Abstract
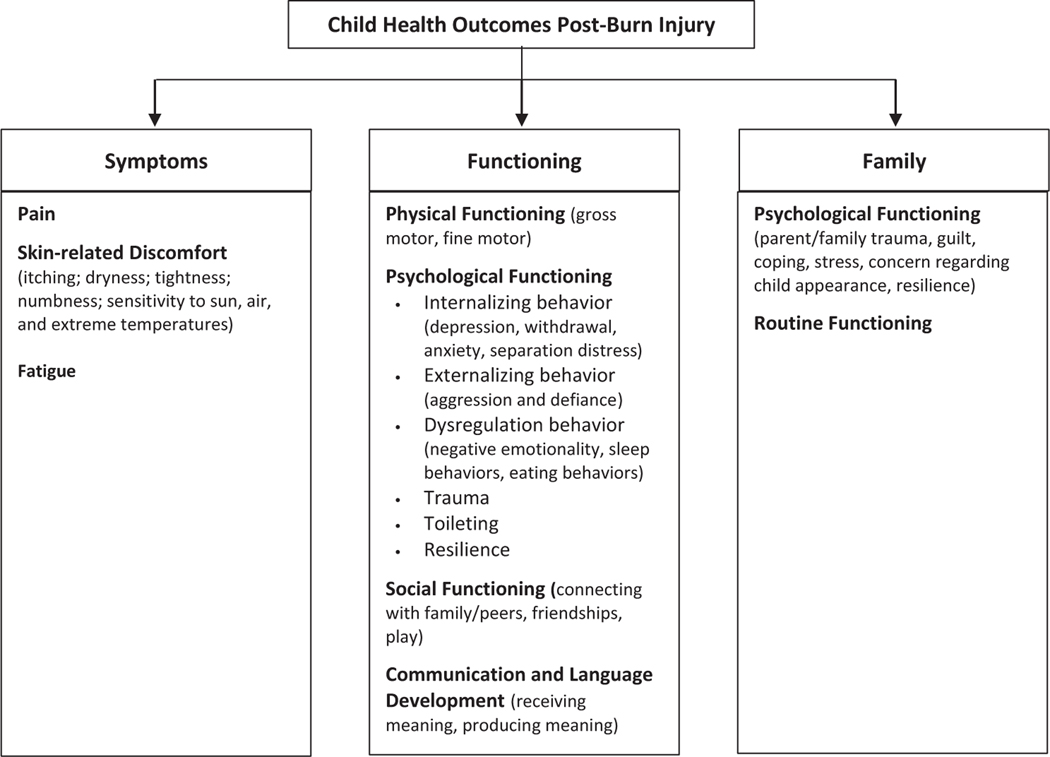
Due to the rapid developmental growth in preschool-aged children, more precise measurement of the effects of burns on child health outcomes is needed. Expanding upon the Shriners Hospitals for Children/American Burn Association Burn Outcome Questionnaire 0 to 5 (BOQ0–5), we developed a conceptual framework describing domains important in assessing recovery from burn injury among preschool-aged children (1–5 years). We developed a working conceptual framework based on the BOQ0–5, the National Research Council and Institute of Medicine’s Model of Child Health, and the World Health Organization’s International Classification of Functioning, Disability, and Health for Children and Youth. We iteratively refined our framework based on a literature review, focus groups, interviews, and expert consensus meetings. Data were qualitatively analyzed using methods informed by grounded theory. We reviewed 95 pediatric assessments, conducted two clinician focus groups and six parent interviews, and consulted with 23 clinician experts. Three child health outcome domains emerged from our analysis: symptoms, functioning, and family. The symptoms domain describes parents’ perceptions of their child’s pain, skin-related discomfort, and fatigue. The functioning domain describes children’s physical functioning (gross and fine motor function), psychological functioning (internalizing, externalizing, and dysregulation behavior; trauma; toileting; resilience), communication and language development (receiving and producing meaning), and social functioning (connecting with family/peers, friendships, and play). The family domain describes family psychological and routine functioning outcomes.
Burns are a leading cause of injury in young children, with children under 5 years of age accounting for the highest incidence of pediatric burn injuries worldwide.1 Compared to the general population, children 5 years and younger are 2.4 times more likely to sustain a burn injury necessitating emergency medical care.2 The majority of pediatric burns are nonfatal and can have a significant impact on the health and development of young children.3 This is at an age where childhood experiences shape lifelong functioning.4 Thus, optimal recovery requires the systematic assessment of child outcomes across physical, psychological, and social health and developmental domains.
The Burn Outcome Questionnaire 0 to 5 (BOQ0–5) is presently one of the few parent-reported, burn-specific measures available to assess child health outcomes postburn injury among children 5 years and younger. The BOQ0–5 is a 55-item questionnaire that assesses child recovery from burn injury across 10 domains.5,6 While the BOQ0–5 is well established,6–8 its precision in assessing the effects of burn injury on the health and development of young children is limited by its fixed-form format as a legacy measure. This limitation is exacerbated by children’s rapid growth during the first 5 years of life, which necessitates increases in the number of items included in a metric to more precisely capture change along the developmental continuum compared to a legacy measure counterpart. Increases in the number of items included in a fixed-form metric like the BOQ0–5, in turn, come at the cost of increased respondent burden. However, developing a computerized adaptive test (CAT) instrument that builds upon BOQ0–5 item content can address this problem.
CAT instruments use item response theory and computer software to tailor the items administered to each respondent based on real-time estimates of a respondent’s ability level on the underlying construct assessed. Using a CAT-based outcome instrument, precise estimates of a person’s location on the underlying continuum can often be obtained after administering only 5 to 10 items. Precise estimates for CATs, in turn, often rely on banks of items with content that spans a hierarchically organized continuum of items assessing the underlying construct(s).
The development of item banks should be informed by a comprehensive conceptual framework designed to ensure adequate item content coverage and, consequently, construct validity and precision. While several models of child health and burn outcomes exist, there is a need for an integrative framework identifying the impact of burn injury on the health and developmental outcomes of preschool-aged children. Drawing upon established conceptual models of child health, development, and burn injury, the goal of this study was to develop a conceptual framework identifying outcomes that are important in the assessment of parent-reported recovery from burn injury among preschool-aged children (1–5 years of age). Through a literature review, focus groups, interviews, and expert consensus meetings, we aimed to identify health domains that 1) are most impacted by burn injuries, 2) reflect the dynamic developmental nature of children’s health between 1 and 5 years, and 3) could be reliably assessed by parent report. Our findings are synthesized in an overarching conceptual framework for assessing health outcomes in preschool-aged children with burn injuries, which will guide the development of item banks for the Preschool Life Impact Burn Recovery Evaluation Profile CAT.
