ± | 13.9 | 56.0 to 62.8 | 60.9 | ± | 13.5 | 55.5 to 66.4 | 0.002 | 0.20 | ||||
| Height [cm] | 167.3 | ± | 8.3 | 165.7 to 168.9 | 166.2 | ± | 8.8 | 164.0 to 168.4 | 160.1 | ± | 7.7 | 157.8 to 164.0 | ||||||
| Weight [kg] | 72.8 | ± | 15.4 | 69.8 to 75.7 | 70.6 | ± | 16.7 | 66.5 to 74.7 | 66.3 | ± | 15.9 | 59.8 to 72.7 | ||||||
| Type of systemic sclerosis | ||||||||||||||||||
| Limited cutaneous SSc [%] | 80 | 74.1% | 47 | 71.2% | 19 | 73.1% | ||||||||||||
| Diffuse cutaneous SSc [%] | 27 | 25% | 17 | 25.8% | 7 | 26.9% | ||||||||||||
| Early SSc [%] | 1 | 0.9% | 2 | 3% | 0 | |||||||||||||
| Duration SSc [days] | 3398.6 | ± | 3432.2 | 2737.6 to 4059.6 | 106 | 2646.8 | ± | 2282.3 | 2081.3 to 3212.3 | 65 | 4829.9 | ± | 4089.4 | 3178.2 to 6481.7 | 0.011 | |||
| WHO-FC, no [%] | Overall <0.0001 | |||||||||||||||||
| I | 27 | 25% | 16 | 24.2% | 2 | 7.7% | ||||||||||||
| II | 60 | 55.6% | 33 | 50.0% | 6 | 23.1% | ||||||||||||
| III | 21 | 19.4% | 17 | 25.8% | 16 | 61.5% | ||||||||||||
| IV | 0 | 0 | 2 | 7.7% | ||||||||||||||
| Lung function | ||||||||||||||||||
| Vital capacity max [l] | 3.1 | ± | 0.9 | 3.0 to 3.3 | 107 | 3.0 | ± | 1.0 | 2.8 to 3.3 | 64 | 2.3 | ± | 0.8 | <0.001 | 0.004 | |||
| Forced expiratory volume in one second [l] | 2.5 | ± | 0.8 | 3.4 to 2.7 | 107 | 2.4 | ± | 0.8 | 2.2 to 2.6 | 65 | 1.9 | ± | 0.6 | 1.6 to 2.1 | 0.001 | 0.010 | ||
| Total lung capacity [l] | 5.2 | ± | 1.2 | 5.0 to 5.5 | 107 | 5.1 | ± | 1.3 | 4.8 to 5.5 | 65 | 4.1 | ± | 1.2 | 3.6 to 4.5 | <0.001 | 0.001 | ||
| Diffusion capacity of the lung for carbon monoxide SB [%] | 66.4 | ± | 16.4 | 63.3 to 69.5 | 49.8 | ± | 13.1 | 46.5 to 53.0 | <0.001 | 38.0 | ± | 13.2 | 32.4 to 43.6 | 24 | <0.001 | 0.004 | ||
| Diffusion capacity of the lung for carbon monoxide/VA [%] | 83.8 | ± | 15.6 | 80.8 to 86.8 | 62.0 | ± | 13.6 | 58.6 to 65.3 | <0.001 | 48.0 | ± | 12.0 | 43.2 to 52.8 | <0.001 | <0.001 | |||
| Laboratory | ||||||||||||||||||
| N-terminal pro-brain natriuretic peptide [ng/l] | 222.7 | ± | 323.9 | 158.8 to 286.7 | 101 | 467.4 | ± | 910.0 | 223.7 to 711.1 | 56 | 908.3 | ± | 1291.9 | 335.5 to 1481.1 | 22 | <0.001 | 0.048 | |
| C-reactive protein [mg/l] | 6.6 | ± | 10.0 | 4.7 to 8.5 | 107 | 5.2 | ± | 4.7 | 4.1 to 6.4 | 64 | 10.0 | ± | 9.6 | 6.1 to 13.8 | ||||
| Glomerular filtration rate [ml/min/1.73m2] | 87.8 | ± | 24.4 | 83.0 to 92.5 | 103 | 87.1 | ± | 29.6 | 79.2 to 94.9 | 57 | 76.3 | ± | 25.1 | 65.1 to 87.4 | 22 | |||
| Creatinine [mg/dl] | 0.78 | ± | 0.18 | 0.75 to 0.82 | 107 | 0.87 | ± | 0.55 | 0.73 to 1.0 | 64 | 1.33 | ± | 2.38 | 0.36 to 2.29 | 0.023 | |||
| 6-minute walking distance [meters] | 459.5 | ± | 82.4 | 443.3 to 475.7 | 102 | 438.1 | ± | 106.1 | 410.9 to 465.3 | 61 | 362.0 | ± | 104.0 | 318.1 to 405.9 | 24 | <0.001 | 0.003 | |
| Echocardiography | ||||||||||||||||||
| Right atrial area [cm2] | 11.7 | ± | 3.2 | 11.1 to 12.3 | 106 | 12.5 | ± | 4.3 | 11.5 to 13.6 | 65 | 14.5 | ± | 4.2 | 12.8 to 16.2 | 25 | |||
| Right ventricular area [cm2] | 14.1 | ± | 3.4 | 13.5 to 14.8 | 107 | 15.1 | ± | 3.8 | 14.2 to 16.1 | 16.7 | ± | 3.7 | 15.2 to 18.2 | |||||
