Abstract
Since March of 2020, billions of people worldwide have been asked to limit their social contacts in an effort to contain the spread of the SARS-CoV-2 virus. However, little research has been carried out to date on the impact of such social distancing measures on the social isolation levels of the population. In this paper, we study the impact of the pandemic on the social isolation of the Spanish population, by means of 32,359 answers to a citizen survey collected over a period of 7 months. We uncover (1) a significant increase in the prevalence of social isolation in the population, reaching almost 26%; (2) gender and age differences, with the largest prevalence of isolation among middle-aged individuals; (3) a strong relationship between economic impact and social isolation; and (4) differences in social isolation, depending on the number of COVID-19 protection measures and on the perception of coronavirus infection risk by our participants. Our research sheds quantitative light on the sociological impact of the pandemic, and enables us to identify key factors in the interplay between the deployment of non-pharmaceutical interventions to contain the spread of an infectious disease and a population’s levels of social isolation.
Subject terms: Public health, Population screening
Introduction
Social isolation is defined as “the relative absence of social relationships”1. It is increasingly recognised as an important public health issue2. In fact, numerous studies have found that social isolation, particularly among older adults, is a risk factor associated with premature death, mainly due to cardiovascular or mental health problems3–6, with an effect similar to that of obesity, a sedentary lifestyle, substance abuse and cigarette smoking7. This negative association with health is found even when controlling for other variables, such as socioeconomic factors, perceived loneliness or life habits7,8. In recent work by Holt-Lunstad and Steptoe9, the authors discuss three elements of social relationships (namely function, structure and quality) and their impact on an individual’s health. While they claim that “none of these three elements alone will adequately capture the full scope of social influence on health”, they hypothesise that social isolation “may be a critical component because a weak structural foundation may limit the potential of other social connection factors to have downstream effects on health”.
For this reason, developing instruments to assess the levels of social isolation in a population is of paramount importance given that social engagement—i.e., the lack of social isolation—is a key pillar for good health. Different instruments have been developed in the literature to quantify the levels of social isolation in individuals, such as the ENRICHD Social Support Instrument, the Berkman-Syme Social Network Index and the Duke Social Support Indices10,11. The Lubben Social Network Scale (LSNS) is one such instrument. The original version of the LSNS scale consists of 10 items and was originally developed by Lubben in 1988 to assess the social isolation in older adults12. Recently, a six-item version of the LSNS, called the LSNS-6, was developed by Lubben and Gironda13–15 and has been validated as a reliable instrument to assess the levels of social isolation both in older13,16–18 and younger adults19.
A related concept to social isolation is that of social capital, which refers to the institutions, relationships and norms that shape the quality and quantity of a society’s social interactions20. Social capital has both an individual and an aggregate component21–23. Generally, social capital consists of three dimensions: structural, relational and cognitive. The LSNS-6 measures the relational and structural elements of the social network of an individual by assessing both the social support and the social network aspects, which are part of a person’s individual social capital24,25.
Older adults have been reported to be the most vulnerable demographic group to social isolation, mainly due to their reduced physical mobility and general decline in health status, life transitions associated with age (e.g. retirement, loss of a partner, relatives and friends) and ageism in society11,26–28. Beyond the elder population, there are few studies that have assessed the prevalence of social isolation in the general population prior to the COVID-19 pandemic29,30.
However, the pandemic has brought social isolation to the public eye, not only in the context of older adults, but for all age groups, because of the impact that confinement and social distancing measures have on everyone’s social support structures31. During the pandemic, billions of people worldwide have been asked to limit their social contacts by physical distancing, home confinements and the temporary closure of many social activities—such as restaurants, bars, gyms, workplaces, soccer stadiums, museums, cinemas and theatres—in an effort to contain the spread of the SARS-CoV-2 virus.
Despite the importance of social isolation in this context, there are few population studies published to date that have analysed the impact of the COVID-19 pandemic on a population’s levels of social isolation32–34. One of the most relevant pieces of previous work is by O’Sullivan et al.35 where they studied the impact of the pandemic on the social isolation of the general population in 101 different countries, mainly from the United States (40%) and the UK (21%). The authors collected the answers to the LSNS-6 survey from 14,302 participants aged over 18 years old (M=53 years, SD=17.6) before and during the coronavirus pandemic. They found a 13% increase in the prevalence of social isolation during the pandemic. The most important factors associated with social isolation—both before and during the coronavirus pandemic—are a lack of financial resources to meet the participants’ needs, their self-rated physical and mental health, living alone not by choice, poor sleep, low physical activity and alcohol consumption. The most cross-cutting aspects correlated with social isolation were economic and mental health factors. During the pandemic, rural residents were found to be significantly at larger risk of social isolation when compared to city dwellers.
In this paper we focus on studying the levels of social isolation in the Spanish population during the COVID-19 pandemic. Spain was one of the most affected countries in the early phases of the pandemic during the spring of 2020. In an effort to contain the spread of the virus, the government implemented an extremely restrictive lockdown that brought the country to a halt for several weeks, with tremendous economic and social implications. Spanish culture is highly social, with low levels of individualism, where families are a fundamental pillar in most people’s lives36–39. People in Spain tend to handle their personal problems through their family, relying on relatives for support when facing difficult situations, such as a pandemic.
In order to measure social isolation, we use the LSNS-6 instrument, delivered as part of an online, anonymous survey called the COVID19ImpactSurvey40, with over 720,000 answers collected since March of 2020. The answers to the survey have been previously analysed for research purposes and extensively used by public authorities, the media and citizens in Spain to measure the impact of the COVID-19 pandemic on people’s behaviours, perceptions and lives41,42. While the original survey did not include any questions to assess the levels of social isolation of the respondents, on June 6th 2021, the LSNS-6 questions were added to the survey. We analyse a sample of 32,359 answers collected in Spain for the time period between June 6th, 2021 and December 16th, 2021.
In our analysis, we aim to answer four research questions on the interplay between the levels of social isolation in the Spanish population, the economic and psychological impact of the COVID-19 pandemic and the self-reported behaviour:
- RQ1:
What is the distribution and the temporal evolution of the levels of social isolation in the Spanish population during six months of the COVID-19 pandemic?
- RQ2:
What is the relationship between social isolation and the economic impact of the pandemic on individuals?
- RQ3:
What is the relationship between social isolation and the psychological impact of the pandemic on individuals?
- RQ4:
Are there differences in the levels of social isolation between those with low perceptions of infection risk associated with common daily activities and those who do not adopt any COVID-19 protective measures when compared to the rest of the sample?
The paper is structured as follows: in the following section, we present the Results of analysing the survey answers to address the four previously stated research questions. Next, we Discuss the results and draw key conclusions from our research. Finally, we describe our “Materials and methods”.
Results
We analyse 32,359 answers to the COVID19ImpactSurvey, which two of the authors designed and launched on March 28th, 2020. Our results are based on analysing a subset of 17 questions of this survey as per Table S3. We focus on the answers collected between June 6th, 2021 and the 16th of December, 2021 in Spain (N = 32,359). Respondents were required to be at least 18 years old. We refer the interested reader to40 for a detailed description of the survey and its methodology.
The gender and age distributions of the collected sample are not proportional to those of the general population of Spain, as shown in Table S5. Thus, we follow the methodology described in Oliver et al.40 and re-weigh the answers, such that the resulting gender and age distributions match the official statistics in Spain in 2020.
All answers are categorical or binary, thus we report the percentage of participants who selected each response and compute the 95% confidence intervals (CI) through the margin of error. All tests of significance have been done by means of t-test or ANOVA as appropriate and post-hoc comparisons have been performed using Tukey tests.