METHODS
Initial Conceptual Framework Development
We developed an initial conceptual framework based on definitions and constructs synthesized from the BOQ0–5,5 National Research Council and Institute of Medicine’s Model of Child Health (MCH),4 and the World Health Organization’s International Classification for Disability, Functioning and Health for Children and Youth (ICF-CY).9 These models take a biopsychosocial approach to conceptualizing the complex interactions among biological, psychological, and social factors that may affect child health outcomes. Next, we reviewed the literature for generic- and burn-specific instruments that assess health and development in children 1 to 5 years of age via MEDLINE/PubMed, Web of Science, and a manual reference check. Drawing conceptual foundations from the BOQ0–5, MCH, and the ICF-CY, we developed both broad and domain-specific search queries (see Supplementary Appendix 1). Our broad search query included child descriptors (eg, child and pediatric), health descriptors (eg, health, development and function), and measure descriptors (eg, measure, scale, and questionnaire). Our domain-specific queries included additional terms related to child health and development in physical, social, emotional, sleep, communication/language, family, and burn symptom (pain and itch) domains. Our manual reference check included a review of: 1) well-known developmental checklists (eg, Bright Futures and Centers for Disease Control and Prevention Developmental Milestones); 2) existing pediatric CAT item banks (PROMIS, Neuro-QOL, and NIH Toolbox); and 3) published reviews of pediatric health and developmental assessments. Instruments and checklists were excluded from our review if they were not in English, did not apply to children 1 to 5 years of age, or were not accessible. From each assessment included in our review, we extracted the domains and item content assessed.
Identifying Gaps and Validating Existing Content
To identify gaps in our working conceptual framework and to validate existing content, we conducted in-person and phone-based clinician focus groups and semi-structured, parent interviews. Clinician participants were asked to share their opinions regarding the effect of a burn injury on the health, development, and family life of children 1 to 5 years of age; parent participants were asked to share their opinions regarding the effect of their child’s burn injury on their child’s health, development, and their family. Clinician focus group participants were convenience sampled from burn centers across the United States. We aimed to sample a diverse group of clinicians with expertise in pediatric burn care and/or child development. Parent interview participants were from a convenience sample based on the electronic health records of children 1 to 5 years of age who received inpatient and/or outpatient burn care at Shriners Hospitals for Children—Boston. The focus group and interview guides were informed by our working conceptual framework, which asked about the impact of a burn injury 1) on particular domains of a child’s health and development and 2) in any other areas that participants felt were important (see Supplementary Appendices 2–4). Focus group and interview data were recorded in notes and audio recordings. Data were collected until thematic saturation was reached.
Data Analysis
Qualitative data from the existing conceptual frameworks, the literature review, clinician focus groups, and parent interviews (notes and transcribed audio recordings) were inductively and deductively analyzed using methods informed by grounded theory.10–12 Constructs drawn from each of these sources were iteratively selected and adapted based on ongoing group consensus meetings with pediatric burn and developmental experts. Our final conceptual framework represents a synthesis of findings from each phase of the study. Quantitative data are described using means and standard deviations and frequencies and proportions (for continuous and categorical variables, respectively). This study was approved by the Western Institutional Review Board and the Boston University Medical Campus Institutional Review Board.
RESULTS
Literature Review
Of the 226 assessments identified in our literature search, 95 (42%) met our inclusion criteria and were included in our review (Supplementary Appendix 5). Included assessments were classified within the health outcome domains that emerged from our analysis: symptoms, functioning, and family. Pain, skin-related discomfort, and fatigue symptoms were assessed in a respective 16, 6, and 8% of the assessments included in our review. Children’s functioning in physical, psychological, social, and communication and language domains were assessed in 30, 53, 43, and 26% of included assessments, respectively. Family psychological functioning and routine functioning were assessed within 8 and 6% of included assessments, respectively.
Clinician Focus Groups and Parent Interviews
Eleven clinicians participated in two focus groups. Focus group participants included: a nurse, nurse practitioners, physical therapists, an occupational therapist, a pediatrician, an elementary school teacher, child life specialists, and a care coordinator (with some participants possessing more than one of these roles). Six parents participated in semi-structured interviews. On average, parent interview participants were 35 years of age with a greater proportion being male (66.6%; Table 1). Children were mostly male (66.6%) and, on average, 41.7 months of age at the time of the interview. The majority of children (83.3%) had a burn located on one or more critical areas, including the face, hands, and feet. All children had a total body surface area (TBSA) burn of ≤15%, were treated as inpatients at the time of their burn injury, and were treated later as outpatients. On average, 1.7 years had elapsed since the date of children’s burn injuries.
Table 1.
Parent and child demographics and characteristics of the burn injury (n = 6)
| Variable | |
|---|---|
|
| |
| Parent | |
| Age (years), mean (SD) | 35 (2.8) |
| Female, n (%) | 2 (33.3%) |
| White, n (%) | 6 (100%) |
| Education, n (%) | |
| Completed high school or equivalent | 1 (16.7%) |
| Completed some college | 2 (33.3%) |
| Completed bachelor’s degree | 2 (33.3%) |
| Completed graduate degree or higher | 1 (16.7%) |
| Living with spouse/partner, n (%) | 6 (100%) |
| Children under 18 living at home, mean (SD) | 2 (0.9) |
| Child | |
| Age (months) at time of burn, mean (SD) | 21.0 (10.8) |
| Age (months) at time of interview, mean (SD) | 41.7 (10.4) |
| Female, n (%) | 2 (33.3%) |
| Burn to one or more critical areas, n (%) | 5 (83.3%) |
| Years elapsed since burn injury, mean (SD) | 1.7 (0.49) |
Expert Feedback
Twenty-three clinicians, researchers, and burn community advocates with expertise in pediatric burn care and/or child development provided expert feedback on iterations of the conceptual framework in group consensus meetings throughout the course of the study. Experts included: burn surgeons, psychologists/clinical psychologists, child and adolescent psychiatrists, nurse practitioners, nurses, occupational therapists, physical therapists, child life specialists, burn community advocates, a licensed independent clinical social worker, a care coordinator, and health services researchers.