| Systolic pulmonary arterial pressure [mmHg] | 26.3 | ± | 5.5 | 25.3 to 27.3 | 32.1 | ± | 12.2 | 29.1 to 35.1 | 0.001 | 55.4 | ± | 17.3 | 48.5 to 62.4 | <0.001 | <0.001 | |||
| Tricuspid annular plane systolic excursion [mm] | 25.1 | ± | 4.2 | 24.3 to 25.9 | 23.9 | ± | 4.2 | 22.9 to 24.9 | 19.4 | ± | 3.9 | 17.8 to 20.9 | <0.001 | <0.001 | ||||
| Right heart catheter | ||||||||||||||||||
| Mean pulmonary arterial pressure [mmHg] | 17.3 | ± | 5.1 | 16.4 to 18.3 | 20.2 | ± | 6.8 | 18.5 to 21.9 | 0.019 | 34.9 | ± | 10.7 | 30.5 to 39.2 | <0.001 | <0.001 | |||
| Cardiac output [l/min] | 5.6 | ± | 1.5 | 5.3 to 5.9 | 5.3 | ± | 1.3 | 5.0 to 5.7 | 5.1 | ± | 1.2 | 4.6 to 5.6 | ||||||
| Pulmonary arterial wedge pressure [mmHg] | 9.1 | ± | 4.2 | 8.3 to 9.9 | 9.7 | ± | 4.0 | 8.7 to 10.7 | 10.7 | ± | 5.1 | 8.7 to 12.8 | ||||||
| Pulmonary vascular resistance [WU] | 1.5 | ± | 0.6 | 1.4 to 1.7 | 2.2 | ± | 1.3 | 1.8 to 2.5 | 0.012 | 5.1 | ± | 2.9 | 3.9 to 6.3 | <0.001 | <0.001 | |||
| Pulmonary arterial compliance [ml/mmHg] | 5.3 | ± | 2.3 | 4.8 to 5.7 | 100 | 4.0 | ± | 2.1 | 3.5 to 4.5 | 60 | 0.001 | 2.1 | ± | 1.0 | 1.7 to 2.6 | 22 | <0.001 | 0.001 |
| RV pulmonary vascular reserve [mmHg/l/min] | 3.1 | ± | 2.0 | 2.8 to 3.5 | 107 | 6.1 | ± | 15.2 | 2.4 to 9.8 | 9.6 | ± | 7.6 | 6.5 to 12.6 | |||||
| Cardiac index [l/min/m2] | 3.1 | ± | 0.8 | 3.0 to 3.3 | 3.1 | ± | 0.8 | 3.1 to 2.9 | 3.0 | ± | 0.5 | 2.8 to 3.2 | ||||||
| Cardiac index increase during exercise [l/min/m2] | 3.3 | ± | 1.6 | 2.9 to 3.6 | 2.7 | ± | 1.5 | 2.4 to 3.1 | 1.5 | ± | 0.8 | 1.2 to 1.8 | ||||||
| Peak cardiac index [l/min/m2] | 6.4 | ± | 1.7 | 6.1 to 6.7 | 5.8 | ± | 1.7 | 5.4 to 6.2 | 4.5 | ± | 1.0 | 4.1 to 4.9 | ||||||
| Right ventricular pump function | Overall <0.0001 | |||||||||||||||||
| Normal | 105 | 98.1% | 59 | 89.4% | 15 | 57.7% | ||||||||||||
| Mild impairment | 0 | 5 | 7.6% | 4 | 15.4% | |||||||||||||
| Moderate impairment | 0 | 0 | 4 | 15.4% | ||||||||||||||
| Severe impairment | 2 | 1.9% | 2 | 3.0% | 3 | 11.5% | ||||||||||||
Only patients with assessment of both risk parameters were included in the analysis
In case of significant differences, p-values are provided
RF risk factor, SB single breath, SSc systemic sclerosis, VA alveolar volume, WHO-FC World Health Organization functional class
*In case of missing values, n is provided
Right heart size and pressure were significantly greater in patients with more risk factors. Though parameters of RV function were significantly more impaired in patients with one or two risk factors at baseline, CI at rest did not significantly differ between groups. The type of SSc and further laboratory parameters including C-reactive protein and glomerular filtration rate showed no difference between groups.
Pulmonary vascular disease at follow-up
During follow-up, 86 patients who did not present with manifest PH at baseline had a follow-up RHC. Eleven developed manifest PH, 7 presented with mPAP ≥25 mmHg and PVR <3 WU and 10 had mPAP 21–24 mmHg and PVR ≥2 WU.
