Abstract
Background and purpose
Erenumab (ERE) is the first anticalcitonin gene‐related peptide receptor monoclonal antibody approved for migraine prevention. A proportion of patients do not adequately respond to ERE.
Methods
Prospective multicenter study involving 110 migraine patients starting ERE 70 mg monthly. Baseline socio‐demographics and migraine characteristics, including mean monthly migraine days (MMDs), migraine‐related burden (MIDAS [Migraine Disability Assessment scale] and Headache Impact Test‐6), and use of abortive medications, during 3 months before and after ERE start were collected. Real‐time polymerase chain reaction was used to determine polymorphic variants of calcitonin receptor‐like receptor and receptor activity‐modifying protein‐1 genes. Logistic regression models were used to identify independent predictors for 50% responder patients (50‐RESP) and 75% responder patients (75‐RESP).
Results
At month 3, MMDs decreased from 17.2 to 9.2 (p < 0.0001), 59/110 (53.6%) patients were 50‐RESP, and 30/110 (27.3%) were 75‐RESP. Age at migraine onset (odds ratio [OR] [95% confidence interval (95% CI)]: 1.062 [1.008–1.120], p = 0.024), number of failed preventive medications (0.753 [0.600–0.946], p = 0.015), and MIDAS score (1.011 [1.002–1.020], p = 0.017) were associated with 75‐RESP. Among the genetic variants investigated, RAMP1 rs7590387 was found associated with a lower probability of being 75‐RESP (per G allele OR [95% CI]: 0.53 [0.29–0.99], p = 0.048]), but this association did not survive adjustment for confounding clinical variables (per G allele, 0.55 [0.28–1.10], p = 0.09]).
Conclusions
In this real‐word study, treatment with ERE significantly reduced MMDs. The number of failed preventive medications, migraine burden, and age at migraine onset predicted response to ERE. Larger studies are required to confirm a possible role of RAMP1 rs7590387 as genetic predictor of ERE efficacy.
Keywords: anti‐CGRP antibodies, erenumab, predictors, treatment response
Clinical predictors of a 75% or higher reduction in monthly migraine days during 3‐month erenumab treatment were older age at migraine onset, lower number of failed preventive medications, and higher migraine burden as measured by the Migraine Disability Assessment score questionnaire. At multivariate analysis, no single nucleotide polymorphisms (SNPs) at calcitonin receptor like receptor (CALCRL) and RAMP1 were found to be an independent predictor of treatment response, despite a modest effect of SNPs cannot be ruled out due to the limited sample size of our study.
INTRODUCTION
Patients with disabling and or frequent migraine attacks qualify for preventive therapy [1]. Until recently, preventive therapies included nonspecific medications such as β‐blockers, calcium channel antagonists, antidepressants, and antiepileptic drugs. These compounds are limited by insufficient efficacy and/or relevant side effects [2].
In recent years, calcitonin gene‐related peptide (CGRP) activity has been shown to be crucial in migraine pathogenesis [3, 4, 5, 6]. Accordingly, targeted therapies such as monoclonal antibodies (mAbs) binding to CGRP receptor or ligand have gained importance as new migraine preventive treatments, showing favorable benefit/risk profile [2].
Erenumab (ERE) was the first anti‐CGRP receptor mAb approved in Switzerland. In registration clinical trials, ERE 70 mg or 140 mg subcutaneously versus placebo monthly for 3–6 months, significantly reduced the mean number of monthly migraine days (MMDs), the use of acute migraine‐specific medications, and decreased the impact of migraine on everyday activities in episodic as well as chronic migraine, including in patients with multiple preventive treatment failures. ERE was generally well tolerated, with constipation and local skin reactions being the most common treatment‐emergent adverse events [7, 8, 9, 10].
In clinical trials, approximately 50% of patients did not achieve the end point of a reduction in MMDs of at least 50% [7, 8, 9, 10]. Considering its substantial costs, favoring the use of ERE in responder patients represents a priority for a tailored therapeutic approach and health resources optimization. However, data on clinical predictors of response to ERE in a real‐word setting are scarce [11].
Besides clinical characteristics, one key parameter determining the efficacy of ERE might be the genetic profile of the mAb target (i.e., the CGRP receptor). ERE has high affinity binding to the CGRP receptor, a heterodimeric complex of the calcitonin receptor like receptor encoded by the CALCRL gene, and the receptor activity modifying protein 1 (RAMP1), which has a key role in postendocytic receptor trafficking [12]. Despite it being widely accepted that interindividual variability of drug responses is explained, at least in part, by genetic factors [13], no studies so far have investigated genetic factors potentially affecting ERE efficacy.
In this study, we aimed at characterizing clinical and genetic predictors of a favorable response to ERE in a population of migraine patients treated at tertiary headache centers in Switzerland.
METHODS
This was a multicenter, observational prospective study including consecutive migraine patients started with ERE at participating Swiss tertiary headache centers (Neurology Department, Ospedale Regionale di Lugano; Neurology Department, Inselspital Bern) between December 2019 and September 2020. The study conforms with the World Medical Association Declaration of Helsinki and was approved by the local ethics committees (referral ethics committee: Comitato Etico canton Ticino, ref. CE 3507). Written informed consent was obtained from all participants.