Conceptualizing Parent-Reported Health Outcomes Postburn Injury for Preschool-Aged Children
Figure 1 presents the conceptual framework developed based on study findings and informed by the conceptual foundations of the BOQ0–5,5 MCH,4 and the ICF-CY.9 This framework describes three health outcome domains that were identified as important in assessing the recovery of preschool-aged children (1–5 years) from burn injury: symptoms, functioning, and family. Each of these outcomes are conceptualized as indicators of different facets of child health. In accordance with the MCH model, we define child health as the extent to which children “are able or enabled to: a) develop and realize their potential, b) satisfy their needs, and c) develop the capacities that allow them to interact successfully with their biological, physical, and social environments”.4 A central feature of this definition is its focus on child development, or the age-specific growth and maintenance of functioning over time, which occurs within the context of the child’s family environment.9 This conceptualization of child health forms the basis for our conceptual framework. Below, we describe the subdomains that comprise each health outcome domain and the data sources that influenced the development of model constructs. In Table 2, we present selected quotations from focus groups and interviews that illustrate the role of each construct as an important health outcome for preschool-aged children postburn injury.
Figure 1. Conceptual framework of parent-reported child health outcomes postburn injury for children 1 to 5 years.
Table 2.
Quotations illustrating conceptual framework outcome domains and subdomains
| Outcome domains | Outcome subdomains | Illustrative quotations |
|---|---|---|
|
| ||
| Symptoms | – | Parent 3: “Immediately after the burn, it certainly changed- the burn was on his chest- and he didn’t want to be held. He wanted to be held but it was painful to be held.” |
| Parent 2: “…like these are the common things to happen after a burn like when your skin is growing back, how itchy you are, or the fact when air touches it, it’s going to hurt worse than if it’s bandaged up...” | ||
| Parent 3: “…we tried to keep him from itching himself while the burns were healing which is difficult to do.” | ||
| Parent 1: “The main thing that affected his life is that he has to wear a sun protection sleeve on his arm…and it does itch sometimes.” | ||
| Parent 6: “If she’s outside [or it’s] very cold, [her] palm is very sensitive” | ||
| Clinician focus group 2: “I’m seeing burn fatigue, especially in large burns.” | ||
| Functioning | – | Clinician focus group 1: “I believe like most of the kids tend to regress in that age domain, whether they’re starting to potty train or sleeping through the night or starting to walk... especially the big injuries but even the smaller injuries... Any kind of trauma tends to let them regress at that age.” |
| Parent 5: “She was way ahead of other kids for her age [before the burn injury], and she really regressed.” | ||
| Clinician focus group 2: “We might not necessarily see a regression, but time almost stands still. There is not a continued development…once the injury happens, we might stop there. A month or two- six months after there’s a regression. Not that they moved backward…but they stopped progressing.” | ||
| Clinician focus group 1: “Some kids don’t regress and use the opportunity to further their growth…and it makes them more resilient.” | ||
| Functioning | Physical functioning | Clinician focus group 2: “Physical development is such a huge part in the success and longterm development in this age group. It’s how they explore, and it’s directly linked to their cognitive development.” |
| Clinician focus group 1: “We regularly see large regression in their motor development in this age range.” | ||
| Clinician focus group 2: “Toddlers are really mastering ambulation, [they] move from just learning how to walk to mastering walking, potentially running, and small jumping. Any kind of lower extremity burn injuries that are large enough can affect that development from that age span [1–2 years].” | ||
| Clinician focus group 2: “If the child that sustains a hand burn injury that limit the ability to use their hand, they lose that ability to master fine motor, ability to feed themselves. So much of their learning and exploration is through the use of those hands- everything from play to mimicking, what they’re seeing adults around them and to what older children are doing.” | ||
| Parent 4: “When we finally took it [a sock] off [his hand] and told him ‘Okay, your thumb has healed. We don’t need to put bandages on any more. He, for a while after that, was just used to not doing anything with that hand. He would just hold his hand out to the side, at like an angle. It took him a while to realize that he can pick things up. He sort of babied it for so long. He just got used to holding it to the side.” | ||
| Parent 6: “Eating was the most prevalent change…After a month, [she was] able [to] eat on her own again…had to hand feed her until [her] hands were better.” | ||
| Parent 3: “Certainly right after the injury, he was in pain and not as active…[he] didn’t want to walk around as much...” | ||
| Functioning | Psychological functioning: internalizing behaviors | Clinician focus group 2: “At this age range, kids are more withdrawn. You expect them to be more social- asking questions, maintain eye contact. You’ll see kids completely crumple into themselves.” |
| Parent 3: “I think within the first month, it was rough on him and he was a little shy.” | ||
| Clinician focus group 2: “Behaviors I typically see [are]: head down, no eye contact, very minimal verbalizations, short words, inability to attain any concentration.” | ||
| Clinician focus group 1: “Separation from caregivers in general could be harder. Any sort of separation from parents like being dropped off at a playdate – are they more clingy? Are they not going to daycare as easily as they once used to?” | ||
| Parent 2: “Right after the burn to up to a year after the burn, I could just let go of him and he’d be holding onto my neck and he’d be like my little koala bear that just hung around my neck. He’s definitely attached to me, now he’s getting a little less of that. He needs me at night to lay down with him and he kind of needs to know where I am, what’s going on and he needs that comfort.” | ||
| Functioning | Psychological functioning: externalizing behaviors | Parent 3: “It took him a couple months or more, until probably the injury went away to some ways be back to normal. For a while, there were certainly fights to take care of him on the changing table, to put lotion on him, to put his compression vest on…He was being poked and prodded and didn’t like that all that much.” |
| Parent 1: “It was mostly directly after…there were a lot of behavioral issues...He didn’t want his bandage changed so there was a lot of screaming and him being scared at home- that was for the first couple of weeks after. Then a lot of throwing things, yelling, trying to hit…really wanted his way all the time…He really acted out for a week or so after the fact. And then slowly returned to normal.” | ||
| Functioning | Psychological functioning: dysregulation behaviors | Parent 2: “He was starting to sleep by himself - that no longer happened. He definitely needs mom around more - that safety issue, sleeping with somebody- that kind of thing…even when he does sleep by himself for a couple hours, after 3 or 4 hours, he’ll wake up, walk into my room and say ‘Hey mom, make sure you’re still there, come sleep with me again’- and I’ll lay with him again.” |
| Parent 5: “Oh yes big time [changes in sleep]. She had been sleeping through the night but started waking up several times throughout the night at first a lot. Before the surgery, she was sleeping in her own bed but after the surgery, she started sleeping in our bed with mommy and daddy. We would put her in her bed in her room, and she wakes up, she comes right back in. She was waking up most nights a lot and very early in the morning.” | ||