Sensitivity for prediction of PVD (mildly increased mPAP 21-24 mmHg and PVR ≥2 WU, increased mPAP ≥25 mmHg and PVR <3 WU or manifest PH) during follow-up for at least one risk factor was 75.0%, with a specificity (of not developing PVD during follow-up when presenting with no risk factor at baseline) of 69.0%. If two out of the three risk factors were present at baseline, the false-negative rate (not predicting PVD during follow-up) was 11.1%.
Discussion
This is the first study illustrating that beside known prognostic predictors such as age, DLCO, presence of pulmonary fibrosis and elevated PVR, haemodynamic parameters of RV function at rest and during exercise are very important for risk stratification in patients with SSc, screened for PH. We identified reduced TAPSE/sPAP ratio and reduced RV pulmonary vascular reserve as new independent risk factors for survival. Furthermore, this study showed, that the newly identified multivariable risk set was able to predict the development of PVD during follow-up. In SSc patients who had no signs of PVD at baseline, RV output reserve, assessed by CI increase during exercise <2 l/min/m2 measured by RHC was the only independent prognostic parameter for survival. Thus, the results of this study suggest that RHC during exercise can give meaningful additional clinical information to identify patients, who need to be followed more closely or to receive an early treatment.
Parameters of RV function and reserve
Impairment of TAPSE/sPAP ratio as parameter signalling beginning inability of RV to adopt to pressure elevation in pulmonary vasculature (RV-PA coupling) has been identified as the most important prognostic predictor in our cohort.
It has been previously shown that PAH patients with a TAPSE/sPAP ratio <0.31 mm/mmHg had a worse prognosis [48]. Almost all analysed parameters were significant predictors of survival in the univariable analysis. Known thresholds from the literature were feasible in our cohort of SSc patients including TAPSE/sPAP ratio ≤0.6 mm/mmHg, TAPSE of 18 mm [39], RV pulmonary vascular reserve of 3 ml/min/mmHg according to the current definition of exercise pulmonary hypertension [31].
For PAC, a threshold of 2 ml/mmHg was identified as prognostically relevant, predicting survival in our study cohort. The prognostic value of PAC has been investigated in several studies with thresholds for survival ranging between 1.26 and 2.5 ml/mmHg [49]. In an analysis of the PATENT and CHEST studies, a PAC ≥1.6 ml/mmHg was associated with better outcomes [50]. In patients with systemic lupus erythematosus-associated PAH, PAC <1.39 ml/mmHg was associated with impaired survival with a 3-fold higher risk of all-cause mortality and clinical worsening and was also the only independent predictor for both survival and clinical worsening [51].
As most studies on prognostic predictors in PH have investigated prediction models within Cox proportional hazard models using metric variables, thresholds for other parameters such as peak CI or CI increase during exercise have to be further investigated and validated. Recent data indicate that RV impairment and dysfunction already occur at 50% of peak oxygen uptake or even earlier [52]. Consequently, the timepoint of RV impairment might also provide information on RV function and reserve.
Prognostic meaning of RV function and reserve in different entities
In our study, the main causes of death were P(A)H, pulmonary fibrosis and left heart disease. Both pulmonary fibrosis and left ventricular ejection fraction have been shown to be independently associated with RV free wall strain [53]. Parameters of the identified multivariable risk set included a known prognostic predictor (DLCO) and an echocardiographic parameter obtained at rest (TAPSE/sPAP ratio). In patients who did not present with signs of PVD at baseline, an invasively assessed parameter of RV function during exercise (CI increase) was identified as the only independent predictor for survival. It therefore covers a wide range of pulmonary, as well as vascular pathologies, which are important for different organ manifestations of SSc.
Exercise tests may unmask impaired RV function when the right ventricle at rest still looks normal and functions well. TAPSE/sPAP ratio has already been shown to be crucial for the identification of patients at risk for PH and has been used as tool to identify SSc patients in need of more extensive diagnostics by RHC [41]. The identification of RV output reserve as an independent risk factor in this study confirms the crucial role of exercise testing in patients with SSc to identify early stages of pulmonary hypertension which has been highlighted before [4, 13, 54–56].
Clinical implications and future research
The identified multivariable risk set was not only able to predict survival, but also to identify patients at risk to develop PVD during follow-up. Whether parameters of RV function may be positively influenced by targeted treatment still remains to be investigated. Part of the pharmacotherapeutic effect may be attributed to indirect improvement of RV function by afterload reduction [57].
Strengths and study limitations
This study enables important insights into different prognostic parameters and values representing RV function and reserve obtained from echocardiography and RHC from routine examinations. A major strength of the study is its real-world nature, which makes the study results more applicable to clinical practice. However, a prospective study including a complete set of RV function parameters and right heart catheterisation results also during follow-up to include positive and negative prediction would be desirable.
