Abstract
Background
Globally, initiation of paediatric advance care planning discussions is advocated early in the illness trajectory; however, evidence suggests it occurs at crisis points or close to end of life. Few studies have been undertaken to ascertain the prevalence and determinants of behaviour related to initiation by the healthcare professional.
Method
Underpinned by the Capability, Opportunity, Motivation–Behaviour (COM‐B) model for behaviour change, a cross‐sectional online survey was conducted in United Kingdom and Ireland using a purposive sample of health professionals. Descriptive and inferential statistics were applied and nonparametric statistical analysis used. Open‐ended questions were mapped and correlations between COM‐B and demographic profiles identified.
Results
Responses (n = 140): Paediatric advance care planning was viewed positively; however, initiation practices were found to be influenced by wide ranging diagnoses and disease trajectories. Whilst some tools and protocols exist, they were not used in a systematic manner, and initiation behaviour was often not guided by them. Initiation was unstandardized, individually led, guided by intuition and experience and based on a range of prerequisites. Such behaviour, combined with inconsistencies in professional development, resulted in varying practice when managing clinical deterioration. Professionals who felt adequately trained initiated more conversations (capability). Those working in palliative care specialties, hospice settings and doctors initiated more discussions (opportunity). There was no difference in Motivation between professions, clinical settings or specialisms, although 25% (n = 35) of responses indicated discomfort discussing death and 34% (n = 49) worried about families' emotional reaction.
Conclusion
Although advocated, paediatric advance care planning is a complex process, commonly triggered by the physical deterioration and rarely underpinned by support tools. The COM‐B framework was useful in identifying fundamental differences in initiation behaviour; however, further research is required to explore the complexity of initiation behaviour and the system within which the care is being delivered to identify influences on initiation.
Keywords: advance care planning, health professionals, life limited, paediatric, palliative care
Key Messages.
Paediatric advance care planning is commonly triggered by the physical deterioration of the child, regardless of the professionals' level of experience.
Initiation of advance care planning is influenced by wide ranging diagnosis and disease trajectories and when combined with inconsistency in professional training and education, limited organizational protocols and underused resources results in inconsistent practice.
It was found that professionals identified certain prerequisites that influenced wording, timing and who leads such discussions. These prerequisites included a rapport with the family, knowledge of the family dynamics, readiness of parents and less important to experienced professionals, the need for a consensus from professional colleagues and a definite prognosis.
Approaches that enhance capability and opportunity of less experienced and non‐palliative care staff, particularly staff already motivated, may facilitate both initiation of advance care discussions and increase motivation to refer children to paediatric palliative care services and thereby improve their opportunity to have a discussion initiated.
1. INTRODUCTION
Planning for end of life also known as advance or anticipatory care planning is a term used to describe ongoing conversations, ideally starting at diagnosis, between a person, family members and health professionals about future care and preferences. Advance care planning is advocated in both adult and children's national and international palliative care policy (DOHA, 2018; NICE, 2016). Advance care planning for adults has been defined (Rietjens et al., 2017) but no definition specific to children currently exists. Paediatric advance care planning is reported to enhance parent satisfaction, enable identification of patient and family wishes and goals, improve quality of care, avoid inappropriate paediatric intensive care admissions or futile treatment and aid the bereavement process (Audigé et al., 2020; Basu & Swil, 2018; DeCourcey et al., 2019; Kelly et al., 2018; Lotz et al., 2017). However, despite the potential benefits, there is little standardization, and the implementation of paediatric advance care planning is variable globally (Mitchell et al., 2014; Together for Short Lives, 2017). A key barrier cited is the initiation of conversations, yet the avoidance or delay may effect recognition and achievement of wishes and goals throughout the life journey and, ultimately, good end of life care (Côté et al., 2020; Lord et al., 2020).
To facilitate palliative care discussions, and the process of advance care planning with adults, conversation starter tool kits have been developed (Blackford & Street, 2013; de Vleminck et al., 2015; Guo et al., 2018; Norals & Smith, 2015; Rodenbach et al., 2017; Yeh et al., 2014). Whilst research has explored paediatric advance care planning implementation, specifically completion of documentation, barriers and content (Basu et al., 2021; Hein et al., 2020) a review of tools, guidance documents and published papers indicated that although a number of interventions and programmes exist for adolescents (Lyon et al., 2018; Zadeh & Wiener, 2015), few, until recently (Ekberg et al., 2020; Fahner et al., 2020; van Breemen et al., 2020) focus on parents of younger children or included initiation (Carr et al., 2020). It is important to examine the initiation of children's advance planning discussions within the clinical context, and the aim of this present study was to identify what current practices, factors and behaviour determinants influence health professionals' approaches to initiation of paediatric advance care planning.
2. METHODS
2.1. Design
A cross‐sectional descriptive correlational study of healthcare professionals with experience in initiation of paediatric advance care planning was undertaken. The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) standard for reporting cross sectional studies was followed (STROBE, 2007) (see Data S1). The data were collected between 12 July and 31 August 2019 in United Kingdom and Ireland.
2.2. Study tool
A questionnaire to examine current practices, factors and behaviour determinants influencing health professionals' approaches to initiation of paediatric advance care planning was developed from a review of the literature and informed by the COM‐B framework (Carr et al., 2020; Michie et al., 2014). The COM‐B model proposes that individuals must be psychologically and physically able (Capable ‘C’), have the social and physical right set of circumstances (Opportunity ‘O’) and be galvanized (Motivated ‘M’) to complete the behaviour more than any other opposing behaviours at this time. COM‐B has been used to study different behaviours but, to our knowledge, has not been applied to pACP providing new possibilities for understanding clinician behaviour in this context.
A 54‐item instrument was divided into the following sections: Demographics, Approach, Capability, Opportunity and Motivation (see Data S2). Multiple choice, open ended and Likert 5‐point rating scale question formats were used.
2.3. Sample
Perspectives were sought from healthcare professionals working with children who are life limited (to childhood) throughout the UK and Ireland who were members of professional groups (Table 1). Acknowledging that initiation of pACP is not specific to one role, but rather the responsibility of generalists and specialists, it was important to ensure representation from non‐palliative care professionals whilst also targeting professionals who recognized the term, concept and responsibility they had in initiating conversations. Membership of the professional organizations included generalists and specialists not solely based in paediatric palliative care. Sample size was based on membership figures of the various groups and calculated using specialized software (Raosoft, 2004). Identified individuals within the professional organizations with access to contact details of members disseminated the invitation to participate via email or their electronic newsletter. Invitations outlined the inclusion/exclusion criteria (Table 1). Individuals were self‐selected to participate and were informed that completion of the questionnaire implied their consent.