| Clinician focus group 2: “…we see lack of sleep a ton. What we see goes hand and hand with that is their itch management for sure.” | ||
| Parent 3: “He was in a lot of pain initially afterwards and for a week or two after [the burn injury], he didn’t sleep as well. I think because he was in pain but after that, it hasn’t affected his sleep.” | ||
| Parent 2: “He was 15 months old, so he was on his way to being done breastfeeding - he went back to breastfeeding while we were in the hospital…we went back to definitely a kid that was a baby again. He lost his independence because he was kind of scared at that point.” | ||
| Parent 4: “Once he got on the right medicine, [his] appetite got better…[initially it was] …all over the place.” | ||
| Functioning | Psychological functioning: trauma | Parent 2: “They said he would never remember anything about the pain and the doctors and stuff, yet he has this fear and anxiety when we go to doctor’s offices, even if it’s for his brother’s checkup and being in there has scared him and has taken us a few years to get over that.” |
| Parent 3: “We would get into the [hospital] parking garage and he all of sudden started crying [and] he would just get very anxious. We found out once when we went to see our pediatrician, who obviously has nothing to do with the care of his burn wounds, that he was suspicious of him for a while. Our last visits haven’t seen that at all but for at least half the year or more, he certainly had an association with doctors and nurses and that being people who cause him pain.” | ||
| Clinician focus group 1: “I was just playing in the kitchen area of the [clinic] playroom, and we were going through the foods and he was adding them to the basket. And out of nowhere, there was a hot dog, and he took the hot dog and threw it. There was some aggression there…a little bit later, out of the blue he said, ‘The hot dogs hurt me.’ This is a child who had dipped his feet into a crock-pot of hot water with hot dogs in it.” | ||
| Functioning | Psychological functioning: toileting | Parent 5: “The injury was before toilet training began. [We] had to wait to start toilet training for [her] hand to heal so just timing was delayed…” |
| Parent 2: “We’re still training her. I believe as if she’s a little behind. Some days are better than others.” | ||
| Functioning | Psychological functioning: resilience | Clinician focus group 1: “Resilience of that 1 to 5-year old [age range] is just amazing.” |
| Clinician focus group 1: “Kids want to play, that’s what they want to do. And if they have a contracture on their hand, the kids we see will find a way around it.” | ||
| Parent 1: “He still talks about coming back to Shriners to play foosball. He would just play with his other hand or play with his bandaged hand.” | ||
| Parent 2: “If anything, I think this (burn injury) made him more outgoing. He was more reserved and shy and turned into always needing to be with me. He is very independent now and thinks that he is older than he is.” | ||
| Parent 3: “I think based on the location and that it was very small- he learned to adapt to using his other hand. You wouldn’t even know something was wrong with him. He would crawl around, move around, use his other hand, his left hand. He didn’t really seem to be phased by it.” | ||
| Parent 4: “Even when he had his little minion [yellow sock on hand] on, he was just whatever - ‘I can still play and keep up with everyone.’” | ||
| Parent 5: “She’s so caring and so loving. It’s amazing to see her. She’s 3 now and to see a 3-year old, who at times, is altruistic. When another child is crying, the look of concern on her face.” | ||
| Parent 6: “[There were] no changes in how she expressed her feelings. [You] would not know she’s burned. [She is] far ahead than where other kids are… [She] kept doing what [she] wanted to do regardless of burn…[she had] two mittens on each hand…still tried to play; engagement and interest stayed the same.” | ||
| Functioning | Social functioning | Clinician focus group 2: “I think it affects all the realms…especially social-wise, they’re interacting, they’re having opportunities to interact with others, becoming more aware of the world around them. And if those opportunities are stifled because of the hospitalization or therapies…that will hold back the child.” |
| Parent 1: “If someone asks ‘Oh what is that [sun sleeve], what are you wearing’- he’ll just rip the sleeve off and show them and say ‘I got burned’- he’s pretty open about it and happy to show- ‘I got burned here, and I got burned here, this is what I was doing.’” | ||
| Functioning | Communication and language development | Parent 1: “He actually was stuttering before he got the burn and he completely stopped stuttering after he got burned. Just kind of strange…So those are our…positive outcomes out of it.” |
| Parent 2: “He had a little set back obviously after it just had happen…At 2 years old, his regular pediatrician - he didn’t have much of a vocabulary as they wanted - how many words he could say…By 26 months, he was all caught-up and now he doesn’t shut up.” | ||
| Parent 5: “She was way ahead of other kids for her age [before the burn injury], and she really regressed…She still goes to speech therapy twice a week- certain sounds or words. She was going to a therapist once a week.” | ||
| Family | Family psychological functioning | Parent 2: “One kid’s injury and the whole family has to deal with the effects of that… but it was me mentally and my other son mentally that had to get through it” |
| Parent 2: “We were just very over protective parents. We turned into crazies. I felt like we lived in a bubble so we had to finally ease out of that. We can’t be people who are putting our kids in bubbles. You just kind of transition out of it. You learn that kids are going to get bumps and bruises…we’re not bad parents…it’s not your fault.” | ||
| Parent 3: “I think my wife and I, at the moment, are more scarred from it than he is, emotionally - or the way it impacted our lives.” | ||
| Clinician focus group 1: “If the parent is anxious about the burn, or anxious about the dressing, whatever it may be, you see that a lot in the development of the kid. When they come in after, they still don’t want to use the hand or they’re still only walking on their toes.” | ||
| Clinician focus group 2: “[Children in] this age range in particular read so much [into] how their parents are responding to stressors. If mom and dad act like things are okay, then the child is going to be much more capable at handling the situation. If mom is sitting in the corner crying hysterically, unable to look at the wound, unable to perform any care…they [children] are going to pick up on that.” | ||
| Clinician focus group 2: “The whole family unit...is such a resource for looking at outcomes… If a parent is stuck, I think it is directly related to how the child is going to move forward.” | ||
| Family | Family routine functioning | Parent 3: “We still put lotion on him every day for that scar so right now it’s an inconvenience then during the process- he didn’t like being poked and prodded…bandages and all of that…we’re still pretty religious about making sure we’re putting lotion on the area and making sure he’s not exposed to the sun and putting sun screen on…you can say it’s a little bit of an inconvenience…changing habits...” |
| Parent 4: “When it happened, I think I probably missed two months of work…trying to work around bringing our oldest to school…It was very, very chaotic and if my mom hadn’t been here, I don’t even know how we would have managed. She was so helpful with cooking and cleaning, trying to keep things as normal as possible...” | ||
– indicates there is no subdomain associated with presented quotations.