RQ1: distribution and temporal evolution of social isolation
Sample characteristics
Complete LSNS-6 scores were available for 27,898 participants 51.49% were women and 48.51% were men in the re-weighted sample. The mean age of the study sample was 42.45 years. The mean LSNS-6 score of the study population was (). The average LSNS-6 scores were 7.66 () and 17.89 () for socially isolated () and socially integrated () individuals, respectively.
Prevalence of social isolation
The prevalence of social isolation was () across all ages in the sample. Social isolation was slightly more prevalent in men when compared to women (men: , women: ), yet we did not identify a statistically significant difference between genders. Conversely, the LSNS-6 average scores among men were larger than among women (men: , ; women: , ).
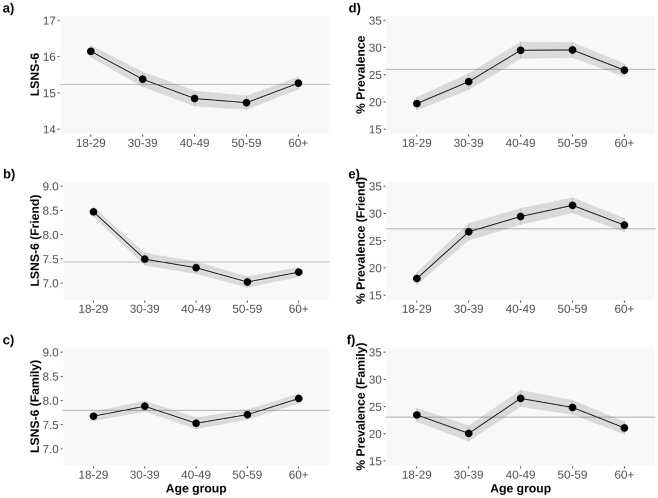
The demographic group with the largest average LSNS-6 scores is the youth (18–29 years old), followed by the elderly (aged 60+ years old) and those aged 30 to 39 years old. Interestingly, the middle-aged (40–59 years old) group exhibits the lowest LSNS-6 values, yielding an “U”-shaped curve of LSNS-6 scores, as shown in Fig. 1a and d. In our data data, 29.54% of the individuals aged 50–59 years old report being socially isolated, a figure significantly larger than what has been previously presented in the literature prior to the pandemic30.
Figure 1.
Average LSNS-6 (a), LSNS-6 Friends (b) and LSNS-6 Family (c) scores per age group. The larger the LSNS-6 score, the lower the levels of social isolation; Proportion of non isolated individuals per age group, defining isolation as a LSNS-6 score (d), a LSNS-6 Friend score (e), and a LSNS-6-Family score (f). The greyed area shows the 95% CI. The grey continuous line corresponds to the overall average LSNS-6 score for all the age groups: , ; , ; , ; , ; ; .
In order to shed light on the contributions of friends vs family relationships in the overall LSNS-6 score, Fig. 1 b, c, e and f show the average LSNS-6 Friend and Family scores and the average prevalence of social isolation per age group. As observed in the Figure, the LSNS-6 scores in the youth (18–29 years old) are strongly reliant on the Friends component whereas the Family component is more important in the elderly (60+ years old): : 7.67 in the youth vs 8.04 in the elderly; : 8.47 in the youth vs 7.22 in the elderly.
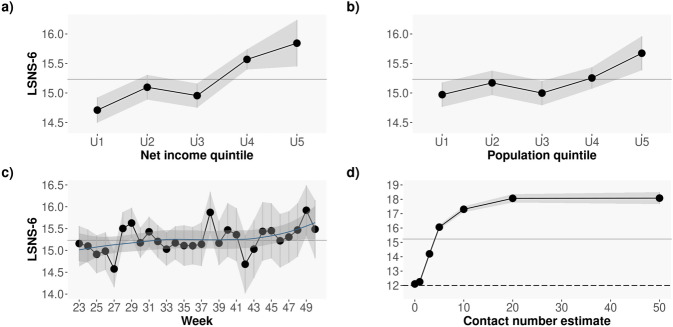
The temporal evolution of the average LSNS-6 scores over time is shown in Fig. 2a. As depicted in the Figure, the average values are generally stable over time except for a notable decrease in the LSNS-6 scores collected during week 27 (5th to 11th of July, 2021) and an increase in the LSNS-6 scores corresponding to week 38 (20th–26th of September, 2021), which might be due to the return to work and school after the summer holidays. A LOESS curve fit reveals a trend of larger average LSNS-6 scores starting in week 43, which might be reflective of the return to the “new normality” and the emergence of pandemic fatigue in the population41.
Figure 2.
Average LSNS-6 score by income (a) and population (b) in thousands, both obtained from the 2020 Spanish official statistics (INE) data according to the participants’ reported postal code. The larger the income and the larger the population, the lower the levels of social isolation; (c) Average LSNS-6 score by week of the year: from June 6th to December 16th, 2021; (d) Average LSNS-6 score by the number of close contacts in the last 7 days. Note how the larger the number of close contacts, the larger the LSNS-6 scores and hence the lower the levels of social isolation. The greyed area shows the 95% CI. The grey continuous line correspond to the overall average LSNS-6 for the entire sample: , .
Associations between social isolation and socio-demographic and economic factors
Previous work has identified significant correlations between social isolation, income and population density5,8. In our data, we observe a similar pattern to that reported in the literature: Fig. 2b and c depict the average LSNS-6 scores for all the participants living in postal codes grouped by their associated income (Fig. 2b) and population (Fig. 2c) as reported by the Spanish National Institute of Statistics (data for 2020). As seen in the Figure, the larger the levels of isolation (i.e. the lower the LSNS-6 score), the lower the income and the lower the population: those living in poorer areas and those living in smaller municipalities exhibit significantly lower LSNS-6 scores than those living in more affluent or/and populated regions.
A logistic regression analysis confirmed associations of age, number of people living in the household, average income and population of the respondents’ zip code with social isolation, as depicted in Table 1. In the Table, the income is divided in three bins: low [12,201–22,064 €/year]; medium [22,065–25,414 €/year]; and high [25,415–60,263 €/year], and so is the population: low [119–44,320 inhabitants]; medium [44,321–312,004 inhabitants]; and high [312,005–5,226,965 inhabitants].
Table 1.
Logistic regression analysis of social isolation with age, gender, number of people in the home, income, population, economic and psychological impact as independent variables. The asterisks denote statistical significance of the coefficient in the logistic model, p-values .
| Odds ratio | Int low | Int sup | |
|---|---|---|---|
| Age Group: Basal value 18–9 | |||
| 30–39 | 1.29 | 1.12 | 1.48 |
| 40–49 | 1.83 | 1.61 | 2.08 |
| 50–59 | 1.89 | 1.67 | 2.14 |
| 60+ | 1.59 | 1.39 | 1.81 |
| Gender: Basal value Female | |||
| Male | 1.07 | 1.00 | 1.16 |
| Number people household: Basal value 1 | |||
| 2 | 0.71 | 0.63 | 0.80 |
| 3 | 0.73 | 0.64 | 0.83 |
| 4+ | 0.65 | 0.57 | 0.74 |
| Income: Basal value Low | |||
| Medium | 1.02 | 0.93 | 1.12 |
| High | 0.77 | 0.68 | 0.86 |
| Population: Basal value Low | |||
| Medium | 0.86 | 0.78 | 0.94 |
| High | 1.00 | 0.90 | 1.11 |
| Economic impact: Basal value None | |||
| Positive | 0.89 | 0.79 | 1.00 |
| Mild | 1.18 | 1.08 | 1.30 |
| Severe | 1.90 | 1.58 | 2.27 |
| Psychological impact: Basal value None | |||
| Mild | 0.84 | 0.74 | 0.95 |
| Severe | 1.39 | 1.27 | 1.51 |
Relationship between the contact number estimate and LSNS-6 scores
Question 9 in the survey (see Table S3) asks participants to estimate the number of different people from outside the home they have had a close contact with in the past week. This question is meant to assess the intensity of social relationships in the survey respondents. Figure 2d shows the relationship between the reported number of close contacts and the LSNS-6 scores of the participants in our sample. As seen in the Figure, the larger the number of close contacts, the higher the LSNS-6 scores, i.e. the lower the probability of social isolation.