TABLE 1.
Inclusion and exclusion criteria
| Inclusion criteria (must meet all inclusion criteria) | Exclusion criteria |
|---|---|
| 1. Experience initiating or observing initiation of paediatric advance care planning (pACP) discussions. | 1. No experience initiating or observing initiation of paediatric advance care planning (pACP) discussions. |
| 2. A health professional affiliated with one of the United Kingdom (UK) or Republic of Ireland (ROI) palliative care organizations listed below | 2. Health professional not affiliated with one of the palliative care organizations listed below |
| Together for Short Lives members (TfSL) | |
| Association of paediatric palliative medicine (APPM) | |
|
Irish Association of Palliative Care (IAPC‐CPC) (inc. LauraLynn Hospice and Jack and Jill service). | |
| Irish hospice foundation National Development Committee (IHF‐NDC‐CPC) | |
| Other relevant paediatric group | |
| 3. Health professionals working in UK or ROI. | 3. Health professionals not working in UK or ROI. |
To enhance response rate, emails and social media reminders with hyperlinks were sent 2 weeks after initial e‐mail and 1 week before access closed (Andrews et al., 2003; Dillman et al., 2014; McPeake et al., 2014).
2.4. Data collection
Face and content validation and a pilot study (n = 6) resulted in the addition of two questions (Q28 and Q29) (see Data S2) and minor formatting changes. The anonymous self‐report online questionnaire was administered via www.qualtrics.com and remained open for 7 weeks.
2.5. Statistical analysis
Each scale item was assessed for reliability to gauge the scale internal consistency and data screed for outliers and multicollinearity (Pallant, 2016). Descriptive participant characteristics were summarized. Surveys were included in the analysis if >95% complete and had behaviour constructs of Capability, Opportunity and Motivation fully completed. Descriptive and inferential statistics were applied using SPSS version 25 (IBM, 2017). Guided by data type (nominal/ordinal), non‐parametric statistical analysis was undertaken using Mann–Whitney; Chi‐Square and Kruskal‐Wallis tests were used to compare differences by demographic characteristics (Pallant, 2016). Exploratory factor analysis was used to group construct Opportunity and Motivation items. Individual questions relating to capability were analysed not capability as a specific construct. Pearson's rank correlation was used to identify any correlation between COM‐B and demographic profiles of health professionals. Qualitative responses to open‐ended questions were limited to categorizing the data in pre‐existing categories'.
Ethical approval was obtained from the University Research Ethics Filter Committee (1 July 2019). Participants were informed of the study aim prior to participation and that return of the questionnaire implied consent.
3. RESULTS
A total of 196 responses were received from which 140 (71%) were eligible for inclusion with >95% item completion. Based on membership of the various groups (n = 327), this constituted a response rate of 43%. Recommended sample size (n = 177) which enabled a confidence level of 95% and a margin of error of 6% was calculated using Raosoft sample size calculator (Raosoft, 2004). Demographic data are displayed in Table 2.
TABLE 2.
Demographic characteristics
| % | n | ||
|---|---|---|---|
| Professions | Medical | 35.7 | 50 |
| Nurses | 59.3 | 83 | |
| Allied health professionals | 5 | 7 | |
| Seniority: Medical | Consultant/general practitioner | 32.1 | 45 |
| Nurses | Specialist | 41 | 58 |
| Main role: Palliative/non‐palliative | Palliative | 57.9 | 81 |
| Non‐palliative | 40.7 | 59 | |
| Medical specialisms a | Palliative | 17.1 | 26 |
| General paediatrics | 12.8 | 18 | |
| Other (neonatology, oncology/haematology, intensive care, neurodisability) | 6.3 | 9 | |
| Nurse specialisms b | Palliative | 36.4 | 51 |
| Oncology | 4.2 | 6 | |
| Advance nurse practitioner | 3.5 | 5 | |
| Community children's nurse | 2.1 | 3 | |
| Condition specific specialist nurse | 2.1 | 3 | |
| Palliative care | Doctors | 18.6 | 26 |
| Nurses | 36.4 | 51 | |
| Years registered | Less than 10 years | 11.4 | 16 |
| 11–20 years | 25.5 | 36 | |
| Registered 21 or more years | 62.8 | 88 | |
| Years caring for life limited children | Less than 10 years | 33.6 | 47 |
| 11–20 years | 36.3 | 51 | |
| More than 21 years’ | 30.1 | 42 | |
| Practice setting (adult hospice and all settings included with children's hospice) | Children's hospice inpatient and/or home care | 36 | 48 |
| Hospital and/or community | 64 | 92 | |
| Gender | Female | 91 | 128 |
| Ethnicity | White (British, Irish, other) | 95 | 133 |
| Religious affiliation | Christian | 62.9 | 88 |
| No religion | 28.6 | 40 | |
| Other | 8.4 | 12 | |
| Affiliation of group in UK or ROI | UK | 84 | 117 |
| Ireland | 16 | 22 | |
Specialism was not mutually exclusive (therefore, values do not add to 100%), e.g., could be oncology and palliative specialist consultant.
Fifteen Nurses indicated no specialism.
3.1. Variation in diagnoses
Respondents reflection on their last discussion initiated or observed initation revealed that the children had a diverse range of diagnoses (n = 79 from 138 completed responses) (Table 3). The majority of conditions were unique to children, and 10% of the 138 children had no confirmed diagnosis (n = 14). A Chi‐square test for independence showed that there was a small association between the number of paediatric advance care planning discussions initiated and the need for a definite prognosis X 2 (3, n = 139) = 8.0, p = .046. These results indicated that staff who initiated more than 12+ paediatric advance care planning discussions in the previous year did not require the child to have a definite prognosis.
TABLE 3.
Diagnosis of child at last ACP initiation or observed initiation
| TfSL category | Description | Number in group | Examples in study |
|---|---|---|---|
| Group 1 | Life‐threatening conditions for which curative treatment may be feasible but can fail | 32 |
Osteosarcoma Intestinal failure |
| Group 2 | Conditions where premature death is inevitable | 23 |
Trisomy 18, 13 Duchenne muscular dystrophy |
| Group 3 | Progressive conditions without curative treatment options | 44 |
Undiagnosed neurodegenerative Mucopolysaccharidosis |
| Group 4 | Irreversible but non‐progressive conditions causing severe disability, leading to susceptibility to health | 39 |
Holosprosenchephaly Lissenchephaly |
| Total | 138 a | 79 different diagnoses |
Two respondents did not complete this question.