Patients were aged between 18 and 70 years and suffered from migraine according to the International Classification of Headache Disorders [14] for at least 1 year. According to Swiss reimbursement criteria for ERE, patients had to provide a prospectively collected diary showing at least 8 days with migraine per month for at least 3 months, with failure of at least two or intolerability/contraindication for all three classes of migraine preventive therapies of the group’s anticonvulsants, β‐blockers, or calcium channel antagonists.
Main exclusion criteria were migraine onset over 50 years of age, a history of hemiplegic migraine, of other primary headache disorders other than migraine, having received botulin toxin injections within 4 months before inclusion, having started/changed the dose of one migraine‐preventive medication within 2 months before inclusion, or having had a head or neck trauma within the past 6 months. Patients with incomplete follow‐up were also excluded.
Patients underwent a baseline evaluation the day they received the first ERE 70 mg injection, and a follow‐up evaluation 3 months thereafter according to routine clinical practice. During the entire study participation, patients continued to fill in a headache diary.
At baseline, socio‐demographic characteristics and migraine history were collected, including sex, age, body mass index, working status, lifestyle habits (alcohol, smoking, physical activity, sleep habits); age at migraine onset, migraine type, presence of aura; number of failed preventive medications; number of first‐degree relatives affected by migraine; lifetime presence and type of comorbidities (anxiety disorder and/or depression; chronic pain; arterial hypertension; insomnia/snoring; other comorbidities); and concomitant medications. At this time point, a blood sample was also collected for genetic analysis.
The number of MMDs, the monthly number of days with triptan/nonsteroidal analgesics use during the 3 months before and after ERE start, was retrieved from the patient's headache diary. Presence of medication overuse was assessed according to the definition reported in the International Classification of Headache Disorders [14]. Additionally, average pain intensity rated on a numerical rating scale ranging from 1 (no pain) to 10 (maximum unbearable pain) and average attack duration (hours) were also collected at baseline and 3 months after ERE start.
To investigate migraine‐related disability and its impact on daily life, at baseline and 3‐month evaluations, patients filled out two validated questionnaires, the Migraine Disability Assessment (MIDAS) scale [15] (score 1–5: little or no disability, 6–10: mild disability, 11–20: moderate disability, >21: severe disability) and the Headache Impact Test (HIT‐6) [16] (score ≤49: little or no impact, 50–55: some impact, 56–59: substantial impact).
Additionally, adverse events reported by the patients at any time during the study and asked by the treating neurologists at 3‐month evaluations were collected and stratified according to severity (mild, moderate, severe) and seriousness (if requiring/prolonging hospitalization or causing permanent disability or death).
Patients were classified as responders to ERE according to two definitions commonly adopted in clinical trials [7, 8, 9, 10]; 50% responders (50‐RESP) were those patients showing a reduction of ≥50% in MMDs at month 3 of ERE treatment compared to the 3 months before ERE start (baseline MMDs), whereas 75% responders (75‐RESP) were those showing a respective reduction of MMDs of ≥75%.
We hypothesized that clinical and genetic profiles of 50‐RESP and 75‐RESP differ from those of nonresponder patients.
The primary study objective was to investigate associations between patients’ demographic and clinical characteristics and 50‐RESP status. Secondary study objectives were to investigate association between patients’ demographic and clinical characteristics and 75‐RESP status, and between selected (see Genotyping section) polymorphisms at CALCRL and RAMP1 genes and 50‐RESP as well as 75‐RESP status.
Genotyping
Genomic DNA was extracted from peripheral blood samples using the QiaAmp DNA Mini Kit (Qiagen) or the Wizard genomic DNA purification kit (Promega) according to the manufacturers’ instructions. A total of 15 common single nucleotide polymorphisms (SNPs) of CALCRL and RAMP1 genes were selected from Variation Viewer (https://www.ncbi.nlm.nih.gov/variation/view) based on minor allele frequency (MAF) of more than 10%. Genotyping of CALCRL and RAMP1 polymorphisms was performed by real‐time polymerase chain reaction (PCR) using Applied Biosystems TaqMan Pre‐Designed SNP Genotyping assays (CALCRL rs696574 Assay ID: C_8726655_10; CALCRL rs6710852 Assay ID: C_189160430_10, CALCRL rs3213738 Assay ID: C_27470324_10; RAMP1 rs302680 Assay ID: C_1071215_20; RAMP1 rs13386048 Assay ID: C_31241845_10; RAMP1 rs12995100 Assay ID: C_31241852_10; RAMP1 rs12465864 Assay ID: C_11739774_10; RAMP1 rs7590387 Assay ID: C_26481962_10; RAMP1 rs75822777 Assay ID: C_101309358_10; RAMP1 rs302676 Assay ID: C_1071223_30; RAMP1 rs11673847 Assay ID: C_176017176_10; RAMP1 rs6431564 Assay ID: C_2149740_10; RAMP1 rs4663269 Assay ID: C_2149726_10; RAMP1 rs7603344 Assay ID: C_11739137_10; RAMP1 rs7578855 Assay ID: C_31241858_10). Real‐time PCR amplification and detection was conducted on genomic DNA in 96‐well PCR plates using a CFX Connect Real‐Time PCR Detection System (Bio‐Rad, Milan, Italy). Thermal cycling was initiated with a denaturation step of 10 min at 95°C, followed by 50 cycles of 15 s at 92°C and 90 s at 60°C. After PCR run was completed, allelic discrimination was analyzed using the Bio‐Rad CFX Manager Software (version 3.1). Negative and positive controls for the three genotypes were included in each real‐time PCR run. For validation purposes, approximately 10% of the samples were re‐genotyped, and results were reproducible with no discrepancies noticed in genotyping. Genotyping was performed blinded to all clinical data.