RQ2: social isolation and economic impact of the pandemic
We address RQ2 by analysing the answers to questions Q20 and Q22 in the survey (see Tables S3 and S4), as described next.
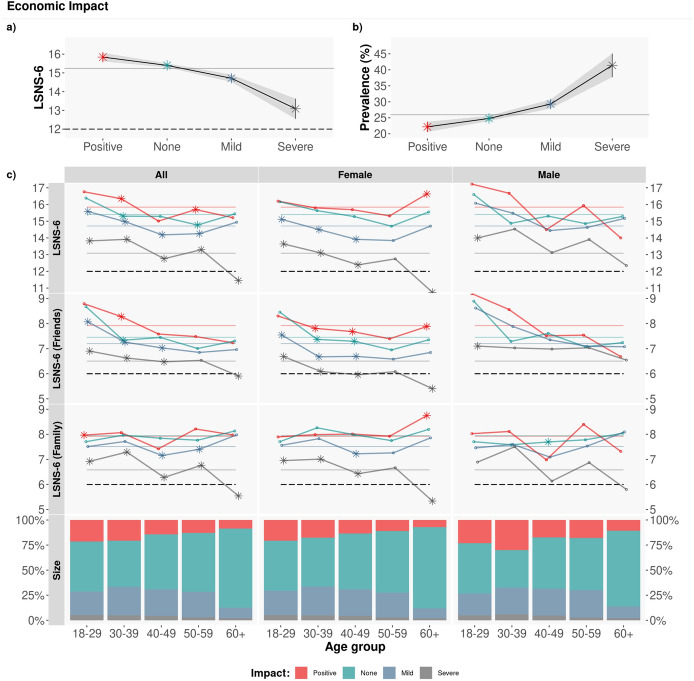
Figure 3 shows the results of the average LSNS-6 scores per age group, gender and severity of the economic impact of the pandemic. As seen in the Figure, those who report severe economic impact have significantly lower LSNS-6 scores when compared to the rest (ANOVA, p , all with post-hoc Tukey p ). Over 40% of participants with severe economic impact report being socially isolated. This difference in the LSNS-6 scores is particularly significant for female respondents when compared to male respondents of the same age with severe economic impact, as illustrated in Fig. 3, bottom. In terms of friends vs family, the LSNS-6 score related to friends is the largest contributor to this very clear gender difference. Regarding age, those aged 60+ with severe economic impact have the lowest LSNS-6 scores of the entire sample: 50.56% of participants in this group report being socially isolated.
Figure 3.
Economic impact. Average LSNS-6 score by age group and gender. The coloured dashed lines correspond to the Overall/Friend/Family average LSNS-6 score per economic impact (Positive/None/Mild/Severe): : [15.84, 15.40,14.71, 13.09]; : [7.92, 7.94, 7.51, 6.58]; : [7.92, 7.45, 7.20, 6.51]. To test the statistical significance of the differences, we applied a Tukey post-hoc test after obtaining a significant difference via an ANOVA test. Asterisks denote statistically significant differences with the rest of groups with . Note how the more severe the economic impact, the lower the LSNS-6 scores and hence the larger the levels of social isolation.
Table 1 shows the results of a logistic regression analysis of social isolation with age, gender, number of people in the home, income, population, economic and psychological impact as independent variables. All levels of psychological and economic impact are positively associated with social isolation: the larger the psychological and/or economic impact, the larger the levels of social isolation.
In addition to the type of economic impact, we analysed the relationship between social isolation and having received any kind of government economic assistance in the past month (Q22 in the survey).
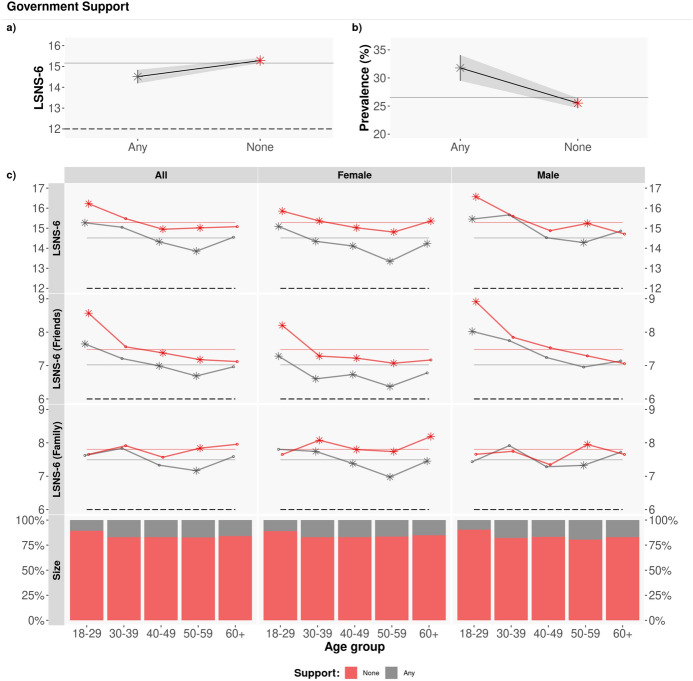
Figure 4 depicts the LSNS-6 scores for those who report receiving government support (red lines) vs those not receiving any type of support by the government (grey lines) per age group and gender. As shown in the Figure, the average LSNS-6 scores of those receiving government support are significantly lower than the scores of those who do not report receiving any kind of support (: 14.50 vs. 15.34 for those receiving government support vs not, t-test with a difference in means of 0.836).
Figure 4.
Government support. Average LSNS-6 score by age group and gender. The coloured dashed lines correspond to the Overall/Friend/Family average LSNS-6 score per government economic assistance (Any/None): : [14.50, 15.34]; : [7.47,7.77]; : [7.03, 7.55]. The asterisks denote statistically significant differences, via a t-test with . The LSNS-6 scores of those receiving government support (gray lines) are significantly lower than the scores of those who do not receive any kind of government support (red lines).
The largest differences are found in the friend component of the LSNS-6 score, particularly in female respondents.
In terms of age, the lowest average LSNS-6 scores correspond to those who receive government support and are 50–59 years old, where 35.35% of individuals in this group report being socially isolated.
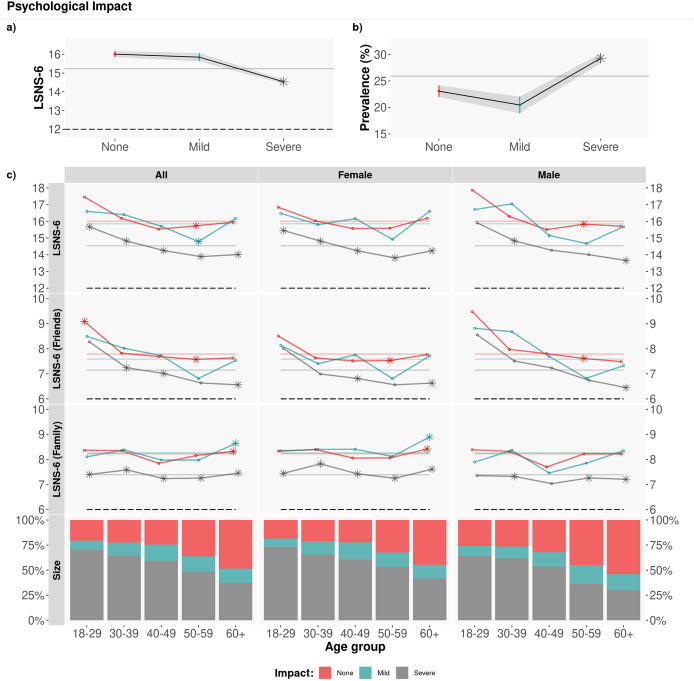
RQ3: social isolation and the psychological impact of the pandemic
We address RQ3 by analysing the answers to question Q31 in the survey (see Tables S3 and S4).