3.2. Practice characteristics
Various practice characteristics influenced the initiation of paediatric advance care planning. Doctors took the lead in the initiation more than any other professional groupings regardless of clinical specialty (p = .043). As would be expected, palliative care professionals initiated discussions more often than those not in palliative care (p = .018). Chi‐square test indicated no association between the clinical areas of acute general hospital/community and Hospice/Hospice community and the number of pACP participated in nor in the number of pACP initiated.
3.3. COM‐B constructs
Mean and standard deviation of individual COM‐B items are represented in Table 4.
TABLE 4.
COM‐B: Results, mean and standard deviation of individual COM‐B items
| COM‐B | Questions | Results (summarized) | Mean | SD | |
|---|---|---|---|---|---|
| Capability refers to individuals' physical and psychological capability (skills, strength or stamina) to engage in a behaviour | |||||
| Physical | No questions addressed this aspect | ||||
| Psychological | 1 | I have received adequate training in how to start pACP discussions |
69% SA/A 16% D |
2.19 | 1.123 |
| 2 | I have developed my own approach to pACP initiation through experience | 89% SA/A | 1.56 | .847 | |
| Opportunity refers to environmental factors that influence behaviour and may be physical or social. | |||||
| Physical | 3 | My work environment facilitates pACP discussions adequately | 73% SA/A | 2.03 | 1.075 |
| 4 | I have enough time to engage in pACP discussions. | 75% SA/A | 2.05 | 1.158 | |
| 5 | We have a nominated team member responsible for initiating pACP discussions | No ‐ 89% | 1.89 | .310 | |
| 6 | There are protocols in place to help me find the words to start pACP discussions | No – 74% | 1.74 | .438 | |
| Social | 7 | I have had opportunities to observe experienced colleagues planning and initiating pACPs | 80% SA/A | 1.85 | 1.090 |
| 8 | My colleagues are supportive of pACP discussions with families | 85% as/Mt | 1.71 | .913 | |
| 9 | My ability to begin pACP discussions is impacted by families' cultural beliefs | 61% SA/A | 3.60 | 1.169 | |
| 10 | My ability to begin pACP discussions is impacted by families' religious beliefs | 56% SA/A | 3.47 | 1.206 | |
| 11 | My ability to begin pACP discussions is impacted by families' spiritual beliefs | 55% SA/A | 3.47 | 1.180 | |
| 12 | I delay starting pACP discussions because I am worried about the family's emotional reaction. |
34% SA/A 41% SD/D |
2.81 | 1.166 | |
| 13 | I delay starting pACP discussions because I expect disagreement with families |
11% SA/A 90% SD/D |
2.33 | 1.010 | |
| 14 | I fear parents may lose confidence in me if I start talking about pACP |
8% SA/A 78% SD/D |
1.83 | .985 | |
| 15 | I worry about families losing hope when I start a pACP discussion |
19% SA/A 61% SD/D |
2.27 | 1.164 | |
| Motivation includes all brain processes that guide behaviour and includes reflective and automatic processes. | |||||
| Reflective motivation includes individuals' evaluations and plans to engage in behaviour | 16 | I am confident in how to start pACP conversations. | 88% SA/A | 1.68 | .838 |
| 17 | I believe that I know when to start a pACP conversation | 90% SA/A | 1.72 | .684 | |
| 18 | I believe pACP are unnecessary | 93% SD/D | 1.22 | .586 | |
| 19 | pACP is useful for health care professionals | 96% SA/A | 1.22 | .572 | |
| 20 | pACP is useful for families | 96% SA/A | 1.25 | .573 | |
| 21 | pACP can have an adverse effect on the relationship the family have with me |
12% SA/A 62% SD/D |
2.16 | 1.064 | |
| 22 | pACP fits well with my usual manner of working | 87% SA/A | 1.50 | .708 | |
| 23 | I believe professionals are responsible for starting pACP conversation not the family | 73% SA/A | 2.22 | .687 | |
| 24 | I believe I am responsible for starting pACP conversation | 52% A/MT n = 73 | 2.64 | .967 | |
| 25 | I believe the initiation of pACP is another professionals' responsibility | 83% SD/D | 2.12 | .740 | |
| 26 | I plan how I start pACP (no‐one reported not planning them) |
87% SA/A |
1.57 | .726 | |
| Automatic motivation refers to emotions, impulses and habits. | 27 | I am very motivated to start pACP discussions with families | 88% SA/A | 1.58 | .681 |
| 28 | I feel that starting pACP is part of my existing work process | 87% SA/A | 1.36 | .647 | |
| 29 | I am very uncomfortable discussing death, even with friends. |
25% SA/A 71% SD/D |
2.04 | 1.543 | |
| 30 | I am emotionally prepared to start pACP discussions with families | 93% SA/A | 1.59 | .915 | |
Abbreviations: A, agree; As, always; D, disagree; Mt, most of the time; pACP, paediatric advance care planning; SA, strongly agree; SD, strongly disagree.
3.3.1. Capability
There was a small statistically significant difference between palliative and non‐palliative professionals in the number of paediatric advance care planning discussions both ‘participated in’ and ‘initiated’ over the previous year and also in ‘developing their own initiation approach’. The number of professionals who felt adequately trained and the number of paediatric advance care planning discussions initiated in the past year was statistically significant (p = .028) (Data S3) when compared to those who indicated training not adequate.
3.3.2. Opportunity
Kruskal–Wallis test revealed a small statistical difference in the construct of opportunity between the clinical settings of hospital and/or community services and hospice (inpatient and at home) services (p = .007), between palliative and non‐palliative care professionals (p = .007.) and also between the numbers of paediatric advance care planning discussions initiated (p = . 022) (Data S3). These combined results implied that those working in palliative care in hospice community or inpatient settings indicated they had more opportunity than those not in these specialties or clinical areas. Those with more opportunity initiated a higher number of advance care plans.
3.3.3. Motivation
Kruskal–Wallis test identified no difference in the Motivation construct between medical and nursing professions (p = .658), clinical settings of acute care and hospice care (p = .252) nor those in palliative professions and other specialties (p = .202). A correlation was identified in the use of a paediatric advance care planning tool in initiation, with professionals not using a tool being more motivated (p = .042). The prerequisite of requiring the parent to indicate readiness was also statistically significant with those needing parents to indicate readiness more motivated (p = .041) (Data S3).
A total of 108 (77%) professionals responded to open text questions asking for initiation comments, resulting in 220+ statements. Statements were mapped to COM‐B constructs and identified as positive or negative. Positive comments on Motivation were identified most frequently (n = 88) with few negative comments identified (Table 5).