The reported clinical data were collected in a specialised PH centre, in which RHC during exercise is routinely performed in SSc patients presenting for PH screening. This quite “invasive” procedure is unusual in the management of SSc patients and needs to be revaluated prospectively. However, the described exercise parameters may help to detect a disease worsening at an earlier stage than the corresponding parameters at rest. Early prognostic markers need to be further investigated in future studies with a prospective design.
The study is limited by its retrospective design leading to inconsistent cohort sizes in the different analyses, because of missing values. Values for TDI TV s were missing in >15% of cases, for RV FAC and systolic PAP increase during exercise values were missing in >50% of cases. Furthermore, not all known parameters of RV function and reserve could be analysed (e.g. no strain at rest and during exercise, no magnetic resonance imaging assessment). However, the used parameters reflect the current clinical workup of patients with SSc and therefore offer real-life data of PH screening in SSc. Follow-up data of patients and changes of parameters over time were also not investigated in this study but would have been interesting with regard to screening and prognosis.
Conclusions
This study highlights the importance of RV function and reserve assessments to predict prognosis and to identify patients at risk for development of PH. Exercise assessments may contribute to risk estimation. Therapeutic implications are still to be investigated.
Acknowledgements
This work is the doctoral thesis of JM.
Abbreviations
- 6MWD
6-min walking distance
- APAH
Associated pulmonary arterial hypertension
- CI
Cardiac index
- CI
Cardiac output
- DLCO
Diffusion capacity of carbon monoxide
- ERS
European Respiratory Society
- ESC
European Society of Cardiology
- mPAP
Mean pulmonary arterial pressure
- NT-proBNP
N-terminal pro-brain natriuretic peptide
- PAC
Pulmonary arterial compliance
- PAH
Pulmonary arterial hypertension
- PAWP
Pulmonary arterial wedge pressure
- PH
Pulmonary hypertension
- PVD
Pulmonary vascular disease
- PVR
Pulmonary vascular resistance
- RHC
Right heart catheterisation
- ROC
Receiver operating characteristic
- RV
Right ventricular
- RV-FAC
Right ventricular fractional area change
- SD
Standard deviation
- SSc
Systemic sclerosis
- lcSSc
Limited cutaneous form of systemic sclerosis
- dcSSc
Diffuse cutaneous form of systemic sclerosis
- SSc-APAH
Systemic sclerosis-associated pulmonary arterial hypertension
- TAPSE
Tricuspid annular plane systolic excursion
- TDI
Tissue Doppler imaging
- WHO-FC
World Health Organization functional class
- WU
Wood Unit(s)
Authors’ contributions
Designing of the study: EG, PX, NBe, CAE. Acquisition of data: PX, JM, EG, NBl, HML, OG, BE, SH, RS, AMM. Analysis and interpretation of data: NBe, EG, JM, PX, AMM, NBl, HML, CAE. Drafting of the manuscript: NBe, JM, EG, CAE. Revision of manuscript, substantial intellectual contribution to the work and final approval: all authors.
Funding
Open Access funding enabled and organized by Projekt DEAL. For the publication fee we acknowledge financial support by Deutsche Forschungsgemeinschaft within the funding programme “Open Access Publikationskosten” as well as by Heidelberg University.
Availability of data and materials
The datasets used and/or analysed during the current study were available in the patient files at Thoraxklinik Heidelberg gGmbH, Heidelberg.
Declarations
Ethics approval and consent to participate
All data were pseudonymised, and the study was approved by the ethics committee of the medical faculty of Heidelberg University Hospital (internal number S-305/2021). The study complies with the Declaration of Helsinki in its current version.
Consent for publication
Not applicable.
Competing interests
PX: has received personal fees from MSD and OMT outside the submitted work.
JM, OJ, RS, CAE, NBe: nothing to declare.
BE: received travel fees, consulting fees, speaking fees, and/or honoraria from Actelion, MSD, Bayer and OMT, outside the submitted work.
SH: received honoraria for lectures, consultancy, or both from Actelion, AOP, Bayer/MSD, GSK, Novartis, OMT, Pfizer, and United Therapeutics out-side the submitted work.
AMM: AMM has received personal fees from Bayer, outside the submitted work.
NBl: has received consulting fees, speaking fees and/or honoraria and unallocated funds from Roche out-side the submitted work.
HML: has received consulting fees, speaking fees and/or honoraria and unallocated funds for scientific talks and consultations from Abbvie, Astra-Zeneca, Actelion, Alexion, Amgen, Bayer Vital, Baxter, Biogen, Boehringer Ingelheim, BMS, Celgene, Fresenius, Genzyme, GSK, Gilead/Galapagos, Hexal, Janssen-Cilag, Lilly, Medac, MSD, Mundipharm, Mylan, Novartis, octapharm, Pfizer, Roche/Chugai, Sandoz, Sanofi, Shire, SOBI, Thermo Fisher, UCB.