Symptoms
The symptoms domain is defined as physiological impairments in body functions due to the burn injury, including burn treatments, related to parents’ perceptions of their child’s 1) pain, 2) skin-related discomfort, and 3) fatigue. This domain is represented in the MCH and mirrors the body functions domain in the ICF-CY,4 which describes impairments to or the integrity of physiological functions of body systems.9 Itching was the most commonly identified outcome related to skin-related discomfort. Other symptoms related to skin-related discomfort that were identified included dryness, tightness, numbness, and sensitivities of children’s skin to the sun, air, and extreme temperatures. These symptoms were most commonly discussed by parents and clinician experts, who identified skin-related discomfort and pain as having a significant negative effect on their child’s/patients’ well-being (Table 2).
Functioning
In accordance with the MCH, the functioning domain represents the direct and indirect effects of burn injury (including burn treatment) on a child’s daily life and activities.4 This domain is conceptually similar to the activities and participation domains of the ICF-CY, which are, respectively, defined by a child’s ability to execute a task or action and involvement in life situations.9 Clinicians described the effect of a burn injury on child functioning as manifesting in both negative and positive outcomes (Table 2). Negative functioning outcomes were defined by either developmental regression or developmental delay (ie, health deficits), whereby a child may lose functional abilities he/she had before the burn injury or take longer to achieve age-appropriate developmental milestones, respectively, due to the burn injury. Positive functioning outcomes were defined by the presence of child competency and capacity (ie, health assets) due to the burn injury. This perspective is mirrored in the MCH, which characterizes child health outcomes by both developmental delay and health potential (capacity, competence, and resilience) in various subdomains of health.4
Synthesis of all data sources revealed four subdomains that are important in the assessment of health outcomes among preschool-aged children postburn injury: physical functioning, psychological functioning, social functioning, and communication and language development.
Physical Functioning
The physical functioning subdomain is characterized by children’s observable gross and fine motor functioning. Based on the ICF-CY, gross motor function includes: changing and maintaining body positions (eg, sitting upright, standing, and bending), walking, and moving around (eg, climbing, jumping, skipping, and running); lifting and carrying objects (eg, lifting a cup or carrying a toy); and moving objects with lower extremities (eg, pushing or kicking a ball).9 Fine motor function includes: picking up, grasping, manipulating, and releasing objects using the hands, fingers, and thumb; pulling, pushing, reaching, throwing, catching, and turning/twisting the hands or arms; fine foot (including toe) use; and fine mouth (lips and tongue) use.9 Clinician focus groups and parent interviews revealed the significant impact that a burn injury can have on the physical functioning outcomes of children in this age group, as well as the impact that physical limitations caused by a burn injury may have on other aspects of children’s development, such as play and feeding oneself (Table 2). Clinician experts and parents also described the limitations that burn-related symptoms, such as pain, can cause in children’s physical functioning.
Psychological Functioning
The psychological functioning subdomain includes: internalizing, externalizing, and dysregulation behavior; trauma; toileting; and resilience. The development of this subdomain was largely informed by expert feedback and our literature review, with clinician focus groups and parent interviews validating much of the subdomain’s content. Our conceptualization of the internalizing, externalizing, and dysregulation behavior domains are adapted from the domain frameworks underlying the Brief Infant and Toddler Social Emotional Assessment (BITSEA) and Survey of Well-Being of Young Children (SWYC), which are widely used instruments assessing the social emotional development of young children.13–15
Internalizing Behaviors.
The internalizing behaviors subdomain of our framework is defined by observable symptoms of depression, withdrawal, anxiety, and separation distress.13,14 Within this subdomain, focus group and interview participants most commonly discussed withdrawal and separation distress as observable effects of the burn injury on psychological functioning.
Externalizing Behaviors.
The externalizing behavior subdomain is defined by behaviors of aggression and defiance.13,14 One parent described their children’s externalizing behaviors as isolated incidents occurring as a result of pain and prodding associated with caring for the burn at home (eg, changing bandages and applying lotion/compression garments), whereas another parent described her child’s externalizing behaviors as occurring both within the context of caring for the burn as well as outside this context in daily life activities (Table 2).
Dysregulation Behaviors.
The dysregulation behavior domain is defined by children’s behaviors of negative emotionality (irritability and inflexibility), sleeping problems (eg, trouble falling asleep, staying asleep, and bad dreams), and eating problems (eg, refusing to eat and poor appetite).13–15 Among the outcomes in this domain, sleeping problems were most commonly discussed. Parents noted observable regressions in their children’s ability to sleep independently and through the night following the burn injury (Table 2). Clinicians and parents highlighted the important role of children’s burn symptoms, such as pain and itch, in determining children’s sleep outcomes. Several parents also discussed the impact of a burn injury on their child’s ability to maintain age-appropriate eating function and a good appetite.
Trauma.
The trauma subdomain is defined by children’s observable traumatic stress symptoms that are not represented by other functioning subdomains (eg, withdrawal and anxiety), such as children’s fear or avoidance related to events that remind the child about the burn injury or children’s re-enactment of the burn injury in play. This subdomain is informed by the domains framework underlying the Child Stress Disorders Checklist.16,17 Notably, several parents described how their children’s traumatic stress symptoms were triggered by the health care environment for up to several years following the burn injury (Table 2). A clinician recounted her observations of child trauma expressed during play.