TABLE 5.
Examples of mapped COM‐B comments and perceived positivity/negativity
| Positive | Negative | |
|---|---|---|
| Capability | ‘I feel able to adapt to differing needs but am mindful’ (8) and ‘I have to be very adaptable’ (64) (oncology nurse specialists working in community and hospital) | ‘It can be hard to judge the best time to introduce this’ ([24] doctor consultant adult hospice) |
| Opportunity | ‘I am fortunate to have close working relationships with families which allows time for discussions on all aspects of care’ (Children's Hospice Community Nurse [37]) | ‘Normally above and beyond normal daily working’ (hospital‐based consultant [89]) |
| Motivation | ‘Having an honest, open well communicated plan helps the family and team’ ([126] oncology nurse specialist) | ‘I have had experience of consultants not wanting me to engage’ (Children's hospice nurse specialist [137]) |
3.4. Prerequisites perceived by respondents
When asked about their approach, respondents indicated that criteria had to be in place before initiation occurred. These included a rapport with the family, knowledge of family dynamics and an indication that the parents were ready for discussion. Less influentially, a consensus from professional colleagues and a definite prognosis were required (Table 6).
TABLE 6.
Prerequisites
| Strongly agree | Somewhat agree | Neither agree/disagree | Somewhat disagree | Strongly disagree | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | n | % | n | % | n | % | n | % | n | |
| Consensus of the health care team | 39.3 | 55 | 40 | 56 | 10 | 14 | 5.7 | 8 | 4.3 | 6 |
| Relationship/rapport with the family | 59.3 | 83 | 35 | 49 | 2.9 | 4 | 1.4 | 2 | .7 | 1 |
| Know the family dynamics | 55.7 | 78 | 37 | 52 | 5.7 | 8 | .7 | 1 | 0 | 0 |
| Indication of readiness from parents | 45.5 | 64 | 49 | 56 | 6.4 | 9 | 6.4 | 9 | 0 | 0 |
| Definite prognosis | 11.4 | 16 | 32.1 | 45 | 17.1 | 24 | 27.9 | 39 | 10.5 | 15 |
3.5. Reflection on last paediatric advance care planning initiation experience
Participants were asked to reflect on their last paediatric advance care planning initiation experience. Aspects were identified in their reflection such as wording, initiation stimulus, tools, protocols and timing.
3.5.1. Wording used
Analysis of the words used for initiation identified that intuitive conversations were held, and different approaches to opening the conversations were adopted (Table 7, for examples). Many professionals began with establishing the parents understanding of the severity of the stage of the disease and/or the child's status upon which to build advance care planning. Alternatively, against a backdrop of the child's deteriorating health or anticipated deterioration, some began by explaining paediatric advance care planning. Others framed the initiation by confirming deterioration, the non‐curative nature of illness or ineffectiveness of curative treatments and moved towards parents' opportunity to express their future wishes and hopes. Finally, an instinctive feeling of the parent being open to engage in such conversations provided a path upon which to frame and verbalize its introduction.
TABLE 7.
Words used in current clinical practice to initiate conversations about paediatric advance care planning
| Topic | Example conversation start | |
|---|---|---|
| 1 | Future planning, wishes and hopes | ‘I would like us to think about the care that you would like us to provide for (child's name) over the coming weeks’ (140) |
| I wish, I worry, I wonder—‘I wish that we will be able to find a treatable cause but I worry that will not be possible and I wonder what are your thoughts, feeling, worries, wishes …’ (65) | ||
| 2 | Explain paediatric advance care planning | ‘We have a plan which we could complete together which will detail all your wishes regarding all aspects of (child's name) … life’ (66) |
| 3 | Checking parent understanding of current condition | ‘What is your understanding of how … is now and what are your wishes should her condition deteriorate further?’ (114) |
| ‘Hi how is (child's name) … doing today?’ ‘How do you feel (Child's name) is?’ (25) | ||
| 4 | Actual and anticipated deterioration and symptom management | ‘I want to talk about what is best for (Child's name) in the event of him taking very unwell—what are your thoughts?’ (54) |
| ‘Would you like to have a discussion about what happens next time (child's name) … becomes really unwell?’ (59) | ||
| 5 | Parent initiation/cue acted upon | Mum raised issue as she was ready to discuss ACP. I asked her if she was thinking about choices for her child if he became unwell again and did she want to discuss these. (37) |
3.5.2. Initiation stimulus
When reflecting on the key stimulus for initiating the paediatric advance care planning conversation, deterioration in health was the main reason with communication (between professionals, parents, places of care and school), parent cues, diagnosis and paediatric intensive care unit admission the next most common reasons (Figure 1).
FIGURE 1.
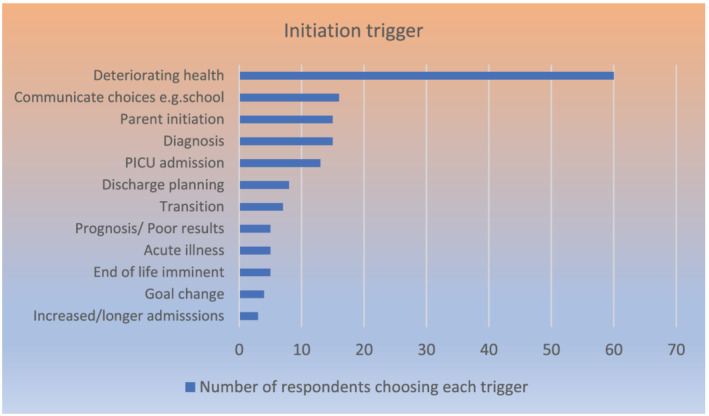
Key trigger for initiating paediatric advance care planning
3.6. Tools and protocols
Respondents were invited to name tools they used within their practice to initiate advance care planning (Data S4). The majority 65% (n = 91) reported no tool use, and for a third of respondents who used a tool, the most common used was the Child and Young Person's Advance Care Plan Collaborative documentation (CYPACP, 2018). Analysis indicated those not using a tool were more motivated than those using a tool and 74% reported they had no protocols in place to help them find the words to start these discussions.
3.7. Timing
When reflecting on their last initiation discussion, 37% (n = 51) of respondents (29 non‐palliative care and 22 palliative care) stated they would have preferred to initiate earlier 21/51 (41%).