Statistical analysis
Categorical variables are reported as absolute (n) and relative frequencies (%), whereas continuous variables are presented as means with SD. To examine the differences between the groups, the Student t test was applied for continuous variables with equal variances and the Welch F test for those with unequal variances, whereas a paired‐samples t test was applied for comparison of continuous variables at the baseline versus month 3 of ERE treatment. The χ2 test was used for assessing differences in the distribution of categorical variables. Clinical variables with a p value < 0.1 from univariate logistic analyses were included in multivariate logistic regression models to identify independent predictors for ERE efficacy at thresholds of 50% or 75%, respectively. Deviation of each SNP from Hardy‐Weinberg equilibrium (HWE) was calculated using Pearson goodness‐of‐fit χ2 test, which is implemented in the online Finetti program (available at: http://ihg.gsf.de/cgi‐bin/hw/hwa1.pl). The association between SNPs and each outcome of interest (50‐RESP or 75‐RESP, respectively) was assessed by logistic regression analysis assuming an additive genetic model of inheritance (i.e., each variant allele has an equal contribution to the outcome). To this end, genotypes from each SNP were coded as 0, 1, or 2 according to the number of variant alleles, and each SNP modeled as a continuous variable. The association between SNPs and response status of patients was also adjusted for confounding clinical variables. All statistical analyses were performed using MedCalc version 13.3.3 (MedCalc Software, Mariakerke, Belgium). Given the exploratory nature of this study, we reported nominal statistical associations (p < 0.05). Power and sample size calculations were performed using the Quanto software version 1.2.4 (University of Southern California).
RESULTS
One‐hundred thirteen patients were screened: three were excluded from analysis (two patients did not receive ERE, one withdrew consent), and 110 patients (91 [82.7%] females) were included and treated with ERE 70 mg monthly. Of those, 55 (50%) patients had chronic migraine and 51 (46.4%) patients had medication overuse (Table 1).
TABLE 1.
Baseline characteristics
| Demographics, n = 110 | Value |
| Age, years, mean (SD) | 47.0 (13.8) |
| Females, n (%) | 91 (82.7) |
| BMI, n = 109, mean (SD) | 23.7 (4.3) |
| Migraine characteristics and medications | |
| Age at migraine onset, years, n = 107, mean (SD) | 17.7 (9.7) |
| Migraine form, n (%) | |
| Episodic | 55 (50.0) |
| Chronic | 55 (50.0) |
| Migraine with aura, n = 109, n (%) | 37 (33.9) |
| Use of triptans | 76 (69.1) |
| Monthly migraine days, mean (SD) | 17.5 (9.2) |
| Average attack duration, h, n = 109, mean (SD) | 21.8 (26.2) |
| Average pain intensity | 7.9 (1.5) |
| No. of failed preventive medications, mean (SD) | 4.2 (2.8) |
| HIT‐6 score, mean (SD) | 65.6 (9.1) |
| MIDAS score, mean (SD) | 66.6 (56.7) |
| Patients using concomitant preventive medications, n (%) | 64 (58.2) |
| Anticonvulsants | 31 |
| Tricyclics | 17 |
| β‐Blockers | 14 |
| SSRI/SNRI | 11 |
| Angiotensin receptor blockers | 8 |
| Onabotulinumtoxin A | 2 |
| Calcium antagonists | 1 |
| No. of current preventive medications, mean (SD) | 1.5 (1.3) |
| Monthly days with use of nontriptan analgesics, last 3 months), mean (SD) | 8.3 (9.5) |
| Patients with medication overuse, n (%) | 51 (46.4) |
| Patients with first‐degree relatives with migraine, n (%) | 79 (71.8) |
| No. of first‐degree relatives with migraine, mean (SD) | 1.2 (1.3) |
| Social, physiological, and lifestyle characteristics, n (%) | |
| Working status | |
| Employed | 70 (63.6) |
| Unemployed | 31 (28.2) |
| Retired | 9 (8.2) |
| Civil status | |
| Single | 30 (27.3) |
| Married | 60 (54.5) |
| Separated/divorced | 19 (17.2.) |
| Widowed | 1 (0.9) |
| Smoking status | |
| Never | 61 (55.5) |
| Past | 24 (21.8) |
| Current | 25 (22.7) |
| Alcohol intake, n = 107 | 50 (46.7) |
| Physical activity, n = 109 | 49 (45.0) |
| Females in menopause, n = 91 | 32 (35.2) |
| Females with pregnancies, n = 91 | 53 (58.2) |
| Insomnia | |
| Present + medication | 27 (24.5) |
| Present − medication | 34 (30.9) |
| Snoring | 35 (31.8) |
| Patients with comorbidities, n (%) | |
| Anxiety | 61 (55.5) |
| Depression | 63 (57.3) |
| Chronic pain | 27 (24.5) |
| Hypertension, n = 109 | 19 (17.4) |
| Other comorbidities | 42 (38.2) |
| Head trauma, n = 109 | 16 (14.7) |
Abbreviations: BMI, body mass index; HIT‐6, Headache Impact Test‐6; MIDAS, Migraine Disability Assessment; SNRI, serotonin and norepinephrine reuptake inhibitors; SSRI, selective serotonine re‐uptake inhibitors.