Figure 5 shows the average LSNS-6 scores per age group, gender and severity of the self-reported psychological impact of the pandemic (: None/Mild/Severe: [16.01, 15.85, 14.54]). Similarly to economic impact, those who report severe psychological impact have significantly lower LSNS-6 scores than the rest of the respondents. Interestingly, we do not identify significant differences by gender or by type of social support (friends or family) among those who report severe psychological impact. The lowest average LSNS-6 scores correspond to those aged 50 to 59 years old: 29.54% of respondents in this age group report being socially isolated, and 34.90% for those who report severe psychological impact.
Figure 5.
Psychological impact. Average LSNS-6 score by age group. The coloured dashed lines correspond to the average overall/friend/family LSNS-6 score depending on the psychological impact (None/Mild/Severe): : [16.01, 15.85, 14.54]; : [8.23, 8.26, 7.39]; : [7.79, 7.59, 7.15]. To test the statistical significance of the differences, we applied a Tukey post-hoc test after obtaining a significant difference via an ANOVA test. Asterisks denote statistically significant differences with the rest of groups with . The average LSNS-6 scores of those with severe psychological impact are significantly lower than the rest.
A logistic regression analysis shown in Table 1 confirmed associations between psychological impact and social isolation in our sample, yet milder than the associations found with economic impact.
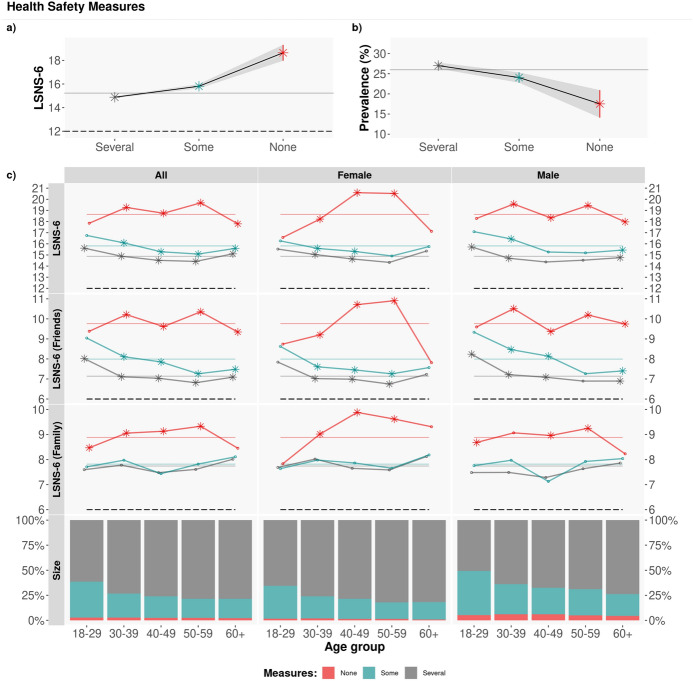
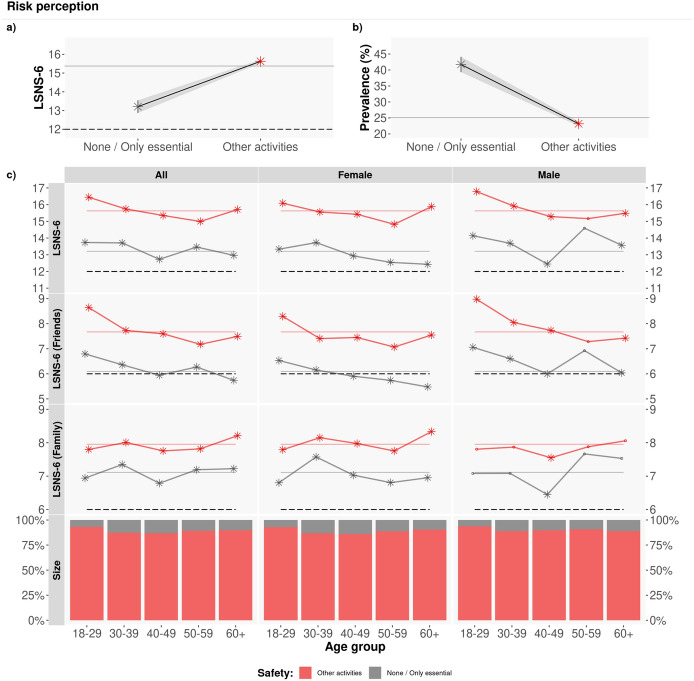
RQ4: social Isolation, Behaviours and Perceptions related to COVID-19 measures
The fourth research question focuses on the relationship between social isolation and the respondents’ behaviours and perceptions regarding the COVID-19 protection measures that they adopt (Q26) and the perceived risk of a coronavirus infection linked to different daily-life activities (Q21). The questions and possible answers are described in Tables S3 and S4.
As noted in Fig. 6, there is a significant difference in the LSNS-6 scores between those who do not adopt any protection measures (red lines) and the rest of participants (blue and grey lines), with a t-test and a difference in means of 3.528. This difference is mainly due to the friends component of the LSNS-6 score: those who do not adopt any COVID-19 protection measures report significantly larger LSNS-6 scores than the rest of respondents, i.e. are significantly less likely to be socially isolated: , with t-test .
Figure 6.
Adopted COVID-19 protection measures. Average LSNS-6 score by age group and gender. The coloured lines correspond to the average Overall/Friend/Family LSNS-6 score per adopted COVID-19 protection measures (Several/Some/None): : [14.88, 15.81, 18.64]; : [7.74, 7.82, 8.88]; : [7.14, 7.99, 9.76]. To test the statistical significance of the differences, we applied a Tukey post-hoc test after obtaining a significant difference via an ANOVA test. Asterisks denote statistically significant differences with the rest of groups with . Those who do not adopt any measures (red lines) have significantly larger LSNS-6 scores than the rest.
Next, we focus on the participants’ perception of COVID-19 infection risk associated with activities that are part of our daily lives (Q21) and their levels of social isolation. As depicted in Fig. 7, the LSNS-6 scores of those who report that none or only essential activities can be carried out with low risk of contracting COVID-19 (grey lines) are significantly lower than the LSNS-6 scores of the rest of respondents (red lines). This difference mainly due to the friends component of the LSNS-6 score: , with t-test p-values .
Figure 7.
Perception of COVID-19 infection risk for different types of activities. Average LSNS-6 score mean by age group and gender. The coloured lines correspond to the average Overall/Friend/Family LSNS-6 score per adopted COVID-19 protection measures (None/Other): : [13.20, 15.63]; : [7.10, 7.95]; : [6.09, 7.68]. The asterisks denote statistically significant differences, with a t-test with . Those who have a lower perception of risk linked to different daily-life activities (red lines) have significantly larger LSNS-6 scores than the rest of respondents (grey lines).