Toileting.
The toileting subdomain is defined in accordance with the WHO ICF-CY as children’s observable abilities to indicate the need for planning and carrying out the elimination of human waste (eg, ability to use the toilet independently).9 Several parents noted their child’s delay in toileting abilities (Table 2). We conceptualize toileting abilities as components of psychological functioning when assessments are focused on the behavioral aspects of these abilities. For example, regression in toileting abilities (not due to physical limitations) may be indicative of child trauma. This conceptualization was present in a number of child developmental assessments included in our literature review. However, when toileting abilities are impacted by physical limitations caused by the burn, we conceptualize toileting abilities as a reflection of children’s gross- and/or fine motor functioning within the physical functioning domain.
Resilience.
Based on the MCH, the resilience subdomain is defined as observable psychological capacities that “add to a child’s ability to deal with and bounce back from adversity,” such as curiosity, imagination, problem-solving abilities, and optimism.4 Clinicians underscored the inherent resiliency of children with burn injuries in this age group (Table 2). Furthermore, every parent shared expressions of their child’s resiliency, which manifested in children continuing to maintain curiosity, social-relatedness, empathy, and interest in play (Table 2). Notably, several parents commented on their child’s ability to adapt physically in their needs for order to continue to satisfy exploration and play.
Social Functioning
The social functioning domain is defined by children’s observable interest and ability to connect with others (family and peers) socially (including through imitation and play); the ability to get along with peers, the ability to make and keep friends; and the ability to participate in ordinary play activities. The conceptualization of this domain was informed by both the MCH and expert clinician feedback.4 Clinician experts and focus group participants felt that frequent hospitalizations or treatment visits can contribute to delays in children’s social functioning by limiting children’s opportunities to participate in routine social interactions (eg, with peers in daycare/preschool) (Table 2).
Parent participants, however, did not feel that the burn injury negatively impacted their child’s social functioning (Table 2). Furthermore, clinicians did not feel that self-consciousness related to children’s perceptions of their own appearance was relevant to this age group.
Communication and Language Development
The communication and language development domain is informed by the ICF-CY and is defined by children’s ability to both receive and produce meaning.9 Receiving meaning includes understanding literal and implied meaning of messages conveyed via spoken language, gestures, symbols, and drawings. Producing meaning includes producing nonverbal messages through gestures or drawings, speaking (including pretalk), and singing. One parent discussed observing an improvement in her child’s language abilities postburn injury, whereas two parents whose child suffered facial burns identified a delay in their child’s language abilities postburn injury (Table 2).
Family
The family domain reflects the indirect negative or positive effects of the child’s burn injury (including burn treatment) on the daily life experiences and activities of the child’s family. The family domain includes two subdomains of outcomes that are relevant to the families of children with burn injuries: 1) family psychological functioning and 2) family routine functioning. The conceptualization of the family domain was largely informed by the BOQ0–5,5 expert clinician feedback, focus groups, and interviews.
Family Psychological Functioning.
The family psychological subdomain is characterized by the effects of the child’s burn injury on parent and family member’s emotional functioning and resilience. Emotional functioning may include experiences with trauma, stress, depression, anxiety, coping, and concerns regarding the child’s appearance. Several parents described their and their family members’ experiences of trauma, anxiety, and guilt in reaction to the burn injury (Table 2). Clinicians noted the central role that parent and family anxiety, stress, coping, and resilience play in determining child recovery outcomes.
Family Routine Functioning.
The family routine functioning subdomain describes the indirect impact of the child’s burn injury (and treatment) on the parents’ and family’s ability to perform ordinary daily life routines (eg, working, running errands, and spending time with friends). Parents highlighted the difficulty of incorporating new burn care regimens, such as applying lotion/sunscreen and changing bandages, into their everyday caregiving routines (Table 2). One parent also shared the difficulty of maintaining regular work and family routines (eg, cleaning, making family dinners, and dropping kids off at school) due to her child’s hospital stays and ongoing outpatient appointments.
DISCUSSION
The assessment of recovery postburn injury among preschool-aged children is critical for ensuring optimal long-term health outcomes but is, nevertheless, marked with challenges due to the rapid developmental nature of children’s health in this age group. In an effort to expand upon the limited assessments and scope of these metrics in the literature, we developed a broad and richly detailed conceptual framework describing health outcomes that are important in the assessment of parent-reported recovery from burn injury among preschool-aged children (1–5 years). Using established models of child health, development, and burn injury to guide our study design and analysis, we conducted an in-depth literature review, clinician focus groups, and parent interviews and garnered ongoing feedback from a diverse group of burn and child development experts.
Our analysis revealed three health outcome domains that are most impacted by preschool-aged children’s burn injury and can be assessed via parent report: symptoms, functioning, and family. Symptoms are defined by observations of children’s pain, itch, and fatigue. Functioning is defined by observations of children’s age-appropriate abilities, capacities, performance, limitations, and/or restrictions in physical (gross and fine motor function), psychological (internalizing behavior, externalizing behavior, dysregulation behavior, trauma, toileting, and resilience), social (connections with family/peers, friendships, and play), and communication/language (receiving and producing meaning) subdomains. The family domain is defined by the psychological and routine functioning of children’s parents and family members. Findings from our focus groups and interviews revealed complex interrelationships among these outcome domains.
Our final conceptual model represents, to the best of our knowledge, one of the more comprehensive syntheses of data available relating to health and developmental outcomes relevant to preschool-aged burn survivors. This work significantly contributes to the literature by broadly synthesizing child health and developmental assessments and taking this synthesis a step further by gleaning new knowledge from parent, clinician, and expert experiences regarding the impact of burn injury on their child/patients. We further synthesize all of this information into a new conceptual framework that is viewed through the lens of the MCH and the ICF-CY and adapted specifically for the assessment of parent-reported health outcomes among preschool-aged burn survivors. Our resulting model can be used by researchers and practitioners to inform the development of family-centered, parent-reported outcome assessments for preschool-aged children with burn injuries. It can also be used to guide the development and evaluation of therapeutic interventions for children and families.