ERE effectiveness and safety
At month 3 of ERE treatment, mean (SD) MMDs significantly decreased from 17.2 (8.3) to 9.2 (8.2), and the number of days with triptans and nontriptan analgesics use dropped from 7.0 (7.7) to 3.8 (5.4) and from 8.3 (9.5) to 5.3 (7.2), respectively (p < 0.0001 for all comparisons; Table 2).
TABLE 2.
Frequency, severity, and impact of migraine as well as use of abortive therapies at baseline and during month 3 after erenumab start
| Clinical variable | Baseline | Month 3 | p value |
|---|---|---|---|
| MMD, mean (SD) a | 17.5 (9.2) | 9.2 (8.2) | <0.0001 |
| Monthly days with triptan use, mean (SD) a | 7.0 (7.7) | 3.8 (5.4) | <0.0001 |
| Monthly days with use of nontriptan analgesics, mean (SD) a | 8.3 (9.5) | 5.3 (7.2) | <0.0001 |
| Patients with medication overuse, n (%) | 51 (46.4) | 19 (17.3) | <0.0001 |
| Patients with chronic migraine, n (%) | 55 (50) | 22 (20.0) | <0.0001 |
| Pain intensity (VAS), mean (SD) | 7.9 (1.5) | 5.5 (1.9) | <0.0001 |
| Attack duration, h, mean (SD) | 21.8 (26.2) | 10.1 (16.6) | <0.0001 |
| HIT‐6 score, mean (SD) | 65.6 (9.1) | 56.3 (10.9) | <0.0001 |
| MIDAS score, mean (SD) | 66.6 (56.7) | 30.7 (38.2) | <0.0001 |
Abbreviations: HIT‐6, Headache Impact Test‐6; MIDAS, Migraine Disability Assessment; MMD, monthly migraine days; VAS, visual analogue scale.
Calculated during the 3 months before erenumab start.
At month 3, mean pain intensity and attack duration were also reduced from 7.9 (1.5) to 5.5 (1.9) and from 21.8 (26.2) to 10.1 (16.6) h, respectively (p < 0.0001).
The number of patients with medication overuse decreased from 51 (46.4%) to 19 (17.3%), and 33/55 (60%) patients with chronic migraine at baseline converted to episodic migraine (p < 0.0001; Table 2). HIT‐6 and MIDAS scores decreased from 65.6 (9.1) to 56.3 (10.9) and from 66.6 (56.7) to 30.7 (38.2), respectively (p < 0.0001).
There were no treatment discontinuations. The most frequent treatment‐related adverse events were constipation (15%), injection site pain (3%), cramps (2%), migraine worsening (2%), and pruritus (1%). All were rated mild or moderate in severity. No serious adverse events were reported.
Predictors of response to ERE therapy
At month 3, 59 (53.6%) patients were 50‐RESP, and 30 (27.3%) were 75‐RESP.
At univariate analysis, lower body mass index (22.9 ± 3.6 vs. 24.6 ± 4.9, p = 0.037), lower number of failed preventive medications (3.7 ± 2.0 vs. 4.8 ± 3.3, p = 0.039), and baseline HIT‐6 score (67.4 ± 5.5 vs. 63.6 ± 11.7, p = 0.038) were associated with 50‐RESP status (Tables S1 and S2). However, no associations survived when including these variables in a multivariate logistic regression model (Table 3).
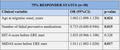
TABLE 3.
Multivariate logistic regression analysis of clinical factors in predicting 50% and 75% responder status
| Clinical variable | OR (95% CI) | p value |
|---|---|---|
| 50% responder status, n = 59 | ||
| BMI | 0.908 (0.812–1.007) | 0.069 |
| No. of failed preventive medications | 0.885 (0.754–1.039) | 0.135 |
| Baseline HIT‐6 score | 1.068 (0.995–1.146) | 0.069 |
| No. first‐degree relatives with migraine | 1.357 (0.934–1.972) | 0.109 |
| 75% responder status, n = 30 | ||
| Age at migraine onset, years | 1.062 (1.008–1.120) | 0.024 |
| No. of failed preventive medications | 0.753 (0.600–0.946) | 0.015 |
| HIT‐6 score before ERE start | 1.035 (0.966–1.108) | 0.328 |
| MIDAS score before ERE start | 1.011 (1.002–1.020) | 0.017 |
Multivariate logistic regression analysis of clinical variables with a significance level of p < 0.1 at the respective univariate analyses. Bold values indicates p < 0.05.
Abbreviations: BMI, body mass index; CI, confidence interval; ERE, erenumab; HIT‐6, Headache Impact Test‐6; MIDAS, Migraine Disability Assessment; OR, odds ratio.
At univariate analysis, 75‐RESP status was associated with older age at migraine onset (20.8 ± 9.4 vs. 16.6 ± 9.6, p = 0.046), lower number of failed preventive medications (3.4 ± 1.8 vs. 4.5 ± 3.0, p = 0.015), and higher baseline MIDAS score (92.4 ± 71.0 vs. 56.9 ± 47.3, p = 0.015), which maintained significance at multivariate analysis (odds ratio [OR] [95% confidence interval (CI)]: 1.062 [1.008–1.120], p = 0.024; 0.753 [0.600–0.946] p = 0.015; 1.011 [1.002–1.020] p = 0.017, respectively) (Tables 3, S1, and S2).