4. DISCUSSION
This study is one of only few studies informed by health professionals that examine the initiation of ACP discussions in children. Starting these conversations late, mainly due to condition deterioration, is something that has been reported frequently in the literature (Basu & Swil, 2018; Durall et al., 2012; Sanderson et al., 2016). Findings suggest capability of engaging in initiation is based on experience and training. Those who felt adequately trained initiated more discussions; however, their style and approach were informed by experience. This emphasized the need for appropriate training as highlighted in past studies (Tatterton, 2018; Zhukovsky et al., 2013). This cohort differs from other studies as respondents in this study consisted of almost 59% professionals who had an identified role within children's palliative care. Arguably, many paediatric palliative professionals represented had generalist experience prior to focusing on palliative care, and 40% were not working in palliative care, a relatively recently recognized specialty in both UK and Ireland. Notwithstanding, there was still an indication of the importance of training required for initiation of these discussions.
Those working in palliative care settings, such as hospice, community and inpatient units, indicated that they had more opportunity for such discussions, and resultingly, a higher number of advance care discussions were initiated. The opportunity for palliative care professional to initiate discussions can only occur if they are integrated in the child's care in a timely manner. Non‐referral and delayed referral to paediatric palliative care services continue to be a concern (Kaye et al., 2018; Mitchell et al., 2020; Moynihan et al., 2021; Neuburg, 2021).
Physical opportunities such as having sufficient time and a facilitative work setting, combined with social opportunities such as having supportive co‐workers and peer‐observation, indicated higher initiation practices. Additional social opportunity aspects such as respondents' approach being influenced by families' cultural, religious and spiritual beliefs were similar to previous research (Basu & Swil, 2018; de Vos et al., 2011; Forbes et al., 2008; Mitchell et al., 2014). However, it is noteworthy the findings of this study indicated that one third of respondents still delayed initiation as they worried about family's emotional reaction.
Capability and Opportunity both impact Motivation and all influence Behaviour. Physical capability in the COM‐B model refers to having the physical strength, skill or stamina, in this case to initiate pACP discussions. This was not questioned as the behaviour itself requires no physical strength, skill or stamina beyond what would be normally required for health professionals for everyday work in the health professions. Physical responses to the stressful emotional situation may impact on their motivation to initiate, hence its inclusion in this aspect of the model. Reflective motivation responses indicated professionals believed they, not parents of ill children, held the responsibility for starting discussions, which echoes previous studies (Basu & Swil, 2018; Durall et al., 2012; Tsai, 2008).
This current study of ‘experienced’ professionals indicated that almost 90% believed they knew how and when paediatric advance care planning conversations should be started. This confidence in knowing how and when to start paediatric advance care planning conversations is not in keeping with previous studies (Forbes et al., 2008; Lotz et al., 2015).
Many automatic motivation responses indicated that respondents were emotionally prepared to engage in such discussions which contrasts with previous work (Basu & Swil, 2018; Lotz et al., 2015) although it is important to note that 25% in this study reported they were ‘uncomfortable discussing death’ even with friends. Previous research found that health professionals who were comfortable discussing death with colleagues were more comfortable initiating discussions with families (Harrison et al., 2014). This study found no difference between comfort levels of professional groups, whereas previous studies indicated that doctors were more comfortable with the initiation of advance care planning discussions (Harrison et al., 2014; Kruse et al., 2017). Existing research identified that professionals with more clinical experience, exposure and practice were more comfortable in initiation (Fahner et al., 2020; Forbes et al., 2008; Harrison et al., 2014; Kruse et al., 2017).
Respondents held the intrinsic belief (reflective motivation) that paediatric advance care plans were useful and necessary and should be advocated early and gradually in the disease trajectory, also supported by previous research (Fahner et al., 2020; Liben et al., 2014; Lotz et al., 2015, 2017; Tsai, 2008). This study found that, although respondents held this belief, initiation was impacted by a range of prerequisites. Similar to previous research these pre‐requisites included the need to attain professional consensus, an indication of parents readiness, knowledge of the family dynamics and rapport with families (Bradford et al., 2014; de Vos et al., 2011; Fahner et al., 2020; Harrop et al., 2018; Haynes et al., 2019; Jack et al., 2018; Mack & Joffe, 2014; Mitchell et al., 2014; Zaal‐Schuller et al., 2016). The need for professionals to have a rapport with families and know the family dynamics followed by an indication of readiness from families superseded the other prerequisites.
This study indicated that professionals working in palliative care in the community with adequate training initiated more advance care planning conversations, therefore implying that when this ‘perfect’ scenario is not available paediatric advance care planning discussions are less likely to be initiated. When it comes to initiation of paediatric advance care planning, the motivation to engage must be stronger than the motivation to avoid. Only one other study has identified motivation to engage with families as a requirement (Sidgwick et al., 2019).
The motivation to engage was often triggered by a physical deterioration in the child's health, similar to previous research (Fahner et al., 2020; Hiscock & Barclay, 2019; Kelly et al., 2018; Stark et al., 2008).
Findings indicated that initiation behaviour was not guided by tools or protocols; rather, it was unstandardized, individually led and guided by intuition and experience. The use of tools is reported to have several benefits such as earlier completion of advance care planning documentation, enhanced communication and facilitation of integration to electronic records (Audigé et al., 2020; Haynes et al., 2019; Kelly et al., 2018). Reasons for the lack of use in this study were not investigated; therefore, it is not clear if respondents were not aware of the range of tools available, chose not to use a tool or if the available tools did not provide initiation advice. The need for individuals to make and take initiation opportunities, or promptly refer to palliative professionals in a timely manner is evident.
4.1. Limitations
A number of surveys have reported on healthcare professionals experience of advance care planning in paediatrics (Fahner et al., 2020; Hilden et al., 2001); however, to our knowledge, this was the first study investigating initiation behaviour. The study has limitations, for example, the sample comprised of members of various children's palliative care organizations who responded to a request or an advertised invitation. Respondents were mainly composed of experienced professionals, and therefore, their views may not be representative of less experienced practitioners or non‐specialist palliative care professionals. As there are no data available from non‐responders, we cannot comment on the characteristics of this group although many may still be responsible for formative initiation of pACP or referring to paediatric palliative care. Results were based upon self‐reported measures, questioning the generalizability. The qualitative aspect of this study mainly consisted of categorizing the data.
5. CONCLUSION
The initiation of advance care planning is a multifaceted complex process requiring healthcare professionals to navigate uncertainty, barriers and facilitators. Whilst such conversations are supported in practice the reality is, they occur late in the trajectory both within children's palliative care and in other specialties and mirrors delayed referral to palliative care services. This has potential implications for the quality of care delivered and bereavement experience of the parent. Further research is required to identify what motivates a professional to want to initiate earlier rather than the need to initiate discussions because they perceive they have no alternative particularly from acute and non‐palliative services perspective. Identifying behaviours associated with avoidance or late initiation will assist in the development of targeted interventions most likely to impact the behaviour and with the greatest likelihood to lead to effective and established behaviour change.