EG: has received grants and personal fees from Actelion, Bayer AG, and MSD; grants from GSK, Novartis, and United Therapeutics and personal fees from SCOPE, OrPha Swiss GmbH, and Zurich Heart House, outside the submitted work. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Denton CP, Khanna D. Systemic sclerosis. Lancet. 2017;390(10103):1685–1699. doi: 10.1016/S0140-6736(17)30933-9. [DOI] [PubMed] [Google Scholar]
- 2.Mukerjee D, St George D, Coleiro B, Knight C, Denton CP, Davar J, Black CM, Coghlan JG. Prevalence and outcome in systemic sclerosis associated pulmonary arterial hypertension: application of a registry approach. Ann Rheum Dis. 2003;62(11):1088–1093. doi: 10.1136/ard.62.11.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wigley FM, Lima JA, Mayes M, McLain D, Chapin JL, Ward-Able C. The prevalence of undiagnosed pulmonary arterial hypertension in subjects with connective tissue disease at the secondary health care level of community-based rheumatologists (the UNCOVER study) Arthritis Rheum. 2005;52(7):2125–2132. doi: 10.1002/art.21131. [DOI] [PubMed] [Google Scholar]
- 4.Hachulla E, Carpentier P, Gressin V, Diot E, Allanore Y, Sibilia J, Launay D, Mouthon L, Jego P, Cabane J, et al. Risk factors for death and the 3-year survival of patients with systemic sclerosis: the French ItinerAIR-Sclerodermie study. Rheumatology (Oxford) 2009;48(3):304–308. doi: 10.1093/rheumatology/ken488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nihtyanova SI, Schreiber BE, Ong VH, Rosenberg D, Moinzadeh P, Coghlan JG, Wells AU, Denton CP. Prediction of pulmonary complications and long-term survival in systemic sclerosis. Arthritis Rheumatol. 2014;66(6):1625–1635. doi: 10.1002/art.38390. [DOI] [PubMed] [Google Scholar]
- 6.Morrisroe K, Stevens W, Huq M, Prior D, Sahhar J, Ngian GS, Celermajer D, Zochling J, Proudman S, Nikpour M, et al. Survival and quality of life in incident systemic sclerosis-related pulmonary arterial hypertension. Arthritis Res Ther. 2017;19(1):122. doi: 10.1186/s13075-017-1341-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galiè N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, Barbera JA, Beghetti M, Corris P, Gaine S, Gibbs JS, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT) Eur Heart J. 2009;30(20):2493–2537. doi: 10.1093/eurheartj/ehp297. [DOI] [PubMed] [Google Scholar]
- 8.Grünig E, Tiede H, Enyimayew EO, Ehlken N, Seyfarth HJ, Bossone E, D'Andrea A, Naeije R, Olschewski H, Ulrich S, et al. Assessment and prognostic relevance of right ventricular contractile reserve in patients with severe pulmonary hypertension. Circulation. 2013;128(18):2005–2015. doi: 10.1161/CIRCULATIONAHA.113.001573. [DOI] [PubMed] [Google Scholar]
- 9.Brown ZR, Nikpour M. Screening for pulmonary arterial hypertension in systemic sclerosis: Now or never! Eur J Rheumatol. 2020;7(Suppl 3):S187–S192. doi: 10.5152/eurjrheum.2020.19114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT) Eur Heart J. 2016;37(1):67–119. doi: 10.1093/eurheartj/ehv317. [DOI] [PubMed] [Google Scholar]
- 11.Coghlan JG, Denton CP, Grünig E, Bonderman D, Distler O, Khanna D, Müller-Ladner U, Pope JE, Vonk MC, Doelberg M, et al. Evidence-based detection of pulmonary arterial hypertension in systemic sclerosis: the DETECT study. Ann Rheum Dis. 2014;73(7):1340–1349. doi: 10.1136/annrheumdis-2013-203301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grünig E, Benjamin N, Krüger U, Kaemmerer H, Harutyunova S, Olsson KM, Ulrich S, Gerhardt F, Neurohr C, Sablotzki A, et al. General measures and supportive therapy for pulmonary arterial hypertension: Updated recommendations from the Cologne Consensus Conference 2018. Int J Cardiol. 2018;272S:30–36. doi: 10.1016/j.ijcard.2018.08.085. [DOI] [PubMed] [Google Scholar]
- 13.Nagel C, Marra AM, Benjamin N, Blank N, Cittadini A, Coghlan G, Distler O, Denton CP, Egenlauf B, Fiehn C, et al. Reduced Right Ventricular Output Reserve in Patients With Systemic Sclerosis and Mildly Elevated Pulmonary Artery Pressure. Arthritis Rheumatol. 2019;71(5):805–816. doi: 10.1002/art.40814. [DOI] [PubMed] [Google Scholar]