While core elements of our framework were informed by the BOQ0–5,5 the MCH,4 and ICF-CY,9 our framework differs from these models in several ways. First, in alignment with the goal of this study, our conceptual framework expands the breadth of most BOQ0–5 domains. The BOQ0–5 behavior, play, and pain/itch domains were expanded the most and are subsumed by the respective psychological, social, and symptoms domains of this framework. Second, despite the BOQ0–5’s inclusion of an outcome domain relating to parents’ concerns about their child’s appearance (i.e., the BOQ0–5 appearance domain), this outcome did not emerge as a major theme within our study. This may be in part due to the fact that we did not ask parents questions directly on this topic to avoid causing them emotional distress. In clinician focus groups, we only asked about children’s own appearance-related concerns, which they identified as not a major outcome for this age group and, instead, found it to be more relevant developmentally to school-age children. Despite this, we included the parental appearance-related concerns construct within the family domain of this framework, given its inclusion in the BOQ0–5 as an important pediatric burn outcome. Third, we did not include the BOQ0–5’s satisfaction with treatment domain, given our study focus was on identifying health outcomes (and not process of care outcomes) most impacted by child burn injury.
Our model differs from the MCH in that we chose to condense the MCH’s functioning and health potential constructs representing deficits and capacities in functioning, respectively, into a single functioning construct within our framework.4 Finally, whereas the ICF-CY includes a self-care subdomain assessing children’s ability to perform in self-care activities (ie, eating, dressing, toileting, and washing oneself), in its respective functioning (activities) domain, we did not include a dedicated self-care subdomain in the functioning component of our model.9 This is because children’s ability to complete self-care activities (eg, a child’s ability to button a shirt, wash one’s hands, and put on a T-shirt) rely upon children’s gross and fine motor function. As such, we conceptualize self-care activities as indicators of children’s physical functioning and, in the cases of toileting and eating behaviors, also as indicators of children’s psychological functioning. We conceptualize toileting and dysregulated eating behaviors as components of psychological functioning when assessments are focused on the behavioral aspects of these behaviors. For example, the occurrence of toileting accidents (after a child has already learned how to use the toilet) or loss of appetite may be indicative of child trauma. The assessment of toileting and eating as a physical functioning construct would be indicated, however, when investigators are interested in assessing children’s limitations in toileting and eating abilities due to their physical abilities. For instance, assessments of a child’s ability to get on and off the toilet or to lift a spoon to his/her mouth are indicators of a child’s gross and fine motor functioning, respectively.
To the best of our knowledge, three other conceptual models of pediatric burn injury by Tyack et al, Simons et al, and Liber et al have been published.18–20 Our conceptual model adds uniquely to this extant literature in several ways. First, whereas the Tyack et al and Liber et al conceptual models of pediatric burn injury focus predominantly on explicating constructs that predict pediatric burn outcomes, our conceptual framework is the first, to the best of our knowledge, to explicate a domains framework of pediatric burn outcomes specifically for children 1 to 5 years of age. The Simon et al model offers rich descriptions of outcomes relevant to pediatric burn survivors; however, its development was based on a sample of school-aged children of 8 to 15 years, whose outcomes greatly differ from those relevant to preschool-aged children. Finally, despite evidence pointing to the role of parent and family functioning as both a determinant and outcome of pediatric burn injuries, existing models do not highlight the effects of the burn injury on the parent and family as an outcome in itself.21–23 Our study attempts to explicate several important family outcomes impacted by children’s burn injury, while recognizing that this is a complex outcome domain worthy of further research.
The assessment of burn impact on preschool-aged children’s health outcomes may be confounded and modified by several factors. Factors that may be both associated with children’s burn injury and child symptoms or functioning outcomes include both child and environmental factors.18,20 Confounding child factors may include demographics, pre-existing health conditions (including pre-existing developmental delay), and whether the child was born prematurely. Confounding environmental factors may include family demographics (eg, socioeconomic status, family composition and size, and geographic location) and family processes (eg, parenting, learning environment, and parent behavioral health).4 Similarly, parent/family and environmental factors may confound the relationship between the child’s burn injury and family functioning outcomes (parent/family psychological functioning, and routine functioning). Factors that may modify the relationship between the burn injury and child health outcomes are burn severity indicators (eg, percent total body surface area of the burn, burn etiology, length of hospital stay, the number and type of past burn treatments/surgical procedures, contractures, wounds, and scarring), burn location(s), and time elapsed since the burn injury.8,18,20,24 The effect of the burn injury on child health outcomes (including family outcomes previously described) are expected to vary based on these factors. Investigators aiming to assess the impact of burn injury on the health outcomes of preschool-aged children should account for these potential confounding and modifying effects of these factors in their assessments. The use of our conceptual framework in conjunction with existing conceptual models, for example, may offer investigators a helpful framework for parsing out relevant outcome, modifying, and confounding variables.
Continued research to develop calibrated item banks will include factor analyses of the items developed based on our proposed conceptual framework. These factor analyses will provide an opportunity to empirically evaluate the proposed conceptual framework and domains. After factor analyses are completed, we will determine if the proposed conceptual framework is supported by the analyses and adjust the model if needed.
The transferability of our findings may be limited for several reasons. Our findings may be biased due to recall problems among parents, who at times expressed difficulty recalling the effects of the burn injury during interviews. We aimed to mitigate this limitation by asking about the effects of the burn in specific life domains, which assisted with their recall. We also found that parents had difficulty with attributing their child’s functioning outcomes to the burn injury. Some parents, for example, described observed changes in their child’s behavior after the burn injury but expressed uncertainty about whether the change was attributable to the child’s personality or the burn injury. Despite these limitations, these findings suggest that investigators aiming to assess parent-reported burn outcomes among preschool-aged children should consider relatively short recall periods and avoid using items that attribute children’s abilities/limitations in physical, psychological, social, and communication/language domains to the burn injury.
Parents interviewed in this study were primarily male, White, and college educated with a child with small burn (≤15% TBSA). Although this study used data from multiple data sources (including an extensive literature review), findings from our parent interviews may not be transferrable to other preschool-aged populations with burn injuries. For example, parent demographic characteristics may have influenced parent reports of how their child’s burn injury affected his/her health and development. Further research evaluating the validity of this conceptual framework across diverse parent/child samples is warranted.