CONFLICT OF INTEREST
The authors declare no competing interest.
ETHICS STATEMENT
Ethical approval for this study was obtained from Ulster University Research Ethics Filter Committee (1 July 2019).
FUNDING INFORMATION
This work was funded by the UK Department of Employment and Learning (DEL) awarded to the lead author to undertake this research as part of a PhD.
Supporting information
Data S1. Supporting Information
Data S2. Supporting Information
Data S3. Supporting Information
Data S4. Supporting Information
ACKNOWLEDGEMENTS
The authors would like to thank the health professionals who advised and provided data and to Dr. Lou Atkins for her expert advice. The author wishes to acknowledge funding received from Department for the Economy (DfE) postgraduate studentship programme which enabled the study, of which this paper reports on one phase.
Carr, K. , Hasson, F. , McIlfatrick, S. , & Downing, J. (2022). Initiation of paediatric advance care planning: Cross‐sectional survey of health professionals reported behaviour. Child: Care, Health and Development, 48(3), 423–434. 10.1111/cch.12943
Funding information UK Department of Employment and Learning (DEL); Department for the Economy (DfE)
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Andrews, D. , Nonnecke, B. , & Preece, J. (2003). Electronic survey methodology: A case study in reaching hard‐to‐involve internet users. International Journal of Human‐Computer Interaction, 16(2), 185–210. 10.1207/S15327590IJHC1602_04 [DOI] [Google Scholar]
- Audigé, M. , Gillam, L. , & Stark, Z. (2020). Treatment limitation and advance planning: Hospital‐wide audit of paediatric death. Journal of Paediatrics and Child Health., 56, 893–899. 10.1111/jpc.14771 [DOI] [PubMed] [Google Scholar]
- Basu, M. R. , Partin, L. , Revette, A. , Wolfe, J. , & DeCourcey, D. D. (2021). Clinician identified barriers and strategies for advance care planning in seriously ill pediatric patients. Journal of Pain and Symptom Management., 62, e100–e111. 10.1016/j.jpainsymman.2021.03.006 [DOI] [PubMed] [Google Scholar]
- Basu, S. , & Swil, K. (2018). Paediatric advance care planning: Physician experience and education in initiating difficult discussions. Journal of Paediatrics and Child Health, 54(5), 510–514. 10.1111/jpc.13818 [DOI] [PubMed] [Google Scholar]
- Blackford, J. , & Street, A. F. (2013). Facilitating advance care planning in community palliative care: Conversation starters across the client journey. International Journal of Palliative Nursing, 19(3), 132–139. 10.12968/ijpn.2013.19.3.132 [DOI] [PubMed] [Google Scholar]
- Bradford, N. , Herbert, A. , Mott, C. , Armfield, N. , Young, J. , & Smith, A. (2014). Components and principles of a pediatric palliative care consultation: Results of a Delphi study. Journal of Palliative Medicine, 17(11), 1206–1213. 10.1089/jpm.2014.0121 [DOI] [PubMed] [Google Scholar]
- Carr, K. , Hasson, F. , McIlfatrick, S. , & Downing, J. (2020). Factors associated with health professionals decision to initiate paediatric advance care planning: A systematic integrative review. Palliative Medicine., 35, 503–528. 10.1177/0269216320983197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Côté, A. J. , Payot, A. , & Gaucher, N. (2020). Paediatric palliative care in practice: Perspectives between acute and long‐term healthcare teams. Acta Paediatrica, 109(3), 613–619. 10.1111/apa.14969 [DOI] [PubMed] [Google Scholar]
- CYPACP . (2018) Guide to using the Child and Young Person's Advance care Plan v1.6 Child and Young Person's Advance Care Plan Collaborative. http://cypacp.uk/wp-content/uploads/2017/01/CYPACP-guide-Final-v1.-6.pdf. accessed May 2020
- de Vleminck, A. , Pardon, K. , Roelands, M. , Houttekier, D. , van den Block, L. , Vander Stichele, R. , & Deliens, L. (2015). Information preferences of the general population when faced with life‐limiting illness. European Journal of Public Health, 25(3), 532–538. 10.1093/eurpub/cku158 [DOI] [PubMed] [Google Scholar]
- de Vos, M. A. , van der Heide, A. , Maurice‐Stam, H. , Brouwer, O. F. , Plötz, F. B. , Schouten‐van Meeteren, A. Y. , Willems, D. L. , Heymans, H. S. , & Bos, A. P. (2011). The process of end‐of‐life decision‐making in pediatrics: A national survey in the Netherlands. Pediatrics, 127(4), e1004–e1012. 10.1542/peds.2010-2591 [DOI] [PubMed] [Google Scholar]
- DeCourcey, D. D. , Silverman, M. , Oladunjoye, A. , & Wolfe, J. (2019). Advance care planning and parent‐reported end‐of‐life outcomes in children, adolescents, and young adults with complex chronic conditions. Critical Care Medicine, 47(1), 101–108. 10.1097/CCM.0000000000003472 [DOI] [PubMed] [Google Scholar]
- Dillman, D. , Smyth, J. , & Christian, L. (2014). Internet, phone, mail and mixed‐mode surveys: The tailored design method (4th ed.). John Wiley. ISBN: 978‐1‐118‐45614‐9 [Google Scholar]
- DOHA . (2018) Advanced care planning Australia. Be open. Be ready. Be heard. Paediatric ACP. https://www.advancecareplanning.org.au/whats-on/event/2019/04/02/default-calendar/be-open-be-heard-and-be-ready
- Durall, A. , Zurakowski, D. , & Wolfe, J. (2012). Barriers to conducting advance care discussions for children with life‐threatening conditions. Pediatrics, 129(4), e975–e982. 10.1542/peds.2011-2695 [DOI] [PubMed] [Google Scholar]
- Ekberg, S. , Herbert, A. , Johns, K. , Tarrant, G. , Sansone, H. , Yates, P. , Danby, S. , & Bradford, N. K. (2020). Finding a way with words: Delphi study to develop a discussion prompt list for paediatric palliative care. Palliative Medicine, 34(3), 291–299. 10.1177/0269216319888988 [DOI] [PubMed] [Google Scholar]
- Fahner, J. C. , Rietjens, J. A. , van der Heide, A. , van Delden, J. J. , & Kars, M. C. (2020). Survey of paediatricians caring for children with life‐limiting conditions found that they were involved in advance care planning. Acta Paediatrica, 109(5), 1011–1018. 10.1111/apa.15061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes, T. , Goeman, E. , Stark, Z. , Hynson, J. , & Forrester, M. (2008). Discussing withdrawing and withholding of life‐sustaining medical treatment in a tertiary paediatric hospital: A survey of clinician attitudes and practices. Journal of Paediatrics and Child Health, 44(7–8), 392–398. 10.1111/j.1440-1754.2008.01351.x [DOI] [PubMed] [Google Scholar]