- 14.Denton CP, Hachulla E. Risk factors associated with pulmonary arterial hypertension in patients with systemic sclerosis and implications for screening. Eur Respir Rev. 2011;20(122):270–276. doi: 10.1183/09059180.00006111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galiè N, McLaughlin VV, Rubin LJ, Simonneau G. An overview of the 6th World Symposium on Pulmonary Hypertension. Eur Respir J. 2019;53(1):1802148. [DOI] [PMC free article] [PubMed]
- 16.Simonneau G, Montani D, Celermajer DS, Denton CP, Gatzoulis MA, Krowka M, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53(1):1801913. [DOI] [PMC free article] [PubMed]
- 17.Thomas CA, Anderson RJ, Condon DF, de Jesus Perez VA. Diagnosis and Management of Pulmonary Hypertension in the Modern Era: Insights from the 6th World Symposium. Pulm Ther. 2020;6(1):9–22. doi: 10.1007/s41030-019-00105-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xanthouli P, Jordan S, Milde N, Marra A, Blank N, Egenlauf B, Gorenflo M, Harutyunova S, Lorenz HM, Nagel C, et al. Haemodynamic phenotypes and survival in patients with systemic sclerosis: the impact of the new definition of pulmonary arterial hypertension. Ann Rheum Dis. 2020;79(3):370–378. doi: 10.1136/annrheumdis-2019-216476. [DOI] [PubMed] [Google Scholar]
- 19.Kovacs G, Berghold A, Scheidl S, Olschewski H. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J. 2009;34(4):888–894. doi: 10.1183/09031936.00145608. [DOI] [PubMed] [Google Scholar]
- 20.Kovacs G, Olschewski A, Berghold A, Olschewski H. Pulmonary vascular resistances during exercise in normal subjects: a systematic review. Eur Respir J. 2012;39(2):319–328. doi: 10.1183/09031936.00008611. [DOI] [PubMed] [Google Scholar]
- 21.Almeida AR, Loureiro MJ, Lopes L, Cotrim C, Lopes L, Repolho D, Pereira H. Echocardiographic assessment of right ventricular contractile reserve in patients with pulmonary hypertension. Rev Port Cardiol. 2014;33(3):155–163. doi: 10.1016/j.repc.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 22.Guo DC, Li YD, Yang YH, Zhu WW, Sun LL, Jiang W, Ye XG, Cai QZ, Lu XZ. Influence of impaired right ventricular contractile reserve on exercise capacity in patients with precapillary pulmonary hypertension: A study with exercise stress echocardiography. Echocardiography. 2019;36(4):671–677. doi: 10.1111/echo.14283. [DOI] [PubMed] [Google Scholar]
- 23.Haddad F, Vrtovec B, Ashley EA, Deschamps A, Haddad H, Denault AY. The concept of ventricular reserve in heart failure and pulmonary hypertension: an old metric that brings us one step closer in our quest for prediction. Curr Opin Cardiol. 2011;26(2):123–131. doi: 10.1097/HCO.0b013e3283437485. [DOI] [PubMed] [Google Scholar]
- 24.Grünig E, Eichstaedt CA, Seeger R, Benjamin N. Right heart size and right ventricular reserve in pulmonary hypertension: impact on management and prognosis. Diagnostics (Basel). 2020;10(12):1110. [DOI] [PMC free article] [PubMed]
- 25.Blumberg FC, Arzt M, Lange T, Schroll S, Pfeifer M, Wensel R. Impact of right ventricular reserve on exercise capacity and survival in patients with pulmonary hypertension. Eur J Heart Fail. 2013;15(7):771–775. doi: 10.1093/eurjhf/hft044. [DOI] [PubMed] [Google Scholar]
- 26.van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, Matucci-Cerinic M, Naden RP, Medsger TA, Jr, Carreira PE, et al. 2013 classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis. 2013;72(11):1747–1755. doi: 10.1136/annrheumdis-2013-204424. [DOI] [PubMed] [Google Scholar]
- 27.LeRoy EC, Medsger TA., Jr Criteria for the classification of early systemic sclerosis. J Rheumatol. 2001;28(7):1573–1576. [PubMed] [Google Scholar]
- 28.Xanthouli P, Koegler M, Marra AM, Benjamin N, Fischer L, Eichstaedt CA, Harutyunova S, Nagel C, Grünig E, Egenlauf B. Risk stratification and prognostic factors in patients with pulmonary arterial hypertension and comorbidities a cross-sectional cohort study with survival follow-up. Respir Res. 2020;21(1):127. doi: 10.1186/s12931-020-01393-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosenkranz S, Preston IR. Right heart catheterisation: best practice and pitfalls in pulmonary hypertension. Eur Respir Rev. 2015;24(138):642–652. doi: 10.1183/16000617.0062-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kovacs G, Avian A, Olschewski A, Olschewski H. Zero reference level for right heart catheterisation. Eur Respir J. 2013;42(6):1586–1594. doi: 10.1183/09031936.00050713. [DOI] [PubMed] [Google Scholar]