Discussion
In this paper, we have quantitatively analysed the prevalence of social isolation in Spain during 7 months of the COVID-19 pandemic by means of the LSNS-6 instrument delivered via an online survey with 32,359 answers. We have also studied the relationship between social isolation and the economic and psychological impact of the pandemic on people’s lives. Finally, we have reported the relationship between social isolation, the COVID-19 protection measures and the perception of infection risk associated with common daily activities by our participants. We draw several implications from these results.
The levels of social isolation have significantly increased during the pandemic
While we do not have data of the prevalence of social isolation as per the LSNS-6 instrument in our sample before the pandemic, the European Quality of Life Survey published in 201743 reports that 78% of European adults and 83.5% of Spanish adults have face-to-face contact at least once a week with their family and friends. According to this report, 75% of European adults and 80% of Spanish adults have telephone or internet contact with their social network at least once a week.
Beyond Spain, a recent German study analysed social isolation data from a sample of 9392 adults (aged 18–79 years old) collected between August 2011 and November 2014. It reports a prevalence of social isolation in their sample of 12.3%30. The average LSNS-6 score in their sample was 17.6 (). Those socially isolated had a mean LSNS-6 score of 8.5 () and the socially integrated individuals of 18.8 ().
In our sample, we find a prevalence of social isolation of 25.98% (), which is almost 14 percentage points larger than that reported in30. The average LSNS-6 score in our sample is of 15.23. Respondents who are socially isolated have an average LSNS-6 score of 7.66 and those socially integrated of 17.89. These figures are significantly lower than those reported in the literature.
Our findings are aligned with those of O’Sullivan et al.35, who report a prevalence of social isolation of 21% in a study with 14,302 participants from different countries carried out between June and November of 2020. The authors find that 13% of the respondents in their survey experienced a substantial increase in social isolation during the COVID-19 pandemic.
Moreover, we find a statistically significant difference in the prevalence of social isolation among participants who report not adopting any COVID-19 protection measures—and hence do not reduce their social contacts and activities ()—when compared to participants who report complying with five or more COVID-19 protection measures ( = 27.02%, test ).
This result probably reflects the fact that many of the COVID-19 protection measures are of social nature—such as reducing close contacts, keeping social distance, avoiding gatherings, hugging and kissing—and thus their impact on social isolation is evident.
Hence, we hypothesise that the increase in the social isolation identified in our study is due to the pandemic and the social distancing and confinement measures that have been implemented in Spain to try to contain the spread of the SARS-CoV-2 virus.
Middle-aged participants are the most socially isolated
Surprisingly, the largest prevalence of social isolation in our sample is among those aged 50–59 years old, with 29.54% of the sample reporting LSNS-6 levels corresponding to social isolation. The LSNS-6 component related to the friends network is the main contributor to this result. This finding might be a consequence of the social distancing and confinement measures adopted by Spain during the period of study. According to our survey, the demographic group of those aged 50-59 years old is among the most compliant with the individual protection measures (washing hands, keeping social distancing, wearing masks, limiting social contacts) while also being a demographic group with a large number of contacts. Hence, the impact of adopting such measures on their friends social network might have been the largest in the sample.
Previous work has obtained similar results in smaller samples and geographies. In a small sample of 214 residents of Wandsworth, a South West London Borough in the United Kingdom34, the authors find that middle-aged people reported a weaker social network and more loneliness, anxiety and depression than younger people. Sugaya et al. carry out a study with 11,333 participants from seven prefectures of Japan during the final phase of the state of emergency in May 2020 and report a greater prevalence of social isolation among male, middle-aged (40–64 years) participants32.
Interestingly, the U-shaped curve in the LSNS-6 scores that we obtain is similar to the previously reported U-shaped curve of happiness depending on age44 where the lowest levels of happiness are reported by those aged 50 years old.
Given the strong correlation between social isolation and mental and physical health, it would be of paramount importance to deploy support programs for individuals particularly in such an age group.
Economic impact and social isolation are strongly related
Previous work has also found a strong relationship between socioeconomic status and social isolation both before5,8,37,45–48 and during the COVID-19 pandemic30,32,34,49–51. The general finding that we corroborate here is that the lower the socioeconomic status, the higher the risk for social isolation.
The economic consequences of the COVID-19 pandemic are evident on a global scale, having been responsible for the second largest global recession in history, with more than a third of the global population at the time being placed on lockdown.
However, we are not aware of previous analyses on the relationship between the economic impact of the pandemic on an individual and their levels of social isolation. In our data, we find a strong correlation between the economic impact of the pandemic and the LSNS-6 scores of individuals: the lower the economic impact, the larger the LSNS-6 scores and hence the lower the social isolation (see Table 1). The prevalence of social isolation among those who report severe economic impact is significantly larger than the prevalence of the overall sample: and for those with severe economic impact vs the general population, respectively.
We also observe gender differences, mainly due to the friends component of the LSNS-6 scores: women who have been severely impacted economically because of the pandemic are more likely to be socially isolated () than men who also report severe economic impact (), with average friend LSNS-6 scores that are almost one point smaller than the men’s scores (: 6.04 : 6.96).
This finding highlights the importance of deploying social programs to support women in vulnerable and economically precarious situations.
The social support by friends matters
We find that the friends component of the LSNS-6 score is a key determinant of social isolation in our sample across all age groups (see Fig. 1d), more so than the family component. This finding might be due to the fact that families are a fundamental pillar in Spanish culture across all demographic and socioeconomic groups, such that there might not be large differences in the social support provided by families. However, the friends networks vary widely with age, gender, education level and socioeconomic status52.
We identify gender differences in the levels of social isolation for those who report severe economic impact due to a much weaker friends social network among women.
There are also significant differences in the friends LSNS-6 scores among those who do not adopt any COVID-19 protection measures (particularly men) and the rest of participants; and those who consider that most activities can be performed with low risk of a SARS-CoV-2 infection and the rest of respondents. In this case, those who do not adopt any COVID-19 protection measures exhibit stronger social support by their friends. Similarly, those who consider that many non-essential activities can be carried out with a low risk of coronavirus infection also have higher LSNS-6 friend scores than the rest of participants.
This finding highlights not only the role that friends play in social isolation—particularly among the youth (see e.g.53), but also the influence that having a strong network of friends plays on wanting to socialise even during pandemic times. Alternatively, this result might be explained by the fact that the COVID-19 protection measures are mostly of social nature and hence have an impact on the levels of social isolation of those who comply with them.
Gender also matters
There are several gender-based differences that can be drawn from our analyses. First, while the average LSNS-6 scores are lower among female () than male () respondents, the prevalence of social isolation is larger among male () than female () participants. This difference, however, is not statistically significant according to a test.
To shed light on this finding, Fig. S2 depicts the distribution of LSNS-6 scores by gender. As can be observed in the Figure, the LSNS-6 scores by female respondents tend to be clustered around the mean of the distribution whereas the upper and lower extremes of the distribution have significantly more male than female respondents. Indeed, we observe a statistically significant difference between the variances of the distributions with a much larger support of answers by male participants in the tails of the distribution when compared to the answers by female respondents (see Tables S1 and S2).
Second, women with severe economic impact are significantly at higher risk of social isolation than men who have also suffered severe economic impact, mostly due to having a weaker support by their friends. Interestingly, this difference is not evident among those with psychological impact due to the pandemic.
The adoption of COVID-19 protection measures is related with social isolation
When we divide our sample according to the COVID-19 protection measures adopted by the participants in our study, significant differences emerge in the respondents’ levels of social isolation: those who report not adopting any measures have significantly larger LSNS-6 scores than those who adopt some or all of the possible COVID-19 protection measures (None/Some/Several: : [18.65, 15.81, 14.88], ANOVA and Tukey tests .