Genotype distribution of all the selected SNPs were consistent with HWE in the overall population (all p > 0.05). Despite no significant associations found between any of the SNPs analyzed and 50‐RESP status (Table S3), at univariate logistic regression analysis, RAMP1 rs7590387 was found to confer a lower probability of being 75‐RESP compared to the rs7590387C allele (for each G allele, OR [95% CI]: 0.53 [0.29–0.99], p = 0.048, Table 4). However, the nominal association of RAMP1 rs7590387 with 75‐RESP was lost after adjustments for clinical confounders (OR [95% CI] 0.55 [0.28–1.10], p = 0.09, Table 4).
TABLE 4.
Association analysis of SNPs with 75% responder status
| SNP |
Patients achieving MMD ≥ 75%, n (%) |
Patients not achieving MMD ≥ 75%, n (%) |
Crude OR (95% CI) | p value | Adjusted OR a (95% CI) | p value |
|---|---|---|---|---|---|---|
| CALCRL rs696574 | ||||||
| CC | 18 (60.0) | 60 (75.0) | 1.60 (0.76–3.34) | 0.21 | 1.50 (0.65–3.47) | 0.34 |
| TC | 11 (36.7) | 17 (21.3) | ||||
| TT | 1 (3.3) | 3 (3.8) | ||||
| CALCRL rs6710852 | ||||||
| TT | 19 (63.3) | 67 (83.8) | 2.13 (0.91–4.95) | 0.08 | 2.36 (0.91–6.10) | 0.08 |
| TG | 11 (36.7) | 11 (13.8) | ||||
| GG | 0 (0) | 2 (2.5) | ||||
| CALCRL rs3213738 | ||||||
| TT | 20 (66.7) | 69 (86.3) | 2.15 (0.90–5.14) | 0.08 | 2.47 (0.92–6.60) | 0.07 |
| TC | 10 (33.3) | 9 (11.3) | ||||
| CC | 0 (0) | 2 (2.5) | ||||
| RAMP1 rs302680 | ||||||
| AA | 21 (70.0) | 62 (77.5) | 1.37 (0.62–3.04) | 0.44 | 1.32 (0.55–3.18) | 0.54 |
| GA | 8 (26.7) | 16 (20.0) | ||||
| GG | 1 (3.3) | 2 (2.5) | ||||
| RAMP1 rs13386048 | ||||||
| GG | 14 (46.7) | 31 (38.8) | 0.90 (0.49–1.65) | 0.74 | 0.89 (0.45–1.78) | 0.74 |
| GA | 11 (36.7) | 38 (47.5) | ||||
| AA | 5 (16.7) | 11 (13.8) | ||||
| RAMP1 rs12995100 | ||||||
| TT | 5 (16.7) | 18 (22.5) | 0.90 (0.47–1.72) | 0.74 | 0.73 (0.35–1.55) | 0.42 |
| TC | 21 (70.0) | 43 (53.8) | ||||
| CC | 4 (13.3) | 19 (23.8) | ||||
| RAMP1 rs12465864 | ||||||
| AA | 21 (70.0) | 51 (63.8) | 0.97 (0.44–2.13) | 0.94 | 0.89 (0.37–2.17) | 0.80 |
| AG | 7 (23.3) | 28 (35.0) | ||||
| GG | 2 (6.7) | 1 (1.3) | ||||
| RAMP1 rs7590387 | ||||||
| CC | 13 (43.3) | 22 (27.5) | 0.53 (0.29–0.99) | 0.048 | 0.55 (0.28–1.10) | 0.09 |
| GC | 14 (46.7) | 38 (47.5) | ||||
| GG | 3 (10.0) | 20 (25.0) | ||||
| RAMP1 rs75822777 | ||||||
| GG | 11 (36.7) | 42 (52.5) | 1.66 (0.87–3.14) | 0.12 | 1.76 (0.85–3.65) | 0.13 |
| GA | 15 (50.0) | 32 (40.0) | ||||
| AA | 4 (13.3) | 6 (7.5) | ||||
| RAMP1 rs302676 | ||||||
| TT | 22 (73.3) | 45 (56.3) | 0.56 (0.24–1.32) | 0.19 | 0.66 (0.26–1.67) | 0.38 |
| TC | 7 (23.3) | 34 (42.5) | ||||
| CC | 1 (3.3) | 1 (1.3) | ||||
| RAMP1 rs11673847 | ||||||
| GG | 19 (63.3) | 54 (67.5) | 1.01 (0.46–2.22) | 0.97 | 1.12 (0.47–2.69) | 0.80 |
| GA | 11 (36.7) | 23 (28.8) | ||||
| AA | 0 (0) | 3 (3.8) | ||||
| RAMP1 rs6431564 | ||||||
| AA | 6 (20.0) | 21 (26.3) | 0.91 (0.48–1.76) | 0.79 | 0.87 (0.41–1.85) | 0.72 |
| AG | 21 (70.0) | 43 (53.8) | ||||
| GG | 3 (10.0) | 16 (20.0) | ||||
| RAMP1 rs4663269 | ||||||
| TT | 6 (20.0) | 19 (23.8) | 1.17 (0.60–2.25) | 0.65 | 0.82 (0.39–1.74) | 0.61 |
| TC | 18 (60.0) | 47 (58.8) | ||||
| CC | 6 (20.0) | 14 (17.5) | ||||
| RAMP1 rs7603344 | ||||||
| AA | 14 (46.7) | 41 (51.3) | 1.35 (0.67–2.70) | 0.40 | 1.69 (0.76–3.72) | 0.20 |
| AG | 13 (43.3) | 36 (45.0) | ||||
| GG | 3 (10.0) | 3 (3.8) | ||||
| RAMP1 rs7578855 | ||||||
| TT | 10 (33.3) | 34 (42.5) | 1.01 (0.56–1.82) | 0.98 | 1.01 (0.52–1.96) | 0.99 |
| CT | 17 (56.7) | 31 (38.8) | ||||
| CC | 3 (10.0) | 15 (18.8) | ||||
Abbreviations: CI, confidence interval; MMD, monthly migraine days; OR, odds ratio; SNP, single nucleotide polymorphism.