CONCLUSIONS
Using established models of child health, development, and burn injury,4,5,9 we developed a conceptual framework describing health outcomes that are important in the assessment of parent-reported recovery from burn injury among preschool-aged children (1–5 years). Our framework expands upon the domains framework underlying the BOQ0–5 and other conceptual frameworks in the burn literature through the synthesis and coherency of the model presented here for preschool-aged children. This work is relevant to researchers and practitioners evaluating the effects of burn injury in young children or designing new outcome metrics. Our findings from this study will inform the development of the Preschool Life Impact Burn Recovery Evaluation Profile CAT, a parent-reported outcome measure evaluating recovery from burns among children 1 to 5 years of age. Future research is needed to establish the empirical validity of our framework as it relates to burn outcomes in preschool-aged children.
Supplementary Material
Funding:
This study was funded by Shriners Hospitals for Children (72000BOS-18) and the National Institute on Disability, Independent Living, and Rehabilitation Research (90DPBU0001).
Footnotes
SUPPLEMENTARY DATA
Supplementary data is available at Journal of Burn Care & Research online.
Conflicts of interest: The authors do not have any conflicts of interests to disclose.
REFERENCES
- 1.Dissanaike S, Rahimi M. Epidemiology of burn injuries: highlighting cultural and socio-demographic aspects. Int Rev Psychiatry 2009;21:505–11. [DOI] [PubMed] [Google Scholar]
- 2.American Burn Association. National burn awareness week 2017. fact sheet; available from http://ameriburn.org/wp-content/uploads/2017/04/nbaw-fact-sheet-rev.pdf. Accessed June 28, 2019.
- 3.Sheridan RL, Remensnyder JP, Schnitzer JJ, Schulz JT, Ryan CM, Tompkins RG. Current expectations for survival in pediatric burns. Arch Pediatr Adolesc Med 2000;154:245–9. [DOI] [PubMed] [Google Scholar]
- 4.National Research Council and Institute of Medicine. Children’s health, the nation’s wealth: assessing and improving child health. Washington (DC): The National Academies Press; 2004. doi: 10.17226/10886. [DOI] [Google Scholar]
- 5.Daltroy LH, Liang MH, Phillips CB, et al. American burn association/shriners hospitals for children burn outcomes questionnaire: construction and psychometric properties. J Burn Care Rehabil 2000;21(1 Pt 1):29–39. [DOI] [PubMed] [Google Scholar]
- 6.Kazis LE, Liang MH, Lee A, et al. The development, validation, and testing of a health outcomes burn questionnaire for infants and children 5 years of age and younger: American Burn Association/Shriners Hospitals for Children. J Burn Care Rehabil 2002;23:196–207. [DOI] [PubMed] [Google Scholar]
- 7.Kazis LE, Lee AF, Hinson M, et al. Methods for assessment oh health outcomes in children with burn injury: the multi-center benchmarking study. J Trauma Acute Care Surg 2012;73:S179–88. [DOI] [PubMed] [Google Scholar]
- 8.Kazis LE, Lee AF, Rose M, et al. Recovery curves for pediatric burn survivors: advances in patient-oriented outcomes. JAMA Pediatr 2016;170:534–42. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. International Classification of Functioning, Disability and Health: Children and Youth Version: ICF-CY. Geneva, Switzerland: WHO Press, World Health Organization; 2007. [Google Scholar]
- 10.Babbie ER. The basics of social research. Belmont, CA: Wadsworth Cengage Learning; 2013. [Google Scholar]
- 11.Berg BL. Qualitative research methods for the social sciences. Boston, MA: Allyn and Bacon; 2001. [Google Scholar]
- 12.Denzin NK, Lincoln YS. The Sage handbook of qualitative research. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- 13.Carter AS, Briggs-Gowan MJ, Jones SM, Little TD. The infant-toddler social and emotional assessment (ITSEA): factor structure, reliability, and validity. J Abnorm Child Psychol 2003;31:495–514. [DOI] [PubMed] [Google Scholar]
- 14.Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The brief infant-toddler social and emotional assessment: screening for social-emotional problems and delays in competence. J Pediatr Psychol 2004;29:143–55. [DOI] [PubMed] [Google Scholar]
- 15.Sheldrick RC, Henson BS, Neger EN, Merchant S, Murphy JM, Perrin EC. The baby pediatric symptom checklist: development and initial validation of a new social/emotional screening instrument for very young children. Acad Pediatr 2013;13:72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saxe G, Chawla N, Stoddard F, et al. Child stress disorders checklist: a measure of ASD and PTSD in children. J Am Acad Child Adolesc Psychiatry 2003;42:972–8. [DOI] [PubMed] [Google Scholar]
- 17.Bosquet Enlow M, Kassam-Adams N, Saxe G. The child stress disorders checklist-short form: a four-item scale of traumatic stress symptoms in children. Gen Hosp Psychiatry 2010;32:321–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tyack ZF, Ziviani J. What influences the functional outcome of children at 6 months post-burn? Burns 2003;29:433–44. [DOI] [PubMed] [Google Scholar]
- 19.Liber JM, List D, Van Loey NE, Kef S. Internalizing problem behavior and family environment of children with burns: a Dutch pilot study. Burns 2006;32:165–71. [DOI] [PubMed] [Google Scholar]
- 20.Kassam-Adams N, Bakker A, Marsac ML, Fein JA, Winston FK. Traumatic stress, depression, and recovery: child and parent responses after emergency medical care for unintentional injury. Pediatr Emerg Care 2015;31:737–42. [DOI] [PubMed] [Google Scholar]
- 21.De Young AC, Hendrikz J, Kenardy JA, Cobham VE, Kimble RM. Prospective evaluation of parent distress following pediatric burns and identification of risk factors for young child and parent posttraumatic stress disorder. J Child Adolesc Psychopharmacol 2014;24:9–17. [DOI] [PubMed] [Google Scholar]
- 22.Bakker A, Maertens KJ, Van Son MJ, Van Loey NE. Psychological consequences of pediatric burns from a child and family perspective: a review of the empirical literature. Clin Psychol Rev 2013;33:361–71. [DOI] [PubMed] [Google Scholar]
- 23.Simons M, Ziviani J, Tyack ZF. Measuring functional outcome in paediatric patients with burns: methodological considerations. Burns 2004;30:411–17. [DOI] [PubMed] [Google Scholar]
- 24.Simons M, Price N, Kimble R, Tyack Z. Patient experiences of burn scars in adults and children and development of a health-related quality of life conceptual model: a qualitative study. Burns 2016;42:620–32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.