- Guo, Q. , Chochinov, H. M. , McClement, S. , Thompson, G. , & Hack, T. (2018). Development and evaluation of the Dignity Talk question framework for palliative patients and their families: A mixed‐methods study. Palliative Medicine, 32(1), 195–205. 10.1177/0269216317734696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison, J. , Evan, E. , Hughes, A. , Yazdani, S. , Federman, M. , & Harrison, R. (2014). Understanding communication among health care professionals regarding death and dying in pediatrics. Palliative & Supportive Care, 12(5), 387–392. 10.1017/S1478951513000229 [DOI] [PubMed] [Google Scholar]
- Harrop, E. J. , Boyce, K. , Beale, T. , & Brombley, K. (2018). Fifteen‐minute consultation: Developing an advance care plan in partnership with the child and family. Archives of Disease in Childhood‐Education and Practice, 103(6), 282–287. 10.1136/archdischild-2017-314430 [DOI] [PubMed] [Google Scholar]
- Haynes, S. , Dorsett, C. , & Wolff, T. (2019). Writing a good anticipatory care plan for a child with severe disability. Paediatrics and Child Health, 29(10), 441–447. 10.1016/j.paed.2019.07.005 [DOI] [Google Scholar]
- Hein, K. , Knochel, K. , Zaimovic, V. , Reimann, D. , Monz, A. , Heitkamp, N. , Borasio, G. D. , & Führer, M. (2020). Identifying key elements for paediatric advance care planning with parents, healthcare providers and stakeholders: A qualitative study. Palliative Medicine, 34(3), 300–308. 10.1177/0269216319900317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilden, J. M. , Emanuel, E. J. , Fairclough, D. L. , Link, M. P. , Foley, K. M. , Clarridge, B. C. , Schnipper, L. E. , & Mayer, R. J. (2001). Attitudes and practices among pediatric oncologists regarding end‐of‐life care: Results of the 1998 American Society of Clinical Oncology survey. Journal of Clinical Oncology, 19(1), 205–212. 10.1200/JCO.2001.19.1.205 [DOI] [PubMed] [Google Scholar]
- Hiscock, A. , & Barclay, S. (2019). ‘It's a hard conversation to have’. Healthcare professionals' views concerning advance care discussions with young people affected by life‐limiting neuromuscular diseases: An interview study. BMJ Supportive & Palliative Care, 9(1), e9–e9. 10.1136/bmjspcare-2017-001369 [DOI] [PubMed] [Google Scholar]
- IBM . (2017) Corp. Released 2017. IBM SPSS statistics for windows, version 25.0. Armonk, NY: IBM Corp.
- Jack, B. A. , Mitchell, T. K. , O'Brien, M. R. , Silverio, S. A. , & Knighting, K. (2018). A qualitative study of health care professionals' views and experiences of paediatric advance care planning. BMC Palliative Care, 17(1), 93. 10.1186/s12904-018-0347-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye, E. C. , Jerkins, J. , Gushue, C. A. , DeMarsh, S. , Sykes, A. , Lu, Z. , Snaman, J. M. , Blazin, L. , Johnson, L. M. , Levine, D. R. , & Morrison, R. R. (2018). Predictors of late palliative care referral in children with cancer. Journal of Pain and Symptom Management, 55(6), 1550–1556. 10.1016/j.jpainsymman.2018.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, J. , Ritchie, J. , Donovan, L. , Graham, C. , & Herbert, A. (2018). A retrospective review of resuscitation planning at a children's hospital. Children, 5(1), 9. 10.3390/children5010009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse, K. E. , Batten, J. , Constantine, M. L. , Kache, S. , & Magnus, D. (2017). Challenges to code status discussions for pediatric patients. PLoS ONE, 12(11), e0187375. 10.1371/journal.pone.0187375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liben, S. , Langner, R. , & Bluebond‐Langner, M. (2014). Pediatric palliative care in 2014: Much accomplished, much yet to be done. Journal of Palliative Care, 30, 311–316. 10.1177/082585971403000414 [DOI] [PubMed] [Google Scholar]
- Lord, S. , Moore, C. , Beatty, M. , Cohen, E. , Rapoport, A. , Hellmann, J. , Netten, K. , Amin, R. , & Orkin, J. (2020). Assessment of bereaved caregiver experiences of advance care planning for children with medical complexity. JAMA Network Open, 3(7), e2010337. 10.1001/jamanetworkopen.2020.10337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotz, J. D. , Daxer, M. , Jox, R. J. , Borasio, G. D. , & Fuhrer, M. (2017). “Hope for the best, prepare for the worst”: A qualitative interview study on parents' needs and fears in pediatric advance care planning. Palliative Medicine, 31(8), 764–771. 10.1177/0269216316679913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotz, J. D. , Jox, R. J. , Borasio, G. D. , & Fuhrer, M. (2015). Pediatric advance care planning from the perspective of health care professionals: A qualitative interview study. Palliative Medicine, 29, 212–222. 10.1177/0269216314552091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon, M. E. , Garvie, P. A. , D'Angelo, L. J. , Dallas, R. H. , Briggs, L. , Flynn, P. M. , Garcia, A. , Cheng, Y. I. , Wang, J. , & Adolescent Palliative Care Consortium . (2018). Advance care planning and HIV symptoms in adolescence. Pediatrics, 142(5), e20173869. 10.1542/peds.2017-3869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack, J. W. , & Joffe, S. (2014). Communicating about prognosis: Ethical responsibilities of pediatricians and parents. Pediatrics, 133(Supplement 1), S24–S30. 10.1542/peds.2013-3608E [DOI] [PubMed] [Google Scholar]
- McPeake, J. , Bateson, M. , & O'Neill, A. (2014). Electronic surveys: How to maximise success. Nurse Researcher, 21(3), 24–26. 10.7748/nr2014.01.21.3.24.e1205 [DOI] [PubMed] [Google Scholar]
- Michie, S. , Atkins, L. , & West, R. (2014). The behaviour change wheel. A guide to designing interventions (1st ed.) (pp. 1003–1010). Silverback Publishing. ISBN 978‐1‐291‐84605‐8 [Google Scholar]