Logistic regression analysis adjusted by age at migraine onset, number of failed preventive medications, and Migraine Disability Assessment score before erenumab start. Association of SNPs was assessed under the additive genetic model.
DISCUSSION
We investigated clinical and genetic characteristics associated with a reduction of MMDs by at least 50% (50‐RESP) or 75% (75‐RESP) at month 3 after ERE start in a population of 110 migraine patients treated at tertiary headache centers in Switzerland.
ERE effectiveness and safety profile in our real‐word setting study were in line with those seen in the registration trials [7, 8, 9, 10] and observational [13, 17, 18, 19, 20] studies. ERE treatment was associated with significant improvements in frequency, intensity, and duration of migraine, which is reflected in a reduced use of acute pain medication and ultimately in an improvement of migraine‐related burden as measured by MMDs, MIDAS, and HIT‐6 scores.
The main finding of our study was that a lower number of failed preventive medications, a higher MIDAS score, and an older age at migraine onset were associated with a higher likelihood to favorable response to ERE as defined by 75‐RESP status, whereas no significant associations were found when using the 50‐RESP definition of treatment responder.
The 75‐RESP group had an average number of previous preventive medications of 3.4 ± 1.8, in line with inclusion criteria of the LIBERTY trial [9]. The respective value for patients with a reduction of MMD inferior to 75% was 4.5 ± 3.0, indicating a particularly difficult‐to‐treat migraine population. When using the 50‐RESP definition, the average number of previous preventive medications did not survive the multivariate analysis. Accordingly, the number of failed preventive medications was not significantly associated with 50‐RESP status in a large study by Barbanti et al. [13] and two further smaller studies [21, 22]. Overall, it is clinically plausible that the number of previously failed preventive medications gains relevance, especially when addressing a more stringent therapeutic target such as 75‐RESP.
A higher MIDAS score indicates that headache is associated with a relevant burden and limits daily activities [16]. It is conceivable that higher MIDAS scores are more likely found in patients with more severe forms of migraine. However, we did not find an association between 50‐ or 75‐RESP status and various characteristics of migraine such as intensity, frequency, and duration when considered individually, highlighting the very complex picture of migraine in individual patients. MIDAS scores were not found to be associated with 50‐RESP by Russo et al. [23] and Matteo et al. [22], whereas this covariate was not investigated in other observational studies assessing factors predictive of treatment response to ERE [13, 21].
Older age at migraine onset was associated with 75‐RESP status, indirectly pointing to the findings by Russo et al. [23] of an association with migraine disease duration.
Interestingly, our study showed that in a real‐word setting, the 75‐RESP definition, and less so the 50‐RESP definition, could contribute to identifying relevant clinic predictors of response to ERE. Compared to 50‐RESP status, 75‐RESP status better segregates those patients with a clear‐cut positive response to ERE, and therefore likely better identifies their respective clinic characteristics.
Our migraine population was treated with ERE 70 mg monthly. According to the Swiss reimbursement criteria, it is possible to increase ERE dose from 70 to 140 mg monthly in case of <50% response after 3 months of therapy. It is therefore conceivable that a proportion of nonresponders under ERE 70 mg monthly treatment would become 50‐ or 75‐RESP following dose increase. For this reason, we are following these patients to capture the effect of any dose changes on our results. This will also allow us to investigate the population of those resistant or refractory migraine patients who do not respond to either ERE dose, representing currently a relevant research topic [24, 25].
We could not identify SNPs with significant association for 75‐RESP or 50‐RESP status after adjustment for various clinical variables. Besides indicating that common SNPs of CALCRL and RAMP1 do not likely exert major effects in predicting response to ERE, this finding might reflect the low statistical power of our study to detect associations with small genetic effect sizes. Despite this, results of univariate logistic regression analysis revealed an allele dosage association between RAMP1 rs7590387G and a lower probability of being 75‐RESP compared to the major rs7590387C allele. No expression or functional data currently exist regarding rs7590387. It should be noted that it is localized 1.4 kb downstream of the RAMP1 gene; however, case‐control genetic association studies [26, 27] have excluded its role as a risk factor for migraine. Despite this, the rs7590387G allele at the RAMP1 locus has been found associated with a lower risk for transformation of episodic migraine into medication‐overuse headache [26], suggesting involvement of RAMP1 rs7590387 in migraine chronification. In view of these findings and the results of our present study, larger studies are needed to confirm a possible effect of RAMP1 rs7590387 on the clinical response to ERE.
When considering the whole class of mAbs targeting the CGRP system in migraine, we are aware of a single study of whole‐genome genotyping presented at the 2019 International Headache Congress (IHC), which failed to show associations between eptinezumab clinical response and patient genotype [28].