This finding might be explained by the role that the friends network plays in influencing human behaviour. Many of the COVID-19 protection measures are meant to limit our social interactions. Those with strong friends networks are therefore more impacted by the adoption of such measures and hence could be less likely to adopt them. As previously reported, the difference in the LSNS-6 scores between those who do not adopt any measures and the rest of participants is of 3.524 points, mostly due to the friends component of the LSNS-6 score.
Alternatively, this result might be explained by the fact that the COVID-19 protection measures are mostly of social nature and hence have an impact on the levels of social isolation of those who comply with such measures.
Higher perception of COVID-19 infection risk is related to social isolation
Similarly, those who report that many daily activities can be performed with a low risk of a coronavirus infection are significantly less likely to be socially isolated than those who have a higher perception of infection risk: = 23.13% vs. = 41.73% ( test with ). Again, the LSNS-6 component that contributes the most to this difference in LSNS-6 values (13.20 vs. 15.63) is the friends component: of the 2.44 points in the difference of the average LSNS-6 scores, 1.59 points are due to the friends component and 0.85 points due to the family component, with a t-test , and with a larger difference between female than male respondents.
Our results might be explained by several factors. First, previous work has found that the larger the social support, the lower the fear towards COVID-19 in a sample of healthcare workers in Jordan54. Second, in the context of the coronavirus pandemic, we tend to lower our perception of infection risk when carrying out activities that involve our friends and/or relatives55: “our evaluation of risk versus safety is inextricably tied to our group memberships”.
Several of our findings highlight the crucial role that the friends support network plays in the levels of social isolation in Spain.
Materials and methods
Data collection and processing
In this paper, we analyse a subset of the answers to the COVID19ImpactSurvey, an extensive, anonymous, online citizen survey about COVID-1940. Launched on March, 28th 2020, in Spain, the survey has since then collected over 700,000 anonymous answers from 11 countries (mostly Spain, Italy, Germany and Brazil), and it is available online at https://covid19impactsurvey.org. Participants must declare being 18 years or older to be able to fill the survey. All research was performed in accordance with relevant guidelines/regulations. Informed consent was obtained from all users and the data was collected in de-identified form.
We filter entries with inconsistent answers (5.19% of answers), which are entries where the respondents provided contradictory answers, such as reporting being a pregnant and aged 60+; being pregnant and male, etc. We also do not consider entries that appear to have been answered too fast (< 120 s) or too slow (> 36000 s), which correspond to 3.34% of answers. Note that the average completion time of the survey in our sample is 509 seconds. Finally, entries not providing age or male/female sex information (0.81%) are also excluded from the analysis. In total, we discard 9.34% of the answers.
The specific answers to the survey that we analyse in this paper collect information about the participants’ demographic and household situation (Q1–Q5); their LSNS-6 scores (Q11–Q16); the economic impact of the pandemic in their lives (Q20, Q22); their perception of COVID-19 infection risk associated with different activities (Q21); the individual protection measures that they adopt to protect themselves against COVID-19 infections (Q26); the psychological impact of the pandemic in their households (Q31). All the questions to the survey are included in Table S3.
We analyse the data from Spain for the time period between June 6th, 2021 and the 16th of December, 2021. During this period, Spain had returned to the “new normality”: the only COVID-19 protection measure implemented in the country was the requirement to wear face masks in indoor public spaces. Figure S3 depicts the daily number of new COVID-19 cases and deaths in Spain. The period of study includes a small wave of infections that took place in the summer of 2021. Survey answers were collected from volunteer respondents who learned about the survey via social media channels, word-of-mouth, universities and news organisations. We used Facebook and Instagram ads as an additional channel to recruit volunteers. This approach gave us a straightforward method to obtain a broad sample of users across different socioeconomic and demographic groups. We did not use any targeting feature except for gender, where we used separate budgets to balance the numbers of male and female respondents. The cost-per-successful-response was €0.24 and €0.11 for men and women respectively. Both men and women had similar completion rates (54%) once they began answering the survey.
The age and gender distribution of our sample is different from the population distribution in Spain. Thus, we follow the methodology described in Oliver et al.40 and re-weight the answers such that the resulting gender and age distributions match the official statistics of each of the seven Nielsen geographical regions in Spain, depicted in Fig. S1, plus the metropolitan areas of Madrid and Barcelona. We compute the weights according to the official data reported by the Spanish National Institute of Statistics (INE) for 2020.
To further validate our methodology, in April 2020 we commissioned an IPSOS.digital FastFacts panel of a cohort of 1000 representative general population respondents aged 18–65 in Spain. This validation was done after we started using Facebook ads, but before the time period covered by this paper. The results of the IPSOS panel were within the margin of error of our survey results for the same time period and ages.
Ethical approval
All methods described in this manuscript were carried out in accordance with relevant guidelines and regulations. The survey instrument was approved by the Ethical Committee of the University Miguel Hernandez, which is called the Office for Responsible Research (OIR), in the context of previous research40,41. Informed consent was obtained from all subjects who had to confirm being at least 18 years old to be able to participate in the survey. The participation in the survey was voluntary and all the collected data was anonymous and confidential. Furthermore, the research complied with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Measures
All the measures used in our analysis are described in Tables S3 and S4.
Social isolation
We measure social isolation using the LSNS-6 instrument included in questions Q11–Q16 in the survey. The LSNS-6 is a quantitative measure of an individual’s social network size that assesses both the number and frequency of contacts with friends and family and the social support received by them. It consists of six items: three questions ask about the frequency of meeting relatives, how many relatives the respondent feels close enough to ask for help and with how many relatives the respondent can talk about private matters; the remaining three questions are identical but concerning friends rather than relatives. Each of the LSNS-6 items is scored on a scale from 0 to 5 and they are all equally weighted. Thus, the total score ranges between 0 and 30. The higher the LSNS-6 scores, the lower the levels of social isolation. Social isolation is given by a score below 12. This corresponds to having less than 2 individuals to reach out to in each of the areas probed by the survey (i.e. family or friends). The LSNS-6 has good psychometric properties13.
Socio-demographic and household characteristics
Demographic variables selected for analysis were: (1) gender, where respondents were asked to self-report their gender as male, female or other. In this study, we only consider the answers of those who responded as male or female, which represent 99.33% of the answers (0.3% of answers selected “other” as their sex and 0.37% of answers did not provide sex information); (2) age, coded in the following bins: 18–29; 30–39; 40–49; 50–59; 60+; (3) zip code of their residence; and (4) number of members in the household, coded as: 1, 2, 3, 4+.
Economic impact
The self-reported economic impact of the pandemic was assessed in Q20 and Q22 of the survey.
Question number 20 asks about the type of economic impact that the pandemic had on the respondents’ lives. Based on the answers provided to Q20, we coded the severity of the economic impact in four levels: [None, Mild, Severe and Positive], as described in Table S3.
Question number 22 focuses on whether participants receive any kind of economic assistance from the government.
Based on the answers provided to Q22, we coded the reliance on government-based economic assistance in two levels: [None, Any], as described in Table S3.
Psychological impact
The self-reported psychological impact of the pandemic was assessed in Q31 of the survey.
Based on the answers provided to Q31, we code the severity of the psychological impact in three levels: [None, Mild and Severe], as described in Table S3.
COVID-19 protection measures
The individual protection measures adopted by participants to limit their exposure to the SARS-CoV-2 virus were captured by Q26.
We code the possible answers into three groups: [All, Some, None], depending on whether respondents report adopting all, none or several of the measures, as described in Table S3.
