A 52‐year‐old woman diagnosed in 2017 with low‐risk myelodysplastic syndrome (MDS) with multilineage dysplasia (R‐IPSS score 1.5) is evaluated for persistent reticulocytosis since 4 years, without evidence of bleeding or hemolysis.
Her laboratory results indicate the following: red blood count 3.56 × 1012/L (reference range: 3.8–5.2 × 1012/L); hemoglobin 10.1 g/dL (11.7–15.7 g/dL); hematocrit 0.32 L/L (0.35–0.47 L/L); MCV 93 fl (81–99 fl); MCHC 313 g/L (310–360 g/L); red cell distribution width 16.7% (11%–15%); reticulocytes 929 × 109/L (20–120 × 109/L), 26.1% (0.5%–1.5%); platelets 146 × 109/L (150–350 × 109/L); and leukocytes 2.2 × 109/L (4.0–10 × 109/L). Of note, MCV, expected to be increased in case of reticulocytosis is normal. Hemolytic parameters (LDH, bilirubin, haptoglobin) and creatinine are normal. The direct antiglobulin test is negative. Scattergram (Image 1A, white circle) shows small‐size reticulocytes with dim fluorescence (low RNA content), corresponding to a population of old reticulocytes. Peripheral blood smear (Image 1B) shows marked anisopoikilocytosis, polychromasia, and anisochromia. Presence of reticulocytes is confirmed on cresyl blue stain (Image 1C, arrows).
IMAGE 1.
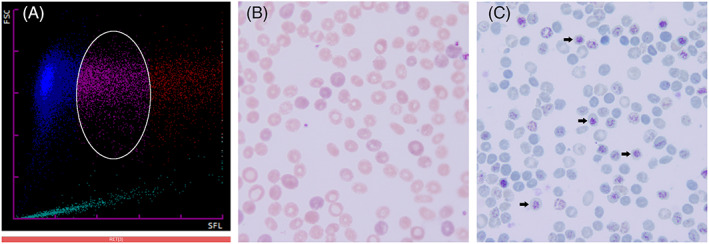
Morphologic and flow cytometry features of old reticulocytes. (A), Scattergram (Sysmex XN9000) (FSC, forward‐scattered light; SFL, side‐fluorescence light) demonstrating a population of low‐size reticulocytes with dim fluorescence (white circle). (B), Peripheral blood smear showing anisopoikilocytosis, polychromasia, and anisochromia (hematoxylin and eosin stain, original magnification ×1000). (C), Peripheral blood smear with arrows showing reticulocytes with dim fluorescence (low RNA content) on cresyl blue stain (original magnification ×1000)
The phenomenon of increased reticulocytes without hemolysis or bleeding among patients with MDS has been described in few publications. 1 , 2 It is a consequence of abnormal erythropoiesis with underlying delayed reticulocyte maturation, which may arise because of altered ribonucleic acid metabolism or a deficiency of ribonuclease. 3 This process results in an increased number of circulating older reticulocytes with smaller size and low RNA content. Under normal conditions, reticulocytes have a half‐life of 24–48 h in the peripheral circulation, before losing their RNA and becoming erythrocytes. Due to delayed maturation, reticulocytes retain their RNA for a longer time, resulting in a prolonged half‐life in peripheral blood and thus in “pseudoreticulocytosis.”
CONFLICT OF INTEREST
All authors declare that they have no conflict of interest.
ACKNOWLEDGMENT
Open access funding enabled and organized by Projekt DEAL.
De Rossi N, Alberio L, Stalder G. Pseudoreticulocytosis in a patient with myelodysplastic syndrome. Am J Hematol. 2022;97(6):841‐842. doi: 10.1002/ajh.26431
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Hertenstein B, Kurrle E, Redenbacher M, Arnold R, Heimpel H. Pseudoreticulocytosis in a patient with myelodysplasia. Ann Hematol. 1993;67(3):127‐128. [DOI] [PubMed] [Google Scholar]
- 2. Carulli G, Marini A, Azzarà A, Lucchetti A, Petrini M. Pseudoreticulocytosis in a case of myelodysplastic syndrome. Acta Haematol. 1998;100(3):156‐158. [DOI] [PubMed] [Google Scholar]
- 3. Riley RS, Ben‐Ezra JM, Goel R, Tidwell A. Reticulocytes and reticulocyte enumeration. J Clin Lab Anal. 2001;15(5):267‐294. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