- 31.Kovacs G, Herve P, Barbera JA, Chaouat A, Chemla D, Condliffe R, Garcia G, Grünig E, Howard L, Humbert M, et al. An official European Respiratory Society statement: pulmonary haemodynamics during exercise. Eur Respir J. 2017;50(5):1700578. doi: 10.1183/13993003.00578-2017. [DOI] [PubMed] [Google Scholar]
- 32.Ghio S, Klersy C, Magrini G, D'Armini AM, Scelsi L, Raineri C, Pasotti M, Serio A, Campana C, Vigano M. Prognostic relevance of the echocardiographic assessment of right ventricular function in patients with idiopathic pulmonary arterial hypertension. Int J Cardiol. 2010;140(3):272–278. doi: 10.1016/j.ijcard.2008.11.051. [DOI] [PubMed] [Google Scholar]
- 33.Avouac J, Huscher D, Furst DE, Opitz CF, Distler O, Allanore Y. group E: Expert consensus for performing right heart catheterisation for suspected pulmonary arterial hypertension in systemic sclerosis: a Delphi consensus study with cluster analysis. Ann Rheum Dis. 2014;73(1):191–197. doi: 10.1136/annrheumdis-2012-202567. [DOI] [PubMed] [Google Scholar]
- 34.Vonk Noordegraaf A, Chin KM, Haddad F, Hassoun PM, Hemnes AR, Hopkins SR, et al. Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: an update. Eur Respir J. 2019;53(1):1801900. [DOI] [PMC free article] [PubMed]
- 35.Vonk Noordegraaf A, Westerhof BE, Westerhof N. The Relationship Between the Right Ventricle and its Load in Pulmonary Hypertension. J Am Coll Cardiol. 2017;69(2):236–243. doi: 10.1016/j.jacc.2016.10.047. [DOI] [PubMed] [Google Scholar]
- 36.Vonk-Noordegraaf A, Haddad F, Chin KM, Forfia PR, Kawut SM, Lumens J, Naeije R, Newman J, Oudiz RJ, Provencher S, et al. Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol. 2013;62(25 Suppl):D22–D33. doi: 10.1016/j.jacc.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 37.Vonk-Noordegraaf A, Westerhof N. Describing right ventricular function. Eur Respir J. 2013;41(6):1419–1423. doi: 10.1183/09031936.00160712. [DOI] [PubMed] [Google Scholar]
- 38.Jain P, Rao S, Macdonald P, Kotlyar E, Jabbour A, Hayward C, Keogh A. Diagnostic Performance of Pulmonary Capacitance at Rest and During Exercise in Idiopathic Pulmonary Arterial Hypertension. Heart Lung Circ. 2019;28(2):289–294. doi: 10.1016/j.hlc.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 39.Forfia PR, Fisher MR, Mathai SC, Housten-Harris T, Hemnes AR, Borlaug BA, Chamera E, Corretti MC, Champion HC, Abraham TP, et al. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med. 2006;174(9):1034–1041. doi: 10.1164/rccm.200604-547OC. [DOI] [PubMed] [Google Scholar]
- 40.Ghio S, Pica S, Klersy C, Guzzafame E, Scelsi L, Raineri C, Turco A, Schirinzi S, Visconti LO. Prognostic value of TAPSE after therapy optimisation in patients with pulmonary arterial hypertension is independent of the haemodynamic effects of therapy. Open Heart. 2016;3(1):e000408. doi: 10.1136/openhrt-2016-000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Colalillo A, Grimaldi MC, Vaiarello V, Pellicano C, Leodori G, Gigante A, et al. In systemic sclerosis TAPSE/sPAP ratio can be used in addition to the DETECT algorithm for pulmonary arterial hypertension diagnosis. Rheumatology (Oxford). 2021;61(6):2450–6. [DOI] [PubMed]
- 42.Lewis GD, Bossone E, Naeije R, Grünig E, Saggar R, Lancellotti P, Ghio S, Varga J, Rajagopalan S, Oudiz R, et al. Pulmonary vascular hemodynamic response to exercise in cardiopulmonary diseases. Circulation. 2013;128(13):1470–1479. doi: 10.1161/CIRCULATIONAHA.112.000667. [DOI] [PubMed] [Google Scholar]
- 43.Naeije R, Vanderpool R, Dhakal BP, Saggar R, Saggar R, Vachiery JL, Lewis GD. Exercise-induced pulmonary hypertension: physiological basis and methodological concerns. Am J Respir Crit Care Med. 2013;187(6):576–583. doi: 10.1164/rccm.201211-2090CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chung L, Domsic RT, Lingala B, Alkassab F, Bolster M, Csuka ME, Derk C, Fischer A, Frech T, Furst DE, et al. Survival and predictors of mortality in systemic sclerosis-associated pulmonary arterial hypertension: outcomes from the pulmonary hypertension assessment and recognition of outcomes in scleroderma registry. Arthritis Care Res (Hoboken) 2014;66(3):489–495. doi: 10.1002/acr.22121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chung L, Farber HW, Benza R, Miller DP, Parsons L, Hassoun PM, McGoon M, Nicolls MR, Zamanian RT. Unique predictors of mortality in patients with pulmonary arterial hypertension associated with systemic sclerosis in the REVEAL registry. Chest. 