Our study has some limitations. First, the small sample size limits the power to detect genetic predictors in response to ERE, particularly if these only confer a weak modulation effect. Considering that our study included 110 migraineurs, of which 27.3% were 75‐RESP, and assuming a power of 80% with significance level of 0.05, the minimal detectable OR under the additive model of SNPs with minor allele frequencies ranging from 0.1 to 0.5, was found to be between 2.4 and 3.1. Therefore, the sample size of our study is adequate for evaluation of clinically relevant SNPs with medium and large effects, but substantially underpowered for investigation of SNPs with small‐effect sizes. Furthermore, confirmation of our findings is warranted in a larger cohort of ERE‐treated migraine patients. Assuming 27.3% of 75‐RESP, the sample size required for an independent study to replicate the association of RAMP1 rs7590387 (MAF = 0.18) under the additive model (ORadjusted = 0.55), with a power of 80% and significance level of 0.05, was calculated to be 308. Second, we did not apply post hoc correction for multiple SNPs testing, because this was a hypothesis‐generating study. Hence, replication studies aiming to also confirm the association of CALCRL gene variants (i.e., rs6710852 and rs3213738) should take into account multiple testing to properly control the false positive rate. Additionally, our study lacked a control group for potential confounding, which would also be recommended in replication studies. Also, RAMP1 gene sequencing should be considered to identify, if any, causal variants with functional effects on ERE binding and/or on signal transduction of the CGRP receptor. In addition, our definitions of 50‐ and 75‐RESP to ERE are based on the respective reduction in MMDs, which does not comprehensively represent all migraine dimensions. Still, these are recognized outcome measures wildly used in clinical trials and observational studies. Our findings are not directly generalizable to other migraine populations, because these might significantly differ from ours, or to other mAbs targeting the CGRP system, because those available so far bind the CGRP ligand rather than the CGRP receptor.
Our study led to the finding that the therapeutic response to ERE can be modulated by clinical variables (number of failed preventive medications, migraine‐related burden and age) and possibly by genetic factors, such as rs7590387 at the RAMP1 locus. If confirmed in larger controlled studies, these factors might be integrated in the treatment‐decision algorithm to optimize individualized patient care and health resources allocation.
CONFLICT OF INTEREST
The authors declared the following potential conflicts of interest with the respect to the research, authorship, and/or publication of this article: the employer of C.Z. receives support for advisor activities, speaking, or grants from Celgene, Genzyme, Lilly, Merck, Novartis, Roche, and grants from Abbvie, Almirall, Biogen Idec, Celgene, Genzyme, Lilly, Merck, Novartis, Roche, Teva Pharma. C.S. reports scientific support, travel support, and/or honoraria from Novartis, Eli Lilly, TEVA Pharmaceuticals, Lundbeck, Allergan, Almirall, Amgen, MindMed, Grünenthal. C.S. is a part‐time employee at Zynnon. C.S. received research grants from German Migraine and Headache Society, Eye on Vision Foundation, and Baasch Medicus Foundation. The employer of C.G. receives support for advisor activities, speaking or grants from Celgene, Genzyme, Lilly, Merck, Novartis, Roche, and grants from Abbvie, Almirall, Biogen Idec, Celgene, Genzyme, Lilly, Merck, Novartis, Roche, Teva Pharma. S.C., G.C.R., S.T., M.V., N.M.G., I.M., and S.S. have no conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
Chiara Zecca: Conceptualization (lead), data curation (lead), formal analysis (equal), investigation (lead), methodology (lead), project administration (lead), resources (lead), supervision (equal), writing–original draft (lead), writing–review & editing (lead). Sarah Cargnin: Formal analysis (equal), writing–review & editing (equal). Christoph Schankin: Data curation (equal), methodology (equal), writing–review & editing (equal). Nadia Mariagrazia Giannantoni: Data curation (equal), writing–review & editing (supporting). Michele Viana: Writing–review & editing (equal). Isabella Maraffi: Data curation (equal), writing–review & editing (supporting). Gianna Carla Riccitelli: Writing–review & editing (supporting). Shairin Sihabdeen: Data curation (equal), writing–review & editing (supporting). Salvatore Terrazzino: Conceptualization (equal), formal analysis (equal), methodology (equal), writing–review & editing (equal). Claudio Gobbi: Conceptualization (equal), funding acquisition (equal), methodology (equal), resources (lead), supervision (lead), writing–review & editing (lead).
Supporting information
Table S1‐S3
ACKNOWLEDGMENTS
C.Z. holds a grant from Ente Ospedaliero Cantonale for senior researchers. S.C. holds a grant from Ministero della Salute (Bando Finalizzata 2016‐GR‐2016‐02363848). Open access funding provided by Universita della Svizzera italiana.