- Mitchell, S. , Plunkett, A. , & Dale, J. (2014). Use of formal advance care planning documents: A national survey of UK Paediatric intensive Care units. Archives of Disease in Childhood, 99(4), 327–330. 10.1136/archdischild-2013-304463 [DOI] [PubMed] [Google Scholar]
- Mitchell, S. , Slowther, A. M. , Coad, J. , & Dale, J. (2020). Experiences of healthcare, including palliative care, of children with life‐limiting and life‐threatening conditions and their families: A longitudinal qualitative investigation. Archives of Disease in Childhood., 106, 570–576. 10.1136/archdischild-2020-320189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moynihan, K. M. , Heith, C. S. , Snaman, J. M. , Smith‐Parrish, M. , Bakas, A. , Ge, S. , Cerqueira, A. V. , Bailey, V. , Beke, D. , Wolfe, J. , & Morell, E. (2021). Palliative Care referrals in cardiac disease. Pediatrics, 147, e2020018580. 10.1542/peds.2020-018580 [DOI] [PubMed] [Google Scholar]
- Neuburg, L. (2021). Early initiation of pediatric palliative care. Journal of Pediatric Health Care, 35(1), 114–119. 10.1016/j.pedhc.2020.05.006 [DOI] [PubMed] [Google Scholar]
- NICE . (2016) End of life care for infants, children and young people with life‐limiting conditions: planning and management. NICE guideline [NG61]Published date: 07 December 2016 Last updated: 25 July 2019 https://www.nice.org.uk/guidance/ng61
- Norals, T. E. , & Smith, T. J. (2015). Advance care planning discussions: Why they should happen, why they don't, and how we can facilitate the process. Oncology, 29(8), 567–571. https://www.cancernetwork.com/view/advance-care-planning-discussions-why-they-should-happen-why-they-dont-and-how-we-can-facilitate [PubMed] [Google Scholar]
- Pallant, J. (2016). SPSS survival manual: A step by step guide to data analysis using SPSS. McGraw Hill Education. http://dspace.uniten.edu.my/jspui/handle/123456789/17829 [Google Scholar]
- Raosoft . (2004) Raosoft sample size calculator. Raosoft. Available at: http://www.raosoft.com/samplesize.html [Accessed 16th April 2019].
- Rietjens, J. A. , Sudore, R. L. , Connolly, M. , van Delden, J. J. , Drickamer, M. A. , Droger, M. , van der Heide, A. , Heyland, D. K. , Houttekier, D. , Janssen, D. J. , & Orsi, L. (2017). Definition and recommendations for advance care planning: An international consensus supported by the European Association for Palliative Care. The Lancet Oncology, 18(9), e543–e551. 10.1016/S1470-2045(17)30582-X [DOI] [PubMed] [Google Scholar]
- Rodenbach, R. A. , Brandes, K. , Fiscella, K. , Kravitz, R. L. , Butow, P. N. , Walczak, A. , Duberstein, P. R. , Sullivan, P. , Hoh, B. , Xing, G. , Plumb, S. , Epstein, R. M. , & Xing, G. (2017). Promoting end‐of‐life discussions in advanced cancer: Effects of patient coaching and question prompt lists. Journal of Clinical Oncology, 35(8), 842–851. 10.1200/JCO.2016.68.5651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson, A. , Hall, A. M. , & Wolfe, J. (2016). Advance Care discussions: Pediatric clinician preparedness and practices. Journal of Pain & Symptom Management, 51(3), 520–528. 10.1016/j.jpainsymman.2015.10.014 [DOI] [PubMed] [Google Scholar]
- Sidgwick, P. , Fraser, J. , Fortune, P. M. , & McCulloch, R. (2019). Parallel planning and the paediatric critical care patient. Archives of Disease in Childhood, 104, 994–997. 10.1136/archdischild-2018-315222 [DOI] [PubMed] [Google Scholar]
- Stark, Z. , Hynson, J. , & Forrester, M. (2008). Discussing withholding and withdrawing of life‐sustaining medical treatment in paediatric inpatients: Audit of current practice. Journal of Paediatrics and Child Health, 44(7–8), 399–403. 10.1111/j.1440-1754.2008.01352.x [DOI] [PubMed] [Google Scholar]
- STROBE . (2007) STrengthening the Reporting of OBservational studies in Epidemiology. https://www.strobe-statement.org/index.php?id=available-checklists
- Tatterton, M. J. (2018). Anticipatory prescribing and advance care planning in palliative care for children and young people. Nurse Prescribing, 16(5), 228–233. 10.12968/npre.2018.16.5.228 [DOI] [Google Scholar]
- Together for Short Lives . (2017) Together for short lives report to NHS England. A national overview of the readiness of the children's palliative care sector to implement the NICE end of life care for infants, children and young people: Planning and management guideline. https://www.nice.org.uk/Media/Default/sharedlearning/NICE%20report%20final.pdf
- Tsai E. Advance care planning for paediatric patients. Paediatrics & Child Health 2008; 13: 791–796 h 10.1093/pch/13.9.791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Breemen, C. , Johnston, J. , Carwana, M. , & Louie, P. (2020). Serious illness conversations in pediatrics: A case review. Children, 7(8), 102. 10.3390/children7080102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh, J. C. , Cheng, M. J. , Chung, C. H. , & Smith, T. J. (2014). Using a question prompt list as a communication aid in advanced cancer care. Journal of Oncology Practice, 10(3), e137–e141. 10.1200/JOP.2013.001295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaal‐Schuller, I. H. , Willems, D. L. , Ewals, F. V. , van Goudoever, J. B. , & de Vos, M. A. (2016). How parents and physicians experience end‐of‐life decision‐making for children with profound intellectual and multiple disabilities. Research in Developmental Disabilities, 59, 283–293. 10.1016/j.ridd.2016.09.012 [DOI] [PubMed] [Google Scholar]
- Zadeh, S. , & Wiener, L. (2015). Opening end‐of‐life discussions: How to introduce voicing My CHOiCES™, an advance care planning guide for adolescents and young adults. Palliative & Supportive Care, 13(3), 591–599. 10.1017/S1478951514000054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhukovsky, D. , Robert, R. , & Levetown, M. (2013). Advance care planning with children and adolescents: It's a choice to make!(SA522). Journal of Pain and Symptom Management, 45(2), 407–408. 10.1016/j.jpainsymman.2012.10.267 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting Information
Data S2. Supporting Information
Data S3. Supporting Information
Data S4. Supporting Information
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