Perception of COVID-19 infection risk
Question 21 asked participants about their perception of risk of a COVID-19 infection associated with different daily-life activities.
We code the possible answers into three groups: [None, Only essential activities and Other non-essential activities], as depicted in Table S3.
Statistical analysis
The prevalence of social isolation is computed in percent with 95% confidence intervals (CIs) from the overall sample. We stratify social isolation by gender and age. We perform tests to determine the existence of statistically significant differences in the prevalence of social isolation among each of the stratified groups. We also use multi-variable logistic regression analysis to test the associations between social isolation and age, gender, number of members of the household, economic and psychological impact of the pandemic, individual COVID-19 protection measures adopted and risk perceptions of coronavirus infection associated with different daily activities. We use a significance level (two-tailed) in all the analyses.
All statistical analyses, data preprocessing and figures were performed and plotted using the R software56 package, version 4.1.2 (2021-11-01).
Limitations
Collecting a large sample of answers via an online survey does not come without limitations. Even if the data size is large and the confidence intervals are small, errors might compound and under- or over-estimate the results57. Moreover, even if we weighted59 the data to mitigate gender and age survey’s biases in each Nielsen region, and we deployed gender-balanced Facebook advertisement campaigns, the data is non-random and biases might still be present. For example, there are self-selection and sampling biases59 as the survey is filled out by volunteers who have learned about the survey via social media, WhatsApp, newspapers’ articles or Facebook ads, and who need to have access to a computing device (smartphone, tablet, PC) with an Internet connection. The survey might also be biased towards people who are more likely to fill-in surveys, such as young and highly educated people. Respondents must be adults—at least 18 years old. Hence, students are only partially covered. We acknowledge all these biases challenge the estimation of inferential statistics, and might lead to overconfidence in incorrect inferences due to the collected large data sample and small confidence intervals57. We also acknowledge that there might be a recall bias as respondents were asked about their perceptions and behaviour in the last seven days (e.g. the number of close contacts in the last week). However, we have taken several measures (re-weighting, contrasting with two polls, comparing with relevant literature) to minimise such biases. Previous work has found that citizen (online) surveys are particularly valuable tools in situations of data scarcity where informed and timely decisions are needed40. Online surveys also allow monitoring people’s perceptions and behaviours, enabling the design of more effective public policies and better education and communication with the public. Thus, we are confident about the value and validity of the results of our analyses.
Supplementary Information
Acknowledgements
This work is partially supported by grants FONDOS SUPERA COVID-19 Santander-CRUE, 2020–2021, Fundación BBVA a equipos de investigación científica SARS-CoV-2 COVID-19, IA4COVID19 2020-2022 and by funding received at the ELLIS Unit Alicante Foundation from the Regional Government of Valencia in Spain (Generalitat Valenciana, Conselleria d’Innovació, Universitats, Ciència i Societat Digital, Dirección General para el Avance de la Sociedad Digital) .
Author contributions
M.M.-G. Defined the methods, conducted the statistical analyses and analysed the results. E.S.-S. Defined the methods, conducted the statistical analyses and analysed the results. R.F Helped with the official statistics data. A.C.H. Performed the literature review. K.R. Designed, deployed and conceived the study. N.O. Designed, deployed and conceived the study, defined the methods, analysed the results Wrote the manuscript, which was reviewed by all authors.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Code availability
The code used to analyse the data will be placed in a publicly available Github server.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Marina Martínez-Garcia, Emilio Sansano-Sansano, Kristof Roomp and Nuria Oliver.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-16628-y.
References
- 1.Smith KP, Christakis NA. Social networks and health. Annu. Rev. Sociol. 2008;34:405–429. doi: 10.1146/annurev.soc.34.040507.134601. [DOI] [Google Scholar]
- 2.WHO. Social isolation and loneliness among older people: Advocacy brief. World Health Organization (2021).
- 3.Leigh-Hunt N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 4.Smith KJ, Victor C. Typologies of loneliness, living alone and social isolation, and their associations with physical and mental health. Ageing Soc. 2019;39:1709–1730. doi: 10.1017/S0144686X18000132. [DOI] [Google Scholar]
- 5.Ge L, Yap CW, Ong R, Heng BH. Social isolation, loneliness and their relationships with depressive symptoms: A population-based study. PLoS ONE. 2017;12:e0182145. doi: 10.1371/journal.pone.0182145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shankar A, Hamer M, McMunn A, Steptoe A. Social isolation and loneliness: Relationships with cognitive function during 4 years of follow-up in the english longitudinal study of ageing. Psychosom. Med. 2013;75:161–170. doi: 10.1097/PSY.0b013e31827f09cd. [DOI] [PubMed] [Google Scholar]
- 7.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 8.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holt-Lunstad J, Steptoe A. Social isolation: An underappreciated determinant of physical health. Curr. Opin. Psychol. 2021 doi: 10.1016/j.copsyc.2021.07.012. [DOI] [PubMed] [Google Scholar]
- 10.Valtorta NK, Kanaan M, Gilbody S, Hanratty B. Loneliness, social isolation and social relationships: What are we measuring? A novel framework for classifying and comparing tools. BMJ Open. 2016;6:e010799. doi: 10.1136/bmjopen-2015-010799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Academies of Sciences, Engineering, and Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System (National Academies Press, 2020). [PubMed]
- 12.Lubben JE. Assessing social networks among elderly populations. Fam. Community Health. 1988;11:42–52. doi: 10.1097/00003727-198811000-00008. [DOI] [Google Scholar]
- 13.Lubben J, et al. Performance of an abbreviated version of the Lubben social network scale among three European community-dwelling older adult populations. Gerontologist. 2006;46:503–513. doi: 10.1093/geront/46.4.503. [DOI] [PubMed] [Google Scholar]
- 14.Lubben, J. & Gironda, M. Centrality of social ties to the health and well-being of older adults. Soc. Work Health Care Aging World 319–350 (2003).
- 15.Lubben, J. & Gironda, M. Social support networks. Comprehens. Geriatr. Assess. 121–137 (2000).
- 16.Jang Y, et al. Performance of an abbreviated Lubben social network scale (LSNS-6) in three ethnic groups of older Asian Americans. Gerontologist. 2020 doi: 10.1093/geront/gnaa156. [DOI] [PubMed] [Google Scholar]
- 17.Vilar-Compte M, Vargas-Bustamante A, Lubben J. Validation study of the abbreviated version of the Lubben social network scale Spanish translation among Mexican and Mexican-American older adults. J. Cross Cult. Gerontol. 2018;33:83–99. doi: 10.1007/s10823-017-9341-5. [DOI] [PubMed] [Google Scholar]
- 18.Kurimoto A, et al. Reliability and validity of the Japanese version of the abbreviated Lubben social network scale. Nihon Ronen Igakkai Zasshi. Jpn. J. Geriatr. 2011;48:149–157. doi: 10.3143/geriatrics.48.149. [DOI] [PubMed] [Google Scholar]
- 19.Villas-Boas S, Oliveira A, Ramos N, Montero-García I. Social support and generational diversity: The potential of the LSNS-6. Pedag. Soc. Rev. interuniv. 2018 doi: 10.7179/PSRI_2018.31.14. [DOI] [Google Scholar]
- 20.Coleman J. Social capital in the creation of human capital. Am. J. Sociol. 1988 doi: 10.1086/228943. [DOI] [Google Scholar]
- 21.Buys, E. & Bow, V. The impact of privacy on social capital 1–16 (Queensland University of Technology, Centre for Social Change Research, 2002).