Zecca C, Cargnin S, Schankin C, et al. Clinic and genetic predictors in response to erenumab. Eur J Neurol. 2022;29:1209–1217. doi: 10.1111/ene.15236
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Dodick DW. Migraine. Lancet. 2018;391(10127):1315‐1330. [DOI] [PubMed] [Google Scholar]
- 2. Sprenger T, Viana M, Tassorelli C. Current prophylactic medications for migraine and their potential mechanisms of action. Neurotherapeutics. 2018;15(2):313‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goadsby PJ, Edvinsson L, Ekman R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol. 1990;28(2):183‐187. [DOI] [PubMed] [Google Scholar]
- 4. Goadsby PJ, Edvinsson L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol. 1993;33(1):48‐56. [DOI] [PubMed] [Google Scholar]
- 5. Lassen LH, Haderslev PA, Jacobsen VB, Iversen HK, Sperling B, Olesen J. CGRP may play a causative role in migraine. Cephalalgia. 2002;22(1):54‐61. [DOI] [PubMed] [Google Scholar]
- 6. Ho TW, Edvinsson L, Goadsby PJ. CGRP and its receptors provide new insights into migraine pathophysiology. Nat Rev Neurol. 2010;6(10):573‐582. [DOI] [PubMed] [Google Scholar]
- 7. Goadsby PJ, Reuter U, Hallström Y, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med. 2017;377(22):2123‐2132. [DOI] [PubMed] [Google Scholar]
- 8. Dodick DW, Ashina M, Brandes JL, et al. ARISE: A Phase 3 randomized trial of erenumab for episodic migraine. Cephalalgia. 2018;38(6):1026‐1037. [DOI] [PubMed] [Google Scholar]
- 9. Reuter U, Goadsby PJ, Lanteri‐Minet M, et al. Efficacy and tolerability of erenumab in patients with episodic migraine in whom two‐to‐four previous preventive treatments were unsuccessful: a randomised, double‐blind, placebo‐controlled, phase 3b study. Lancet. 2018;392(10161):2280‐2287. [DOI] [PubMed] [Google Scholar]
- 10. Tepper S, Ashina M, Reuter U, et al. Safety and efficacy of erenumab for preventive treatment of chronic migraine: a randomised, double‐blind, placebo‐controlled phase 2 trial. Lancet Neurol. 2017;16(6):425‐434. [DOI] [PubMed] [Google Scholar]
- 11. Barbanti P, Aurilia C, Egeo G, et al. Erenumab in the prevention of high‐frequency episodic and chronic migraine: Erenumab in Real Life in Italy (EARLY), the first Italian multicenter, prospective real‐life study. Headache. 2021;61(2):363‐372. [DOI] [PubMed] [Google Scholar]
- 12. Garces F, Mohr C, Zhang LI, et al. Molecular insight into recognition of the CGRPR complex by migraine prevention therapy Aimovig (Erenumab). Cell Rep. 2020;30(6):1714‐23.e6. [DOI] [PubMed] [Google Scholar]
- 13. Roden DM, McLeod HL, Relling MV, et al. Pharmacogenomics. Lancet. 2019;394(10197):521‐532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders. Cephalalgia. 2018;38(1):1‐211. [DOI] [PubMed] [Google Scholar]
- 15. Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache‐related disability. Neurology. 2001;56(6 Suppl. 1):S20‐S28. [DOI] [PubMed] [Google Scholar]
- 16. Houts CR, Wirth RJ, McGinley JS, et al. Content validity of HIT‐6 as a measure of headache impact in people with migraine: a narrative review. Headache. 2020;60(1):28‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cheng S, Jenkins B, Limberg N, Hutton E. Erenumab in chronic migraine: an Australian experience. Headache. 2020;60(10):2555‐2562. [DOI] [PubMed] [Google Scholar]
- 18. Lambru G, Hill B, Murphy M, Tylova I, Andreou AP. A prospective real‐world analysis of erenumab in refractory chronic migraine. J Headache Pain. 2020;21(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Robblee J, Devick KL, Mendez N, Potter J, Slonaker J, Starling AJ. Real‐world patient experience with erenumab for the preventive treatment of migraine. Headache. 2020;60(9):2014‐2025. [DOI] [PubMed] [Google Scholar]
- 20. Scheffler A, Messel O, Wurthmann S, et al. Erenumab in highly therapy‐refractory migraine patients: First German real‐world evidence. J Headache Pain. 2020;21(1):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ornello R, Casalena A, Frattale I, et al. Real‐life data on the efficacy and safety of erenumab in the Abruzzo region, central Italy. J Headache Pain. 2020;21(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Matteo E, Favoni V, Pascazio A, et al. Erenumab in 159 high frequency and chronic migraine patients: real‐life results from the Bologna Headache Center. Neurol Sci. 2020;41(Suppl. 2):483‐484. [DOI] [PubMed] [Google Scholar]
- 23. Russo A, Silvestro M, Scotto di Clemente F, et al. Multidimensional assessment of the effects of erenumab in chronic migraine patients with previous unsuccessful preventive treatments: a comprehensive real‐world experience. J Headache Pain. 2020;21(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sacco S, Braschinsky M, Ducros A, et al. European headache federation consensus on the definition of resistant and refractory migraine: developed with the endorsement of the European Migraine & Headache Alliance (EMHA). J Headache Pain. 2020;21(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ornello R, Tiseo C, Frattale I, et al. The appropriate dosing of erenumab for migraine prevention after multiple preventive treatment failures: a critical appraisal. J Headache Pain. 2019;20(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cargnin S, Pautasso C, Viana M, et al. Association of RAMP1 rs7590387 with the risk of migraine transformation into medication overuse headache. Headache. 2015;55(5):658‐668. [DOI] [PubMed] [Google Scholar]
- 27. Sutherland HG, Buteri J, Menon S, et al. Association study of the calcitonin gene‐related polypeptide‐alpha (CALCA) and the receptor activity modifying 1 (RAMP1) genes with migraine. Gene. 2013;515(1):187‐192. [DOI] [PubMed] [Google Scholar]
- 28. Misura KYS, Madan A, Olson C, Smith J, Latham J. Genetic assessment of eptinezumab response in the prevention of migraine. Cephalalgia. 2019;39(1_suppl):1‐337. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1‐S3
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