2014;146(6):1494–1504. doi: 10.1378/chest.13-3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Panopoulos S, Bournia VK, Konstantonis G, Fragiadaki K, Sfikakis PP, Tektonidou MG. Predictors of morbidity and mortality in early systemic sclerosis: Long-term follow-up data from a single-centre inception cohort. Autoimmun Rev. 2018;17(8):816–820. doi: 10.1016/j.autrev.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 47.Fischer L, Benjamin N, Blank N, Egenlauf B, Fischer C, Harutyunova S, Koegler M, Lorenz HM, Marra AM, Nagel C, et al. Right heart size and function significantly correlate in patients with pulmonary arterial hypertension - a cross-sectional study. Respir Res. 2018;19(1):216. doi: 10.1186/s12931-018-0913-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tello K, Wan J, Dalmer A, Vanderpool R, Ghofrani HA, Naeije R, Roller F, Mohajerani E, Seeger W, Herberg U, et al. Validation of the Tricuspid Annular Plane Systolic Excursion/Systolic Pulmonary Artery Pressure Ratio for the Assessment of Right Ventricular-Arterial Coupling in Severe Pulmonary Hypertension. Circ Cardiovasc Imaging. 2019;12(9):e009047. doi: 10.1161/CIRCIMAGING.119.009047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rajdev K, Lahan S, Wichman T. Role of pulmonary arterial capacitance in predicting mortality in patients with pulmonary hypertension: A systematic review and meta-analysis. Int J Cardiol. 2021;333:202–209. doi: 10.1016/j.ijcard.2021.02.043. [DOI] [PubMed] [Google Scholar]
- 50.Thenappan T, Al-Naamani N, Ghio S, Ghofrani HA, Hassoun PM, Pritzker M, Torbicki A, Nikkho S, Busse D, Preston IR. Effect of riociguat on pulmonary arterial compliance in the PATENT and CHEST studies. Pulm Circ. 2020;10(4):2045894020963836. doi: 10.1177/2045894020963836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guo X, Lai J, Wang H, Tian Z, Zhao J, Li M, Fang Q, Fang L, Liu Y, Zeng X. Predictive Value of Pulmonary Arterial Compliance in Systemic Lupus Erythematosus Patients With Pulmonary Arterial Hypertension. Hypertension. 2020;76(4):1161–1168. doi: 10.1161/HYPERTENSIONAHA.120.15682. [DOI] [PubMed] [Google Scholar]
- 52.Singh I, Oliveira RKF, Heerdt P, Brown MB, Faria-Urbina M, Waxman AB, Systrom DM. Dynamic right ventricular function response to incremental exercise in pulmonary hypertension. Pulm Circ. 2020;10(3):2045894020950187. doi: 10.1177/2045894020950187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yiu KH, Ninaber MK, Kroft LJ, Schouffoer AA, Stolk J, Scherer HU, Meijs J, de Vries-Bouwstra J, Tse HF, Delgado V, et al. Impact of pulmonary fibrosis and elevated pulmonary pressures on right ventricular function in patients with systemic sclerosis. Rheumatology (Oxford) 2016;55(3):504–512. doi: 10.1093/rheumatology/kev342. [DOI] [PubMed] [Google Scholar]
- 54.D'Alto M, Ghio S, D'Andrea A, Pazzano AS, Argiento P, Camporotondo R, Allocca F, Scelsi L, Cuomo G, Caporali R, et al. Inappropriate exercise-induced increase in pulmonary artery pressure in patients with systemic sclerosis. Heart. 2011;97(2):112–117. doi: 10.1136/hrt.2010.203471. [DOI] [PubMed] [Google Scholar]
- 55.Chia EM, Lau EM, Xuan W, Celermajer DS, Thomas L. Exercise testing can unmask right ventricular dysfunction in systemic sclerosis patients with normal resting pulmonary artery pressure. Int J Cardiol. 2016;204:179–186. doi: 10.1016/j.ijcard.2015.11.186. [DOI] [PubMed] [Google Scholar]
- 56.Hachulla E, Gressin V, Guillevin L, Carpentier P, Diot E, Sibilia J, Kahan A, Cabane J, Frances C, Launay D, et al. Early detection of pulmonary arterial hypertension in systemic sclerosis: a French nationwide prospective multicenter study. Arthritis Rheum. 2005;52(12):3792–3800. doi: 10.1002/art.21433. [DOI] [PubMed] [Google Scholar]
- 57.Tello K, Seeger W, Naeije R, Vanderpool R, Ghofrani HA, Richter M, Tedford RJ, Bogaard HJ. Right heart failure in pulmonary hypertension: Diagnosis and new perspectives on vascular and direct right ventricular treatment. Br J Pharmacol. 2021;178(1):90–107. doi: 10.1111/bph.14866. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study were available in the patient files at Thoraxklinik Heidelberg gGmbH, Heidelberg.