- 22.Newton K. Social capital and democracy. Am. Behav. Sci. 1997;40:575–586. doi: 10.1177/0002764297040005004. [DOI] [Google Scholar]
- 23.Slangen LH, van Kooten GC, Suchánek P. Institutions, social capital and agricultural change in central and eastern Europe. J. Rural. Stud. 2004;20:245–256. doi: 10.1016/j.jrurstud.2003.08.005. [DOI] [Google Scholar]
- 24.Scrivens K, Smith C. Four interpretations of social capital: An agenda for measurement. OECD. 2013 doi: 10.1787/18152031. [DOI] [Google Scholar]
- 25.Siegler, V. Measuring social capital in the UK. Office for National Statistics (2014).
- 26.Nicholson NR. A review of social isolation: An important but underassessed condition in older adults. J. Prim. Prevent. 2012;33:137–152. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 27.Kaye LW, Singer C. Social Isolation of Older Adults: Strategies to Bolster Health and Well-Being. New York: Springer Publishing Company; 2018. [Google Scholar]
- 28.Cotterell N, Buffel T, Phillipson C. Preventing social isolation in older people. Maturitas. 2018;113:80–84. doi: 10.1016/j.maturitas.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 29.Hämmig O. Health risks associated with social isolation in general and in young, middle and old age. PLoS ONE. 2019;14:e0219663. doi: 10.1371/journal.pone.0219663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Röhr S, et al. Social factors and the prevalence of social isolation in a population-based adult cohort. Soc. Psychiatry Psychiatr. Epidemiol. 2021 doi: 10.1007/s00127-021-02174-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holt-Lunstad J. A pandemic of social isolation? World Psychiatry. 2021;20:55–56. doi: 10.1002/wps.20839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sugaya N, Yamamoto T, Suzuki N, Uchiumi C. Social isolation and its psychosocial factors in mild lockdown for the COVID-19 pandemic: A cross-sectional survey of the japanese population. BMJ Open. 2021;11:e048380. doi: 10.1136/bmjopen-2020-048380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Padala K, et al. Relationship between social determinants of health and loneliness during COVID-19 pandemic. Innov. Aging. 2021;5:736. doi: 10.1093/geroni/igab046.2719. [DOI] [Google Scholar]
- 34.Jaspal R, Breakwell GM. Socio-economic inequalities in social network, loneliness and mental health during the COVID-19 pandemic. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020976694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Sullivan R, et al. Impact of the COVID-19 pandemic on loneliness and social isolation: A multi-country study. Int. J. Environ. Res. Public Health. 2021 doi: 10.3390/ijerph18199982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Green EG, Deschamps J-C, Paez D. Variation of individualism and collectivism within and between 20 countries: A typological analysis. J. Cross Cult. Psychol. 2005;36:321–339. doi: 10.1177/0022022104273654. [DOI] [Google Scholar]
- 37.Böhnke P. Are the poor socially integrated? The link between poverty and social support in different welfare regimes. J. Eur. Soc. Policy. 2008;18:133–150. doi: 10.1177/0958928707087590. [DOI] [Google Scholar]
- 38.Hofstede G, Hofstede GJ, Minkov M. Cultures and Organizations: Software of the Mind. New York: Mcgraw-Hill; 2005. [Google Scholar]
- 39.Gouveia VV, Clemente M, Espinosa P. The horizontal and vertical attributes of individualism and collectivism in a Spanish population. J. Soc. Psychol. 2003;143:43–63. doi: 10.1080/00224540309598430. [DOI] [PubMed] [Google Scholar]
- 40.Oliver N, Barber X, Roomp K, Roomp K. Assessing the impact of the COVID-19 pandemic in Spain: Large-scale, online, self-reported population survey. J. Med. Internet Res. 2020;22:e21319. doi: 10.2196/21319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martinez-Garcia M, et al. Key factors affecting people’s unwillingness to be confined during the COVID-19 pandemic in Spain: A large-scale population study. Nat. Sci. Rep. 2021 doi: 10.1038/s41598-021-97645-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.De Nadai M, Roomp K, Lepri B, Oliver N. The impact of control and mitigation strategies during the second wave of coronavirus infections in Spain and Italy. Nat. Sci. Rep. 2021 doi: 10.1101/2021.05.11.21256876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eurofound. European quality of life survey 2016: Quality of life, quality of public services, and quality of society 10.5255/UKDA-SN-7348-3 (2017).
- 44.Blanchflower D. Is happiness u-shaped everywhere? Age and subjective well-being in 145 countries. J. Popul. Econ. 2021;34:575–624. doi: 10.1007/s00148-020-00797-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jang Y, et al. Social isolation in Asian Americans: Risks associated with socio-demographic, health, and immigration factors. Ethnicity Health. 2021 doi: 10.1080/13557858.2021.1881765. [DOI] [PubMed] [Google Scholar]
- 46.Mood C, Jonsson JO. The social consequences of poverty: An empirical test on longitudinal data. Soc. Indic. Res. 2016;127:633–652. doi: 10.1007/s11205-015-0983-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Böhnke P, Link S. Poverty and the dynamics of social networks: An analysis of German panel data. Eur. Sociol. Rev. 2017;33:615–632. doi: 10.1093/esr/jcx063. [DOI] [Google Scholar]
- 48.Eckhard J. Does poverty increase the risk of social isolation? Insights based on panel data from Germany. Sociol. Q. 2018;59:338–359. doi: 10.1080/00380253.2018.1436943. [DOI] [Google Scholar]
- 49.Menec VH, Newall NE, Mackenzie CS, Shooshtari S, Nowicki S. Examining individual and geographic factors associated with social isolation and loneliness using Canadian longitudinal study on aging (CLSA) data. PLoS ONE. 2019;14:e0211143. doi: 10.1371/journal.pone.0211143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yamada K, Wakaizumi K, Kubota Y, Murayama H, Tabuchi T. Loneliness, social isolation, and pain following the COVID-19 outbreak: Data from a nationwide internet survey in Japan. Nat. Sci. Rep. 2021 doi: 10.1038/s41598-021-97136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.O’sullivan R, et al. Impact of the COVID-19 pandemic on loneliness and social isolation: A multi-country study. Int. J. Environ. Res. Public Health. 2021;18:9982. doi: 10.3390/ijerph18199982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Groenou MIB, Van Tilburg T. Network size and support in old age: Differentials by socio-economic status in childhood and adulthood. Ageing Soc. 2003;23:625–645. doi: 10.1017/S0144686X0300134X. [DOI] [Google Scholar]
- 53.Bruine de Bruin W, Parker AM, Strough J. Age differences in reported social networks and well-being. Psychol. Aging. 2020;35:159. doi: 10.1037/pag0000415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alnazly E, Khraisat O, Al-Bashaireh A, Bryant C. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS ONE. 2021;16:e0247679. doi: 10.1371/journal.pone.0247679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cruwys T, Stevens M, Greenaway KH. A social identity perspective on COVID-19: Health risk is affected by shared group membership. Br. J. Soc. Psychol. 2020;59:584–593. doi: 10.1111/bjso.12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria (2021).
- 57.Bradley, V. C. et al. Unrepresentative big surveys significantly overestimated us vaccine uptake. Nature 1–6 (2021). [DOI] [PMC free article] [PubMed]
- 58.Wiegand, H. & Kish, L. Survey Sampling (John Wiley and Sons Inc, New York, London, 1965). IX + 643 S., 31 Abb., 56 Tab., Preis 83 s., vol. 10 (Wiley, 1968).
- 59.Eysenbach G, Wyatt J. Using the internet for surveys and health research. J. Med. Internet Res. 2002;4:e13. doi: 10.2196/jmir.4.2.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].
The code used to analyse the data will be placed in a publicly available Github server.